Abstract
Purpose
To perform a systematic review on clinical and radiologic outcomes for meniscus tears treated nonoperatively with platelet-rich plasma (PRP).
Methods
A literature search was performed according to the 2020 Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines using keywords and Boolean operators in SCOPUS, PubMed, Medline, and the Cochrane Central Register for Controlled Trials in April 2023. Inclusion criteria were limited to Level I to IV human studies reporting on outcomes of meniscus tears treated nonoperatively with PRP.
Results
A total of 6 studies, consisting of 184 patients, were identified. There was 1 Level I study and 5 Level IV studies. Mean patient age was 47.8 ± 7.9 years, with 62% (n = 114/184) being female. The medial meniscus was treated in 95.7% (n = 157/164) of patients. Mean follow-up ranged from 75.9 days to 31.9 months. Meniscus tears were generally described as chronic, degenerative, or intrasubstance. In 4 studies, magnetic resonance imaging revealed variable improvement in meniscus grade with complete healing in 0% to 44% of patients and partial healing in 0% to 40% of patients. Four of 5 studies reported significant statistical improvement in pain from baseline to final follow-up. Studies reporting on clinical outcomes showed significant improvements Lysholm score (2 studies), Knee injury and Osteoarthritis Outcome Score total score (2 studies), and Tegner score (1 study). Successful return to sport occurred in 60% to 100% of patients. Two studies reported that most patients were either very satisfied or satisfied following treatment.
Conclusions
The use of PRP injections for the treatment of meniscus tears led to variable results based on postoperative magnetic resonance evaluation and improvements in clinical outcomes, although the clinical significance remains unclear. The heterogeneity of PRP protocols, short-term follow-up, and lack of comparative studies limit findings.
Level of Evidence
Level IV, systematic review of Level I to IV studies.
Meniscal tears represent the most commonly encountered pathology within the knee, leading to altered knee biomechanics, pain, and disability.1 Meniscal tears may lead to increased localized contact pressures to the chondral surfaces secondary to the loss of native pressure distribution, increasing the potential for cartilage damage and progression.2,3 While often symptomatic, especially in active patients, over 30% of athletes have been observed to be asymptomatic despite the presence of meniscal injury on magnetic resonance imaging (MRI).4
First-line treatment for symptomatic meniscal tears generally consists of nonoperative modalities, including activity modification, anti-inflammatory medication, physical therapy, and corticosteroid injections. For patients without advanced degenerative changes and persistent mechanical symptoms despite a trial of nonoperative management, arthroscopic evaluation to assess for potential meniscal repair versus debridement is often indicated to alleviate pain and restore function.5 Operative decision-making for meniscus tears often depends on tear size, pattern, and location, as well as the status of the chondral surface within the affected compartment. Complex, degenerative tears within the avascular (white-white) zone in an arthritic knee possess a low potential for successful healing following repair and may be better managed through debridement.5,6 Meanwhile, for meniscal tears within the red-white or red-red zone, in the setting of healthy tissue within minimal to no chondral wear, especially in younger patients, meniscal repair is recommended to preserve the native tissue and joint biomechanics.6, 7, 8
Recent investigations have examined the role of platelet-rich plasma (PRP) as a potential adjunct to help optimize meniscal repair healing.9, 10, 11 PRP is theorized to aid with meniscal healing by increasing the local concentration of growth factors and cytokines involved in the healing process.12, 13, 14 However, the role of PRP in isolation as a nonsurgical treatment for patients with meniscal tearing remains largely undefined. The purpose of this study is to perform a systematic review on clinical and radiologic outcomes for meniscus tears treated nonoperatively with PRP. The authors hypothesize that PRP would yield favorable patient-reported outcomes with low rates of complications.
Methods
A systematic review was conducted according to the 2020 Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement.15 A literature search identifying studies reporting outcomes in patients with meniscus tears identified on physical examination and MRI undergoing treatment using PRP was conducted on February 28, 2023, using PubMed, MEDLINE, Scopus, the Cochrane Database for Systematic Reviews, and the Cochrane Central Register for Controlled Trials. The search included a combination of the following terms combined with Boolean operators: “Meniscus,” “Meniscal,” “Degenerative,” “Tear,” “Lesion,” “Injury,” “Chronic,” “Acute,” “Injection,” “Platelet-Rich Plasma,” “PRP,” “Outcomes,” “Magnetic Resonance Imaging,” “Radiographic,” “MRI,” “Radiographs,” “CT,” “Computed Tomography,” and “Complication.”
Eligibility Criteria
Inclusion criteria consisted of Level I to IV studies written in English or with English-language translation, reporting on clinical and radiologic outcomes of patients with meniscus tears treated nonoperatively using PRP. Exclusion criteria consisted of non-English-language studies, review articles, editorial commentaries, case reports, biomechanical studies, and epidemiological and database studies. Studies reporting on patients undergoing operative treatment, studies reporting on meniscus tears treated nonoperatively without PRP, studies with patients younger than 18 years, studies with a follow-up period of 4 weeks or shorter, and studies with overlapping patient data sets (study with most recent mean follow-up was retained) were similarly excluded. Studies reporting on the use of other orthobiologics at the time of PRP injection (hyaluronic acid, bone marrow aspirate concentrate, mesenchymal stromal cells) were excluded.
Data Extraction
Two medical students (V.G. and A.K.B.) performed an independent title and abstract screening, followed by full-text review to determine whether studies met inclusion or exclusion criteria. An attending, board-certified, fellowship-trained orthopaedic surgeon (D.M.K.) was consulted to discuss and resolve any disagreements. Reference lists from the studies were reviewed to ensure that all potential articles meeting inclusion criteria were included in the systematic review and meta-analysis.
