Abstract
Purpose
To report a case of metallic corneal foreign-body (CFB) penetrating the Laser in situ keratomileusis (LASIK) flap and its successful outcome. To highlight usefulness of Anterior Segment Optical Coherence Tomography (ASOCT) in diagnosis and management of post-LASIK CFB. To enumerate other similar cases published in literature.
Method
A 30-year-old male presented to the emergency department of a tertiary eye care centre with a metallic CFB. He had undergone uneventful LASIK elsewhere 4-years back. He was unaware of any trauma. CFB removal was attempted elsewhere but abandoned as CFB appeared deeply embedded. ASOCT showed CFB had penetrated LASIK flap and lodged into midstroma, 207 μm deep. CFB was successfully removed in operation theatre along with the application of cyanoacrylate glue and bandage contact lens. A review of literature for CFB in post-LASIK patients was done through PubMed search.
Result
Postoperative course was uncomplicated and there was a follow up period of 4 months. Vision improved to unaided 20/20 and N/6 from preoperative 20/60 and N/10. Review of literature of 24 patients showed Post-LASIK FB was more common in males (79%). None of the patients except for one had protective eye-wear. Metallic FB was most common followed by organic FB. Flap complications were present in seven patients. Diffuse lamellar keratitis (DLK) and epithelial ingrowth were the most common post-FB removal complications occurring in six (25%) and four (16.6%) patients respectively.
Conclusion
Post-LASIK patients with CFB need to be inspected for flap related complications. CFB can be successfully removed, although DLK, epithelial ingrowth, microbial keratitis, astigmatism, can occur post-CFB removal. ASOCT can delineate CFB and flap related details and thus is an additional useful imaging tool in such scenarios.
Keywords: Anterior segment optical coherence tomography, ASOCT, Laser insitu keratomileusis, LASIK, Corneal foreign body
1. Introduction
Laser in situ keratomileusis (LASIK) is a commonly used procedure to correct refractive errors.1 Ocular trauma or injury is a common cause of emergency interventions across the world accounting for 5–16% of ophthalmology consultations.2 Post-LASIK patients have a risk of suffering additional flap related complications when sustaining trauma or foreign body (FB) fall.3 Occurrence and management of trauma related flap complications like flap tear, avulsion, diffuse lamellar keratitis (DLK),4, 5, 6 etc have been well reported in literature but there are very few reports describing the incidence of penetrating trauma or corneal foreign bodies (CFB) and their management. Post-LASIK eyes in addition to routine foreign body work up require careful inspection of flap and stromal bed. We report a case of metallic FB penetrating through the LASIK flap, causing a buttonhole of flap and embedded in the anterior part of the stromal bed as well as its diagnosis and management.
2. Case description
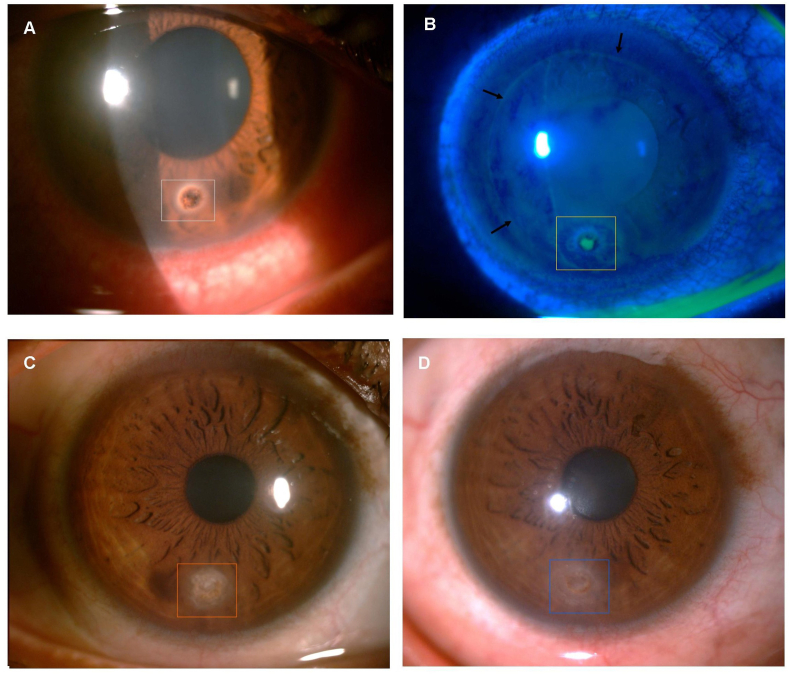
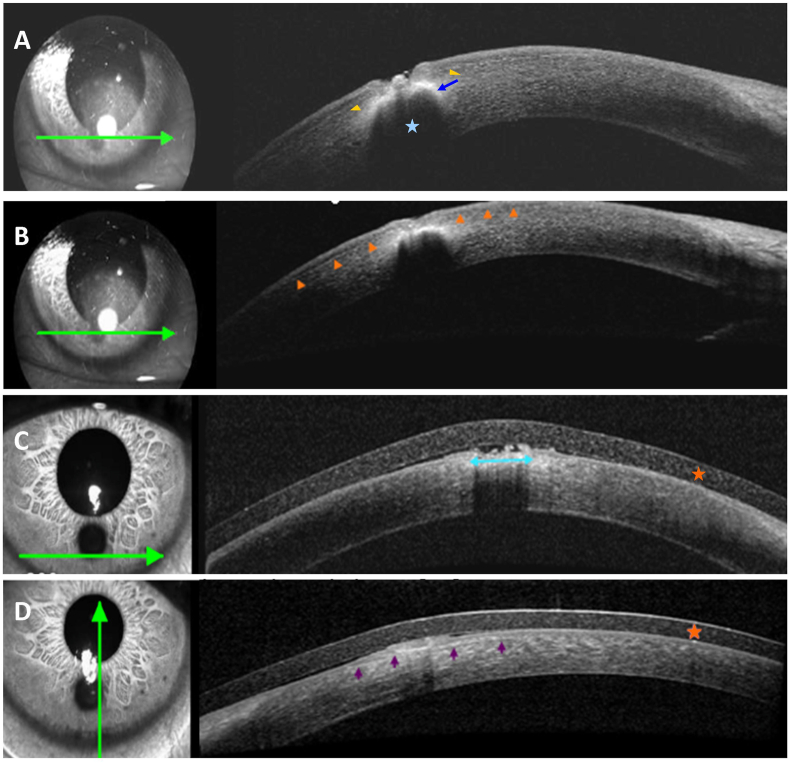
