Abstract
Coronavirus disease 2019 (COVID-19) pneumonia caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has resulted in significant mortality in pandemic proportions. Inflammation in response to the infection contributes to the pathogenesis of pneumonia. This review will discuss prior studies on the use of glucocorticoids to treat respiratory infections, the rationale for the use glucocorticoids in COVID-19, and review of existing data. We will also highlight outstanding research questions for future studies.
Keywords: glucocorticoid, treatment, COVID-19
Pneumonia, especially in most severe forms, can be considered a systemic inflammatory disease.1 Inflammation is a key element in pneumonia pathogenesis, and the balance between proinflammatory and anti-inflammatory cytokines is crucial in determining its clinical severity.2 This is why inflammation has been proposed as a potential therapeutic target in patients with pneumonia.3 Systemic corticosteroids exert pleiotropic anti-inflammatory activities, and are widely used in the treatment of several inflammatory diseases.4 They also have been suggested as adjunctive therapy in some pneumonia subtypes. For example, a clear benefit from glucocorticoid administration has been demonstrated in patients with Pneumocystis jirovecii and Mycoplasma pneumoniae pneumonia.5,6 However, conflicting data have been reported in other respiratory infections, such is the case of community-acquired pneumonia (CAP) and influenza.7,8
Severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2) infection has a wide spectrum of clinical manifestations, ranging from asymptomatic carriage to acute respiratory distress syndrome (ARDS). Severe forms of disease are generally characterized by a prominent inflammatory syndrome, with elevated C-reactive protein, hyper-ferritinemia, thrombocytopenia, and high fever.9,10 Moreover, COVID-19 can lead to the development of immunologic complications characterized by hyper-inflammatory damage, such is the case of cytokine storm and macrophage activating syndrome (MAS).11
Current guidelines recommend offering treatment with systemic glucocorticoids to patients with SARS-CoV-2 infection and concurrent respiratory insufficiency.12 Furthermore, there is increasing evidence on the efficacy of inflammatory cytokine signaling inhibition (e.g., IL-1, IL-6, Janus kinase [JAK] pathway) in severe COVID-19.13 Herein we review the most significant immune mechanisms involved in COVID-19 pathogenesis, as a rationale to discuss the potential therapeutic role for glucocorticoids in SARS-CoV-2 infection, compared with other pulmonary infections and ARDS.
Corticosteroids in Community-Acquired Pneumonia
The adjunctive use of corticosteroids in CAP is controversial. Although some studies have shown benefit, currently, the American Thoracic Society (ATS)/Infectious Diseases Society of America (IDSA) guideline recommends against their routine use.14 However, they do recommend the use of IV hydrocortisone (200 mg/d) in patients with severe CAP and septic shock that is refractory to fluid resuscitation and vasopressor support, although the recommendation is weak, and the evidence quality is low. ►Table 1 summarizes the main RCTs regarding the use of glucocorticoids in CAP.15–22
Table 1.
RCT evaluating the use of glucocorticoids in community-acguired pneumonia
| Study, year, journal | Study design | Drug and dose | Sample size | Inclusion criteria | Primary outcome | Results (primary outcome) | Secondary outcome results | Adverse effects |
|---|---|---|---|---|---|---|---|---|
| Wittermans et al, 2021, Eur Resplr J15 | Double-blind, placebo-controlled, RCT 1:1 | DXM (6 mg qd) vs. placebo for 4 d | 401 | Adult CAP Immunocompetent | Median length of stay (days) | Achieved. 4.5 (4.0–5.0) d in DXM group vs. 5.0 (4.6–5.4) d in placebo group, p = 0.033 |
Significant reduction in secondary ICU admission rate in the DXM group. | Hyperglycemia |
| Torres et al, 2015, JAMA16 | Double-blind, placebo-controlled, RCT 1:1 | MP (0.5 mg/kg for 5 d) vs. placebo | 120 | Adult Symptoms New chest X-ray infiltrate Severe CAP CRP >150 mg/L | Rate of treatment failure: Early (<72 h) Late (72–120 h) | Achieved. 59 in the MP group vs. 1628 in the placebo group. Mean difference 1 9 (5–33), p = 0.01 Not achieved for early treatment failure: 35 in the MP group vs. 47 in the placebo group. Mean difference 2 (−7 to 11 ), p> 0.99 Achieved for late treatment failure 24 in the MP group vs. 1425 in the placebo group. Mean difference 21 (9–33), p = 0.002 |
Not significant differences in time to clinical stability, length of hospital stay, length of ICU stay, in-hospital mortality. | No significant differences |
| Blum et al 2015, Lancet17 | Double-blind, placebo-controlled, RCT 1:1 | PDN (50 mg qd for 7 d) vs. placebo | 802 | Adult CAP | Time to clinical stability (days) | Achieved. 3.0 (2.5–3.4) d in PDN group vs. 4.4 (4.0–5.0) d in placebo group. HR 1.33 (1.15–1.50), p <0.0001 |
Significant reduction in time to hospital discharge and duration of intravenous antibiotic treatment in the PDN group. No significant difference in recurrent pneumonia, re-admission to hospital, ICU admission, time to ICU admission, time in ICU, death from any cause, time to death, total duration of antibiotic therapy, CAP score at days 5 and 30. |
Hyperglycemia |
| Meijvis et al 2011, Lancet18 | Double-blind, placebo-controlled, RCT 1:1 | DXM (5 mg gd for 4 d) vs. placebo | 304 | Adult CAP | Length of hospital stay (d) | Achieved. 6.5 (5.0–9.0) d in DXM group vs. 7.5 (5.3–11.5) d in placebo group, p = 0.0480 |
No significant differences in in-hospital mortality, time to death, 30-d mortality, ICU admission, time to ICU admission, length of stay in ICU, empyema or pleural effusion, re-admission within 30 d. | Hyperglycemia |
| Fernández-Serrano et al, 2011, Crit Care19 | Double-blind, RCT | MP (200 mg bolus, then 20 mg g6h for 3 d, then 20 mg q 12h for 3 d, then 20 mg gd) vs. placebo | 56 | Adult Consolidation at chest X-ray P/F <300 | Need for MV at day 9 | Not achieved. 1/28 in MPN group vs. 5/28 in placebo group, p> 0.05 |
Significant reduction in time to resolution of morbidity and IL-6 decrease in the MP group. No significant difference in ICU admission, duration of ICU stay, early and late mortality, length of stay. |
No significant differences |
| Snijders et al 2010, Am J Respir Crit Care Med20 | Double-blind, placebo-controlled, RCT 1:1 | PDN (40 mg gd for 7 d) vs. placebo | 213 | Adult symptoms new consolidation on chest X-ray | Clinical cure at day 7 | Not achieved. 84 (80.8) in PDN group vs. 93 (85.3) in placebo group. OR 0.72 (0.35–1.49), p = 0.38 |
Significant increase in late failure in the PDN group. No significant differences in clinical cure at day 30, 30-d mortality, length of stay, time to clinical stability, and early failure. |
No significant differences |
| Mlkaml et al 2007, Lung21 | Open-label, RCT 1:1 | PDN (40 mg gd for 3 d) vs. no PDN | 31 | Adult CAP | Length of hospital stay (days) | Not achieved. 11.3 (5.5) d in PDN group vs. 15.5 (1 0.7) d in no steroid group, p = 0.1 82 |
Significant reduction in duration of IV antibiotic, time to normalization of temperature, respiratory rate, and CRP in the PDN group. No differences in time to normalization of SpO2 and pulse rate. |
No significant differences |
| Confalonieri et al 2005, Am J Resplr Crit Care Med22 | Double-blind, placebo-controlled, RCT 1:1 | HCS 200 mg bolus, then 240 mg qd at 10 mg/h for 7 d vs. placebo | 48 | Severe CAP | Improvement of P/F and MODS score at day 8 and development of delayed septic shock. | Achieved for P/F Improvement. 2087 in HCS group vs. 939 in placebo group, p = 0.0018 Achieved for delayed septic shock. 0 (0) in HCS group vs. 1052 in placebo group, p <0.001 Achieved for MODS score Improvement. 0.3 (0.5) in HCS group vs. 1.0 (0.9) in placebo group, p = 0.003 |
Significant reduction in ICU mortality, hospital mortality, 60-d mortality, length of ICU stay, length of hospital stay, and duration of mechanical ventilation in the HCS group. | Increased incidence of major complication in the placebo group |
Abbreviations: ARDS, acute respiratory distress syndrome; CAP, community-acquired pneumonia; CRP, C-reactive protein; CT, computed tomography; DXM, dexamethasone; HCS, hydrocortisone; HR, hazard ratio; ICU, intensive care unit; IL-6: interleukin-6; IMV, invasive mechanical ventilation; iv, intravenous; MODS, multiple organ dysfunction syndrome; MP, méthylprednisolone; MV, mechanical ventilation; NIMV, noninvasive mechanical ventilation; P/F: arterial oxygen partial pressure out of FiO2; PDN, prednisolone; q6h/q12h, every 6/12 h administration; qd: once a day; RCT, randomized controlled trial; SpO2, peripheral oxygen saturation; vs: versus.
Several systematic reviews and meta-analyses have reported that the use of corticosteroids in CAP improves outcomes.8,23–27 However, the benefit is inconsistent, partly related to the studies included and the heterogeneity of illness severity. Additionally, a range of primary and secondary outcomes are utilized creating more inconsistency. One study showed a 3% decrease in mortality, 5% reduction in the need for mechanical ventilation, and decreased length of hospital stay by 1 day.28
A Cochrane review of randomized controlled trial (RCT) of corticosteroid use versus placebo in severe CAP showed significant reduction in mortality in the treatment arm with risk ratio of 0.58.24 Early clinical failure defined as death from any cause, radiographic progression, or clinical instability at day 5 and 8, was significantly reduced in the steroid arm. In this meta-analysis, hyperglycemia was more common in the treatment group but there was no significant increase in secondary infections. The number needed to treat to prevent one death was 18 (95% confidence interval [CI]: 12–49). The quality of evidence on themortality benefit in severe CAP was deemed to be moderate. Others have reported that patients with severe CAP with high initial C-reactive protein level showed to have benefited from methylprednisolone.16 Of note, there was no mortality difference in the nonsevere CAP group, but a reduction in morbidity was observed.
