Abstract
Purpose of Review
Mast cell (MC) activation syndromes (MCAS) are conditions defined by recurrent episodes of severe systemic anaphylaxis or similar systemic events triggered by MC-derived mediators that can be measured in biological fluids. Since some symptoms of MC activation may occur due to other, non-MC etiologies and lead to confusion over diagnosis, it is of crucial importance to document the involvement of MC and their products in the patients´ symptomatology.
Recent Findings
The most specific and generally accepted marker of severe systemic MC activation is an event-related, transient increase in the serum tryptase level over the individual baseline of the affected individual. However, baseline concentrations of serum tryptase vary among donors, depending on the genetic background, age, kidney function, and underlying disease. As a result, it is of critical importance to provide a flexible equation that defines the diagnostic increase in tryptase qualifying as MCAS criterion in all patients, all situations, and all ranges of baseline serum tryptase. In 2012, the consensus group proposed the 120% + 2 ng/ml formula, which covers the great majority of groups, including cases with low, normal, or elevated basal serum tryptase level.
Summary
This formula has been validated in subsequent studies and has proven to be a robust and consistent diagnostic criterion of MCAS. The present article is discussing the impact of this formula and possible limitations as well as alternative markers and mediators that may be indicative of MCAS.
Keywords: MCAS, Anaphylaxis, Allergy, Mast cells, Mastocytosis, Histamine, Tryptase
Introduction
Mast cells (MC) are multi-functional leukocytes that reside in various organs and tissues and play an important role in diverse immunological processes and pathologies [1–3, 4•, 5•]. In common with other leukocytes, including tissue-resident macrophages, basophils, and other immune effector cells, MC derive from hematopoietic stem and progenitor cells. MC synthesize and release various pro-inflammatory mediators, including histamine, leukotrienes, and prostaglandins as well as specific proteases (tryptase, chymase) and distinct proteoglycans, including heparin, which is largely a MC-specific compound [1–3, 4•]. During an anaphylactic or allergic reaction caused by immunoglobulin-E receptor (IgER) cross-linking, MC instantly release their mediators into the extracellular space [1–3, 4•, 6–9]. Apart from allergens, a number of other triggers and receptor-activating ligands can provoke MC activation and can thus participate in hypersensitivity reactions [3, 6, 8, 9].
Tryptases are a group of serine proteases that are almost exclusively synthesized and stored in MC, and less abundantly in basophils [10, 11, 12•, 13]. In MC, tryptases have been described to account for up to 30% of their total protein content [12•]. Whereas the mature tryptase proteins are preferentially stored in the heparin-containing, secretory metachromatic granules of MC, the enzymatically inactive precursor (pro) forms of tryptase, are released continuously by resting cells, independent of the maturation stage of MC, the tissue and organ site, and the underlying pathology [10, 11, 12•, 14, 15]. As a result of steady-state release of the enzyme and its chemical stability under various conditions, the basal serum tryptase level in individual (healthy) donors is remarkably consistent, although slight variations (fluctuations) of the individual baseline have been described, especially in individuals with hereditary alpha tryptasemia (HαT), a condition leading to elevated baseline serum tryptase levels due to multiple copy numbers of TPSAB1 encoding alpha tryptase [16, 17, 18•]. The basal serum tryptase level can also be elevated in various reactive processes and in diverse malignancies but usually remains stable in individual patients when tested over time, unless the malignancy progresses or is successfully treated [19–22, 23•, 24].
However, in the course of a severe systemic MC activation (anaphylaxis) where large quantities of mediator substances, including tryptase, are released from MC, serum tryptase levels usually increase substantially over the individual´s baseline [23•, 24–27, 28•]. Thereafter, serum tryptase levels return to the individual´s baseline, a process that usually takes several hours, depending on reaction-type and response to therapy [23•, 24–27, 28•]. The sustained tryptase peak provides a diagnostic window of testing for several hours (recommended: up to 4 h) after the event occurred.
In the past 30 years, basal serum tryptase has emerged as a preferred biochemical marker of the total body burden of MC, whereas a substantial, event-related increase in tryptase over the individual´s baseline has emerged as the preferred biochemical marker of severe systemic MC activation and anaphylaxis [19–27, 28•, 29•, 30, 31•, 32, 33, 34•].
Other MC-derived compounds and/or their metabolites, such as histamine or prostaglandin D2 (PGD2), may also serve as markers of MC activation and anaphylaxis under certain conditions [3, 6–9, 27]. However, these molecules are less specific for MC and less specific for severe anaphylaxis, but are also found elevated in other (less severe) allergic reactions, and have not been studied extensively in non-allergic diseases. In addition, only a few studies have assessed the event-related, diagnostic, increase over the individual´s baseline of such other MC mediators in the context of MC activation and anaphylaxis [35].
Severe systemic MC activation resembling anaphylaxis is most commonly found in patients with IgE-dependent allergies [1–3, 4•, 6–9]. When the symptoms are severe and recurrent and involve at least two organ systems, a MC activation syndrome (MCAS) may be diagnosed, provided that MCAS criteria are fulfilled [29•, 30, 31•, 32, 33, 34•]. In these patients, MCAS is further divided into distinct MCAS variants, based on the underlying pathology. In particular, MCAS can be split into i) primary (mono/clonal) MCAS defined by the presence of KIT-mutated clonal MC, ii) secondary MCAS characterized by an underlying allergic or other reactive disorder triggering MC activation, and iii) idiopathic MCAS where neither clonal MC nor an underlying allergic or reactive disease triggering MC activation, can be identified [29•, 30, 31•, 32, 33, 34•].
