Abstract
Purpose
To evaluate the experiences and outcomes of arthroscopic partial meniscectomy in symptomatic non-Wrisberg discoid lateral meniscus in children younger than 12 years old at a single center.
Methods
We retrospectively reviewed the medical records of all pediatric patients who were treated for non-Wrisberg discoid meniscus at our institute between 2013 and 2021. Patients were separated into 2 groups: Patients who underwent partial resection with saucerization (group A) or patients who underwent saucerization, tear repair, and fixation (group B). Clinical outcomes were compared between the 2 groups.
Results
A total of 20 patients (22 knees) were treated for non-Wrisberg discoid meniscus and included in this study. Nine patients underwent partial resection with saucerization (group A) whereas 11 patients underwent saucerization, tear repair, and fixation (group B). The average follow-up was 3 years (range 2-10 years). The results showed that 17 of the 20 patients had excellent outcomes whereas the other 3 had good outcomes after a minimum follow-up of 2 years. The average Knee Injury and Osteoarthritis Outcome Score for Children score was 93.
Conclusions
Arthroscopic saucerization of symptomatic non-Wrisberg discoid lateral meniscus, with additional repair as indicated results in excellent or good outcomes in children younger than 12 years of age.
Level of Evidence
Level III, case–control study.
Non-Wrisberg discoid meniscus is an abnormal congenital variant of the fibrocartilaginous meniscus of the knee in which the meniscus is discoid in shape rather than semilunar in shape.1 Most cases of discoid menisci involve the lateral meniscus; Davidson et al. reported female sex preponderance.2, 3, 4 It is not uncommon for the lateral discoid meniscus to be present bilaterally.2, 3, 4
The classification of discoid meniscus consists of 3 types according to the Watanabe system5 as follows: complete type, incomplete type, and the Wrisberg-ligament type. The reported incidence of discoid meniscus in the literature is between 0.4% and 17%.6,7 In the Caucasian population, it is less than 5%,8,9 rising to 12.5% in the Korean population10 and 17% in the Japanese population.11 The cause for this prevalence dispersal is unknown.
Most cases of lateral discoid meniscus are undiagnosed, as the malformation may show few to no symptoms.4 Surgical treatment consists of either partial or total meniscectomy, and reattachment to the tibia in the Wrisberg variant.12 Typically, these procedures are performed between 9 and 12 years of age.4,13,14
For symptomatic discoid meniscus, nonoperative treatment may consist of immobilization, restricted activities, and exercises of the quadriceps muscles.4 Indication for surgery is recommended only after failed nonoperative care for 3 to 6 months in symptomatic cases with persistent mechanical symptoms and/or pain.4 Surgical options of the non-Wrisberg discoid meniscus include partial removal of the torn portion and restoration of the normal semilunar configuration of the meniscus and/or reattachment of meniscus or total resection of the meniscus.15 In this study, only partial meniscectomy and/or repair was conducted. Symptomatic discoid menisci traditionally have been treated with total meniscectomy7; reports at that time showed considerable symptomatic improvement.15, 16, 17 However, more recent investigations have reported that total meniscectomy is associated with osteoarthritic changes on radiography as well as peripheral rim instability.10,11,16,18, 19, 20 The purpose of our study was to evaluate the experience and outcomes of arthroscopic partial meniscectomy in symptomatic non-Wrisberg discoid lateral meniscus in children younger than 12 years old at a single center. Our hypothesis was that arthroscopic discoid meniscus partial meniscectomy with or without repair in children younger than the age of 12 years is safe and effective at minimum 2-year follow-up.
The purpose of our study was to evaluate the experience and outcomes of arthroscopic partial meniscectomy in symptomatic non-Wrisberg discoid lateral meniscus in children younger than 12 years old at a single center. Our hypothesis was that arthroscopic discoid meniscus partial meniscectomy with or without repair in children under the age of 12 is safe and effective at minimum 2-year follow-up.
