Abstract
Introduction/Objectives:
Thailand has approached an aged society in which the proportion of older adults rose from 5% in 1995 to 20.7% in 2022 and is projected to increase to 27.2% in 2030. Older adults face health risks and challenges, requiring supportive care. This research aimed to promote the wellness of older adults through Integrated Health-Promoting Programs and Supportive Peers (IHPP-SP) in semi-urban communities.
Methods:
A one-group pretest-posttest quasi-experimental study was conducted among 229 older adults from 22 communities. The interventions covered analyzing community situations and determinants, designing and developing IHPP-SP, enhancing the capabilities of supportive peers, and establishing a support system. Mean and proportion differences were analyzed using the paired t-test and McNemar test.
Results:
After implementing IHPP-SP, the mean score significantly increased for happiness (P = .004), Activities of Daily Living: ADLs (P = .034), and family support (P < .001), but did not differ regarding depression (P = .413). The proportion of healthy behaviors significantly increased for tobacco use (P = .035), dietary intake (P = .018), and physical activity (P < .001), but not for alcohol consumption (P = .377).
Conclusions:
The IHPP-SP provided potential benefits to promote the wellness of older adults.
Keywords: well-being, elderly, integrated program, multi-sectors, participation
Introduction
The term, “older persons” or “older adults” refers to individuals 60 years of age or older. Although the World Health Organization (WHO) later recommended changing the definition of older persons to 65 years and older,1 -3 Thailand still uses the previous definition due to the context, development plans, and related laws.4 -6 Thailand is the second-fastest aging country in the Association of Southeast Asian Nations (ASEAN) after Singapore. 5 The proportion of older adults in Thailand rose from 5% of the total population in 1995 to 13% in 2010 and 20.7% in 2022 and is projected to increase to 27.2% in 2030 and over 30% by 2040. 6 Nakhon Ratchasima Province has the largest area with the second most populated province, located in northeastern Thailand.7,8 The proportion of older adults in Nakhon Ratchasima has increased similarly to that of the country; 19.4% in 2022.9,10 The transition to an increasingly aging society is a result of decreased births and deaths as well as increased life expectancy which has risen from 70.67 years in 2000 to 77.74 in 2022 and is projected to rise to 80.72 years in 2040. 11 Older adults may become the country’s main workforce in place of younger working-age groups and become a burden in maintaining their health and improving their quality of life.
People of advanced age will experience changes in physical, mental, and social roles, including health problems, illnesses, and decreased daily activities and quality of life. Common health problems among older adults include hypertension, diabetes, heart diseases, musculoskeletal system diseases, depression, and the sequelae of these conditions.12 -18 Older adults are more likely to use Emergency Medical Services (EMS) than younger ages including repeat EMS use and pre-hospital emergency care.19 -21 Approximately one-half of older adults sought care for issues including accessibility to healthcare services, financial support, social support, and long-term care. 22 In addition, one-half of older adults with active lifestyles and exercise were also reported for functionally limited, indicating an increased risk for mobility and activity of daily living disability 4 years later. 23 An aging society and the implications for services highlight the need that older adults require care and support from themselves, family members, communities, and relevant institutions in a holistic manner. Related studies have found that programs for Thai older adults are not well-grounded. Most intervention programs developed by researchers focus on increasing the knowledge and developing the skills of family caregivers, such as by providing information, skills training, and home visits.24 -27 These studies have used theories and concepts such as the Transitional Care Model, Orem’s Self Care Deficit Nursing Theory, and the Chronic Care Model.28 -30 The limitations of the programs presented in related studies may stem from their focus on the individual level, for example, family caregivers, rather than the family and community system, including the whole family as a unit. Few intervention studies have assessed family variables that may affect outcomes or measured family functioning in caring for older adults. Community-based elderly care encourages local government organizations to demonstrate the capacity to lead elderly care at the community level. They have the advantage of residing close to local communities. Therefore, they know the local population characteristics and specific health problems, helping them determine the best solutions to fit local contexts. 31 The current research aimed to assess the wellness of older adults compared before and after implementing the integrated health-promoting programs and supportive peers (IHPP-SP) participatory developed by stakeholders from communities and involving sectors.
