Abstract
OBJECTIVE:
To assess trends in recent human papillomavirus (HPV) vaccination initiation and factors associated with vaccination among adolescents.
METHODS:
The 2015 to 2020 National Immunization Survey–Teen data were used to assess vaccination trends. Multivariable logistic regression analysis were conducted to assess factors associated with vaccination.
RESULTS:
Overall, HPV vaccination coverage (≥1 dose) among adolescents significantly increased from 56.1% in 2015 to 75.4% in 2020. There were larger increases in coverage among males (4.7 percentage points annually) than females (2.7 percentage points annually) and coverage differences between males and females decreased in 2015 through 2020. Coverage in 2020 was 75.4% for adolescents aged 13 to 17 years; 73.7% for males and 76.8% for females (P < .05); 80.7% for those with a provider recommendation and 51.7% for those without (P < .05); and 80.3% for those with a well child visit at age 11 to 12 years, and 64.8% for those without (P < .05). Multivariable logistic regression results showed that main characteristics independently associated with a higher likelihood of vaccination included: a provider recommendation, age 16 to 17 years, non-Hispanic Black, Hispanic, or American Indian or Alaskan Native, Medicaid insurance, ≥2 provider contacts in the past 12 months, a well–child visit at age 11 to 12 years and having 1 or 2 vaccine providers (P < .05).
CONCLUSIONS:
Overall, HPV vaccination coverage among adolescents increased during 2015 to 2020. Coverage increased faster among males than females and differences by sex narrowed during this time. Receiving a provider recommendation vaccination was important to increase vaccination coverage.
Human papillomavirus (HPV) is the most common sexually transmitted infection in men and women in the United States.1 Vaccination is an important tool to prevent and control HPV infection and associated outcomes, including genital warts, precancerous lesions, and cancers, such as cervical, vaginal, vulvar, anal, penile, and oropharyngeal cancers.2–6 Since 2006, routine HPV vaccination of females aged 11 or 12 years (vaccine can be administered as young as age 9 years), as well as those aged 13 through 26 years not previously vaccinated, has been recommended by the Advisory Committee on Immunization Practices (ACIP).2 In 2011, ACIP recommended routine vaccination of males aged 11 to 12 years and those aged 13 to 21 years not previously vaccinated; recommendations stated that males aged 22 to 26 years may be vaccinated.3 Initially, ACIP recommended a 3-dose schedule for HPV vaccine. However, in 2016, this recommendation was revised to allow a 2-dose schedule (with an interval of at least 5 months between doses) if the vaccination series is initiated before the 15th birthday.5 In 2019, recommendations for catch-up HPV vaccination were harmonized across genders through age 26 years.6
HPV vaccination coverage among adolescents has been reported previously.7,8 The purpose of this study is to assess trends in recent HPV vaccination coverage and factors associated with vaccination among adolescents aged 13 to 17 years using data from the 2015 to 2020 National Immunization Survey–Teen (NIS–Teen). We could not provide HPV vaccination coverage on a wider age range since NIS-Teen is designed to assess vaccination coverage among adolescents aged 13 to 17 years.
METHODS
NIS–Teen is a national, random–digit–dial (RDD) telephone survey conducted by the Centers for Disease Control and Prevention (CDC). Survey data are collected in 2 phases. In the first phase, an RDD telephone interview is conducted to identify households with age–eligible adolescents (aged 13 to 17 years at the time of interview) and to collect demographic information from the parent or guardian on adolescent, maternal, and household characteristics. The interview also includes questions about the adolescent’s reported vaccination history. After completing the interview, parents or guardians are asked for consent to contact the adolescent’s vaccination provider(s). If consent is obtained, the adolescent’s vaccination providers are mailed a questionnaire to collect provider–reported vaccination histories for each recommended adolescent vaccine and selected childhood vaccines. The provider reported histories are used for determining vaccination coverage estimates.7–10 Beginning in 2018, the NIS–Teen used a single-frame sample of cell phone numbers. The landline telephone sample frame that was used from 2006 through 2017 was discontinued because of the declining number of landline-only households in the United States.11
NIS-Teen data from 2015 through 2020 were used to assess HPV vaccination coverage by year based on provider report. SUDAAN 11.0.1 was used to calculate point estimates and 95% confidence intervals (CIs). All analyses account for the complex sampling design of the NIS–Teen.9,10 T–tests were used to conduct trend analysis and comparison tests with the significance level set at P < .05. Multivariable logistic regression and predictive marginal modeling were conducted to derive the adjusted vaccination coverage estimates and adjusted prevalence ratios using the 2020 NIS–Teen. The NIS–Teen was approved by the CDC, National Center for Health Statistics Research Ethics Review Board and the National Opinion Research Center at the University of Chicago Institutional Review Board.
RESULTS
The Council of American Survey Research Organizations (CASRO) response rate for the 2020 NIS–Teen was 20.7%, and 45.2% of adolescents with completed interviews had adequate provider data. Sample characteristics of the study population by demographic and access-to-care characteristics are shown in Table 1. During 2015 through 2020, the prevalence of receiving a provider recommendation for HPV vaccine among adolescents aged 13 to 17 years increased from 68.4% in 2015 to 81.5% in 2020. During 2015 through 2020, the prevalence of having a well-child visit at age 11 to 12 years ranged from 46.3% to 50.4%, and the proportion of adolescents living in non-metropolitan statistical area (MSA) areas ranged from 10.7% to 13.0% among adolescents aged 13 to 17 years (Table 1).
TABLE 1.
Sample Characteristics of Adolescents Aged 13 to 17 Years in the United States, by Demographic and Access-to-Care Variables, NIS-Teen, 2015 to 2020
| Survey Year | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | |||||||
