Abstract
Background
Current guidelines include an algorithm for predicting choledocholithiasis. Presence of any very strong predictor or both strong predictors confers a high (>50%) probability of choledocholithiasis. Absence of predictors confers low risk (<10%) of choledocholithiasis. Other combinations have an intermediate risk of choledocholithiasis.
Aim
Determine accuracy of the proposed algorithm in predicting choledocholithiasis.
Methods
Retrospective analysis of all endoscopic retrograde cholangiopancreatographies performed for suspected choledocholithiasis in 3 years in a Tertiary care hospital and a community hospital serviced by The University of Texas Health Science Center at Houston Division of Gastroenterology. Application of the guidelines, and comparing results to endoscopic retrograde cholangiopancreatography findings.
Results
A total of 1080 endoscopic retrograde cholangiopancreatographies were performed; 521 for choledocholithiasis. Most patients were Hispanic and female. Univariate analysis: presence of any very strong predictor and both strong predictors had an OR for choledocholithiasis of 3.30 and 2.36 respectively. Multivariate analysis: odds of choledocholithiasis with any very strong predictor was 2.87, and both strong predictors 3.24. Choledocholithiasis was present in 71.5%, and 41% of patients with high, and intermediate risk respectively.
Conclusion
This study confirms the utility of clinical predictors for the diagnosis of choledocholithiasis. All of the very strong predictors and one of the strong predictors increased the odds of choledocholithiasis. Patients with high risk for choledocholithiasis had a probability of 79% of choledocholithiasis. Sensitivity and specificity of current predictors are too low to obviate the possible need of non-invasive tests to confirm or exclude choledocholithiasis in all risk groups.
Keywords: Choledocholithiasis, Clinical predictors, Endoscopic retrograde, cholangiopancreatography
1. Introduction
Gallstone disease affects approximately 20 million Americans per year with an overall cost greater than $6 billion dollars [1]. Epidemiologic and clinical studies have reported that cholesterol gallstones occur infrequently in childhood and adolescence, and the prevalence of cholesterol gallstones increases linearly with age in both genders and approaches 50% at age 70 in women [2,3]. Choledocholithiasis occurs in 15% of patients with cholelithiasis, 5–10% of patients undergoing laparoscopic cholecystectomy for symptomatic cholelithiasis and up to 33% of patients with acute biliary pancreatitis [4–7]. Stones in the common bile duct (CBD) are more likely to cause complications due to obstruction such as cholecystitis, cholangitis and pancreatitis. Management options for choledocholithiasis include invasive procedures like endoscopic retrograde cholangiopancreatography (ERCP), surgery with bile duct exploration and percutaneous transhepatic drainage. Liver biochemical tests and/or transabdominal ultrasound (US) lack good accuracy to predict choledocholithiasis when used as a single test. Recently ASGE proposed risk stratification scheme based on the clinical parameters, biochemical testing and imaging studies and proposed a management algorithm for evaluation and management of suspected choledocholithiasis.
According to the present American Society of Gastrointestinal Endoscopy (ASGE) guidelines the presence of a single strong predictor (CBD stone on abdominal ultrasound (US), clinical ascending cholangitis or total bilirubin > 4 mg/dL) or the presence of both strong predictors (dilated CBD on ultrasound > 6 mm with gallbladder in situ and total bilirubin between 1.8 and 4 mg/dL) confer a high (>50%) probability of choledocholithiasis. Based on this probability a management algorithm has been suggested for patients with symptomatic cholelithiasis [8]. The aim of the present study was to assess the validity and accuracy of the current ASGE guidelines on choledocholithiasis in a large cohort of patients.
2. Patients and methods
2.1. Patients
We conducted a retrospective analysis of all ERCPs performed between September 2007 and September 2010 at The University of Texas Health Science Center at Houston. All ERCPs were performed at a tertiary care hospital and a community hospital serviced by The University of Texas Health Science Center at Houston Division of Gastroenterology, Hepatology and Nutrition. All procedures were performed by 2 endoscopists (DSW and FJL). Both endoscopists had performed more than 500 ERCPs prior to beginning of study period. The study protocol was approved by the Institution review board of The University of Texas Health Science Center at Houston. By retrospective chart review, we created a database that included variables such as clinical presentation, biochemical tests, imaging study results, diagnostic and therapeutic interventions, short term and long term complications and outcomes.