Methods
Study Areas
This study was conducted in Sung Noen District of Nakhon Ratchasima Province, possessing the largest area with the second most populous province located as a gateway to other provinces in northeastern Thailand. Sung Noen District comprises 11 subdistricts totaling 72,559 residents in 2022. Industrial estates and large industrial companies are located in the district and most residents are farmers and industrial workers.10,32
Study Design and Samples
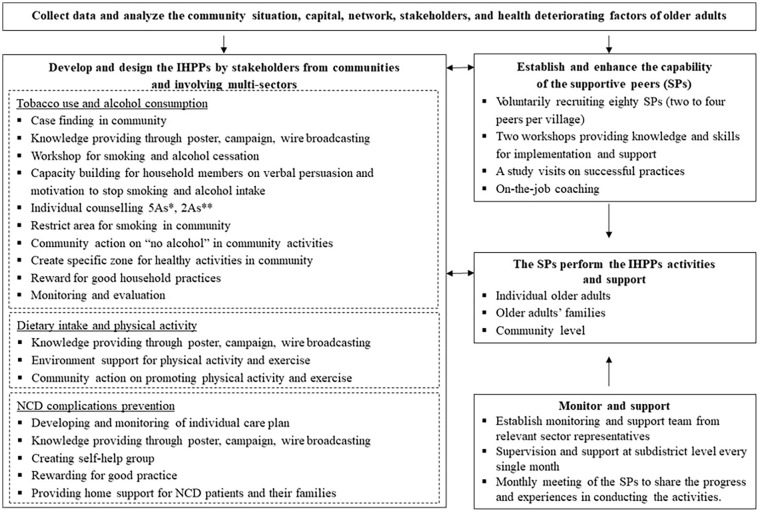
A quasi-experimental study was carried out from August 2018 to October 2019 using a one-group pretest-posttest design as illustrated in the following diagram:
where O1 and O2 were the variables evaluated before and 8 months after implementing interventions consisting of physical and mental health (happiness, depression, Barthel Index for Activities of Daily Living (ADLs), family support) and health behaviors (tobacco use, alcohol consumption, dietary intake, and physical activity); X were the interventions implemented to promote the wellness of the older adults through integrated health-promoting programs and supportive peers (IHPP-SP) as seen in Figure 1. The IHPP-SP was developed by stakeholders from communities, for example, community leaders, village health volunteers, representatives of elderly clubs, and caregivers, and involved multi-sectors (universities, district health office, community hospital, community development office, and private companies). Two participatory workshops among the stakeholders were conducted. The first workshop started by envisioning determining the desirable image of healthy older adults. Current situations from the baseline survey were discussed and gaps compared with the desirable image were identified. The prioritized health problems and health needs of older adults were noncommunicable diseases (NCDs); hypertension, hyperlipidemia, and diabetes mellitus; and their complications, risk behaviors for NCDs (dietary intake, physical activity, tobacco use, alcohol consumption), depression, obstacles in performing daily activities, and lack of practical guidance and support for ongoing self-care. In the second workshop, approaches and strategies for promoting the wellness of older adults based on social capital and community context were brainstormed. Action plans were developed along with implementation mechanisms at the individual, household, and community levels. The supportive peers (SPs) were nominated by the communities and took part in the project on a voluntary basis. Two workshops, study visits on successful practices and a coaching system from the relevant sectors were conducted to improve their skills and implementation. The SPs then carried out activities with the individual older adults, their families and at community level. These included knowledge transfer, counseling, care plan monitoring, capacity building of family members, home visits, moral support, self-help group formation, community and environmental management, and evaluation.
Figure 1.
Research interventions to promote the wellness of older adults through integrated health-promoting programs and supportive peers (IHPP-SP); *5As refer to Ask, Assess, Advise, Assist, and Arrange; **2As refer to Ask and Act.
Our sample size was calculated by the following formula for comparing 2 dependent population means. 33
where the standard deviation (σ) of depression scores among older adults was 3.75 34 ; the difference in means (∆) of depression scores between before and after implementation was 0.75; significant level (α) was 0.05, and type II error probability (β) was 0.20. Two subdistricts, municipality and outside municipality area, were randomly selected by simple random sampling. Households having older adults aged 60 and older from all communities (22 villages) were then randomly selected using a simple random sampling method. The samples comprised 229 older adults who could communicate in Thai, voluntarily participated in the project, signed the consent form, and stayed in the area throughout the implementation. Older adults who became sick and needed to be hospitalized for more than 4 weeks consecutively, as well as those who later withdrew from the project, were excluded. No compensation was provided for participating in this project apart from activities and services related to the project.
Research Tools and Measurements
The structured questionnaires used before and after implementing the programs were developed and corrected for content validity by 5 experts from universities and colleges, academic institutes, and public health organizations in the study area. Thereafter, the questionnaires were piloted among ten older adults in nearby areas to check for understanding, and ensure a smooth interview process and were revised for collecting data in the study areas. Study variables and measurements are described below.
General characteristics consisting of sex, age, marital status, education, religion, occupation, income, and current illnesses were assessed using 8 multiple-choice and open-ended questions.
