Abstract
Objectives:
The circadian system is the main regulator of almost all human physiological processes. The aim of this study was to assess sleep in the working population, in relation to the share of remote working.
Material and Methods:
An online survey was conducted among students and staff representing 3 universities in Łódź, Poland (N = 1209). The participants were divided into 3 groups according to the percentage of time they worked remotely. Group I consisted of respondents performing tasks remotely for ≤45% of their working time; group II included respondents performing their duties remotely for >45–75% of their working time, and group III included those working >75% of their time remotely.
Results:
In the study, the authors found the association between the length of time spent on a computer, the percentage of time working remotely, and the occurrence of physical symptoms and the prevalence of sleep disorders. The most significant difference between working days and days off in terms of the mid-point of sleep (1.5 h) was observed in group I, where there was the greatest variability in the form of work performance. The participants who worked most of their time remotely (group III) shifted their bedtime to midnight, both on working days and on days off.
Conclusions:
The study highlights that increased remote computer use leads to a shift in sleeping patterns towards midnight. The participants with later midpoint of sleep hours were found to have a higher incidence of sleep disorders. The prevalence of sleep disorders was significantly impacted by prolonged mobile phone use before bedtime and long hours of computer use. Thus, limiting both the time spent in front of a computer and the use of mobile phones before bedtime is recommended.
Keywords: sleep disorders, computer, chronotype, remote work, circadian system, external synchronizers of sleep
INTRODUCTION
The circadian system is the main regulator of almost all human physiological processes [1]. In addition to changes in daylight intensity, air temperature, rainfall and other environmental factors also change cyclically, which has a major impact on living organisms. In order to adapt to daily recurring environmental changes, cyclical behavior and physiology changes occur, which include sleep and wakefulness cycles, as well as a number of less visible processes in neurological, metabolic, endocrine, cardiovascular and immune functions. Circadian rhythmicity is created endogenously by genetically encoded molecular clocks, the components of which work together to generate cyclical changes in their own activity, at a frequency of approx. 24 h. Throughout the body, molecular clocks transmit temporal control to organ and tissue functions by regulating the corresponding downstream programs. Synchronization between various circadian oscillators and resonance with the daylight are largely enabled by the neural pacemaker, which responds directly to certain environmental cues and is able to transmit internal representations of daytime to the whole body [2,3].
An important function of the biological clock is to anticipate changes in the environment during the day, and to prepare both the organs and whole systems for activity or sleep, before there is even a change in the intensity of the external environment. Thus, by the time we wake up in the morning and leave bed, our body is already prepared for daytime activity. In contrast, in the evening, the clock inhibits processes related to activity while activating those related to sleep, such as lowering body temperature and inducing the production of the sleep hormone – melatonin. The melatonin level is the highest at night (2:00–4:00 a.m.) and the lowest during the day. The duration and quality of human sleep varies by age as well as by environmental and lifestyle related factors. It should last about 8 h. In addition to its restorative functions, sleep also ensures the adequate hormonal and immunological regulation, consolidation of cognitive functions, and central control of autonomic processes.
Sleep and circadian rhythm disturbances (SCRDs) are a common feature of today's society. Studies in groups of shift workers have shown that SCRDs can lead to cognitive impairment, metabolic syndrome, and psychiatric disorders, including depression. They also increase the risk of cancer, particularly breast and colorectal cancer [4–6]. In addition, disruptions of the circadian rhythm have been shown to bring a number of negative effects on physiological rhythms, in the form of altered expressions of certain genes, changes in enzyme activity, endocrine disruption and gastrointestinal, cardiovascular, as well as neurological disorders [7–9].
Social jetlag is one of the causes of circadian disturbances. This term refers to the difference in sleep time (bedtime and wake-up time) between working days and days off [10,11]. On days off, people usually wake up at a time of their own choice, while on weekdays they have to wake up in line with the time they start work or school. In industrialized countries, >70% of the population has more than 1 h of jetlag, most often caused by the time required to get to work. To help determine the impact of sleep schedules on possible disorders, the concept of mid-point of sleep was introduced [11,12]. Social jetlag and the consequent disruption of the circadian rhythm are associated with physical and mental health problems, such as obesity, metabolic diseases, cancer and mental disorders [7–9,13–17]. The multiplicity and severity of negative health effects will depend, inter alia, on a person's chronotype [18,19]. As is well known, some people function and work more effectively in the morning while others prefer later hours, thus the terms “larks” and “owls” are frequently used to describe these 2 groups, respectively [20,21].