Methods
The clinical, radiologic, and operative records of all pediatric patients treated for meniscal disorders at our institute between 2013 and 2021 were reviewed retrospectively. Twenty patients were diagnosed with and subsequently treated for non-Wrisberg discoid meniscus at a single center by the senior surgeon. Two patients were diagnosed with bilateral discoid lateral menisci, 21 knees were classified as complete discoid menisci, and 1 knee was classified as incomplete discoid menisci. Two patients were diagnosed with discoid meniscus but refused surgery. Diagnosis was made based on patient history, supplemented by magnetic resonance imaging (MRI) findings supporting a diagnosis of discoid meniscus (a meniscal width that is greater than 1.5 cm).21 The inclusion criteria of this study were based on the presence of symptoms such as pain, restriction of movement, and abnormalities in gait in patients younger than the age of 12 with imaging consistent with discoid meniscus. We excluded patients who had imaging significant for discoid meniscus but were otherwise asymptomatic or those who refused to undergo surgical treatment. Treatment consisted of partial meniscectomy with saucerization in 9 cases (group A) and partial meniscectomy with saucerization (to restore the normal semilunar shape of the meniscus) and repair of the peripheral tear using FAST-FIX sutures (Smith & Nephew, Andover, MA) in the other 11 cases (group B). Saucerization included using shaving and cutting techniques where we aimed to keep 8 mm of the peripheral rim while recreating the normal semilunar shape of the meniscus (Fig 1). All surgeries were performed by a senior surgeon (L.N./V.G.) at a single center. Ethical approval and parental consent were obtained for each patient.
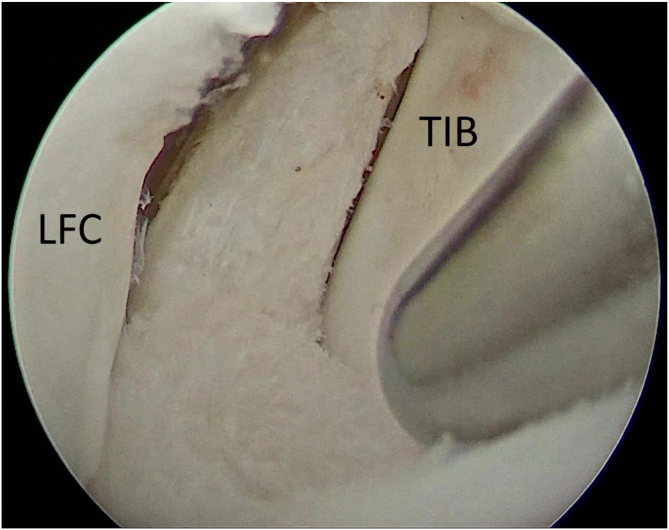
Fig 1.
View of the right knee joint form the anterolateral portal revealing a complete discoid meniscus with radial damage in the posterior horn, which was subsequently repaired and saucerized. Saucerization included using shaving and cutting techniques in which we aimed to keep 8 mm of the peripheral rim while recreating the normal semilunar shape of the meniscus. (LFC, lateral femoral condyle; TIB, tibial plateau.)
Each case of discoid meniscus was classified with the Watanabe classification5,22 by MRI or at the time of surgery. Nonoperative treatment was initially prescribed for patients, ranging from 3 to 6 months, and included limited activity, immobilization and/or bracing, and subsequently physiotherapy to increase range of motion and knee strength.
Ikeuchi’s7 classification was used to analyze the results. The classifications are excellent—full range of motion, no knee snapping and no pain; good—infrequent pain with exertion and full range of motion; fair—slight pain, knee snapping on motion and full range of knee motion; and poor—constant pain or recurrent locking of the knee, or both. We also used the Knee Injury and Osteoarthritis Outcome Score for Children (KOOS-Child)23,24 scoring system to evaluate pre- and postoperative knee function.