2.2. Variable definitions
CBD stone on US was the presence of a hyperechoic lesion with posterior shadowing in the common bile duct described on ultrasonography by the staff radiologist. Ascending cholangitis was defined as the presence of fever, jaundice and right upper quadrant abdominal pain. Gallstone pancreatitis was defined as absence alcohol induced pancreatitis (consumption of alcohol intake 7 days prior to the admission based on clinical history) and the presence of gallstones or sludge within the gallbladder, abdominal pain in the epigastric and/or right upper quadrant areas, and elevated lipase 3 times the upper limit of normal for the institutions reference test. Abnormal liver function tests (LFT) other than bilirubin were defined as elevated laboratory values for parameters such as alanine aminotransferase (ALT), aspartate aminotransferase (AST), and alkaline phosphatase based on institution’s reference test. Prior history of LFT elevation and/or history of liver disease was not taken into consideration as part of the present study. Choledocholithiasis was defined as the presence of stones or stone material at the time of ERCP and balloon sweep.
ERCP Technique: Olympus duodenoscopes (TJF-160 and GIFH180) were utilized in one institution, while Pentax doudenoscopes (ED-3670TK and ED-3490TK) were used in the second institution. The duodenoscope was inserted to the second portion of the duodenum. Deep biliary cannulation was achieved with a preloaded papillotome. Cholangiogram was obtained; filling defects and bile duct anatomy and size assessed. Biliary sphincterotomy was carried out based on the clinical decision of the endoscopist, followed by bile duct sweeping using the stone extractor balloon. Finally, occlusion cholangiogram was performed.
Data collection was performed after the original presentation. All patients who underwent ERCPs for suspected or confirmed choledocholithiasis were included in the study. Patients diagnosed with choledocholithiasis at the time of cholecystectomy via intraoperative cholangiograms were also included in the analysis; the information collected was the clinical data prior to cholecystectomy. Exclusion criteria included ERCP for reasons other than suspected choledocholithiasis, incomplete data and cholecystectomy performed at a time other than the current admission.
After patient inclusion we applied the guideline’s predictors to all patients. The presence of all of the predictors of choledocholithiasis suggested by the ASGE choledocholithiasis guidelines were documented and tabulated. Patients were then classified as high, intermediate or low risk for choledocholithiasis based on established guidelines.
The results were compared to ERCP results: presence or absence of choledocholithiasis.
2.3. Statistical analysis
All available data was represented as frequencies (percentages), and stratified based on the presence or absence of a CBD stone on ERCP. Logistic regression was used to derive bivariate and multivariate odds ratios. The presence or absence of a CBD stone on ERCP was treated as a dependent variable. In separate models, we evaluated the bivariate and multivariate odds of predicting CBD stone on ERCP, first using the individual clinical predictors, and then ASGE guidelines-based grouping of high-risk and intermediate risk categories. Furthermore, sensitivity, specificity, positive predictive value (PPV), negative predictive values (NPV), and probabilities were derived. Independent variables were included in the multivariate models if they were significant (p < 0.05) on bivariate analysis. Hosmer and Lemeshow goodness of fit tests were done to evaluate the quality of model fit. A p-value < 0.05 was considered statistically significant for all analyses. Data was analysed using SAS software version 9.2 (SAS Institute Inc, Cary, North Carolina).
3. Results
In the 3 year study period, a total of 1080 ERCP’s were performed. Of the 1080, 521 ERCPs were performed for suspected choledocholithiasis. In 293 of the 521 (56%) ERCPs, choledocholithiasis was present; while 228 of the 521 (44%) did not have common bile duct stones (Fig. 1). The majority of patients were female (78%) and Hispanic (74%). Baseline characteristics of the study populations are shown in detail in Table 1.
Fig. 1.
