Abstract
Purpose:
To examine trends and racial and ethnic disparities in early adolescent suicidal thoughts and behaviors in the years immediately prior to the COVID-19 pandemic.
Methods:
This study used pooled data from CDC’s middle school Youth Risk Behavior Survey (n=127,912) between 2015–2019. Three dichotomized measures of suicide-related behaviors were assessed: suicidal thoughts, planning, and attempts. Weighted prevalence estimates with 95% confidence intervals were calculated for each survey year. Linear trends examined disparities in the prevalence of suicidal thoughts and behaviors, overall and by student demographic characteristics. Main effects odds ratios compared estimates among racial and ethnic minority adolescents with non-Hispanic White students, controlling for sex and grade.
Results:
Significant linear increases were observed for the percentage of middle school students who reported seriously thinking about suicide (18.2% to 22.3%), ever making a suicide plan (11.8% to 14.7%), and ever attempting suicide (6.9% to 9.3%). Racial and ethnic minority students, other than non-Hispanic Asian, showed higher odds of suicidal thoughts and behaviors compared with non-Hispanic White students.
Conclusions:
Findings indicate a need for comprehensive suicide prevention to address health equity and disparities in suicide-related behaviors among middle school-aged adolescents.
Keywords: suicide, adolescent, middle school, health equity, racial disparities
Introduction
Since the emergence of COVID-19 in the U.S., much attention has been paid to understanding the pandemic’s impact on adolescent mental health. Data collected during the height of the pandemic demonstrate increased rates of poor mental health among adolescents, including increased reports of suicidal thoughts, attempts, and related emergency department visits.1,2 These findings validate present concern about adolescent mental health, suicidal thoughts, and behaviors during the pandemic.3 However, there is also evidence that adolescent mental health was in decline prior to the onset of COVID-19.4 As such, it is important to understand the status of youth mental health in the years immediately prior to the pandemic and consider the forces behind pre-pandemic trends for both younger and older adolescents alike.
Social determinants of health have long been utilized as indicators of youth well-being in the U.S. and provide a useful foundation for considering the social influences of health trends and disparities.5 In the decade prior to the pandemic, perceived inequities related to social determinants (e.g., economic security, family and social stability, physical and environmental safety) spurred several significant national responses and events, which researchers have also linked with the mental health outcomes of youth. For example, there is evidence that youth bystanders of fatal school shootings or community homicides show higher rates of anxiety, depression, and/or antidepressant use.6,7 Among Black youth, exposure to publicized police killings of Black individuals can contribute to poor mental health outcomes.8 Similarly, exposure to distressing rhetoric or policies targeting youth’s own identity or immigration status can negatively impact mental health through vicarious traumatization and increased violence victimization.8,9 Such research complements robust evidence of racism, discrimination, and violence as social and structural determinants of health that demonstrate significant impact on health, well-being, and quality of life.10,11 For example, these experiences have been shown to influence suicidal thoughts and behaviors among adolescents from racial and ethnic minority groups.12 Among youth ages 10–19, non-Hispanic American Indian/Alaska Native adolescents had the highest rates of suicide fatalities in 2021, followed by non-Hispanic White, non-Hispanic Black, non-Hispanic Asian, non-Hispanic more than one race, and Hispanic adolescents.13 Among high-school students, research on 20+ year suicide behavior trends highlights significant and enduring increases for racial and ethnic minority adolescents from 1991–2017, with Black adolescents experiencing the greatest increases in suicide attempts.14 Further, suicide rates among non-Hispanic Black youth aged 10–24 years increased significantly during 2018–2021.15 Such data demonstrate a need to further explore shifting trends in suicidal thoughts and behaviors among adolescents of different racial and ethnic groups, particularly during early adolescence where such patterns begin to emerge. Additionally, exploration of effective strategies to mitigate risk factors related to social determinants of health that may disproportionately burden adolescents from racial and ethnic minority groups is needed.
As adolescent mental health and suicide-related trends evolve, this study aims to address several gaps in the current literature. First, while research among younger adolescents is growing in many health topic areas (e.g., sexual health), less is known about younger adolescents’ mental health and suicidal thoughts and behaviors.16 Further, while existing research documents disproportionate COVID-19 burden – both physical and social/emotional – experienced by racial and ethnic minority populations within the U.S.,17 an understanding of the trajectories of racial and ethnic differences in adolescent suicide risk in the years immediately prior to the onset of COVID-19 is needed, particularly given existing research that links national events from this period with adolescent mental health outcomes.6–9 This analysis can help provide context to researchers and practitioners in the field seeking to understand the impact of the pandemic on suicidal thoughts and behaviors in younger adolescents and take informed public health action. As such, the purpose of this study was to investigate racial and ethnic differences in suicidal thoughts and behaviors in a sample of U.S. middle school adolescents during 2015–2019.
Methods
Study Population
This study used pooled data from the 2015 (n = 41,650), 2017 (n = 44,750), and 2019 (n = 41,512) middle school Youth Risk Behavior Surveys conducted in 10 states as part of CDC’s Youth Risk Behavior Surveillance System (YRBSS). The YRBSS includes cross-sectional, biennial school-based surveys conducted in states, territories, tribes, and local school districts since 1991. Each survey year since 1995, some states have collected data from select state-representative samples of middle school students (grades 6–8) who attend public schools. Participation in the survey is voluntary through a self-administered questionnaire and state agencies follow local parental permission procedures. Additional information about sampling, data collection, response rates, and processing is available for the high school Youth Risk Behavior Survey (YRBS).18 The middle school surveys follow the same procedures, except that samples are designed to represent students in grades 6–8. Youth Risk Behavior Surveys conducted in middle schools are exempt from IRB review at CDC because they are considered public health surveillance and not research. States conducting these surveys, however, follow all state and local IRB requirements.
Following standard practice for YRBSS, data from participating states with response rates of ≥60% for each survey year were weighted to be representative of that state. States needed 3 years of weighted data to be included in analyses. The analytic sample included 127,912 students from a combined middle school YRBS dataset for the years 2015–2019. Analyses included data from a total of 10 states (Delaware, Hawaii, Kentucky, Maine, New Mexico, North Dakota, Rhode Island, Vermont, Virginia, West Virginia); sample sizes and response rates varied across states and years.