A 30-year-old male, sports player, presented to the ophthalmic emergency clinic of a tertiary eye care centre with complaints of redness in the right eye (OD) since 4 days. He had undergone uncomplicated LASIK elsewhere in both eyes (OU) 4 years back. He was unaware of any preceding history of trauma or FB entering the eye. He gave a history of attempted CFB removal elsewhere the same morning as the day of presentation which was abandoned after partial removal of superficial part as CFB appeared deeply embedded and was then referred to a speciality clinic. His uncorrected visual acuity was 20/60; N10 in the right eye (OD) and 20/30; N6 in the left eye (OS). Slit lamp examination (SLE) of OD showed mild upper lid edema, circumcorneal congestion, single metallic CFB located peripherally at 6 o'clock position approximately 2 mm from limbus with overlying epithelial defect and surrounding rust ring (Fig. 1a). LASIK flap margin could easily be delineated on fluorescein stain with a nasal hinge. Flap appeared to be well apposed clinically with no striae (Fig. 1b). Anterior chamber was quiet. No tarsal FB was noted after lid eversion or in the fornices. SLE of OS was normal with a well apposed LASIK flap. The intraocular pressure and fundus examination were normal in both eyes. ASOCT using Spectralis Anterior Segment Module (Heidelberg Engineering GmbH, Heidelberg, Germany) of OD revealed an area of hyper-reflectivity in the anterior stroma at a depth of 207 μm with total posterior back shadowing, no descemet's breach, and overlying crater-like lesion (Fig. 2a). Flap thickness was noted around 107 μm. Flap looked like a meniscus flap suggestive of microkeratome LASIK.6 CFB caused a buttonhole in the flap with the flap margin delineated inferiorly (Fig. 2b). Although FB penetrated the flap and lodged in underlying stromal bed, no flap dehiscence or interface gap or flap displacement was seen (Fig. 2b). The patient was taken up for FB removal in operation theatre under local anaesthesia. The epithelium around the FB was carefully and gently debrided starting nasally and going temporally to avoid flap displacement.7 CFB was removed with 26G needle in totality. The surrounding rust ring was removed with a diamond burr to the extent possible without disturbing the flap. After removal of the FB, there was a circular tissue defect of approximately 2 mm along with thinning forming a well configuration. As the edges were not approximated and we wanted to avoid suturing, cyanoacrylate glue and a bandage contact lens (BCL) was placed to seal the tissue defect. (Fig. 1c).8 Topical dexamethasone (0.1%) eye drops four times per day with weekly tapering, topical moxifloxacin (0.5%) eye drops six times per day till BCL was in place and carboxymethycellulose sodium (0.5%) eye drops four to six times per day were started. Patient was examined on postoperative day (POD) 1, 5,9,16,45, 60, 90 and 120. In immediate postoperative period, tissue adhesive and BCL were in place and the flap seemed opposed to margins and underlying stroma (Fig. 1, Fig. 2c). Few Descemet's membrane folds were seen which resolved by 1 week postoperatively (Fig. 1c). On POD 5, the flap margin near the affected area could be clearly delineated. At 2 months glue and BCL were removed with no underlying defect. A nebulo-macular scar with minimal thinning was noted at the site of removed CFB(Fig. 1d) with well apposed flap (Fig. 2d). OD unaided visual acuity improved to 20/20 and N/6 by POD 7 and was maintained till last follow up. No complication was noted till last follow up period of 4 months.
