Abstract
Background:
To prepare for rollout of a COVID-19 vaccine in fall 2020, there was an urgent need to understand barriers to ensuring equitable access and addressing vaccine skepticism and resistance. This study aimed to understand the association between trusted sources of COVID-19 information and likelihood of vaccination during that time, focusing on lessons learned to prepare for future public health crises.
Methods:
From December 2020-March 2021, we surveyed a probability-based, cross-sectional sample of 955 patients across seven federally qualified health centers (FQHCs) serving predominantly low-income, Black and White populations in southeastern Louisiana. Vaccination likelihood was measured on a 7-point scale; “very likely to vaccinate” was defined as score=7. Trust in healthcare provider was measured with a single survey item. High trust in personal contacts, government, and media, respectively, were defined as the highest tertiles of summative scores of trust items. Weighted multivariable logistic regression estimated adjusted odds ratios (aOR) and 95% confidence intervals (CI) for being very likely to vaccinate.
Results:
Participants were 56% Black, 64% women, mean age 44.6 years; 33% were very likely to vaccinate. High trust in healthcare provider (aOR=4.14, 95% CI 2.26-7.57) and government sources (aOR=3.23, 95% CI 1.98-5.28) were associated with being very likely to vaccinate.
Conclusions:
During initial COVID-19 vaccination rollout, trust in healthcare providers and government sources of COVID-19 information was associated with likelihood to vaccinate in FQHC patients. To inform public health planning for future crises, we highlight lessons learned for translating community-relevant insights into direct action to reach those most impacted.
Keywords: COVID-19, vaccination likelihood, federally qualified health centers
Introduction
At the onset of the COVID-19 pandemic, racial disparities in COVID-19 cases and deaths emerged in Louisiana, with Black Louisianans accounting for a disproportionately high share of COVID-19 mortality.1 Even with initial mortality concentrated in Orleans Parish, where Black residents comprise 60% of the populace,2 the earliest mortality estimates were out of proportion to the Black share of the population. There was a clear and urgent need to understand factors underlying these disparities and identify preventive strategies that were responsive to community concerns and preferences. In addition, to prepare for the rollout of a COVID-19 vaccine, public health and medical professionals needed to understand the barriers they were likely to encounter to ensuring equitable access to the vaccine and addressing vaccine skepticism and resistance,3 which was widely acknowledged to be rooted in historical and contemporary mistreatment and racism against communities of color by scientists and medical professionals.4
Against this backdrop, the Community Engagement Alliance Against COVID-19 Disparities (CEAL) was funded by the National Institutes of Health to provide trustworthy, science-based information through active community engagement and outreach to those hardest-hit by the COVID-19 pandemic.5 Louisiana was one of 11 states initially funded to build upon existing partnerships with federally qualified health centers (FQHCs) and other community partners to understand and respond to community concerns about COVID-19 preventive and treatment strategies. FQHCs are health centers that qualify for federal funding and enhanced reimbursement from Medicare and Medicaid to provide comprehensive health services in a designated medically-underserved area or to a medically-underserved population.6 In 2019, Louisiana FQHCs served over 460,000 patients, two-thirds of whom were categorized as racial and/or ethnic minorities, including 57% Black.7
This study aims to understand the association between trust in sources of information about COVID-19 and likelihood to get vaccinated among predominantly low-income, Black and White patients of FQHCs in southeastern Louisiana. By studying vaccine likelihood in FQHC patients, a group with access to more affordable and convenient healthcare than the general population with similar demographics and exposures to social determinants of health, we can isolate barriers related to vaccine skepticism and resistance from those related to healthcare access.8 We also describe the motivations for and against vaccination in the sample, distinguishing individuals who are at the extremes of the spectrum of complete resistance or complete acceptance of a vaccine from those comprising the “movable middle”.9 Finally, findings are presented across race and gender subgroups with insights for tailoring messaging approaches and content to specific demographic subgroups.
Methods
Study population and sampling strategy
Survey participants were selected from patients of 19 clinics representing seven partnering FQHCs distributed across three urban COVID-19 hotspot areas (Orleans, East Baton Rouge, and Jefferson Parishes) and surrounding rural parishes in southeastern Louisiana. Prospective participants were recruited by telephone or in person. The telephone sample frame was extracted from partner organization electronic health records (EHR), listing all adult, English-speaking patients seen in the last year. A random sample of 100 patients per clinic was selected using Stata 14.2 (StataCorp, College Station, TX), with successive random samples drawn, as needed, until at least 25 patients per clinic were surveyed. For the in-person sampling frame, FQHC staff listed all adult, English-speaking patients on the clinic schedule for a particular day and attempted to recruit every patient meeting these criteria.
A total of 958 participants were recruited across the 19 clinics (median 50; range 25-201). Three observations with no response to the vaccine likelihood question were excluded, leaving an analytic sample size of 955.
Data collection
From December 2020 to March 2021, surveys were administered by trained interviewers (FQHC and study staff) either in person or over the telephone. In-person participants were also given the option to self-complete the questionnaire. Data were entered directly into REDCap (Research Electronic Data Capture) via study tablets or computers. The study was approved by the Tulane University Institutional Review Board, and the human subjects procedures were conducted in accordance with institutional guidelines; participants provided verbal informed consent.