Measures
The YRBS questionnaire asked two self-report questions about race and ethnicity: 1) “Are you Hispanic or Latino?” (Yes/No), and 2) “What is your race? (Select one or more responses).” Informed by prior research,19 responses were collapsed into seven categories for race and ethnicity including non-Hispanic White, Hispanic or Latino, non-Hispanic Black or African American, non-Hispanic Asian, non-Hispanic American Indian/Alaska Native, non-Hispanic Native Hawaiian/other Pacific Islander, and non-Hispanic multiple races. Questions related to sex and grade, which were used as covariates and to create relevant strata in analyses, included: “What is your sex?” (Male/Female) and “In what grade are you?” (6th grade, 7th grade, 8th grade, ungraded or other grade). Three questions assessed suicide behaviors and were all dichotomized (Yes/No): 1) “Have you ever seriously thought about killing yourself?” (Suicidal thoughts); 2) “Have you ever made a plan about how you would kill yourself?” (Suicide planning); and 3) “Have you ever tried to kill yourself?” (Suicide attempt).
Statistical Analysis
Data from the 2015, 2017, and 2019 YRBS were examined for trends in the prevalence of suicidal thoughts and behaviors by race and ethnicity. Data were analyzed using Stata (version 17) and assessed using complete case analysis; missing data were not included. Unadjusted weighted prevalence estimates of the suicide-related outcomes with 95% confidence intervals (CIs) were calculated for each survey year and each racial/ethnic subgroup. Logistic regression analyses controlling for sex and grade were used to assess linear trends, both overall and stratified by race and ethnicity, with each of the suicide-related variables serving as dichotomous outcomes. Survey year was treated as a continuous predictor variable and coded with orthogonal coefficients in Stata. Main effects odds ratios (ORs) of the suicide-related outcomes comparing adolescents in different racial and ethnic groups with non-Hispanic White adolescents were also calculated using multivariate logistic regression for the pooled 2015–2019 period, adjusting for sex and grade. In a subsequent model, sex-stratified main effects ORs were also calculated. Linear trends were considered statistically significant if p<0.05. Main effects ORs were considered statistically significant if 95% CIs did not include 1.0.
Results
Table 1 presents demographic and behavioral characteristics of the overall study sample. Of the 127,912 adolescents in the study, 51.4% were male and 48.6% were female, and there were fewer 6th grade students compared with 7th and 8th grade students (30.3% 6th graders, 35.0% 7th graders, 34.7% 8th graders). Most adolescents were non-Hispanic White (57.8%); 16.4% were Hispanic/Latino, 13.4% non-Hispanic Black or African American, 4.6% non-Hispanic Asian, 4.2% non-Hispanic multiple races, 2.1% non-Hispanic American Indian/Alaska Native, and 1.5% non-Hispanic Native Hawaiian/other Pacific Islander.
Table 1.
Demographic characteristics and suicidal thoughts and behaviors of U.S. middle school adolescents – 10 states*, Youth Risk Behavior Survey, 2015–2019
| Characteristics | Total No.† |
Prevalence % § |
|---|---|---|
| Ten state surveys combined * | 127,912 | 100.0 |
| Sex | ||
| Female | 63,075 | 48.6 |
| Male | 63,850 | 51.4 |
| Race/Ethnicity | ||
| White¶ | 66,827 | 57.8 |
| Hispanic/Latino | 20,245 | 16.4 |
| Black or African American¶ | 6,873 | 13.4 |
| Asian¶ | 6,114 | 4.6 |
| American Indian/Alaska Native¶ | 3,901 | 2.1 |
| Native Hawaiian/other Pacific Islander¶ | 6,816 | 1.5 |
| Multiple races¶ | 8,480 | 4.2 |
| Grade | ||
| 6th | 28,504 | 30.3 |
| 7th | 48,442 | 35.0 |
| 8th | 49.803 | 34.7 |
| Suicidal thoughts and behaviors | ||
| Suicidal thoughts | 25,767 | 20.3 |
| Suicide planning | 17,544 | 13.3 |
| Suicide attempt | 10,303 | 8.0 |
States included here: Delaware, Hawaii, Kentucky, Maine, New Mexico, North Dakota, Rhode Island, Vermont, Virginia, West Virginia
n = unweighted
prevalence = weighted
Non-Hispanic
Suicidal Thoughts
Between 2015–2019, overall suicidal thoughts among middle school adolescents significantly increased (β = 0.107), with 22.3% of adolescents reporting ever seriously having considered suicide as of 2019. Linear trends show variation by race and ethnicity, with non-Hispanic White (β = 0.107), Hispanic/Latino (β = 0.133), and non-Hispanic American Indian/Alaska Native (β = 0.136) middle school adolescents showing significant increases in reports of having ever seriously considered suicide during this period (Figure 1a; Table A1). Adolescents in every racial and ethnic group other than non-Hispanic Asian showed overall higher odds of suicidal thoughts compared with non-Hispanic White adolescents (Table 2). When stratified by sex, this trend persisted among female middle school adolescents. Among male adolescents, non-Hispanic Native Hawaiian/other Pacific Islander, non-Hispanic American Indian/Alaska Native, and non-Hispanic multiple race adolescents had significantly higher odds of suicidal thoughts compared with non-Hispanic White adolescents. Overall and among female and male adolescents, respectively, non-Hispanic Native Hawaiian/other Pacific Islander (aOR = 1.71; CI: 1.54, 1.91), non-Hispanic American Indian/Alaska Native (aOR = 1.47; CI: 1.31, 1.66), and non-Hispanic multiple race (aOR = 1.58; CI: 1.39, 1.81) adolescents demonstrated the highest odds of suicidal thoughts (Figure 2).
Figure 1.