Fig. 1.
Pre and Postoperative slit lamp images (a)-preoperative diffuse slit lamp image showing metallic CFB at 6 o'clock (white box) approximately 2 mm from limbus. (b)-Preoperative diffuse fluorescein stained slit lamp image with cobalt blue filter showing epithelial defect over CFB(yellow box). Flap margins can be delineated with good flap apposition and no macrostriae. (c)- Postoperative 1 week diffuse slit lamp image with clear cornea, well apposed flap margins and cyanoacrylate glue (orange box) and BCL in place. (d)-Postoperative day 61 diffuse slit lamp image after glue and BCL removal. There is nebular scar with residual rust ring (blue box). (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
Fig. 2.
Pre and Postoperative ASOCT images (a)-preoperative ASOCT horizontal single line image through the CFB showing anterior hyper-reflective border (blue arrow) with total posterior backshadowing (blue asterix) suggestive of metallic CFB at mid-stromal level below the flap (yellow arrowhead) (b) preoperative ASOCT horizontal single line image through the CFB showing extension of the flap margin beyond the CFB inferiorly (orange arrowhead). Also note absence of any flap dehiscence or displacement. (c) Postoperative ASOCT horizontal single line image at site of previous CFB showing anterior hyper-reflectivity of the cyanoacrylate glue filling the crater (blue horizontal arrow) with overlying BCL(orange asterix). (d) Postoperative ASOCT vertical single line image at site of previous CFB showing well apposed flap post-FB removal (violet arrows) with a clear apposed interface and absence of any discernible macrostriae. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
3. Review of literature
We did a literature search on PubMed using terms: corneal foreign body, LASIK and trauma and found 60 relevant articles. Articles related to Interface debris noted in early post operative period9 and articles involving only blunt trauma without any corneal FB post-LASIK trauma were excluded. Table 1 enlists various articles about different FB in cornea and anterior chamber post-LASIK.
Table - 1.
Review of literature: FB status post LASIK.
| Authors | History of trauma | Eye affected | Gender | Type of FB | Duration after LASIK | Flap dislo-dged | Interface/underlying stromal bed | Location of FB | Imaging investigations | Management | Complications |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Weisenthal et al.28 (2000) | Yes Noticed irritation while fixing sink | OS | M | Metallic | 6 months | No | Clear | Metallic FB in the inferotemporal cornea in OS overlying the LASIK flap | Nil | FB was removed without disruption of the flap and minimal disruption of the epithelium leaving a small residual rust ring. | DLK (24 hours) (managed with topical steroids) |
| Porges et al.15(2001) [8 patients] |
Yes(4) No (4) |
M-7 F-1 |
Mostly metallic FB | 1 day to 18 months | No | – | Corneal FB | Nil | CFB removal was carried out with a 27-gauge needle | Corneal hyposensitivity leading to delayed diagnosis in 3 patients. | |
| Cosar et al.3 (2002) | Yes Penetrating trauma to the OD while hammering |
OD | M | Metallic FB | 17 months | No | Full-thickness peripheral corneal laceration at 11-o'clock in OD extending over the edge of the previous LASIK flap. | Partially embedded in the superior iris | Nil | FB removed in OT by kelmanforcep through scleral tunnel | No |
| Crowther et al.1 (2005) | NO | OU | M | Ferrous FB | 18 months | Flap lifted | Interface debris | OD had a LASIK flap scar with debris in the interface. | Nil | FB removed with needle bevel | (1) Flap lift on attempted removal, thus rust ring was left behind (2) High astigmatism (3) corneal hyposensitivity leading to multiple incidents of OU FB |
| OS had central rust ring and debris within | |||||||||||
| the interface, extending from the rust-ring | |||||||||||
| position to the peripheral rim inferotemporally. | |||||||||||
| 2 scars were present from previous corneal FBs | |||||||||||
| Cheung et al.10 (2006) | Yes Gouging by a seagull claw |
OD | M | Organic material | 34 months | Flap dehiscence | Flap dislocation | Interface organic fb debris | Microbiological work up showed enterrobacter species | Flap reflected, fb debride from flap and stromal bed, irrigation done, flap repositioned | Enterobacter keratitis |
| Jin et al.16 (2006) [2 patients] |
1.Yes With construction material while cutting vinyl board in OD 2.Yes Hit in OS by a wood chip when using an axe to break up particleboard |
1-OD 2-OS |
