Summary
Looking at SRHR as an isolated set of elements, as is the current practice, does not do justice to the needs and rights of people and communities and may be one of the reasons why challenges remain in the attainment of SRHR for all. SRHR Infographic snapshots were developed for all 194 WHO Member States and included 120 indicators covering a broad range of policy, health systems and service delivery interventions. The snapshots were created using data less than 10 years old publicly available in data repositories maintained by international and global agencies. Data availability was not consistent across countries with low and lower-middle income countries having higher data availability (71%) compared to high income countries (40%). SRHR data that is easily accessible and consistently reported can improve accountability and opportunities for learning to improve people-centred approaches to accelerate the attainment of SRHR for all.
Keywords: Sexual and reproductive health and rights, National data, International databases, Data availability, Equity, Accountability
Search strategy and selection criteria.
Data for this Review were sourced from the WHO SRHR Infographic Snapshots 2021. The snapshots were created using publicly available national data from 2011 until 2021 sourced from data repositories maintained by international and global agencies: the Sustainable Development Goal (SDG) database, WHO Global Health Observatory, UNAIDS (Global AIDS Monitoring Database, Epidemiological estimates database, and Laws and Policies Analytics database), Demographic Health Survey Statcompiler, UNICEF, United Nations Statistics Division, United Nations Population Division, Guttmacher Institute, World Economic Forum, and the World Bank Group.
Introduction
Sexual and reproductive health and rights (SRHR) is a broad term that covers a range of aspects of health, gender, and human rights.1,2 Given the scope and complexity of SRHR, ranging from issues as diverse as unmet need for contraception, access to timely antenatal care, condom use, and reducing sexual violence experienced by women, data are often reported separately for each SRHR area at the national level.3 Yet, a single person has multiple SRHR needs and they often interact with one another, such as gender based violence and women's risk of HIV acquisition, condom use at last sex amongst adolescents and teenage pregnancy; and number of skilled health professionals, proportion of births attended by skilled birth personnel and maternal mortality.3, 4, 5 However, data are not always easily available for all countries to allow for comparisons and build on best practices. Given that more than half of the world's population continues to have limited or no access to sexual and reproductive health services over their lifetime, many health systems actions including access to quality data remain important to advance SRHR.5
The key argument in this Review is that more easily accessible and consistently reported sexual and reproductive health data can be used to support integrated, people-centred approaches to accelerate the attainment of SRHR for all.2
SRHR infographic snapshots
One of the core functions of the World Health Organization (WHO) is to monitor health situations and assess health trends, including by regularly compiling data for certain indicators from Member States. Given the dispersed nature of data reporting on SRHR, the 2021 SRHR infographic snapshots aimed to bring together existing data reported in international health datasets on some core elements of SRHR to support national policy makers, health programme managers and civil society advocates to easily see where good progress is being made and where there are gaps hindering progress.
Looking at SRHR as an isolated set of elements—as is the current practice—does not do justice to the needs and rights of people and communities and may be one of the reasons why challenges remain in the attainment of SRHR for all (see Panel 1). These silos have been driven by both funding and institutional factors with separate funding streams and organisations or departments focusing on maternal health, reproductive health, and HIV. To help solve this problem, SRHR Infographic snapshots were developed for all 194 WHO Member States. Each country snapshot includes 120 indicators and 174 items of data once disaggregation by sex and age is included for some indicators. The indicators cover a broad range of policy, health systems and service delivery interventions for sexual and reproductive health—including maternal health, contraceptives, safe abortion, HIV and other STIs, sexual and gender based violence, sexual health and well-being, comprehensive sexuality education and infertility—to support an enabling environment for integrated, people-centred health care, including self-care interventions for SRHR (see Panel 2).6,7 Indicators with a specific focus on sexual rights and reproductive rights include laws and policies that create a safe and supportive enabling environment that meets the SRH needs of all people, especially key and vulnerable populations. Also included are indicators related to the ability of adolescents, young women, and key populations are meeting their SRH needs. The SRHR Infographic Snapshots—within which the full list of indicators can be found—are publicly available on the WHO website.6
Panel 1. Challenges to attaining SRHR.