In many patients with allergic disorders or other MC-related pathologies, signs and symptoms of MC activation are observed and are relevant clinically, but may be localized or not severe enough to diagnose MCAS [33, 34•]. Indeed, the criteria to diagnose MCAS are stringent and specific for severe systemic MC activation. According to the proposal of the EU/US consensus group, MCAS can be diagnosed when the following diagnostic criteria are met: i) recurrent episodic occurrence of typical systemic symptoms that are induced by MC mediators and are involving two or more organ-systems, ii) an event-related, transient, increase in the serum tryptase concentration to at least 120% of the individual´s baseline plus 2 ng/ml, and iii) a documented response to drugs directed against MC mediator effects (for example: histamine receptor blocker) or MC activation (MC stabilizers) [29•, 30, 31•, 32, 33, 34•].
In the present article, we discuss the clinical value and limitations of tryptase as a most specific and robust biochemical marker of severe systemic MC activation and MCAS. Moreover, we explain why the increase in tryptase over the individual´s baseline to at least 120% + 2 ng/mL is a specific qualifying criterion of MCAS.
The Basal Serum Tryptase Level in Healthy Controls
The basal tryptase level is remarkably stable over time in individual healthy donors provided that no underlying disease associated with MC activation or MC expansion is present [16, 17, 18•]. Moreover, in contrast to many other MC-derived mediators (histamine, PGD2, heparin, others), tryptase is a biologically stable protein that is not degraded, removed, or de-activated by changes in temperature, by other plasma proteins, or by short-term storage.
However, the basal serum tryptase level varies among healthy individuals, depending on the genetic background, sex, age, kidney function, and presence of an underlying disease associated with MC expansion and/or activation [16, 17, 18•].
The normal serum tryptase level ranges between 0 and 15 ng/mL in healthy adults of Caucasian origin [18•, 19–21]. In those with HαT, tryptase levels are either within normal range or are elevated (> 15 ng/mL), depending on the number of extra-copies of the TPSAB1 gene, and independent of the symptoms recorded or the presence of co-morbidities. When excluding HαT carriers from the pool of healthy controls, the normal basal serum tryptase level amounts to approximately 0–11.4 ng/mL [16, 17, 18•]. However, most HαT carriers are asymptomatic or have non-specific co-morbidities not attributable to MC activation or tryptase, so that these individuals must be included in calculating the normal range of serum tryptase levels [36]. Therefore, these individuals (at least asymptomatic) should be included when defining the normal range of basal serum tryptase [18•]. It is also worth noting that many individuals with HαT have tryptase levels < 10 ng/mL or even < 8 ng/mL [37].
Etiologies Underlying an Elevated Basal Serum Tryptase Level
A number of conditions and pathologies can cause an elevated basal serum tryptase level. The most prevalent underlying condition is HαT, an autosomal dominant genetic trait associated with two or multiple copy numbers of the TPSAB1 gene encoding alpha tryptase [38•, 39, 40•]. HαT is detectable in approximately 4–7.5% of the general population in the Western world [36, 41, 42•]. Many of these individuals have slightly or moderately increased tryptase levels [36, 38•, 39, 40•, 41, 42•]. The excess of tryptase also correlates with the total copy numbers of the TPSAB1 gene. However, most of the HαT carriers have only one extra gene copy and many of these cases present with a normal serum tryptase level [37].
It is important to state that HαT per se cannot be regarded as a biomarker of anaphylaxis or MCAS. Rather, HαT appears to be a modifying factor predisposing for severe symptoms resulting from MC activation in patients who are suffering from an underlying allergic disease and/or a clonal MC disorder [36, 41, 42•]. Overall, the occurrence of severe symptoms of anaphylaxis cannot be predicted in individual patients by their TPSAB1 gene status or their basal serum tryptase level.
Another condition that may produce elevated basal serum tryptase levels is a markedly reduced renal function in patients with chronic kidney disease [43, 44]. Tryptase levels may also increase during chronic infections associated with MC hyperplasia and in those who are treated with recombinant stem cell factor (= MC growth factor) [45].
Finally, basal tryptase levels may increase in patients with myeloid malignancies, including myelodysplastic syndromes (MDS), myeloproliferative neoplasm (MPN), chronic myeloid leukemia (CML), acute myeloid leukemia (AML), MDS/MPN overlap disorders, and mast cell neoplasms, including systemic mastocytosis (SM) (Table 1) [19–22, 40•, 42•]. Patients with eosinophil-related myeloid neoplasms with rearranged PDGFR fusion genes may also have increased basal serum tryptase levels (Table 1).
Table 1.
Conditions associated with an elevated basal serum tryptase level
| Condition | Typical range of serum tryptase in ng/ml* | Increased risk for MCAS |
|---|---|---|
| Hereditary alpha tryptasemia | 15–50** | +/-*** |
| Cutaneous mastocytosis | 5–15 | + |
| Indolent systemic mastocytosis | 15–200 | ++ |
| Smoldering systemic mastocytosis | 200–1000 | + |
| Advanced systemic mastocytosis**** | 100–1000 | + |
| Myelodysplastic syndromes | 10–50 | - |
| Myeloproliferative neoplasms | 10–100 | - |
| Chronic eosinophilic leukemia | 10–50 | - |
| Myeloid neoplasms with PDGFR mutation | 10–50 | - |
| Chronic myeloid leukemia | 10–50 | - |
| Acute myeloid leukemia (AML) | 10–1000 | - |
| Core binding factor (CBF) AML | 10–1000 | - |
| Non-CBF AML | 10–200 | - |
| Chronic helminth infection | 10–20 | -*** |
| Chronic renal failure | 10–30 | - |
Table 1 was reproduced in slightly modified form from Valent et al., Int Arch Allergy Immunol [48] with the Editor´s permission
Score: ++ substantial risk to develop MCAS events one or more times per year despite therapy with anti-mediator-type drugs, + increased risk to develop MCAS events one or more times over several years, +/- MCAS events have been reported in individual patients, but the precise incidence is not clear, - no increased risk to develop MCAS events compared to the general population (± allergic individuals).