M (both) | 1.Debris from construction site in 2. Wooden FB |
(1)7 years (2)4 years |
1.Flap laceration 2.Flap displaced |
1. Interface foreign debris 2.FB trapped in wound |
1. Triangular linear flap laceration with some interface foreign debris 2. Displaced flap at 9 o'clock with a curvilinear laceration and a superficial laceration of the stromal bed Vertical macrofolds were seen. A small wood fragment was trapped in the wound. |
1.Nil 2. Nil |
1.surgical removal of epithelial ingrowth and fb 2.The corneal flap was surgically lifted, debrided, the striae stretched out, and tissue fragments carefully repositioned |
1.Epithelial ingrowth (pre-operative) 2. Mild DLK (pod-1), astigmatism |
| Pan et al.14 (2007) | No | OD | M | Eyelash | 5 weeks | No | Epithelial ingrowth | Eyelash lodged under the lower half of an oedematous LASIK flap in OD with mild surrounding infiltrates | Nil | Flap lifted, FB removed, epithelial cells curetted, flap repositioned | Epithelial ingrowth (preoperative), Mild DLK (pod-1) |
| Maeda et al.26 (2008) | Yes Accidental trauma with patients own hand while applying eye shadow powder in OS |
OS | F | Eye shadow particles | 6.5 years | Yes | Interface had few infiltrates and no FB reaction. | Displaced LASIK flap at 6 o'clock with eye-shadow powder deposited under the lower quarter of the flap | Nil | Flap was partially lifted sparring VA, eye-shadow deposits were copiously irrigated | Mild DLK (pod-1) |
| Lin et al.17(2011) | Yes Bee sting while riding scooters or motorcycles |
OD | M | Stinger of bee in OD | 2 years | No | Adjacent stromal infiltration | Periphery of the cornea penetrated through the LASIK flap, tearing the flap. | Nil | Stinger was removed and the lacerated conjunctiva and corneal flap were repaired | Epithelial ingrowth (post-operative) |
| Choi et al.18 (2012) | Yes OD scratched by a tree spring during recreational mountain climbing. |
OD | F | Crystalline material | 4 years | No | Stromal infiltrate at interface | Interface and under flap | Microbiological work up revealed Staphylococcus epidermidis | Flap lifted, crystalline foreign bodies grasped from the stromal bed and undersurface of the lamellar flap with fine corneal forceps Topicals for staphylococcal infection |
Staphylococcal keratitis |
| Prakash et al.12 (2012) |
No | OS | F | Cotton fibre | 10 days | No | Clear | Cotton fiber was noticed in the intralamellar space, inferotemporal to the pupillary axis | Nil | Conservative Spontaneous dissolution of FB was noted |
Nil |
| Huang et al.30 (2012) |
Yes With plastic pole to OS |
OS | M | Fb debris | 5 years | Yes Flap dislocated |
Fb debris present on exposed stromal bed | Dislocated Lasik flap misdiagnosed as corneal epithelial defect and foreign body material over the lesion | Nil | dislocated flap lifted, stromal surfaces of flap and bed scraped to remove debris and epithelial cells, flap repositioned | nil |
| Baenninger et al.25 (2014) | Yes | OD | M | Concrete | 6 months post femtoLASIK | No | Preoperative- clear POD 1: diffusely distributed, white to gray granular material concentrated around the impact location of the FB |
FB within the plane of flap in OD. | Nil | FB removed without disturbing flap | Mild-moderate DLK (pod-1) |
| Boutillier et al.13 (2018) | No | OD | M | Insect larva | 6 days | No | Inflammatory reaction, with localized neovascularization in response to the insect larva | Interface | AS-OCT: hyperreflectivity of insect larvae under LASIK flap with back-shadowing | Conservative- topical antibiotics and steroids | Nil |
| Maki et al.11(2018) | Yes Tree branch injury to OD |
OD | M | Vegetative matter | 5 years | No | Well apposed full thickness laceration of stromal bed underlying an intact LASIK flap. | Large dark piece of FB at core with surrounding hypopyon in anterior chamber | AS-OCT: posterior, penetrating, corneal laceration located underneath an intact LASIK flap. | FB removed in OT through paracentesis | Mild DLK (pod-2), Epithelial ingrowth (post-operative) |
| Our study | Yes | OD | M | Metallic | 4 years | Buttonhole of flap | clear | Penetrating the flap and embedded in the anterior stroma | AS-OCT: high reflectivity in the anteriorwith back shadowing and overlying crater lesion |
FB removed with 26G needle in OT. Glue, BCL placed | Nil |
DLK: Diffuse lamellar keratitis, BCL: Bandage contact lens, FB: Foreign body, OD: right eye, OS: Left eye, VA:visual axis, POD: post operative day, ASOCT: Anterior segment optical coherence tomography, LASIK: laser insitu keratomileusis.