| Subgroup and Age Group, y | Sample | Weighted % | Sample | Weighted % | Sample | Weighted % | Sample | Weighted % | Sample | Weighted % | Sample | Weighted % |
|
| ||||||||||||
| Total | 21 875 | 100 | 20 475 | 100 | 20 949 | 100 | 18 700 | 100 | 18 788 | 100 | 17 970 | 100 |
| Parental report of provider recommendation for HPV vaccine | ||||||||||||
| Yes | 13 964 | 68.4 (67.1–69.6) | 13 733 | 71.4 (70.2–72.7) | 14906 | 75.3 (74.1–76.5) | 13 559 | 77.5 (76.4–78.7) | 14054 | 79.6 (78.2–80.9) | 13 786 | 81.5 (80.4–82.7) |
| No | 5935 | 31.6 (30.4–32.9) | 4908 | 28.6 (27.3–29.8) | 4294 | 24.7 (23.5–25.9) | 3693 | 22.5 (21.3–23.6) | 3280 | 20.4 (19.1–21.8) | 2747 | 18.5 (17.3–19.6) |
| Age, y | ||||||||||||
| 13–15 | 13 488 | 60.7 (59.4–61.9) | 12 578 | 60.5 (59.2–61.7) | 12 924 | 60.7 (59.5–62.0) | 11 468 | 60.5 (59.2–61.8) | 11 687 | 61.2 (59.6–62.6) | 11 071 | 60.6 (59.2–61.9) |
| 16–17 | 8387 | 39.3 (38.1–40.6) | 7897 | 39.5 (38.3–40.8) | 8025 | 39.3 (38.0–40.5) | 7232 | 39.5 (38.2–40.8) | 7101 | 38.8 (37.4–40.4) | 6899 | 39.4 (38.1–40.8) |
| Sex | ||||||||||||
| Male | 11 367 | 51.1 (49.8–52.4) | 10814 | 51.1 (49.8–52.3) | 11 104 | 51.0 (49.7–52.3) | 9772 | 51.0 (49.7–52.4) | 9872 | 51.0 (49.5–52.6) | 9445 | 51.5 (50.1–52.9) |
| Female | 10 508 | 48.9 (47.6–50.2) | 9661 | 48.9 (47.7–50.2) | 9845 | 49.0 (47.7–50.3) | 8928 | 49.0 (47.6–50.3) | 8916 | 49.0 (47.4–50.5) | 8525 | 48.5 (47.1–49.9) |
| Race or ethnicity | ||||||||||||
| Non-Hispanic White | 12 835 | 53.5 (52.3–54.8) | 12 883 | 52.7 (51.5–54.0) | 13010 | 52.3 (51.1–53.6) | 11 128 | 51.9 (50.6–53.2) | 11 883 | 52.0 (50.5–53.5) | 11 348 | 50.7 (49.4–52.0) |
| Non-Hispanic Black | 2228 | 14.0 (13.2–14.9) | 1990 | 13.7 (12.9–14.6) | 1743 | 13.8 (12.9–14.8) | 1488 | 13.7 (12.7–14.7) | 1367 | 13.7 (12.6–14.8) | 1614 | 14.2 (13.2–15.2) |
| Hispanic | 4610 | 22.8 (21.6–24.0) | 3223 | 23.2 (22.0–24.5) | 3882 | 23.7 (22.4–24.9) | 4021 | 24.2 (23.0–25.4) | 3466 | 24.7 (23.2–26.3) | 3007 | 23.6 (22.3–25.0) |
| American Indian or Alaskan Native | 290 | 0.8 (0.7–1.0) | 300 | 1.0 (0.8–1.2) | 257 | 0.8 (0.6–1.1) | 247 | 0.7 (0.6–0.9) | 237 | 0.8 (0.6–1.0) | 195 | 0.7 (0.6–1.0) |
| Asian | 751 | 4.0 (3.5–4.6) | 862 | 4.2 (37–4.8) | 818 | 4.4 (3.8–5.0) | 601 | 4.0 (3.4–47) | 607 | 3.6 (3.1–4.2) | 689 | 4.8 (41–5.5) |
| Other | 1161 | 4.8 (4.3–5.3) | 1217 | 5.1 (4.6–57) | 1239 | 5.0 (4.6–5.5) | 1215 | 5.5 (5.0–6.2) | 1228 | 5.3 (47–5.9) | 1117 | 6.0 (5.4–6.7) |
| Mother’s educational level | ||||||||||||
| <High school | 2955 | 13.5 (12.5–14.5) | 2205 | 13.4 (12.4–14.4) | 2565 | 13.2 (12.3–14.1) | 2368 | 12.3 (11.4–13.1) | 1780 | 11.5 (10.6–12.5) | 1516 | 12.3 (11.2–13.5) |
| High school | 3626 | 22.9 (21.7–24.1) | 3253 | 22.4 (21.3–23.6) | 3141 | 22.1 (21.0–23.3) | 2929 | 21.9 (20.7–23.2) | 2679 | 21.8 (20.4–23.3) | 2700 | 20.9 (19.8–22.1) |
| Some college or college graduate | 5776 | 25.8 (24.7–26.9) | 5369 | 25.0 (23.9–26.1) | 5166 | 23.8 (22.7–24.9) | 4721 | 24.2 (23.1–25.3) | 4918 | 23.6 (22.3–24.9) | 4570 | 24.3 (23.1–25.5) |
| >College graduate | 9518 | 37.9 (36.7–39.1) | 9648 | 39.2 (38.0–40.4) | 10 077 | 40.9 (39.7–42.1) | 8682 | 41.7 (40.4–43.0) | 9411 | 43.1 (41.6–44.6) | 9184 | 42.5 (41.2–43.8) |
| Mother’s married status | ||||||||||||
| Married or living with partner | 16 403 | 69.3 (68.1–70.5) | 15 544 | 69.3 (68.1–70.5) | 16 000 | 70.4 (69.2–71.7) | 14095 | 70.0 (68.7–71.2) | 14 327 | 70.2 (68.6–71.7) | 13 528 | 70.3 (69.0–71.5) |
| Widowed, divorced, or separated | 3778 | 22.4 (21.3–23.5) | 3448 | 22.0 (20.9–23.1) | 3503 | 21.2 (20.1–22.3) | 3257 | 21.1 (20.1–22.3) | 3155 | 20.9 (19.6–22.4) | 3058 | 20.6 (19.5–21.7) |
| Never married | 1475 | 8.3 (7.7–9.0) | 1301 | 8.7 (8.0–9.5) | 1240 | 8.4 (77–9.2) | 1182 | 8.9 (8.1–9.8) | 1139 | 8.9 (8.0–9.9) | 1233 | 9.2 (8.4–10.0) |
| Mother’s age, y | ||||||||||||
| ≤34 | 1866 | 9.0 (8.3–9.8) | 1686 | 8.9 (8.2–97) | 1599 | 8.4 (77–9.2) | 1407 | 7.9 (7.2–87) | 1286 | 7.7 (6.9–8 6) | 1187 | 7.3 (6.6–8.1) |
| 35–44 | 9241 | 44.2 (42.9–45.5) | 8310 | 44.1 (42.8–45.4) | 8447 | 42.8 (41.5–44.1) | 7955 | 43.4 (42.1–44.7) | 8097 | 44.7 (43.2–46.2) | 7623 | 43.6 (42.2–44.9) |
| ≥45 | 10 768 | 46.8 (45.5–48.0) | 10 479 | 47.0 (45.7–48.3) | 10 903 | 48.8 (47.6–50.1) | 9338 | 48.7 (47.3–50.0) | 9405 | 47.6 (46.1–49.1) | 9160 | 49.2 (47.8–50.5) |
| Place of birth | ||||||||||||
| Born in United States | 20 825 | 95.1 (94.5–95.6) | 19 403 | 93.9 (93.2–94.6) | 19 723 | 93.1 (92.3–93.9) | 17 605 | 93.8 (93.1–94.5) | 17 932 | 95.0 (94.3–95.7) | 17111 | 94.9 (94.1–95.6) |
| Born outside United States | 891 | 4.9 (4.4–5.5) | 948 | 6.1 (5.4–68) | 1097 | 6.9 (6.1–77) | 975 | 6.2 (5.5–6.9) | 740 | 5.0 (4.3–57) | 732 | 5.1 (44–5.9) |
| Income to poverty ratio | ||||||||||||
| <133% | 6307 | 33.1 (31.8–34.4) | 5103 | 31.7 (30.5–33.0) | 5277 | 31.3 (30.1–32.5) | 4860 | 29.1 (27.9–30.4) | 4073 | 27.3 (25.9–28.8) | 3741 | 27.2 (25.9–28.5) |
| 133% to <322% | 5987 | 28.3 (27.2–29.5) | 5787 | 28.8 (27.6–30.0) | 5469 | 27.1 (25.9–28.2) | 4976 | 27.2 (26.0–28.5) | 5100 | 28.1 (26.7–29.6) | 4846 | 28.9 (27.6–30.2) |
| 322% to <503% | 4851 | 19.7 (18.8–20.7) | 4121 | 17.6 (16.8–18.6) | 4160 | 17.2 (16.3–18.1) | 3614 | 18.3 (17.4–19.3) | 3899 | 17.4 (16.4–18.4) | 3836 | 18.4 (17.4–19.3) |
| ≥503% | 4730 | 18.9 (18.0–19.8) | 5464 | 21.8 (20.8–22.8) | 6043 | 24.4 (23.4–25.5) | 5250 | 25.3 (24.2–26.5) | 5716 | 27.2 (25.9–28.5) | 5547 | 25.6 (24.5–26.7) |
| Medical insurancea | ||||||||||||
| Private only | 12157 | 51.4 (50.1–52.7) | 11 889 | 51.2 (49.9–52.5) | 11 919 | 50.5 (49.2–51.8) | 10315 | 52.1 (50.8–53.5) | 11 183 | 54.3 (52.8–55.9) | 10 764 | 53.5 (52.1–54.9) |
| Any Medicaid | 7010 | 36.5 (35.2–37.8) | 6203 | 37.2 (35.9–38.5) | 6504 | 37.5 (36.3–38.8) | 5999 | 35.8 (34.5–37.2) | 5366 | 34.5 (33.0–36.0) | 5259 | 35.4 (34.0–36.8) |
| Otherb | 1800 | 7.7 (7.0–8.4) | 1679 | 7.6 (7.0–8.2) | 1708 | 7.6 (7.0–8.2) | 1605 | 7.5 (6.9–8.1) | 1545 | 7.1 16.4–7.8) | 1343 | 6.8 16.2–7.5) |
| Uninsured | 908 | 4.4 (3.9–5.0) | 702 | 4.1 13.5–4.7) | 818 | 4.4 13.9–4.9) | 781 | 4.5 (4.0–5.1) | 694 | 4.1 13.6–4.7) | 604 | 4.3 (3.7–5.0) |
| Provider contacts within past year | ||||||||||||
| None | 2932 | 14.9 (14.0–15.9) | 2608 | 14.9 (13.9–16.0) | 2816 | 15.8 (14.8–16.8) | 2402 | 14.6 (13.6–15.6) | 2252 | 14.1 (13.0–15.3) | 2433 | 16.7 (15.6–17.8) |
| 1 | 6119 | 30.0 (28.8–31.3) | 5884 | 30.4 (29.2–31.6) | 5798 | 29.7 (28.5–30.9) | 5303 | 29.8 (28.5–31.1) | 5281 | 29.9 (28.6–31.4) | 5499 | 32.4 (31.1–33.7) |