Corticosteroids in Influenza
Corticosteroids have been used to treated influenza-infected patients including pandemic influenza. The rationale of their use similarly relates to early viral-mediated cytokine release and an excessive inflammatory response.29 Case series during the H1N1 pandemic showed some promise of steroid use30 but other studies revealed the opposite.27,31 Even though the data was controversial, most patients (69%) hospitalized with severe illness during the H1N1 pandemic received corticosteroids.32 There is onlyone RCTon the use of steroids in patients with influenza, the rest were observation studies. However, the one RCT was designed to assess the adjunctive use of corticosteroids in CAP, and only a subgroup analysis was completed for patients who were positive for influenza.33
A Cochrane meta-analysis review of corticosteroids in influenza revealed increased mortality.7 However, the heterogeneity of studies including steroid dosing and concomitant conditions may have influenced the corticosteroid use and clinical outcomes (e.g., asthma exacerbations and refractory shock). There were inconsistent indications, end points, clinical severity scores, dose and type of corticosteroid, timing, duration of use, and co-interventions. The authors graded the certainty of the results as “very low.” Another meta-analysis focused on H1N1 infections specifically found corticosteroid use was associated with a risk ratio for mortality of 1.85.34
Although corticosteroid use in respiratory infections has shown benefit in some studies, there is a theoretical risk of superimposed or increased risk of secondary bacterial or fungal infection. Meta-analysis of its use in influenza revealed an increased risk of hospital-acquired infection with an odds ratio of 3.16.35 Therefore, overall, the ATS/IDSA guidelines recommended against the use of corticosteroids in influenza pneumonia.
Corticosteroids in Acute Respiratory Distress Syndrome
►Table 2 summarizes the main RCTs regarding the use of glucocorticoids in ARDS.36–40 Early study on corticosteroid use in ARDS was performed in the 1980s with extraordinary doses of methylprednisolone of 30 mg/kg every 6 hours for a total of four doses over 24 hours which did not reveal significant mortality benefit.41 However, an RCT in 1998 showed a mortality reduction in patients with unresolving ARDS treated with corticosteroids initiated after 7 days of mechanical ventilation, albeit limited by the small sample size.40 Later studies incorporating larger sample size showed no differences in mortality, including a larger study by Meduri and colleagues.38,39 The latter studies initiated corticosteroids within 72 hours of ARDS although they did not show mortality benefit but did show increase in ventilator free days and improvement of pulmonary and extrapulmonary organ dysfunction.38 Study using hydrocortisone in sepsis-associated ARDS showed improvement in pulmonary physiology but no mortality benefit.37 Because of the conflicting outcomes, corticosteroid is not routinely used for ARDS.
Table 2.
RCT evaluating the use of glucocorticoids in acute respiratory distress syndrome
| Study, year, journal | Study design | Drug and dose | Sample size | Inclusion criteria | Primary outcome | Results (primary outcome) | Secondary outcome results | Adverse effects |
|---|---|---|---|---|---|---|---|---|
| Villar et al, 2020, Lancet Respir Med36 | RCT 1:1 | DXM (20 mg gd days 1–5, then 10 mg gd days 6–10) vs. no steroid | 277 | Adult IMV ARDS | Ventilator-free days at day 28 | Achieved. 12.3 (9.9) d in DXM group vs. 7.5 (9.0) d in no steroid group. Mean difference 4.8 (2.57–7.03), p <0.0001 |
Significant reduction in all-cause mortality at day 60, ICU mortality, hospital mortality, duration of MV in ICU survivors, duration of MV in survivors at day 60 in the DXM group. | No significant differences |
| Tongyoo et al, 2016, Crlt Care37 | Double-blind, placebo-controlled, RCT 1:1 | HCS (50 mg g6h for 7 d)vs. placebo | 206 | Adult Severe sepsis or septic shock ARDS | Mortality at day 28 | Not achieved. 22 (22.5) in HCS group vs. 27 (27.3) in placebo group. RR 0.82 (0.50–1.34), p = 0.51 |
No significant differences in mortality at 60 d, duration of MV at day 28, MV-free days at day 28, duration of vasopressor treatment, RRT, duration of RRT, need for organ support, organ support-free days at day 28. | Hyperglycemia |
| Medurl et al, 2007, Chest38 | Double-blind, placebo-controlled, RCT 2:1 | MP (1 mg/kg load, then 1 mg/kg gd for 14 d, then 0.5 mg/kg gd for 7 d, then 0.25 mg/kg gd for 4 d, then 0.1 25 mg/kg gd for 3 d) vs. placebo | 91 | Adult IMV ARDS | Improvement in LIS at day 7 | Achieved. 44 (69.8) in MP group vs. 10 (35.7) in placebo group. RR 1.96 (1.16–3.30), p = 0.002 |
Significant reduction in need for breathing assistance, PEEP, MV-free days, MODS score, CRP, plasma cortisol, and increase in P/F in ventilated patients in the MP group at day 7. No significant differences in new infections, VAP, and mortality at day 7. |
Increased incidence of pneumonia in the placebo group |
| Steinberg et al 2006, N Engl J Med39 | Double-blind, placebo-controlled, RCT 1:1 | MP (2 mg/kg load, then 0.5 mg/kg g6h for 14 d, then 0.5 mg/kg q 12h for 7 d, then tapering) vs. placebo | 180 | IMV 7–28 d after diagnosis of ARDS MV Persistent bilateral infiltrates P/F <200 | Mortality at day 60 | Not achieved. 28.6 (20.8–38.6) in MP vs. 29.2 (20.8–39.4) in placebo group, p = 1.0 |
Significant reduction in ventilator-free days, and cardiovascular failure free days at day 28 in the MP group. No significant differences in coagulation abnormalities, hepatic failure, renal failure, and ICU free days at day 28. | Increased incidence of pneumonia and shock events in the placebo group |
| Meduri et al, 1998, JAMA40 | Double-blind, placebo-controlled, RCT 2:1 | MP (2 mg/kg bolus, then 2 mg/kg for 14 d, then 1 mg/kg for 7 d, then 0.5 mg/kg for 7 d, then 0.25 mg/kg for 2 d, then 0.1 25 mg/kg for 2 d) vs. no steroid | 24 | Adult ARDS 7 d of MV | Improvement in lung function and mortality | Achieved for P/F at day 10. 26219 in MP group vs. 14835 in no steroid group, p <0.001 Achieved for LIS. 1.7 (0.1) in MP group vs. 3.0 (0.2) in no steroid group, p <0.001 |
Significant reduction in pulmonary artery pressure, successful extubation, MODS score, and duration of MV in the MP group. No significant differences in new infections, new VAP, and survivors. |
No significant differences |
Abbreviations: ARDS, acute respiratory distress syndrome; CRP C-reactive protein; DXM, dexamethasone; HCS, hydrocortisone; ICU, intensive care unit; IMV: invasive mechanical ventilation; iv, intravenous; LIS, lung injury score; MODS, multiple organ dysfunction syndrome; MP, méthylprednisolone; MV, mechanical ventilation; NIMV, noninvasive mechanical ventilation; P/F, arterial oxygen partial pressure out of FiO2; PEEP, positive end expiratory pressure; PDN, prednisolone; q6h/q12h, every 6/12 h administration; qd, once a day; RCT, randomized controlled trial; RR, risk ratio; RRT, renal replacement therapy; SpO2, peripheral oxygen saturation; VAP, ventilator-acquired pneumonia; vs, versus.
A very recent study of corticosteroid treatment in ARDS has shown more promise. A multicenter randomized controlled DEXA-ARDS trial involving 277 patients with moderate to severe ARDS demonstrated increase in ventilator-free days and absolute decrease in mortality in patients receiving dexamethasone (20 mg daily for 5 days, followed by 10 mg daily for an additional 5 days).42 Seventy-seven percent of patients had pneumonia or sepsis as the etiology for their ARDS. At 60 days, 21% of the patients in the treatment group had died compared with 36% of the control group. The proportion of adverse effects did not differ between the groups.42
Corticosteroids for COVID-19: Pathophysiology and Rationale
Pathophysiology of COVID-19 and Related Systemic Inflammatory Syndrome
SARS-CoV-2 is mainly transmitted through respiratory droplets and direct contact,43 has a median incubation period of 5 days,44 and in approximately 40 to 45% cases the infection is asymptomatic.45 Among symptomatic patients, the majority develops a mild flu-like syndrome with concomitant anosmia, ageusia, and fatigue; a smaller percentage develops severe and potentially life-threatening pneumonia and respiratory failure with viral sepsis and multiorgan dysfunction.10 At early stages, SARS-CoV-2 infects nasal epithelial cells, and propagates through the respiratory tract. During replication, viral double-stranded RNA intermediates are recognized by cytoplasmic pattern recognition receptors, in particular melanoma differentiation antigen 5 and retinoic acid-inducible gene 1, which activate the signaling pathways leading to type I and III interferon (IFN) synthesis, as well as nuclear factor kappa-light-chain-enhancer of activated B-cells (NF-kB)-dependent synthesis of inflammatory cytokines.46 Thus, upper airway infection leads to an IFN-mediated immune response that is capable of clearing the virus in most cases.