Since the COVID-19 epidemic in 2020, remote working has become more popular. It originally fulfilled its role to reduce the epidemic risk, but once introduced into legislation, it has remained a possible form of work [22]. The health effects of remote working can be considered in both positive and negative aspects. Remote working eliminates commuting time and allows for flexible working hours, thus reducing the phenomenon of social jetlag. However, given that, in most cases, it is not possible to fully carry out work in a remote form, a question arises whether the variability of sleep patterns depends on the proportion of time spent working remotely, i.e., the hybrid form. Therefore, the aim of this study was to assess the duration and quality of sleep in the working population, in relation to the share of remote working.
MATERIAL AND METHODS
Population
An online survey was conducted among students and staff representing 3 universities in Łódź, Poland. They were asked to answer questions about the period of October 2020–June 2021, during which the university manage ment maintained a remote form of teaching/working. The inclusion criteria for the current analysis were: being a student or an employee of the university, and providing responses to the survey questions regarding computer use and sleep. Responses from 1209 people were eventually included in the analysis. The survey participants in the study were divided into 3 groups according to the percentage of time they worked remotely, based on the responses to the question: “What percentage of your working/learning time was taken up remotely during the period concerned?” The first group (group I) consisted of respondents performing tasks remotely for <45% of their working time; the second group (group II) included respondents performing their duties remotely for >45–75% of their working time, and the third group (group III) included those working >75% of their working time remotely. There were no differences in age between the groups.
The study was approved by the Research Ethics Committee of the Nofer Institute of Occupational Medicine in Łódź (Resolution No. 1/2021 of December 23, 2021).
Questionnaire
The full methodology of the study was described in previous articles [23,24]. The questionnaire included demographic questions characterizing the study population, the time of computer use, as well as questions regarding sleep distribution and quality, the type of activities performed before sleep, symptoms of sleep disorders, and taking sleep medications. It also covered physical symptoms, including musculoskeletal disorders, stress and headaches. Based on the data on bedtime and sleep length, the mid-sleep hour (or the mid-point of sleep) was calculated for working days and days off.
Statistical analyses
Baseline analyses were carried out taking into account the distribution of data which determined the follow-up. For general interdependencies, χ2 tests were used. For interval data, an analysis of variance was performed using the Brownian-Forsythe test, and for the remaining data, analyses were performed using the Kruskal-Wallis test. This was followed by analyses with the ANOVA test and the Mann-Whitney U test.
RESULTS
Demographic data are shown in Table 1. Group I performing tasks/work remotely for <45% of their time included 276 people with the age (M±SD) of 34.1±12.5 years. Group II working >45%–75% of their time remotely was composed of 457 people with the age (M±SD) of 29.8±13.4 years. Finally, 476 people were included in group III (>75% of the working time performed remotely) and their age (M±SD) was 26.6±10.3 years. In all these groups, women accounted for about 70% of the population.
Table 1.
Demographic information of the survey participants – university employees and students in Łódź, Poland, during the COVID-19 pandemic (June 2021)
| Variable | Participants (N = 1209) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| group I (N = 276) | group II (N = 457) | group III (N = 476) | |||||||
| n | M±SD | min-max | n | M±SD | min.-max | n | M±SD | min.-max | |
| Sex | |||||||||
| female | 203 | 334 | 328 | ||||||
| male | 73 | 123 | 148 | ||||||
| Age [years] | 34.09±12.45 | 19.00–63.00 | 29.84±13.40 | 19.00–68.00 | 26.57±10.27 | 20.00–67.00 | |||
| Height [cm] | 169.76±7.90 | 152.00–190.00 | 170.06±8.45 | 152.00–195.00 | 170.76±8.44 | 150.00–197.00 | |||
| Body weight [kg] | 69.70±14.82 | 41.00–125.00 | 68.75±14.97 | 41.50–123.00 | 69.29±15.85 | 39.00–150.00 | |||
Group I – remote working time ≤45%; group II – remote working time >45–75%; group III – remote working time >75%.
The distribution of the mid-point of sleep across the study population was age-dependent (Figure 1). Group I exhibited the largest differences between working days and days off, in terms of the mid-point of sleep (Table 2). The median time of falling asleep in group III was midnight, regardless of whether it was a day off or a working day; however, in this group, the participants slept 2 h longer on weekends.