| 2–3 | 7929 | 35.2 (34.0–36.4) | 7385 | 35.3 (34.1–36.5) | 7600 | 35.1 (33.9–36.3) | 6724 | 35.8 (34.5–37.1) | 6978 | 36.3 (34.9–37.8) | 6443 | 34.1 (32.8–35.3) |
| ≥4 | 4681 | 19.9 (18.9–20.9) | 4392 | 19.4 (18.5–20.4) | 4524 | 19.5 (18.5–20.4) | 4085 | 19.9 (18.9–20.9) | 4123 | 19.6 (18.5–20.8) | 3447 | 16.9 (15.9–17.9) |
| Well child visit at age 11–12 yc | ||||||||||||
| Yes | 10 472 | 47.1 (45.8–48.4) | 9898 | 46.3 (45.1–47.6) | 10 325 | 47.6 (46.3–48.9) | 9260 | 48.5 (47.2–49.9) | 9948 | 50.4 (48.9–51.9) | 9016 | 49.9 (48.5–51.3) |
| No | 5341 | 22.8 (21.8–23.8) | 4785 | 22.7 (21.7–23.8) | 4733 | 21.6 (20.6–22.7) | 4139 | 20.5 (19.5–21.6) | 4053 | 21.1 (19.9–22.4) | 3171 | 17.6 (16.6–18.7) |
| Don’t know | 6062 | 30.2 (29.0–31.4) | 5792 | 30.9 (29.7–32.2) | 5891 | 30.8 (29.6–32.0) | 5301 | 30.9 (29.7–32.3) | 4787 | 28.5 (27.0–29.9) | 5783 | 32.5 (31.2–33.8) |
| Number of providers | ||||||||||||
| 1 | 12138 | 58.2 (56.9–59.5) | 11 760 | 59.2 (57.9–60.5) | 12216 | 60.5 (59.2–61.7) | 10 721 | 60.5 (59.2–61.8) | 10 497 | 58.7 (57.2–60.2) | 10 867 | 62.1 (60.7–63.4) |
| 2 | 6150 | 26.3 (25.2–27.5) | 5578 | 26.2 (25.1–27.3) | 5617 | 26.6 (25.4–27.8) | 5098 | 26.4 (25.3–27.5) | 5147 | 26.9 (25.5–28.3) | 4777 | 26.0 (24.8–27.2) |
| ≥3 | 3539 | 15.5 (14.6–16.4) | 3061 | 14.6 (13.7–15.6) | 3050 | 12.9 (12.1–13.8) | 2817 | 13.1 (12.3–14.0) | 3078 | 14.4 (13.5–15.4) | 2277 | 12.0 (11.1–12.9) |
| MSA | ||||||||||||
| MSA principal city | 9105 | 39.8 (38.6–41.0) | 7979 | 40.1 (38.9–41.4) | 8544 | 41.2 (40.0–42.5) | 7564 | 42.4 (41.1–43.7) | 7354 | 40.0 (38.5–41.5) | 6927 | 40.6 (39.2–41.9) |
| MSA non-principal city | 8459 | 47.4 (46.1–48.6) | 8248 | 46.9 (45.6–48.1) | 8282 | 46.9 (45.7–48.2) | 7543 | 46.9 (45.6–48.2) | 7745 | 49.3 (47.8–50.8) | 7720 | 48.7 (47.4–50.1) |
| Non-MSA | 4311 | 12.8 (12.2–13.5) | 4248 | 13.0 (12.4–13.6) | 4123 | 11.8 (11.2–12.4) | 3593 | 10.7 (10.2–11.3) | 3689 | 10.7 (10.0–11.3) | 3323 | 10.7 (10.1–11.3) |
| Region | ||||||||||||
| Northeast | 4049 | 16.6 (16.2–17.1) | 4049 | 16.5 (16.0–16.9) | 3975 | 16.4 (15.9–16.8) | 3437 | 16.2 (15.6–16.8) | 3597 | 16.0 (15.4–16.6) | 4020 | 17.5 (17.0–18.1) |
| Midwest | 4666 | 21.6 (21.0–22.1) | 4313 | 21.4 (20.9–22.0) | 4485 | 21.3 (20.9–21.8) | 4094 | 21.2 (20.7–21.8) | 3985 | 21.2 (20.5–21.8) | 4508 | 23.4 (22.8–24.1) |
| South | 8355 | 38.0 (37.3–38.8) | 7620 | 38.3 (37.5–39.0) | 8032 | 38.4 (37.6–39.2) | 7184 | 38.6 (37.8–39.4) | 7057 | 38.8 (37.8–39.8) | 7189 | 43.2 (42.3–44.2) |
| West | 4805 | 23.8 (22.9–24.7) | 4493 | 23.8 (23.0–24.7) | 4457 | 23.9 (23.0–24.8) | 3985 | 24.0 (23.0–25.0) | 4149 | 24.1 (22.8–25.4) | 2253 | 15.8 (14.9–16.8) |
| Facility type | ||||||||||||
| All private facilities | 10 891 | 54.7 (53.5–56.0) | 10146 | 53.0 (51.7–54.3) | 10 337 | 52.5 (51.3–53.8) | 9038 | 52.8 (51.5–54.2) | 9257 | 53.4 (51.8–54.9) | 8840 | 54.3 (53.0–55.7) |
| All public facilities | 3157 | 13.6 (12.8–14.5) | 2925 | 14.5 (13.6–15.5) | 3123 | 16.3 (15.3–17.3) | 2724 | 15.2 (14.1–16.2) | 2616 | 15.2 (14.0–16.5) | 2392 | 13.7 (12.7–14.7) |
| All hospital facilities | 2311 | 9.1 18.5–9.8) | 2426 | 10.1 (9.4–10.9) | 2485 | 9.9 (9.2–10.6) | 2267 | 10.2 (9.5–10.9) | 2469 | 10.9 (10.0–11.8) | 2742 | 12.4 (11.6–13.2) |
| All sexually transmitted diseases, school, and teen clinics or other facilities | 331 | 1.6 (1.3–2.0) | 328 | 2.0 (1.6–2.5) | 377 | 2.3 (1.8–2.8) | 302 | 1.8 (1.5–2.2) | 278 | 1.8 (1.3–2.4) | 260 | 1.5 (1.2–1.9) |
| Mixedd | 4753 | 19.7 (18.7–20.7) | 4209 | 19.0 (18.1–20.0) | 4173 | 17.8 (16.9–18.8) | 3974 | 18.8 (17.8–19.8) | 3762 | 17.6 (16.5–18.8) | 3410 | 17.1 (16.1–18.1) |
| Othere | 301 | 1.2 (1.0–1.5) | 289 | 1.3 (1.1–1.6) | 310 | 1.2 (1.0–1.4) | 262 | 1.2 (1.0–1.5) | 274 | 1.1 (0.9–1.4) | 213 | 1.0 (0.8–1.3) |
Insurance categories are mutually exclusive.
Indian Health Service, Children’s Health Insurance Program, military, and some private.
Status of health-care visit at age 11 to 12 y based on provider reported data.
Mixed indicates that the facility is identified to be in more than 1 of the facility categories such as private, public, hospital, sexually transmitted diseases, school, or teen clinics.
Includes military, WIC clinics, and pharmacies.
Overall, HPV vaccination coverage (≥1 dose) among adolescents aged 13 to 17 years significantly increased from 56.1% in 2015 to 75.4% in 2020, with a total increase of 19.1 percentage points and an average increase of 3.8 percentage points annually (Table 2). HPV vaccination series completion coverage among adolescents aged 13 to 17 years significantly increased from 40.3% in 2015 to 59.3% in 2020, with a total increase of 18.4 percentage points and an average increase of 3.6 percentage points annually. From 2015 through 2020, HPV vaccination coverage among adolescents significantly increased across almost all levels of demographic and access-to-care characteristics (Table 2).
TABLE 2.
HPV Vaccination Coverage (≥1 Dose) of Adolescents Aged 13–17 Years in the United States, by Demographic, and Access-to-Care Variables, NIS–Teen, 2015 to 2020
| Survey Year | ||||||||
|---|---|---|---|---|---|---|---|---|
| 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | Average Annual Change % | ||
| Subgroup and Age Group, y | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | Total Change % | |
|
| ||||||||
| Total | 56.1 (54.9 to 57.4) | 60.4 (59.2 to 61.6)a | 65.5 (64.3 to 66.7)a | 68.1 (66.8 to 69.3)a | 71.5 (70.1 to 72.8)a | 75.4 (74.2 to 76.6)a | 19.1 (17.4 to 20.8)b | 3.8 (3.4 to 4.1)b |
| Parental report of provider recommendation for HPV vaccine | ||||||||
| Yes | 69.3 (67.8 to 70.8)d | 71.1 (69.7 to 72.4)d | 73.2 (71.8 to 74.5)a,d | 74.7 (73.3 to 76.0)d | 77.5 (76.0 to 79.0)a,d | 80.7 (79.6 to 81.9)a,d | 11.4 (9.5 to 13.3)b | 2.2 (1.9 to 2.6)b |
| Noc | 30.7 (28.5 to 33.0) | 37.1 (34.5 to 39.8)a | 44.1 (41.1 to 47.1 )a | 46.7 (43.8 to 49.6) | 49.1 (45.6 to 52.7) | 51.7 (48.2 to 55.3) | 21.0 (16.8 to 25.2)b | 4.3 (3.5 to 5.1)b |
| Age, y | ||||||||
| 13 to 15c | 54.4 (52.7 to 56.1) | 58.3 (56.7 to 59.9)a | 64.1 (62.6 to 65.7)a | 66.4 (64.8 to 68.0)a | 71.0 (69.4 to 72.7)a | 73.4 (71.8 to 74.9)a | 19.0 (16.7 to 21,2)b | 3.9 (3.5 to 4.3)b |
| 16–17 | 58.8 (56.8 to 60.7)d | 63.6 (61.7 to 65.4)a,d | 67.7 (65.8 to 69.5)a,d | 70.7 (68.7 to 72.5)a,d | 72.1 (69.8 to 74.3) | 78.1 (76.4 to 79.8)a,d | 19.3 (16.7 to 21,9)b | 3.6 (3.1 to 4.1)b |
| Sex | ||||||||