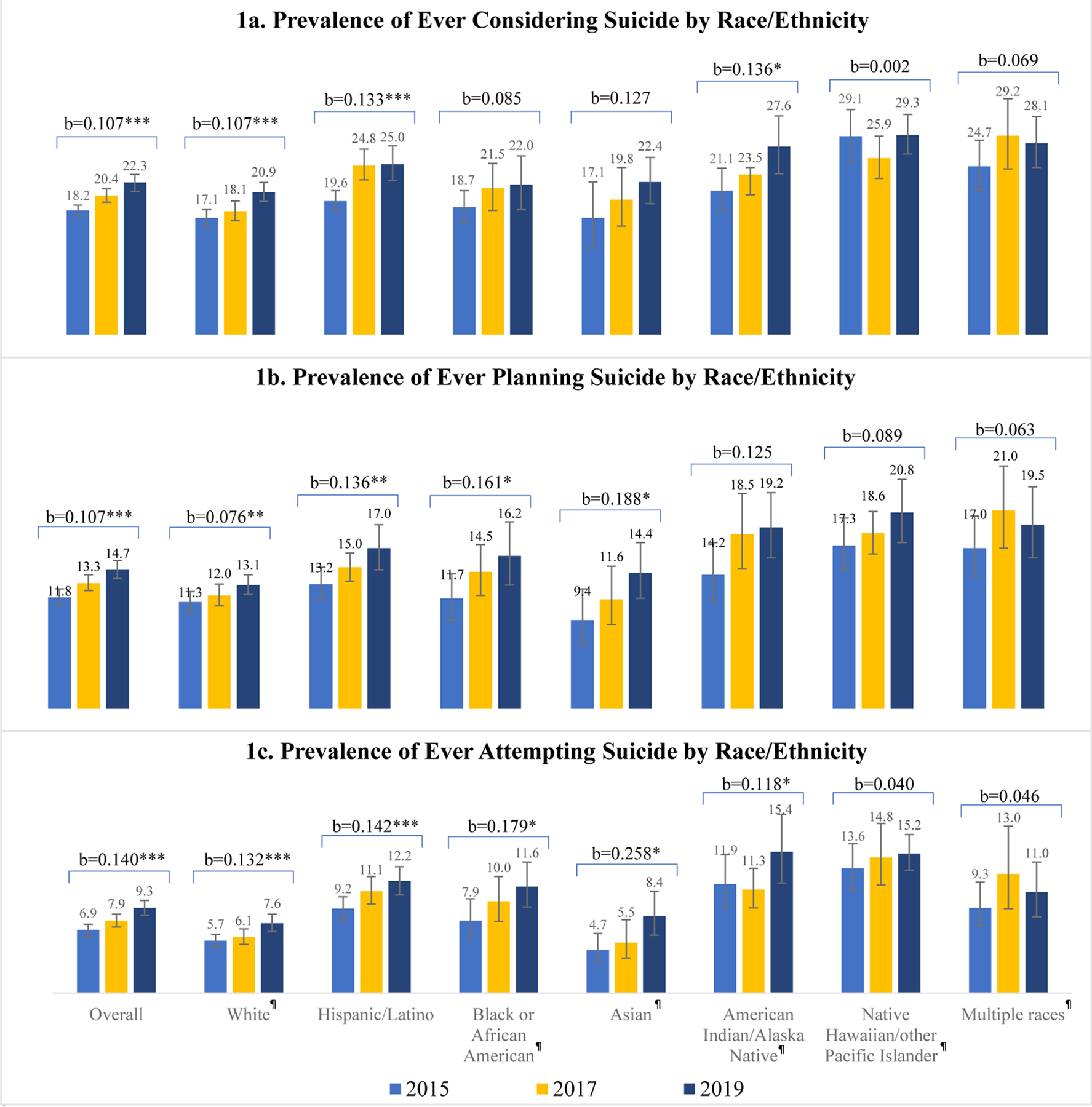
Linear trends in the prevalence of suicidal thoughts and behaviors among U.S. middle school adolescents, by race/ethnicity — 10 states, Youth Risk Behavior Survey, 2015–2019†
†Logistic regression models were used to assess linear trends in the prevalence of suicidal thoughts and behaviors by race/ethnicity for 2015–2019, controlling for sex and grade.
*Statistical significance is defined as p<0.05.
**Statistical significance is defined as p<0.01.
***Statistical significance is defined as p<0.001.
*Statistical significance is defined as 95% Confidence Interval that does not include 1.00.
¶ Non-Hispanic
Table 2. .
Adjusted odds ratios for suicidal thoughts and behaviors among U.S. middle school adolescents, by race/ethnicity and sex – 10 states, Youth Risk Behavior Survey, 2015–2019
| Suicidal Thoughts and Behaviors | Main Effect† | Female | Male |
|---|---|---|---|
| aOR (95%CI) | aOR (95%CI) | aOR (95%CI) | |
| Suicidal thoughts (ever) | |||
| White¶ | 1.0 (Ref.) | 1.0 (Ref.) | 1.0 (Ref.) |
| Hispanic/Latino | 1.35 (1.24, 1.46) | 1.55 (1.40, 1.71) | 1.07 (0.95, 1.22) |
| Black or African American¶ | 1.20 (1.03, 1.39) | 1.31 (1.14, 1.50) | 1.04 (0.82, 1.32) |
| Asian¶ | 1.06 (0.91, 1.25) | 1.17 (0.96, 1.41) | 0.92 (0.70, 1.20) |
| American Indian/Alaska Native¶ | 1.47 (1.31, 1.66) | 1.64 (1.43, 1.87) | 1.23 (1.06, 1.52) |
| Native Hawaiian/other Pacific Islander¶ | 1.71 (1.54, 1.91) | 1.86 (1.63, 2.13) | 1.51 (1.30, 1.76) |
| Multiple races¶ | 1.58 (1.39, 1.81) | 1.62 (1.36, 1.94) | 1.53 (1.23, 1.92) |
| Suicide planning (ever) | |||
| White¶ | 1.0 (Ref.) | 1.0 (Ref.) | 1.0 (Ref.) |
| Hispanic/Latino | 1.32 (1.21, 1.43) | 1.50 (1.34, 1.68) | 1.04 (0.93, 1.19) |
| Black or African American¶ | 1.27 (1.06, 1.51) | 1.46 (1.20, 1.76) | 1.01 (0.77, 1.32) |
| Asian¶ | 0.97 (0.81, 1.17) | 1.10 (0.85, 1.42) | 0.79 (0.62, 1.00) |
| American Indian/Alaska Native¶ | 1.63 (1.40, 1.89) | 1.90 (1.58, 2.29) | 1.28 (1.04, 1.58) |
| Native Hawaiian/other Pacific Islander¶ | 1.69 (1.45, 1.97) | 1.76 (1.52, 2.04) | 1.57 (1.19, 2.08) |
| Multiple races¶ | 1.66 (1.42, 1.95) | 1.71 (1.39, 2.11) | 1.59 (1.26, 2.02) |
| Suicide attempt (ever) | |||
| White¶ | 1.0 (Ref.) | 1.0 (Ref.) | 1.0 (Ref.) |
| Hispanic/Latino | 1.80 (1.60, 2.02) | 1.98 (1.73, 2.27) | 1.50 (1.25, 1.81) |
| Black or African American¶ | 1.67 (1.38, 2.02) | 1.89 (1.54, 2.32) | 1.33 (1.00, 1.76) |
| Asian¶ | 0.96 (0.77, 1.20) | 1.13 (0.88, 1.46) | 0.68 (0.50, 0.92) |
| American Indian/Alaska Native¶ | 2.29 (1.93, 2.72) | 2.65 (2.16, 3.25) | 1.77 (1.28, 2.46) |
| Native Hawaiian/other Pacific Islander¶ | 2.50 (2.16, 2.88) | 2.66 (2.23, 3.16) | 2.24 (1.82, 2.75) |
| Multiple races¶ | 1.71 (1.41, 2.08) | 1.64 (1.29, 2.09) | 1.88 (1.39, 2.55) |
Abbreviations: aOR = adjusted odds ratio; CI = confidence interval; Ref. = referent group.