Figure 1.
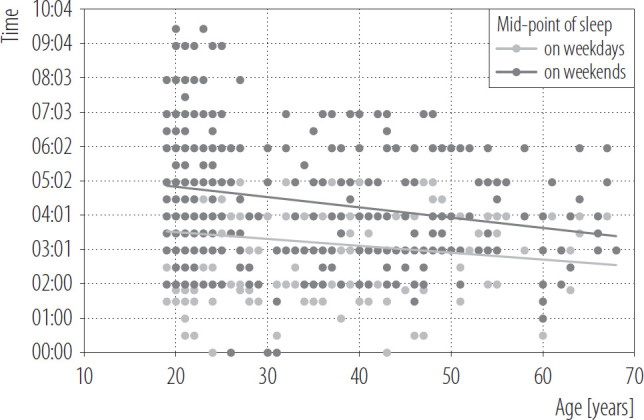
Distribution of mid-point of sleep hours on weekdays and weekends in the general study population – university employees and students Łódź, Poland, during the COVID-19 pandemic (June 2021)
Table 2.
Distribution of sleep parameters in the groups divided by the length of time spent working remotely – university employees and students in Łódź, Poland, October 2020–June 2021
| Variable | Participants (N = 1209) | |||||
|---|---|---|---|---|---|---|
| group I (N = 276) | group II (N = 457) | group III (N = 476) | ||||
| weekdays | weekends | weekdays | weekends | weekdays | weekends | |
| Falling asleep hour (Me) | 23:00 | 23:50 | 23:30 | 0:00 | 0:00 | 0:00 |
| Mid-point of sleep hour | 2:30 | 4:00 | 3:00 | 4:00 | 3:30 | 4:30 |
| Wake up time (Me) | 6:00 | 8:00 | 6:30 | 8:00 | 7:00 | 9:00 |
| Sleep time [h] | 7 | 8 | 7 | 8 | 7 | 9 |
Group I – remote working time ≤45%; group II – remote working time >45–75%; group III – remote working time >75%.
Table 3 presents the data and analysis of selected variables in the groups divided according to the share of remote work. There were some significant differences in the frequency of falling asleep after midnight on working days (p < 0.001) between group I (30%) and group II (46%), and between group I and group III (53%), using the Mann-Whitney U test. The percentage of people in each group falling asleep after midnight on days off was even higher (Table 3). It has to be acknowledged that the length of sleep on working days was significantly different, depending on the time of remote working (p = 0.001, ANOVA). On days off, the average sleep duration increased to >8 h, with differences between groups I and III (p < 0.001), and groups II and III (p = 0.002). The participants who went to bed after midnight were more likely to suffer from sleep disorders (p < 0.0001), as revealed by the Mann-Whitney U test.
Table 3.
Analysis of selected variables depending on the time of remote working among university employees and students in Łódź, Poland, October 2020–June 2021
| Variable | Participants (N = 1209) | p between groups | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| group I (N = 276) | group II (N = 457) | group III (N = 476) | p | I/II | II/III | I/III | ||||
| M±SD | % | M±SD | % | M±SD | % | |||||
| Time of computer use [h] | ||||||||||
| per weekday | 6.72±2.88 | 7.38±2.75 | 8.23±3.03 | <0.001 | 0.011 | <0.001 | <0.001 | |||
| per weekend day | 3.93±2.51 | 4.52±2.75 | 4.84±2.86 | <0.001 | 0.018 | 0.001 | ||||
| per weekday for non-occupational reasons | 2.62±1.96 | 2.84±1.85 | 3.07±1.99 | 0.008 | 0.009 | |||||
| total | 9.35 ±3.31 | 10.20±3.38 | 11.28±3.39 | <0.001 | 0.004 | <0.001 | <0.001 | |||
| Time of remote working followed by an active break [min] | 68.40±54.14 | 78.61 ±55.22 | 84.49±54.14 | 0.024 | <0.001 | |||||
| Breaks in less than every 60 min | 28 | 40 | 49 | <0.001 | 0.035 | <0.001 | ||||
| Health problems | ||||||||||
| prevalence of MSD complaints | 73 | 78 | 81 | |||||||
| MSD complaint severity (0-10 VAS) | 3.14±2.99 | 3.62±2.77 | 4.16±2.83 | <0.001 | 0.014 | <0.001 | ||||
| at least moderate stress level | 82 | 88 | 84 | |||||||
| headaches | ||||||||||
| presence | 66 | 75 | 79 | |||||||
| seventy (0-10 VAS) | 3.25±3.10 | 3.50±2.69 | 4.83±5.39 | <0.001 | 0.008 | |||||
| Falling asleep after midnight | ||||||||||
| on weekdays | 30 | 46 | 53 | <0.001 | 0.001 | <0.001 | ||||