| Malec | 49.8 (48.0 to 51.6) | 56.0 (54.3 to 57.7)a | 62.6 (60.9 to 64.2)a | 66.3 (64.6 to 68.0)a | 69.8 (67.9 to 71.7)a | 73.7 (72.1 to 75.4)a | 24.0 (21.5 to 26.4)b | 4.7 (4.3 to 5.2)b |
| Female | 62.8 (61.0 to 64.5)d | 65.1 (63.3 to 66.8)d | 68.6 (66.9 to 70.2)a,d | 69.9 (68.1 to 71.6)d | 73.2 (71.3 to 75.0)a,d | 76.8 (75.2 to 78.4)a,d | 14.0 (11.6 to 16.4)b | 2.7 (2.3 to 3.2)b |
| Race or ethnicity | ||||||||
| Non-Hispanic Whitec | 51.4 (49.9 to 52.9) | 54.7 (53.2 to 56.1 )a | 60.0 (58.6 to 61,5)a | 63.5 (62.0 to 65.1 )a | 68.3 (66.8 to 69.9)a | 71.4 (69.9 to 72.8 a | 19.9 (17.9 to 22.0)b | 4.1 (3.8 to 4.5)b |
| Non-Hispanic Black | 60.1 (56.7 to 63.4)d | 65.9 (62.5 to 69.1 )a,d | 70.0 (66.4 to 73.3)d | 72.8 (69.3 to 76.1 )d | 72.0 (67.8 to 75.9) | 78.3 (75.0 to 81.5)a,d | 18.2 (13.5 to 22.9)b | 3.2 (2.3 to 4.1)b |
| Hispanic | 63.6 (60.1 to 67.0)d | 69.8 (66.6 to 72.7)a,d | 74.5 (71.7 to 77.1 )a,d | 75.5 (72.7 to 78.2)d | 76.8 (73.3 to 79.9)d | 80.7 (77.9 to 83.5)d | 17.1 (12.6 to 21.5)b | 3.1 (2.2 to 3.9)b |
| American Indian or Alaskan Native | 64.2 (55.0 to 72.5)d | 62.3 (52.5 to 71.3) | 60.2 (45.5 to 73.2) | 70.1 (59.6 to 78.9) | 71.1 (58.2 to 81.3) | 85.6 (79.3 to 91.9)a,d | 21.4 (10.5 to 32.2)b | 3.9 (1.2 to 6.7)b |
| Asian | 56.6 (49.7 to 63.2) | 62.5 (55.7 to 68.9)d | 70.4 (64.5 to 75.7)d | 65.3 (56.5 to 73.2) | 74.8 (68.1 to 80.5) | 75.8 (70.0 to 81.6) | 19.2 (10.3 to 28.1)b | 3.6 (1.9 to 5.3)b |
| Other | 60.2 (55.0 to 65.3)d | 60.6 (55.2 to 65.7)d | 64.9 (60.3 to 69.2)d | 68.0 (63.0 to 72.6) | 73.8 (68.7 to 78.4)d | 77.6 (72.8 to 82.5)d | 17.4 (10.3 to 24.5)b | 3.7 (2.4 to 5.1)b |
| Mother’s educational level | ||||||||
| <High schoolc | 69.0 (65.3 to 72.6) | 71.9 (68.0 to 75.5) | 74.6 (71.2 to 77.7) | 77.6 (74.6 to 80.3) | 78.0 (73.6 to 81.9) | 84.2 (80.7 to 87.8)a | 15.2 (10.1 to 20.3)b | 2.8 (1.8 to 3.8)b |
| High school | 54.8 (51.8 to 57.8)d | 62.2 (59.5 to 64.8)a,d | 66.4 (63.6 to 69.0)a,d | 67.9 (64.8 to 70.8)d | 71.3 (67.8 to 74.5)d | 73.1 (70.3 to 76.0)d | 18.4 (14.2 to 22.5)b | 3.5 (2.7 to 4.3)b |
| Some college or college graduate | 52.2 (49.7 to 54.6)d | 56.2 (53.7 to 58.6)a,d | 63.0 (60.5 to 65.4)a,d | 65.1 (62.7 to 67.4)d | 68.7 (65.9 to 71.4)d | 71.8 (69.4 to 74.2)d | 19.6 (16.2 to 23.1)b | 4.0 (3.3 to 4.6)b |
| >College graduate | 55.1 (53.3 to 56.8)d | 58.2 (56.4 to 59.9)a,d | 63.6 (61.9 to 65.4)a,d | 67.1 (65.2 to 69.0)a,d | 71.3 (69.5 to 73.1 )a,d | 75.6 (74.1 to 77.2)a,d | 20.6 (18.2 to 22.9)b | 4.2 (3.7 to 4.6)b |
| Mother’s married status | ||||||||
| Married or living with partnerc | 54.6 (53.1 to 56.1) | 58.8 (57.3 to 60.2)a | 64.0 (62.5 to 65.3)a | 66.5 (65.0 to 67.9)a | 69.7 (68.2 to 71.2)a | 74.0 (72.6 to 75.4)a | 19.4 (17.4 to 21.4)b | 3.8 (3.4 to 4.2)b |
| Widowed, divorced, or separated | 57.0 (54.0 to 60.0) | 61.3 (58.4 to 64.1 )a | 67.3 (64.6 to 70.0)a,d | 69.7 (67.0 to 72.3)d | 73.9 (70.4 to 77.1 )d | 77.2 (74.7 to 79.7)d | 20.3 (16.4 to 24.2)b | 4.1 (3.2 to 4.9)b |
| Never married | 66.3 (62.4 to 70.1 )d | 70.0 (65.8 to 73.8)d | 73.7 (69.4 to 77.7)d | 75.9 (71.1 to 80.1 )d | 77.5 (72.3 to 82.0)d | 80.0 (76.3 to 83.8)d | 13.7 (8.3 to 19.1)b | 2.7 (1.6 to 3.7)b |
| Mother’s age | ||||||||
| ≤34 yc | 63.4 (59.2 to 67.5) | 66.2 (62.0 to 70.1) | 70.2 (66.1 to 74.0) | 70.6 (65.9 to 74.8) | 78.7 (74.6 to 82.3)a | 73.3 (68.8 to 77.8) | 9.9 (3.8 to 16.0)b | 2.6 (1.5 to 3.7)b |
| 35–44 y | 56.7 (54.7 to 58.7)d | 59.7 (57.7 to 61,5)a,d | 66.2 (64.3 to 68.1 )a | 67.4 (65.6 to 69.2) | 69.6 (67.4 to 71.7)d | 75.1 (73.4 to 76.8)a | 18.4 (15.8 to 21.0)b | 3.5 (3.0 to 4.0)b |
| ≥45 y | 54.2 (52.4 to 55.9)d | 60.0 (58.3 to 61,8)a,d | 64.1 (62.5 to 65.8)a,d | 68.3 (66.5 to 70.1 )a | 72.1 (70.2 to 73.8)a,d | 75.7 (74.0 to 77.4)a | 21.5 (19.0 to 23.9)b | 4.2 (3.8 to 4.7)b |
| Place of birth | ||||||||
| Born in United Statesc | 55.9 (54.6 to 57.2) | 60.0 (58.7 to 61,2)a | 65.0 (63.8 to 66.2)a | 67.7 (66.4 to 69.0)a | 71.3 (69.9 to 72.6)a | 75.0 (73.8 to 76.2)a | 19.1 (17.4 to 20.9)b | 3.8 (3.5 to 4.1)b |
| Born outside United States | 60.3 (54.3 to 66.0) | 67.4 (61.3 to 73.0)d | 73.1 (68.1 to 77.5)d | 74.8 (69.9 to 79.2)d | 75.7 (70.0 to 80.7) | 79.7 (73.5 to 85.9) | 19.4 (10.9 to 28.0)b | 3.5 (1.9 to 5.1)b |
| Income to poverty ratio | ||||||||
| <133%c | 63.2 (60.8 to 65.6) | 67.7 (65.5 to 69.9)a | 72.7 (70.5 to 74.7)a | 74.7 (72.4 to 76.8) | 76.2 (73.3 to 78.9) | 81.2 (79.0 to 83.4)a | 18.0 (14.7 to 21.2)b | 3.4 (2.7 to 4.0)b |
| 133% to <322% | 51.3 (48.9 to 53.7)d | 56.6 (54.3 to 58.9)a,d | 60.8 (58.5 to 63.1 )a,d | 64.0 (61.5 to 66.4)d | 67.7 (65.0 to 70.2)a,d | 70.2 (67.7 to 72.7)d | 18.9 (15.5 to 22.4)b | 3.8 (3.1 to 4.4)b |
| 322% to <503% | 51.4 (48.7 to 54.0)d | 53.0 (50.2 to 55.8)d | 61.1 (58.4 to 63.8)a,d | 63.7 (60.9 to 66.4)d | 67.7 (64.9 to 70.3)a,d | 70.4 (67.9 to 72.8)d | 19.0 (15.4 to 22.6)b | 4.0 (3.34.7)b |
| ≥503% | 56.0 (53.4 to 58.5)d | 60.8 (58.3 to 63.2)a,d | 64.7 (62.3 to 67.0)a,d | 68.1 (65.5 to 70.6)d | 73.1 (70.6 to 75.5)a | 78.1 (76.1 to 80.0)a,d | 22.1 (18.9 to 25.3)b | 4.3 (3.7–5.0)b |
| Medical insurancec | ||||||||
| Private onlyc | 52.5 (50.9 to 054.1) | 56.0 (54.4 to 57.6)a | 62.5 (60.8 to 64.1 )a | 65.4 (63.7 to 67.1 )a | 70.6 (68.9 to 72.2)a | 73.5 (71.9 to 75.0)a | 21.0 (18.7 to 23.2)b | 4.3 (3.9 to 4.8)b |
| Any Medicaid | 64.1 (61.8 to 66.3)d | 68.0 (65.9 to 70.1 )a,d | 71.3 (69.3 to 73.3)a,d | 74.4 (72.3 to 76.3)a,d | 75.0 (72.4 to 77.5)d | 79.8 (77.9 to 81.8)a,d | 15.8 (12.8 to 18.8)b | 2.9 (2.4 to 3.5)b |
| Othere,f | 51.6 (47.1 to 56.1) | 55.4 (51.4 to 59.4) | 62.0 (57.8 to 65.9)a | 63.7 (59.7 to 67.4) | 67.4 (62.9 to 71.7) | 71.3 (67.1 to 75.5) | 19.7 (13.5 to 25.8)b | 3.9 (2.7 to 5.1)b |
| Uninsured | 41.0 (34.8 to 47.5)d | 55.5 (48.2 to 62.5)a | 57.5 (51.8 to 62.9) | 56.2 (50.1 to 62.2)d | 60.3 (53.4 to 66.8)d | 65.6 (58.4 to 72.7)d | 24.6 (15.0 to 34.2)b | 3.9 (2.2 to 5.7)b |
| Provider contacts within past year | ||||||||
| Nonec | 46.8 (43.2 to 50.3) | 52.9 (49.1 to 56.6)a | 60.2 (56.8 to 63.5)a | 58.7 (55.2 to 62.2) | 62.9 (58.7 to 67.0) | 69.2 (65.9 to 72.6)a | 22.5 (17.6 to 27.4)b | 4.0 (3.1 to 5.0)b |
| 1 | 53.7 (51.2 to 56.2)d | 59.3 (57.0 to 61,6)a,d | 64.7 (62.3 to 66.9)a,d | 67.4 (65.0 to 69.6)d | 70.9 (68.2 to 73.4)a,d | 75.4 (73.3 to 77.6)a,d | 21.7 (18.4 to 25.0)b | 4.2 (3.5 to 4.8)b |
| 2–3 | 59.4 (57.4 to 61.3)d | 63.2 (61.2 to 65.1 )a,d | 67.5 (65.5 to 69.4)a,d | 69.9 (67.8 to 71.9)d | 73.7 (71.6 to 75.7)a,d | 76.8 (75.0 to 78.7)a,d | 17.4 (14.8 to 20.1 )b | 3.5 (3.0 to 4.0)b |