Study characteristics from each article were extracted and recorded, consisting of authors, journal of publication, year published, level of evidence, number of patients treated, mean age, sex, knee laterality, meniscus laterality, meniscus tear grading, meniscus tear characterization, treatment indications, and mean follow-up. PRP characteristics and protocols were recorded, including chemical formulations and volume as well as the time between injections for studies using multiple PRP injections. For each study, all radiologic outcomes, patient-reported outcome measures, pain, patient satisfaction, return-to-sport data, and complications were recorded.
Risk of Bias
To minimize bias, 2 medical students (V.G. and A.K.B.) independently performed a methodological quality assessment using the Methodological Index for Non-Randomized Studies (MINORS) criteria. An attending orthopaedic surgeon (D.M.K.) was consulted to resolve any discrepancies if an assigned score of >2 was encountered. The MINORS criteria include a numerical scale used for noncomparative, nonrandomized studies. The MINORS criteria include up to 12 questions (8 for noncomparative studies). Each question is given a score from 0 to 2: 0 if not reported, a 1 if reported but inadequate, or 2 if reported and adequate. The ideal score for noncomparative, nonrandomized studies is 16, while the ideal score for comparative studies is 24. All included studies were assessed using the MINORS criteria.
Data Analysis
Study characteristics and patient demographic information were analyzed using Microsoft Excel (Version 2207; Microsoft Corporation). Patient characteristics were compiled and pooled by either reporting mean ± standard deviation or proportions when appropriate. Return-to-sport rate, complications, patient satisfaction, and radiologic outcomes were pooled and reported as proportions. Pain and patient-reported outcome measures reported from baseline to final follow-up were gathered and evaluated with random-effects models using Review Manager (Version 5.4; The Cochrane Collaboration).
Results
The initial literature search identified 610 articles (Fig 1). Following removal of duplicates, 253 articles remained and underwent title and abstract screening. A total of 12 articles were then selected to undergo full-text review. Following full-text review, 6 studies were found to meet inclusion criteria and included in this review. Five studies9,10,16, 17, 18 were of Level IV evidence and 1 study19 was Level I evidence.
Fig 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses diagram.
Study and Patient Characteristics
Of the 6 included studies, a total of 184 patients were included, possessing a mean age of 47.8 ± 7.9 years (Table 1). Females comprised 62% (n = 114/184) of patients. Meniscal tears in the right knee (55.7%, n = 73/131) were more commonly treated than the left, with most patients undergoing treatment for medial meniscus tears (95.7%, n = 157/164). Mean follow-up ranged from 75.9 days17 to 31.9 months.18 Meniscal tears were characterized in 4 studies, described as “chronic,”19 “degenerative,”9,10,18 and/or “intrasubstance”16,18 (Table 2). Meniscal lesions were graded in 5 studies, with 3 studies16, 17, 18 using the classification from Reicher et al.,20 1 study10 using the grading system described by Stoller et al.,21 and 1 study9 using the grading system proposed by Crues et al.22 (Table 2). Three of 6 studies excluded patients who had undergone prior corticosteroid injections to the injured knee.9,16,17 Five of the 6 studies excluded patients with advanced degenerative changes, primarily based on Kellgren-Lawrence grade.9,10,16,18,19
Table 1.
Patient Demographics
| Characteristic | Value |
|---|---|
| Total patient population, n | 184 |
| Patient age, mean ± SD, y | 47.8 ± 7.9 |
| Sex | |
| Female | 62.0% (n = 114/184) |
| Male | 38.0% (n = 70/184) |
| Left vs right knee | |
| Right | 55.7% (n = 73/131) |
| Left | 44.3% (n = 58/131) |
| Meniscus laterality | |
| Medial | 95.7% (n = 157/164) |
| Lateral | 4.3% (n = 7/164) |
Table 2.
Overview of Included Studies
| Author | Journal (Year) | LOE | Number of Patients | Age, Mean ± SD (Range), y | Sex, M/F, n | Knee, Right/Left, n | Meniscus Laterality (Medial/Lateral) | Meniscus Tear Grading | Meniscus Tear Characterization | Treatment Indications | Mean Follow-Up |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Alessio-Mazzola et al.9 | Sports Health (2022) | 4 | 69 | 52.1 ± 7.8 (36-62) | 21/48 | 36/33 | 69 medial | Grade 3 (Crues et al.22) | Degenerative; horizonal tears (63), complex tears (6) | Insidious onset; mechanical symptoms; positive McMurray, Apley, or Thessaly test; joint line tenderness; MRI evidence of degenerative meniscus tear; no bony edema; KL grade >1 excluded | Minimum 12 mo |
| Blanke et al.16 | Muscle, Ligaments, and Tendons Journal (2015) | 4 | 10 | 53.3 ± 13.9 | 6/4 | NR | NR | Grade 2b (Reicher et al.20) | Intrasubstance | Persistent joint pain >6 mo, grade 2 meniscus lesion on MRI, failed 6 mo of conservative treatment, KL grade >2 excluded | 6 mo |
| Guenoun et al.10 | Diagnostic and Interventional Imaging (2020) | 4 | 10 | 40.4 ± 13.6 (18-59) | 7/3 | 7/3 | NR | Grade 1 (2), grade 2 (4), grade 3 (4) (Stoller et al.21) | Degenerative | Degenerative meniscus tear without knee osteoarthritis | 6 mo |
| Kaminski et al.19 | International Journal of Molecular Sciences (2019) | 1 | 72. Control group (n = 3), PRP group (n = 42) | Control group: 46 (27-68), PRP group: 44 (18-67) | Control group: 19/11, PRP group: 22/20 | NR | Control group: 30 medial, PRP group: 41 medial/1 lateral | NR | Chronic horizontal meniscal tear | Chronic horizontal tear assessed via MRI, tear in the vascular/avascular zone of meniscus, single tear of medial or lateral meniscus, KL grade >2 excluded | 92 (54-157) wk |
| Medina-Porqueres et al.17 | International Journal of Environmental Research and Public Health (2022) | 4 | 38 | 50.68 ± 9.65 (29-72) | 8/30 | 25/12 | 32 medial/6 lateral | Grade 1 (1), grade 2 (6), grade 3 (31) (Reicher et al.20) | NR | Failed conservative treatment for 6 wk | 75.92 ± 31.7 (39-190) d |
| Ozyalvac et al.18 | Journal of Orthopaedic Surgery (2019) | 4 | 15 | 33.2 ± 8.2 (19-45) | 6/9 | 5/10 | 15 medial | Grade 2 (Reicher et al.20) | Intrasubstance /degenerative, Ahlback grade 2 or higher excluded | Prescence of intrasubstance meniscus degeneration | 31.9 ± 5.6 (19-39) mo |
KL, XXX; L, left; LOE, level of evidence; MRI, magnetic resonance imaging; NR, not recorded; PRP, platelet-rich plasma; R, right.