| on weekend days | 49 | 66 | 67 | <0.001 | <0.001 | |||||
| Sleep time [h] | ||||||||||
| per weekday | 7.00±1.27 | 6.77±1.41 | 7.07±1.28 | 0.001 | 0.002 | |||||
| per weekend day | 8.20±1.56 | 8.41 ±1.60 | 8.75±1.38 | <0.001 | 0.002 | <0.001 | ||||
| Sleep disorders | 46 | 55 | 54 | 0.047 | ||||||
| difficulty falling asleep | 34 | 38 | 43 | 0.047 | ||||||
| waking up too early | 18 | 16 | 14 | |||||||
| waking up several times during sleep and having problems | 29 | 26 | 24 | |||||||
| falling asleep again | ||||||||||
| restless sleep (excessive activity) | 14 | 13 | 12 | |||||||
| feeling sleepless when getting out of bed | 24 | 35 | 34 | 0.008 | ||||||
| drowsiness during the day | 26 | 33 | 37 | 0.015 | ||||||
| loud snoring during sleep | 3 | 2 | 4 | |||||||
| increased sweating | 3 | 4 | 6 | |||||||
| shortness of breath, choking during sleep | 0 | 0 | 3 | <0.001 | ||||||
| morning fatigue | 16 | 29 | 29 | <0.001 | 0.009 | 0.009 | ||||
| morning headaches | 4 | 7 | 13 | <0.001 | ||||||
| Reasons for sleep disorders | ||||||||||
| sickness | 12 | 7 | 7 | |||||||
| environmental noise | 5 | 7 | 6 | |||||||
| problems at work/study | 16 | 21 | 22 | |||||||
| shift work or night work | 4 | 6 | 6 | |||||||
| stress | 36 | 46 | 42 | 0.032 | ||||||
| working/learning remotely | 18 | 28 | 32 | <0.001 | 0.006 | |||||
| Activities before bedtime | ||||||||||
| reading | 22 | 18 | 10 | <0.001 | 0.015 | |||||
| watching TV | 20 | 10 | 9 | <0.001 | 0.033 | |||||
| computer, laptop, tablet use | 14 | 16 | 24 | <0.001 | ||||||
| mobile phone use | 39 | 52 | 57 | <0.001 | 0.008 | <0.001 | ||||
| Sleeping medication | ||||||||||
| never or occasionally | 76 | 81 | 88 | 0.021 | ||||||
| sometimes | 18 | 16 | 12 | 0.044 | ||||||
| often | 0 | 0 | 0 | |||||||
| very often or always | 6 | 4 | 0 | <0.001 | ||||||
MSD – musculoskeletal disorders; VAS – Visual Analogue Scale.
The table includes only values of p ≤ 0.05.
Group I – remote working time ≤45%; group II – remote working time >45–75%; group III – remote working time >75%.
Sleep disorders occurred to a similar extent in all study groups, with differences being on the borderline of statistical significance (p = 0.05). The most common sleep disorders in group I included difficulty falling asleep, waking up several times during sleep and having problems falling back asleep, daytime sleepiness, and feeling sleepless after getting out of bed. Group II had the highest incidence of difficulty falling asleep, feeling sleep deprived after getting out of bed, daytime sleepiness, morning tiredness, and waking up several times during sleep and having problems falling back asleep. Difficulty falling asleep also accounted for the highest percentage of reported symptoms in group III. Those who went to bed after midnight were more likely to feel sleepless after getting out of bed and to experience daytime sleepiness, compared to those who went to bed before midnight (p = 0.001), as revealed by the Kruskal-Wallis test.
The most frequently reported causes of sleep disorders in all groups were stress (group I – 36%, group II – 46%, group III – 42%) and remote work (group I – 18%, group II – 28%, group III – 32%). Activities performed before sleep, such as using a mobile phone, had a significant impact on the occurrence of sleep disturbances (p = 0.002). The percentage of sleep medication users was the highest in group I (24%).