Statistical significance is defined as 95% CI that does not include 1.00.
Logistic regression models were used to assess pooled odds of suicidal thoughts and behaviors by race/ethnicity for 2015–2019, controlling for sex and grade.
Non-Hispanic
Figure 2.
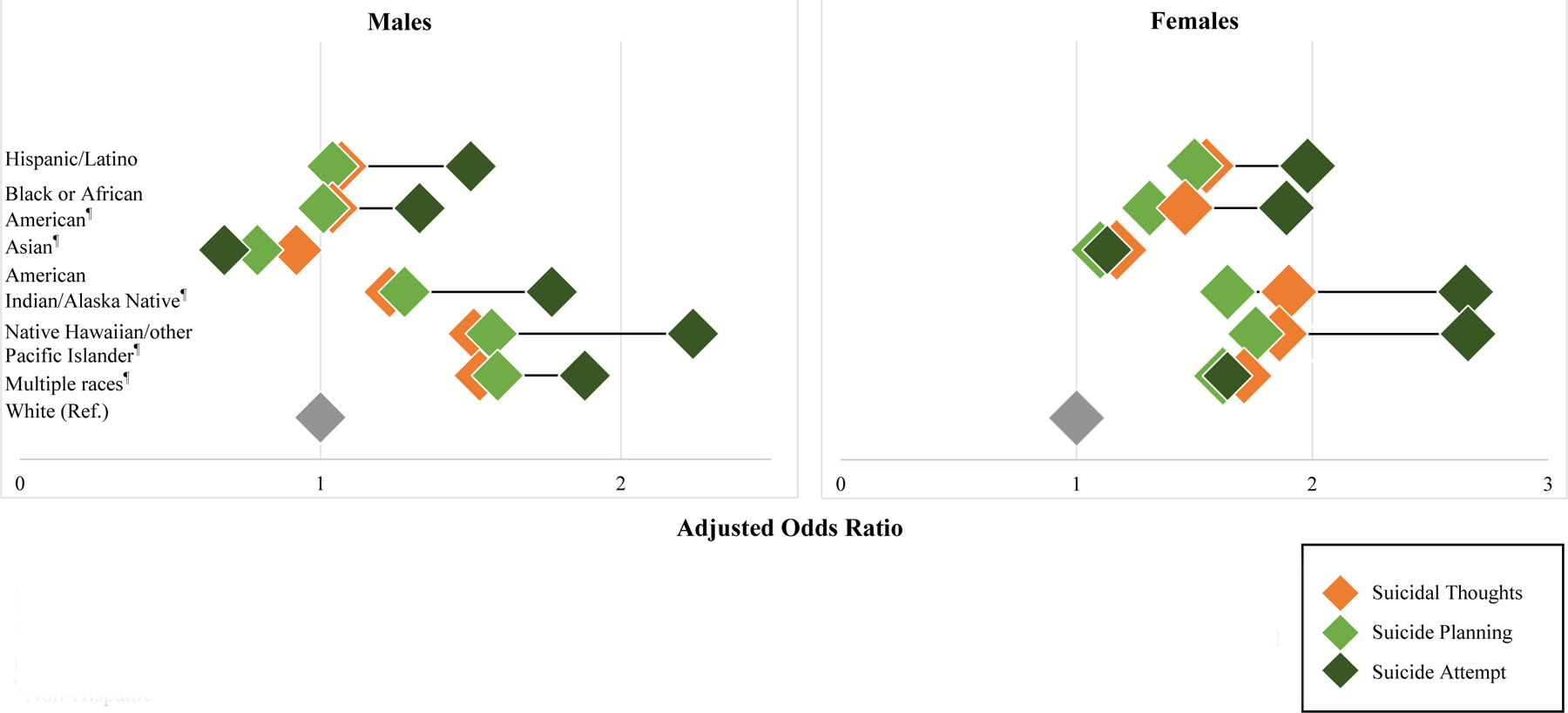
Adjusted odds of suicidal thoughts and behaviors among U.S. middle school adolescents, by sex and race/ethnicity – 10 states, Youth Risk Behavior Survey, 2015–2019†
Abbreviations: aOR = adjusted odds ratio; CI = confidence interval; Ref. = referent group.
*See Table 2 for aORs and Cis
†Logistic regression models were used to assess pooled odds of suicidal thoughts and behaviors by race/ethnicity for 2015–2019, stratified by sex.
¶ Non-Hispanic
Suicide Planning
Reports of ever making a suicide plan also showed a significant overall increase among middle school adolescents between 2015–2019 (β = 0.105), with 14.7% of adolescents in 2019 reporting ever having made a suicide plan. Looking at trends among racial and ethnic groups, this significant increase occurred among non-Hispanic White (β = 0.076), Hispanic/Latino (β = 0.136), non-Hispanic Black or African American (β = 0.161), and non-Hispanic Asian (β = 0.188) adolescents. Although American Indian/Alaska Native, non-Hispanic Native Hawaiian/other Pacific Islanders, and non-Hispanic multiple race adolescents did not demonstrate statistically significant increases, they had consistently higher reports of making a suicide plan compared with the overall sample across years (Figure 1b; Table A1). Like suicidal thoughts, adolescents in every racial and ethnic group other than non-Hispanic Asian adolescents showed significantly higher odds of suicide planning compared with non-Hispanic White adolescents (Table 2). Again, this trend persisted among female middle school adolescents when stratified by sex. Among male adolescents, non-Hispanic Native Hawaiian/other Pacific Islander, non-Hispanic American Indian/Alaska Native, and non-Hispanic multiple race adolescents had significantly higher odds of suicide compared with non-Hispanic White adolescents. Non-Hispanic Native Hawaiian/other Pacific Islander, non-Hispanic American Indian/Alaska Native, and non-Hispanic multiple race adolescents had the highest odds of suicide planning, overall (aORs = 1.69; 1.63; 1.66), and these disparities persisted when stratified by sex (Figure 2).