Overall happiness was self-assessed by the older adults. A score from 0 to 10 for “not happy at all” to “happiest” was classified by applying the Happinometer assessment as “very unhappy” (0.00-2.49), “unhappy” (2.50-4.99), “happy” (5.00-7.49), and “very happy” (7.50-10.00). 35
Depression was assessed to detect the risk of depression using 9 rating scale questions (PHQ-9) revised for the Thai central dialect. A score of 0 to 4 for “none” to “every day” was assigned. A total score (0-27) classified the older adults into 4 groups: “no symptoms or very few symptoms of depression” (0-6); “mild symptoms of depression” (7-12); “moderate symptoms of depression” (13-18) and; “having symptoms of severe depression” (19-27).34,36
ADLs were assessed using ten ordinal scale questions of the Barthel ADLs in the Thai central dialect. It comprised 10 questions with 2 to 4 response options. A score of 0 to 3 for “unable” to “independent” was assigned. A total score (0-20) classified older adults into the following 3 groups: a “social-bound” group (12-20) refers to older adults who are self-reliant and able to help others, community members, and society; a “home-bound” group (5-11) refers to older adults who can partially take care of themselves and can partially help themselves; a “bed-bound or bed-ridden” group (0-4) refers to older adults who are unable to rely on themselves, are unable to help themselves, and are disabled or handicapped.37,38
Family support was assessed using 3 ordinal scale questions: indoor activities, discussing, and outdoor activities. A score of 0 to 3 for “none” to “regular” was assigned. A total score (0-9) was classified using the 75th percentile as the cutoff point in “poor to moderate family support” (0-6) and “good family support” (7-9).
Tobacco use and alcohol consumption were assessed using two-choice questions. Tobacco use was categorized as “never or rarely used” and “used regularly” meanwhile alcohol consumption was categorized as “never or rarely consumed” and “consumed regularly.” Dietary intake focused on a healthy diet to prevent and reduce NCD risks; vegetables and fruits, low-fat foods, low-sodium foods, and low-sugar foods and drinks. Dietary intake was assessed using 7 ordinal scale questions. A score of 0 to 4 for “never ate” to “ate every day” was assigned. A total score (0-28) was classified using the cutoff point at the 75th percentile in “moderate to high risk for NCDs” (0-20) and “low risk for NCDs” (21-28). Physical activity was assessed based on WHO guidelines for adults aged 18 to 64 years and adults aged 65 years and above who should have physical activity for at least 75 to 300 min throughout the week. 39 Five multiple-choice with open-ended questions were developed comprising vigorous, moderate, and light physical activity or exercise. A score of 0 was given to “having physical activity less than 30 minutes/week,” while 1 was awarded to “having physical activity at least 30 minutes/week.” A total score (0-5) was classified using a cutoff point at the 75th percentile in “improper physical activity” (0-3)” and “proper physical activity” (4-5).
Data Collection
Face-to-face interviews, both before and after implementing IHPP-SP were conducted by public health students from universities and colleges in the study area. The interviewers attended a 1-day training on interview objectives, questions, interview techniques, and unbiased interview guidelines including compliance with human research ethics. The respondents were informed of the research details, voluntarily participated in the project, and signed a consent form before being interviewed.
Data Analysis
Data were processed and analyzed using EpiData Version 3.10 and SPSS for Windows Version 18.0.40,41 Study variables were described using percentage, arithmetic mean, and standard deviation. Mean differences between pre-and post-test were determined by Paired t-test, while proportion difference was analyzed using the McNemar test. P < .05 was considered as statistical significance.
Research Ethics
This research was conducted according to human research ethics practices. Written informed consent was introduced and the respondents signed for voluntary participation. This project was approved by the Human Research Ethics Committee, Faculty of Public Health, Mahidol University [COA. No. MUPH 2018-168; Protocol No. 151/2018].
Results
Characteristics of Older Adults
The majority of older adults were female, 60 to 69 years old, married with spouses remaining together, educated at primary school or lower, and unemployed. About two-thirds had monthly income ≤1000 THB (about 28.89 USD) which was lower than the poverty line (78.83 USD/person/month) and one-half resided in a house with 4 or more members. More than half of them presented hypertension, while about one-third presented hyperlipidemia, and diabetes mellitus (Table 1).
Table 1.
Characteristics of Older Adults Participating in the IHPP-PS Program (n = 229).
| Characteristic of older adults | No. | % |
|---|---|---|
| Sex | ||
| Female | 149 | 65.1 |
| Male | 80 | 34.9 |
| Age (years) | ||
| 60 to 69 | 101 | 44.1 |
| 70 to 79 | 85 | 37.1 |
| 80 and above | 43 | 18.8 |
| Mean ± SD: 71.71 ± 7.87; Min.-Max.: 60 to 93 | ||
| Marital status | ||
| Single | 17 | 7.4 |
| Married and spouse remaining together | 136 | 59.4 |
| Separated/widowed | 76 | 33.2 |
| The highest education | ||
| Primary school or lower | 193 | 84.3 |
| High school | 28 | 12.2 |
| Diploma or higher | 8 | 3.5 |
| Religion: Buddhist | 229 | 100.0 |
| Occupation | ||
| No occupation or unemployed | 147 | 64.2 |
| Employees or daily hire | 26 | 11.4 |
| Agriculture | 25 | 10.9 |
| Trading or small business | 22 | 9.6 |
| Retirement (governmental organizations or state enterprise) | 9 | 3.9 |
| Monthly income (THB) | ||
| ≤1000 | 145 | 63.3 |
| 1001 to 3000 | 22 | 9.6 |
| ≥3001 | 62 | 27.1 |
| Mean ± SD: 3376.85 ± 5260.99; Min.-Max.; 600 to 30,000 | ||
| Family members | ||
| 1 to 3 | 112 | 48.9 |
| 4 to 6 | 103 | 45.0 |
| 7 and above | 14 | 6.1 |
| Illness | ||
| None | 81 | 35.4 |
| Diseases (multiple response) | ||
| Hypertension | 121 | 52.8 |
| Hyperlipidemia | 87 | 38.0 |
| Diabetes mellitus | 73 | 31.9 |
| Others (heart disease, stroke, emphysema, kidney failure, cancer, etc.) | 25 | 10.9 |
Physical and Mental Health of Older Adults
After implementation, most older adults were very happy, had no symptoms or very few symptoms of depression, and had ADLs in a social-bound group. While one-half of them received good family support. The mean score of happiness, ADLs, and family support after implementing IHPP-PS was significantly higher than before implementation (P = .004, P = .034, and P < .001, respectively), while the mean score of depression did not differ (P = .413) (Table 2).