M: Male, F: Female.
A total of 24 patients including ours have been reported to have post-LASIK FB. Post-LASIK FB was more common in males (19, 79%). None of the patients except for one10 had protective eye-wear. 2 patients had AC FB3,11 and in other 2 patients, interface FB12,13 were probably left behind during LASIK surgery itself. Definitive history of trauma was present in 15 patients (62.5%). One patient had a probable microtrauma which lifted the flap slightly allowing the lash to migrate.14 6 patients (25%) were unaware of any history of preceding trauma probably due to corneal hyposensitivity. Metallic FB was most common, followed by organic FB. Trauma occurred as early as 1 day15 to maximum 7 years16 after LASIK. Flap complications were present in 7 patients. FB was removed in OPD in 11 patients (45.8%) while 11 (45.8%) required FB removal in OT. In 2 patients, conservative approach was preferred.12,13 DLK and epithelial ingrowth were the most common post-FB removal complication occurring (6,25%; 4,16.6%). DLK occurred within 24–48 hours in all patients and was successfully treated with steroids in all cases. In two patients, epithelial ingrowth was secondary to FB itself and was removed by flap lift and epithelial debridement while in other two patients it occurred post-FB removal. Epithelial ingrowth was noticed by two weeks in both patients post-FB removal. It regressed after suture removal in one patient,17 while in another11 it remained stationary with no further intervention. Two patients (8.3%) had microbial keratitis which was successfully managed medically.10,18
4. Discussion
In the USA, over the last twenty-five years, 20–25 million eyes were treated with Laser Vision Correction (LVC) with around 800,000 eyes being treated each year for the last ten years and LASIK being the most common procedure performed.19 CFBs are the second most common type of ocular injury, accounting for approximately 30.8% of all eye injuries.20 Diagnosis and management of CFB in post-LASIK patients merits diligence. A study conducted among Chinese military personnel reported 95.8% mechanical ocular injury post-LASIK of which 4.35% presented with ocular surface FB's.21 LASIK involves creation of an anterior flap with a potential space between the flap and the stroma which is a relatively vulnerable area as there is minimal wound healing except at the edges of the flap.18 This weakness of flap predisposes patients to more severe sequelae of impacted CFB removal.9 Trauma associated flap complications and interface debris have been well documented in literature, but there are only few isolated case reports about occurrence and management of CFB post-LASIK.
Pre-operative assessment in post-LASIK CFB includes but is not limited to involve detailed history about the type of LASIK done,6 mode of injury, type of FB, depth and location of FB, any associated flap complications like flap displacement, avulsion, tear; any micro or macro-striae, interface apposition and underlying stromal bed status. In addition to clinical examination, ASOCT is a novel additional tool helpful in assessing all above parameters.