The number of hours spend on a computer was significantly associated with the number of sleep disturbances (p < 0.001). Significant differences were found in the number of hours of computer use on weekdays and weekends (p < 0.001), and on working days for non-occupational reasons (p = 0.008). The sum of hours of computer use for occupational and non-occupational reasons was significantly higher in group III (p < 0.001), compared to other groups, amounting to 11.3 h (SD = 3.4). There were no significant differences in the occurrence of musculoskeletal symptoms between the studied groups (Table 3). However, the severity of musculoskeletal symptoms was significantly higher in group III (p < 0.001, ANOVA). The lowest level of complaints was recorded in group I, with M±SD of 3.1±3.0 pts. All groups had a very high percentage of people experiencing at least medium levels of stress. Again, group III had the highest percentage of participants experiencing headaches (79%), and the severity of headaches was significantly higher in that group, compared to group I (p = 0.008). The increase in the prevalence of headaches (p = 0.001) and above-moderate levels of stress (p < 0.001) was directly proportionally greater in those experiencing sleep disorders, for the general population.
DISCUSSION
In this study, the authors found the association between the prevalence of sleep disorders and the amount of time spent on a computer, the percentage of time working remotely, and the occurrence of physical symptoms. Based on the International Classification of Sleep Disorders [9], which includes disorders of the circadian rhythm, such as delayed sleep phase syndrome, accelerated sleep phase syndrome or irregular sleep-wake rhythm, it is important to emphasize the significance of maintaining the level and frequency of the sleep-wake rhythm.
In this study, a high degree of variability was revealed as regards the hours of falling asleep in the group of people working remotely for <45% of their working time. Additionally, in this group, the waking phase was prolonged on days off. The phenomenon of sleep procrastination is related to attempting to make the most of one's free time, i.e., trying to catch up on household duties, hobbies or work backlogs. All these can cause social jetlag, the effects of which are seen mostly on the day after a night not fully slept, when the next day's waking up time is early. The more frequent changes in the regularity of sleep and wakefulness periods, the greater the likelihood of disruption of the circadian rhythm, and the consequent disruption of the physiological processes.
Sleep duration in the study groups was 7–8 h, which should ensure optimal regeneration of the organism adequate to the participants' age. Although the participants slept for quite a long time, the sleep disturbances they reported indicated a lack of sleep continuity. The most common sleep disorders included difficulty falling asleep, waking up several times during sleep and problems falling asleep again, daytime sleepiness, and feeling sleepy after waking up. At the same time, these are the symptoms that, when revealing themselves 3 times a week for more than a month, constitute the criteria for the diagnosis of insomnia according to the International Classification of Sleep Disorders.
The mid-point of sleep is a kind of exponent of the chronotype of a person, when maintained on a continuous basis. The accumulation of the so-called sleep debt due to daily activities on working days is suggested by the results of studies conducted to date. The exception is the very early chronotype, for which the mid-point of sleep is the earliest [11,12]. It is worth noting that the mid-point of sleep is age-dependent. Similarly, in this study, young people were characterized by an evening chronotype, which was associated with fatigue perceived later. Changing external and internal environmental conditions affect the regulation of the biological clock and, therefore, age-dependent changes in the chronotype. In the study, the authors found the most significant difference between working days and days off in terms of the mid-point of sleep (1.5 h) in group I, where there was the greatest variability in the form of work performance.
People working most of their working hours remotely shifted their bedtime to midnight, both on working days and on days off. This resulted in a late mid-point of sleep, which might then affect the time of peak melatonin concentration in the blood. However, new scientific evidence suggests that not all individuals with the clinical criteria for a delayed sleep-wake phase actually have a delayed circadian melatonin phase [25,26]. Exposure to light is an extremely important element in regulating the circadian rhythm. The staggered bedtime and the prolonged use of computer screens emitting 380–500 nm of blue light may constitute additional factors contributing to the occurrence of circadian rhythm disturbances, through excessive stimulation of intrinsically photosensitive retinal ganglion cells (ipRGc) [27,28]. It is worth noting that if these factors are related to the evening chronotype, it may prove that workers are more efficient in avoiding negative health consequences. Therefore, further research is needed, taking into account the distribution of melatonin concentrations in the blood of remote workers.