Study measures
All survey items were taken from the CEAL Common Survey. Likelihood to vaccinate was measured on a 7-point scale ranging from 1, “not at all likely”, to 7, “very likely”, in response to the question, “How likely are you to get an approved COVID-19 vaccine when it becomes available?” To distinguish the “movable middle” from those at the extremes of vaccine likelihood, data were dichotomized to generate two separate measures: “not at all likely” to vaccinate was defined as a score of 1 on the scale; “very likely” to vaccinate was defined as a score of 7 on the scale.
Trust in sources of information about COVID-19, including healthcare providers, faith-based leaders, family/close friends, acquaintances, traditional news media, social media contacts, the U.S. government, the U.S. Coronavirus Task Force, the Louisiana state government, and local city or town government, was measured on a 3-point Likert scale. All items were dichotomized as “a great deal” (score = 1) versus “a little”, “not at all”, or “not applicable” (score = 0). “Trust in personal contacts” was calculated as the sum of dichotomized items for faith leader, family/close friends, and acquaintances (Cronbach’s alpha for this sample = 0.66). “Trust in government” and “trust in media” were calculated as the sums of dichotomized items for the U.S., Louisiana, and local governments, and the U.S. Coronavirus Task Force (Cronbach’s alpha = 0.89); and traditional news and social media (Cronbach’s alpha = 0.52), respectively. “Low trust in healthcare provider” was defined as a score of 0 for that dichotomized item. “Low trust” was defined as the lowest tertile for each summative trust score (equivalent to trusting 0 items on the media, government, and personal contacts subscales, respectively), while “high trust” was defined as the two highest tertiles.
Reasons to vaccinate were collected using the question, “Why would you get a COVID-19 vaccine?” Participants were allowed to select all responses that applied from a list and were given the option to provide “other” reasons in a free text field. The question was asked only of those who responded other than “not at all likely” to the likelihood to vaccinate question. Reasons NOT to vaccinate were collected in the same way using the question, “Why would you NOT get a COVID-19 vaccine?”, asked only of those who responded other than “very likely” to vaccinate.
Race and gender were collected via self-report. Age was estimated from month and year of birth and categorized into meaningful categories (young adulthood 18-24, moderate adulthood 25-39, older adulthood 40-64, and elderly 65+). Education and work status were collected by a single question and dichotomized as “high school education or less” versus “greater than high school education” and “working for pay” versus “not working for pay”, respectively. Healthcare access and COVID-19 testing history were measured using single yes/no items about whether the participant saw a healthcare provider in the past month and whether the participant had ever been tested for COVID-19, respectively.
Low health literacy was defined as a “sometimes”, “often”, or “always” response to the question, “How often do you need someone to help you read written information from your doctor or drug store?” Engaged in preventive behaviors was defined as having done each of the following “very often” or “all of the time” in the past 7 days: wore a face covering or mask, washed hands with soap or used hand sanitizer several times per day, stayed at least 6 feet away from other people not from household. Location was assigned based on the location of the clinic from which a participant was recruited (Orleans, Jefferson, East Baton Rouge Parishes, or surrounding rural parishes) and date of survey administration was categorized into months (December 2020-March 2021).
Weighting and statistical analysis
Survey weights were calculated as the product of design weights and non-response weights. Design weights were calculated as the inverse probability of selection from each clinic’s EHR download (with the assumption that those surveyed in clinic also appeared in the EHR download given that they are adult, active patients). Non-response weights were calculated using the logistic regression approach to weighting. A data download of all active adult patients for each clinic and including data on age, race, ethnicity, and gender was extracted from FQHC EHRs and appended with the survey sample data. The predicted probability of being in the sample (versus the larger clinic population) was obtained from logistic regression; the non-response weight was calculated as the inverse of the predicted probability.
All analyses were conducted using svy procedures in Stata 14.2, which adjust for the impact of survey weights on standard errors. All analyses accounted for clustering at the FQHC level and robust standard errors were generated. Participant characteristics are presented as weighted proportions for the whole sample. Pearson’s chi-squared tests were used to test for differences in weighted proportions for participant characteristics and trusted sources of COVID-19 information by race (limited to the subsample self-identifying as Black or White) and gender (women versus men). Separate weighted multivariable logistic regression models were used to generate adjusted odds ratios (aOR) and 95% confidence intervals (CI) for factors associated with two outcomes – “not at all likely” and “very likely” to vaccinate – both overall and in race (Black, White) and gender (women, men) subgroups. The results for the “very likely” to vaccinate model are not presented for the subgroups comprised of White respondents and men because estimates were unstable due to small cell sizes for those models. Finally, motivations for and against vaccination are presented for the subsamples of respondents who scored >1 (greater than “not at all likely”) and <7 (less than “very likely”), respectively, on the vaccine likelihood scale. Differences in weighted proportions endorsing each motivation between respondents “somewhat” vs. “very” likely (for motivations favoring vaccination) and between respondents “not at all” versus “somewhat” likely (for motivations against vaccination) were tested using Pearson’s chi-squared tests.
Results
Participant characteristics
The weighted sample was 56% Black and 41% White, with fewer than 3% made up of Asian, American Indian/Alaska Native, and multiracial participants (Table 1). Women comprised 64% of the weighted sample. Participants aged 40-64 years made up 47% of the weighted sample, followed by those aged 25-39 years (30%), aged 65 years or older (12%), and aged 18-24 years (10%). A third of the sample (32%) had education beyond high school, and 56% were working for pay. Over half of the weighted sample (57%) was drawn from rural parishes surrounding the three urban areas (Orleans Parish (6%), Jefferson Parish (13%), and Baton Rouge parishes (24%)). Finally, most of the sample was surveyed in December 2020 (48%) and January 2021 (38%) before vaccines were widely available to the public, with smaller proportions surveyed in February 2021 (9%) and March 2021 (5%).