-
•
Disease outbreaks including COVID-19, climate change, conflicts and humanitarian crises requiring new approaches to maintaining and prioritising essential sexual and reproductive health services;
-
•
epidemiological and demographic trends such as increased numbers of older people and adolescents, each with distinct sexual and reproductive health needs;
-
•
persistent high mortality rates and morbidities due to lack of accessible, available, affordable, acceptable and quality sexual and reproductive health services and products, including self-care interventions;
-
•
insufficient progress in addressing social determinants of health, including stigma, discrimination, violence, human rights violations, and gender inequality and inequities;
-
•
harmful traditional practices such as child marriage and female genital mutilation as well as politicisation and policing of sexual health; and
-
•
limited human and financial resources compounded by persistent institutional and funding silos in health, undermining a more efficient integrated approach and reducing potential of multisectoral synergies to support achievement of joint health outcomes.
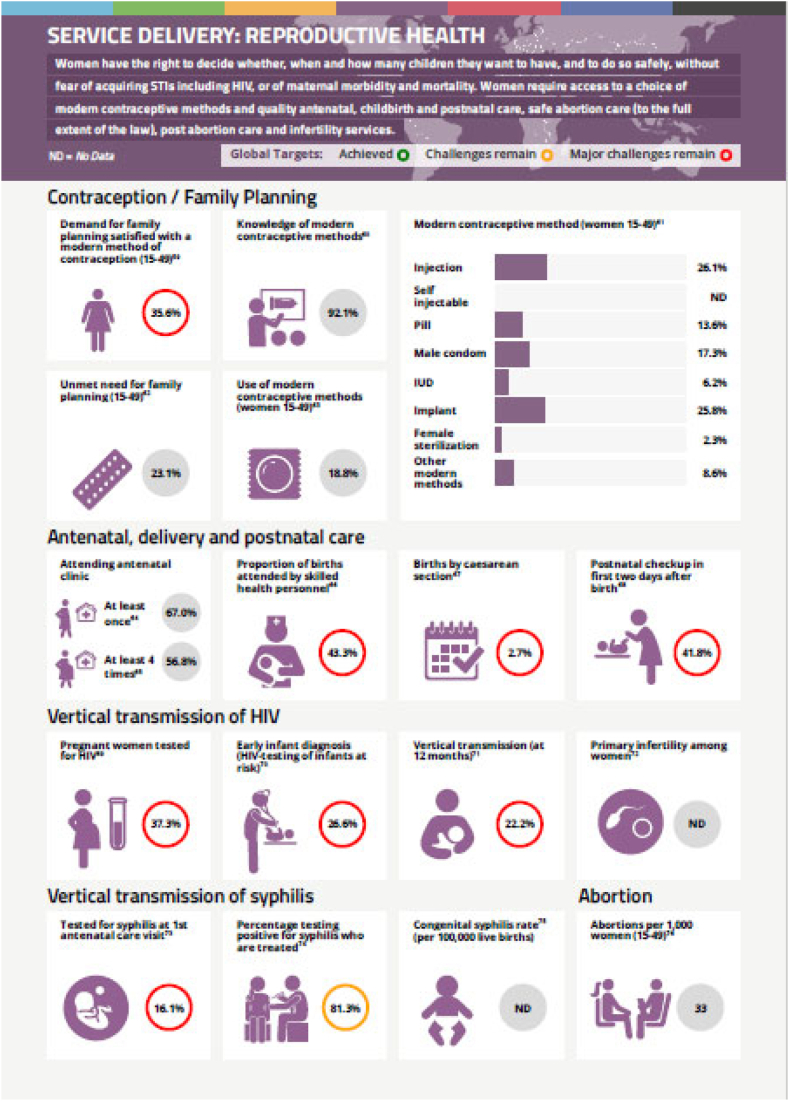
Panel 2. Sexual and reproductive health and rights infographic snapshot 2021: Nigeria.