Suicide Attempt
In line with increases in suicide thoughts and planning between 2015–2019, linear trends show significant overall increases in suicide attempts among middle school adolescents during this period (β = 0.140), with 9.3% of adolescents in 2019 reporting ever having attempted suicide. Among racial and ethnic groups, a significant increase in suicide attempts occurred among non-Hispanic White (β = 0.132), Hispanic/Latino (β = 0.142), non-Hispanic Black or African American (β = 0.161), and non-Hispanic Asian (β = 0.188) adolescents. However – as with suicidal thoughts and planning – while non-Hispanic American Indian/Alaska Native, non-Hispanic Native Hawaiian/other Pacific Islanders, and non-Hispanic multiple race adolescents did not demonstrate statistically significant increases, they had consistently higher prevalence of suicide attempts compared with the overall sample across years (Figure 1c; Table A1). Also, like suicidal thoughts and planning, adolescents in all racial and ethnic groups other than non-Hispanic Asian adolescents had higher overall odds of attempting suicide compared with non-Hispanic White adolescents (Table 2). When stratified by sex, trends persisted among female adolescents; among male adolescents, however, Hispanic/Latino, non-Hispanic Native Hawaiian/other Pacific Islander, non-Hispanic American Indian/Alaska Native, and non-Hispanic multiple race adolescents had significantly greater odds of suicide attempts compared with non-Hispanic White adolescents; non-Hispanic Asian male adolescents showed significantly lower odds of suicide attempt (aOR = 0.68; CI: 0.50, 0.92). Non-Hispanic Native Hawaiian/other Pacific Islander and non-Hispanic American Indian/Alaska Native had approximately two times the odds of suicide attempts compared with non-Hispanic White adolescents, and these disparities persisted when stratified by sex (Figure 2).
Discussion
Our research demonstrates an increase in suicidal thoughts, planning, and attempts among U.S. middle school students in the years immediately prior to the COVID-19 pandemic. Further, we found disparities in suicide trends and risk by race, ethnicity, and sex. Between 2015–2019, significant linear increases in suicide thoughts occurred among White, Hispanic/Latino, and American Indian/Alaska Native youth. For suicide planning and attempt, these linear increases were significant for White, Hispanic/Latino, Black or African American, and Asian middle school youth. Non-Hispanic Native Hawaiian/other Pacific Islander youth consistently were among the groups with the highest prevalence for suicide thoughts, planning, and attempt across years. Additionally, compared with White, non-Hispanic youth, these adolescents often had the highest odds of suicide thoughts, planning, and attempt for both males and females.
This research fills a gap in the field’s understanding of multi-year trends in suicidal thoughts and behaviors among younger adolescents. Increasing trends for this age group are comparable to high school aged adolescents,20 and findings corroborate existing research showing recent increases in suicide behaviors, experiences, and deaths among younger and older adolescents.21–23 Further, findings allude to the presence of pre-pandemic forces that may have influenced an upward trajectory of suicidal thoughts and behaviors among early adolescents between 2015–2019. With recent literature noting increases in adolescent mental health challenges since the pandemic,1,23 this trajectory of trends in the years leading up to the pandemic’s onset offers the field a critical and more complete context within which to understand and evaluate adolescent suicide-related behaviors, risk, and trends in the coming years. Additionally, it reinforces calls for increased attention to the mental health of children and younger adolescents in both research and practice.3,23 Future studies investigating persistent trends in young adolescents’ suicidal thoughts and behaviors throughout pandemic recovery are needed.
This research also captures significant racial and ethnic differences in suicide trends between 2015–2019. In alignment with previous research on older adolescents,20,23 we found younger adolescents from racial and ethnic minority groups (apart from non-Hispanic Asian adolescents) had a higher prevalence and odds of suicidal thoughts and behaviors compared with their non-Hispanic White peers. Significant increases in more serious suicidal behaviors across many racial and ethnic minority groups are of particular concern. For example, while Black or African American and Asian adolescents did not demonstrate significant linear increases in suicidal thoughts between 2015–2019, they did experience significant increases in more serious suicidal behaviors (i.e., suicide planning and attempt). For Hispanic/Latino, Black or African American, and Asian adolescents, rates of increase for suicide planning and attempt were also greater than for suicidal thoughts. Although adolescents identifying as American Indian/Alaska Native, Native Hawaiian/other Pacific Islander, and Multiple races did not demonstrate significant linear increases in more serious suicide behaviors (apart from suicide attempts for American Indian/Alaska Native adolescents), these groups consistently had some of the highest prevalence of suicide planning and attempts compared with other racial and ethnic groups. When looking at patterns by sex and race/ethnicity, both for male and female adolescents, all racial and ethnic groups (except for Asian males) had higher odds of suicidal thoughts, planning, and attempt compared with their White peers of the same sex, and the difference in odds was greatest for the most serious of suicidal behaviors (suicide attempts) (Figure 2).
Trends toward more serious suicide behaviors in early adolescence help contextualize recent increases in suicide deaths among 10–14 year olds.22 Though non-Hispanic White 10–14-year-olds have higher prevalence of suicide death than most other racial and ethnic groups (apart from American Indian/Alaska Native), suicide deaths among adolescents in racial and ethnic minority groups increased at higher rates than White adolescents between 2015–2019.22 Findings from this study expand upon research among older adolescents that show racial, ethnic, and sex differences in more serious suicide behaviors, but among fewer racial and ethnic groups.14,15,20,21 To understand the mechanisms behind such trends, research that represents more racial and ethnic groups within both younger and older adolescent populations is needed.
These patterns may be affected by experiences with racism and discrimination – stressors that are directly linked with depressive symptoms and psychiatric distress that may increase risk for suicide.24 In a recent study by Mpofu et al., researchers found over one-third of U.S. high school adolescents perceived racism in school, and these adolescents also experienced a higher prevalence of poor mental health outcomes compared with peers who did not perceive racism in school.19 Disparities in the burden of other social and behavioral risk factors for suicide, such as structural racism, adverse childhood experiences, poverty may also serve as stressors contributing to increased racial and ethnic disparities in suicide-related behaviors.3,24,25 Such risk factors are compounded by disparities in access to mental health services for lower-income, rural, and racial and ethnic minority populations,26,27 as well as a lack of culturally responsive providers who reflect the diversity of the U.S. population.28 These stressors existed and were the focus of national attention prior to the pandemic. Coupled with research demonstrating that such stressors may have been exacerbated by COVID-19, there is a critical need for suicide prevention strategies across multiple sectors.29
Suicide prevention strategies in school, healthcare, and community settings can help to address racial and ethnic disparities and promote mental health and well-being among U.S. adolescents. In school settings, comprehensive K-12 health education that attends to mental and emotional health can help students gain essential health knowledge and skills (e.g., emotional regulation, coping, relationship-building) that foster emotional self-efficacy and reduce risk for suicidal thoughts and attempt in adolescence.30,31 Although recent nationwide estimates suggests that over 80% of secondary schools provide suicide prevention to students in grades 6–12 through required courses,32 few programs explicitly designed for and evaluated among middle school students exist.33 Our findings from a sample of younger adolescents suggest a need for future research focused on comprehensive and developmentally appropriate suicide prevention education for students beginning before and throughout middle school.