PRP Characteristics and Protocols
Platelet-rich plasma characteristics were reported in 5 studies (Table 3).9,10,16,18,19 Two studies reported the mean PRP platelet concentration of 600,000/mL9 and 497 ± 154 g/L.10 In 3 studies, leukocytes were removed and/or classified as leukocyte poor.9,10,16 Two studies used PRP containing a high concentration of leukocytes.18,19 Three studies used a single PRP injection,10,18,19 2 studies used 3 injections,16,17 and 1 study administered 4 injections.9 Among the 3 studies using multiple injections, all studies administered injections at 1-week intervals.9,16,17 Additionally, Kaminski et al.19 performed a concomitant ultrasound-guided meniscal trephination in patients receiving PRP. Two studies reported PRP classification by Mishra et al.24 as type 2B18 and type 3A,16 respectively.
Table 3.
Treatment Protocols
| Author | PRP Characteristics | PRP Protocol | Rehabilitation |
|---|---|---|---|
| Alessio-Mazzola et al.9 | Mean platelet concentration: 600,000 Leukocyte-poor leukocytes: <1000 WBC/mL23 |
Number of injections: 4 Interval: 1 wk Volume: 5 mL |
NSAIDs discouraged, no formal exercise or PT, allowed gradual return to work and sports |
| Blanke et al.16 | Leukocyte poor Type 3A class (Mishra et al.24) |
Number of injections: 3 Interval: 1 wk Volume: 2-5 mL |
Allowed to weight bear, avoid physical activity for 4 wk, NSAIDs not allowed for 6 mo, no formal PT |
| Guenoun et al.10 | Platelet concentration: 497 ± 154 G/L 0.1% leukocytes: 0.58 ± 0.51 G/L |
Number of injections: 1 Volume: 4 mL |
NR |
| Kaminski et al.19 | Red-L-PRPIIB-1 class Contains leukocytes |
Number of injections: 1 Volume: 6-8 mL Concomitant ultrasound-guided meniscal trephination |
Referred to PT, hinged knee brace for 4 wk, ROM for 6 wk, weightbearing as tolerated, slow increase in exercises from 6 to 12 wk onward |
| Medina-Porqueres et al.17 | NR | Number of injections: 3 Interval: 1 wk Volume: 6 mL |
Avoid NSAIDs for 2 wk after last injection, apply ice and full weightbearing, avoid impact activities for 2 wk with gradual return over 4 to 8 wk |
| Ozyalvac et al.18 | Type 2B class (Mishra et al.24) | Number of injections: 1 Volume: 4 mL |
NR |
NR, not recorded; NSAID, nonsteroidal anti-inflammatory drug; PRP, platelet-rich plasma; PT, physical therapy; ROM, range of motion; WBC, white blood cells.
Rehabilitation
Rehabilitation following PRP injections was described in 4 studies.9,16,17,19 In 3 studies,9,16,17 nonsteroidal anti-inflammatory drugs were discouraged, with 2 studies requiring cessation of anti-inflammatory medications for a duration of 2 weeks17 or 6 months16 following the final PRP injection. Full weightbearing as tolerated was allowed following treatment, with a gradual increase in physical activity and exercise.9,16,17,19 Two studies9,16 did not report having patients engage in formal physical therapy. Use of a hinged knee brace for 4 weeks following injection was reported in a single study.19
Radiologic Outcomes
Four studies, consisting of 57 patients, reported radiologic outcomes (Table 4).10,16,18,19 Three studies10,16,18 used MRI, whereas 1 study19 used MRI arthrography. Blanke et al.16 reported that all patients were grade 2B (intrasubstance defect without extension to the surface) at baseline, whereas at 6-month follow-up, 1 patient was grade 1, 2 were grade 2A, 5 were grade 2B, and 2 were grade 3. Guenoun et al.10 observed that 70% (n = 7/10) of patients undergoing MRIs possessed a stable meniscus tear but no evidence of healing following treatment. Kaminski et al.19 reported that on MRI, 11 patients had a fully healed meniscus, 4 were partially healed, and 10 showed evidence of failure, defined by contrast within the meniscal body or conversion to meniscectomy or meniscal repair. All 15 patients in the study by Ozyalvac et al.18 were grade 2 at baseline. At follow-up, 4 were normal, 6 were grade 1, 4 were grade 2, and 1 was grade 3.
Table 4.