Extract of page 5. Source WHO sexual and reproductive health and rights: infographic snapshots https://iris.who.int/bitstream/handle/10665/349679/WHO-SRH-21.146-eng.pdf
The snapshots were created using publicly available data up to 15 April 2021 that were less than 10 years old. Data were sourced from data repositories maintained by international and global agencies: the Sustainable Development Goal (SDG) database, WHO Global Health Observatory, UNAIDS (Global AIDS Monitoring Database, Epidemiological estimates database, and Laws and Policies Analytics database), Demographic Health Survey Statcompiler, UNICEF, United Nations Statistics Division, United Nations Population Division, Guttmacher Institute, World Economic Forum, and the World Bank Group. Whilst the purpose of the snapshots was to show existing SRHR data in one document, data availability was not consistent across all countries. The average data availability for all 194 countries was 57% but the level of data availability differs depending on country income level (see Fig. 1). Low and lower-middle income countries (LMICs) have an average data availability of 71%, upper-middle income countries have 60% data availability and high-income countries (HICs) have 40% data availability across all the SRHR data collected in the snapshots. The top five countries for data availability for the snapshots were Nepal with 88.5% data availability, followed by Benin with 87.4%, Senegal with 86.8%, Côte d'Ivoire and Guatemala both with 85.6%.
Fig. 1.
Availability of SRHR data in international datasets in each country in 2021.
There are some obvious reasons for this difference in data reporting between LMICs and HICs. First, is the requirement for reporting linked to funding. LMICs receive foreign direct assistance for health and are required to report data as part of multilateral donor funding conditions. The World Bank requires borrowers to report on a range of data as a condition of the loan and non-borrowers, i.e. HICs, are not required to report data on certain topics, such as poverty.8 Secondly, some of the data reported in the SRHR infographic snapshots is collected only through Demographic Health Surveys (DHS) or Multiple Indicator Cluster (MICs) surveys which are only conducted in low and middle income countries. This accounted for seven out of 174 items of data included within the snapshot, 4% of the total. Thus, this does account for some of the differential between LMICs and HICs but only a very small part of it.
Data reporting: importance and implications
Why does this difference in data availability matter? To answer, it is important to look at data reporting and the implications for not doing so. What are the implications for lower data reporting? There are three key reasons, i) meeting the Sustainable Development Goals; ii) an opportunity to learn; and iii) increased accountability.
The SDGs are universal and apply to all signatories.9 Whilst not all indicators are relevant for all countries, the SDGs are global goals for global challenges.
SRHR appears specifically in SDG 3 (good health and well-being) and SDG 5 (gender equality) and the snapshot dataset includes all 11 SDG indicators directly related to SRHR (see Table 1). When data availability compared to country income level was analysed for each, data availability is very similar—if not a little low—for each of the country income levels at 69%, 57% and 38% for LMIC, UMIC and HIC's, respectively. This compares to 71%, 60% and 40% respectively for the overall data available in the snapshots.
Table 1.
Data availability by country income level for each SDG indicator.