Inert FBs like glass/plastic can be left alone whereas metallic/organic FBs require removal.2 Central CFBs should be removed, as they have an impact on the vision.22 FB's like insect larvae and cotton fibres under flap have been successfully managed with conservative approach.12,13 These FB being biodegradable could have been disintegrated by keratocytes over time. However, if an inert FB is associated with epithelial ingrowth, it requires surgical intervention.14 Superficial CFB removal post-LASIK can be attempted on the slit lamp but there is always a risk of flap lift.1 In our patient also, an unsuccessful attempt at CFB removal was done elsewhere leaving behind a crater. FB deeper than the flap should however be removed in OT like in our case because when the flap integrity is compromised, the removal of FB poses difficulty with higher risks of flap dislodgement and flap related complications during and after removal. AC FB can be removed via a paracentesis incision without disturbing the flap.3,11 In patient with AC FB, attempt to delineate entry tract might be difficult on slit lamp due to associated corneal edema or haze. In addition, an entry tract would sometimes be a nidus for epithelial ingrowth. In both the above circumstances, ASOCT is a helpful tool to exactly delineate the tract.11
Complications like DLK, epithelial ingrowth, microbial keratitis and astigmatism can occur post-FB removal. DLK is a non-infectious inflammatory condition that involves the interface in 0.13%–18.9% of cases,23, 24, 25 for which underlying cause is not known.24 It is most common keratitis occurring post-LASIK14,25 and has been reported to occur following CFB removal also.14,26, 27, 28 Epithelial ingrowth was observed in 0%–3.9% of cases undergoing primary treatment and 10%–20% in retreatment cases29 with 79 % cases being picked up by 1st postoperative month.30 Presence of blood, fibres, DLK, ointment under the flap in immediate postoperative period are all associated with epithelial ingrowth. Epithelial defect that occurs post-CFB removal or tract of FB are also a risk factor for epithelial ingrowth.30 It has been suggested that whenever there is disruption in flap apposition, careful removal of all epithelial cells should be done to prevent epithelial ingrowth.15 In our case, epithelial debridement was done over and in the surrounding area before attempting to remove the FB. All corneal FB's carry a risk of associated infectious keratitis. In post-LASIK patients, CFB may lead to interface keratitis even without any sign of flap displacement.10,18 A keen eye for detecting interface infectious keratitis and early flap lift, scraping from interface and microbiological work up with irrigation with antimicrobials to prevent progression of infective keratitis is imperative.18,25 Significant astigmatism subsequent to corneal scar or secondary to thinning or movement of the LASIK flap is another complication post CFB removal regarding which proper counselling and patient awareness is necessary in such patients.1,9 Retreatment with flap lift or surface ablation procedures are an option for successful correction of the astigmatism.16 In our patient, none of the above described complications occurred till last follow-up.
Huang et al.,31 described a patient where dislocated LASIK flap with FB debris was mis-diagnosed as corneal abrasion. Attempt to remove the FBs by general practitioner in another patient led to flap lift with debris tracking below the flap.1 Thus all patients presenting to emergency department with CFB or trauma should be asked about past refractive surgery and should seek subspecialty care to prevent a delay in diagnosis and minimize potential complications.31 ASOCT serves as an additional useful tool that can help delineate type of LASIK flap (microkeratome or femtolasik)6; type, depth, location and path of FB2; flap apposition or displacement, interface apposition or separation, any breach in descemet's membrane,2 occult FB tract, occult stromal bed laceration, macrostriae, amount of anterior chamber reaction,11 and corneal thinning after FB removal.2
5. CONCLUSION
Management of FB post-LASIK poses a great challenge. Eliciting proper and accurate history about prior refractive surgery is of utmost importance in a patient presenting with trauma to the emergency clinic. One must be cognizant about the presence of a flap, to be able to recognise the flap integrity, depth of FB in relation to the flap, striae or any associated infection or inflammation. ASOCT is a useful adjuvant tool to delineate even the finest details with regard to the depth of corneal involvement. Prompt recognition and treatment of specific complications like DLK and epithelial ingrowth is equally important. Use of protective eye-wear must be emphasised during counselling in all patients undergoing refractive surgery especially in people involved in contact sports and military personnel. Flapless procedures like photorefractive keratectomy should be advocated wherever applicable as flap based procedures always carry the risk of flap dislodgement.
Patient consent
Consent to publish this case report has been obtained from the patient in writing - the authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that his name and initials will not be published and due efforts will be made to conceal the identity.
Source(s) of support
Nil.
Financial support
Nil.
Prior presentation
None.
None.
Funding
No funding or grant support
Authorship
All authors attest that they meet the current ICMJE criteria for authorship.
CRediT authorship contribution statement
Mona Bhargava: Conceptualization, Methodology, Supervision. Varsha Bhambhani: Writing – original draft, Writing – review & editing. Ahana Sen: Writing – original draft, Writing – review & editing. Aditi Johri: Methodology, Supervision, Writing – review & editing.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
None.