In complement to educational curricula, school-wide approaches are important for building broader awareness among students, parents and caregivers, and school personnel about warning signs of mental health conditions and suicidality, as well as about how to connect others to care or a trusted adult.30 Ensuring that such approaches are inclusive of and responsive to the specific mental health challenges and experiences of adolescents, families, and school personnel who have been historically marginalized (e.g., racial and ethnic minority groups, sexual and gender minority groups) or experienced other hardship or trauma is also vital to address documented disparities in suicide-related behaviors and experiences. Purposeful implementation of robust school policies and practices to promote inclusivity and equity (e.g., restorative practices, trauma-informed approaches), and to address both direct and indirect discrimination experienced by racial and ethnic minority adolescents, are also essential for creating learning environments that reduce “minority stress” and facilitate peer and school connectedness to promote mental health and well-being in both middle and high school settings.31,34,35
In partnership with primary care and community mental health providers, schools also play a key role in suicide prevention through the implementation of school-based health services and referral systems.36 On-site school-based mental health services delivered by trained mental health professionals can reduce key barriers to mental healthcare such as transportation, cost, and stigma, and research supports the use of targeted interventions and referral systems in reducing mental health problems among children and adolescents.37 Additionally, school-based mental health services can have a positive effect on academic engagement and performance by reducing missed instructional time for youth seeking care.38 However, such approaches require strong school-community partnerships with primary care and community-based health providers,39 as well as a robust pediatric mental health workforce trained to provide developmentally appropriate, trauma-informed, and culturally relevant care to children and adolescents from diverse backgrounds, communities, and regions in the U.S.3,31 Evidence suggests that community mental health providers may be particularly well-suited to mitigate mental health disparities in low-income and racially and ethnically diverse communities in the U.S.40 As such, school leaders and primary care physicians may consider ways in which to strengthen collaborations with community health workers in the delivery of evidence-based mental health interventions. Multi-level investments in mental health infrastructure and workforce training across federal, state, and local levels may be helpful in facilitating this work to mitigate inequities in access and care.31
For both educational and healthcare institutions alike, engaging and partnering with parents and caregivers in mental health promotion and suicide prevention efforts is also recommended.31 Research shows that family members can play a key role in reducing suicide risk for children;41 however, not all parents and caregivers may have the knowledge or self-efficacy needed to intervene when their child exhibits mental health challenges or suicidality.42 Additionally, stigma related to help-seeking for suicidal thoughts and behaviors along with high costs for suicide care are barriers that some parents/caregivers face.31 Schools and health providers can engage families in suicide prevention, first, by establishing clear communication protocol to inform parents and caregivers about child mental health concerns. Further, families should be informed about who they can contact in school or clinical settings if they are concerned about their child’s wellbeing, as well as about how and where to seek additional professional mental health supports for their child, if needed. Beyond communication, creating opportunities for parents and caregivers to gain knowledge and skills related to suicide prevention and talking with their children about mental health may increase self-efficacy and decrease stigmatizing attitudes that serve as barriers to parent-led prevention and intervention.31,42
Limitations
This analysis is subject to at least four limitations. First, data represent students attending public middle schools in states included in the analysis (n=10). Although every state included in the study had three years of state-representative data, these data are not nationally representative. Demographically, White students were slighted over-represented in the sample compared with the U.S. school-aged population (57.8% in sample; 48% U.S.), while Black or African American (13.4% in sample; 15% U.S.) were and Hispanic/Latino students (16.4% in sample; 27% U.S.) were under-represented. While the proportion of male and female respondents was comparable to the U.S. school-aged population, non-binary gender response options were not offered in YRBS for these survey years; as such, trends for non-binary middle school students were not assessed. YRBS data are also self-reported, and as such, both over- and underreporting are possible. Additional general limitations regarding the YRBSS and YRBS sampling and methodologies can be found in the YRBS methodology report.18 Second, only three cycles of YRBS data were available and included in this study, not allowing for a more robust assessment of pre-pandemic trends. Further, YRBS measures lifetime prevalence of suicidal thoughts and behaviors, which could have occurred prior to the 2015–2019 period of focus. As such, continued research on suicide-related behavior and experience trends among young adolescents is important, as is continued examination of disparities in these trends among historically marginalized youth. A third limitation is the potential statistical underpowering of racial and ethnic subgroups included in analysis. Smaller sample sizes for non-Hispanic American Indian/Alaska Native and non-Hispanic Native Hawaiian/Pacific Islander populations may have prevented us from detecting significant trends. However, analyses still found that these groups of youth may have the highest levels of suicide risk, and intentional efforts to support these youth and reduce suicidal thoughts and behaviors are needed. Sample size constraints also prompted the classification of all students who identified as Hispanic/Latino into one group, limiting our ability to explore suicide trends among students who identify as Hispanic/Latino and with a racial minority group. Related, covariates associated with suicidal thoughts and behaviors and experiences, such as bullying and substance use, were not included in analyses due to small sample sizes within racial and ethnic subgroups, representing another limitation of the study. Future studies on suicidal thoughts and behaviors among younger adolescents may benefit from oversampling of racial and ethnic minority youth underrepresented in research, such as American Indian/Alaska Native and Native Hawaiian/Pacific Islander youth, to better characterize patterns of risk experienced by these youth.
Conclusion
Among younger adolescents, suicidal thoughts and behaviors showed significant increases prior to the COVID-19 pandemic with demonstrated racial and ethnic disparities. Research from other studies has also demonstrated that stress from the COVID-19 pandemic and other prior traumatic social events have disproportionately affected youth and families from racial and ethnic minority groups, potentially exacerbating these disparities and demonstrating a continued public health need for action that addresses sizable disparities, particularly in the wake of COVID-19.3,29 Schools, communities, and healthcare providers can play a role in addressing structural racism, inequities, and barriers to mental health access and care, buffering its effects on adolescents during key developmental periods and transitions. Additionally, future studies that assess the impact of suicide prevention programs in multiple settings across ages (e.g., kindergarten through grade 12), and utilizing data that allows for analysis of multiple adolescent identities, contextual factors, and co-occurring behaviors associated with suicidal thoughts and behaviors can enhance the field’s understanding of a comprehensive public health approach to prevention based on the best available evidence for suicide prevention.31
Supplementary Material
Implications and Contribution:
In complement to prior research on older adolescents, findings highlight a concerning trajectory of early adolescent suicide trends and disparities in the years leading up to the COVID-19 pandemic, offering a more complete context for understanding and evaluating middle school-aged adolescents’ suicide thoughts and behaviors during the pandemic.