In the study groups, the external synchronizer of sleep was the time of computer use, which was very prolonged on working days. The authors found the association between the length of time working remotely and the frequency of sleep disorders. The observed correlation was due to the time spent using the computer for both occupational and non-occupational reasons, with computer use for non-occupational reasons acting as a contributory factor. Lim et al. [29] also indicated an increase in the prevalence of sleep disorders resulting from the number of hours of remote working. Other authors attributed the increase in remote working hours to a combination of work and other daily life activities intermingled into working hours [30–32].
The length of computer use also influenced a higher percentage of at least medium levels of stress, which may have been due to the specific situation in which the respondents found themselves. As the occurrence of migraine headaches requires specific clinical differentiation, the authors were unable to draw reliable conclusions as to whether the occurrence and severity of migraine headaches were related to remote working or to high levels of stress. However, it seems that the headaches reported by the respondents could be related to long hours spent in front of the computer and were probably tension-type headaches. Another consequence of longer hours spent in front of the computer, combined with less frequent breaks, was an increase in the severity of musculoskeletal complaints [23,24,30,31]. It is also worth emphasizing that an additional reason for the occurrence of the above-discussed problems are inadequate, in terms of ergonomics, home workstations [23,33,34].
When working remotely, people tend to use their computers longer than when working at a stationary work-place, because all work-related activities, as well as contacts with colleagues, clients, etc., have to be carried out using the computer. This research indicates that the time spent using the computer for non-occupational reasons has also increased.
It should be taken into account that the study was conducted during the pandemic period, which entailed limited interpersonal contacts – hence social contacts, going to the cinema, etc. were replaced by the computer. Since there was no need to get up early during the day (one of the assets of remote work), computer use shifted to evening hours, resulting in late bedtime among those who declared the highest proportion of remote work in the period covered by the survey. Increased computer use had its consequences in terms of musculoskeletal disorders, headaches, and stress. Shifting bedtime on working days due to remote work reduced the difference in the mid-point of sleep between working days and days off, which is an indicator of reduced social jetlag. However, it would be more beneficial to shift the time of sleep on either working days or weekends to hours before midnight.
The strength of the study is related to a large group of participants and an extensive questionnaire allowing numerous analyses.
Taking into account the cross-sectional nature of the study, the major limitation of the study was the use of a retrospective format with excessively broad questions, thus hindering the clarity of the overall result interpretation. Further research is needed to determine the cause of sleep difficulties after using a mobile phone before going to bed. Educational activities are required to promote certain pre-sleep habits for maintaining good health. Limiting both the time spent on a computer and the use of mobile phones before bedtime is recommended.
CONCLUSIONS
The study highlights that increased remote computer use leads to a shift in sleeping patterns towards midnight. The participants with later mid-point of sleep hours were found to have a higher incidence of sleep disorders. The prevalence of sleep disorders was significantly impacted by prolonged mobile phone use before bedtime and long hours of computer use.
Footnotes
Funding: this research was supported by the Minister of Health under the National Health Program 2021–2025 (grant No. 6/16/85195/NPZ/2021/312/1196 entitled “Monitorowanie zagrożeń fizycznych, chemicznych i biologicznych w miejscu pracy. Prowadzenie monitoringu oceniającego ekspozycję na związki chemiczne w środowisku pracy i służby żołnierzy zawodowych i funkcjonariuszy oraz zamieszkania,” grant manager: Prof. Marta Wiszniewska).