*Range of basal serum tryptase concentration where a majority of cases are found; **In patients with hereditary alpha tryptasemia, the serum tryptase level increases 7–15 ng/ml with each additional TPSAB1 gene copy; in those with multiple copies, tryptase levels can increase up to 100 ng/ml; ***In these conditions, the incidence of severe anaphylaxis (MCAS) is not known although some reports suggest an increased risk; ****Advanced systemic mastocytosis includes patients with aggressive systemic mastocytosis and mast cell leukemia. In these patients, the basal tryptase level may increase to > 500 or even > 1000 ng/ml. Abbreviations: MCAS, mast cell activation syndrome
The highest levels of basal serum tryptase are found in patients with smoldering SM (SSM) and advanced SM, including MC leukemia (MCL) and some patients with AML, especially those who have core binding factor AML [19, 21, 46•, 47]. In these patients, basal serum tryptase levels may increase to over 1000 ng/mL (Table 1). In most patients with non-advanced SM, in most with HαT with more than 2 extra TPSAB1 gene copy numbers, and some patients with high risk (accelerated phase) CML, basal serum tryptase levels are between 50 and 200 ng/mL. In all other groups of patients, basal serum tryptase levels are usually below 50 ng/mL. All in all, serum tryptase levels greatly vary among patients and among healthy controls, depending on genetic factors, renal function, and co-morbidities.
Diagnostic Increase in Serum Tryptase in Anaphylaxis and MCAS: Scientific Basis and Discussion of the 120% + 2 ng/mL Formula
During an anaphylactic reaction, MC activation (degranulation) and the massive (additional) release of tryptase usually leads to a substantial and transient increase in serum tryptase levels over the individual´s baseline (Fig. 1) [23•, 24–27, 28•]. In many cases, pre-event serum is not available and was not measured for basal serum tryptase levels. However, basal serum tryptase levels can also be determined in an event-free interval following anaphylaxis. In fact, after a short latency period of several hours following an anaphylactic event, tryptase levels return back to baseline. Therefore, it is important to follow the patients, and to measure the basal serum tryptase level after an event, preferably 24–48 h after resolution of all symptoms of an anaphylactic reaction. However, baseline levels of tryptase may also show some fluctuations over time in symptom-free intervals [16, 17, 18•].
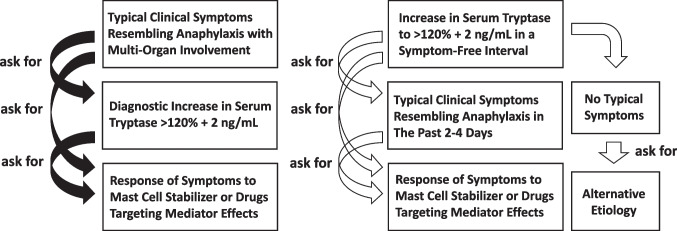
Fig. 1.
Step-wise approach and application of diagnostic criteria in patients with suspected mast cell activation syndrome (MCAS). In patients with clinical signs and symptoms of anaphylaxis (severe hypotension, collapse, acute urticaria, allergic asthma, red skin rash, edema, abdominal pain plus vomiting and diarrhea, others), it is a reasonable diagnostic approach to ask for an event-related increase in tryptase. To define the increase in tryptase, serum samples have to be collected during or shortly after the anaphylactic event and in a symptom-free interval. A diagnostic increase in the event-related tryptase > 120% + 2 ng/mL confirms the involvement of the mast cell (MC) lineage and serves as diagnostic criterion of MCAS. In these cases, the symptoms will respond to drugs stabilizing MC and/or drugs targeting MC mediator effects. In patients without clinical symptoms of MC activation or anaphylaxis, the tryptase level may also be increased to 120% + 2 ng/mL compared to previous examinations (right panel). In these cases, the etiology of the (further) increase in tryptase (for example: progression of mastocytosis) should be explored. If no such etiology is detectable, the increase may be due to a recent anaphylactic event (then the final diagnosis may be MCAS), or may be due to fluctuations in the basal serum tryptase: in these patients, the increase to > 120% + 2 ng/mL (over baseline) does not count as criterion of MCAS
In order to propose a robust minimal diagnostic increase in serum tryptase over the individual´s baseline indicative of severe systemic MC activation in all patients (those with very high levels, high baseline levels, and very low levels), a consensus equation was prepared during the 2010 working conference on MC disorders [31•]. This equation was also adjusted to slight variations in the individual´s baseline serum tryptase level and was created to exclude mild systemic or local forms of MC activation [31•, 48].
It is also worth noting that a persistently elevated serum tryptase level that may be found in patients with HαT or SM, is not indicative of severe systemic MC activation, but is indicative of increased basal secretion of tryptase in HαT, and an increased total body burden of MC in SM.
Overall, the idea was to develop a criterion that confirms with certainty that MC are involved in the reaction, and that the reaction is systemic and severe and caused by MC-derived mediator products. After a workgroup review of tryptase levels at baseline and after anaphylactic reactions, the resulting equation that was selected as a diagnostic criterion of MCAS appeared to be the 120% + 2 ng/mL formula [31•, 48]. This formula defines the minimal increase in serum tryptase that qualifies as robust sign of severe MC activation in individual donors and thus as criterion of MCAS [31•, 48]. The 120% + 2 ng/mL formula was initially tested against data published in the available literature and retrospective case report series. Later, the equation did undergo clinical validation by various independent study groups.