Surgical Technique
Patients were operated on under laryngeal anesthesia using the standard dual-portal technique with the standard 30° arthroscope. On arthroscopic examination, the meniscus was visualized and probed to determine the type of discoid meniscus, location, and type of potential tear (Fig 2). Meniscal stability was assessed and then partial central meniscectomy was performed, removing the discoid portion and any unstable/torn areas while trimming the meniscus down to a 6- to 8-mm remnant.16, 17, 18, 19, 20 Saucerization involved using a 4.2-mm size shaver to smooth out the inner rim and recreate the natural semilunar meniscus shape.16,17 In the group with longitudinal paracapsular tears of the posterior horn, meniscal paracapsular repair and reconstruction was performed using 2 to 3 Smith & Nephew “FAST-FIX” meniscal sutures (Fig 3).18, 19, 20 For cases with a longitudinal tear near the anterior portion of the meniscus, a lateral incision was made to allow for improved visualization and subsequent repair.18,19 The rehabilitation protocol was the same for both groups. Our rehabilitation protocol involved applying a cylinder splint and a brace, as well as an isometric exercise program followed by rest with gradual progression to full weight-bearing over several weeks.
Fig 2.
View from the anterolateral portal revealing a complete discoid lateral meniscus. (LFC, lateral femoral condyle.)
Fig 3.
View from the anterolateral portal. The upper and lower layers of the meniscus were debrided to expose bleeding. A longitudinal paracapsular tear of the posterior horn of meniscus was then revealed and repaired with 2 to 3 Smith & Nephew “FAST-FIX” meniscal sutures. (LFC, lateral femoral condyle; TIB, tibial plateau.)
Results
Twenty of our patients (9 boys, 11 girls) were treated for discoid meniscus, 2 bilaterally, totaling 22 knees in all. Eleven of those patients were diagnosed with a suspected discoid meniscal tear on MRI based on the presence of a linear hyperintensity extending to either the superior or inferior meniscal surface. The average age was 8 years 4 months (ranging from 3 years, 2 months to 11 years, 6 months) at time of surgery. Minimum follow-up was 2 years, with an average of 3 years and ranged from 2 to 10 years. All 22 knees involved the lateral meniscus. All 22 knees had good-to-excellent results and an average KOOS-Child score of 93 at a minimum of 2 year follow-up. There was a total of 19 excellent (86%) and 3 good (14%) results at the time of the most recent follow up (Figs 4 and 5) (Table 1). Postoperative radiographs were not significant for any osteoarthritic changes for all patients according to the Kellgren and Lawrence classification system25 (Fig 6). Nonoperative treatment was unsuccessful in all 20 cases and no patients were lost to follow-up. There were 2 patients (10%) who had bilateral knee involvement and 1 patient (5%) had a trauma, 1 year after surgery and tore the initially repaired meniscus, was not reparable and required partial resection. All cases were good to excellent at 2 years’ follow-up. Both groups performed comparatively (good-to-excellent outcomes).
Fig 4.

Cases distributed by sex.
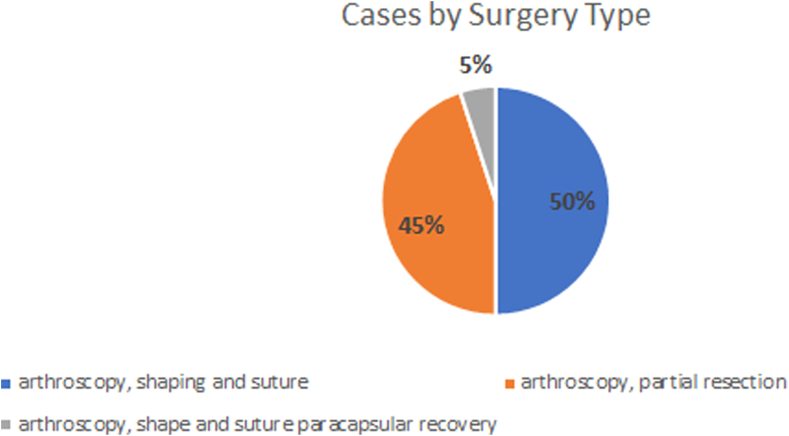
Fig 5.
Cases distributed by surgery type.
Table 1.