Table 2.
Physical and Mental Health Among Older Adults and Analysis of the Difference in Mean Scores Compared Before and After Implementing IHPP-PS (n = 229).
| Physical and mental health | Before implementation | After implementation | P a |
|---|---|---|---|
| Happiness (10 points); Mean (SD) | 8.00 (1.38) | 8.59 (1.46) | .004* |
| Very happy; No. (%) | 156 (68.1) | 188 (82.1) | |
| Happy; No. (%) | 73 (31.9) | 10 (17.9) | |
| Depression (27 points); Mean (SD) | 3.09 (3.25) | 3.25 (2.84) | .413 |
| No or very few symptoms; No (%) | 196 (85.6) | 204 (89.1) | |
| Mild symptoms; No. (%) | 30 (13.1) | 22 (9.6) | |
| Moderate symptoms; No. (%) | 3 (1.3) | 3 (1.3) | |
| ADLs (20 points); Mean (SD) | 18.89 (3.10) | 19.14 (2.76) | .034* |
| Social-bound; No. (%) | 220 (96.1) | 222 (96.9) | |
| Home-bound; No. (%) | 5 (2.2) | 3 (1.3) | |
| Bed-bound; No. (%) | 4 (1.7) | 4 (1.7) | |
| Family support (9 points); Mean (SD) | 4.24 (1.89) | 6.15 (2.44) | <.001* |
| Good; No (%) | 0 (0.00) | 116 (50.7) | |
| Poor to moderate; No. (%) | 229 (100.0) | 113 (49.3) |
Paired t-test.
Significance at P < .05.
Health Behaviors of Older Adults
After implementing the IHPP-PS, most older adults never or rarely used tobacco and never or rarely consumed alcoholic beverages, meanwhile, approximately two-thirds had proper physical activity, and one-half consumed low-risk foods for NCDs. The proportion of older adults who exhibited improved behaviors significantly increased after implementing the IHPP-PS in terms of tobacco use (P = .035), dietary intake (P = .018), and physical activity (P < .001). Nonetheless, the proportion did not differ for alcohol consumption (P = .377) (Table 3).
Table 3.
Analysis of the Difference in Proportions of Behaviors Among Older Adults Compared Before and After Implementing IHPP-PS (n = 229).
| Behaviors | No. (%) | P a | |
|---|---|---|---|
| Before implementation | After implementation |
||
| Tobacco used | .035* | ||
| Never or rarely used | 213 (93.0) | 222 (96.9) | |
| Used regularly | 16 (7.0) | 7 (3.1) | |
| Alcohol consumption | .377 | ||
| Never or rarely consumed | 205 (89.5) | 199 (86.9) | |
| Consumed regularly | 24 (10.5) | 30 (13.1) | |
| Dietary intake | .018* | ||
| Low risk for NCDs | 109 (47.6) | 134 (58.5) | |
| Moderate to high risk for NCDs | 120 (52.4) | 95 (41.5) | |
| Physical activity | <.001* | ||
| Proper physical activity | 94 (41.0) | 151 (65.9) | |
| Improper physical activity | 135 (59.0) | 78 (34.1) | |
McNemar test.
Significance at P < .05.