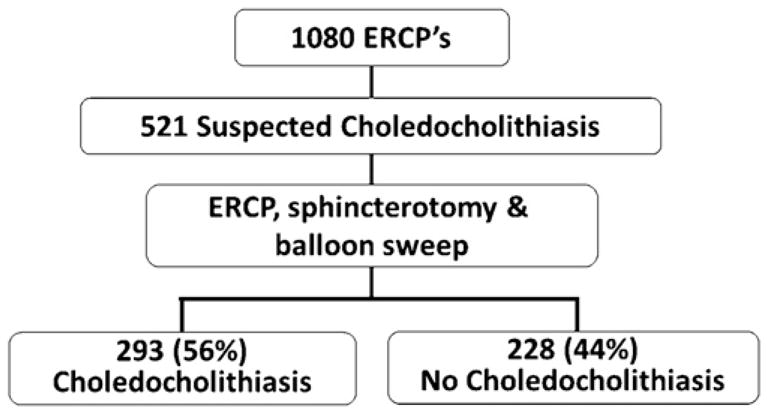
Number of endoscopic retrograde cholangiopancreatographies performed for suspected choledocholithiasis; including number and percentage of patients with choledocholithiasis. ERCP, endoscopic retrograde cholangiopancreatography.
Table 1.
Baseline characteristics of the study population.
| Variable | Total N = 521 (%) | Choledocholithiasis on ERCP N = 293 (%) | No choledocholithiasis on ERCP N = 228 (%) | p value |
|---|---|---|---|---|
| Gender, female | 409 (78) | 236 (80) | 173 (76) | 0.20 |
| Race, Hispanic | 388 (74) | 215 (73) | 173 (76) | 0.81 |
| Very strong predictors | ||||
| Total bilirubin > 4 mg/dL | 167 (32) | 120 (41) | 47 (21) | <0.001 |
| Common bile duct stone on ultrasound | 43 (8) | 38 (13) | 5 (2) | <0.001 |
| Clinical ascending cholangitis | 23 (4) | 19 (7) | 4 (2) | <0.01 |
| Strong predictors | ||||
| Total bilirubin, 1.8–4.0 mg/dL | 172 (33) | 93 (32) | 79 (35) | 0.48 |
| Dilated common bile duct on ultrasound | 260 (50) | 171 (59) | 89 (39) | <0.001 |
| Moderate predictors | ||||
| Abnormal liver function tests | 499 (95) | 286 (98) | 213 (93) | 0.02 |
| Age > 55 years | 86 (16) | 54 (19) | 32 (14) | 0.18 |
| Gallstone pancreatitis | 134 (26) | 64 (22) | 70 (31) | 0.02 |
| Very strong predictors | <0.001 | |||
| None | 316 (61) | 143 (49) | 173 (76) | |
| One | 177 (34) | 125 (43) | 52 (23) | |
| Two | 27 (5) | 24 (8) | 3 (1) | |
| Three | 1 (0.2) | 1 (0.3) | (0) | |
| Strong predictors | <0.01 | |||
| None | 158 (30) | 75 (26) | 83 (37) | |
| One | 294 (56) | 171 (58) | 123 (54) | |
| Two | 69 (13) | 47 (16) | 22 (10) | |
| Moderate predictors | 0.33 | |||
| None | 18 (3) | 7 (2) | 11 (5) | |
| One | 323 (62) | 189 (65) | 134 (59) | |
| Two | 154 (30) | 82 (28) | 72 (32) | |
| Three | 26 (5) | 15 (5) | 11 (5) | |
| High probability | 264 (51) | 189 (65) | 75 (33) | <0.001 |
| Intermediate probability | 249 (48) | 102 (35) | 147 (65) | <0.001 |
| Low probability | 8 (2) | 2 (1) | 6 (3) | 0.07 |
ERCP, endoscopic retrograde cholangiopancreatography; CBD, common bile duct; US, ultrasound; LFT, liver function test.
3.1. Sensitivities and specificities for predictors
Sensitivity, specificity, positive predictive values (PPV) and negative predictive values were calculated for each individual predictor.
Overall, the very strong predictors had high specificities and low sensitivity. The highest specificity (98%) was observed with the presence of CBD stone on US and clinical ascending cholangitis, but the corresponding sensitivity was extremely low. The PPV and NPV for all of the very strong predictors performed poorly (Table 2).
Table 2.