Validation of the 120% + 2 ng/mL Equation in Clinical Practice
In the past 5 years, the value of the 120% + 2 ng/mL formula has been confirmed in several validation studies in patients with hypersensitivity reactions, defined allergies, and MC neoplasms. In patients with SM, the 120% + 2 ng/mL equation is a reliable marker of severe MC activation, that delineates between an anaphylactic (MCAS) event and less severe forms of MC activation (or other pathologies) not fulfilling MCAS criteria, independent of the variant of SM, co-morbidities, or basal tryptase concentrations [48–52]. These data confirmed previous studies that have shown that a substantial increase in tryptase is a reliable parameter to document MC activation during anaphylactic episodes in patients with SM [23•, 24, 26]. It has also been described that the 120% + 2 ng/mL formula is a robust equation to confirm perioperative anaphylaxis and anaphylaxis in children presenting to the emergency department [53•, 54, 55]. By contrast, in patients with local MC activation or less severe mediator-induce symptoms, including cases with pollen or food allergies, the serum tryptase level may remain below the 120% + 2 ng/mL threshold, even if the symptoms are clinically relevant [53•, 54–58]. It is also worth noting that the serum tryptase level may rarely exceed the individual´s baseline by 120% + 2 ng/mL in the absence of any signs or symptoms of MC activation or anaphylaxis [52] which may be due to natural variations (fluctuations) of the enzyme level, unrecognized MC activation (pre-analytical issues), or unrecognized kidney failure (Fig. 1). However, in this regard, it is of utmost importance to be aware of the practical algorithm that guides the clinician in the evaluation of patients with suspected MCAS (Fig. 1). In fact, this algorithm should be started by assessing the patient for signs and symptoms of anaphylaxis, and if such clinical signs (criteria) of MC activation are found, tryptase levels are measured during or shortly after the event as well as in a symptom-free interval (baseline level) (Fig. 1). However, MCAS criteria should not be applied in patients without symptoms, apparently mild symptoms, or symptoms that are not directly attributable to or less specific for MC activation. On the other hand, an increase in (basal) tryptase over the previous baseline in a routine test (symptom-free interval) should prompt the clinician to ask for potential causes, such as progression of an underlying disease (SM), decrease in kidney function, or recent anaphylaxis (Fig. 1). If indeed recent anaphylaxis is reported, MCAS criteria will (again) apply.
It is also important to state that severe systemic MC activation and symptoms of anaphylaxis (with or without fulfilled MCAS criteria) always have therapeutic implications. In fact, these patients usually need immediate therapy with anti-histamines, glucocorticosteroids and/or even epinephrine to bring the acute event under control. Moreover, depending on the underlying condition, these patients are often treated with MC stabilizers, KIT-targeting drugs, anti-IgE-based drugs or specific immunotherapy for long-term prophylaxis. In most cases, treatment of the acute event should (must) start in the absence of knowledge on basal serum tryptase levels and event-related tryptase.
However, it is important to collect these important laboratory test results for several reasons. First, an elevated basal serum tryptase level may be indicative of an underlying HαT, underlying SM, or other myeloid neoplasm. Indeed, in patients with severe IgE-dependent allergy and anaphylaxis, SM may be diagnosed, especially when a hymenoptera venom allergy is detected [58–61]. Second, a diagnostic increase in the event-related tryptase beyond 120% + 2 ng/mL of baseline will confirm the presence of MCAS and thus the involvement of the MC lineage.
Alternative Biochemical Markers of MC Activation and MCAS
In the past 3 decades, a number of efforts have been made to define additional robust markers of severe MC activation and anaphylaxis. Most of these studies focused on other MC-derived chemical substances, such as histamine and its metabolites, prostaglandin D2 (PGD2) and its metabolites, or heparin [27, 62–67] (Table 2). The metabolites of histamine, PGD2 and LTC4 are often measured in urinary samples, since the primary mediators are unstable in serum and are rapidly metabolized. However, unlike heparin, these compounds are not specific for MC but also expressed in several other cell types (Table 2). For example, histamine is also displayed by basophils, and less abundantly by platelets, and may be spuriously ´elevated´ due to blood draw, storage issues, and/or processing conditions.
Table 2.
Biomarkers indicating systemic severe mast cell activation in patients
| Biomarker | Specificity for | Sensitivity in | Commonly used in |
|---|---|---|---|
| mast cells | anaphylaxis | daily practice | |
| Tryptase | + +* | +** | ++ |
| Plasma histamine | +/- | + | + |
| Urinary histamine metabolites*** | +/- | ++ | ++ |
| Prostaglandin D2 metabolites**** | +/- | ++ | + |
| Urinary cysLT levels | -/+ | ++ | +/- |
| Heparin | +++ | -/+***** | - |
Table 2 was reproduced with slight modifications from Valent et al., Int Arch Allergy Immunol [48] with the Editor´s permission
*Basophils express very low amounts of tryptase – but mast cells are a primary and major source of the enzyme; **The relatively low sensitivity of tryptase qualifies as a biomarker of massive mast cell activation and thus as a criterion of MCAS; ***Relevant 24-h urinary histamine metabolites include N-methylhistamine and N-methylimidazoleacetic acid; ****Among prostaglandin D2 metabolites the most commonly measured substance is urinary 11β-prostaglandinF2α; *****An increase in heparin is usually not measurable during an anaphylactic episode, unless the burden of mast cells is very high (like in mast cell leukemia). Abbreviations: cysLT, cysteinyl leukotriene
Another major problem is that no (minimal) event-related increase of these markers over the individual´s baseline documenting MC activation and anaphylaxis (and thus MCAS) has been defined so far. In addition, commercial assays to measure these mediators (and their metabolites) are not widely available in all centers. Furthermore, some of these molecules (urinary metabolites) have to be quantified in 24-h urine samples collected under certain guidelines, including dietary restrictions, to obtain reproducible results [62–66].
Finally, histamine and PGD2 metabolites also increase in various (MC-independent) reactive conditions and also in situations where only mild, but not severe MC activation is found, such as aspirin exacerbated respiratory disease and chronic urticaria. Therefore, these chemical compounds may better qualify as sensitive screen markers (or follow up markers) of MC activation, but may not qualify as specific markers or criteria of severe systemic MC activation and MCAS. The minimal threshold-increase of these compounds that would qualify as a robust sensitive marker of MC activation remains to be defined in clinical studies. Table 2 shows an overview of MC-dependent compounds, their specificity for MC, and their sensitivity in MC activation-related events and anaphylaxis.