| ≥4 | 60.6 (57.9 to 63.1 )d | 63.1 (60.5 to 65.6)d | 67.1 (64.6 to 69.5)a,d | 72.2 (69.4 to 74.7)a,d | 73.0 (70.4 to 75.5)d | 77.3 (74.8 to 79.7)a,d | 16.7 (13.2 to 20.3)b | 3.4 (2.7 to 4.1)b |
| Well child visit at age 11–12 yg | ||||||||
| Yes | 61.6 (59.8 to 63.4)d | 66.9 (65.3 to 68.5)a,d | 71.7 (70.1 to 73.2)a,d | 73.7 (72.0 to 75.3)d | 78.0 (76.4 to 79.5)a,d | 80.3 (78.8 to 81.8)a,d | 18.7 (16.3 to 21,0)b | 3.7 (3.2 to 4.1)b |
| Noc | 47.1 (44.6 to 49.6) | 51.6 (48.9 to 54.3)a | 55.8 (53.2 to 58.4)a | 60.5 (57.8 to 63.2)a | 61.8 (58.7 to 64.8) | 64.8 (61.8 to 67.9) | 17.8 (13.8 to 21,7)b | 3.6 (2.9 to 4.3)b |
| Don’t know | 54.4 (51.9 to 56.8)d | 57.2 (54.8 to 59.5)d | 62.8 (60.5 to 65.1 )a,d | 64.4 (61.9 to 66.8)d | 67.1 (64.0 to 70.1 )d | 73.0 (70.9 to 75.1 )a,d | 18.7 (15.4 to 21,9)b | 3.6 (3.0 to 4.2)b |
| Number of providers | ||||||||
| 1 | 56.6 (55.0 to 58.3) | 63.1 (61.6 to 64.7)a,d | 67.4 (65.9 to 68.9)a,d | 70.1 (68.4 to 71.7)a,d | 74.3 (72.6 to 76.0)a,d | 76.7 (75.2 to 78.1 )a,d | 20.0 (17.8 to 22.2)b | 3.9 (3.5 to 4.3)b |
| 2 | 56.7 (54.2 to 59.2) | 57.5 (55.2 to 59.8) | 63.3 (60.8 to 65.6)a | 66.7 (64.4 to 68.9)a,d | 68.0 (65.3 to 70.6) | 75.5 (73.3 to 77.6)a,d | 18.7 (15.5 to 22.0)b | 3.6 (3.0 to 4.3)b |
| ≥3c | 53.6 (50.3 to 56.9) | 55.3 (51.7 to 58.8) | 61.9 (58.7 to 65.1 )a | 62.3 (58.9 to 65.6) | 67.2 (63.8 to 70.4)a | 68.5 (64.7 to 72.4) | 14.9 (9.8 to 20.0)b | 3.2 (2.3 to 4.1)b |
| MSA | ||||||||
| MSA principal cityc | 62.2 (60.1 to 64.2) | 65.9 (64.0 to 67.9)a | 70.1 (68.2 to 71,9)a | 71.9 (69.8 to 73.9) | 73.8 (71.5 to 75.9) | 77.8 (75.9 to 79.7)a | 15.6 (12.8 to 18.4)b | 2.9 (2.4 to 3.5)b |
| MSA nonprincipal city | 53.3 (51.4 to 55.2)d | 58.5 (56.6 to 60.3)a,d | 63.1 (61.3 to 64.8)a,d | 66.6 (64.8 to 68.4)a,d | 71.2 (69.2 to 73.1 )a | 74.7 (73.0 to 76.3)a,d | 21.4 (18.9 to 23.9)b | 4.2 (3.8 to 4.7)b |
| Non–MSA | 47.8 (45.2 to 50.4)d | 50.4 (47.8 to 53.0)d | 59.3 (56.6 to 61,9)a,d | 59.5 (56.8 to 62.2)d | 64.2 (61.2 to 67.2)a,d | 68.0 (65.2 to 70.8)d | 20.2 (16.4 to 24.0)b | 4.1 (3.4 to 4.8)b |
| Region | ||||||||
| Northeast | 62.6 (60.2 to 64.9) | 67.3 (65.0 to 69.5)a | 70.3 (68.1 to 72.5) | 71.1 (68.4 to 73.7) | 74.1 (71.5 to 76.6) | 79.4 (77.3 to 81 5)a | 16.8 (13.7 to 20.0)b | 3.0 (2.4 to 3.6)b |
| Midwest | 54.0 (51.9 to 56.0)d | 57.9 (55.7 to 60.0)a,d | 64.7 (62.8 to 66.6)a,d | 69.3 (67.3 to 71.2)a | 71.3 (69.2 to 73.2) | 75.5 (73.7 to 77.4)a | 21.6 (18.8 to 24.3)b | 4.4 (3.8 to 4.9)b |
| South | 52.1 (50.2 to 53.9)d | 54.8 (53.0 to 56.6)a,d | 61.4 (59.7 to 63.2)a,d | 63.8 (62.0 to 65.6)d | 68.0 (66.1 to 69.9)a,d | 72.3 (70.5 to 74.2)a,d | 20.3 (17.7 to 22.8)b | 4.1 (3.6 to 4.6)b |
| Westc | 60.1 (56.4 to 63.7) | 67.0 (63.6 to 70.2)a | 69.5 (66.1 to 72.7) | 71.9 (68.3 to 75.2) | 75.5 (71.5 to 79.1) | 78.1 (74.2 to 82.0) | 18.0 (12.7 to 23.3)b | 3.4 (2.4 to 4.4)b |
| Facility type | ||||||||
| All private facilitiesc | 55.9 (54.1 to 57.7) | 60.7 (59.0 to 62.4)a | 65.6 (63.9 to 67.2)a | 68.4 (66.6 to 70.1 )a | 72.2 (70.3 to 73.9)a | 76.5 (75.0 to 78.0)a | 20.6 (18.2 to 22.9)b | 4.0 (3.5 to 4.5)b |
| All public facilities | 55.4 (52.1 to 58.7) | 61.1 (57.9 to 64.2)a | 64.9 (61.6 to 68.0) | 67.2 (63.7 to 70.6) | 69.7 (65.6 to 73.5) | 73.5 (69.9 to 77.1) | 18.0 (13.1 to 22.9)b | 3.4 (2.5 to 4.3)b |
| All hospital facilities | 59.2 (55.5 to 62.7) | 66.3 (62.8 to 69.6)a,d | 67.9 (64.3 to 71.4) | 70.6 (67.1 to 74.0) | 74.4 (70.9 to 77.5) | 75.7 (72.7 to 78.6) | 16.5 (11.8 to 21.1 )b | 3.1 (2.2 to 3.9)b |
| All sexually transmitted diseases, school, and teen clinics or other facilities | 49.6 (37.7 to 61.5) | 59.2 (47.1 to 70.3) | 63.9 (54.3 to 72.6) | 70.1 (61.2 to 77.8) | 72.3 (60.9 to 81.3) | 70.2 (59.4 to 80.9) | 20.6 (4.4 to 36.8)b | 4.3 (1.0 to 7.7)b |
| Mixede,h | 58.0 (55.2 to 60.7) | 58.6 (55.8 to 61.3) | 66.9 (64.3 to 69.4)a | 69.8 (67.2 to 72.3) | 71.8 (68.6 to 74.7) | 76.4 (73.6 to 79.2)a | 18.5 (14.5 to 22.4)b | 3.9 (3.1 to 4.6)b |
| Otherc | 42.9 (33.1 to 53.2)d | 43.6 (33.2 to 54.5)d | 52.0 (43.1 to 60.8)d | 33.9 (25.1 to 44.0)a,d | 49.5 (38.8 to 60.4)a,d | 38.1 (27.0 to 49.2)d | −4.7 (−19.8 to 10.3) | −0.6 (−3.2–2.0) |
CI, confidence interval.
P < .05 for comparison with the previous year (t test for comparison between 2 y, with the prior year as the reference group- for example, 2016 vs 2015, 2017 vs 2016, 2018 vs 2017, 2019 vs 2018, and 2020 vs 2019).
P < .05 for overall trend (Linear trend test for trend from 2015 through 2020).
Reference level.
P < .05 compared with reference for each year within each variable.
Insurance categories are mutually exclusive.
Children’s Health Insurance Program, Indian Health Service, military, and some private.
Status of health-care visit at age 11–12 y based on provider reported data.
Mixed indicates that the facility is identified to be in more than one of the facility categories such as private, public, hospital, STD, school, and teen clinics.
Includes military, WIC clinics, and pharmacies.
Vaccination coverage among adolescents aged 16 to 17 years (range:58.8% in 2015 to 78.1% in 2020) was significantly higher than those aged 13 to 15 years in all survey years assessed (P < .05) except 2019 (P > .05) (range:54.4% in 2015 to 73.4% in 2020) (P < .05) (Table 2). Vaccination coverage among female adolescents (range:62.8% in 2015 to 76.8% in 2020) was significantly higher than male adolescents in all survey years assessed (range:49.8% in 2015 to 73.7% in 2020) (P < .05) (Table 2, Fig 1). Overall, HPV vaccination coverage (≥1 dose) among male adolescents aged 13 to 17 years significantly increased from 2015 to 2020, with a total increase of 24.0 percentage points and an average increase of 4.7 percentage points annually (Table 2, Fig 1). Overall, HPV vaccination coverage (≥1 dose) among female adolescents aged 13 to 17 years significantly increased from 2015 to 2020, with a total increase of 14.0 percentage points and an average increase of 2.7 percentage points annually (Table 2, Fig). Coverage increased faster among males than females and difference between males and females narrowed during this time. Vaccination coverage among non-Hispanic Black (range: 60.1% in 2015 to 78.3% in 2020) and Hispanic adolescents (range: 63.6% in 2015 to 80.7% in 2020) was significantly higher than non-Hispanic White adolescents in all years assessed (P < .05) except 2019, where coverage among non-Hispanic Black adolescents was not higher than coverage among non-Hispanic White adolescents (P > .05) (range: 51.4% in 2015 to 71.4% in 2020) (P < .05) (Table 2).