Predictors of cholelithiasis: sensitivity, specificity, NPV and PPV.
| Sensitivity | Specificity | PPV | NPV | |
|---|---|---|---|---|
| Very strong predictors | ||||
| Common bile duct stone on ultrasound | 13 | 98 | 88 | 47 |
| Clinical ascending cholangitis | 7 | 98 | 83 | 45 |
| Total bilirubin > 4 mg/dL | 41 | 79 | 72 | 51 |
| Strong predictors | ||||
| Dilated common bile duct on ultrasound | 58 | 61 | 66 | 53 |
| Total bilirubin, 1.8–4 mg/dL | 32 | 63 | 54 | 43 |
| Moderate predictors | ||||
| Abnormal liver function tests | 98 | 7 | 57 | 68 |
| Age > 55 years old | 18 | 86 | 63 | 45 |
| Gallstone pancreatitis | 22 | 69 | 48 | 41 |
CBD, common bile duct; US, ultrasound; LFT, liver function test; PPV, positive predictive value; NPV, negative predictive value.
The strong predictors as a group had poor sensitivity, specificity, PPV and NPV.
The moderate predictor that had the highest sensitivity was “abnormal LFT’s other than bilirubin” with 98%, but the specificity was only 7%. The other moderate predictors had on average lower sensitivities and higher specificities when compared to the strong predictors. In this group of predictors the NPV and PPV were not clinically useful (Table 2).
3.2. Results based on predictors
Table 3 illustrates the rate of choledocholithiasis based on predictor category. In the very strong predictor category 88%, 82% and 72% of the patients with CBD stone on US, cholangitis and total bilirubin > 4 mg/dL had choledocholithiasis on ERCP respectively. Among patients in the “strong” predictor category 65% of patients with a dilated CBD on US had choledocholithiasis and 54% of patient with a bilirubin between 1.8 and 4 mg/dL had choledocholithiasis.
Table 3.
Occurrence of choledocholithiasis.
| Predictors | Number of patients | Common bile duct stones | Percentage |
|---|---|---|---|
| Very strong predictors | |||
| Common bile duct stone on ultrasound | 43 | 38 | 88% |
| Clinical ascending cholangitis | 23 | 19 | 82% |
| Total bilirubin > 4 mg/dL | 167 | 120 | 72% |
| Strong predictors | |||
| Dilated common bile duct on ultrasound | 260 | 171 | 65% |
| Total bilirubin 1.8–4 mg/dL | 172 | 93 | 54% |
| Moderate predictors | |||
| Abnormal liver function tests | 499 | 286 | 57% |
| Age > 55 years old | 86 | 54 | 63% |
| Gallstone pancreatitis | 134 | 64 | 48% |
CBD, common bile duct; US, ultrasound; LFT, liver function test.
The unadjusted odds of choledocholithiasis with the presence of any of the very strong predictors was 3.30 (2.26–4.83, 95% CI, p < 0.0001). Individually the odds of choledocholithiasis with the presence of a stone on abdominal ultrasound, clinical ascending cholangitis and a bilirubin > 4.0 mg/dL were 6.65, 3.88 and 2.67 respectively. All of them achieving statistical significance with a p value < 0.05 (Table 4).
Table 4.
Clinical predictors: unadjusted odds of choledocholithiasis.
| Predictors | Odds ratio (OR) | Lower 95% CL | Upper 95% CL | p value |
|---|---|---|---|---|
| Unadjusted odds | ||||
| Very strong predictors | ||||
| Common bile duct stone on ultrasound | 6.65 | 2.57 | 17.18 | <.0001 |
| Clinical ascending cholangitis | 3.88 | 1.30 | 11.58 | 0.015 |
| Total bilirubin > 4 mg/dL | 2.67 | 1.80 | 3.97 | <.0001 |
| Strong predictors | ||||
| Dilated common bile duct on ultrasound | 2.19 | 1.54 | 3.12 | <.0001 |
| Total bilirubin, 1.8–4 mg/dL | 0.88 | 0.61 | 1.27 | 0.483 |
| Moderate predictors | ||||
| Abnormal liver function test | 2.88 | 1.15 | 7.18 | 0.023 |
| Age > 55 years old | 1.38 | 0.86 | 2.23 | 0.181 |
| Gallstone pancreatitis | 0.63 | 0.42 | 0.94 | 0.022 |
| Multivariate odds | ||||
| Common bile duct stone on ultrasound | 5.40 | 2.04 | 14.30 | 0.0179 |
| Clinical ascending cholangitis | 2.82 | 0.90 | 8.8 | 0.0007 |
| Total bilirubin > 4 mg/dL | 2.46 | 1.62 | 3.73 | <.0001 |
| Dilated common bile duct on ultrasound | 1.56 | 1.05 | 2.34 | 0.029 |
CBD, common bile duct; US, ultrasound; LFT, liver function test.