| Indicator | Indicator description | Data availability |
|||
|---|---|---|---|---|---|
| Low & lower-middle income country | Upper-middle income country | High income country | |||
| SDG 3.1.1. | The estimated number of women, between the age of 15 and 49, who die from pregnancy-related causes while pregnant or within 42 days of termination of pregnancy, per 100,000 live births | 100% | 94% | 89% | |
| SDG 3.1.2. | Proportion of births attended by skilled health personnel | 95% | 96% | 82% | |
| SDG 3.2.2. | Neonatal mortality | 100% | 100% | 100% | |
| SDG 3.7.1. | Percentage of total demand for family planning among married or in union women aged 15 to 49 that is satisfied with modern methods | 90% | 70% | 12% | |
| SDG 3.8.1 | UHC service coverage index | 100% | 94% | 89% | |
| SDG 3.8.2. | Population with large health expenditures as a share of total expenditure or income greater than: | 10% | 59% | 49% | 25% |
| 25% | 59% | 49% | 25% | ||
| SDG 5.2.1. | Proportion of ever married or partnered women aged 15–49 who experienced physical or sexual violence from a current or former intimate partner in the past 12 months | 48% | 26% | 5% | |
| SDG 5.3.1. | Child marriage (%), married by 18 | 89% | 70% | 16% | |
| SDG 5.3.2. | Proportion of girls and women aged 15–49 years who have undergone female genital mutilation/cutting (FMG/C). | 31% | 4% | 0% | |
| SDG 5.6.1. | Proportion of women who make their own informed decisions regarding sexual relations, contraceptive use and reproductive health care (% of women aged 15–49 years) | 51% | 28% | 0% | |
| SDG 5.6.2. | Extent to which countries have laws and regulations that guarantee full and equal access to women and men aged 15 years and older to SRH care, information, and education | Maternity care | 48% | 42% | 30% |
| Family Planning | 64% | 55% | 39% | ||
| CSE | 62% | 53% | 33% | ||
| Sexual Health | 60% | 55% | 39% | ||
| Total | 47% | 38% | 28% | ||
| Average data availability | 69% | 57% | 38% | ||
A World Bank report found that HICs reported on just 25% of the indicators on gender equality (goal 5). Yet, ending discrimination and violence against women (targets 5.1 and 5.2) and universal access to sexual and reproductive health (5.6) are not priorities for low-income countries alone.
National ownership is a key feature of the SDGs and reporting on progress by countries is voluntary but encouraged.10 In its first national SDG report, in 2017, the United Kingdom had acquired data on only 39% of SDG indicators but by 2021 had managed to increase this figure to 83%.11 The story is not the same across other HICs. The 2021 United States of America Development Report showed state-level gaps in data, including on access to contraception for example, lack of disaggregation by sex and age, and time lags in data reporting with sexual violence not included as an indicator as recent data were not available.12 The report states that in some cases, academic and advocacy groups have attempted to fill the data gaps but lack the resources to do so routinely, while in others national agencies have not released data. As well as a lack of systems and processes to aggregate each State's data to the federal level to monitor national progress12 according to the World Bank, there is also a lack of political will to do so.13 The old adage of “what gets measured gets done” was found to have a positive correlation on measuring progress towards the Millennium Development Goals (MDG), with countries with higher data gaps having a lower probability of MDG success.14 This points to the need to take the performance measurement of the SDGs seriously, as it not only shows where work still needs to be done, but it also shows which countries are making progress providing an opportunity to learn from what they are doing.
There are two big consequences of relatively fewer high-income countries reporting their data on SRHR into international datasets. The first is it is impossible to tell where the gaps still are and what progress still needs to be made at the national level. As stated earlier, the World Bank does not require high income countries to report on poverty as their focus is LMIC's yet, as anyone in a high-income country would attest, poverty does not just exist in low-income countries. Similarly, access to sexual and reproductive health and rights or gender equality cannot be assumed because a country is a high-income country. For example, the Global Gender Gap Report 2023 compiled by the World Economic Forum, found that the Middle East and North Africa, a region that includes several high-income countries, remains the furthest away from gender parity, in comparison to other regions.15—Thus, reporting on SRHR and gender equality indicators are important for high income countries as they are issues that affect people within these countries and if SDGs 3 and 5 are going to be attained, they also need to be reported on. Also important here is disaggregation to see which income groups, genders, ethnic groups, ages of people have poor SRHR outcomes or are struggling to access the healthcare they need. Underserved populations within HICs often lack access to services and have poor health outcomes. Racial and socioeconomic status, for example, can particularly impact health outcomes, and these populations are often overlooked and under-resourced in health research.16 Social injustices such as these are often hidden in aggregated datasets. It is likely that demographically disaggregated data is collected at country level as much is being done by WHO and other organisations in terms of providing tools for data stratification, but when it is not reported into international datasets, this disaggregated data cannot be applied to learn where the gaps are.17,18
Secondly, a lack of reporting by HICs leads to a skewing of the data in international datasets. As a result, important lessons are lost, especially if these are lessons of success that do not appear in the dataset. For example, the strong data collection system in Sweden19 is supporting national learning and improving health services and therefore health outcomes. Webster (2014) explains that these large datasets give studies great statistical power allowing researchers to detect or rule out small effects.19 Using the same logic, large sets of global data should be able to allow for greater learning and understanding of different healthcare issues. Yet, these data are missing. Data were only reported for Sweden on global datasets for 58 of the 174 items of data within the SRHR country snapshot—67% of data were missing. The social determinants of health—shown through the impact of other SDGs, such as climate change, on SRHR and gender equality are harder to see if the dataset is incomplete.20,21 We offer ourselves the biggest opportunity to learn if data is openly accessible in international datasets which have been verified and also ensure that the data included is comparable.