References
- 1.Crowther Katharine, Ellingham Roger. Complicated removal of corneal foreign bodies 18 months after laser in situ keratomileusis. J Cataract Refract Surg. 2005;31:851–852. doi: 10.1016/j.jcrs.2004.10.054. [DOI] [PubMed] [Google Scholar]
- 2.Bhargava M., Bhambhani V., Paul R.S. Anterior segment optical coherence tomography characteristics and management of a unique spectrum of foreign bodies in the cornea and anterior chamber. Indian J Ophthalmol. 2022;70(12):4284–4292. doi: 10.4103/ijo.IJO_878_22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cosar C.B., Rapuano C.J., Cohen E.J. Corneal laceration and intraocular foreign body in a post-LASIK eye. Cornea. 2002;21(2):234–236. doi: 10.1097/00003226-200203000-00025. [DOI] [PubMed] [Google Scholar]
- 4.Leung A.T., Rao S.K., Lam D.S. Traumatic partial unfolding of laser in situ keratomileusis flap with severe epithelial ingrowth. J Cataract Refract Surg. 2000;26(1):135–139. doi: 10.1016/s0886-3350(99)00326-0. [DOI] [PubMed] [Google Scholar]
- 5.Moshirfar M., Anderson E., Taylor N., Hsu M. Management of a traumatic flap dislocation seven years after LASIK. Case Rep Ophthalmol Med. 2011;2011 doi: 10.1155/2011/514780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kanclerz P., Khoramnia R. Flap thickness and the risk of complications in mechanical microkeratome and femtosecond laser in situ keratomileusis: a literature review and statistical analysis. Diagnostics. 2021;11(9):1588. doi: 10.3390/diagnostics11091588. Published 2021 Aug 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chaudhry N.A., Smiddy W.E. Displacement of corneal cap during vitrectomy in a post-LASIK eye. Retina. 1998;18(6):554–555. doi: 10.1097/00006982-199806000-00011. [DOI] [PubMed] [Google Scholar]
- 8.Agrawal S., Raj S.J., Modaboyina S., Bafna R.K., Gupta S., Das D. Management of impacted corneal foreign bodies: a review. IP Int J Ocular Oncol Oculoplasty. 2021;7(2):131–138. [Google Scholar]
- 9.Eisemann J., Carkeet A., Swann P.G. Large interface particles from LASIK surgery. Clin Exp Optom. 2006;89(4):253–256. doi: 10.1111/j.1444-0938.2006.00046.x. [DOI] [PubMed] [Google Scholar]
- 10.Cheng A.C., Rao S.K., Leung G.Y., Young A.L., Lam D.S. Late traumatic flap dislocations after LASIK. J Refract Surg. 2006;22(5):500–504. doi: 10.3928/1081-597X-20060501-13. [DOI] [PubMed] [Google Scholar]
- 11.Maki S., Hou J.H. Case report: penetrating corneal injury under an intact laser-assisted in situ keratomileusis flap. Optom Vis Sci. 2018;95(11):1083–1086. doi: 10.1097/OPX.0000000000001297. [DOI] [PubMed] [Google Scholar]
- 12.Prakash G., Sharma N., Choudary V., Titiyal J.S. Spontaneous, uncomplicated dissolution of a large cotton fiber in the laser in situ keratomileusis interface. Middle East Afr J Ophthalmol. 2012;19(3):343–345. doi: 10.4103/0974-9233.97960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Boutillier G., Hubault D., Muraine M. A surprise guest-insect larva under an uncomplicated laser-assisted in situ keratomileusis surgical flap. JAMA Ophthalmol. 2018;136(9) doi: 10.1001/jamaophthalmol.2018.3084. [DOI] [PubMed] [Google Scholar]
- 14.Pan J.C., Crawford G.J. Unusual complication after laser in situ keratomileusis: eyelash under the flap. J Cataract Refract Surg. 2007;33(3):540–541. doi: 10.1016/j.jcrs.2006.10.049. [DOI] [PubMed] [Google Scholar]
- 15.Porges Y., Landau D., Douieb J., Levinger S. Removal of corneal foreign bodies following laser in situ keratomileusis. J Refract Surg. 2001;17(5):559–560. doi: 10.3928/1081-597X-20010901-10. [DOI] [PubMed] [Google Scholar]