Author contributions
Research concept: Magdalena Janc, Teresa Makowiec-Dabrowska
Research methodology: Magdalena Janc, Teresa Makowiec-Dabrowska
Collecting material: Magdalena Janc, Zbigniew Jozwiak
Statistical analysis: Magdalena Janc
Interpretation of results: Magdalena Janc, Teresa Makowiec-Dabrowska, Agnieszka Jankowska, Joanna Jurewicz, Kinga Polanska
References: Magdalena Janc, Agnieszka Jankowska
REFERENCES
- 1.Ko CH, Takahashi JS. Molecular components of the mammalian circadian clock. Hum Mol Genet. 2006;15(2): R271–7. 10.1093/hmg/dd1207. [DOI] [PubMed] [Google Scholar]
- 2.Klarsfeld A, Birman S, Rouyer F. [Nobel time for the circadian clock – Nobel Prize in Medicine 2017: Jeffrey C. Hall, Michael Rosbash and Michael W. Young]. Med Sci (Paris). 2018;34(5):480–484. 10.1051/medsci/20183405023.French. [DOI] [PubMed] [Google Scholar]
- 3.Moore RY. Suprachiasmatic nucleus in sleep-wake regulation. Sleep Med. 2007;8(Suppl 3):27–33. 10.1016/j.sleep.2007.10.003. [DOI] [PubMed] [Google Scholar]
- 4.Arendt J. Shift work: coping with the biological clock. Occup Med (Lond). 2010;60(1):10–20. 10.1093/occmed/kqp162. [DOI] [PubMed] [Google Scholar]
- 5.Wulff K, Gatti S, Wettstein JG, Foster RG. Sleep and circadian rhythm disruption in psychiatric and neurodegenerative disease. Nat Rev Neurosci. 2010;11(8):589–99. 10.1038/nrn2868. [DOI] [PubMed] [Google Scholar]
- 6.Scott J, Etain B, Miklowitz D, Crouse JJ, Carpenter J, et al. A systematic review and meta-analysis of sleep and circadian rhythms disturbances in individuals at high-risk of developing or with early onset of bipolar disorders. Neurosci Biobehav Rev. 2022;135:104585. 10.1016/j.neubiorev.2022.104585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jagannath A, Taylor L, Wakaf Z, Vasudevan SR, Foster RG. The genetics of circadian rhythms, sleep and health. Hum Mol Genet. 2017;26(R2):R128–38. 10.1093/hmg/ddx240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dasari SS, Archer M, Mohamed NE, Tewari AK, Figueiro MG, Kyprianou N. Circadian rhythm disruption as a contributor to racial disparities in prostate cancer. Cancers (Basel). 2022;14(20):5116. 10.3390/cancers14205116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McGlashan EM, Burns AC, Murray JM, Sletten TL, Magee M, et al. The pupillary light reflex distinguishes between circadian and non-circadian delayed sleep phase disorder (DSPD) phenotypes in young adults. PLoS One. 2018; 13(9): e0204621. 10.1371/journal.pone.0204621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wittmann M, Dinich J, Merrow M, Roenneberg T. Social jetlag: misalignment of biological and social time. Chronobiol Int. 2006;23(1-2):497–509. 10.1080/07420520500545979. [DOI] [PubMed] [Google Scholar]
- 11.Jankowski KS. Social jet lag: Sleep-corrected formula. Chronobiol Int. 2017;34(4):531–5. 10.1080/07420528.2017.1299162. [DOI] [PubMed] [Google Scholar]
- 12.Roenneberg T, Pilz LK, Zerbini G, Winnebeck EC. Chronotype and social jetlag: A (self-) critical review. Biology (Basel). 2019;8(3):54. 10.3390/biology8030054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Taillard J, Sagaspe P, Philip P, Bioulac S. Sleep timing, chronotype and social jetlag: Impact on cognitive abilities and psychiatric disorders. Biochem Pharmacol. 2021;191:114438. 10.1016/j.bcp.2021.114438. [DOI] [PubMed] [Google Scholar]
- 14.Roenneberg T, Allebrandt KV, Merrow M, Vetter C. Social jetlag and obesity. Curr Biol. 2012;22(10):939–43. 10.1016/j.cub.2012.03.038. [DOI] [PubMed] [Google Scholar]
- 15.Caliandro R, Streng AA, van Kerkhof LWM, van der Horst GTJ, Chaves I. Social jetlag and related risks for human health: a timely review. Nutrients. 2021;13,4543. 10.3390/nu13124543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Khaper N, Bailey CDC, Ghugre NR, Reitz C, Awosanmi Z, et al. Implications of disturbances in circadian rhythms for cardiovascular health: A new frontier in free radical biology. Free Radic Biol Med. 2018;119:85–92. 10.1016/j.freeradbiomed.2017.11.006. [DOI] [PubMed] [Google Scholar]
- 17.Lamia KA. Ticking time bombs: connections between circadian clocks and cancer. F1000Res. 2017;6:1910. 10.12688/f1000research. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fischer D, Lombardi DA, Marucci-Wellman H, Roenneberg T. Chronotypes in the US – Influence of age and sex. PLoS One. 2017;12(6):e0178782. 10.1371/journal.pone.0178782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jankowski KS, Díaz-Morales JF, Randler C. Chronotype, gender, and time for sex. Chronobiol Int. 2014;31(8):911–6. 10.3109/07420528.2014.925470. [DOI] [PubMed] [Google Scholar]
- 20.Kossowski B, Drozdziel D, Rode K, Michałowski J, Jankowski KS, Wypych M, et al. The influence of light exposure and chronotype on working memory in humans. Acta Neurobiol Exp (Wars). 2021;81(2):111–20. [PubMed] [Google Scholar]
- 21.Schmidt C, Collette F, Reichert CF, Maire M, Vandewalle G, et al. Pushing the limits: chronotype and time of day modulate working memory-dependent cerebral activity. Front Neurol. 2015;6:199. 10.3389/fneur.2015.00199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.[Ustawa z dnia 1 grudnia 2022 r. o zmianie ustawy – Kodeks pracy oraz niektórych innych ustaw]. J Laws 2023, item 240. Polish.