The unadjusted odds of choledocholithiasis with the presence of any of the strong predictors was 1.66 (1.14–2.42, 95% CI, p = 0.008). The odds of choledocholithiasis with both strong predictors present was 2.36 (1.30–4.29, 95% CI, p = 0.0046). When evaluated individually, dilated CBD on US was the only strong predictor that increased the odds of choledocholithiasis (OR 2.19, 1.97–4.30, 95% CI, p < 0.0001) (Table 4).
Multivariate analysis of the predictors of choledocholithiasis revealed that all three of the very strong predictors and one of the strong (dilated CBD on US) were independently associated with an increased risk of having choledocholithiasis at the time of ERCP. The highest odds ratios were observed in the very strong predictors group ranging from 2.5 to 5.4 times higher, with a statistically significant p value. The presence of dilated CBD on US did increase the odds of choledocholithiasis but only 1.5 times higher (Table 4).
3.3. Results based on patient risk
Of the 521 patients, 50% were high risk, 48% were intermediate risk and 2% were low risk for choledocholithiasis. Of the patients in the high risk group, 71.5% had choledocholithiasis on ERCP; while the rate of choledocholithiasis in the intermediate and low risk groups were 41% and 25% respectively.
Univariate analysis of patient risk showed that high risk patients (one very strong predictor or both strong predictors) had a statistically significant increased odds of having choledocholithiasis on ERCP (OR ranging from 2.36 to 3.3). On the other hand in the intermediate risk groups only the presence of any of the strong predictors had a statistically significant increase rate of choledocholithiasis (Table 5).
Table 5.
Patient risk: unadjusted and multivariate odds of choledocholithiasis.
| Predictors | Odds ratio (OR) | Lower 95% CI | Upper 95% CI | p value |
|---|---|---|---|---|
| Unadjusted odds | ||||
| High risk | ||||
| Presence of any very strong predictor | 3.30 | 2.26 | 4.83 | <.0001 |
| Presence of two very strong predictors | 9.68 | 2.86 | 32.80 | 0.0003 |
| Presence of both strong predictors | 2.36 | 1.30 | 4.29 | 0.0046 |
| Intermediate risk | ||||
| Presence of any strong predictor | 1.66 | 1.14 | 2.42 | 0.008 |
| Presence of one strong predictor | 1.54 | 1.04 | 2.27 | 0.029 |
| Presence of any moderate predictor | 2.07 | 0.79 | 5.43 | 0.138 |
| Multivariate odds | ||||
| High risk | ||||
| Presence of any very strong predictor | 2.87 | 1.55 | 5.32 | 0.0008 |
| Presence of both strong predictors | 3.24 | 1.69 | 6.22 | 0.0004 |
We independently calculated the risk of choledocholithiasis on ERCP in those high risk patients that had 2 of the very strong predictors. The risk of choledocholithiasis was 9.68 times higher with a p < 0.05, but the number of patients with 2 very strong predictors was relatively small (24/27).
Multivariate analysis of patient risk groups revealed that only those patients in the high risk category had and increased risk of choledocholithiasis on ERCP. This result was true with either one of the very strong predictors or both strong predictors. The independent odds of choledocholithiasis with any of the very strong predictors was 2.87 (1.55–5.32, 95% CI, p = 0.0008), and 3.24 (1.68–6.9, 95% CI, p = 0.0006) with 2 strong predictors (Table 5).
8 of the patients evaluated had low risk for choledocholithiasis but still underwent ERCP. The reasons for endoscopic intervention in these patients were positive intraoperative cholangiograms at the time of cholecystectomy and increasing bilirubin levels and persistent abdominal pain.
3.4. Probability of choledocholithiasis
The calculated probability of choledocholithiasis in the patient risk categories were 79, 23 and 20.3% in the high risk, intermediate risk and low risk patient category respectively. This calculation was performed to adequately compare our results with the current guidelines.