Clinical and Radiologic Outcomes
| Author | MR Evaluation | Lysholm | KOOS | Tegner | Pain | Return to Sport | Patient Satisfaction | Complications | Other Clinical Outcomes |
|---|---|---|---|---|---|---|---|---|---|
| Alessio-Mazzola et al.9 | NR | Baseline: 72.9 ± 7.3 (59-95) 1 mo: 78.2 ± 7.95 (66-100) 3 mo: 85.7 ± 7.1 (72-100) 6 mo: 87.8 ± 5.9 (76-100) 12 mo: 85.6 ± 5.6 (75-94) |
NR | Baseline: 4.3 ± 1.1 Follow-up: 4.3 ± 0.99 |
VAS grading Baseline: 5.3 ± 2.0 (2-8) 1 mo: 4.1 ± 2.0 (0-7) 3 mo: 2.8 ± 1.5 (0-5) 6 mo: 2.6 ± 1.2 (0-4) 12 mo: 2.6 ± 1.3 (0-4) |
NR | Very satisfied (n = 33, 47.8%), satisfied (n = 26, 37.7%), partially satisfied (n = 8, 11.6%), not satisfied (n = 2, 2.9%) Willing to repeat same treatment (n = 62, 89.8%) |
None | WOMAC Baseline: 77.7 ± 11.3 (59.1-97.0) 1 mo: 81.5 ± 10.2 (57.0-98.5) 3 mo: 89.4 ± 6.5 (75.0-98.5) 6 mo: 91.9 ± 4.9 (82.0-98.5) 12 mo: 90.7 ± 4.7 (82-96.2) ROM Baseline: 131 ± 7.7 (110-135) 1 mo: 131 ± 135 (110-135) 3 mo: 133 ± 5.2 (120-135) 6 mo: 133 ± 5.2 (120-135) 12 mo: 133 ± 5.2 (120-135) |
| Blanke et al.16 | Baseline: all patients grade 2b 6 mo: 1 grade 1, 2 grade 2a, 5 grade 2b, 2 grade 3 4 patients showed decline in intrasubstance signal |
NR | NR | NR | NRS-11 grading Baseline: 6.9 ± 0.99 6 mo: 4.5 ± 2.99 |
6/10 returned to sport | NR | 4 patients required surgery for persistent knee pain | NR |
| Guenoun et al.10 | 7 patients undergoing MRI showed stability of meniscus tear but no MRI healing | NR | Total Baseline: 56.6 ± 15.7 3 mo: 70.2 ± 16.8 6 mo: 72.7 ± 18.5 Other symptoms Baseline: 68.7 ± 15.3 3 mo: 81.4 ± 9.2 6 mo: 84.9 ± 10.5 Pain Baseline: 64.5 ± 14.1 3 mo: 75.6 ± 15.1 6 mo: 76.2 ± 17.6 KOOS function in daily living Baseline: 79.2 ± 20.1 3 mo: 86.8 ± 14.3 6 mo: 85.1 ± 17.5 Sport and recreation Baseline: 40.1 ± 24.9 3 mo: 58.5 ± 25.8 6 mo: 60.9 ± 28.5 QoL Baseline: 30.6 ± 18.1 3 mo: 48.6 ± 32.4 6 mo: 56.2 ± 28.1 |
NR | VAS grading Baseline: 57.0 ± 11.6 6 mo: 36.3 ± 31.1 P = .18 |
6/6 returned to sport | NR | No major complications Pain at injection site lasting for 10 min |
NR |
| Kaminski et al.19 | 11 healed, 4 partially healed, 10 failed Assessed via MRI arthrography |
NR | Pain Baseline: 57.48 ± 0.30 (57.18-57.78 Follow-up: 87.24 ± 0.36 (82.99-91.48) Symptoms Baseline: 63.65 ± 0.39 Follow-up: 92.03 ± 0.27 ADL Baseline: 63.70 ± 0.37 (63.40-64.00) Follow-up: 89.36 ± 0.36 (85.07-93.64) Sport/recreation Baseline: 35.83 ± 0.51 (35.53-36.14) Follow-up: 69.52 ± 0.77 (60.29-78.74) QoL Baseline: 37.90 ± 0.26 (37.59-38.20) Follow-up: 67.06 ± 0.55 (60.56-73.56) |
NR | VAS grading Baseline: 5.38 ± .05 (4.77-5.99) Follow-up: 1.97 ± 0.05 (1.40-2.55) |
NR | NR | None | WOMAC Baseline: 34.36 ± 0.36 (29.90-38.82) Follow-up: 9.72 ± 0.32 IKDC Baseline: 51.99 ± 0.34 (47.62-56.36) Follow-up: 85.98 ± 0.52 (79.79-92.16) |
| Medina-Porqueres et al.17 | NR | NR | Baseline: 41.89 ± 22.96 Follow-up: 85.94 ± 13.50 |
Baseline: 3.73 ± 1.67 Follow-up: 4.74 ± 1.70 |
NPRS scale Baseline: 5.86 ± 1.91 Follow-up: 1.59 ± 1.34 |
NR | Very satisfied (25), satisfied (13) | None | Feeling thermometer Baseline: 67.89 ± 16.42 Follow-up: 86.31 ± 6.74 |
| Ozyalvac et al.18 | Baseline: all grade 2 Follow-up: 4 normal, 6 grade 1, 4 grade 2, 1 grade 3 |
Baseline: 71.1 ± 6.9 Follow-up: 91.9 ± 6.6 |
NR | NR | NR | NR | NR | NR | NR |
ADL, activities of daily living; IKDC, International Knee Documentation Committee; KOOS, Knee injury and Osteoarthritis Outcome Score; MR, magnetic resonance; MRI, magnetic resonance imaging; NPRS, numeric pain rating scale; NR, not recorded; NRS-11, 11-point numeric rating scale; QoL, quality of life; ROM, range of motion; VAS, visual analog scale; WOMAC, Western Ontario and McMaster Universities Arthritis Index.