Table 1.
Participant characteristics
| Overall (n=955) Weighted % (n) |
Race | Gender | ||||||
|---|---|---|---|---|---|---|---|---|
| Black (n=615) Weighted % (n) |
White (n=258) Weighted % (n) |
p-value | Women (n=688) Weighted % (n) |
Men (n=263) Weighted % (n) |
p-value | |||
| Race | White | 41.0% (258) | -- | -- | -- | 40.1% (182) | 41.0% (73) | 0.726 |
| Black | 56.0% (603) | 56.5% (437) | 56.5% (166) | |||||
| Asian | 1.1% (41) | 0.9% (24) | 1.3% (17) | |||||
| American Indian/Alaska Native | 0.5% (3) | 0.6% (2) | 0.4% (1) | |||||
| More than one race | 1.5% (15) | 1.8% (12) | 0.8% (2) | |||||
| Woman | 63.7% (688) | 63.5% (446) | 63.0% (185) | 0.867 | -- | -- | -- | |
| Age category | 18-24 years old | 10.3% (80) | 10.6% (45) | 9.9% (25) | 0.461 | 7.1% (56) | 14.9% (23) | 0.098 |
| 25-39 years old | 30.2% (271) | 26.6% (152) | 32.8% (80) | 35.7% (215) | 21.0% (55) | |||
| 40-64 years old | 47.2% (476) | 50.6% (332) | 44.8% (120) | 45.2% (335) | 51.3% (139) | |||
| 65+ years old | 12.2% (122) | 12.2% (84) | 12.5% (33) | 12.0% (77) | 12.9% (45) | |||
| Greater than high school education | 31.7% (337) | 28.0% (205) | 34.8% (94) | 0.401 | 34.1% (264) | 28.1% (73) | 0.377 | |
| Working for pay | 55.7% (494) | 55.5% (313) | 54.5% (138) | 0.902 | 58.1% (381) | 51.6% (112) | 0.282 | |
| Saw healthcare provider, past 12 months | 87.2% (855) | 89.0% (560) | 84.7% (223) | 0.061 | 89.6% (626) | 84.1% (226) | 0.065 | |
| Low health literacy | 12.1% (124) | 13.7% (89) | 10.7% (27) | 0.670 | 9.0% (71) | 17.8% (52) | 0.032 | |
| Engaged in preventive behaviors | 72.7% (771) | 80.1% (532) | 62.4% (174) | 0.009 | 76.7% (568) | 66.9% (201) | 0.206 | |
| Ever tested for COVID-19 | 60.2% (587) | 64.9% (385) | 54.0% (148) | 0.173 | 59.3% (421) | 61.1% (163) | 0.678 | |
| Location | Orleans parish | 5.5% (253) | 6.0% (173) | 4.9% (38) | 0.159 | 3.5% (166) | 9.0% (86) | 0.001 |
| Jefferson parish | 13.1% (174) | 13.4% (116) | 10.7% (41) | 12.1% (118) | 15.1% (56) | |||
| Baton Rouge parishes | 24.1% (101) | 33.9% (76) | 11.6% (22) | 25.5% (84) | 22.4% (17) | |||
| Rural parishes | 57.3% (427) | 46.7% (250) | 72.8% (157) | 58.8% (320) | 53.6% (104) | |||
| Month | December 2020 | 48.3% (450) | 52.9% (310) | 41.3% (89) | 0.583 | 49.5% (327) | 46.1% (122) | 0.504 |
| January 2021 | 37.8% (390) | 35.1% (243) | 44.3% (131) | 38.0% (282) | 37.8% (107) | |||
| February 2021 | 9.3% (77) | 7.9% (41) | 9.8% (26) | 8.0% (51) | 11.6% (25) | |||
| March 2021 | 4.6% (38) | 4.0% (21) | 4.7% (12) | 4.4% (28) | 4.5% (9) | |||
| Trust in healthcare provider | 71.7% (696) | 63.3% (428) | 84.0% (208) | 0.011 | 73.6% (505) | 69.6% (189) | 0.413 | |
| Trust in U.S. Coronavirus Task Force | 37.4% (378) | 39.9% (250) | 32.8% (88) | 0.490 | 39.7% (275) | 34.3% (103) | 0.143 | |
| Trust in faith leader | 35.3% (347) | 42.7% (263) | 25.5% (63) | <0.001 | 38.2% (270) | 31.0% (76) | 0.012 | |
| Trust in Louisiana state government | 34.0% (317) | 36.9% (218) | 29.0% (69) | 0.390 | 37.2% (233) | 29.2% (84) | 0.211 | |
| Trust in family/close friends | 33.7% (330) | 32.1% (214) | 34.9% (84) | 0.680 | 34.6% (238) | 33.0% (91) | 0.757 | |
| Trust in city/town government | 30.4% (297) | 32.6% (204) | 26.4% (64) | 0.487 | 33.1% (217) | 26.4% (80) | 0.342 | |
| Trust in U.S. government | 28.2% (254) | 29.6% (172) | 25.6% (58) | 0.654 | 29.9% (180) | 26.0% (74) | 0.532 | |
| Trust in news | 21.4% (223) | 23.2% (161) | 19.0% (41) | 0.670 | 24.5% (161) | 16.4% (62) | 0.158 | |
| Trust in acquaintances | 18.0% (180) | 17.8% (117) | 17.8% (47) | 0.998 | 18.2% (129) | 18.0% (51) | 0.955 | |
| Trust in social media contacts | 7.6% (81) | 9.1% (64) | 5.7% (10) | 0.412 | 9.5% (62) | 4.5% (19) | 0.054 | |
Black respondents were more likely than White respondents to indicate that they had engaged in COVID-19 preventive behaviors (80% versus 62%, p=0.009). Men were more likely than women to have low health literacy (18% versus 9%, p=0.032) and the weighted proportion of men and women differed across location, with a higher proportion of men than women from the Orleans Parish (9% versus 4%) and Jefferson Parish (15% versus 12%) and a lower proportion of men than women from Baton Rouge parishes (22% versus 26%,) and surrounding rural parishes (54% versus 59%) (p-value for gender differences across location=0.001).
