Abstract
Background
Congenital portosystemic shunt (CPSS) is a vascular malformation in which portal blood drains toward the systemic circulation, leading to pulmonary hypertension.
Case presentation
A 10-year-old patient was brought for evaluation because of dyspnea on exertion. Echocardiography revealed a pulmonary hypertension of 75 mmHg, and multi-slice CT angiography revealed the presence of a CPSS. Closure was finally implemented using a muscular ventricular septal defect device. Follow-up of the patient revealed a gradual decline in pulmonary hypertension.
Conclusions
CPSS is an overlooked cause of reversible pulmonary hypertension (PH). Closure of such lesions and reversal pulmonary hypertension are possible via catheterization. The preferred device type depends largely on the intervening team. Plugs are the first choice for interventional radiologists, while ventricular and atrial septal occluder devices and duct occluders are preferred by pediatric cardiologists.
Keywords: CPSS, Unexplained pulmonary hypertension, mVSD device
Background
Congenital portosystemic shunt (CPSS), also known as Abernethy malformation, is a rare vascular malformation in which portal blood drains into the systemic circulation, eluding the liver [1, 2].
According to the physiopathological theory, when vasoactive substances present in the intestinal circulation (e.g., serotonin, histamine, estrogen, glucagon) bypass the liver without being metabolized and pass through a CPSS, this results in pulmonary arterial hypertension (PAH) caused by the induction of long-lasting pulmonary vasoconstriction [3, 4].
CPSS has a wide spectrum of manifestations that can occur at any point in an individual's life, although asymptomatic cases that are incidentally detected on imaging are also common. In children, long-term portosystemic shunting leads to the most prominent manifestations such as hepatopulmonary syndrome, pulmonary hypertension, and hepatic encephalopathy. Even before birth, a disruption in fetal venous circulation caused by shunting may result in reduced liver perfusion and signs of intrauterine growth restriction, without the presence of hypoxia, maternal infections, and/or chromosomal abnormalities. Neonatal cholestasis and galactosemia are among the complications that may arise and should be distinguished from other congenital defects such as biliary atresia and metabolic disorders that may coexist [5, 6].
Case presentation
Case description
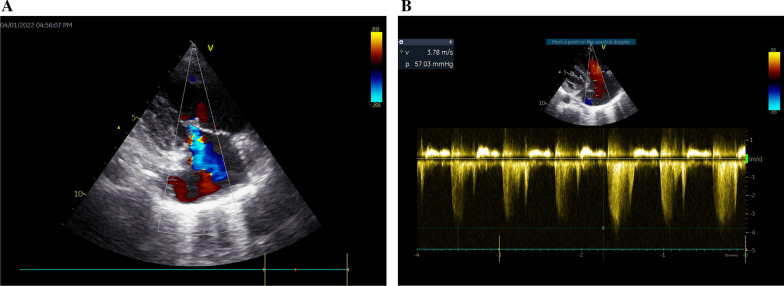
A 10-year-old patient was brought for evaluation because of easy fatigability and dyspnea on exertion, with no clinically appreciable cyanosis. Patient anthropometric measurements showed mainly failure to thrive with a preserved stature centile; weight was 19 kg (< 5th percentile for age and sex), while stature was 125 cm (25th percentile for age and sex). Pulmonary hypertension was evident in the accentuated pulmonary component of the 2nd heart sound. Significant right atrial and ventricular dilatation were elicited by echocardiography, along with an estimated systolic pulmonary arterial pressure of 62–67 mmHg, obtained via tricuspid regurgitant jet (Fig. 1A–B). Left-to-right shunts and underlying cardiac abnormalities were not observed.
Fig. 1.
A Tricuspid regurgitant jet. B Continuous wave Doppler gradient across the across the tricuspid regurgitant jet
Before concluding the diagnosis of primary pulmonary hypertension, multi-slice CT angiography was performed, which revealed the presence of CPSS.