However, SARS-CoV-2 is able to evade the IFN response,47 and about one-fifth of the patients progress to a more severe stage, characterized by lower respiratory tract involvement, with prominent inflammatory response. Through the activation of toll-like receptor 3 and NLRP3,48 infected pneumocytes release large amounts of proinflammatory cytokines (i.e., interleukin-6 [IL-6], IL-1β, and tumor necrosis factor-α [TNF-α]) that act as chemoattractants for other immune cells, such as neutrophils and lymphocytes. This strong inflammatory milieu, which is essential for enhancing viral clearance, is also responsible for local and systemic inflammatory damage, culminating in severe pneumonia, ARDS, viral sepsis, and cytokine storm.49,50 Interstitial edema, endothelial disruption, local and systemic inflammation are responsible for impaired oxygen diffusion, hypoxemia, and aberrant activation of the coagulation cascade with formation of microthrombi which are prominent features of severe COVID-19.51 Moreover, neutrophil extracellular traps (NETs) formation has been described in patients affected by SARS-CoV-2. These structures are associated with sustained local inflammation and pulmonary damage.52 On the other hand, direct viral injury is not the only contributor in precipitating organ dysfunction in patients with COVID-19.53 It has been postulated that factors as impaired viral clearance (due to genetic, acquired, or viral-related causes), low type I IFN signature,54 and increased NETosis might predispose to the development of severe forms of COVID-19, which can culminate in cytokine storm.11 However, predictors and risk factors for the occurrence of severe SARS-CoV-2 infection and cytokine storm remain largely unknown.
The term “cytokine storm syndrome” encompasses a group of disorders of different etiologies, culminating in systemic inflammatory syndrome, hemodynamic instability, and organ failure.55 SARS-CoV-2 has been proven to be an established cause of cytokine storm.56 Classification criteria for COVID-cytokine storm have been recently proposed, emphasizing the prominent role of the immune system in severe COVID-19 pathogenesis and clinical presentation.57 Thus, it has been suggested to screen for cytokine storm syndrome in patients with severe SARS-CoV-2 infection.58 Moreover, such inflammatory mediators might stimulate autoreactive lymphocytes via bystander activation, and this could explain the appearance of autoimmune phenomena in late stages or severe forms of the disease.56
With these biological assumptions, immunomodulation was postulated to play a relevant role in the treatment of COVID-19, particularly in most severe forms when systemic inflammatory syndrome is present or incipient. By modulating a potentially harmful (hyper)immune response, anti-inflammatory drugs might exert a disease-modifying activity. Thus, hyperinflammation is regarded as a potential “treatable trait” in SARS-CoV-2 infection. Risk stratification of patients (through medical tools, such as clinical, biochemical, radiological biomarkers, as well as artificial intelligence applications) is urgently required.
Pharmacology of Systemic Glucocorticoids and Rationale for Their Administration in Patients with COVID-19
Glucocorticoids are among the most potent inhibitors of inflammation. They have been proposed as an adjunctive therapy in other forms of pneumonia, although with contrasting results.3 Moreover, they have already been administered in certain types of viral pneumonia, such as influenza, SARS, and Middle-East respiratory syndrome.59 Corticosteroids exert pleiotropic effects through both genomic and nongenomic activities, resulting in modulation of the inflammatory response and immunosuppression.60 Among the most elucidated mechanisms, glucocorticoids bind their receptor (GR) located in the cytoplasm of inflammatory cells, then migrate inside the cell nucleus and repress the activity of proinflammatory transcription factors, such as NF-kB and activator protein-1. This results into reduction of the synthesis of inflammatory cytokines (i.e., IL-6, IL-1, TNF-α, etc.), as well as other proteins and enzymes that would enhance inflammation through different mechanisms (e.g., phospholipase A2).61 Apart from transcription-mediated effects, glucocorticoids also exert nongenomic effects, such as regulating intracellular calcium homeostasis, reactive oxygen and nitrogen species metabolism, and cyclooxygenase-2 expression.60,62 Due to their rapidity of onset, nongenomic activities might be responsible for the short-term benefits obtained with high-dose steroid therapy in acute inflammatory conditions. Dexamethasone and methylprednisolone display a more potent nongenomic activity compared with prednisone, and should be preferred for systemic high-dose treatment.63 Moreover, systemic glucocorticoids have been classified according to their pharmacokinetic profile into short- (cortisone and hydrocortisone), medium- (prednisone, prednisolone, and methylprednisolone), and long-acting (dexamethasone and betamethasone) molecules.64
Systemic glucocorticoid therapy was able to reduce the activity of NF-kB, as well as the synthesis of inflammatory cytokines, in a cohort of patients with unresolving ARDS.65 A recent meta-analysis has demonstrated corticosteroids efficacy in hospitalized patients with COVID-19 and respiratory insufficiency,66 and current guidelines recommend considering steroid therapy in this subset of patients.12 ►Fig. 1 synthesizes the key elements in the immune pathogenesis of SARS-CoV-2 infection and the therapeutic targets of glucocorticoids.
Fig.1.
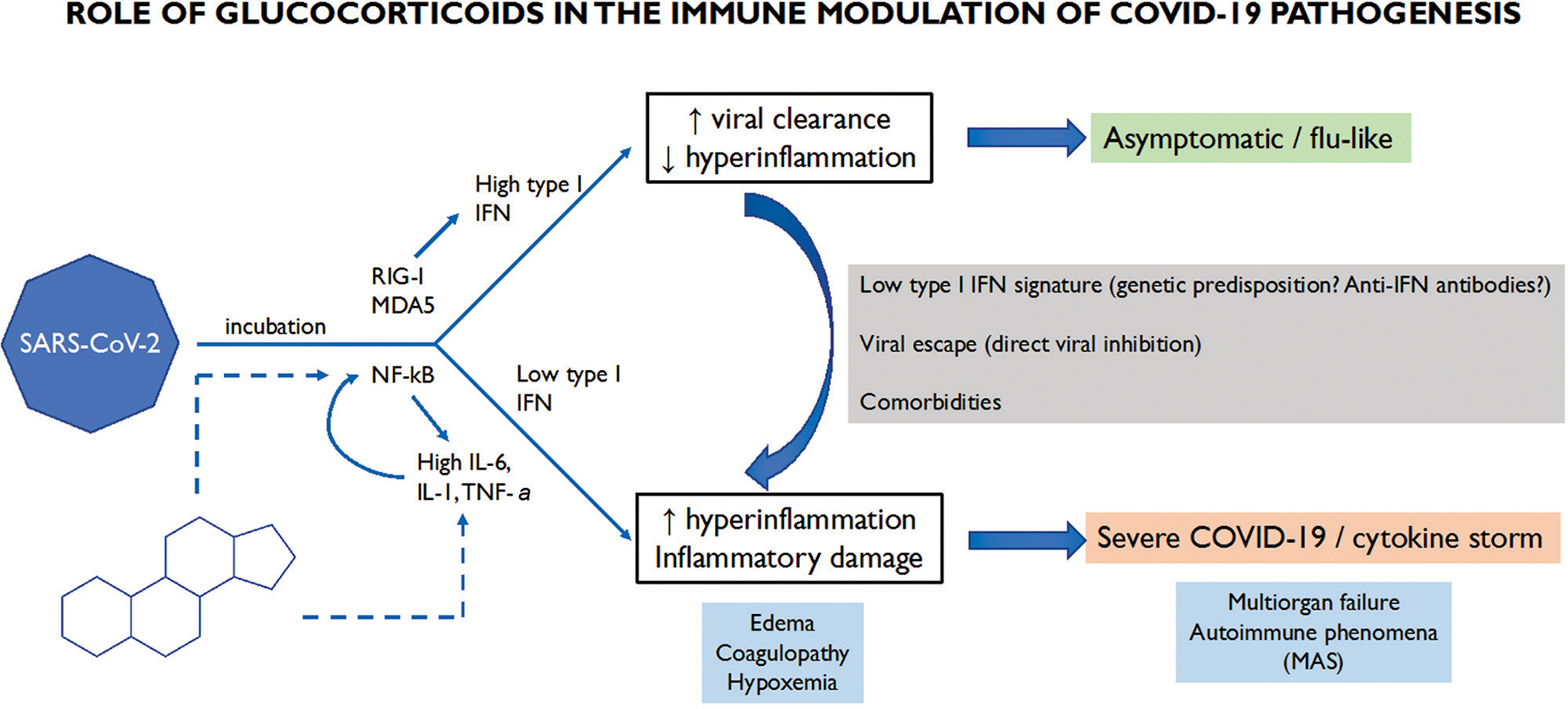
Immune pathogenesis of SARS-CoV-2 infection and possible therapeutic targets for the rationale of glucocorticoids employment. A type I IFN response is elicited by SARS-CoV-2 and contributes to viral clearance, leading to mild forms of the infection. In patients with a low type I IFN response, NF-kB activation predominates, culminating in the production of great amounts of inflammatory cytokines (i.e., IL-6, IL-1, and TNF-α) which in turn amplify the mechanism of NF-kB-mediated inflammation. This exuberant inflammatory response leads to hyperinflammatory syndrome, severe COVID-19, and cytokine storm. Glucocorticoids inhibit NF-kB activation, thus attenuating this harmful and dysregulated inflammatory response (Dashed arrows stand for inhibition). COVID-19, coronavirus disease 2019; IFN, interferons; IL, interleukin; MAS, macropahge activating syndrome; SARS-CoV-2, severe acute respiratory syndrome coronavirus-2.
From Pathophysiology to Therapy: Inflammation as a “Treatable Trait”
At the beginning of the pandemic, a three-phase model of COVID-19 pathogenesis has been proposed.67 In the first stages of infection, viral damage predominates, with low systemic inflammation. Effective treatment can be achieved with antiviral agents, and judicious glucocorticoid administration should be advised. Opposite, late stages of disease become more independent from viral replication, while systemic inflammatory response predominates and, sometimes, culminates into overt cytokine storm. Immunomodulatory therapy is warranted in late stages in which it may improve outcomes.