Trusted sources of COVID-19 information
The most trusted source of COVID-19 information was healthcare provider (72%), followed by the U.S. Coronavirus Task Force (37%), and faith-based leader (35%) (Table 1). Of the remaining government sources, the Louisiana state government was most trusted (34%), followed by local government (30%), and then the federal government (28%). Traditional news was trusted by a higher weighted proportion of the sample (21%) than social media (8%). Family/close friends (34%) were more trusted as sources of COVID-19 information than acquaintances (18%). Black respondents were less likely than White respondents to indicate trust in health care providers (63% versus 84%, p=0.011) but more likely to indicate trust in faith-based leaders (43% versus 26%, respectively, p<0.001). Women were more likely than men to trust faith-based leaders as a source of COVID-19 information (38% versus 31%, p=0.012). Overall, the proportion of respondents with low trust in media sources, government sources, personal contacts, and healthcare providers for COVID-19 information was 77%, 53%, 52%, and 28%, respectively.
Likelihood to vaccinate
Overall, 37% of the sample indicated that they were “not at all likely” to vaccinate and 33% were “very likely” to vaccinate, leaving 30% of the sample “somewhat likely” to vaccinate. In the multivariable adjusted models (Table 2), low trust in government sources of COVID-19 information was associated with being “not at all likely” to vaccinate among the whole sample (aOR=2.69, 95% CI 1.55, 4.68) and in each race and gender subgroup (Black: aOR=2.17, 95% CI 1.30, 3.64; White: aOR=4.67, 95% CI 1.91, 11.41; Women: aOR=2.33, 95% CI 1.68, 3.24; Men: aOR=5.24, 95% CI 2.45, 11.19). Low trust in healthcare provider was associated with being “not at all likely” to vaccinate in the whole sample (aOR=1.70, 95% CI 1.07, 2.69).
Table 2.
Factors associated with “not at all likely” to vaccinate, overall and by race & gender
| Overall (n=840) aOR (95% CI) |
Black (n=596) aOR (95% CI) |
White (n=244) aOR (95% CI) |
Women (n=609) aOR (95% CI) |
Men (n=231) aOR (95% CI) |
||
|---|---|---|---|---|---|---|
| Black | 2.04 (0.84, 4.96) | -- | -- | 1.92 (0.95, 3.92) | 1.79 (0.44, 7.28) | |
| Woman | 1.22 (0.86, 1.73) | 1.27 (0.76, 2.14) | 0.95 (0.48, 1.86) | -- | -- | |
| Age category | 18-24 years old | Ref | Ref | Ref | Ref | Ref |
| 25-39 years old | 0.95 (0.3, 2.96) | 0.60* (0.39, 0.93) | 3.14 (0.59, 16.6) | 2.19 (0.4, 11.96) | 0.33 (0.01, 10.31) | |
| 40-64 years old | 0.57 (0.12, 2.67) | 0.28** (0.13, 0.59) | 2.68 (0.2, 35.91) | 1.29 (0.27, 6.12) | 0.27 (0.00, 17.95) | |
| 65+ years old | 0.27* (0.09, 0.83) | 0.16** (0.05, 0.53) | 0.63 (0.04, 10.63) | 0.59 (0.06, 6.37) | 0.13 (0, 22.41) | |
| Greater than high school education | 1.39 (0.78, 2.46) | 1.60 (0.53, 4.78) | 1.3 (0.50, 3.4) | 1.22 (0.61, 2.47) | 1.79 (0.29, 11.05) | |
| Working for pay | 0.89 (0.37, 2.15) | 0.91 (0.27, 3.05) | 0.83 (0.43, 1.61) | 1.34 (0.89, 2.02) | 0.34 (0.06, 2.13) | |
| Saw healthcare provider, past 12 months | 1.77 (0.63, 4.93) | 1.48 (0.52, 4.24) | 2.67* (1.28, 5.58) | 1.90 (0.45, 7.96) | 1.81 (0.47, 7.02) | |
| Low health literacy | 1.19 (0.47, 3.02) | 1.57 (0.55, 4.52) | 0.46 (0.14, 1.47) | 1.73 (0.97, 3.1) | 0.60 (0.13, 2.8) | |
| Engaged in preventive behaviors | 0.64** (0.49, 0.83) | 0.76 (0.46, 1.25) | 0.53 (0.26, 1.07) | 0.86 (0.45, 1.63) | 0.43 (0.16, 1.15) | |
| Ever tested for COVID-19 | 0.53* (0.3, 0.94) | 0.72 (0.37, 1.37) | 0.41* (0.19, 0.88) | 0.48* (0.28, 0.82) | 0.66 (0.34, 1.29) | |
| Location | Orleans parish | Ref | Ref | Ref | Ref | Ref |
| Jefferson parish | 1.99*** (1.52, 2.61) | 1.80 (0.95, 3.44) | 1.49 (0.52, 4.24) | 3.69** (2.03, 6.71) | 0.58 (0.17, 1.93) | |
| Baton Rouge parishes | 1.9** (1.36, 2.67) | 2.22** (1.32, 3.74) | 0.17 (0.01, 3.78) | 2.90** (1.51, 5.56) | 0.59 (0.15, 2.28) | |