Acknowledgements:
The authors have no acknowledgements to name.
Footnotes
Conflicting Interests: The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Disclaimer: The findings and conclusions in the manuscript are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- 1.Jones SE, Ethier KA, Hertz M, DeGue S, Le VD, Thornton J, Lim C, Dittus PJ, Geda S. Mental health, suicidality, and connectedness among high school students during the COVID-19 pandemic — Adolescent Behaviors and Experiences Survey, United States, January–June 2021. MMWR Suppl 2022;71(Suppl-3):16–21. 10.15585/mmwr.su7103a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yard E, Radhakrishnan L, Ballesteros MF, Sheppard M, Gates A, Stein Z, Hartnett K, Kite-Powell A, Rodgers L, Adjemian J, Ehlman DC, Holland K, Idaikkadar N, Ivey-Stephenson A, Martinez P, Law R, Stone DM. Emergency department visits for suspected suicide attempts among persons aged 12–25 years before and during the COVID-19 pandemic - United States, January 2019-May 2021. MMWR Morb Mortal Wkly Rep 2021;70(24):888–894. 10.15585/mmwr.mm7024e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.American Academy of Pediatrics. AAP-AACAP-CHA Declaration of a National Emergency in Child and Adolescent Mental Health, https://www.aap.org/en/advocacy/child-and-adolescent-healthy-mental-development/aap-aacap-cha-declaration-of-a-national-emergency-in-child-and-adolescent-mental-health/; 2021
- 4.Kauhanen L, Wan Mohd Yunus W, Lempinen L, Peltonen K, Gyllenberg D, Mishina K, Gilbert S, Bastola K, Brown J, Sourander A. A systematic review of the mental health changes of children and young people before and during the COVID-19 pandemic. Eur Child Adolesc Psychiatry 2023; 32:995–1013. 10.1007/s00787-022-02060-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Krause KH, Verlenden JV, Szucs LE, Swedo EA, Merlo CL, Holditch Niolon P, Leroy ZC, Sims VM, Deng X, Lee S, Rasberry CN, Underwood JM. Disruptions to School and Home Life Among High School Students During the COVID-19 Pandemic - Adolescent Behaviors and Experiences Survey, United States, January-June 2021. MMWR Suppl 2022;71(3):28–34. doi: 10.15585/mmwr.su7103a5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cimolai V, Schmitz J, Sood AB. Effects of mass shootings on the mental health of children and adolescents. Curr Psychiatry Reps 2021;23:1–10. 10.1007/s11920-021-01222-2 [DOI] [PubMed] [Google Scholar]
- 7.Leibbrand C, Hill H, Rowhani-Rahbar A, Rivara F. Invisible wounds: Community exposure to gun homicides and adolescents’ mental health and behavioral outcomes. SSM Popul Health 2020;12:100689. doi: 10.1016/j.ssmph.2020.100689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tynes BM, Willis HA, Stewart AM, Hamilton MW. Race-related traumatic events online and mental health among adolescents of color. J Adolesc Health 2019;65(3):371–377. 10.1016/j.jadohealth.2019.03.006 [DOI] [PubMed] [Google Scholar]
- 9.Eskenazi B, Fahey CA, Kogut K, Gunier R, Torres J, Gonzales NA, Holland N, Deardorff J. Association of perceived immigration policy vulnerability with mental and physical health among US-born Latino adolescents in California. Pediatrics 2019;173(8):744–753. 10.1001/jamapediatrics.2019.1475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Trent M, Dooley DG, Dougé J. Section on Adolescent Health, Council on Community Pediatrics, Committee on Adolescence. The impact of racism on child and adolescent health. Pediatrics 2019;144(2):e20191765. 10.1542/peds.2019-1765 [DOI] [PubMed] [Google Scholar]
- 11.Bailey ZD, Krieger N, Agénor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: evidence and interventions. Lancet 2017;389(10077):1453–1463. doi: 10.1016/S0140-6736(17)30569-X [DOI] [PubMed] [Google Scholar]
- 12.Oh H, Stickley A, Koyanagi A, Yau R, DeVylder JE. Discrimination and suicidality among racial and ethnic minorities in the United States. J Affect Disord 2019;245:517–523. 10.1016/j.jad.2018.11.059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention. Centers for Disease Control and Prevention, National Center for Health Statistics. National Vital Statistics System, Mortality 2018–2021 on CDC WONDER Online Database, released in 2021, http://wonder.cdc.gov/ucd-icd10-expanded.html. Data are from the Multiple Cause of Death Files, 2018-2021, as compiled from data provided by the 57 vital statistics jurisdictions through the Vital Statistics Cooperative Program; 2021.
- 14.Lindsey MA, Sheftall AH, Xiao Y, Joe S. Trends of suicidal behaviors among high school students in the United States: 1991–2017. Pediatrics 2019;144 (5): e20191187. 10.1542/peds.2019-1187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stone DM, Mack KA, Qualters J. Notes from the field: Recent changes in suicide rates, by race and ethnicity and age group — United States, 2021. MMWR Morb Mortal Wkly Rep 2023;72:160–162. 10.15585/mmwr.mm7206a4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moore MJ, Barr EM, Johnson TM. (2013). Sexual behaviors of middle school students: 2009 Youth Risk Behavior Survey results from 16 locations. J Sch Health 2013;83(1):61–68. 10.1111/j.1746-1561.2012.00748.x [DOI] [PubMed] [Google Scholar]
- 17.Fortuna LR, Tolou-Shams M, Robles-Ramamurthy B, Porche MV. Inequity and the disproportionate impact of COVID-19 on communities of color in the United States: The need for a trauma-informed social justice response. Psychol Trauma 2020;12(5):443–445. 10.1037/tra0000889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Underwood JM, Brener N, Thornton J, Harris WA, Bryan LN, Shanklin SL, Deputy N, Roberts AM, Queen B, Chyen D, Whittle L, Lim C, Yamakawa Y, Leon-Nguyen M, Kilmer G, Smith-Grant J, Demissie Z, Jones SE, Clayton H, Dittus P. Overview and methods for the Youth Risk Behavior Surveillance System - United States, 2019. MMWR Suppl 2020;69(1):1–10. 10.15585/mmwr.su6901a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mpofu JJ, Cooper AC, Ashley C, Geda S, Harding RL, Johns MM, Spinks Franklin A, Njai R, Moyse D, Underwood JM. Perceived racism and demographic, mental health, and behavioral characteristics among high school students during the COVID-19 pandemic - Adolescent Behaviors and Experiences Survey, United States, January-June 2021. MMWR Suppl 2022;71(3):22–27. 10.15585/mmwr.su7103a4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ivey-Stephenson AZ, Demissie Z, Crosby AE, Stone DM, Gaylor E, Wilkins N, Lowry R, Brown M. Suicidal ideation and behaviors among high school students — Youth Risk Behavior Survey, United States, 2019. MMWR Suppl 2020;69(Suppl-1):47–55. 10.15585/mmwr.su6901a6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ruch DA, Sheftall AH, Schlagbaum P, Rausch J, Campo JV, Bridge JA. Trends in suicide among youth aged 10 to 19 years in the United States, 1975 to 2016. JAMA Netw Open 2019;2(5):e193886. 10.1001/jamanetworkopen.2019.3886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention. Web-based Injury Statistics Query and Reporting System (WISQARS): Leading causes of death and injury reports, www.cdc.gov/ncipc/wisqars; 2022.