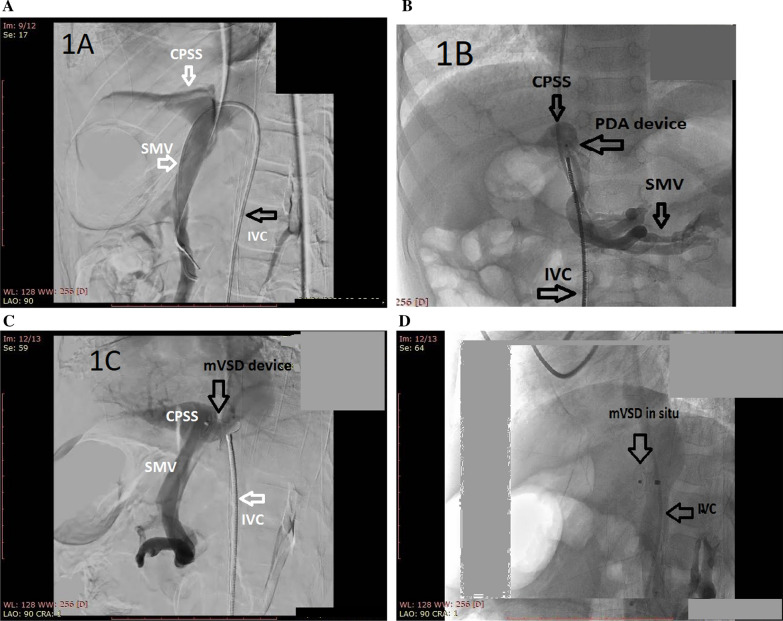
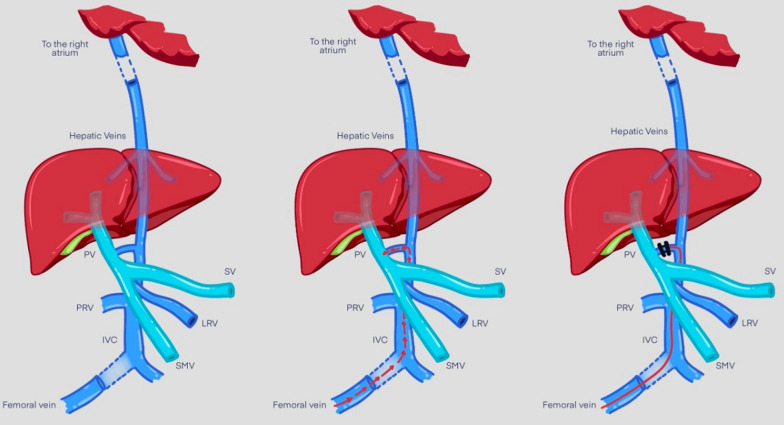
Transcatheter closure of the portosystemic shunt was then attempted. For this purpose, a 6 Fr femoral vein, a 5 Fr Internal jugular vein access, and a 5 Fr femoral arterial access were prepared. Invasive hemodynamics were observed, which revealed elevated pulmonary vascular resistance. Inferior vena cava (IVC) injection revealed a previously identified fistulous malformation between it and the portal vein. It is conical in shape, with the largest diameter at the vena cava side (approximately 8 mm). The first attempt was performed using a Lifetech ductal occluder I DOI (8/6) device (Lifetech Scientific, Shenzhen, China) for shunt closure, but unfortunately, it was unstable in position and slipped into the IVC. A decision was made to close it using a Lifetech muscular mVSD device with a size of 8 mm (Lifetech Scientific, Shenzhen, China). A 4F Judkins Rt catheter under Terumo wire guidance in the IVC was used to cross the fistula to the portal vein. The Terumo wire was withdrawn and replaced by a stiff wire 0.035 × 260 cm to secure the position in the portal vein, which was then withdrawn and replaced by a multipurpose 5 Fr catheter to support the delivery system of the muscular device. The device was loaded onto a 7 Fr Lifetech delivery system, and the entire system was advanced along the guidewire and multipurpose catheter. Once part of the portal vein adjacent to the fistula was reached, the device was released progressively to seal the CPSS. Repeated injections revealed adequate closure of the fistula. (Figs. 2A–D and 3).
Fig. 2.
A IVC angiogram showing CPSS. CPSS Congenital portosystemic shunt, IVC Inferior vena Cava, SMV Superior mesenteric vein. B Prolapsed ADO device. ADO Amplatzer duct occluder, CPSS Congenital portosystemic shunt, IVC Inferior vena Cava, PDA Patent ductus arteriosus, SMV Superior mesenteric vein. C Muscular Device placed across the fistula before deployment CPSS Congenital portosystemic shunt, IVC Inferior vena Cava, SMV Superior mesenteric vein. D Muscular Device placed across the fistula after deployment. IVC Inferior Vena Cava, mVSD Muscular ventricular septal defect
Fig. 3.