Concluding Remarks and Future Perspectives
Depending on the genetic background, underlying disease, and co-morbidities, baseline levels of serum tryptase greatly vary among individual donors. The most prevalent genetic condition associated with elevated tryptase is HαT, and the most prevalent MC neoplasm with elevated tryptase is SM. However, even in the groups of HαT and SM, tryptase level may be very low, normal, elevated or highly elevated. Therefore, a robust biomarker of MC activation needs flexibility to cover all ranges of basal tryptase. The 120% + 2 equation (also known as + 20% + 2 equation) fulfills this important criterion. In addition, a tryptase elevation to 120% + 2 over the individual´s baseline is specific for severe systemic MC activation (anaphylaxis) and thus MCAS, as in most individuals with local or less severe forms of MC activation, the 120% + 2 threshold is not reached. For these patients with less severe forms of anaphylaxis, more sensitive biomarkers of MC activation have to be applied. For example, an event-related increase in histamine, histamine metabolites or PGD2 metabolites may be indicative of MC activation. Whether these biomarkers are robust and specific enough to be employed as criteria of MC activation in patients remains to be determined in clinical trials and controlled validation studies.
Author Contributions
Our manuscript was read and approved by all co-authors and all persons listed as authors made significant contribution to its content.
Funding
Open access funding provided by Medical University of Vienna. This project did not receive funding.
Data Availability
No datasets were generated or analysed during the current study.
Compliance with Ethical Standards
Conflict of Interest
Peter Valent: received 1. a research grant from AOP Orphan and Celgene (BMS), and 2. consultancy honoraria from Novartis, Celgene, AOP Orphan, Blueprint, Pfizer, Stemline, and Cogent. Cem Akin: received 1. a research grant from Blueprint and Cogent, and 2. consultancy honoraria from Blueprint, Cogent, and Novartis. Michel Arock received 1. a research grant from Blueprint, and 2. consultancy honoraria from AB Science, Blueprint, Novartis, and ThermoFisher.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects.
Figure Originality Statement
The Fig. 1 is an original Figure and has never been published before.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Papers of particular interest, published recently, have been highlighted as: • Of Importance •• Of major importance
- 1.Metcalfe DD. Mast cells and mastocytosis. Blood. 2008;112:946–956. doi: 10.1182/blood-2007-11-078097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Galli SJ, Tsai M. IgE and mast cells in allergic disease. Nat Med. 2012;18:693–704. doi: 10.1038/nm.2755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Theoharides TC, Valent P, Akin C. Mast cells, mastocytosis, and related disorders. N Engl J Med. 2015;373:163–172. doi: 10.1056/NEJMra1409760. [DOI] [PubMed] [Google Scholar]
- 4.Valent P, Akin C, Hartmann K, Nilsson G, Reiter A, Hermine O, et al. Mast cells as a unique hematopoietic lineage and cell system: From Paul Ehrlich's visions to precision medicine concepts. Theranostics. 2020;10:10743–10768. doi: 10.7150/thno.46719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Valent P, Akin C, Sperr WR, Horny HP, Arock M, Metcalfe DD, Galli SJ. New insights into the pathogenesis of mastocytosis: emerging concepts in diagnosis and therapy. Annu Rev Pathol. 2023;18:361–386. doi: 10.1146/annurev-pathmechdis-031521-042618. [DOI] [PubMed] [Google Scholar]
- 6.Metcalfe DD, Peavy RD, Gilfillan AM. Mechanisms of mast cell signaling in anaphylaxis. J Allergy Clin Immunol. 2009;124:639–646. doi: 10.1016/j.jaci.2009.08.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kalesnikoff J, Galli SJ. Anaphylaxis: mechanisms of mast cell activation. Chem Immunol Allergy. 2010;95:45–66. doi: 10.1159/000315937. [DOI] [PubMed] [Google Scholar]
- 8.Lieberman P. Mechanisms of anaphylaxis beyond classically mediated antigen- and IgE-induced events. Ann Allergy Asthma Immunol. 2017;118:246–248. doi: 10.1016/j.anai.2017.01.009. [DOI] [PubMed] [Google Scholar]
- 9.Galli SJ, Gaudenzio N, Tsai M. Mast cells in inflammation and disease: recent progress and ongoing concerns. Annu Rev Immunol. 2020;38:49–77. doi: 10.1146/annurev-immunol-071719-094903. [DOI] [PubMed] [Google Scholar]
- 10.Schwartz LB. Tryptase from human mast cells: biochemistry, biology and clinical utility. Monogr Allergy. 1990;27:90–113. [PubMed] [Google Scholar]
- 11.Schwartz LB. Tryptase, a mediator of human mast cells. J Allergy Clin Immunol. 1990;86:594–598. doi: 10.1016/S0091-6749(05)80222-2. [DOI] [PubMed] [Google Scholar]
- 12.Schwartz LB, Lewis RA, Austen KF. Tryptase from human pulmonary mast cells. Purification and characterization J Biol Chem. 1981;256:11939–11943. [PubMed] [Google Scholar]
- 13.Jogie-Brahim S, Min HK, Fukuoka Y, Xia HZ, Schwartz LB. Expression of alpha-tryptase and beta-tryptase by human basophils. J Allergy Clin Immunol. 2004;113:1086–1092. doi: 10.1016/j.jaci.2004.02.032. [DOI] [PubMed] [Google Scholar]