- 23.Centers for Disease Control and Prevention. Youth Risk Behavior Survey: Data Summary and Trends Report, 2011–2021, https://www.cdc.gov/healthyyouth/data/yrbs/pdf/YRBS_Data-Summary-Trends_Report2023_508.pdf; 2023.
- 24.Pascoe EA, Smart Richman L. Perceived discrimination and health: a meta-analytic review. Psychol Bull 2009;135(4):531–54. 10.1037/a0016059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lee CS, Wong YJ. Racial/ethnic and gender differences in the antecedents of youth suicide. Cultur Divers Ethnic Minor Psychol 2020;26(4):532–543. 10.1037/cdp0000326 [DOI] [PubMed] [Google Scholar]
- 26.Whitney DG, Peterson MD. US national and state-level prevalence of mental health disorders and disparities of mental health care use in children. JAMA Pediatrics 2019;173(4):389–391. 10.1001/jamapediatrics.2018.5399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Duong MT, Bruns EJ, Lee K, Cox S, Coifman J, Mayworm A, Lyon AR. Rates of mental health service utilization by children and adolescents in schools and other common service settings: A systematic review and meta-analysis. Adm Policy Ment Health, 2021;48(3):420–439. 10.1007/s10488-020-01080-9 [DOI] [PubMed] [Google Scholar]
- 28.Cama SF, Sehgal P. Racial and ethnic considerations across child and adolescent development. Acad Psychiatry 2021;45:106–109. 10.1007/s40596-020-01354-2 [DOI] [PubMed] [Google Scholar]
- 29.Liu SR, Davis EP, Palma AM, Stern HS, Sandman CA, Glynn LM. Experiences of COVID-19-related racism and impact on depression trajectories among racially/ethnically minoritized adolescents. J Adolesc Health 2021;S1054–139X(23):00011–3. Advance online publication. 10.1016/j.jadohealth.2022.12.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zalsman G, Hawton K, Wasserman D, van Heeringen K, Arensman E, Sarchiapone M, Carli V, Höschl C, Barzilay R, Balazs J, Purebl G, Kahn JP, Sáiz PA, Lipsicas CB, Bobes J, Cozman D, Hegerl U, Zohar J. Suicide prevention strategies revisited: 10-year systematic review. Lance Psychiat 2016;3(7):646–659. 10.1016/S2215-0366(16)30030-X [DOI] [PubMed] [Google Scholar]
- 31.Centers for Disease Control and Prevention. National Center for Injury Prevention and Control. Suicide Prevention Resource for Action: A Compilation of the Best Available Evidence, https://www.cdc.gov/suicide/pdf/preventionresource.pdf; 2022.
- 32.Centers for Disease Control and Prevention. School Health Profiles 2020: Characteristics of Health Programs Among Secondary Schools, https://www.cdc.gov/healthyyouth/data/profiles/pdf/2020/cdc-profiles-2020.pdf, 2022
- 33.Surgenor PWG, Quinn P, Hughes C. Ten recommendations for effective school-based, adolescent, suicide prevention programs. Sch Ment Health 2016;8:413–424. 10.1007/s12310-016-9189-9 [DOI] [Google Scholar]
- 34.Marraccini ME, Brier ZMF. School connectedness and suicidal thoughts and behaviors: A systematic meta-analysis. Sch Psychol Q 2017;32(1):5–21 10.1037/spq0000192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Augustine CH, Engberg J, Grimm GE, Lee E, Wang EL, Christianson K, Joseph AA. Can restorative practices improve school climate and curb suspensions? An evaluation of the impact of restorative practices in a mid-sized urban school district, https://www.rand.org/content/dam/rand/pubs/research_reports/RR2800/RR2840/RAND_RR2840.pdf; 2018.
- 36.Ali MM, West K, Teich JL, Lynch S, Mutter R, Dubenitz J. Utilization of mental health services in educational setting by adolescents in the United States. J School Health 2019;89:393–401. 10.1111/josh.12753 [DOI] [PubMed] [Google Scholar]
- 37.Sanchez AL, Cornacchio D, Poznanski B, Golik AM, Chou T, Comer JS. The effectiveness of school-based mental health services for elementary-aged children: A meta-analysis. J Am Acad Child Adolesc Psychiatry, 2018;57(3):153–165. 10.1016/j.jaac.2017.11.022 [DOI] [PubMed] [Google Scholar]
- 38.Suldo SM, Gormley MJ, DuPaul GJ, Anderson-Butcher D. The impact of school mental health on student and school-level academic outcomes: Current status of the research and future directions. Sch Ment Health 2014;6:84–98. 10.1007/s12310-013-9116-2 [DOI] [Google Scholar]
- 39.Hertz MF, Barrios LC. Adolescent mental health, COVID-19, and the value of school-community partnerships. Inj Prev 2021;27:85–86. 10.1136/injuryprev-2020-044050 [DOI] [PubMed] [Google Scholar]
- 40.Barnett ML, Gonzalez A, Miranda J, Chavira DA, Lau AS. Mobilizing community health workers to address mental health disparities for underserved populations: A systematic review. Adm Policy Ment Health, 2018;45(2):195–211. 10.1007/s10488-017-0815-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hom MA, Stanley IH, Joiner TE. Evaluating factors and interventions that influence help-seeking and mental health service utilization among suicidal individuals: A review of the literature. Clin Psychol Rev 2015;40:28–39. 10.1016/j.cpr.2015.05.006 [DOI] [PubMed] [Google Scholar]
- 42.Schuck A, Gryglewicz K, Bender A, Nam E, McNeil M, Cosare M, Rosler M, Karver M. Examining the effectiveness of a family-focused training to prevent youth suicide. Fam Relat 2023;72(1):325–346. 10.1111/fare.12700 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