Discussion
Based on major health problems of older adults, health behaviors in this research focused on health-promoting behaviors for reducing NCD risk factors; tobacco use, alcohol consumption, dietary intake, and physical activity.39,42 -46 The IHPP-SP affected to protective factors including happiness, ADLs, family support, and healthy behaviors, although it did not differ regarding depression and alcohol consumption. Unlike some developed countries, this research defined older individuals starting at 60 years according to “The Act on Older Persons B.E. 2546 (2003 A.D.)” of Thailand, which defined that “Older persons are persons who have attained the age of at least sixty years and are of Thai nationality.” 4 Although the WHO has later advised changing the definition of older person from the starting age of 60 to 65 years, the definition of older person has not yet been enforced for the reason that different countries have different definitions of the older person, both by age at birth and by society, culture, and functional markers.1 -3 For Thailand, visions and policies to improve the quality of life for older adults of relevant ministries and agencies were targeted starting at 60 years old.6,37,42,43 Although Thailand has promoted various measures for older adults under the National Plan for the Elderly since 2002, the measures implemented by the relevant organizations have not been implemented in the same direction and integration. The measures to implement the National Agenda on Aged Society were developed. The goal was for Thai older adults to be “Active Ageing: healthy, security, participation.” The key measures for improving elder and all generation quality of life included welfare and social protection, employment and income, health system, housing and public spaces, Time Bank system, and education for the young generation. In semi-urban communities, such measures are carried out by the community people and local institutions, such as volunteers for older adults, village health volunteers, elderly clubs, schools, Sub-district health-promoting hospitals, local administrative offices (municipalities and Sub-district administrative organizations), District Health Board, and so on. 47 However, ongoing operations have shown that many older adults are still exposed to various threats and require holistic and close care and support.48 -50
After implementing IHPP-SP, older adults exhibited better wellness concerning ADLs, happiness, family support, tobacco use, dietary intake, and physical activity. These may have been due to the project’s activities developed based on baseline data from quantitative and qualitative surveys at the personal, household, and community levels, as well as gathering ideas and resources using a participatory learning process from relevant organizations and key actors including government, private, and community sectors, to ensure that the activities conducted aligned with the needs and were practically feasible for the target group. Additionally, activities in the project were conducted in a holistic and integrated manner that encompassed the promotion and modifying important risk factors affecting older adults’ wellness. These activities included individual, family, and community-level covering knowledge providing, counseling, care plan monitoring, capacity building for household members, home visits, self-help group creating, and community and environment managing. The SPs were the main individuals of those implementation and provided close assistance to older adults and their families. This enabled older adults and their families to participate and engage in activities more thoroughly and continuously. Besides training on knowledge and skills for promoting the health of older adults, the SPs participated in the study visits in the successful community-based project, which helped them work more concretely and effectively. Moreover, as a result of being nominated by the community, the older adults and their families tend to trust and cooperate with the SPs’ advice. Additionally, having SPs provide advice and assistance to the older adults’ family members resulted in more support from their families to older adults, gaining better ADLs, better health behaviors, and greater happiness. Older adults who were educated, had sufficient income, had less morbidity, and were socially-bounded were more likely to engage in activities outside the home than the home-bounded people, who often relied on others when traveling and spent most of their time resting and sleeping.26,27,38,51,52
The SPs willing to support older adults and their families without compensation may be due to cultural and religious aspects. In Thailand, gratitude is an important part of Thai culture. Thais cultivate gratitude and an obligation to care for benefactors with sincere love.53,54 Moreover, SPs take on the caregiving role because of love and attachment. It constitutes a good opportunity to take care and show gratitude to benefactors and has become an accepted duty to care for older adults. Even though economic, social, and family conditions have changed in Thai society, the duty of taking care of older adults remains with the family members and community members. Furthermore, SPs think they need to care for older adults because of their personal belief in the Law of Karma. According to Buddhist influences, Thai perspectives on life highlight spiritual well-being and compassionate action for oneself and others as in the performance of a good deed. 54 Age is an incredibly important marker of one’s place in the community and pervades every aspect of daily life in Thai culture. Older people command respect whether or not, they deserve it and individuals must listen and abide by their advice, whether or not they agree with it. Thus, older people deserve to be cared for by their families. However, caring for older adults within the family faces numerous challenges and obstacles for family members, especially time constraints, emotional stress, and hands-on care. The SPs play a role in helping family members to care for older adults by providing guidance, caregiving skills, encouragement, and mental support, as well as assisting families experiencing problems and older people who live alone.
Depression and alcohol consumption did not differ between before and after implementing IHPP-PS. This might due to most of older adults in this study had no symptoms or very few symptoms of depression (score < 7) since before the project started, resulting in very little change in depression score after the project ended. In addition, more than one-half resided in an extended family, which 4 or more members living together. 55 Thai culture addresses a sense of duty and responsibility from the young towards the older adults. Accordingly, extended families living in community is generally social connected within and with surrounding communities. This might lessen the possibility of depression among the older adults.
For alcohol consumption, approximately one-tenth of older adults consumed alcoholic beverages regularly during the past year both before and after the implementation. Drinks (any kind of drinks) are part of Thai culture, and enjoying them is a way to bond with locals and experience their lifestyle. Having a drink with someone is a special way to socialize. However, the number of drinkers slightly increased after the intervention, which was likely due to the assessment of drinking considering only the frequency without the amount of drinking. Therefore, older adults who consumed small amounts of alcohol or herbal liquor were also counted as regular drinkers. Regularly consuming small amounts of alcoholic beverages or herbal liquors among older adults was a hard-to-change behavior because participants believed that “Drinking for health” helped improve blood circulation, energy, appetite, and high-quality sleep.