Clinical Outcomes
All 6 studies reported clinical outcomes following treatment. Five studies reported outcomes in pain using the visual analog scale (VAS),9,10,19 11-point numeric rating scale,16 or numeric pain rating scale (NPRS).17 Four studies9,16,17,19 reported significant decreases in pain following PRP, whereas 1 study10 reported a nonsignificant decrease in pain following treatment. Significant improvement in Lysholm score was reported in 2 studies, ranging from 12.7 to 20.8 points.9,18 Knee injury and Osteoarthritis Outcome Score (KOOS) total score from baseline to follow-up was reported in 2 studies, with significant improvement in both studies ranging from 16.1 to 44.1 points.10,17 Baseline to follow-up Tegner score was reported in 2 studies, with significant improvement from 4.74 to 3.73 in Medina-Porqueres et al.17 and unclear improvement in Alessio-Mazzola et al.9 When evaluating clinically significant outcomes, Kaminski et al.19 observed that 78% of patients achieved the minimal clinically important differences (MCIDs) for International Knee Documentation Committee, 86% for Western Ontario and McMaster Universities Arthritis Index score, and a minimum of 70% across all KOOS outcome measures. A significantly greater percentage of patients achieved MCID with PRP compared with the control group based on VAS (65% vs 39%, P = .046) and KOOS symptoms (76% vs 48%, P = .028).19
Return to sport was reported in 2 studies in 16 patients,10,16 with a successful return-to-sport rate ranging from 60% to 100%. Patient satisfaction was reported in 2 studies.9,17 In Alessio-Mazzola et al.,9 47.8% (n = 33/69) of patients were very satisfied, 37.7% (n = 26/69) were satisfied, 11.6% (n = 8/69) were partially satisfied, and 2.9% (n = 2/69) were not satisfied. In Medina-Porqueres et al.,17 65.8% (n = 25/38) patients were very satisfied and 34.2% (n = 13/38) were satisfied.
Complications and Failures
The significant complication rate across studies was 0%, reported in 5 studies.9,10,16,17,19 Mild postinjection pain was reported in 17 patients, reported to resolve within 10 minutes10 or within 5 days following icepack treatment and paracetamol.16 In their investigation examining outcomes following PRP injection, Blanke et al.16 reported that 40% (4 of 10) patients underwent operative intervention due to persistent knee pain.
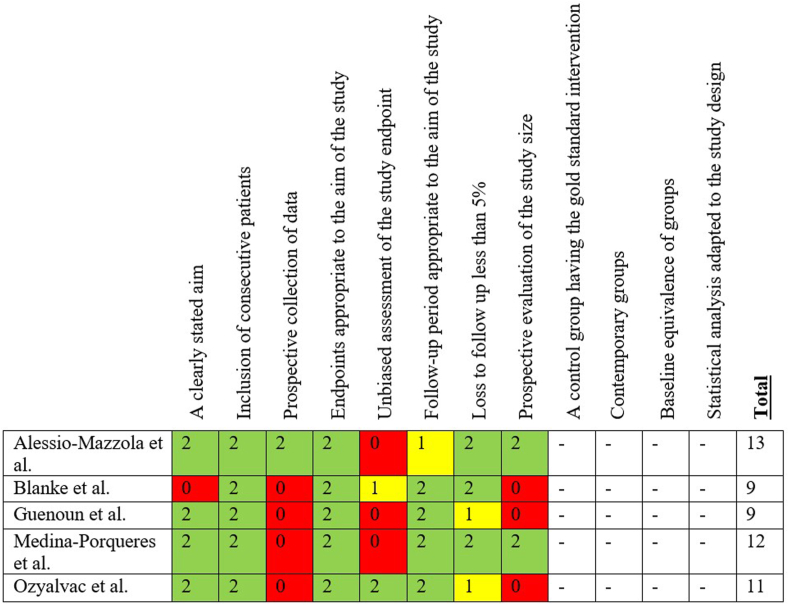
Risk of Bias Assessment
For the 5 noncomparative, nonrandomized studies, the mean MINORS score was 10.8 ± 1.8 (range, 9-13) (Fig 2).9,10,16, 17, 18 The double-blinded randomized controlled trial did not meet criteria to be assessed with the MINORS criteria.19
Fig 2.
Risk of bias using the Methodological Index for Non-Randomized Studies criteria.
Discussion
The most important findings from this study were that the use of injectable PRP for management of meniscal tears characterized as “chronic,” “degenerative,” or “intrasubstance,” as reported in 6 studies in 184 patients, led to (1) variable improvements on postoperative MRI in meniscal status based on MRI; (2) improvements in pain, Lysholm, and total KOOS scores with unclear clinical significance; and (3) a high rate of patient satisfaction following treatment.
When appropriately indicated based on chondral status, meniscal tissue integrity, and tear pattern, arthroscopic meniscal repair is indicated to prevent the development of further meniscal and chondral damage. However, meniscus repair has been reported to possess a failure rate ranging from 12% to 15%, with failure rates increasing over time.25, 26, 27 Specifically, Nepple et al.28 reported a 19.5% overall failure rate of meniscus repairs at a minimum 5-year follow-up. Given the potential complications and failure rate of surgical management, nonoperative treatment for patients with stable, degenerative meniscus tears using biologic augmentation may be a suitable initial option prior to proceeding with arthroscopic intervention. Another potential adjunct during orthobiologic treatment includes meniscal trephination, performed in the single Level 1 study included in this systematic review.19 The authors observed that PRP used with ultrasound-guided meniscal trephination led to greater survival and a greater proportion of patients achieving the minimally clinically significant difference for VAS and KOOS symptom measures compared with meniscal trephination without PRP. Although the isolated use of PRP for meniscal tearing represents an interesting treatment option, further investigations identifying optimal indications based on patient and tear characteristics evaluated on MRI are necessary.
Platelet-rich plasma has gained popularity in orthopaedic sports medicine, from its use in augmentation of rotator cuff repairs to its treatment of patellar tendinopathy.29,30 However, the use of PRP remains controversial due to variable outcomes, as well as heterogeneity in preparation methods and concentrations, with experts achieving consensus on only 62% of statements regarding PRP.31 Several studies have reported improved outcomes and reduced failure rate following PRP augmentation during operative management for meniscal tears, although multiple systematic reviews have reported no significant differences between PRP augmented and nonaugmented meniscus repairs.32, 33, 34, 35 PRP is hypothesized to improve healing and outcomes for meniscus tears, particularly in the inner avascular (white-white) zone by recruiting numerous growth factors to help promote and facilitate healing.14,36 Similar to meniscus repair, animal studies examining nonoperative treatment of meniscus tears with PRP have yielded conflicting results. Shin et al.37 and Lee et al.38 applied PRP to rabbit menisci and observed that PRP administration did not enhance healing and may promote fibrosis instead of the regeneration of meniscal cartilage. Meanwhile, Xiao et al.14 reported improved healing when PRP was administered compared with a control group in beagle dogs with meniscus tears in the white-white zone. As such, additional investigations are warranted to better understand the efficacy and quality of repair tissue generated using PRP for the treatment of meniscus tears.