Diagram of the approach used for closure of the CPSS. Parts: Part 1 showing the fistula/Part 2: Shows the pathway used for closure, Part 3 shows the device across the fistula. IVC Inferior vena cava, LRV Left renal vein, PV Portal vein, SV Splenic vein, SMV Superior mesenteric vein.
Discussion of the case
Due to the increased levels of humoral substances in the lung tissue, chronic pulmonary vasoconstriction can occur in patients with CPSS. Our patient presented with difficulty breathing due to severe pulmonary hypertension, in addition to hyperammonemia due to concomitant liver dysfunction [4].
Kuo and colleagues performed the first endovascular closure of a portosystemic shunt in 2010. They used a three-stage approach due to associated portal vein hypoplasia. Subsequently, several studies have been published [7].
It is noticeable from the cases summarized in our table that interventional radiologists rely on vascular plugs in the closure of this malformation, whereas pediatric cardiologists perform most of their procedures using duct, atrial septal, and ventricular septal occluders. Vascular plugs are primarily used to treat extracardiac defects. Perhaps this is the reason why they are rarely used by interventional cardiologists and thus rarely available in pediatric cardiac catheter laboratories. This probably explains the bias in the devices used by different teams to close the same defect.
Table 1 shows reports where the endovascular approach was used for CPSS closure [7–13].
Table 1.
Examples of endovascular approach to congenital portosystemic shunts
| Year | Type of publication/number of patients | Author | Service provided by | Presenting manifestation | Age | Size of the shunt | Type of occluding device |
|---|---|---|---|---|---|---|---|
| 2010 | Case report/1 | Kuo et al | Interventional radiology | Progressive cyanosis | 11 years | 14 mm | Graded closure using covered stents to allow growth of portal veins followed by complete closure by vascular plug |
| 2012 | Case report/1 | Passalacqua et al | Interventional Radiology | Progressive cyanosis | 3 years | 10 mm | Vascular plug 10 mm |
| 2013 | Case Series/4 | Bruckheimer et al | Pediatric cardiology | Four patients all presenting with hepatic encephalopathy | 2.5 years, 4 years, 8 and 10 years | Not reported | Graded closure using covered stents followed by duct occluder |
| 2017 | Case report/1 | AlHarbi et al | Pediatric Cardiology and Interventional radiology | Hepatic encephalopathy | 1 month-old | 4 mm | Duct occluder 12 × 6 mm |
| 2017 | Case series/2 | Tomiyama et al | Pediatric Radiology | Two patients presenting with Hepatic encephalopathy | 75 and 83 years old | Not reported | 22- and 14-mm vascular plugs, respectively |
| 2021 | Case report/1 | Facas et al | Interventional Radiology | Asymptomatic: during routine screening of liver functions before isotretinoin therapy for acne | 15 years | 16 mm | 16 mm atrial septal occluder followed by 14 mm vascular plug |
| 2021 | Case report/1 | Shnayder et al | Interventional Radiology | Hepatic encephalopathy | 2 years | 14 mm | 18 mm patent foramen ovale device |
| 2022 | Case series/21 | Koneti et al | Pediatric cardiology |
11 with progressive cyanosis 6 with pulmonary hypertension 2 with hepatic encephalopathy 2 with pulmonary hypertension and progressive cyanosis |
0.45 to 19 years | 7–16 mm |
Ten with vascular plugs Six with muscular ventricular septal defect (VSD)device Four by septal occluder Graded closure using covered stents followed by Muscular VSD One by duct occluder |
A very important consideration to be taken into consideration, during and after closure, is the possible hypoplasia of intrahepatic pulmonary veins. This hypoplasia is either managed with staged repair or with close follow-up every 3–6 months for any signs of portal hypertension and serial ammonia measurements after shunt closure. Nevertheless, prolonged intrahepatic hypoxia can stimulate neoplastic activity and nodule formation; therefore, experts recommend annual abdominal ultrasound to detect any liver neoplasm [6].
Conclusions
When dealing with PAH patients, CPSS should be ruled out, despite its rarity, especially in the pediatric field. The damage caused by PAH can be reversed by transcatheter shunt closure. The endovascular approach has supervened classic surgical ligation, and off-label use of intracardiac devices is increasingly being implemented.
Acknowledgements
Medicine has never been about curing as much as it is about caring, to those who care, and their care is in itself a cure.