- 14.Schwartz LB, Min HK, Ren S, Xia HZ, Hu J, Zhao W, et al. Tryptase precursors are preferentially and spontaneously released, whereas mature tryptase is retained by HMC-1 cells, Mono-Mac-6 cells, and human skin-derived mast cells. J Immunol. 2003;170:5667–5673. doi: 10.4049/jimmunol.170.11.5667. [DOI] [PubMed] [Google Scholar]
- 15.Fukuoka Y, Schwartz LB. The B12 anti-tryptase monoclonal antibody disrupts the tetrameric structure of heparin-stabilized beta-tryptase to form monomers that are inactive at neutral pH and active at acidic pH. J Immunol. 2006;176:3165–3172. doi: 10.4049/jimmunol.176.5.3165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Skarbø BR, Vinnes EW, Wentzel-Larsen T, Sylte MS, Apelseth TO. Estimating the within-subject (CVI) and between-subject (CVG) biological variation of serum tryptase. Immun Inflamm Dis. 2022;10:e578. doi: 10.1002/iid3.578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chovanec J, Tunc I, Hughes J, Halstead J, Mateja A, Liu Y, et al. Genetically defined individual reference ranges for tryptase limit unnecessary procedures and unmask myeloid neoplasms. Blood Adv. 2023;7:1796–1810. doi: 10.1182/bloodadvances.2022007936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Valent P, Hoermann G, Bonadonna P, Hartmann K, Sperr WR, Broesby-Olsen S, et al. The normal range of baseline tryptase should be 1 to 15 ng/mL and covers healthy individuals with HαT. J Allergy Clin Immunol Pract. 2023;11:3010–3020. doi: 10.1016/j.jaip.2023.08.008. [DOI] [PubMed] [Google Scholar]
- 19.Sperr WR, Jordan JH, Fiegl M, Escribano L, Bellas C, Dirnhofer S, et al. Serum tryptase levels in patients with mastocytosis: correlation with mast cell burden and implication for defining the category of disease. Int Arch Allergy Immunol. 2002;128:136–141. doi: 10.1159/000059404. [DOI] [PubMed] [Google Scholar]
- 20.Sperr WR, Stehberger B, Wimazal F, Baghestanian M, Schwartz LB, Kundi M, et al. Serum tryptase measurements in patients with myelodysplastic syndromes. Leuk Lymphoma. 2002;43:1097–1105. doi: 10.1080/10428190290021470. [DOI] [PubMed] [Google Scholar]
- 21.Sperr WR, El-Samahi A, Kundi M, Girschikofsky M, Winkler S, Lutz D, et al. Elevated tryptase levels selectively cluster in myeloid neoplasms: a novel diagnostic approach and screen marker in clinical hematology. Eur J Clin Invest. 2009;39:914–923. doi: 10.1111/j.1365-2362.2009.02184.x. [DOI] [PubMed] [Google Scholar]
- 22.Valent P, Sperr WR, Sotlar K, Reiter A, Akin C, Gotlib J, et al. The serum tryptase test: an emerging robust biomarker in clinical hematology. Expert Rev Hematol. 2014;7:683–690. doi: 10.1586/17474086.2014.955008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schwartz LB, Metcalfe DD, Miller JS, Earl H, Sullivan T. Tryptase levels as an indicator of mast-cell activation in systemic anaphylaxis and mastocytosis. N Engl J Med. 1987;316:1622–1626. doi: 10.1056/NEJM198706253162603. [DOI] [PubMed] [Google Scholar]
- 24.Schwartz LB, Sakai K, Bradford TR, Ren S, Zweiman B, Worobec AS, Metcalfe DD. The alpha form of human tryptase is the predominant type present in blood at baseline in normal subjects and is elevated in those with systemic mastocytosis. J Clin Invest. 1995;96:2702–2710. doi: 10.1172/JCI118337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schwartz HJ. Elevated serum tryptase in exercise-induced anaphylaxis. J Allergy Clin Immunol. 1995;95:917–919. doi: 10.1016/S0091-6749(95)70139-7. [DOI] [PubMed] [Google Scholar]
- 26.Schwartz LB. Diagnostic value of tryptase in anaphylaxis and mastocytosis. Immunol Allergy Clin North Am. 2006;26:451–463. doi: 10.1016/j.iac.2006.05.010. [DOI] [PubMed] [Google Scholar]
- 27.Lin RY, Schwartz LB, Curry A, Pesola GR, Knight RJ, Lee HS, et al. Histamine and tryptase levels in patients with acute allergic reactions: An emergency department-based study. J Allergy Clin Immunol. 2000;106:65–71. doi: 10.1067/mai.2000.107600. [DOI] [PubMed] [Google Scholar]
- 28.Schwartz LB, Yunginger JW, Miller J, Bokhari R, Dull D. Time course of appearance and disappearance of human mast cell tryptase in the circulation after anaphylaxis. J Clin Invest. 1989;83:1551–1555. doi: 10.1172/JCI114051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Akin C, Valent P, Metcalfe DD. Mast cell activation syndrome: Proposed diagnostic criteria. J Allergy Clin Immunol. 2010;126:1099–1104. doi: 10.1016/j.jaci.2010.08.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hamilton MJ, Hornick JL, Akin C, Castells MC, Greenberger NJ. Mast cell activation syndrome: a newly recognized disorder with systemic clinical manifestations. J Allergy Clin Immunol. 2011;128:147–52.e2. doi: 10.1016/j.jaci.2011.04.037. [DOI] [PubMed] [Google Scholar]
- 31.Valent P, Akin C, Arock M, Brockow K, Butterfield JH, Carter MC, et al. Definitions, criteria and global classification of mast cell disorders with special reference to mast cell activation syndromes: a consensus proposal. Int Arch Allergy Immunol. 2012;157:215–225. doi: 10.1159/000328760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Valent P. Mast cell activation syndromes: definition and classification. Allergy. 2013;68:417–424. doi: 10.1111/all.12126. [DOI] [PubMed] [Google Scholar]