Overall, learning from data allows current gaps to be exposed, progress to be monitored and successes to be celebrated and then learning to occur from why the success happened. All of these improve performance on SRHR by improving accountability.
WHO recognises that data collected by Member States belong to the countries where they are generated and should be shared, but with a policy for countries to opt out, provided they clearly indicate the scope of the data and specific reasons for opting out.22 All 194 Members States of the WHO have signed up to the system and whilst they are not mandated to report on their own progress towards health, there is a joint accountability to do so. This is not to say data in some instances do not exist. Many countries, for instance, have population-based and nation-wide health data, sometimes spanning decades such as Sweden as mentioned earlier. To make health related data for a comprehensive approach to SRHR easily accessible—including to design research protocols, inform policy decisions, and foster international partnerships—all countries should share their health-related data as per their commitment as signatories to different international resolutions in appropriate, reliable international directories or data repositories such as those that feed into WHO's Global Health Observatory. It is often assumed that lower levels of data reporting by HIC for indicators included in the SRHR infographic snapshots are due to many indicators focusing on areas not relevant in HICs, for example due to lower incidence of infections such as HIV. However, a closer examination of the SRHR related indicators in the snapshots reveals that this rationale does not hold up as the majority of indicators are not disease specific. There are indicators on the enabling environment such as protection against discrimination for people living with HIV and key populations, access to safe abortion and protection for women against marital rape and domestic violence. There are health systems indicators on the number of skilled health workers per 10,000 population, health information systems and health financing. There are indicators on the ability of people to access reproductive health such as have their demand for family planning satisfied or know they will be tested for HIV and syphilis during pregnancy to protect both themselves and their unborn child. There are indicators in support of sexual health such as the availability of screening programmes for cervical cancer, and the availability of support in cases of rape or incest, they can access treatment if living with HIV. There are indicators supporting adolescent sexual health so they can have the knowledge to reduce the chances of HIV, STIs and unintended pregnancy, and can access condoms. There are indicators that highlight the size, HIV prevalence and condom use among key populations. These are not only issues of low-income countries but of all countries globally.
Accountability is important to peers and to citizens. Data help governments prioritize health challenges and allocate resources but also provide important data for global monitoring and learning, such as for the SDGs.18 With no publicly published data on standard indicators in international datasets it is difficult to tell how well countries are doing on any of the above and this affects both citizens and progress towards regional and international goals and targets.23 It could be argued that there is a moral argument for data reporting as by being open and transparent in sharing data, what is working and what is not working, countries can help each other to learn and improve to jointly meet the SDGs and support the health and rights for all their citizens.