The entity of the individual patient’s immune response can be evaluated through laboratory biomarkers, and has been described as a determinant of morbidity and mortality in COVID-19.68 Endotypes are disease subsets characterized by common identifiable pathophysiological mechanisms through biomarkers, which are likely targetable by specific therapies. Four different endotypes have been recently described in hospitalized patients with COVID-19, based on laboratory data. Such type of approach should divide hospitalized cases of SARS-CoV-2 infection into different categories corresponding to different pathogenic mechanisms, different prognosis, and, perhaps, different response totherapies.69 Moreover, two distinct pheno-endotypes of SARS-CoV-2-related ARDS have been individuated: type 1 is characterized by a strong hyperinflammatory response, and is likely to benefit from immunosuppressive therapies, while coagulopathy and end-organ disfunction are the hallmarks of type 2, with minor contribution of inflammation.70 Thus, cytokine profiling could be useful to identify two different endotypes in patients with COVID-19: a hyperinflammatory endotype which is supposed to benefit from immunosuppressive drugs and a hypoinflammatory endotype.71,72
A treatable trait is a therapeutic target identified as a phenotype or endotype through validated biomarkers.73 An endotype-based treating approach could help selecting patients who could most benefit from corticosteroid (or other immunosuppressive) therapy. Thus, the degree of inflammatory response might constitute a treatable trait in patients with SARS-CoV-2 infection, and a precision medicine-based approach might improve outcomes, other than leading to a better targeting of resources. There is a need to classify patients into different pheno- and endotypes who could benefit from glucocorticoids in different measures. Furthermore, the pathogenesis of SARS-CoV-2 infection is much complex, undergoing different stages with different consequences on the immune system, so that glucocorticoid administration might result in different outcomes depending on timing, disease phase, and immune status.67,74 Multidisciplinary team discussion could help improving outcomes, especially in those patients who may benefit from immunomodulation, despite not fulfilling current criteria for steroid initiation.75 It is noteworthy to mention that the clinical application of corticosteroids might be limited by their adverse effects, such as hyperglycemia, arterial hypertension, osteoporosis, and myopathy.60,61,76
Current Evidence on Glucocorticoids in COVID-19
Systemic glucocorticoids are widely administered in patients with SARS-CoV-2 infection, and current guidelines recommend their use in patients with COVID-19 and hypoxemia.12 ►Table 3 summarizes the main RCTs regarding the use of glucocorticoids in COVID-19.77–91 Several RCTs have proven the efficacy and safety of corticosteroids in COVID-19.77–82 However, several factors should be considered.
Table 3.
RCT evaluating the use of glucocorticoids in COVID-19
| Study, year, journal | Study design | Drug and dose | Sample size | Inclusion criteria | Primary outcome | Results (primary outcome) | Results (secondary outcomes) | Significant adverse effects |
|---|---|---|---|---|---|---|---|---|
| Les et al 2022, Front Med (Lausanne)83 | Double-blind, placebo controlled, parallel design RCT 1:1 | MP (120 mg for 3 d) vs. placebo | 71 | Adult At least one: CRP > 60 mg/L, IL-6 > 40 pg/mL, ferritin> 1000 μg/L Not on respiratory insufficiency, not if SpO2 <94% | Treatment failure: death, ICU admission, initiation of MV, or clinical worsening up to 14 d post-randomization | Not achieved. 10 (29.4) in MP vs. 1027 in placebo group (p = 0.823) |
No differences in mortality, ICU admission at 28 d, need for high-flow oxygen therapy, radiological worsening and length of hospital stay. | Decompensated diabetes 9 (26.5%) in MP group (26.5) vs. 2 (5.4%) in placebo group (p = 0.021). Infection other than COVID-19 more common in placebo group |
| Maskin et al 2022, J Intensive Care Med84 | Multicenter, open-label RCT 1:1 | DXM (1 6 mg qd for 5 d, then 8 mg qd for 5 d) vs. DXM (6 mg qd for 10 d) | 100 | Adults ARDS due to SARS-CoV-2 Less than 72 h of MV |
Ventilator-free days at 28 d | No differences. 0 (0–1) d in the high dose vs. 0 (0–14) d in the low dose group (p = 0.231) |
No difference in total time on MV, ICU mortality, ICU length of stay, in-hospital mortality, hospital length of stay, mortality at 28 d, mortality at 90 d. | No significant differences |
| Toroghi et al 2022, Pharmacol Rep85 | Three-arm, single blind, RCT 1:1:1 | DXM (8 mg qd vs. 8 mg bid vs. 8 mg tid; for 10 d or until hospital discharge) | 144 | Adult Oxygen therapy | Time to clinical response | Reduced with lower doses. 4.3 ± 1.9 d in 8 mg qd vs. 5.3 ± 2.0 d in 8 mg bid vs. 6.1 ±3.3 d in 8 mg tid group (p = 0.025) | No difference in time to 50% decrease in serum CRP, time to respiratory rate ≤20, time to SpO2≥ 93%, need for MV, duration of MV, duration of hospital stay, need for ICU admission, duration of ICU stay, hospital readmission, 60-d mortality. | Infections more common in high-dose group |
| COVID STEROID 2 Trial Group, 2021, JAMA86 | Parallel group, stratified, blinded, RCT 1:1 | DXM (1 2 mg qd vs. 6 mg qd) | 1000 | Adult Hospitalized Oxygen ≥ 10 L/min or Nl MV or CPAP or IMV | Number of days alive without life support (IMV, circulatory support, kidney replacement therapy) at 28 d after randomization | No difference. 22.0 (6.0–28.0) d in the 12 mg vs. 20.5 (4.0–28.0) d in the 6 mg group, mean difference 1.3 (0–2.6) d (p = 0.07) |
No difference in number of days alive without life support and number of days alive out of hospital at 90 d, mortality at day 28 and at day 90, serious adverse reactions. | No significant differences |
| Ghanei et al 2021, Respir Res77 | Three-arm, open-label, RCT 1:1:1 | PDN (25 mg gd) + HCQ+AZT +naproxen (A) vs HCQ+AZT +naproxen (B) vs HCQ + lopinavir/ritonavir (C) |
352 | Age ≥ 16 years old SpO2 < 94% | Number of admissions to ICU | No difference. 1 admission in the (A) vs. 3 admissions in the (B) vs. 4 admissions in the (C)group (p = 0.27) |
Length of hospital stay significantly reduced in the PDN group No difference in mortality and intubation. |
No significant differences |
| Munch et al 2021, Acta Anaesthesiol Scand87 | Parallel-group, placebo-controlled, blinded, RCT 1:1 | HCS (200 mg qd for 7 d) vs. placebo | 30 | Adult Requiring IMV or NIMVor CPAPor oxygen ≥ 10 L/min | Days alive without life support (IMV, circulatory support, renal replacement therapy) at day 28 | No difference. 7 (2.24) in the HCS vs. 10 (3.26) in the placebo group, mean difference −1.1 (−9.5 to 7.3) d (p = 0.79) |
No difference in all-cause mortality at day 28 and 90, days alive without life support and days alive and out of hospital at day 90. | No significant differences |
| Horby et al 2021, N Engl J Med78 | Open-label, RCT 2:1 | DXM (6 mg qd, oral or iv) vs. standard of care | 6425 | Adult Hospitalized | All-cause mortality at day 28 | Reduced in DXM arm. 482/2104 (22.9) deaths in DXM vs. 1110/4321 (25.7) deaths in the standard of care group (RR 0.83 [0.75–0.93]) |
DXM associated with discharge from hospital within 28 d], reduced IMV requirement, IMV cessation, reduced need for renal replacement therapy. | No significant differences 4 serious adverse events in the DXM arm |
| Jeronimo et al, 2021, Clin Infect Dis88 | Parallel, double-blind, placebo-controlled, phase lib, RCT 1:1 | MP (0.5 mg/kg bid) vs. placebo | 416 | Adult Hospitalized One among: SpO2 ≤ 94% in room air; oxygen requirement; IMV requirement | Mortality at day 28 | No difference. 76/199 (38.2) in MP vs. 72/194 (37.1) in standard of care group (HR 0.924 (0.669–1.275), p = 0.629) |
No difference in mortality at day 7 and 14, nasal swab RT-PCR positive at day 5 and 7, need for IMV at day 7, P/F <100 at day 7, pulmonary fibrosis and BOOPafterday 7, positive blood culture on day 7, need for insulin therapy at day 28, sepsis at day 28, length of hospitalization. | N.A. |
| Corral-Gudino et al 2021, Wien Klin Wochenschr.82 | Open-label, controlled, two-arm, parallel-group RCT 1:1 | MP (40 mg bid for 3 d, then 20 mg bid for 3 d) vs. placebo | 64 | Adult Symptoms ≥ 7 d Lung disease on chest imaging P/F <300 or SaO2/F <400 or at least two criteria of the BRESCIA-COVID Respiratory Severity Scale Any of: CRP > 15 mg/dL, D-dimer > 800 ng/mL, ferritin > 1,000 mg/dL, or IL-6 > 20 pg/mL |
composite endpoint: in-hospital all-cause mortality, ICU admission, NIMV requirement | Reduced occurrence of the composite endpoint in MP group 30% in MP vs. 50% in placebo group, absolute difference 20% (RR 0.42 (95% Cl 0.20–0.89), p = 0.043) | N.A. | No significant differences |
| Dequin et al, 2020, JAMA89 | Sequential, double-blind, RCT 1:1 | HCS (200 mg qd continuous infusion for 7 d, then 100 mg qd for 4 d, then 50 mg qd for3 d) vs. placebo If improvement at day 4 (spontaneous breath, P/F> 200, SOFA score on day 4 ≤day 1, strong probability of being discharged from ICU before day 14), short regimen was used (8 d) | 149 | Adult ICU One of: need for PEEP ≥ 5 mm Hg; P/F <300 on high-flow oxygen with FiO2 ≥ 50%; P/F <300 if reservoir mask; Pulmonary Severity Index >130 | Treatment failure on day 21 (death or persistent dependency on MV or high-flow oxygen therapy) | No difference. 32/76 (42.1) in HCS vs. 37/73 (50.7) in placebo group, mean difference −8.6 (−24.9–7.7) (p = 0.29) | No difference in endotracheal intubation, need for prone position, need for ECMO, need for inhaled nitric oxide, nosocomial infections at day 28, death on day 21. | No significant differences 3 serious adverse effects with HCS. |