FIGURE 1.
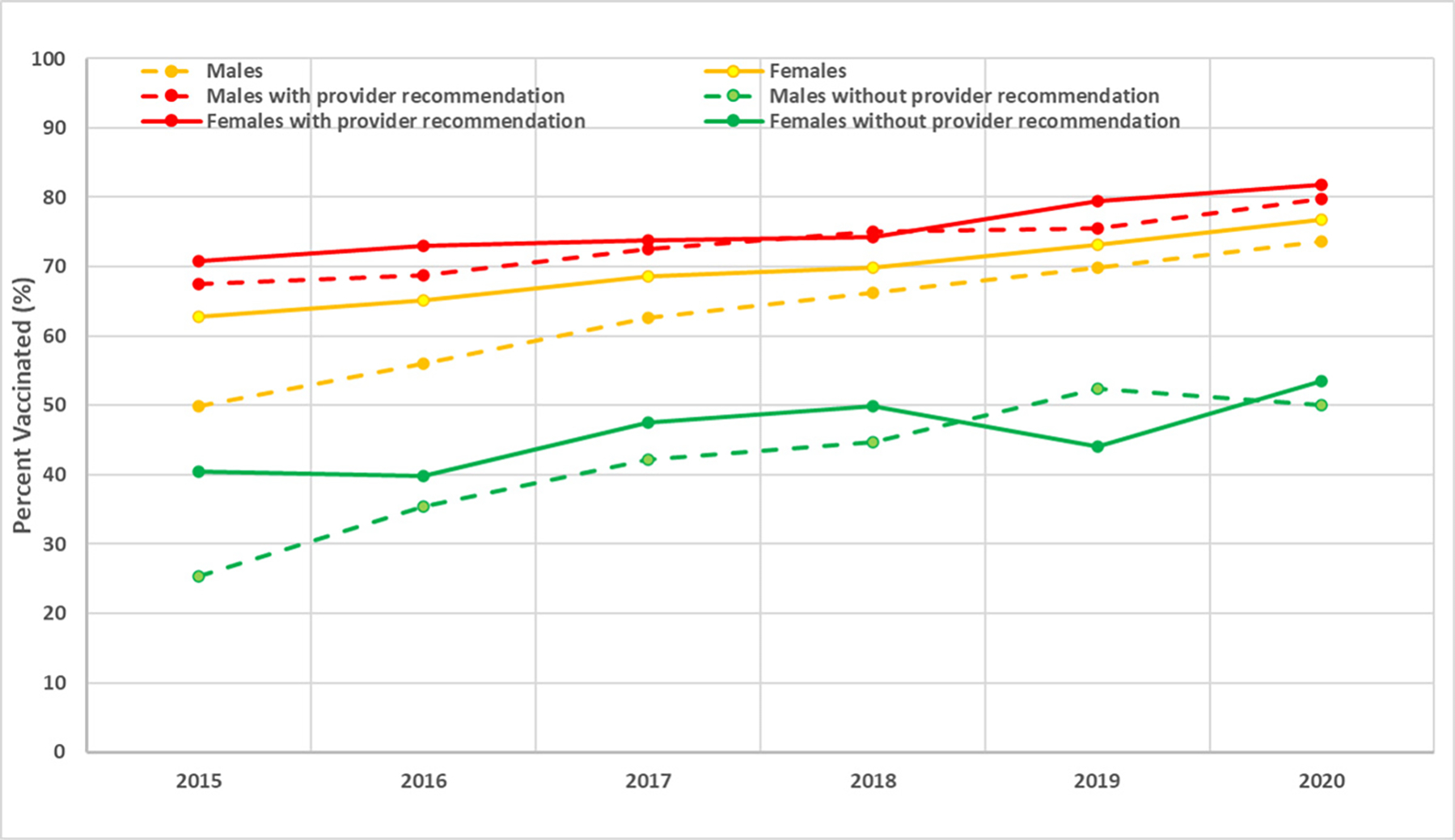
HPV vaccination coverage (≥1 dose) among adolescents 13 to 17 years, United States, 2015 to 2020. Source: national immunization survey teen, 2015 to 2020. Males, females, males with provider recommendation, males without provider recommendation, females with provider recommendation, and females without provider recommendation.
HPV vaccination coverage among adolescents aged 13 to 17 years with a reported provider recommendation significantly increased from 69.3% in 2015 to 80.7% in 2020 (test for trend, P <), and vaccination coverage of adolescents with a provider recommendation was consistently and significantly higher than those without a provider recommendation in all years assessed (range: 30.7% in 2015 to 51.7% in 2020) (P < .05) (Table 2). HPV vaccination coverage among male adolescents aged 13 to 17 years with a provider recommendation significantly increased from 67.5% in 2015 to 79.7% in 2020 (test for trend, P < .05), and vaccination coverage of male adolescents with a provider recommendation was consistently and significantly higher than those without a provider recommendation in all years assessed (range: 25.4% in 2015 to 52.4% in 2019) (P < .05) (Fig 1). HPV vaccination coverage among female adolescents aged 13 to 17 years with a provider recommendation significantly increased from 70.8% in 2015 to 81.8% in 2020 (test for trend, P < .05), and vaccination coverage of female adolescents with a provider recommendation was consistently and significantly higher than those without a provider recommendation in all years assessed (range: 39.8% in 2016 to 53.5% in 2020) (P < .05) (Fig 1). HPV vaccination coverage among adolescents aged 13 to 17 years with a well–child visit at age 11 to 12 years significantly increased from 61.6% in 2015 to 80.3% in 2020 (test for trend, P < .05), and vaccination coverage of adolescents with a well–child visit at age 11 to 12 years was consistently and significantly higher than those without a well–child visit at age 11 to 12 years over all years assessed (range: 47.1% in 2015 to 64.8% in 2020) (P < .05) (Table 2). Vaccination coverage among adolescents with 1 or more provider contacts within the past year was significantly higher than those without a provider contact within the past year in all years assessed (P < .05).
Additionally, vaccination coverage among adolescents with a mother who had equal to or more than a high school education was significantly lower than those with less than high school education in all years assessed (P < .05) (Table 2). Coverage among adolescents living in non-MSA areas was significantly lower than those living in MSA principal cities in all years assessed (P < .05) (Table 2).
In multivariable analyses of 2020 data, characteristics independently associated with a higher likelihood of HPV vaccination included: receiving a provider recommendation, being age 16 to 17 years, being of non-Hispanic Black, Hispanic, or American Indian or Alaskan Native (AIAN) adolescents (reference: non-Hispanic White adolescents), having a mother who is widowed, divorced, or separated (reference: married), having Medicaid insurance (reference: private insurance), having ≥2 provider contacts in the past 12 months (reference: without a provider contact), having a well–child visit at age 11 to 12 years (reference: without a well–child visit), and having 1 or 2 vaccination providers (reference: ≥3 vaccination provider) (P < .05). Participants having a mother with high school, some college or college graduate (reference: <high school), those with an income to poverty ratio between 133% and 503% (reference: <133%) and those living in non-MSA – more rural MSAs (reference: MSA principal city) had a lower likelihood of HPV vaccination (P < .05) (Table 3).
TABLE 3.