- 33.Valent P, Akin C, Bonadonna P, Hartmann K, Brockow K, Niedoszytko M, et al. Proposed diagnostic algorithm for patients with suspected mast cell activation syndrome. J Allergy Clin Immunol Pract. 2019;7:1125–33.e1. doi: 10.1016/j.jaip.2019.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Valent P, Hartmann K, Bonadonna P, Gülen T, Brockow K, Alvarez-Twose I, et al. Global classification of mast cell activation disorders: an ICD-10-CM-adjusted proposal of the ECNM-AIM consortium. J Allergy Clin Immunol Pract. 2022;10:1941–1950. doi: 10.1016/j.jaip.2022.05.007. [DOI] [PubMed] [Google Scholar]
- 35.Butterfield JH. Increased excretion of mast cell mediator metabolites during mast cell activation syndrome. J Allergy Clin Immunol Pract. 2023;11:2542–2546. doi: 10.1016/j.jaip.2023.02.017. [DOI] [PubMed] [Google Scholar]
- 36.Chollet MB, Akin C. Hereditary alpha tryptasemia is not associated with specific clinical phenotypes. J Allergy Clin Immunol. 2022;149:728–35.e2. doi: 10.1016/j.jaci.2021.06.017. [DOI] [PubMed] [Google Scholar]
- 37.González-de-Olano D, Navarro-Navarro P, Muñoz-González JI, Sánchez-Muñoz L, Henriques A, de-Andrés-Martín A, et al. Clinical impact of the TPSAB1 genotype in mast cell diseases: A REMA study in a cohort of 959 individuals. Allergy. 2024. [DOI] [PubMed]
- 38.Lyons JJ, Yu X, Hughes JD, Le QT, Jamil A, Bai Y, et al. Elevated basal serum tryptase identifies a multisystem disorder associated with increased TPSAB1 copy number. Nat Genet. 2016;48:1564–1569. doi: 10.1038/ng.3696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lyons JJ, Stotz SC, Chovanec J, Liu Y, Lewis KL, Nelson C, et al. A common haplotype containing functional CACNA1H variants is frequently coinherited with increased TPSAB1 copy number. Genet Med. 2018;20:503–512. doi: 10.1038/gim.2017.136. [DOI] [PubMed] [Google Scholar]
- 40.Sabato V, Chovanec J, Faber M, Milner JD, Ebo D, Lyons JJ. First identification of an inherited TPSAB1 quintuplication in a patient with clonal mast cell disease. J Clin Immunol. 2018;38:457–459. doi: 10.1007/s10875-018-0506-y. [DOI] [PubMed] [Google Scholar]
- 41.Lyons JJ, Chovanec J, O'Connell MP, Liu Y, Šelb J, Zanotti R, et al. Heritable risk for severe anaphylaxis associated with increased α-tryptase-encoding germline copy number at TPSAB1. J Allergy Clin Immunol. 2020;S0091–6749(20):31029. doi: 10.1016/j.jaci.2020.06.035. [DOI] [PubMed] [Google Scholar]
- 42.Greiner G, Sprinzl B, Górska A, Ratzinger F, Gurbisz M, Witzeneder N, et al. Hereditary α tryptasemia is a valid genetic biomarker for severe mediator-related symptoms in mastocytosis. Blood. 2021;137:238–247. doi: 10.1182/blood.2020006157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dugas-Breit S, Schöpf P, Dugas M, Schiffl H, Ruëff F, Przybilla B. Baseline serum levels of mast cell tryptase are raised in hemodialysis patients and associated with severity of pruritus. J Dtsch Dermatol Ges. 2005;3:343–347. doi: 10.1111/j.1610-0387.2005.05706.x. [DOI] [PubMed] [Google Scholar]
- 44.Jesky MD, Stringer SJ, Fenton A, Ng KP, Yadav P, Ndumbo M, et al. Serum tryptase concentration and progression to end-stage renal disease. Eur J Clin Invest. 2016;46:460–474. doi: 10.1111/eci.12622. [DOI] [PubMed] [Google Scholar]
- 45.Costa JJ, Demetri GD, Harrist TJ, Dvorak AM, Hayes DF, Merica EA, et al. Recombinant human stem cell factor (kit ligand) promotes human mast cell and melanocyte hyperplasia and functional activation in vivo. J Exp Med. 1996;183:2681–2686. doi: 10.1084/jem.183.6.2681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sperr WR, Jordan JH, Baghestanian M, Kiener HP, Samorapoompichit P, Semper H, et al. Expression of mast cell tryptase by myeloblasts in a group of patients with acute myeloid leukemia. Blood. 2001;98:2200–2209. doi: 10.1182/blood.V98.7.2200. [DOI] [PubMed] [Google Scholar]
- 47.Sperr WR, Mitterbauer M, Mitterbauer G, Kundi M, Jäger U, Lechner K, Valent P. Quantitation of minimal residual disease in acute myeloid leukemia by tryptase monitoring identifies a group of patients with a high risk of relapse. Clin Cancer Res. 2005;11:6536–6543. doi: 10.1158/1078-0432.CCR-05-0732. [DOI] [PubMed] [Google Scholar]
- 48.Valent P, Bonadonna P, Hartmann K, Broesby-Olsen S, Brockow K, Butterfield JH, et al. Why the 20% + 2 tryptase formula is a diagnostic gold standard for severe systemic mast cell activation and mast cell activation syndrome. Int Arch Allergy Immunol. 2019;180:44–51. doi: 10.1159/000501079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Boehm T, Reiter B, Ristl R, Petroczi K, Sperr W, Stimpfl T, Valent P, Jilma B. Massive release of the histamine-degrading enzyme diamine oxidase during severe anaphylaxis in mastocytosis patients. Allergy. 2019;74:583–593. doi: 10.1111/all.13663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Valent P, Akin C, Nedoszytko B, Bonadonna P, Hartmann K, Niedoszytko M, et al. Diagnosis, classification and management of mast cell activation syndromes (MCAS) in the era of personalized medicine. Int J Mol Sci. 2020;21(23):9030. doi: 10.3390/ijms21239030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Matito A, Escribese MM, Longo N, Mayorga C, Luengo-Sánchez O, Pérez-Gordo M, et al. Clinical approach to mast cell activation syndrome: a practical overview. J Investig Allergol Clin Immunol. 2021;31:461–470. doi: 10.18176/jiaci.0675. [DOI] [PubMed] [Google Scholar]