Of the 4 studies reporting MRI outcomes of meniscus tears treated with PRP, in 2 studies, less than 50% of patients achieved any level of meniscal healing.10,16 However, this systematic review revealed significant improvements in pain, Lysholm, and total KOOS scores in studies reporting clinical outcomes. Although knee arthritic changes may confound the true effect of PRP on treating meniscus tears, most studies excluded patients with osteoarthritis. Favorable clinical outcomes despite poor healing on MRI have been reported for degenerative meniscus tears and horizontal-cleavage tears.39,40 Namely, Kaminski et al.19 observed that healing of degenerative meniscus lesions following meniscal trephination with and without PRP was not observed despite patients achieving clinically significant outcome measures. Furthermore, MRI evaluation likely does not provide accurate data regarding the quality of meniscus healing.41 We hypothesize the discrepancy between clinical and radiologic results may be due to the short-term follow-up of included studies. The authors suspect that the mediocre radiologic outcomes may suggest the limited long-term durability of PRP treatment for meniscal tears, with deteriorating clinical outcomes and increasing failure rates occurring over time despite the short-term symptomatic relief. Future high-level, comparative studies at long-term follow-up are needed to establish PRP injections during the nonoperative management of meniscus tears as an effective option.
Limitations
This study was not without limitations. This study was primarily limited due to the small sample size and the inclusion of a low level of quality of included studies, which is an inherent limitation based on the available literature. Moreover, the lack of a comparative group in most studies limits any understanding of the true efficacy of PRP on improving outcomes for meniscus tears when compared with meniscal tears treated nonoperatively without PRP. Furthermore, due to the limited amount of data available regarding meniscal tear pathology, as well as the presence of any concomitant injuries, the ideal tear type and patient for PRP treatment remain unknown and warrant further examination. Concomitant meniscal trephination was performed in patients in a single investigation, serving as a potential confounding variable.19 Due to the small sample size, the authors were limited in performing any further meaningful statistical analysis assessing the impact of PRP volume or type on clinical or radiographic outcomes, as well as the incidence of any injection-related complications. Most studies excluded patients with advanced degenerative changes in the knee, limiting the generalizability of these findings to patients with osteoarthritis. As the mean follow-up was under 1 year in most studies, the longevity of PRP treatment at mid- and long-term follow-up cannot be extrapolated and requires further investigation. Furthermore, given the high heterogeneity in PRP characteristics, including leukocyte concentration, PRP volume, number of PRP injections administered, and rehabilitation protocols, standardization is necessary to determine the ideal regimen to yield successful outcomes. Despite most tears being described as degenerative, there was high variability in the use of grading classifications. Moreover, as most studies included degenerative tears, the results of this study do not reflect the outcomes of PRP for traumatic meniscus tears that are ideal in appropriately selected patients for acute meniscal repair.
Conclusions
The use of PRP injections for the treatment of meniscus tears led to variable results based on postoperative magnetic resonance evaluation and improvements in clinical outcomes, although the clinical significance remains unclear. The heterogeneity of PRP protocols, short-term follow-up, and lack of comparative studies limit findings.
Disclosures
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: J.C. has received consulting fees from Arthrex, CONMED Linvatec Corporation, Ossur, Smith & Nephew, Vericel, RTI Surgical, Stryker Corporation, and DePuy Synthes Products; support for education from Arthrex, Medwest Associates, and Smith & Nephew; speaking fees from Linvatec, Arthrex, and Smith & Nephew; hospitality payments from Medical Device Business Services, Medwest Associates, Smith & Nephew, Linvatec, and Stryker; and a grant from Arthrex. M.V.S. has received speaking and faculty, education, and hospitality payments from Arthrex; education and hospitality payments from Elite Orthopaedics; and hospitality payments from Medical Device Business Services. M.J.M. has received consulting, faculty and speaking, and hospitality payments from Arthrex; education payments from Elite Orthopaedics; consulting and hospitality payments from Heron Therapeutics; and consulting and hospitality payments from Pacira Pharmaceuticals. R.H.B. has received support for education and hospitality payments from Elite Orthopaedics. D.M.K. has received support for education from Smith & Nephew, Elite Orthopedics, and Medwest Associates; hospitality payments from Arthrex, Encore Medical, Stryker, and Smith & Nephew; honoraria from Encore Medical; and a grant from Arthrex. All other authors (V.G., A.K.B.) declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Supplementary Data
References
- 1.Berg B., Roos E.M., Kise N.J., Engebretsen L., Holm I., Risberg M.A. On a trajectory for success—9 in every 10 people with a degenerative meniscus tear have improved knee function within 2 years after treatment: A secondary exploratory analysis of a randomized controlled trial. J Orthop Sports Phys Ther. 2021;51:289–297. doi: 10.2519/jospt.2021.10025. [DOI] [PubMed] [Google Scholar]