| Tomazini et al, 2020, JAMA79 | Open-label, RCT 1:1 | DXM (20 mg qd for 5 d, then 10 mg qd for 5 d) vs. standard of care | 299 | Adult Receiving MV within 48 h of meeting criteria for moderate-severe ARDS (P/F ≤200) | Ventilator-free days during the first 28 d | DXM reduced ventilator-free days. 6.6 (5.0–8.2) in DXM vs. 4.0 (2.9–5.4) in standard of care group, mean difference 2.26 (0.2–4.38) d (p = 0.04) |
DXM reduced SOFA score at day 7. No difference in 6-point ordinal scale at day 28, mortality at day 28, ICU free days, MV duration days, SOFA score at 48 h, SOFA score at 72 h. |
No significant differences |
| Angus et al 2020, JAMA80 | Open-label, RCT 1:1:1 | HCS (50 or 100 mg q6h) vs. HCS (50 mg q6h only if shock vs.) no-HCS | 403 | Adult ICU IMVor NIMVor high-flow NC ≥30 F/min, FiO2 40% or vasopressors or inotropes | Days free from respiratory or cardiovascular support at day 21 | No difference. 0 (−1 to 15) in fixed-dose vs. 0 (−1 to 13) in shock-dependent vs. 0 (−1 to 11) in no-HCS group |
No difference in in-hospital mortality, time to death, respiratory support free days, cardiovascular organ support free days, length of ICU stay, length of hospital stay, WHO scale at day 14, progression to intubation/ECMO/ death in those not intubated at baseline. | No significant differences 2 serious adverse events in the fixed-dose group |
| Edalatifard et al, 2020, EurRespirJ81 | Single-blind, parallel, RCT 1:1 | MP (250 mg qd per 3 d) vs. standard of care | 68 | Adult SpO2 < 90% Elevated CRP and IL-6 | Time to improvement, time to discharge,and timeto death | Reduction in time to discharge/death in MP group. 11.62 ±4.81 d in MP vs. 17.61 ±9.84 d in standard of care group (p = 0.006) Reduction in time to improvement in MP group. 11.84 ±4.88 d in MP vs. 16.44 ±6.93 d in standard of care group (p = 0.011) Outcome (p <0.001): Recovery 32 (94.1) in MP vs. 16 (57.1) in standard of care group Death 2 (5.9) in MP vs. 12 (42.9) in standard of care group |
Significant improvement at day 3 and at discharge/death in the MP group for: Borg score, SpO2, SBP, heart rate, respiratory rate, body temperature, gastrointestinal symptoms, myalgia, chest pain, cough, need for oxygen therapy. | No significant differences |
| Tang et al, 2021, Respiration90 | Single-blind, RCT 1:1 | MP (1 mg/kg qd) vs. placebo | 86 | Adult Pneumonia at chest CT Admitted < 72 h to general ward | Clinical deterioration at day 14 | No difference. 2 (4.8) in MP vs. 2 (4.8) in placebo group (OR 1 (0.134–7.442), p = 1.000) |
No difference in clinical cure at day 14, time to clinical cure, ICU admission, hospitalization duration, in hospital mortality. | Increased time (days) to virus shedding in the MP [11 (6–1 6)] vs. placebo [8 (2–12)] (p = 0.030) |
| Ranjbar et al, 2021, BMC Infect Dis91 | Stratified, triple-blind, RCT 1:1 | MP (2 mg/kg qd for 10 d) vs. DXM (6 mg qd for 10 d) | 86 | Adult Hospitalized SpO2 <92% | All-cause mortality at day 28 Clinical status after 5 and 10 d after enrollment (9-point WHO ordinal scale) |
No difference in mortality. 8 (18.6) in MP vs. 15 (37.5) in DXM group (p = 0.076) Clinical status at day 5 improved in the MP arm. 4.02 (1.64) in MP vs. 5.21 (1.733) in DXM group (p = 0.002) Clinical status at day 10 improved in the MP arm. 2.90 (2.42) in MP vs. 4.71 (2.35) in DXM group (p = 0.001) |
Reduced need for IMV (p = 0.040) and duration of hospital stay (p = 0.01 5) in the MP arm. | N.A. |
Abbreviations: ARDS, acute respiratory distress syndrome; AZT, azithromycin; bid, twice a day; BOOP, bronchiolitis obliterans-organizing pneumonia; CPAP, continuous positive airway pressure; CRP, C-reactive protein; CT, computed tomography; DXM, dexamethasone; ECMO, extracorporeal membrane oxygenation; FiO2, fraction of inspired oxygen; HCQ, hydroxychloroquine; HCS, hydrocortisone; HR, hazard ratio; ICU, intensive care unit; IL-6, interleukin-6; IMV, invasive mechanical ventilation; iv, intravenous; MP, methylprednisolone; MV, mechanical ventilation; N.A., not applicable; NC, nasal canula; NIH, national institute of health; NIMV, noninvasive mechanical ventilation; OR, odds ratio; P/F, arterial oxygen partial pressure out of FiO2; PDN, prednisolone; PEEP, positive end-expiratory pressure; qd, once a day; RCT, randomized controlled trial; RR, risk ratio; RT-PCR, real time polymerase chain reaction; SBP, systolic blood pressure; SOFA, sequential organ failure assessment score; SpO2, peripheral oxygen saturation; tid, thrice a day; WHO, world health organization.
First, different outcomes were analyzed in different studies. The RECOVERY trial demonstrated a clear benefit in reducing 28-day mortality in hospitalized patients with respiratory failure due to SARS-CoV-2 infection receiving dexamethasone 6 mg daily. Favorable outcomes were observed even when steroid therapy was initiated after 7 days from the beginning of clinical symptoms, and this might confirm the hypothesis of a prominent inflammatory component in later phases of the disease.67,78 Instead, such difference in mortality was not reported in a smaller cohort in which, however, a subgroup analysis demonstrated clinical improvement from glucocorticoids in older patients with more pronounced systemic inflammation. Moreover, in the same study, the length of treatment was much shorter than in the RECOVERYprotocol.88 Other clinical trials explored the impact of steroid therapy in preventing or reducing measures of clinical failure (e.g., proportion or time to intensive care unit [ICU] admission, requirement for life support after an established time point, etc.). However, there was much heterogeneity in the definition of end points among different research groups.77,79–83,87,89,90 In two cohorts, glucocorticoid administration reduced the need for intensive care, respiratory, or cardiovascular support. In both cases, no difference in mortality could be observed.79,80 In one study, methylprednisolone reduced the risk of severe respiratory failure and ARDS occurrence in nonventilated patients with SARS-CoV-2 pneumonia and intense systemic inflammatory response.82 Conversely, treatment failure was equally distributed between the steroid and nonsteroid arms in other clinical trials.77,87,89
Second, inclusion criteria are mainly based on clinical severity. With the exception of three RCTs,78,83,90 all the other studies included the need or degree of respiratory support as an inclusion criterion. Data from the RECOVERY trial suggested no clinical benefit from dexamethasone administration in patients who did not require oxygen supplementation.78 These results were recently confirmed in a small cohort: given at pulse doses, methylprednisolone failed in reducing mortality, preventing clinical worsening or respiratory insufficiency in patients with baseline oxygen saturation (SpO2)≥ 94%. The authors hypothesized that this patient phenotype could exhibit a better prognosis. However, no data are available on patients with SpO2 values between 90 and 93%.83 Severity of COVID-19 was assessed based on clinical data and only three studies considered the degree of systemic inflammation (e.g., serum C-reactive protein and IL-6) as an inclusion criterion.81–83 Indeed, inflammation could be regarded as a “treatable trait” in patients with SARS-CoV-2 infection.73 An endotyping approach based on inflammatory biomarkers might help to stratify patients into subgroups that are likely (or not) to benefit from steroids, independent from other clinical features or oxygen requirement.71 Glucocorticoid administration was associated with decreased mortality in a high-inflammatory subtype of COVID-19-related ARDS. This was not observed in patients with a hypo-inflammatory disease.92 Moreover, corticosteroid exposure was associated with a trend toward increased mortality in the hypo-inflammatory phenotype.60 In an RCT, an early biomarker-guided steroid dosing strategy led to an increase in oxygen-free days and hospital-free days; also, there was a concurrent reduction in cumulative steroid exposure.93
Third, few studies have compared among different dosages of corticosteroids in patients with SARS-CoV-2 infection.84–86 The large COVID STEROID 2 trial failed in demonstrating a reduction in time alive without support in patients receiving 12 mg daily of dexamethasone, compared with a 6 mg daily dosage. Notwithstanding, higher doses might be associated with reduced mortality at 28 and 90 days, without significant differences in terms of adverse effects.86 Even at a 180-day follow-up, there was a tendency toward better outcomes in patients receiving 12 mg daily, even in the absence of a significant difference in mortality or health-related quality of life.94 Recently, Maskin and colleagues described a reduction in time of weaning from ventilator in a cohort of patients with SARS-CoV-2-associated ARDS treated with high-dose steroids, even in the absence of significant mortality reduction. The incidence of adverse events did not differ between the two arms of the study.84 However, no clinical advantage was observed with high doses of dexamethasone in another cohort, while lower doses seemed to reduce time to clinical response, 60-day mortality, and infectious risk.85 Methylprednisolone, administered at 1 mg/kg daily, delayed time to viral clearance in a small population, but this was not associated with clinical deterioration.90 Favorable results were obtained with corticosteroids given at boluses in early phases of disease in patients requiring oxygen and with elevated inflammatory biomarkers,81 whereas there was no clear benefit in those without respiratory insufficiency.83 So far, there is no unique opinion on which steroid dosage could optimize the cost-to-benefit ratio, and further research is required on this topic. Inflammation-based endotyping might be helpful in choosing the right doses of glucocorticoids for patients with COVID-19. Moreover, such a precision-medicine approach may guide clinicians in deciding the most appropriate duration of anti-inflammatory therapy, also improving the cost-to-benefit ratio.