- 52.Mateja A, Wang Q, Chovanec J, Kim J, Wilson KJ, Schwartz LB, et al. Defining baseline variability of serum tryptase levels improves accuracy in identifying anaphylaxis. J Allergy Clin Immunol. 2022;149:1010–17.e10. doi: 10.1016/j.jaci.2021.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Baretto RL, Beck S, Heslegrave J, Melchior C, Mohamed O, Ekbote A. Validation of international consensus equation for acute serum total tryptase in mast cell activation: a perioperative perspective. Allergy. 2017;72:2031–2034. doi: 10.1111/all.13226. [DOI] [PubMed] [Google Scholar]
- 54.Ebo DG, De Puysseleyr LP, Van Gasse AL, Elst J, Poorten MV, Faber MA, et al. Mast cell activation during suspected perioperative hypersensitivity: a need for paired samples analysis. J Allergy Clin Immunol Pract. 2021;9:3051–59.e1. doi: 10.1016/j.jaip.2021.03.050. [DOI] [PubMed] [Google Scholar]
- 55.Wongkaewpothong P, Pacharn P, Sripramong C, Boonchoo S, Piboonpocanun S, Visitsunthorn N, et al. The utility of serum tryptase in the diagnosis of food-induced anaphylaxis. Allergy Asthma Immunol Res. 2014;6:304–309. doi: 10.4168/aair.2014.6.4.304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.De Schryver S, Halbrich M, Clarke A, La Vieille S, Eisman H, Alizadehfar R, et al. Tryptase levels in children presenting with anaphylaxis: temporal trends and associated factors. J Allergy Clin Immunol. 2016;137:1138–1142. doi: 10.1016/j.jaci.2015.09.001. [DOI] [PubMed] [Google Scholar]
- 57.Dua S, Dowey J, Foley L, Islam S, King Y, Ewan P, Clark AT. Diagnostic value of tryptase in food allergic reactions: a prospective study of 160 adult peanut challenges. J Allergy Clin Immunol Pract. 2018;6:1692–98.e1. doi: 10.1016/j.jaip.2018.01.006. [DOI] [PubMed] [Google Scholar]
- 58.González de Olano D, de la Hoz Caballer B, Núñez López R, Sánchez Muñoz L, Cuevas Agustín M, Diéguez MC, et al. Prevalence of allergy and anaphylactic symptoms in 210 adult and pediatric patients with mastocytosis in Spain: a study of the Spanish network on mastocytosis (REMA). Clin Exp Allergy. 2007;37:1547–55. [DOI] [PubMed]
- 59.Bonadonna P, Perbellini O, Passalacqua G, Caruso B, Colarossi S, Dal Fior D, et al. Clonal mast cell disorders in patients with systemic reactions to Hymenoptera stings and increased serum tryptase levels. J Allergy Clin Immunol. 2009;123:680–686. doi: 10.1016/j.jaci.2008.11.018. [DOI] [PubMed] [Google Scholar]
- 60.Akin C. Anaphylaxis and mast cell disease: what is the risk? Curr Allergy Asthma Rep. 2010;10:34–38. doi: 10.1007/s11882-009-0080-8. [DOI] [PubMed] [Google Scholar]
- 61.Brockow K, Jofer C, Behrendt H, Ring J. Anaphylaxis in patients with mastocytosis: a study on history, clinical features and risk factors in 120 patients. Allergy. 2008;63:226–232. doi: 10.1111/j.1398-9995.2007.01569.x. [DOI] [PubMed] [Google Scholar]
- 62.Watkins J, Wild G. Improved diagnosis of anaphylactoid reactions by measurement of serum tryptase and urinary methylhistamine. Ann Fr Anesth Reanim. 1993;12:169–172. doi: 10.1016/S0750-7658(05)81026-3. [DOI] [PubMed] [Google Scholar]
- 63.Keyzer JJ, de Monchy JG, van Doormaal JJ, van Voorst Vader PC. Improved diagnosis of mastocytosis by measurement of urinary histamine metabolites. N Engl J Med. 1983;309:1603–1605. doi: 10.1056/NEJM198312293092603. [DOI] [PubMed] [Google Scholar]
- 64.Awad JA, Morrow JD, Roberts LJ. Detection of the major urinary metabolite of prostaglandin D2 in the circulation: demonstration of elevated levels in patients with disorders of systemic mast cell activation. J Allergy Clin Immunol. 1994;93:817–824. doi: 10.1016/0091-6749(94)90371-9. [DOI] [PubMed] [Google Scholar]
- 65.Ono E, Taniguchi M, Mita H, Akiyama K. Salicylamide-induced anaphylaxis: increased urinary leukotriene E4 and prostaglandin D2 metabolite. Allergy. 2008;63:480–482. doi: 10.1111/j.1398-9995.2007.01616.x. [DOI] [PubMed] [Google Scholar]
- 66.Ravi A, Butterfield J, Weiler CR. Mast cell activation syndrome: improved identification by combined determinations of serum tryptase and 24-hour urine 11β-prostaglandin2α. J Allergy Clin Immunol Pract. 2014;2:775–778. doi: 10.1016/j.jaip.2014.06.011. [DOI] [PubMed] [Google Scholar]
- 67.Vysniauskaite M, Hertfelder HJ, Oldenburg J, Dreßen P, Brettner S, Homann J, Molderings GJ. Determination of plasma heparin level improves identification of systemic mast cell activation disease. PLoS ONE. 2015;10:e0124912. doi: 10.1371/journal.pone.0124912. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.