Multivariable Logistic Regression and Predictive Marginal Analysis of HPV Vaccination (≥1 Dose) of Adolescents Aged 13 to 17 Years in the United States, by Demographic and Access-to-Care Variables, NIS–Teen, 2020
| Characteristic | Adjusted Coverage % (95% CI) | Adjusted Prevalence Ratio % (95% CI) |
|---|---|---|
|
| ||
| Parental report of provider recommendation for vaccine | ||
| Yes | 64.4 (62.9–65.9) | 1.52 (1.41–1.62)a |
| Nob | 35.8 (32.6–39.0) | ref. |
| Age, y | ||
| 13–15b | 55.5 (53.7–57.3) | ref. |
| 16–17 | 65.3 (63.3–67.3) | 1.05 (1.02–1.09)a |
| Sex | ||
| Maleb | 57.4 (55.5–59.3) | ref. |
| Female | 61.3 (59.5–63.2) | 1.02 (0.99–1.05) |
| Race and ethnicity | ||
| Non–Hispanic Whiteb | 55.6 (53.8–57.4) | ref. |
| Non–Hispanic Black | 63.2 (59.3–67.0) | 1.10 (1.05–1.15)a |
| Hispanic | 65.6 (62.4–68.8) | 1.11 (1.07–1.16)a |
| American Indian or Alaskan Native | 74.6 (66.6–82.6) | 1.18 (1.08–1.27)a |
| Asian | 54.8 (47.7–61.9) | 1.00 (0.92–1.09) |
| Other | 60.7 (55.9–65.4) | 1.06 (1.00–1.13) |
| Mother’s educational level | ||
| <High schoolb | 62.7 (57.3–68.1) | ref. |
| High school | 57.5 (54.2–60.8) | 0.91 (0.85–0.97)a |
| Some college or college graduate | 56.1 (53.4–58.8) | 0.90 (0.84–0.96)a |
| >College graduate | 61.2 (59.1–63.3) | 0.94 (0.88–1.01) |
| Mother’s married status | ||
| Married or living with partnerb | 59.1 (57.4–60.8) | ref. |
| Widowed, divorced, or separated | 61.0 (58.1–63.9) | 1.04 (1.01–1.08)a |
| Never married | 57.5 (52.5–62.5) | 1.03 (0.96–1.10) |
| Mother’s age | ||
| ≤34 yb | 58.9 (54.0–63.9) | ref. |
| 35–44 y | 58.5 (56.5–60.5) | 1.02 (0.96–1.09) |
| ≥45 y | 60.2 (58.1–62.3) | 1.02 (0.95–1.08) |
| Place of birth | ||
| Born in United Statesb | 59.2 (57.8–60.6) | ref. |
| Born outside United States | 63.1 (55.4–70.8) | 1.06 (0.97–1.15) |
| Income to poverty ratio | ||
| <133%b | 62.3 (58.9–65.7) | ref. |
| 133% to <322% | 55.0 (52.3–57.7) | 0.94 (0.89–0.98)a |
| 322% to <503% | 58.9 (56.1–61.7) | 0.93 (0.88–0.99)a |
| ≥503% | 61.5 (58.7–64.4) | 1.02 (0.96–1.07) |
| Medical insurancec | ||
| Private onlya | 58.2 (56.1–60.4) | ref. |
| Any Medicaid | 62.6 (59.7–65.4) | 1.07 (1.02–1.12)a |
| Otherd | 56.2 (51.3–61.2) | 1.03 (0.97–1.08) |
| Uninsured | 52.4 (43.9–60.9) | 0.94 (0.83–1.05) |
| Provider contacts within past year | ||
| Noneb | 52.5 (48.8–56.2) | ref. |
| 1 | 58.6 (56.3–61.0) | 1.05 (0.99–1.11) |
| 2–3 | 61.8 (59.7–63.9) | 1.08 (1.02–1.14)a |
| ≥4 | 61.9 (58.9–64.9) | 1.06 (1.00–1.13)a |
| Well child visit at age 11–12 ye | ||
| Yes | 64.4 (62.6–66.3) | 1.17 (1.11–1.23)a |
| Nob | 46.5 (43.2–49.8) | ref. |
| Don’t know | 58.0 (55.5–60.4) | 1.07 (1.00–1.13)a |
| Number of providers | ||
| 1 | 61.1 (59.3–62.9) | 1.12 (1.05–1.19)a |
| 2 | 59.3 (56.7–61.8) | 1.10 (1.03–1.17)a |
| ≥3b | 50.9 (46.9–54.9) | ref. |
| MSA | ||
| MSA Principal Cityb | 60.0 (57.9–62.2) | ref. |
| MSA Non–Principal City | 59.8 (57.9–61.8) | 0.98 (0.95–1.02) |
| Non–MSA | 54.4 (51.1–57.7) | 0.94 (0.89–0.98)a |
| Region | ||
| Northeast | 64.4 (61.8–67.0) | 1.02 (0.96–1.07) |
| Midwest | 61.6 (59.4–63.9) | 1.01 (0.96–1.07) |
| South | 56.0 (53.9–58.1) | 0.96 (0.91–1.01) |
| Westb | 59.4 (55.1–63.7) | ref. |
| Facility type | ||
| All private facilitiesb | 58.6 (56.7–60.5) | ref. |
| All public facilities | 56.3 (52.1–60.6) | 1.01 (0.96–1.07) |
| All hospital facilities | 59.6 (56.1–63.1) | 1.00 (0.96–1.05) |
| All sexually transmitted diseases, school, and teen clinics or other facilities | 54.7 (44.1–65.4) | 0.94 (0.80–1.07) |
| Mixedf | 64.7 (61.4–67.9) | 1.07 (1.03–1.12)a |
| Otherg | 45.8 (33.8–57.8) | 0.70 (0.55–0.85)a |
CI, confidence interval; ref., reference.
P <05 compared with reference level.
Reference level.
Insurance categories are mutually exclusive.
Children’s Health Insurance Program, Indian Health Service, military, and some private.
Status of health-care visit at age 11 to 12 y based on provider reported data.
Mixed indicates that the facility is identified to be in more than one of the facility categories such as private, public, hospital, STD, school, and teen clinics.
Includes military, WIC clinics, and pharmacies.
DISCUSSION
Overall, HPV vaccination coverage among adolescents increased from 2015 to 2020. Vaccination coverage (≥1 dose) significantly increased across almost all levels of variables assessed. There were larger increases among males than females and difference between males and females narrowed during this time. Vaccination coverage significantly differed over the years assessed by age group, race and ethnicity, provider recommendation, well-child visit, number of provider visits within previous 12 months, and other characteristics. Even though coverage substantially increased over the years, ~25% of adolescents had not received at least 1 dose of HPV vaccination in 2020. Targeted strategies are needed to increase coverage and narrow down inequalities.
Overall, HPV vaccination coverage (≥1 dose) among adolescents 13 to 17 years in 2020 was 76.8% among females, and 73.7% among males. Historically, coverage in female adolescents increased from 25.1% in 2007 to 62.8% in 2015 (about 8 years since vaccination was initially recommended).12–14 Likewise, among males, HPV vaccination coverage has also substantially increased since the vaccine was first recommended for males in 2011.15 Coverage among males increased from 20.9% in 2012 to 73.7% in 2020 (about 9 years since vaccination was first recommended for male adolescents).16 Data from our study found that coverage in adolescents during 2015 through 2020 significantly increased a total of 24.0 percentage points for males and 14.0 percentage points for females, with an average increase of 4.7 percentage points annually for males and 2.7 percentage points annually for females. During this time, the difference between coverage among males and females decreased from 13 to 3 percentage points. Coverage among adolescents substantially increased in recent years is encouraging, especially among males.
Studies consistently have found that a provider recommendation is highly associated with HPV vaccination.17–19 Results from our study confirmed this association. One study showed that the prevalence of providers strongly recommending HPV vaccination substantially increased over the years for female and male children.20 However, based on data from the 2020 NIS-Teen, even among those who reported a provider recommendation for the vaccine, only 80.7% received vaccination, indicating that other factors might also contribute to adolescents not being vaccinated. The result from our study also showed that the prevalence of receiving a provider recommendation among adolescents substantially increased during 2015 to 2020. One study found coverage in female adolescents (≥1 dose) was 58.3% in 2008 to 2009 among adolescents with a provider recommendation compared with those without (20.7%).21 Another study among male adolescents showed that “a provider recommendation was associated with higher HPV vaccination coverage across the majority of states.”18 Studies also showed that “recommendations from providers increase parental acceptance of HPV vaccination and that parents change their minds about delaying and refusing vaccines because of information or assurances from health care providers.”22,23 However, our study showed that 18.5% of parents of adolescents did not receive a provider recommendation. Providers should routinely recommend the vaccine and highlight importance of vaccination in preventing HPV-related cancers.
The results from our study demonstrated that provider contacts and a well–child visit had a positive impact on vaccination coverage. Persons with more provider contacts may have more chance to consult with providers regarding their immunization situation, get a recommendation, and receive vaccination. The ACIP and partner organizations recommend a well–child visit to vaccinate teens who have not initiated vaccinations; administer a booster dose if needed; and provide other recommended preventive services.24,25 Even though the well–child visit provides a chance to discuss vaccination status and receive recommended vaccinations, only 46.3% to 50.4% of children had a well–child visit at age 11 to 12 years based on the 2015 to 2020 NIS–Teen. Providers should educate parents and adolescents about the diseases that can be prevented by vaccines, review medical records, and administer all age-appropriate vaccinations at all health care visits.26
Findings from our study indicated that coverage for adolescents residing in non-MSA areas was consistently and significantly lower than those residing in MSA principal cities in all years assessed, and this association remained after controlling for other variables. The inequity in coverage by MSA is not clear; however, the lower provider recommendation rate and less vaccination-related information available in non-MSA areas might contribute to coverage disparity.8,27,28
HPV vaccination coverage among adolescents was higher for non-Hispanic Black, Hispanic, and AIAN adolescents compared with non-Hispanic White adolescents. Increased vaccine access by the Vaccine for Children program (providing free recommended vaccines to children without health insurance and children who are under-insured) or risk-based provider recommendations for HPV on the perceived level of the patient’s risk for HPV-related cancer morbidity and mortality might contribute to the increased HPV vaccination coverage in these minority groups.29–31
Findings from our study indicated that mothers with higher education were associated with decreased HPV vaccination coverage, which is similar to the findings from the previous reports.18,27 Another study also found that intent to have their child vaccinated was lower among mothers with higher education.31 Further research should be conducted to understand why teens whose mothers with a higher education had lower HPV vaccination coverage.
The findings in this study are subject to 2 limitations. First, the overall household response rate in 2020 was 20.7%, and 45.2% of adolescents with completed interviews had adequate provider data. However, the estimated total survey error of HPV vaccination coverage from the 2018 NIS–Teen is −1.6 percentage points, indicating HPV vaccination coverage based on NIS–Teen was only ~1.6 percentage points too low.9 Additionally, the distribution of characteristics (eg, age, gender, and race and ethnicity) from the 2020 NIS–Teen were close to those observed in the child core data of the 2020 National Health Interview Survey (CDC unpublished data). Second, bias in estimates might remain even after adjustment for household and provider nonresponse and phoneless households.
In conclusion, HPV vaccination coverage among adolescents aged 13 to 17 years increased during 2015 to 2020. Vaccination coverage significantly differed over the years when assessed by provider recommendation, well-child visit at age 11 to 12 years, number of provider contacts in the past 12 months, age group, race and ethnicity, and other characteristics. Targeted strategies should be implemented to providers who serve different communities, particularly those who serve non-Hispanic White children. The association between mother’s education and HPV vaccination coverage indicated that interventions should consider maternal education attainment, and further research should be conducted to understand why teens whose mothers with a higher education had lower HPV vaccination coverage. It is encouraging that coverage among male adolescents substantially increased in recent years. To increase HPV vaccination coverage and further reduce HPV-related morbidity and mortality, providers, parents, and adolescents should use every health care visit as a chance to review vaccination histories and ensure that every adolescent receives the HPV vaccine and other needed vaccines.32–36
WHAT’S KNOWN ON THIS SUBJECT
Human Papillomavirus (HPV) is the most common sexually transmitted infection. Vaccination is an important tool to prevent and control HPV infection and its complications. HPV vaccination in the United States has been recommended for girls since 2006 and for boys since 2011.