Accountability is one of the key principles of the Cape Town Global Action Plan for Sustainable Development, which called on governments, policy makers, and the international statistical community to mobilise resources to strengthen and modernise national statistical systems, yet five years after it was operationalised, a global survey of national statistical offices shows that transformative change is yet to be realised.24,25
National self-interest is also a factor; sharing data requires trust and recognition of the benefits of the act of sharing, and the benefits of international cooperation are not always clear.26 Trust within countries, between citizens and the state, is also key to inclusive data sharing. Lack of stakeholder engagement by governments can lead to concerns over privacy and security. By making data available, governments can also increase transparency and accountability to citizens. Indeed, the Organisation for Economic Cooperation and Development (OECD) describes its Open Government Data initiative as “a philosophy–and increasingly a set of policies–that promotes transparency, accountability, and value creation by making government data available to all.“27
Future directions and policy recommendations
To encourage countries to report their data there needs to be a higher value attached to data reporting for countries. Here are three ways countries and global institutions can act to improve access to and learning from global data:
First, where feasible donor countries should start reporting on all the health data they are requiring others to report on. It is recognised there is a cost to reporting data to international bodies but where data is already collected and available at the national level the additional reporting cost is negligible. For countries who invest millions of dollars each year in global health, ensuring their data is included in the global data sets they are requiring LMIC countries to also report on is not just the right thing to do but will enable better global learning on what works. It is recognised that there are some indicators that are not currently collected but this does not mean they are no important issues—such as the prevalence of gender-based violence. There needs to be commitment to start collecting these indicators routinely, especially those that are part of the Sustainable Development Goal reporting framework.
Second, reporting data in international datasets makes it visible and available for analysis and learning. International agencies that curate databases of health data, should ensure that where data is not available and hasn't been reported on by a country this is clearly highlighted in the visualisations that go with the dataset. Publications such as the SRHR Infographic Snapshots assist with this. Making data gaps visible can help to add pressure to the relevant decision makers in government to provide the data. Providing useful data aggregation and comparison tools can also encourage countries to provide data as they benefit from the tool provided.
Third, international organisations that collect data need to hold countries accountable for the obligations they have signed up to. For example, HIV-related data is reported to UNAIDS via the Global AIDS Monitoring tool and is a requirement for all 161 signatories of the 2021 high level meeting declaration on HIV/AIDS.28 Thus UNAIDS have a responsibility for calling out countries not living up to their obligations. WHO stipulates that data collected by Member States under its technical programmes should be shared in equitable, ethical, and efficient ways.29 This does not only apply to data collected from routine surveillance systems and national population-based surveys (e.g. DHS, MICS) but also to data and evidence generated from rigorous widescale health research studies, especially of national, sub-national or provincial scale. The biggest focus should be on reporting on progress towards the Sustainable Development Goals, data availability (or the lack of it) highlighted with countries asked to provide an action plan towards collecting the missing data—especially on key global indicators such as ending discrimination and violence against women and universal access to sexual and reproductive health.
Added to the above, it is important to learn why national level data is not currently being reported in international datasets. It is currently unclear why some HICs are not reporting data. There may be political, cultural, legal, operational, or motivational constraints that are stopping countries from reporting. Further research is needed to explore the current barriers to data reporting from both the country perspective and the database perspective. These barriers then need to be reduced and systems enhanced to make the reporting of data into international datasets as simple as possible and even automated where possible.
Conclusion
The SRHR infographic snapshots provide a visual representation of the national SRHR situation—including successes, areas for improvement, and data gaps, especially among HICs. Data transparency has become important in the face of pandemics, such as COVID-19. There is an urgent need for better data governance, sharing and reporting practices for all countries. Improving the availability of SRHR data including through reliable international datasets can lead to more agile, responsive, and timely actions by all relevant stakeholders.
Technological advances mean there is now more data available than any other time in history and this provides opportunities to optimally organise to deliver the best outcomes, advance knowledge and understand what works to being positive change.30 If existing SRHR data can be reported by all countries then there will be more opportunities to learn from this data to better meet SDG 3—ensuring healthy lives and promoting well-being at all ages, and SDG 5 bringing about gender equality. These goals are intimately linked and there is much to be learnt from HICs such as Sweden who are progressing well towards these SDGs but not yet reporting. There is also a need to disaggregate national data and understand the populations currently being left behind with poor access to SRH services that result in poor SRH outcomes. SRHR data from all countries needs to be shared regardless of the income level of the country.