Due to the limited time for conducting the program activities, this study did not compare biological and clinical changes of older adults which should be evaluated in the long term. However, the findings indicated that the IHPP-SP provided potential benefits to promote the wellness of older adults, which in the long run will help prevent illness, control risk indexes, for example, blood glucose and blood pressure levels, and prevent complications. To ensure the sustainable wellness of older adults, the interventions should be strengthened including reducing local salt and restricting calorie intake for older adults at risk of NCDs and complications. Effective systems should be in place to continuously monitor, support, and incentivize the SPs’ performance. Periodic refresher training on knowledge, work strategies, and aesthetic techniques for conversing with older adults and their families should be provided to the SPs. Resources should be coordinated and mobilized from relevant sectors to support continuous operations in promoting the wellness of older adults holistically at the individual, household, and community levels.
The study encountered limitations. This research was not designed to have a comparison group, due to resource limitations and ethics, which affected the robustness of the project’s impact. Moreover, the influence of demographic and socioeconomic factors was not controlled, which may obscure the results. The relatively short implementation period may also raise questions about the sustainability and strength of operations over the long term. Although the questionnaires were checked for content validity as well as piloted, the overall happiness was assessed using a single question which may have caused older adults to have difficulty determining their score. In addition, the assessment was based on answering a questionnaire, so the results may have deviated from the real behavior of respondents.
Conclusion
After implementing the IHPP-SP, nearly all indicators of physical and mental health and healthy behaviors of older adults improved. This reflected that the IHPP-SP provided potential benefits to promote the wellness of older adults.
Acknowledgments
We would like to thank Mr. Kittipong Vubsunthear, Deputy Chief of Sung Noen District Health Office, Nakhon Ratchasima Province for coordinating multi-sectors and supporting the project implementation. The study was supported for publication by the Faculty of Public Health and Mahidol University, Bangkok, Thailand.
Footnotes
Author Contributions: TS, AP, and PP conceptualized and designed the project and article. TS, AP, PP, and NN trained supportive peers and monitored the program implementations. TS and NN collected, analyzed, and interpreted data. TS, AP, PP, and NN drafted and edited the manuscript. All authors have read and agreed to the published version of the manuscript. All authors agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This project was supported by the Thai Health Promotion Foundation (ThaiHealth).
Ethics Considerations: The study protocol was approved by the Ethics Review Committee of the Faculty of Public Health, Mahidol University (COA no. MUPH 2018-168, protocol no. 151/2018). Written informed consent was obtained from all the respondents and the study was conducted according to the Declaration of Helsinki.
ORCID iDs: Tassanee Silawan  https://orcid.org/0000-0002-2146-6403
https://orcid.org/0000-0002-2146-6403
Arpaporn Powwattana  https://orcid.org/0000-0003-3499-7809
https://orcid.org/0000-0003-3499-7809
References
- 1. World Health Organization. Ageing. 2023. Accessed March 27, 2023. https://www.who.int/health-topics/ageing
- 2. Kowal P, Dowd J. Definition of an older person. Proposed working definition of an older person in Africa for the MDS Project. World Health Organ. 2001;10(2.1):5188-9286. [Google Scholar]
- 3. Orimo H, Ito H, Suzuki T, Arki A, Hosoi T, Sawabe M. Reviewing the definition of “elderly”. Geriatr Gerontol Int. 2006;6:149-58. doi: 10.1111/j.1447-0594.2006.00341.x [DOI] [Google Scholar]
- 4. Thailand. Department of Older Persons. The act on older persons B.E. 2546 (2003 A.D.), 2003. Government Gazette. No. 120:130a. [Google Scholar]
- 5. World Bank. Caring for Thailand’s aging population. 2023. Accessed August 23, 2023. https://www.worldbank.org/en/country/thailand/publication/caringfor-thailand-s-aging-population
- 6. Knodel J, Prachuabmoh V, Chayovan N. The Changing Well-Being of Thai Elderly: An Update From the 2011 Survey of Older Persons in Thailand. HelpAge International, 2013. http://hdl.handle.net/2027.42/100344 [Google Scholar]
- 7. Britannica. Nakhon Ratchasima, Thailand. 2023. Accessed November 29, 2022. https://www.britannica.com/place/Nakhon-Ratchasima
- 8. Wikipedia. Nakhon Ratchasima province. 2022. Accessed November 29, 2022. https://en.wikipedia.org/w/index.php?title=Nakhon_Ratchasima_province&oldid=1123199580
- 9. National Statistical Office. Important statistics and indicators. 2023. Accessed September 6, 2023. https://www.nso.go.th/nsoweb/nso/statistics_and_indicators?impt_branch=300