- 2.Yang Q., Zhu X-y, Bao J-y, et al. Medial meniscus posterior root tears and partial meniscectomy significantly increase stress in the knee joint during dynamic gait. Knee Surg Sports Traumatol Arthrosc. 2022;31:2289–2298. doi: 10.1007/s00167-022-07285-9. [DOI] [PubMed] [Google Scholar]
- 3.Ohori T., Mae T., Shino K., et al. Different effects of the lateral meniscus complete radial tear on the load distribution and transmission functions depending on the tear site. Knee Surg Sports Traumatol Arthrosc. 2020;29:342–351. doi: 10.1007/s00167-020-05915-8. [DOI] [PubMed] [Google Scholar]
- 4.Beals C.T., Magnussen R.A., Graham W.C., Flanigan D.C. the prevalence of meniscal pathology in asymptomatic athletes. Sports Med. 2016;46:1517–1524. doi: 10.1007/s40279-016-0540-y. [DOI] [PubMed] [Google Scholar]
- 5.Wasserburger J.N., Shultz C.L., Hankins D.A., et al. Long-term national trends of arthroscopic meniscal repair and debridement. Am J Sports Med. 2021;49:1530–1537. doi: 10.1177/0363546521999419. [DOI] [PubMed] [Google Scholar]
- 6.Marigi E.M., Keyt L.K., LaPrade M.D., et al. Surgical treatment of isolated meniscal tears in competitive male wrestlers: Reoperations, outcomes, and return to sport. Orthop J Sports Med. 2021;9 doi: 10.1177/2325967120969220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cinque M.E., DePhillipo N.N., Moatshe G., et al. Clinical Outcomes of Inside-Out Meniscal Repair According to Anatomic Zone of the Meniscal Tear. Orthop J Sports Med. 2019;7 doi: 10.1177/2325967119860806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rogers M., Dart S., Odum S., Fleischli J. A cost-effectiveness analysis of isolated meniscal repair versus partial meniscectomy for red-red zone, vertical meniscal tears in the young adult. Arthroscopy. 2019;35:3280–3286. doi: 10.1016/j.arthro.2019.06.026. [DOI] [PubMed] [Google Scholar]
- 9.Alessio-Mazzola M., Felli L., Trentini R., et al. Efficacy of autologous platelet-rich plasma injections for grade 3 symptomatic degenerative meniscal lesions: A 1-year follow-up prospective study. Sports Health. 2021;14:227–236. doi: 10.1177/19417381211011074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Guenoun D., Magalon J., de Torquemada I., et al. Treatment of degenerative meniscal tear with intrameniscal injection of platelets rich plasma. Diagn Interv Imaging. 2020;101:169–176. doi: 10.1016/j.diii.2019.10.003. [DOI] [PubMed] [Google Scholar]
- 11.Delen V., Ediz L., Alpaycı M. The clinical effect of platelet-rich plasma injections on symptomatic meniscal tears of the knee. East J Med. 2021;26:367–370. [Google Scholar]
- 12.Le A.D.K., Enweze L., DeBaun M.R., Dragoo J.L. Current clinical recommendations for use of platelet-rich plasma. Curr Rev Musculoskelet Med. 2018;11:624–634. doi: 10.1007/s12178-018-9527-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Qi Y., Tang R., Shi Z., Feng G., Zhang W. Wnt5a/platelet-rich plasma synergistically inhibits IL-1β-induced inflammatory activity through NF-κB signaling pathway and prevents cartilage damage and promotes meniscus regeneration. J Tissue Eng Regen Med. 2021;15:612–624. doi: 10.1002/term.3198. [DOI] [PubMed] [Google Scholar]
- 14.Xiao W.F., Yang Y.T., Xie W.Q., et al. Effects of platelet-rich plasma and bone marrow mesenchymal stem cells on meniscal repair in the white-white zone of the meniscus. Orthop Surg. 2021;13:2423–2432. doi: 10.1111/os.13089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Page M.J., McKenzie J.E., Bossuyt P.M., et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Blanke F., Vavken P., Haenle M., von Wehren L., Pagenstert G., Majewski M. Percutaneous injections of platelet rich plasma for treatment of intrasubstance meniscal lesions. Muscles Ligaments Tendons J. 2015;5:162–166. doi: 10.11138/mltj/2015.5.3.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Medina-Porqueres I., Martin-Garcia P., Sanz-De-Diego S., et al. Clinical and functional outcome of meniscal injuries treated with platelet-rich plasma: A single-center case series. Int J Environ Res Public Health. 2022;19:7118. doi: 10.3390/ijerph19127118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Özyalvaç O.N., Tüzüner T., Gürpinar T., Obut A., Acar B., Akman Y.E. Radiological and functional outcomes of ultrasound-guided PRP injections in intrasubstance meniscal degenerations. J Orthop Surg (Hong Kong) 2019;27 doi: 10.1177/2309499019852779. [DOI] [PubMed] [Google Scholar]
- 19.Kaminski R., Maksymowicz-Wleklik M., Kulinski K., Kozar-Kaminska K., Dabrowska-Thing A., Pomianowski S. Short-term outcomes of percutaneous trephination with a platelet rich plasma intrameniscal injection for the repair of degenerative meniscal lesions: A prospective, randomized, double-blind, parallel-group, placebo-controlled study. Int J Mol Sci. 2019;20:856. doi: 10.3390/ijms20040856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Reicher M.A., Hartzman S., Duckwiler G.R., Bassett L.W., Anderson L.J., Gold R.H. Meniscal injuries: Detection using MR imaging. Radiology. 1986;159:753–757. doi: 10.1148/radiology.159.3.3754645. [DOI] [PubMed] [Google Scholar]
- 21.Stoller D.W., Martin C., Crues J.V., III, Kaplan L., Mink J.H. Meniscal tears: Pathologic correlation with MR imaging. Radiology. 1987;163:731–735. doi: 10.1148/radiology.163.3.3575724. [DOI] [PubMed] [Google Scholar]
- 22.Crues J.V., III, Mink J., Levy T.L., Lotysch M., Stoller D.W. Meniscal tears of the knee: Accuracy of MR imaging. Radiology. 1987;164:445–448. doi: 10.1148/radiology.164.2.3602385. [DOI] [PubMed] [Google Scholar]