Contributors
JH drafted the original text with inputs from MN, MA, RS and AM. RS created Fig. 1. All authors reviewed the final version before it was submitted.
Data sharing statement
JH accessed and verified the data and all authors were responsible for the decision to submit the manuscript.
Declaration of interests
The authors declare no competing interests.
Acknowledgements
The authors thank Soe Soe Thwin and Manju Rani for their helpful feedback on an earlier version of this manuscript.
The views presented here represent those of the authors and not the organisation.
References
- 1.World Health Organization . 2004. Reproductive health strategy to accelerate progress towards the attainment of international development goals and targets.http://apps.who.int/iris/bitstream/handle/10665/68754/WHO_RHR_04.8.pdf;jsessionid=70551BB5610CA76D28E90DC0BB8DB33?sequence=1 Available from: [DOI] [PubMed] [Google Scholar]
- 2.Starrs A.M., Ezeh A.C., Barker G., et al. Accelerate progress—sexual and reproductive health and rights for all: report of the Guttmacher–Lancet Commission. 2018. Lancet. 2018;391:2642–2692. doi: 10.1016/S0140-6736(18)30293-9. [DOI] [PubMed] [Google Scholar]
- 3.Leddy A.M., Weiss E., Yam E., Pulerwitz J. Gender-based violence and engagement in biomedical HIV prevention, care and treatment: a scoping review. BMC Public Health. 2019;19(1) doi: 10.1186/s12889-019-7192-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jonas K., Crutzen R., van den Borne B., Sewpaul R., Reddy P. Teenage pregnancy rates and associations with other health risk behaviours: a three-wave cross-sectional study among South African school-going adolescents. Reprod Health. 2016;13(1) doi: 10.1186/s12978-016-0170-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rosser J.I., Aluri K.Z., Kempinsky A., Richardson S., Bendavid E. The effect of healthcare worker density on maternal health service utilization in sub-Saharan Africa. Am J Trop Med Hyg. 2022 doi: 10.4269/ajtmh.21-0727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization . 2021. Sexual and reproductive health and rights: infographic snapshots.https://www.who.int/publications/i/item/WHO-SRH-21.21 Available from: [Google Scholar]
- 7.World Health Organization . World Health Organization; Geneva: 2022. WHO guideline on self-care interventions for health and well-being, 2022 revision. Licence: CC BY-NC-SA 3.0 IGO. [PubMed] [Google Scholar]
- 8.World Bank Why is there missing data for high-income countries? https://datahelpdesk.worldbank.org/knowledgebase/articles/198559-why-is-there-missing-data-for-high-income-countries Available from:
- 9.World Health Organization International health Regulations. https://www.who.int/europe/health-topics/international-health-regulations#tab=tab_1 Available from:
- 10.United Nations . 2017. Guidelines to support country reporting on the sustainable development goals.https://unsdg.un.org/sites/default/files/Guidelines-to-Support-Country-Reporting-on-SDGs-1.pdf Available from: [Google Scholar]
- 11.Office for National Statistics . December; UK: 2021. Sustainable development goals data update.https://www.ons.gov.uk/economy/environmentalaccounts/articles/sustainabledevelopmentgoalstakingstockprogressandpossibilities/december2021 Available from: [Google Scholar]
- 12.Lynch A., Sachs J. SDSN; New York: 2021. The United States sustainable development report 2021.https://www.sdgindex.org/reports/united-states-sustainable-development-report-2021/ Available from: [Google Scholar]
- 13.Kitzmueller L., Stacy B., Mahler D.G. 2021. Are we there yet? Many countries don't report progress on all SDGs according to the World Bank's new Statistical Performance Indicators.https://blogs.worldbank.org/opendata/are-we-there-yet-many-countries-dont-report-progress-all-sdgs-according-world-banks-new Available from: [Google Scholar]
- 14.Jacob A. Mind the gap: analyzing the impact of data gap in millennium development goals' (MDGs) indicators on the progress toward MDGs. World Dev. 2017;93:260–278. doi: 10.1016/j.worlddev.2016.12.016. [DOI] [Google Scholar]