Abbreviations
- ADO
Amplatzer duct occluder
- CPSS
Congenital portosystemic shunt
- EPSS
Congenital extrahepatic portosystemic shunt
- IVC
Inferior vena cava
- PAH
Pulmonary arterial hypertension
- PFO
Patent foramen ovale
- VSD
Ventricular septal defect
Author contributions
HA and HK diagnosed the case. HA, SM, MG and AA performed the transcatheter closure of the fistula. HA, HK, SM, MG, HG, and AA participated equally in drafting the manuscript and its revision. They read and approved the final form of the manuscript.
Funding
This research received no specific grant from any funding agency, commercial or not for-profit sectors.
Availability of data and materials
Catheter images have been submitted with manuscript.
Declarations
Ethics approval and consent to participate
The case report was approved by the ethical committee of pediatrics’ department, Cairo University.
Consent for publication
A written informed consent was taken from the father of the patient.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Yi J-E, Jung H-O, Youn H-J, et al. A case of pulmonary arterial hypertension associated with congenital extrahepatic portocaval shunt. J Korean Med Sci. 2014;29:604. doi: 10.3346/jkms.2014.29.4.604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ecochard-Dugelay E, Lambert V, Schleich J-M, et al. Portopulmonary hypertension in liver disease presenting in childhood. J Pediatr Gastroenterol Nutr. 2015;61:346–354. doi: 10.1097/MPG.0000000000000821. [DOI] [PubMed] [Google Scholar]
- 3.Simonneau G, Gatzoulis MA, Adatia I, et al. Updated clinical classification of pulmonary hypertension. J Am Coll Cardiol. 2013;62:D34–D41. doi: 10.1016/j.jacc.2013.10.029. [DOI] [PubMed] [Google Scholar]
- 4.Ivy DD, Abman SH, Barst RJ, et al. Pediatric pulmonary hypertension. J Am Coll Cardiol. 2013;62:D117–D126. doi: 10.1016/j.jacc.2013.10.028. [DOI] [PubMed] [Google Scholar]
- 5.Papamichail M, Pizanias M, Heaton N. Congenital portosystemic venous shunt. Eur J Pediatr. 2018;177:285–294. doi: 10.1007/s00431-017-3058-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Xu S, Zhang P, Hu L, et al. Case report: clinical features of congenital portosystemic shunts in the neonatal period. Front Pediatr. 2021 doi: 10.3389/fped.2021.778791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kuo MD, Miller FJ, Lavine JE, et al. Exploiting phenotypic plasticity for the treatment of hepatopulmonary shunting in abernethy malformation. J Vasc Interv Radiol. 2010;21:917–922. doi: 10.1016/j.jvir.2010.01.038. [DOI] [PubMed] [Google Scholar]
- 8.Alharbi A, Abdulrahman S, AlOtaibi M, et al. Congenital extrahepatic portosystemic shunt embolization with the use of a duct occluder in a neonate with liver dysfunction and hyperammonemia. J Vasc Interv Radiol. 2017;28:1291–1293. doi: 10.1016/j.jvir.2017.05.016. [DOI] [PubMed] [Google Scholar]
- 9.Facas J, Cruz M, Costa JF, et al. Multistage closure of a congenital extrahepatic portosystemic shunt. CVIR Endovasc. 2021;4:3. doi: 10.1186/s42155-021-00267-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tomiyama A, Oguro S, Kato M, et al. Successful embolisation of intrahepatic portosystemic venous shunt using AMPLATZER Vascular Plug II. BJR Case Rep. 2017;3:20160061. doi: 10.1259/bjrcr.20160061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Passalacqua M, Lie KT, Yarmohammadi H. Congenital extrahepatic portosystemic shunt (abernethy malformation) treated endovascularly with vascular plug shunt closure. Pediatr Surg Int. 2012;28:79–83. doi: 10.1007/s00383-011-2944-y. [DOI] [PubMed] [Google Scholar]
- 12.Bruckheimer E, Dagan T, Atar E, et al. Staged transcatheter treatment of portal hypoplasia and congenital portosystemic shunts in children. Cardiovasc Intervent Radiol. 2013;36:1580–1585. doi: 10.1007/s00270-013-0581-7. [DOI] [PubMed] [Google Scholar]
- 13.Koneti NR, Bakhru S, Jayranganath M, Kappanayil M, Bobhate P, Srinivas L, Kulkarni S, Sastry UM, Kumar RK. Transcatheter closure of congenital portosystemic shunts—a multicenter experience. Ann Pediatr Cardiol. 2022;15(2):114–120. doi: 10.4103/apc.apc. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Catheter images have been submitted with manuscript.