- 23.Kon E., Di Matteo B., Delgado D., et al. Platelet-rich plasma for the treatment of knee osteoarthritis: an expert opinion and proposal for a novel classification and coding system. Expert Opin Biol Ther. 2020;20:1447–1460. doi: 10.1080/14712598.2020.1798925. [DOI] [PubMed] [Google Scholar]
- 24.Mishra A., Harmon K., Woodall J., Vieira A. Sports medicine applications of platelet rich plasma. Curr Pharm Biotechnol. 2012;13:1185–1195. doi: 10.2174/138920112800624283. [DOI] [PubMed] [Google Scholar]
- 25.Ow Z.G.W., Law M.S.N., Ng C.H., et al. All-cause failure rates increase with time following meniscal repair despite favorable outcomes: A systematic review and meta-analysis. Arthroscopy. 2021;37:3518–3528. doi: 10.1016/j.arthro.2021.05.033. [DOI] [PubMed] [Google Scholar]
- 26.Schweizer C., Hanreich C., Tscholl P.M., Blatter S., Windhager R., Waldstein W. Meniscal repair outcome in 3829 patients with a minimum follow-up from 2 years up to 5 years: A meta-analysis on the overall failure rate and factors influencing failure. Am J Sports Med. 2023;52:822–831. doi: 10.1177/03635465231158385. [DOI] [PubMed] [Google Scholar]
- 27.Costa G.G., Grassi A., Zocco G., et al. What is the failure rate after arthroscopic repair of bucket-handle meniscal tears? A systematic review and meta-analysis. Am J Sports Med. 2021;50:1742–1752. doi: 10.1177/03635465211015425. [DOI] [PubMed] [Google Scholar]
- 28.Nepple J.J., Block A.M., Eisenberg M.T., Palumbo N.E., Wright R.W. Meniscal repair outcomes at greater than 5 years: A systematic review and meta-analysis. J Bone Joint Surg Am. 2022;104:1311–1320. doi: 10.2106/JBJS.21.01303. [DOI] [PubMed] [Google Scholar]
- 29.Barman A., Sinha M.K., Sahoo J., et al. Platelet-rich plasma injection in the treatment of patellar tendinopathy: A systematic review and meta-analysis. Knee Surg Relat Res. 2022;34:22. doi: 10.1186/s43019-022-00151-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Li Y., Li T., Li J., Tang X., Li R., Xiong Y. Platelet-rich plasma has better results for retear rate, pain, and outcome than platelet-rich fibrin after rotator cuff repair: A systematic review and meta-analysis of randomized controlled trials. Arthroscopy. 2022;38:539–550. doi: 10.1016/j.arthro.2021.05.023. [DOI] [PubMed] [Google Scholar]
- 31.Hurley E.T., Sherman S.L., Stokes D.J., et al. Experts achieve consensus on a majority of statements regarding platelet-rich plasma treatments for treatment of musculoskeletal pathology. Arthroscopy. 2024;40:470–477.e471. doi: 10.1016/j.arthro.2023.08.020. [DOI] [PubMed] [Google Scholar]
- 32.Belk J.W., Kraeutler M.J., Thon S.G., Littlefield C.P., Smith J.H., McCarty E.C. Augmentation of meniscal repair with platelet-rich plasma: A systematic review of comparative studies. Orthop J Sports Med. 2020;8 doi: 10.1177/2325967120926145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Everhart J.S., Cavendish P.A., Eikenberry A., Magnussen R.A., Kaeding C.C., Flanigan D.C. Platelet-rich plasma reduces failure risk for isolated meniscal repairs but provides no benefit for meniscal repairs with anterior cruciate ligament reconstruction. Am J Sports Med. 2019;47:1789–1796. doi: 10.1177/0363546519852616. [DOI] [PubMed] [Google Scholar]
- 34.Migliorini F., Cuozzo F., Cipollaro L., Oliva F., Hildebrand F., Maffulli N. Platelet-rich plasma (PRP) augmentation does not result in more favourable outcomes in arthroscopic meniscal repair: A meta-analysis. J Orthop Traumatol. 2022;23:8. doi: 10.1186/s10195-022-00630-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zaffagnini S., Poggi A., Reale D., Andriolo L., Flanigan D.C., Filardo G. Biologic augmentation reduces the failure rate of meniscal repair: A systematic review and meta-analysis. Orthop J Sports Med. 2021;9 doi: 10.1177/2325967120981627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hutchinson I.D., Rodeo S.A. The current role of biologics for meniscus injury and treatment. Curr Rev Musculoskelet Med. 2022;15:456–464. doi: 10.1007/s12178-022-09778-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shin K.H., Lee H., Kang S., et al. Effect of leukocyte-rich and platelet-rich plasma on healing of a horizontal medial meniscus tear in a rabbit model. Biomed Res Int. 2015;2015 doi: 10.1155/2015/179756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lee H.R., Shon O.J., Park S.I., et al. Platelet-rich plasma increases the levels of catabolic molecules and cellular dedifferentiation in the meniscus of a rabbit model. Int J Mol Sci. 2016;17:120. doi: 10.3390/ijms17010120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ogawa H., Matsumoto K., Sengoku M., Yoshioka H., Akiyama H. Arthroscopic repair of horizontal cleavage meniscus tears provides good clinical outcomes in spite of poor meniscus healing. Knee Surg Sports Traumatol Arthrosc. 2020;28:3474–3480. doi: 10.1007/s00167-019-05782-y. [DOI] [PubMed] [Google Scholar]
- 40.Zhu S., Li X., Lu Z., et al. Arthroscopic repair of degenerative medial meniscus tears in patients aged over 45 years resulted in favorable clinical outcomes and low clinical failure rates at a minimum 2-year follow-up. Knee Surg Sports Traumatol Arthrosc. 2022;31:1815–1823. doi: 10.1007/s00167-022-07133-w. [DOI] [PubMed] [Google Scholar]
- 41.Hoffelner T., Resch H., Forstner R., Michael M., Minnich B., Tauber M. Arthroscopic all-inside meniscal repair—Does the meniscus heal? A clinical and radiological follow-up examination to verify meniscal healing using a 3-T MRI. Skeletal Radiol. 2011;40:181–187. doi: 10.1007/s00256-010-0965-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.