- 16.Jin George, Merkley Kevin. Laceration and partial dislocation of LASIK flaps 7 and 4 Years postoperatively with 20/20 visual acuity after repair. J Refract Surg. 1995;22 doi: 10.3928/1081-597X-20061101-11. Thorofare, N.J. 904-5. [DOI] [PubMed] [Google Scholar]
- 17.Lin P.H., Wang N.K., Hwang Y.S., Ma D.H., Yeh L.K. Bee sting of the cornea and conjunctiva: management and outcomes. Cornea. 2011;30(4):392–394. doi: 10.1097/ICO.0b013e3181f234a6. [DOI] [PubMed] [Google Scholar]
- 18.Choi J.A., Kim M.S. LASIK interface-captured foreign bodies after mild traumatic corneal scratch without flap displacement. Kor J Ophthalmol. 2012;26(3):222–225. doi: 10.3341/kjo.2012.26.3.222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Joffe S.N. The 25th anniversary of laser vision correction in the United States. Clin Ophthalmol. 2021;15:1163–1172. doi: 10.2147/OPTH.S299752. Published 2021 Mar 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McGwin G., Jr., Owsley C. Incidence of emergency department-treated eye injury in the United States. Arch Ophthalmol. 2005;123(5):662–666. doi: 10.1001/archopht.123.5.662. [DOI] [PubMed] [Google Scholar]
- 21.Xiao J.H., Zhang M.N., Jiang C.H., Zhang Y., Qiu H.Y. Laser in situ keratomileusis surgery is not safe for military personnel. Chin J Traumatol. 2012;15(2):77–80. [PubMed] [Google Scholar]
- 22.Camodeca A.J., Anderson E.P. StatPearls. Treasure Island (FL) StatPearls Publishing; April 21, 2022. Corneal foreign body. [PubMed] [Google Scholar]
- 23.Gritz D.C. LASIK interface keratitis: epidemiology, diagnosis and care. Curr Opin Ophthalmol. 2011;22(4):251–255. doi: 10.1097/ICU.0b013e3283477b52. [DOI] [PubMed] [Google Scholar]
- 24.Smith R.J., Maloney R.K. Diffuse lamellar keratitis. A new syndrome in lamellar refractive surgery. Ophthalmology. 1998;105(9):1721–1726. doi: 10.1016/S0161-6420(98)99044-3. [DOI] [PubMed] [Google Scholar]
- 25.Moshirfar M., Welling J.D., Feiz V., Holz H., Clinch T.E. Infectious and noninfectious keratitis after laser in situ keratomileusis Occurrence, management, and visual outcomes. J Cataract Refract Surg. 2007 Mar;33(3):474–483. doi: 10.1016/j.jcrs.2006.11.005. [DOI] [PubMed] [Google Scholar]
- 26.Baenninger P.B., Kaufmann C., Weisskopf F. Diffuse lamellar keratitis induced by a corneal foreign body six months after Femto-LASIK. KlinMonblAugenheilkd. 2014;231(4):307–308. doi: 10.1055/s-0034-1368275. [DOI] [PubMed] [Google Scholar]
- 27.Maeda I., Miyazaki D., Shimizu Y., Takeda S., Inoue Y., Shimizu M. Eye-shadow particles under a laser in situ keratomileusis flap following corneal trauma. Jpn J Ophthalmol. 2009;53(1):64–65. doi: 10.1007/s10384-008-0618-7. [DOI] [PubMed] [Google Scholar]
- 28.Weisenthal R.W. Diffuse lamellar keratitis induced by trauma 6 months after laser in situ keratomileusis. J Refract Surg. 2000;16(6):749–751. doi: 10.3928/1081-597X-20001101-12. [DOI] [PubMed] [Google Scholar]
- 29.Ting D.S.J., Srinivasan S., Danjoux J.P. Epithelial ingrowth following laser in situ keratomileusis (LASIK): prevalence, risk factors, management and visual outcomes. BMJ Open Ophthalmol. 2018;3(1) doi: 10.1136/bmjophth-2017-000133. Published 2018 Mar 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Asano-Kato N., Toda I., Hori-Komai Y., Takano Y., Tsubota K. Epithelial ingrowth after laser in situ keratomileusis: clinical features and possible mechanisms. Am J Ophthalmol. 2002;134(6):801–807. doi: 10.1016/s0002-9394(02)01757-9. [DOI] [PubMed] [Google Scholar]
- 31.Huang Y.H., Huang F.C. Ocular trauma. JAMA. 2012;308(7):710–711. doi: 10.1001/jama.2012.9348. [DOI] [PubMed] [Google Scholar]