- 10. Registration Administration Office, Department of Provincial Administration. Population statistics from the civil registration. 2023. Accessed September 6, 2023. https://stat.bora.dopa.go.th/stat/statnew/statMONTH/statmonth/#/view
- 11. Macrotrends. Thailand life expectancy 1950-2023. 2023. Accessed August 23, 2023. https://www.macrotrends.net/countries/THA/thailand/life-expectancy
- 12. World Health Organization. Ageing and health. 2023. Accessed March 27, 2023. https://www.who.int/news-room/fact-sheets/detail/ageing-and-health
- 13. National council on aging. Top 10 chronic conditions affecting older adults. 2023. Accessed August 24, 2023. https://www.ncoa.org/article/the-top-10-mostcommon-chronic-conditions-in-older-adults
- 14. Aung TNN, Moolphate S, Koyanagi Y, et al. Depression and associated factors among community-dwelling Thai older adults in northern Thailand: the relationship between history of fall and geriatric depression. Int J Environ Res Public Health. 2022;19(17):10574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Khongboon P, Kespichayawatt J. Accidental falls and associated factors among the elderly in Thailand: a national cross-sectional study in 2007, 2011, 2014 and 2017. J Health Res. 2021;36(4):767-780. [Google Scholar]
- 16. Whangmahaporn P, Simmonds P, Whangmahaporn B. Factors affecting quality of life of the elderly in Thailand. Asian Political Sci Rev. 2018;2(2):79-87. [Google Scholar]
- 17. Seangpraw K, Auttama N, Kumar R, Somrongthong R, Tonchoy P, Panta P. Stress and associated risk factors among the elderly: a cross-sectional study from rural area of Thailand. F1000Research. 2020;8:655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ethisan P, Somrongthong R, Ahmed J, Kumar R, Chapman RS. Factors related to physical activity among the elderly population in rural Thailand. J Prim Care Community Health. 2017;8(2):71-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Duong HV, Herrera LN, Moore JX, et al. National characteristics of emergency medical services responses for older adults in the United States. Prehospital Emerg Care. 2018;22(1):7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Evans CS, Platts-Mills TF, Fernandez AR, et al. Repeat emergency medical services use by older adults: analysis of a comprehensive statewide database. Ann Emerg Med. 2017;70(4):506-515.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Silawan T, Khansakorn N, Laothong U. Factors influencing perceived needs for emergency medical services among elderly patients from four provinces in Thailand. Southeast Asian J Trop Med Public Health. 2019;50(5):925-934. [Google Scholar]
- 22. Suriyanrattakorn S, Chang CL. Long-term care (LTC) policy in Thailand on the homebound and bedridden elderly happiness. Health Policy Open. 2021;2:100026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Brach JS, Simonsick EM, Kritchevsky S, Yaffe K, Newman AB. The association between physical function and lifestyle activity and exercise in the health, aging and body composition study. J Am Geriatr Soc. 2004;52(4):502-509. doi: 10.1111/j.1532-5415.2004.52154.x [DOI] [PubMed] [Google Scholar]
- 24. Asian Development Bank. Lessons from Thailand’s national community-based long-term care program for older persons. In: Aging Asia and the Pacific. 2020. Accessed February 23, 2024. https://www.adb.org/publications/thailand-long-term-care-older-persons
- 25. Prachuabmoh V. A lesson learned from community-based integrated long-term care in Thailand. Asia Pac J Soc Work Dev. 2015;25(4):213-224. doi: 10.1080/02185385.2015.1119526 [DOI] [Google Scholar]
- 26. Aroonsrimorakot S, Laiphrakpam M, Metadilogkul O, Sharma ARS. Interventions to reduce the negative impact of ageing, social isolation, and loneliness on the health and well-being of elderlies in Thailand and India. J Public Health Dev. 2022;20(2):183-195. [Google Scholar]
- 27. Aung TNN, Aung MN, Moolphate S, et al. Thai older people’s willingness (intention) to participate in a care prevention, community group exercise program: an assessment before implementing an intervention trial in Chiang Mai, northern Thailand. Int J Environ Res Public Health. 2021;18(8):4044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kasornsunt P. A transitional care model for stroke patients at Chaopraya Yommarat Hospital. Nurs J Minist Public Health. 2015;25(1):83-96. [Google Scholar]
- 29. Senasana S, Komjakraphan P, Isaramalai S. Development of the home-based skill training program for caregivers of stroke patients. J Prev Med Assoc Thail. 2017;7(2):212-222. [Google Scholar]
- 30. Phinyo K, Limtragool P, Tiamkao S, et al. Care improvement for patients with stroke through community participation. J Res Nurs-Midwifery Health Sci. 2015;35(2):93-112. [Google Scholar]
- 31. National Health Security Office. Long-term care program: Thailand’s preparation for entering an aged society. 2020. Accessed January 10, 2024. http://eng.nhso.go.th/view/1/DescriptionNews/Long-Term-Care-program-Thailands-preparation-for-entering-an-aged-society/212/EN-US