4. Discussion
This is the first study that evaluates the most current guidelines proposed by the ASGE for the diagnosis, approach and treatment of choledocholithiasis. Our study confirms that the ASGE guideline for suspected choledocholithiasis accurately stratifies patients in determining the presence or absence of choledocholithiasis and recommends the best management options [8].
The guidelines describe a broad range of probabilities for the presence of choledocholithiasis based on the patient’s likelihood which was determined by the presence of specific clinical predictors. In patients with a high risk of choledocholithiasis the guidelines report a probability greater than 50%, in our study cohort we were able to determine the probability is closer to 80% and that the presence of any of the very strong predictors or both strong predictors (high risk group) are very specific in establishing the presence of choledocholithiasis. Therefore the recommendation of preoperative ERCP is valid, and accurate [8].
In patients with intermediate risks the stated probability of choledocholithiasis is between 10 and 50%. In our cohort the number was closer to 20%, again agreeing with the guidelines that further testing is required to confirm or exclude the presence of choledocholithiasis prior to ERCP [9–11]. Two approaches that have been recommended, and have been demonstrated to be both cost effective and carry the least morbidity and mortality are laparoscopic cholecystectomy with intraoperative cholangiogram or single session EUS/ERCP in those patients with choledocholithiasis on EUS versus EUS followed by laparoscopic cholecystectomy in the group of patients without choledocholithiasis on EUS [9,10,12–15]. MRCP is an option to consider in those institutions where the expertise and/or equipment for EUS are not available, as a recent systematic review and prospective study have demonstrated that both techniques have statistically similar diagnostic accuracy, sensitivity and specificity [16,17]. Unfortunately, MRCP has been shown to be more expensive than EUS and would add significant amount of cost to the patients hospital stay and care [18]. In our view in institutions without EUS capabilities, laparoscopic cholecystectomy and intraoperative cholangiogram may be the best approach as all patients will eventually require surgical removal of their gallbladder.
Our multivariate analysis confirms that all of the very strong predictors increase the odds of choledocholithiasis by 2.5–5.4 times. The only strong predictor that individually increased the likelihood of choledocholithiasis was the presence of a dilated CBD on ultrasound. In support of our findings, a trial by Liu et al. confirmed the occurrence of choledocholithiasis was 92.6% in patients that presented clinically with biliary symptoms, a dilated CBD greater than 5 mm and 2 out of 4 biochemical parameters (total bilirubin ≥ 1.5 mg/dL, alkaline phosphatase ≥ 150 U/L, AST ≥ 100 U/L, ALT ≥ 100 U/L) in the absence of acute pancreatitis or cholecystitis [11].
One interesting finding of our study is that the presence or diagnosis of gallstone pancreatitis was not associated with an increased risk of choledocholithiasis on ERCP. This seems counterintuitive since gallstone pancreatitis can only occur in the setting of a stone or stone material in the CBD obstructing the Sphincter of Oddi. In our cohort, 134 of the 521 patients evaluated had gallstone pancreatitis, 48% of which had choledocholithiasis on ERCP. The sensitivity and specificity of gallstone pancreatitis for the diagnosis of choledocholithiasis were 22 and 67% respectively. In three separate randomized controlled trials, early ERCP in patients with acute biliary pancreatitis demonstrated a decrease in morbidity and mortality. These trials did include patients with evidence of biliary obstruction and/or cholangitis which alone would confer high risk status and need for ERCP [19–21]. On the other hand, Folsch et al. in a randomized controlled trial, demonstrated that early ERCP in the management for acute biliary pancreatitis did not improve morbidity and or mortality in patients with bilirubin levels lower than 5 mg/dL [22]. A Potential explanation for this phenomenon is that the stone material that causes gallstone pancreatitis is likely to be smaller, and pass through the sphincter of Oddi after the obstruction. In a recent trial, a Monte Carlo model showed that in severe acute biliary pancreatitis an EUS-first strategy was cost equivalent to other modalities and incurred in less morbidity compared to other invasive strategies [18].