- 23.Janc M, Jozwiak Z, Jankowska A, Makowiec-Dabrowska T, Kujawa J, Polanska K. Ergonomics of e-learning workstations and the prevalence of musculoskeletal disorders-study among university students. Int J Environ Res Public Health. 2023;20(4):3309. 10.3390/ijerph20043309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Janc M, Jóźwiak Z, Jankowski W, Makowiec-Dąbrowska T, Polańska K. Wpływ pracy/nauki zdalnej na występowanie dolegliwości mięśniowo-szkieletowych w grupie pracowników i studentów uczelni wyższych. Med Pr. 2023; 74(1): 63–78. 10.13075/mp.5893.01345.Polish. [DOI] [PubMed] [Google Scholar]
- 25.Murray JM, Sletten TL, Magee M, Gordon C, Lovato N, Bartlett DJ, Kennaway DJ, et al. Delayed sleep on melatonin (DelSoM) study group. prevalence of circadian misalignment and its association with depressive symptoms in delayed sleep phase disorder. Sleep. 2017;40(1):zsw002. 10.1093/sleep/zsw002. [DOI] [PubMed] [Google Scholar]
- 26.Skeldon, AC, Dijk, D-J. Weekly and seasonal variation in the circadian melatonin rhythm in humans: Entrained to local clock time, social time, light exposure or sun time? J Pineal Res. 2021;71:e12746. 10.1111/jpi.12746. [DOI] [PubMed] [Google Scholar]
- 27.Holzman DC. What's in a color? The unique human health effect of blue light. Environ Health Perspect. 2010; 118(1): A22–7. 10.1289/ehp.118-a22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dijk DJ, Archer SN. Light, sleep, and circadian rhythms: together again. PLoS Biol. 2009;7(6):e1000145. 10.1371/journal.pbio.1000145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lim J, Lee H, Park JB, Lee KJ, Jeong I, Jung J. Combined effect of work from home and work during nonwork time on sleep disturbance. Ann Occup Environ Med. 2023;35:e28. 10.35371/aoem.2023.35.e28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Olsen HM, Brown WJ, Kolbe-Alexander T, Burton NW. Physical activity and sedentary behaviour in a flexible officebased workplace: Employee perceptions and priorities for change. Health Promot J Austr. 2018;29(3):344–52. 10.1002/hpja.164. [DOI] [PubMed] [Google Scholar]
- 31.Crawford JO, MacCalman L, Jackson CA. The health and well-being of remote and mobile workers. Occup Med (Lond). 2011;61(6):385–94. 10.1093/occmed/kqr071. [DOI] [PubMed] [Google Scholar]
- 32.Awada M, Lucas G, Becerik-Gerber B, Roll S. Working from home during the COVID-19 pandemic: Impact on office worker productivity and work experience. Work. 2021; 69(4): 1171–89. 10.3233/WOR-210301. [DOI] [PubMed] [Google Scholar]
- 33.Costa C, Teodoro M, Mento C, Giambò F, Vitello C, et al. Work performance, mood and sleep alterations in home office workers during the COVID-19 pandemic. Int J Environ Res Public Health. 2022;19(4):1990. 10.3390/ijerph19041990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wütschert MS, Romano-Pereira D, Suter L, Schulze H, Elfering A. A systematic review of working conditions and occupational health in home office. Work. 2022;72(3):839–52. 10.3233/WOR-205239. [DOI] [PMC free article] [PubMed] [Google Scholar]