- 32. Wikipedia. Sung Noen district. 2022. Accessed November 29, 2022. https://en.wikipedia.org/w/index.php?title=Sung_Noen_district&oldid=1092541770#Geography
- 33. Ngamjarus C, Chongsuvivatwong V, McNeil E. n4Studies: Sample Size Calculation for an epidemiological study on a smart device. Siriraj Med J. 2016;68(3):160-170. [Google Scholar]
- 34. Lotrakul M, Sumrithe S, Saipanish R. Reliability and validity of the Thai version of the PHQ-9. BMC Psychiatry. 2008;8(1):46. doi: 10.1186/1471-244X-8-46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Kittisuksathit S, Tangchonlatip K, Jarassit S, Saiprasert C, Boonyatearana P, Aree W. Happinometer: The Happiness Self-Assessment. Thammada Press Co. Ltd.; 2012. Accessed June 2, 2018. https://ipsr.mahidol.ac.th/en/post_research/happinometer-the-happiness-self-assessment/ [Google Scholar]
- 36. Kongsuk T, Arunpongpaisal S, Janthong S, Prukkanone B, Sukhawaha S, Leejongpermpoon J. Criterion-related validity of the 9 questions depression rating scale revised for Thai central dialect. J Psychiatr Assoc Thail. 2018;63(4):321-334. [Google Scholar]
- 37. Department of Medical Services, Ministry of Public Health. Handbook for Screening and Evaluating the Health of the Elderly 2021, Ministry of Public Health. Najanta Creation Co. Ltd.; 2021. [Google Scholar]
- 38. Putthinoi S, Lersilp S, Chakpitak N. Performance in daily living activities of the elderly while living at home or being home-bound in a Thai suburban community. Procedia Environ Sci. 2016;36:74-77. [Google Scholar]
- 39. World Health Organization. Physical activity. 2022. Accessed November 10, 2023. https://www.who.int/news-room/fact-sheets/detail/physical-activity
- 40. Christiansen TB, Lauritsen JM. EpiData – Comprehensive Data Management and Basic Statistical Analysis System. EpiData Association; 2010. Accessed June 2, 2018. http://www.epidata.dk [Google Scholar]
- 41. PASW Statistics for Windows . SPSS Inc; 2009. [Google Scholar]
- 42. Prasartkul P, Vapattanawong P, Kanchanachitra M, et al. Situation of the Thai Elderly 2016. Printery Co. Ltd.; 2017. Accessed March 13, 2018. https://ipsr.mahidol.ac.th/en/?s=situation+of+the+thai+elderly [Google Scholar]
- 43. Prasartkul P, Vapattanawong P, Rittirong J, et al. Situation of the Thai Elderly 2017. Deuan Tula Printing House; 2019. Accessed January 14, 2024. https://ipsr.mahidol.ac.th/en/?s=situation+of+the+thai+elderly [Google Scholar]
- 44. Ayenigbara I. The role of healthy nutrition and diet in the prevention of non-communicable diseases among the aged. Geriatr Care. 2019;5:7961. doi: 10.4081/gc.2019.7961 [DOI] [Google Scholar]
- 45. Sutipan P, Intarakamhang U. Healthy lifestyle behavioral needs among the elderly with hypertension in Chiang Mai, Thailand. J Behav Sci. 2017;12(1):1–12. [Google Scholar]
- 46. Wakabayashi M, McKetin R, Banwell C, et al. Alcohol consumption patterns in Thailand and their relationship with non-communicable disease. BMC Public Health. 2015;15(1):1297. doi: 10.1186/s12889-015-2662-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Department of Older Persons, Ministry of social Development and Human security. Measures to national agenda on aged society. 2023. Accessed February 23, 2024. https://www.dop.go.th/download/knowledge/th1560926865-155_0.pdf
- 48. Damrikarnlerd L, Pothisiri W, Prasartkul P, et al. Situation of the Thai Elderly 2019. Printery Co. Ltd.; 2020. Accessed January 14, 2024. https://ipsr.mahidol.ac.th/en/?s=situation+of+the+thai+elderly [Google Scholar]
- 49. Foundation of Thai Gerontology Research and Development institute (TGRI). Situation of the Thai Older Persons 2021. Institute for Population and Social Research, Mahidol University; 2021. https://thaitgri.org/?p=40108 [Google Scholar]
- 50. Foundation of Thai Gerontology Research and Development institute (TGRI). Situation of the Thai Older Persons 2022. Institute for Population and Social Research, Mahidol University; 2022. https://thaitgri.org/?p=40218 [Google Scholar]
- 51. Somrongthong R, Wongchalee S, Ramakrishnan C, Hongthong D, Yodmai K, Wongtongkam N. Influence of socioeconomic factors on daily life activities and quality of life of Thai elderly. J Public Health Res. 2017;6:862. doi: 10.4081/jphr.2017.862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Punyakaew A, Lersilp S, Putthinoi S. Active ageing level and time use of elderly persons in a thai suburban community. Occup Ther Int. 2019;2019;e7092695. doi: 10.1155/2019/7092695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Thongprateep T. The end of life care: spiritual care. In: Thongprateep T, ed. Spirituality: A Dimension of Nursing. Pun-Siri Printing; 2005. [Google Scholar]
- 54. Thavaro S, Attakit K, Wattananukul K, Anothai S. The application guideline of gratefulness in the present Thai society. J MCU Nakhondhat. 2019;6(6):2700-2711. [Google Scholar]
- 55. Global Data Lab. Average household size. 2024. Accessed January 3, 2024. https://globaldatalab.org/areadata/table/hhsize/THA/