| Rural parishes | 2.84** (1.85, 4.36) | 2.56 (0.99, 6.59) | 1.97 (0.57, 6.75) | 5.02** (2.35, 10.73) | 0.82 (0.24, 2.82) | |
| Month | December 2020 | Ref | Ref | Ref | Ref | Ref |
| January 2021 | 0.85 (0.56, 1.30) | 0.99 (0.45, 2.19) | 0.88 (0.37, 2.12) | 0.72 (0.33, 1.57) | 1.00 (0.28, 3.58) | |
| February 2021 | 0.73* (0.55, 0.97) | 0.78 (0.36, 1.66) | 0.57 (0.09, 3.56) | 1.15 (0.86, 1.53) | 0.24 (0.05, 1.13) | |
| March 2021 | 0.49 (0.22, 1.05) | 0.34** (0.17, 0.69) | 1.05 (0.33, 3.31) | 0.32*** (0.27, 0.37) | 1.03 (0.14, 7.36) | |
| Low trust in healthcare provider | 1.70* (1.07, 2.69) | 1.67 (0.94, 2.97) | 1.93 (0.86, 4.34) | 1.44 (0.68, 3.08) | 1.72 (0.53, 5.59) | |
| Low trust in personal contacts | 1.44 (0.87, 2.38) | 1.95 (0.97, 3.92) | 0.96 (0.28, 3.3) | 1.5 (0.78, 2.88) | 1.56 (0.72, 3.42) | |
| Low trust in government | 2.69** (1.55, 4.68) | 2.17* (1.30, 3.64) | 4.67** (1.91, 11.41) | 2.33*** (1.68, 3.24) | 5.24** (2.45, 11.19) | |
| Low trust in media | 1.54 (0.72, 3.29) | 1.4 (0.69, 2.85) | 1.18 (0.62, 2.26) | 1.62 (0.79, 3.35) | 1.60 (0.46, 5.57) | |
aOR – adjusted odds ratio; CI – confidence interval
Multivariable models include all variables listed in the table
Both high trust in healthcare provider and in government sources of COVID-19 information were associated with being “very likely to vaccinate” overall (aOR=4.14, 95% CI 2.26, 7.57; aOR=3.23, 95% CI 1.98, 5.28, respectively) and among Black respondents (aOR=3.29, 95% CI 2.32, 4.66; aOR=2.58, 95% CI 1.95, 3.41, respectively) and men (aOR=3.41, 95% CI 1.74, 6.67; aOR=2.10, 95% CI 1.24, 3.55, respectively) (Table 3).
Table 3.
Factors associated with “very likely” to vaccinate, overall and by race & gender1
| Overall (n=840) aOR (95% CI) |
Black (n=596) aOR (95% CI) |
Women (n=609) aOR (95% CI) |
||
|---|---|---|---|---|
| Black | 0.60 (0.24, 1.52) | -- | 0.72 (0.31, 1.67) | |
| Woman | 0.70 (0.47, 1.05) | 0.99 (0.43, 2.31) | -- | |
| Age category | 18-24 years old | Ref | Ref | Ref |
| 25-39 years old | 1.79 (0.98, 3.26) | 0.94 (0.29, 3.04) | 0.98 (0.29, 3.33) | |
| 40-64 years old | 3.75** (1.59, 8.88) | 2.07 (0.96, 4.45) | 2.56 (0.87, 7.49) | |
| 65+ years old | 9.18** (2.63, 32.08) | 2.93 (0.78, 11.04) | 7.25* (1.87, 28.21) | |
| Greater than high school education | 0.96 (0.48, 1.95) | 0.84 (0.32, 2.16) | 0.76 (0.27, 2.12) | |
| Working for pay | 1.18 (0.53, 2.63) | 0.86 (0.26, 2.86) | 1.64 (0.78, 3.46) | |
| Saw healthcare provider, past 12 months | 1.14 (0.30, 4.29) | 2.02 (0.57, 7.19) | 1.09 (0.4, 2.97) | |
| Low health literacy | 0.60 (0.26, 1.38) | 0.86 (0.48, 1.55) | 0.44 (0.17, 1.17) | |
| Engaged in preventive behaviors | 1.27 (0.86, 1.88) | 0.91 (0.57, 1.45) | 1.15 (0.69, 1.91) | |
| Ever tested for COVID-19 | 1.10 (0.55, 2.23) | 1.07 (0.44, 2.57) | 1.13 (0.63, 2.03) | |
| Location | Orleans parish | Ref | Ref | Ref |
| Jefferson parish | 0.52* (0.30, 0.90) | 0.47 (0.14, 1.60) | 0.58** (0.41, 0.82) | |
| Baton Rouge parishes | 1.06 (0.79, 1.42) | 0.55 (0.16, 1.87) | 1.26* (1.01, 1.57) | |
| Rural parishes | 0.32* (0.14, 0.74) | 0.46 (0.11, 1.93) | 0.36** (0.19, 0.70) | |
| Month | December 2020 | Ref | Ref | Ref |
| January 2021 | 1.51* (1.08, 2.13) | 1.45 (0.65, 3.25) | 1.95*** (1.49, 2.55) | |
| February 2021 | 2.12* (1.14, 3.96) | 1.31 (0.25, 6.99) | 2.88*** (2.12, 3.92) | |
| March 2021 | 3.58** (1.88, 6.80) | 3.26*** (2.07, 5.14) | 7.05*** (3.96, 12.56) | |
| High trust in healthcare provider | 4.14** (2.26, 7.57) | 3.29*** (2.32, 4.66) | 3.41** (1.74, 6.67) | |
| High trust in personal contacts | 1.12 (0.64, 1.96) | 1.04 (0.68, 1.57) | 0.97 (0.45, 2.13) | |
| High trust in government | 3.23** (1.98, 5.28) | 2.58*** (1.95, 3.41) | 2.10* (1.24, 3.55) | |
| High trust in media | 2.10 (1.03, 4.30) | 2.22 (1.09, 4.54) | 1.98 (0.44, 8.99) | |
The results for the subgroups comprised of White respondents and men are not presented; estimates were unstable due to small cell sizes for those models