The major strengths of this study are the all patients underwent ERCP regardless of risk stratification category, and ERCP is the gold standard for diagnosis, confirmation and treatment of choledocholithiasis. The second strength of this study is that it is the largest cohort of patients evaluated for the presence or absence of choledocholithiasis and comparing the results to the guidelines. On the other hand the limitations of the study include that it is a retrospective nature of the analysis and that the large number Hispanic patients which may create a population bias and not may applicable to all geographic regions. In a retrospective cohort, the potential for confirmation bias cannot be excluded. We would estimate that the probability of choledocholithiasis is probably at the upper limit of true population prevalence given the strong clinical suspicion that led to ERCP. We would, however, estimate that the odds of choledocholithiasis would be significantly altered between groups evaluated.
Based on our results we conclude that the present ASGE choledocholithiasis guidelines are valid and accurate. All of the very strong predictors and one of the strong predictors independently increase the odds of choledocholithiasis. Nonetheless, there are still a significant number of patients in the high and intermediate risk groups that undergo ERCP unnecessarily, and the sensitivity and specificity of the current predictors are too low to obviate the need for non-invasive tests (EUS/MRCP) to confirm the presence of choledocholithiasis in all the risk groups. This finding allows room to identify new predictors and combination of clinical data that can better predict the presence or absence of choledocholithiasis.
Acknowledgments
Grant support
None.
Footnotes
Conflict of interest statement
None declared.
Contributor Information
Moises Ilan Nevah Rubin, Email: Moises.I.Nevah@uth.tmc.edu.
Frank J. Lukens, Email: lukens.frank@mayo.edu.
References
- 1.Everhart JE, Khare M, Hill M, et al. Prevalence and ethnic differences in gall-bladder disease in the United States. Gastroenterology. 1999;117:632–9. doi: 10.1016/s0016-5085(99)70456-7. [DOI] [PubMed] [Google Scholar]
- 2.Everhart JE, Ruhl CE. Burden of digestive diseases in the United States. Part I. Overall and upper gastrointestinal diseases. Gastroenterology. 2009;136:376–86. doi: 10.1053/j.gastro.2008.12.015. [DOI] [PubMed] [Google Scholar]
- 3.Hunter JG. Laparoscopic transcystic common bile duct exploration. The American Journal of Surgery. 1992;163:53–8. doi: 10.1016/0002-9610(92)90252-m. [DOI] [PubMed] [Google Scholar]
- 4.Robinson BL, Donohue JH, Gunes S, et al. Selective operative cholangiography: appropriate management for laparoscopic cholecystectomy. Archives of Surgery. 1995;130:625–31. doi: 10.1001/archsurg.1995.01430060063012. [DOI] [PubMed] [Google Scholar]
- 5.Petelin JB. Laparoscopic common bile duct exploration. Surgical Endoscopy. 2003;17:1705–15. doi: 10.1007/s00464-002-8917-4. [DOI] [PubMed] [Google Scholar]
- 6.O’Neill CJ, Gillies DM, Gani JS. Choledocholithiasis: overdiagnosed endoscopically and undertreated laparoscopically. ANZ Journal of Surgery. 2008;78:487–91. doi: 10.1111/j.1445-2197.2008.04540.x. [DOI] [PubMed] [Google Scholar]
- 7.Chang L, Lo SK, Stabile BE, et al. Gallstone pancreatitis: a prospective study on the incidence of cholangitis and clinical predictors of retained common bile duct stones. American Journal of Gastroenterology. 1998;93:527–31. doi: 10.1111/j.1572-0241.1998.159_b.x. [DOI] [PubMed] [Google Scholar]
- 8.Maple JT, Ben-Menachem T, Anderson MA, et al. The role of endoscopy in the evaluation of suspected choledocholithiasis. Gastrointestinal Endoscopy. 2010;71:1–9. doi: 10.1016/j.gie.2009.09.041. [DOI] [PubMed] [Google Scholar]