Fourthly, different molecules were tested in the aforementioned studies; since there is great variability in terms of glucocorticoid and mineralocorticoid activity among such compounds,95 this could partially explain the heterogeneity of results. One study compared methylprednisolone, given at 2 mg/kg daily, and dexamethasone, 6 mg/kg daily, for 10 days. The former molecule was superior to the latter in reducing all-cause mortality at 28 days and was associated with a higher proportion of clinical improvement in the short term and reduced the length of hospital stay. However, if we consider equivalent dosages, patients on methylprednisolone received a much higher dose of corticosteroids than patients in the dexamethasone arm. This could explain the more favorable outcomes seen in the methylprednisolone group.91 Further research is required to determine which steroid compound may offer the greatest benefits in patients affected by COVID-19. Moreover, pharmacokinetics and pharmacodynamics of corticosteroids are still widely unexplored. Nongenomic effects, which may account at least partially for their role in case of hyperinflammatory states (e.g., cytokine storm),60 remain largely unknown.
Fifthly, data on long-term outcomes are scarce. Since SARS-CoV-2 infection can be associated with high mortality in the acute phase,96 the majority of clinical trials have analyzed the short-term effectiveness of glucocorticoids. However, COVID-19 has been associated with a multitude of chronic sequelae and, even if practice guidelines have been proposed,97 no consensus exists on how to approach “long COVID” syndrome. Long-term effects of steroid therapy have been in part described during the follow-up of the COVID STEROID 2 cohort. The study aimed at comparing the effect of two different dosages of glucocorticoid therapy. No significant difference was found in terms of mortality or quality of life change between patients who were administered high (12 mg daily) versus low (6 mg daily) doses of dexamethasone, but a tendency toward favoring higher dosages was described. “Long-term” follow-up was defined to be at 180 days after initial infection.94 In another small population, methylprednisolone did not influence the incidence of post-COVID interstitial lung disease, in terms of organizing pneumonia and fibrosis.53 However, these data may have been affected by inadequate sample size.88 Currently, no RCT has explored long-term outcomes in patients undergoing steroid therapy for COVID-19. Moreover, there is paucity of data on pulmonary (functional disorders and radiologic stigmata) and systemic sequelae, for which steroid and/or immunosuppressive therapy could be conceivable. Efforts must be given to understand which patients are at risk of developing pulmonary and/or systemic complications from SARS-CoV-2 infection, how these could be prevented and, in case they are established, how they should be treated.
Lastly, no significant difference was reported in the incidence of glucocorticoid-related adverse events in the trials. In the RECOVERY study, which included the largest population sample, four serious events were reported: hyperglycemia (n = 2), gastrointestinal bleeding (n = 1), and psychosis (n = 1).78 In another study cohort, methylprednisolone seemed to increase by 3 days the time from virus shedding, but the finding was not associated with significant clinical differences.90
Thus, corticosteroid utilization in COVID-19 is still an area of uncertainty. There has been much heterogeneity in the type of corticosteroid, dosing, timing of initiation, duration, and route of administration of steroid therapy in patients with SARS-CoV-2 infection, and the most effective approach yet needs to be clarified. Moreover, different outcomes have been explored in various RCTs and this contributes to difficulty in translating the results into real-life practice. Further research is required to individualize steroid therapy in patients with COVID-19, based on the integration of clinical features, radiologic patterns, and biomarkers. Thus, a role for computational scores is desirable. Biomarkers should be representative of the underlying disease pathogenesis,98 so that therapies could be tailored on different phenotypes and endotypes, as well as targeted against ultimate disease mechanisms. Artificial intelligence has shown promising results in the field of COVID-19 detection and diagnosis,99 and could be applied into models for evaluating prognosis and predicting response to therapies. Infections have been widely reported as complications of steroid therapy,100 and high doses of glucocorticoids have been associated with such risk in patients with COVID-19.85 Efforts are required to optimize immunosuppressive therapy in this subset of patients, to balance protective and harmful effects, in an antimicrobial stewardship approach. Finally, few data are available on the role of glucocorticoid therapy in patients with long-term consequences of SARS-CoV-2 infection in terms of (1) efficacy to reduce the incidence of sequelae, and (2) eventual therapeutic role in the “long COVID” setting. ►Table 4 summarizes the main unmet needs in clinical research on the role of glucocorticoids in COVID-19.
Table 4.
Outstanding clinical and research questions concerning glucocorticoids in COVID-19
| Unmet needs | Research questions |
|---|---|
| Molecule | 1. Which molecule should be used? 2. What is the best dosage? 3. What is the best route of administration? |
| Patients’ profiling | 1. Which phenotypes predict good response to glucocorticoids? 2. Which endotypes predict good response to glucocorticoids? (i.e., what are the inflammatory mechanisms that can be targeted to improve outcomes?) |
| Timing | 1. What is the correct timing of initiation? 2. How long should it be administered? |
| Effects | 1. What are the expected short-term effects? 2. How to monitor for short-term effects? 3. Which phenotypes/endotypes are predictors of short-term effects or failure? 4. What are the expected long-term effects? 5. How to monitor for long-term effects? 6. Which phenotypes/endotypes are predictors of long-term effects or failure? |
| Adverse events | 1. Which are the most common? 2. Which are the most severe? 3. How to monitor for adverse events? 4. Who is at highest risk of adverse events? |
Conclusion
Inflammation has been proposed as a potential therapeutic target in pneumonia and, in particular, COVID-19 pneumonia. Systemic corticosteroids are widely used in the treatment of several inflammatory diseases. However, conflicting data have been reported in case of CAP and ARDS and further RCTs are needed to clarify their role in these conditions. Systemic glucocorticoids are widely administered in patients with SARS-CoV-2 infection, and current guidelines recommend their use in patients with hypoxemia due to COVID-19. Several aspects should be clarified in patients with SARS-CoV-2 infection such as the type of corticosteroid, dosing, timing of initiation, duration, and route of administration of steroid therapy. Further research is required to individualize steroid therapy in patients with COVID-19, based on the integration of clinical features, radiologic patterns, and biomarkers.
Footnotes
Conflict of Interest
None declared.
References
- 1.Feldman C, Anderson R. Pneumonia as a systemic illness. Curr Opin Pulm Med 2018;24(03):237–243 [DOI] [PubMed] [Google Scholar]
- 2.Mizgerd JP. Inflammation and pneumonia: why are some more susceptible than others? Clin Chest Med 2018;39(04):669–676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cazzola M, Matera MG, Pezzuto G. Inflammation – a new therapeutic target in pneumonia. Respiration 2005;72(02):117–126 [DOI] [PubMed] [Google Scholar]
- 4.Adcock IM, Mumby S. Glucocorticoids. Handb Exp Pharmacol 2017;237:171–196 [DOI] [PubMed] [Google Scholar]
- 5.Huang L, Gao X, Chen M. Early treatment with corticosteroids in patients with Mycoplasma pneumoniae pneumonia: a randomized clinical trial. J Trop Pediatr 2014;60(05):338–342 [DOI] [PubMed] [Google Scholar]
- 6.Bozzette SA, Sattler FR, Chiu J, et al. ; California Collaborative Treatment Group. A controlled trial of early adjunctive treatment with corticosteroids for Pneumocystis carinii pneumonia in the acquired immunodeficiency syndrome. N Engl J Med 1990;323(21):1451–1457 [DOI] [PubMed] [Google Scholar]
- 7.Lansbury L, Rodrigo C, Leonardi-Bee J, Nguyen-Van-Tam J, Lim WS. Corticosteroids as adjunctive therapy in the treatment of influenza. Cochrane Database Syst Rev 2019;2:CD010406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Marti C, Grosgurin O, Harbarth S, et al. Adjunctive corticotherapy for community acquired pneumonia: a systematic review and meta-analysis. PLoS One 2015;10(12):e0144032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gandhi RT, Lynch JB, Del Rio C. Mild or moderate COVID-19. N Engl J Med 2020;383(18):1757–1766 [DOI] [PubMed] [Google Scholar]
- 10.Berlin DA, Gulick RM, Martinez FJ. Severe COVID-19. N Engl J Med 2020;383(25):2451–2460 [DOI] [PubMed] [Google Scholar]
- 11.Soy M, Keser G, Atagündüz P, Tabak F, Atagündüz I, Kayhan S. Cytokine storm in COVID-19: pathogenesis and overview of anti-inflammatory agents used in treatment. Clin Rheumatol 2020;39(07):2085–2094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chalmers JD, Crichton ML, Goeminne PC, et al. Management of hospitalised adults with coronavirus disease 2019 (COVID-19): a European Respiratory Society living guideline. Eur Respir J 2021; 57(04):2100048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.van de Veerdonk FL, Giamarellos-Bourboulis E, Pickkers P, et al. A guide to immunotherapy for COVID-19. Nat Med 2022;28(01):39–50 [DOI] [PubMed] [Google Scholar]