aOR – adjusted odds ratio; CI – confidence interval
Multivariable models include all variables listed in the table
Motivations for and against vaccination
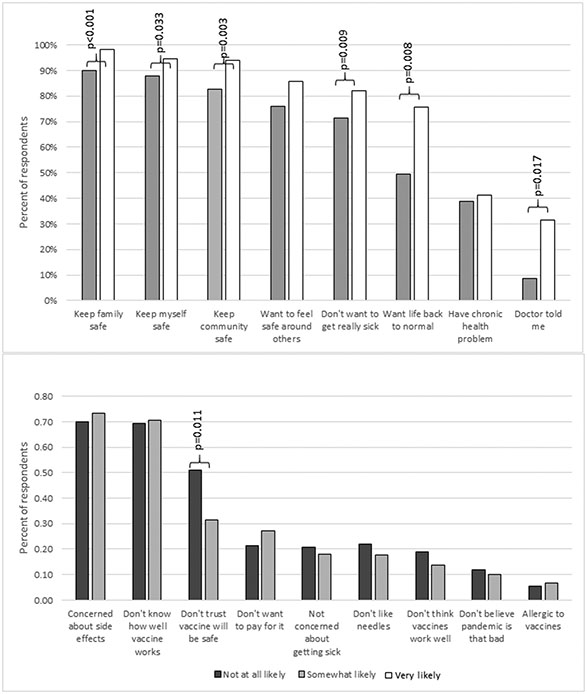
Among respondents somewhat or very likely to vaccinate, the most common reasons for vaccination included wanting to keep family (94%), self (91%), and community (88%) safe (Figure 1, top panel). Motivations that differed between those who were “somewhat” versus “very likely” to vaccinate included wanting to keep family safe (90% versus 98%, respectively; p<0.001), wanting to keep self safe (88% versus 95%, respectively; p=0.033), wanting to keep community safe (83% versus 94%, respectively; p=0.003), not wanting to get really sick (71% versus 82%, respectively; p=0.009), wanting life to get back to normal (50% versus 76%, respectively; p=0.008), and “because a doctor told me to” (9% versus 32%, respectively; p=0.017).
Figure 1.
Reasons to Vaccinate (top panel) and Not to Vaccinate (bottom panel) by Likelihood to Vaccinate among patients in federally qualified health centers, southeast Louisiana, December 2020-March 2021
Top panel: Percent of respondents endorsing each reason FOR vaccination; survey respondents who were “not at all likely” to vaccinate were not asked to respond to this item; p-values <0.05 reported from Pearson’s chi-squared test of difference between respondents “somewhat” versus “very” likely to vaccinate for each reason.
Bottom panel: Percent of respondents endorsing each reason NOT to vaccinate; survey respondents who were “very likely” to vaccinate were not asked to respond to this item; p-values <0.05 reported from Pearson’s chi-squared test of difference between respondents “somewhat” versus “not at all” likely to vaccinate for each reason.
Among respondents not at all or only somewhat likely to vaccinate, the most common reasons not to vaccinate included concerns about side effects (71%), not knowing how well the vaccine works (70%), and not trusting that the vaccine will be safe (42%) (Figure 1, bottom panel). Those who were not at all likely to vaccinate were more likely than those somewhat likely to vaccinate to indicate “not trusting that the vaccine will be safe” as a motivation against vaccination (51% versus 32%, respectively; p=0.011).
Differences in motivations for and against vaccination by likelihood to vaccinate in race and gender subgroups are presented in Supplemental Tables S1 and S2.
Discussion
In late 2020, in light of Black versus White racial disparities in COVID-19 outcomes among Louisianans, and in anticipation of vaccine access barriers and resistance to uptake of the forthcoming COVID-19 vaccine, this study aimed to understand the association between trust in sources of information about COVID-19 and likelihood to get vaccinated. These data, combined with additional insights around motivations for and against vaccination and race and gender differences, would help the Louisiana CEAL (LA-CEAL) to identify the optimal messengers and most appropriate messages to reach the populations most impacted by COVID-19.
Trust is a key issue in much of the literature on COVID-19 vaccine acceptance and uptake, with high variability across studies in how it is operationalized.10 Existing literature examines generalized trust,11,12 medical trust,13,14 governmental trust,15,16 trust in the vaccine development and approval process,11,16,17 trust in vaccine safety and efficacy,11 general trust in vaccines,18 trust in scientists,19 trust in “authorities”,20 and trust in healthcare provider,11 all of which may affect vaccine acceptance.10 Fewer studies have examined associations between trust in sources of information and vaccine acceptance,3,11 which may provide insights that are relevant for community-engaged action.