- 9.Sahai AV, Mauldin PD, Marsi V, et al. Bile duct stones and laparoscopic cholecystectomy: a decision analysis to assess the roles of intraoperative cholangiography, EUS, and ERCP. Gastrointestinal Endoscopy. 1999;49:334–43. doi: 10.1016/s0016-5107(99)70010-6. [DOI] [PubMed] [Google Scholar]
- 10.Urbach D, Khajanchee Y, Jobe B, et al. Cost-effective management of common bile duct stones. Surgical Endoscopy. 2001;15:4–13. doi: 10.1007/s004640000322. [DOI] [PubMed] [Google Scholar]
- 11.Liu T, Consorti E, Kawashima A, et al. Patient evaluation and management with selective use of magnetic resonance cholangiography and endoscopic retrograde cholangiopancreatography before laparoscopic cholecystectomy. Annals of Surgery. 2001;234:33–40. doi: 10.1097/00000658-200107000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee YT, Chan FKL, Leung WK, et al. Comparison of EUS and ERCP in the investigation with suspected biliary obstruction caused by choledocholithiasis: a randomized study. Gastrointestinal Endoscopy. 2008;67:660–8. doi: 10.1016/j.gie.2007.07.025. [DOI] [PubMed] [Google Scholar]
- 13.Polkowski M, Regula J, Tilszer A, et al. Endoscopic ultrasound versus endoscopic retrograde cholangiography for patients with intermediate probability of bile duct stones: a randomized trial comparing two management strategies. Endoscopy. 2007;39:296–303. doi: 10.1055/s-2007-966264. [DOI] [PubMed] [Google Scholar]
- 14.Liu CL, Fan ST, Lo CM, et al. Comparison of early endoscopic ultrasonography and endoscopic retrograde cholangiopancreatography in the management of acute biliary pancreatitis: a prospective randomized study. Clinical Gastroenterology and Hepatology. 2005;3:1238–44. doi: 10.1016/s1542-3565(05)00619-1. [DOI] [PubMed] [Google Scholar]
- 15.Karakan T, Cindoruk M, Alagozlu H, et al. EUS versus endoscopic retrograde cholangiography for patients with intermediate probability of bile duct stones: a prospective randomized trial. Gastrointestinal Endoscopy. 2009;69:244–52. doi: 10.1016/j.gie.2008.05.023. [DOI] [PubMed] [Google Scholar]
- 16.Ledro-Cano D. Suspected choledocholithiasis: endoscopic ultrasound or magnetic resonance cholangiopancreatography? A systematic review. European Journal of Gastroenterology & Hepatology. 2007;19:1007–11. doi: 10.1097/MEG.0b013e328133f30b. [DOI] [PubMed] [Google Scholar]
- 17.Fernandez-Esparrach G, Gines A, Sanchez M, et al. Comparison of endoscopic ultrasonography and magnetic resonance cholangiopancreatography in the diagnosis of pancreatobiliary diseases: a prospective study. American Journal of Gastroenterology. 2007;102:1632–9. doi: 10.1111/j.1572-0241.2007.01333.x. [DOI] [PubMed] [Google Scholar]
- 18.Romagnuolo J, Currie G the Calgary Advanced Therapeutic Endoscopy Center study g. Noninvasive vs. selective invasive biliary imaging for acute biliary pancreatitis: an economic evaluation by using decision tree analysis. Gastrointestinal Endoscopy. 2005;61:86–97. doi: 10.1016/s0016-5107(04)02472-1. [DOI] [PubMed] [Google Scholar]
- 19.Nowak A, Nowakowska-Dulawa E, Marek TA, Rybicka J. Final results of the prospective, randomized, controlled study on endoscopic sphincterotomy versus conventional management in acute biliary pancreatitis. Gastroenterology. 1995;108:A380. [Google Scholar]
- 20.Fan S-T, Lai E, Mok F, et al. Early treatment of acute biliary pancreatitis by endoscopic papillotomy. New England Journal of Medicine. 1993;328:228–32. doi: 10.1056/NEJM199301283280402. [DOI] [PubMed] [Google Scholar]
- 21.Neoptolemos JP, London NJ, James D, et al. Controlled trial of urgent endoscopic retrograde cholangiopancreatography and endoscopic sphincterotomy versus conservative treatment for acute pancreatitis due to gallstones. The Lancet. 1988;332:979–83. doi: 10.1016/s0140-6736(88)90740-4. [DOI] [PubMed] [Google Scholar]
- 22.Fölsch UR, Nitsche R, Lüdtke R, et al. Early ERCP and papillotomy compared with conservative treatment for acute biliary pancreatitis. New England Journal of Medicine. 1997;336:237–42. doi: 10.1056/NEJM199701233360401. [DOI] [PubMed] [Google Scholar]