- 15.Global gender gap report. World Economic Forum; 2023. https://www.weforum.org/publications/global-gender-gap-report-2023/digest/ [cited 2023 Dec 1]. Available from: [Google Scholar]
- 16.Rani M., Buckley B.S. Systematic archiving and access to health research data: rationale, current status and way forward. Bull World Health Organ. 2012;90(12):932–939. doi: 10.2471/BLT.12.105908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.United Nations Statistical Commission . 2021. Complication of tools and resources for data disaggregation.https://unstats.un.org/unsd/statcom/52nd-session/documents/BG-3a-Compilation_of_tools_and_resources_for_data_disaggregation-E.pdf Available from: [Google Scholar]
- 18.WHO . 2021. Global report on health data systems and capacity, 2020.https://assets.bbhub.io/dotorg/sites/64/2021/04/who_2021-01-31_global-report-score_tb_v2.pdf Available from: [Google Scholar]
- 19.Webster P.C. Sweden's health data goldmine. Can Med Assoc J. 2014;186(9):E310. doi: 10.1503/cmaj.109-4713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Women Deliver . 2021. The link between climate change and sexual and reproductive health and rights.https://womendeliver.org/wp-content/uploads/2021/02/Climate-Change-Report.pdf Available from: [Google Scholar]
- 21.World Health Organisation Social determinants of health. https://www.who.int/health-topics/social-determinants-of-health [cited 2023 Dec 1]. Available from:
- 22.World Health Organization . 2017. Policy on use and sharing of data collected in Member States by the World Health Organization (WHO) outside the context of public health emergencies (Provisional)https://cdn.who.int/media/docs/default-source/publishing-policies/who-data-sharing-policy-collected-by-member-states-outside-of-public-health-emergencies61d03608e6134ba786ad94403e947013.pdf?sfvrsn=bb52b31d_33 Available from: [Google Scholar]
- 23.United Nations . 2019. Best practices in data flows and global data reporting for the sustainable development goals.https://unstats.un.org/unsd/statcom/50th-session/documents/BG-3a-Best-Practices-in-Data-Flows-and-Global-Data-Reporting-for-theSDGs-E.pdf Available from: [Google Scholar]
- 24.United Nations Statistical Division . 2017. Cape Town global action plan for sustainable development data prepared by the high-level group for partnership, coordination and capacity-building for Statistics for the 2030 agenda for sustainable development.https://unstats.un.org/sdgs/hlg/cape-town-global-action-plan/ Available from: [Google Scholar]
- 25.World Bank; UNSD; Paris21 Survey on the implementation of the Cape Town global action plan for sustainable development data (English). Washington, D.C.: World Bank Group. http://documents.worldbank.org/curated/en/826351643712794722/Survey-on-the-Implementation-of-the-Cape-Town-Global-Action-Plan-for-Sustainable-Development-Data
- 26.van Panhuis W.G., Paul P., Emerson C., et al. A systematic review of barriers to data sharing in public health. BMC Public Health. 2014;14:1144. doi: 10.1186/1471-2458-14-1144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lencucha R., Bandara S. Trust, risk, and the challenge of information sharing during a health emergency. Glob Health. 2021;17:21. doi: 10.1186/s12992-021-00673-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.UNAIDS Global AIDS monitoring 2023. Frequently asked questions. https://www.unaids.org/sites/default/files/media_asset/faq-global-aids-monitoring_en.pdf Available from:
- 29.World Health Organization . 2022. Sharing and reuse of health-related data for research purposes: WHO policy and implementation guidance.https://www.who.int/publications/i/item/9789240044968 Available from: [Google Scholar]
- 30.Dash S., Shakyawar S.K., Sharma M., et al. Big data in healthcare: management, analysis and future prospects. J Big Data. 2019;6:54. doi: 10.1186/s40537-019-0217-0. [DOI] [Google Scholar]