Among this sample of predominantly low-income, Black and White patients of FQHCs in southeastern Louisiana, healthcare providers were the most trusted source of COVID-19 information, overall and across all demographic subgroups. This finding is highly consistent with published results from around the world.16,21,22 Counter to findings from a study among patients of a safety net health system in Louisiana,22 trust in healthcare providers among White respondents in our sample exceeded that among Black respondents. The reverse trend was identified with respect to trust in faith-based leaders, suggesting that faith-based leaders may have a special role in reaching Black communities.4 Trust in healthcare providers and government sources of COVID-19 information had the strongest and most consistent effects on vaccine likelihood. While we did not find an association between trust in media and vaccine likelihood, other studies examining exposure to various types of news sources have found an association.19 Identifying individuals with low trust in healthcare providers or government sources of information could help to distinguish groups that may require timely and accurate messaging from alternative sources in order to increase vaccine uptake.
Many COVID-19 vaccine promotion efforts have focused on nudging the “movable middle” toward vaccine uptake.9 Our findings regarding motivations for and against vaccination provide insights around what distinguishes the movable middle (those “somewhat likely” to vaccinate) from those at the extremes of the vaccine likelihood continuum. While keeping family, self, and community safe were the most common messages favoring vaccination, levels of endorsement also differed between the movable middle and those very likely to vaccinate. “Because a doctor told me to” was the least endorsed motivation favoring vaccination, likely due to the fact that a majority of survey responses were collected before a vaccine was widely available (indeed, in a study conducted among patients of a safety-net health system in Louisiana after vaccine rollout, over 80% of respondents indicated a doctor had discussed the vaccine with them).22 However, endorsement of that motivation distinguished the movable middle from those very likely to vaccinate, suggesting advice to vaccinate from a medical professional may be an effective strategy to inform patient decision-making supporting vaccination. Our finding that vaccine safety, effectiveness, and side effects were the most common concerns about vaccination aligns with other studies.14,20,22,23
Strengths and limitations
This study has several strengths, including a large sample of diverse patients (allowing comparisons between Black and White, men and women) from FQHCs from both urban and rural areas in southeast Louisiana, a population with high exposure to detrimental social determinants of health and therefore higher risk for poor health outcomes related to COVID-19. The restriction of our sample to active patients in FQHCs minimizes confounding effects of healthcare access. The use of probability-based sampling and weighting techniques minimizes non-response bias, ensuring that results are representative of FQHC patients across the clinics included in the study.
The results of this analysis should be considered in the context of study limitations. The sample was restricted to English-speaking, adult, active patients of partnering FQHCs in the southeast region of Louisiana; results may not be generalizable to other populations. The rollout of COVID-19 vaccines in the middle of data collection may have impacted survey responses related to vaccine likelihood, trust in sources of information, and motivations for and against vaccination; however, a majority of the data were collected prior to widespread public availability and uptake of the vaccine, and we controlled for month of survey completion in the multivariable models. Finally, due to small cell sizes in the very likely to vaccinate models for the subgroups comprised of White respondents and men, those estimates could not be presented. Further research with larger subgroup samples is needed to understand factors associated with being very likely to vaccinate in these groups.
Informing public health planning for future crises
This work may serve as a blueprint in future public health crises for translating insights from community-engaged research into direct action. In response to findings related to trusted sources of COVID-19 information, LA-CEAL positioned healthcare providers and faith-based leaders as “trusted messengers”, engaging them to serve on our Speakers Bureau and make appearances on traditional and social media and other forums (e.g., Town Halls) to deliver timely and accurate COVID-19 information. In addition, LA-CEAL has used lunch-and-learn sessions to equip FQHC providers and staff with information, skills, and resources to engage patients in COVID-19 conversations. In light of research suggesting that vaccine hesitancy and concerns among healthcare workers may mirror that of the general population,17 future research is needed to understand the barriers trusted messengers themselves face with respect to their role, and strategies for building their capacity in the context of high levels of healthcare worker turnover and burnout. LA-CEAL programming was also responsive to findings related to vaccine motivations – a March 2021 paid and earned media campaign designed by the LA-CEAL team centered on messages about getting vaccinated for safety of “my family”, “my community”, and “myself.” Finally, in response to the most common motivations against COVID-19 vaccination endorsed by our survey respondents, all LA-CEAL vaccine education efforts addressed concerns about side effects, effectiveness, and vaccine safety. In these ways, LA-CEAL translated community-relevant insights from this community-engaged research into direct public health impact, addressing key barriers and employing the most promising strategies for reaching those most impacted by COVID-19 with up-to-date and timely information to inform health decisions.