WHAT THIS STUDY ADDS
This study examines HPV vaccination trends. HPV vaccination coverage among adolescents increased during 2015 to 2020. Coverage increased faster among males than females and differences by sex narrowed. Receiving provider recommendation is important to increase vaccination coverage.
ACKNOWLEDGMENTS
We thank James A. Singleton of the Immunization Services Division, National Center for Immunization and Respiratory Diseases, Centers for Disease Control and Prevention, for his important review and contributions.
FUNDING:
No external funding.
ABBREVIATIONS
- HPV
human papillomavirus
- ACIP
Advisory Committee on Immunization Practices
- PR
prevalence ratio
- 95% CI
95% confidence interval
- RDD
random-digit–dial
- CDC
Centers for Disease Control and Prevention
- STD
sexual transmitted diseases
- WIC
Women, Infants, and Children
- MSA
metropolitan statistical area
- NIS-Teen
National Immunization Survey-Teen
- VFC
Vaccines for Children
- CASRO
The Council of American Survey Research Organizations
- NORC
National Opinion Research Center
Footnotes
CONFLICT OF INTEREST DISCLOSURES: The authors have indicated they have no potential conflicts of interest to disclose.
REFERENCES
- 1.Kreisel KM, Spicknall IH, Gargano JW, et al. Sexually transmitted infections among US women and men: prevalence and incidence estimates, 2018. Sex Transm Dis. 2021;48(4):208–214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Markowitz LE, Dunne EF, Saraiya M, Lawson HW, Chesson H, Unger ER; Centers for Disease Control and Prevention (CDC); Advisory Committee on Immunization Practices (ACIP). Quadrivalent human papillomavirus vaccine: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2007;56(RR-2):1–24 [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention (CDC). Recommendations on the use of quadrivalent human papillomavirus vaccine in males–Advisory Committee on Immunization Practices (ACIP), 2011. MMWR Morb Mortal Wkly Rep. 2011;60(50):1705–1708 [PubMed] [Google Scholar]
- 4.Petrosky E, Bocchini JA Jr, Hariri S, et al. ; Centers for Disease Control and Prevention (CDC). Use of 9-valent human papillomavirus (HPV) vaccine: updated HPV vaccination recommendations of the advisory committee on immunization practices. MMWR Morb Mortal Wkly Rep. 2015;64(11):300–304 [PMC free article] [PubMed] [Google Scholar]
- 5.Meites E, Kempe A, Markowitz LE. Use of a 2-dose schedule for human papillomavirus vaccination — updated recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep. 2016;65(49):1405–1408 [DOI] [PubMed] [Google Scholar]
- 6.Meites E, Szilagyi PG, Chesson HW, Unger ER, Romero JR, Markowitz LE. Human papillomavirus vaccination for adults: updated recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep. 2019;68(32):698–702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention (CDC). National and state vaccination coverage among adolescents aged 13–17 years – United States, 2020. MMWR Morb Mortal Wkly Rep. 2021;70(35):1183–1190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention (CDC). National and state vaccination coverage among adolescents aged 13–17 years – United States, 2019. MMWR. 2020;69(33):1109–1116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention (CDC). National Immunization Survey–Teen. Available at: https://www.cdc.gov/vaccines/imz-managers/nis/downloads/NIS-TEEN-PUF20-DUG.pdf. Accessed January 16, 2022 [Google Scholar]
- 10.Centers for Disease Control and Prevention (CDC). National Immunization Survey–Teen. Available at: https://www.cdc.gov/vaccines/imz-managers/nis/datasets-teen.html. Accessed January 16, 2022 [Google Scholar]
- 11.Centers for Disease Control and Prevention (CDC). Impact of a methodological change from a dual-frame landline and cell-phone sample design to a single-frame cell-phone sample design on vaccination coverage estimates among adolescents 13–17 years, National Immunization Survey–Teen, 2016–2017. Available at: https://www.cdc.gov/vaccines/imz-managers/coverage/teenvaxview/pubs-presentations/dual-to-single-frame-teen.html. Accessed April 8, 2022 [Google Scholar]
- 12.Centers for Disease Control and Prevention (CDC). Vaccination coverage among adolescents aged 13–17 years - United States, 2007. MMWR Morb Mortal Wkly Rep. 2008;57(40):1100–1103 [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention (CDC). National and state vaccination coverage among adolescents aged 13–17 years – United States, 2014. MMWR Morb Mortal Wkly Rep. 2015;64(29):784–792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reagan-Steiner S, Yankey D, Jeyarajah J, et al. ; Centers for Disease Control and Prevention (CDC). National, regional, state, and selected local area vaccination coverage among adolescents aged 13–17 years - United States, 2015. MMWR Morb Mortal Wkly Rep. 2016;65(33):850–858 [DOI] [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention (CDC). National and state vaccination coverage among adolescents aged 13–17 years–United States, 2011. MMWR Morb Mortal Wkly Rep. 2012;61(34):671–677 [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention (CDC). National and state vaccination coverage among adolescents aged 13–17 years–United States, 2012. MMWR Morb Mortal Wkly Rep. 2013;62(34):685–693 [PMC free article] [PubMed] [Google Scholar]
- 17.Lu PJ, Yankey D, Jeyarajah J, et al. Impact of provider recommendation on Tdap vaccination of adolescents aged 13–17 years. Am J Prev Med. 2017;53(3):373–384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lu PJ, Yankey D, Fredua B, et al. Association of provider recommendation and human papillomavirus vaccination initiation among male adolescents aged 13–17 years-United States. J Pediatr. 2019;206:33–41.e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Smith PJ, Stokley S, Bednarczyk RA,Orenstein WA, Omer SB. HPV vaccination coverage of teen girls: the influence of health care providers. Vaccine. 2016;34(13):1604–1610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cataldi JR, O’Leary ST, Markowitz LE, et al. Changes in strength of recommendation and perceived barriers to HPV vaccination: longitudinal analysis of primary care physicians, 2008–2018 [published online ahead of print March 6, 2021]. J Pediatr. doi: 10.1016/j.jpeds.2021.03.00 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dorell CG, Yankey D, Santibanez TA,Markowitz LE. Human papillomavirus vaccination series initiation and completion, 2008–2009. Pediatrics. 2011; 128(5):830–839 [DOI] [PubMed] [Google Scholar]
- 22.Gust DA, Darling N, Kennedy A, Schwartz B. Parents with doubts about vaccines: which vaccines and reasons why. Pediatrics. 2008;122(4):718–725 [DOI] [PubMed] [Google Scholar]
- 23.Gerend MA, Weibley E, Bland H. Parental response to human papillomavirus vaccine availability: uptake and intentions. J Adolesc Health. 2009;45(5):528–531 [DOI] [PubMed] [Google Scholar]
- 24.Jain N, Stokley S, Cohn A. Receipt of tetanus-containing vaccinations among adolescents aged 13 to 17 years in the United States: National Immunization Survey-Teen 2007. Clin Ther. 2010;32(8):1468–1478 [DOI] [PubMed] [Google Scholar]
- 25.Centers for Disease Control and Prevention (CDC). Immunization of adolescents. recommendations of the Advisory Committee on Immunization Practices, the American Academy of Pediatrics, the American Academy of Family Physicians, and the American Medical Association. MMWR Recomm Rep. 1996;45(RR-13):1–16 [PubMed] [Google Scholar]
- 26.Centers for Disease Control and Prevention (CDC). HPV vaccine. Available at: https://www.cdc.gov/hpv/hcp/index.html Accessed April 5, 2022 [Google Scholar]
- 27.Walker TY, Elam-Evans LD, Williams CL, et al. Trends in human papillomavirus (HPV) vaccination initiation among adolescents aged 13–17 by metropolitan statistical area (MSA) status, National Immunization Survey - Teen, 2013 – 2017. Hum Vaccin Immunother. 2020;16(3):554–561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Boyd ED, Phillips JM, Schoenberger YM, Simpson T. Barriers and facilitators to HPV vaccination among rural Alabama adolescents and their caregivers. Vaccine. 2018;36(28):4126–4133 [DOI] [PubMed] [Google Scholar]
- 29.Hughes CC, Jones AL, Feemster KA, Fiks AG. HPV vaccine decision making in pediatric primary care: a semi-structured interview study. BMC Pediatr. 2011;11:74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sexual Health. Health disparities inHPV-related cancers. Available at: https://www.verywellhealth.com/health-disparities-in-hpv-related-cancers-4173225\. Accessed April 9, 2022 [Google Scholar]
- 31.Mohammed KA, Vivian E, Loux TM, Arnold LD. Factors associated with parents’ intent to vaccinate adolescents for human papillomavirus: findings from the 2014 National Immunization Survey–Teen. Prev Chronic Dis. 2017;14:E45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gilkey MB, Calo WA, Moss JL, Shah PD, Marciniak MW, Brewer NT. Provider communication and HPV vaccination: the impact of recommendation quality. Vaccine. 2016;34(9):1187–1192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Guide to Community Preventive Services. Vaccination. Available at www.thecommunityguide.org/index.html. Accessed November 25, 2021
- 34.National Center for Immunization and Respiratory Diseases. General recommendations on immunization — recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2011;60(2):1–64 [PubMed] [Google Scholar]
- 35.McClung NM, Lewis RM, Gargano JW, Querec T, Unger ER, Markowitz LE. Declines in vaccine-type human papillomavirus prevalence in females across racial/ethnic groups: data from a national survey. J Adolesc Health. 2019;65(6):715–722 [DOI] [PubMed] [Google Scholar]
- 36.Gargano JW, Park IU, Griffin MR, et al. ; HPV-IMPACT Working Group. Trends in high-grade cervical lesions and cervical cancer screening in 5 states, 2008–2015. Clin Infect Dis. 2019;68(8):1282–1291 [DOI] [PMC free article] [PubMed] [Google Scholar]