- 14.Metlay JP, Waterer GW, Long AC, et al. Diagnosis and treatment of adults with community-acquired pneumonia. An Official Clinical Practice Guideline of the American Thoracic Society and Infectious Diseases Society of America. Am J Respir Crit Care Med 2019;200(07):e45–e67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wittermans E, Vestjens SMT, Spoorenberg SMC, et al. ; Santeon-CAP Study Group Members of the Santeon-CAP Study Group. Adjunctive treatment with oral dexamethasone in non-ICU patients hospitalised with community-acquired pneumonia: a randomised clinical trial. Eur Respir J 2021;58(02):2002535. [DOI] [PubMed] [Google Scholar]
- 16.Torres A, Sibila O, Ferrer M, et al. Effect of corticosteroids on treatment failure among hospitalized patients with severe community-acquired pneumonia and high inflammatory response: a randomized clinical trial. JAMA 2015;313(07):677–686 [DOI] [PubMed] [Google Scholar]
- 17.Blum CA, Nigro N, Briel M, et al. Adjunct prednisone therapy for patients with community-acquired pneumonia: a multicentre, double-blind, randomised, placebo-controlled trial. Lancet 2015;385(9977):1511–1518 [DOI] [PubMed] [Google Scholar]
- 18.Meijvis SCA, Hardeman H, Remmelts HHF, et al. Dexamethasone and length of hospital stay in patients with community-acquired pneumonia: a randomised, double-blind, placebo-controlled trial. Lancet 2011;377(9782):2023–2030 [DOI] [PubMed] [Google Scholar]
- 19.Fernández-Serrano S, Dorca J, Garcia-Vidal C, et al. Effect of corticosteroids on the clinical course of community-acquired pneumonia: a randomized controlled trial. Crit Care 2011;15(02):R96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Snijders D, Daniels JMA, de Graaff CS, van der Werf TS, Boersma WG. Efficacy of corticosteroids in community-acquired pneumonia: a randomized double-blinded clinical trial. Am J Respir Crit Care Med 2010;181(09):975–982 [DOI] [PubMed] [Google Scholar]
- 21.Mikami K, Suzuki M, Kitagawa H, et al. Efficacy of corticosteroids in the treatment of community-acquired pneumonia requiring hospitalization. Lung 2007;185(05):249–255 [DOI] [PubMed] [Google Scholar]
- 22.Confalonieri M, Urbino R, Potena A, et al. Hydrocortisone infusion for severe community-acquired pneumonia: a preliminary randomized study. Am J Respir Crit Care Med 2005;171(03):242–248 [DOI] [PubMed] [Google Scholar]
- 23.Briel M, Spoorenberg SMC, Snijders D, et al. ; Ovidius Study Group Capisce Study Group STEP Study Group. Corticosteroids in patients hospitalized with community-acquired pneumonia: systematic review and individual patient data meta-analysis. Clin Infect Dis 2018;66(03):346–354 [DOI] [PubMed] [Google Scholar]
- 24.Stern A, Skalsky K, Avni T, Carrara E, Leibovici L, Paul M. Corticosteroids for pneumonia. Cochrane Database Syst Rev 2017;12:CD007720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wu WF, Fang Q, He GJ. Efficacy of corticosteroid treatment for severe community-acquired pneumonia: a meta-analysis. Am J Emerg Med 2018;36(02):179–184 [DOI] [PubMed] [Google Scholar]
- 26.Wan YD, Sun TW, Liu ZQ, Zhang SG, Wang LX, Kan QC. Efficacy and safety of corticosteroids for community-acquired pneumonia: a systematic review and meta-analysis. Chest 2016;149(01):209–219 [DOI] [PubMed] [Google Scholar]
- 27.Diaz E, Martin-Loeches I, Canadell L, et al. ; H1N1 SEMICYUC-CIBERES-REIPI Working Group (GETGAG) Corticosteroid therapy in patients with primary viral pneumonia due to pandemic (H1N1) 2009 influenza. J Infect 2012;64(03):311–318 [DOI] [PubMed] [Google Scholar]
- 28.Siemieniuk RAC, Meade MO, Alonso-Coello P, et al. Corticosteroid therapy for patients hospitalized with community-acquired pneumonia: a systematic review and meta-analysis. Ann Intern Med 2015;163(07):519–528 [DOI] [PubMed] [Google Scholar]
- 29.Lee N, Wong CK, Chan PKS, et al. Cytokine response patterns in severe pandemic 2009 H1N1 and seasonal influenza among hospitalized adults. PLoS One 2011;6(10):e26050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Quispe-Laime AM, Bracco JD, Barberio PA, et al. H1N1 influenza A virus-associated acute lung injury: response to combination oseltamivir and prolonged corticosteroid treatment. Intensive Care Med 2010;36(01):33–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liem NT, Tung CV, Hien ND, et al. Clinical features of human influenza A (H5N1) infection in Vietnam: 2004–2006. Clin Infect Dis 2009;48(12):1639–1646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Brun-Buisson C, Richard JCM, Mercat A, Thiébaut ACM, Brochard LREVA-SRLFA/H1N1v 2009 Registry Group. Early corticosteroids in severe influenza A/H1N1 pneumonia and acute respiratory distress syndrome. Am J Respir Crit Care Med 2011;183(09):1200–1206 [DOI] [PubMed] [Google Scholar]
- 33.Wirz SA, Blum CA, Schuetz P, et al. ; STEP Study Group. Pathogen- and antibiotic-specific effects of prednisone in community-acquired pneumonia. Eur Respir J 2016;48(04):1150–1159 [DOI] [PubMed] [Google Scholar]
- 34.Zhang Y, Sun W, Svendsen ER, et al. Do corticosteroids reduce the mortality of influenza A (H1N1) infection? A meta-analysis. Crit Care 2015;19:46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yang JW, Fan LC, Miao XY, et al. Corticosteroids for the treatment of human infection with influenzavirus: a systematic review and meta-analysis. Clin Microbiol Infect 2015;21(10):956–963 [DOI] [PubMed] [Google Scholar]
- 36.Villar J, Ferrando C, Martínez D, et al. ; dexamethasone in ARDS network. Dexamethasone treatment for the acute respiratory distress syndrome: a multicentre, randomised controlled trial. Lancet Respir Med 2020;8(03):267–276 [DOI] [PubMed] [Google Scholar]
- 37.Tongyoo S, Permpikul C, Mongkolpun W, et al. Hydrocortisone treatment in early sepsis-associated acute respiratory distress syndrome: results of a randomized controlled trial. Crit Care 2016;20(01):329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Meduri GU, Golden E, Freire AX, et al. Methylprednisolone infusion in early severe ARDS: results of a randomized controlled trial. Chest 2007;131(04):954–963 [DOI] [PubMed] [Google Scholar]
- 39.Steinberg KP, Hudson LD, Goodman RB, et al. ; National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome (ARDS) Clinical Trials Network. Efficacy and safety of corticosteroids for persistent acute respiratory distress syndrome. N Engl J Med 2006;354(16):1671–1684 [DOI] [PubMed] [Google Scholar]
- 40.Meduri GU, Headley AS, Golden E, et al. Effect of prolonged methylprednisolone therapy in unresolving acute respiratory distress syndrome: a randomized controlled trial. JAMA 1998; 280(02):159–165 [DOI] [PubMed] [Google Scholar]
- 41.Bernard GR, Luce JM, Sprung CL, et al. High-dose corticosteroids in patients with the adult respiratory distress syndrome. N Engl J Med 1987;317(25):1565–1570 [DOI] [PubMed] [Google Scholar]
- 42.Villar J, Belda J, Añón JM, et al. ; DEXA-ARDS Network. Evaluating the efficacy of dexamethasone in the treatment of patients with persistent acute respiratory distress syndrome: study protocol for a randomized controlled trial. Trials 2016;17:342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Guan W-J, Ni Z-Y, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020;382(18): 1708–1720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lauer SA, Grantz KH, Bi Q, et al. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann Intern Med 2020;172(09):577–582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Oran DP, Topol EJ. Prevalence of asymptomatic SARS-CoV-2 infection: a narrative review. Ann Intern Med 2020;173(05):362–367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yin X, Riva L, Pu Y, et al. MDA5 governs the innate immune response to SARS-CoV-2 in lung epithelial cells. Cell Rep 2021;34(02):108628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hadjadj J, Yatim N, Barnabei L, et al. Impaired type I interferon activity and inflammatory responses in severe COVID-19 patients. Science 2020;369(6504):718–724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Brodin P Immune determinants of COVID-19 disease presentation and severity. Nat Med 2021;27(01):28–33 [DOI] [PubMed] [Google Scholar]
- 49.Parasher A COVID-19: current understanding of its pathophysiology, clinical presentation and treatment. Postgrad Med J 2021; 97(1147):312–320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Choudhary S, Sharma K, Silakari O. The interplay between inflammatory pathways and COVID-19: a critical review on pathogenesis and therapeutic options. Microb Pathog 2021; 150:104673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wiersinga WJ, Rhodes A, Cheng AC, Peacock SJ, Prescott HC. Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19): a review. JAMA 2020;324(08):782–793 [DOI] [PubMed] [Google Scholar]
- 52.Tan LY, Komarasamy TV, Rmt Balasubramaniam V. Hyperinflammatory immune response and COVID-19: a double edged sword. Front Immunol 2021;12:742941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Merad M, Blish CA, Sallusto F, Iwasaki A. The immunology and immunopathology of COVID-19. Science 2022;375(6585):1122–1127 [DOI] [PubMed] [Google Scholar]
- 54.Tonutti A, Motta F, Ceribelli A, Isailovic N, Selmi C, De Santis M. Anti-MDA5 antibody linking COVID-19, type I interferon, and autoimmunity: a case report and systematic literature review. Front Immunol 2022;13:937667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Fajgenbaum DC, June CH. Cytokine storm. N Engl J Med 2020;383(23):2255–2273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Rodríguez Y, Novelli L, Rojas M, et al. Autoinflammatory and autoimmune conditions at the crossroad of COVID-19. J Autoimmun 2020;114:102506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mehta P, Fajgenbaum DC. Is severe COVID-19 a cytokine storm syndrome: a hyperinflammatory debate. Curr Opin Rheumatol 2021;33(05):419–430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJHLH Across Speciality Collaboration, UK. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet 2020;395(10229):1033–1034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zhang W, Qin C, Fei Y, et al. Anti-inflammatory and immune therapy in severe coronavirus disease 2019 (COVID-19) patients: An update. Clin Immunol 2022;239:109022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.RhenT Cidlowski JA. Antiinflammatory action of glucocorticoids—new mechanisms for old drugs. N Engl J Med 2005;353(16): 1711–1723 [DOI] [PubMed] [Google Scholar]