Supplementary Material
Acknowledgements
We are grateful to the following individuals for their contributions to the LA-CEAL survey effort: Tulane University – Ariela Bass, Haley Gomes, Taylor Johnson, Celeste Levy, Emily Maranets, James Marsh, Alexandra McNally, Divya Polu, Julia Silver, Kaitlynn Winder; Access Health Louisiana – Sydney Soublet; CareSouth Medical & Dental – Sheneka Dunn, Stephanie Harold, Dominique Landry; InclusivCare – Dwana Green, Keyra Harrison, Ramesh Prabhu; NOELA – Jose Flores, Graciela Grande, Jennifer Hoang, Diem Pham; RKM Primary Care – Lakerria Griffin, Gloria Harris, Christi Hunt, Arianna Smith, Tammy Spangler, Kari Vicknair, Nichole Whetstone, Brenda Wilson; Southeast Community Health Systems – Nanette Bester, Ashley Clement, Gail Dunn, Sylvia H. Gordon, Rosa Locascio, Debra Stampley; Teche Action Clinic – Shenik Barkey, Lashawn Druilhet, Brittany Millien
Funding Source:
Research reported in this NIH Community Engagement Alliance (CEAL) Against COVID-19 Disparities publication was supported by the National Institutes of Health under Award Number OT2 HL158287. The authors also receive funding from the National Institute of General Medical Sciences of the National Institutes of Health, which funds the Louisiana Clinical and Translational Sciences Center (U54 GM10490; Krousel- Arnold, Wood, Davis, Sarpong, Williams), and from U54 TR001368 (Krousel-Wood), R33 AG068481 (Krousel-Wood, Peacock), R01 HL133790 (Krousel-Wood, Peacock), and K12 AR084224 (Krousel-Wood, Peacock). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflicts of Interest: Nothing to disclose
REFERENCES
- 1.Hu G, Hamovit N, Croft K, et al. Assessing inequities underlying racial disparities of COVID-19 mortality in Louisiana parishes. Proc Natl Acad Sci U S A. 2022;119(27):e2123533119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.United States Census Bureau. Quick Facts, Orleans Parish. https://www.census.gov/quickfacts/orleansparishlouisiana. Accessed 1/22/23. [Google Scholar]
- 3.Malik AA, McFadden SM, Elharake J, et al. Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine. 2020;26:100495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Privor-Dumm L, King T. Community-based Strategies to Engage Pastors Can Help Address Vaccine Hesitancy and Health Disparities in Black Communities. J Health Commun. 2020;25(10):827–830. [DOI] [PubMed] [Google Scholar]
- 5.National Institutes of Health. About CEAL. https://covid19community.nih.gov/about. Accessed January 9, 2023.
- 6.Medicare Learning Network. Federally Qualified Health Center (MLN006397), October 2022. Centers for Medicare and Medicaid. https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/Downloads/fqhcfactsheet.pdf. Accessed January 9, 2023. [Google Scholar]
- 7.Health Resources & Services Administration. Louisiana Aggregated Health Center Data. https://data.hrsa.gov/tools/data-reporting/program-data. Accessed January 9, 2023.
- 8.Nguyen LH, Joshi AD, Drew DA, et al. Racial and ethnic differences in COVID-19 vaccine hesitancy and uptake. MedRxiv. 2021. [Google Scholar]
- 9.Barsade J, Exactor FC, Mellon GCC, et al. COVID-19 Vaccination Uptake, Behavioral Science Task Force Final Report. 2021. [Google Scholar]
- 10.Sapienza A, Falcone R. The Role of Trust in COVID-19 Vaccine Acceptance: Considerations from a Systematic Review. International Journal of Environmental Research and Public Health. 2022;20(1):665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Szilagyi PG, Thomas K, Shah MD, et al. The role of trust in the likelihood of receiving a COVID-19 vaccine: Results from a national survey. Preventive medicine. 2021;153:106727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Eisnecker PS, Kroh M, Kühne S. The role of generalized trust in COVID-19 vaccine acceptance. PloS one. 2022;17(12):e0278854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thompson HS, Manning M, Mitchell J, et al. Factors associated with racial/ethnic group–based medical mistrust and perspectives on COVID-19 vaccine trial participation and vaccine uptake in the US. JAMA Network Open. 2021;4(5):e2111629–e2111629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Khubchandani J, Macias Y. COVID-19 vaccination hesitancy in Hispanics and African-Americans: A review and recommendations for practice. Brain, behavior, & immunity-health. 2021;15:100277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Morales DX, Beltran TF, Morales SA. Gender, socioeconomic status, and COVID-19 vaccine hesitancy in the US: An intersectionality approach. Sociology of Health & Illness. 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Plunk A, Sheehan B, Orr S, et al. Stemming the tide of distrust: A mixed-methods study of vaccine hesitancy. Journal of Clinical and Translational Science. 2022;6(1):e128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Caiazzo V, Stimpfel AW. ‘Vaccine Hesitancy in American Healthcare Workers During the COVID-19 Vaccine Roll Out: An Integrative Review. Public Health. 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Willis DE, Andersen JA, Bryant-Moore K, et al. COVID-19 vaccine hesitancy: Race/ethnicity, trust, and fear. Clinical and translational science. 2021;14(6):2200–2207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Viswanath K, Bekalu M, Dhawan D, et al. Individual and social determinants of COVID-19 vaccine uptake. BMC Public Health. 2021;21(1):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Joshi A, Kaur M, Kaur R, et al. Predictors of COVID-19 vaccine acceptance, intention, and hesitancy: a scoping review. Frontiers in public health. 2021;9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Solís Arce JS, Warren SS, Meriggi NF, et al. COVID-19 vaccine acceptance and hesitancy in low- and middle-income countries. Nat Med. 2021;27(8):1385–1394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Davis TC, Beyl R, Bhuiyan MA, et al. COVID-19 concerns, vaccine acceptance and trusted sources of information among patients cared for in a safety-net health system. Vaccines. 2022;10(6):928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Troiano G, Nardi A. Vaccine hesitancy in the era of COVID-19. Public health. 2021;194:245–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.