- 61.Coutinho AE, Chapman KE. The anti-inflammatory and immunosuppressive effects of glucocorticoids, recent developments and mechanistic insights. Mol Cell Endocrinol 2011;335(01):2–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Panettieri RA, Schaafsma D, Amrani Y, Koziol-White C, Ostrom R, Tliba O. Non-genomic effects of glucocorticoids: an updated view. Trends Pharmacol Sci 2019;40(01):38–49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Lipworth BJ. Therapeutic implications of non-genomic glucocorticoid activity. Lancet 2000;356(9224):87–89 [DOI] [PubMed] [Google Scholar]
- 64.Czock D, Keller F, Rasche FM, Häussler U. Pharmacokinetics and pharmacodynamics of systemically administered glucocorticoids. Clin Pharmacokinet 2005;44(01):61–98 [DOI] [PubMed] [Google Scholar]
- 65.Meduri GU, Tolley EA, Chrousos GP, Stentz F. Prolonged methylprednisolone treatment suppresses systemic inflammation in patients with unresolving acute respiratory distress syndrome: evidence for inadequate endogenous glucocorticoid secretion and inflammation-induced immune cell resistance to glucocorticoids. Am J Respir Crit Care Med 2002;165(07):983–991 [DOI] [PubMed] [Google Scholar]
- 66.Wagner C, Griesel M, Mikolajewska A, et al. Systemic corticosteroids for the treatment of COVID-19. Cochrane Database Syst Rev 2021;8:CD014963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Siddiqi HK, Mehra MR. COVID-19 illness in native and immunosuppressed states: a clinical-therapeutic staging proposal. J Heart Lung Transplant 2020;39(05):405–407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wang X, Jehi L, Ji X, Mazzone PJ. Phenotypes and subphenotypes of patients with COVID-19: a latent class modeling analysis. Chest 2021;159(06):2191–2204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ranard BL, Megjhani M, Terilli K, et al. Identification of endotypes of hospitalized COVID-19 patients. Front Med (Lausanne) 2021;8:770343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ranjeva S, Pinciroli R, Hodell E, et al. Identifying clinical and biochemical phenotypes in acute respiratory distress syndrome secondary to coronavirus disease-2019. EClinicalMedicine 2021;34:100829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Amati F, Dela Cruz CS. One size does not fit all: moving towards a personalized approach for steroids in COVID-19. Chest 2021;159(05):1693–1695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Chen H, Xie J, Su N, et al. Corticosteroid therapy is associated with improved outcome in critically ill patients with COVID-19 with hyperinflammatory phenotype. Chest 2021;159(05):1793–1802 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Agusti A, Bel E, Thomas M, et al. Treatable traits: toward precision medicine of chronic airway diseases. Eur Respir J 2016;47(02):410–419 [DOI] [PubMed] [Google Scholar]
- 74.Liu Y, Li Y, Xu D, Zhang J, Peng Z. Severe COVID-19: immunosuppression or hyperinflammation? Shock 2021;56(02):188–199 [DOI] [PubMed] [Google Scholar]
- 75.Papadopoulou C, Al Obaidi M, Moraitis E, Compeyrot-Lacassagne S, Eleftheriou D, Brogan P. Management of severe hyperinflammation in the COVID-19 era: the role of the rheumatologist. Rheumatology (Oxford) 2021;60(02):911–917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Akter F, Araf Y, Hosen MJ. Corticosteroids for COVID-19: worth it or not? Mol Biol Rep 2022;49(01):567–576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ghanei M, Solaymani-Dodaran M, Qazvini A, et al. The efficacy of corticosteroids therapy in patients with moderate to severe SARS-CoV-2 infection: a multicenter, randomized, open-label trial. Respir Res 2021;22(01):245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Horby P, Lim WS, Emberson JR, et al. ; RECOVERY Collaborative Group. Dexamethasone in hospitalized patients with COVID-19. N Engl J Med 2021;384(08):693–704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Tomazini BM, Maia IS, Cavalcanti AB, et al. ; COALITION COVID-19 Brazil III Investigators. Effect of dexamethasone on days alive and ventilator-free in patients with moderate or severe acute respiratory distress syndrome and COVID-19: the CoDEX randomized clinical trial. JAMA 2020;324(13):1307–1316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Angus DC, Derde L, Al-Beidh F, et al. ; Writing Committee for the REMAP-CAP Investigators. Effect of hydrocortisone on mortality and organ support in patients with severe COVID-19: the REMAP-CAP COVID-19 corticosteroid domain randomized clinical trial. JAMA 2020;324(13):1317–1329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Edalatifard M, Akhtari M, Salehi M, et al. Intravenous methylprednisolone pulse as a treatment for hospitalised severe COVID-19 patients: results from a randomised controlled clinical trial. Eur Respir J 2020;56(06):2002808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Corral-Gudino L, Bahamonde A, Arnaiz-Revillas F, et al. ; GLUCOCOVID investigators. Methylprednisolone in adults hospitalized with COVID-19 pneumonia : an open-label randomized trial (GLUCOCOVID). Wien Klin Wochenschr 2021;133(7–8):303–311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Les I, Loureiro-Amigo J, Capdevila F, et al. Methylprednisolone pulses in hospitalized COVID-19 patients without respiratory failure: a randomized controlled trial. Front Med (Lausanne) 2022;9:807981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Maskin LP, Bonelli I, Olarte GL, et al. High- versus low-dose dexamethasone for the treatment of COVID-19-related acute respiratory distress syndrome: a multicenter, randomized open-label clinical trial. J Intensive Care Med 2022;37(04):491–499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Toroghi N, Abbasian L, Nourian A, et al. Comparing efficacy and safety of different doses of dexamethasone in the treatment of COVID-19: a three-arm randomized clinical trial. Pharmacol Rep 2022;74(01):229–240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Munch MW, Myatra SN, Vijayaraghavan BKT, et al. ; COVID STEROID 2 Trial Group. Effect of 12 mg vs 6 mg of dexamethasone on the number of days alive without life support in adults with COVID-19 and severe hypoxemia: the COVID STEROID 2 randomized trial. JAMA 2021;326(18):1807–1817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Munch MW, Meyhoff TS, Helleberg M, et al. Low-dose hydrocortisone in patients with COVID-19 and severe hypoxia: the COVID STEROID randomised, placebo-controlled trial. Acta Anaesthesiol Scand 2021;65(10):1421–1430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Jeronimo CMP, Farias MEL, Val FFA, et al. Methylprednisolone as adjunctive therapy for patients hospitalized with COVID-19 (Metcovid): a randomised, double-blind, phase IIb, placebo-controlled trial. Clin Infect Dis 2021;72(09):e373–e381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Dequin PF, Heming N, Meziani F, et al. ; CAPE COVID Trial Group and the CRICS-TriGGERSep Network. Effect of hydrocortisone on 21-day mortality or respiratory support among critically ill patients with COVID-19: a randomized clinical trial. JAMA 2020;324(13):1298–1306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Tang X, Feng YM, Ni JX, et al. Early use of corticosteroid may prolong SARS-CoV-2 shedding in non-intensive care unit patients with COVID-19 pneumonia: a multicenter, single-blind, randomized control trial. Respiration 2021;100(02):116–126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Ranjbar K, Moghadami M, Mirahmadizadeh A, et al. Methylprednisolone or dexamethasone, which one is superior corticosteroid in the treatment of hospitalized COVID-19 patients: a triple-blinded randomized controlled trial. BMC Infect Dis 2021;21(01):337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Sinha P, Furfaro D, Cummings MJ, et al. Latent class analysis reveals COVID-19-related acute respiratory distress syndrome subgroups with differential responses to corticosteroids. Am J Respir Crit Care Med 2021;204(11):1274–1285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Odeyemi YE, Chalmers SJ, Barreto EF, Jentzer JC, Gajic O, Yadav H. Early, biomarker-guided steroid dosing in COVID-19 pneumonia: a pilot randomized controlled trial. Crit Care 2022;26(01):9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Granholm A, Kjær MN, Munch MW, et al. Long-term outcomes of dexamethasone 12mg versus 6mg in patients with COVID-19 and severe hypoxaemia. Intensive Care Med 2022;48(05):580–589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Liu D, Ahmet A, Ward L, et al. A practical guide to the monitoring and management of the complications of systemic corticosteroid therapy. Allergy Asthma Clin Immunol 2013;9(01):30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020;395(10229):1054–1062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.COVID-19 rapid guideline: managing the long-term effects of COVID-19. London: National Institute for Health and Care Excellence (NICE); 2020. (National Institute for Health and Care Excellence: Clinical Guidelines). Accessed May 09, 2022, at: http://www.ncbi.nlm.nih.gov/books/NBK567261/ [Google Scholar]
- 98.Bivona G, Agnello L, Ciaccio M. Biomarkers for prognosis and treatment response in COVID-19 patients. Ann Lab Med 2021;41(06):540–548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Gudigar A, Raghavendra U, Nayak S, et al. Role of artificial intelligence in COVID-19 detection. Sensors (Basel) 2021;21(23):8045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Youssef J, Novosad SA, Winthrop KL. Infection risk and safety of corticosteroid use. Rheum Dis Clin North Am 2016;42(01):157–176, ix–x [DOI] [PMC free article] [PubMed] [Google Scholar]