Patients Sex, Age, Date of Surgery, and Follow-Up Status
| Case No. | Sex | Age (y + mo) | Date of Surgery | Type of Surgery | Tear Present? | Tear Pattern | Number of Stitches | 1 Month Follow-Up | Most Recent Follow-Up |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Female | 7+4 | 2020 | Arthroscopy, shaping and suture | Yes | Peripheral | 2 | Excellent | Excellent (3 years) |
| 2 | Female | 6+3 | 2020 | Arthroscopy, shaping and suture | Yes | Peripheral | 2 | Excellent | Excellent (3 years) |
| 3 | Female | 11+5 | 2020 | Arthroscopy, partial resection | No | N/A | N/A | Good | Good (3 years) |
| 4 | Female | 6+7 | 2019 | Arthroscopy, shape and suture | Yes | Radial | 3 | Excellent | Good (3 years) |
| 5 | Female | 7+7 | 2020 | Arthroscopy, shape and suture | Yes | Longitudinal | 3 | Excellent | Excellent (2 years) |
| 6 | Female | 10+1 | 2020 | Arthroscopy, shape and suture | Yes | Radial | 2 | Excellent | Excellent (2 years) |
| 7 | Female | 10+12 | 2019 | Arthroscopy, partial resection | No | N/A | N/A | Excellent | Excellent (4 years) |
| 8 | Female | 9+4 | 2018 | Arthroscopy, partial resection | No | N/A | N/A | Excellent | Excellent (4 years) |
| 9 | Female | 11+9 | 2014 | Arthroscopy, partial resection | No | N/A | N/A | Excellent | Excellent (8 years) |
| 10 | Male | 11+3 | 2019 | Arthroscopy, partial resection | No | N/A | N/A | Excellent | Excellent (4 years) |
| 11 | Male | 11+4 11+7 |
2019 | Arthroscopy, shaping and suture for the right knee and arthroscopy, partial resection for the left knee after 3 months | Yes No |
PeripheralN/A | 3N/A | Good | Excellent (4 years) |
| 12 | Female | 3+1 | 2021 | Arthroscopy, shape and suture paracapsular recovery | Yes | Radial | 3 | Excellent | Excellent (2 years) |
| 13 | Male | 10+7 | 2018 | Arthroscopy, shape and suture | Yes | Longitudinal | 3 | Excellent | Excellent (4 years) |
| 14 | Male | 11+9 | 2018 | Arthroscopy, shape and suture | Yes | Peripheral | 2 | Excellent | Excellent (5 years) |
| 15 | Male | 8+12 | 2018 | Arthroscopy, shape and suture | Yes. | Excellent | Excellent (5 years) | ||
| Simple | 2 | ||||||||
| 16 | Male | 9+2 | 2013 | Arthroscopy, partial resection | No | N/A | N/A | Excellent | Excellent (10 years) |
| 17 | Male | 9+2 | 2018 | Arthroscopy, partial resection | No | N/A | N/A | Excellent | Excellent (5 years) |
| 18 | Male | 10+11 | 2015 | Arthroscopy, partial resection | No | N/A | N/A | Excellent | Excellent (7 years) |
| 19 | Female | 11+3 11+7 |
2019 | Arthroscopy, shape and suture for both knees, 4 months apart | Yes | Peripheral Longitudinal |
3 3 |
Poor | Good (4 years) |
| 20 | Male | 6+1 | 2019 | Arthroscopy, partial resection | No | N/A | N/A | Good | Excellent (3 years) |
N/A, not available.
Fig 6.
Postoperative anteroposterior radiograph of the left knee showing no significant osteoarthritic changes.
Discussion
The most important finding based on our results is that arthroscopic discoid lateral meniscus partial meniscectomy with or without repair shows good-to-excellent outcomes, is highly safe, and supports a standard of treatment going forward, especially when operated on younger patients.9,24 The primary characteristic for diagnosis of discoid meniscus is a history of snapping or clicking in the knee7; yet, recent studies have reported pain being the more common complaint preoperatively.2,13,26 Numerous studies have indicated that plain radiographs are not useful in establishing the diagnosis; however, arthrography and arthroscopy are supportive.3,26, 27, 28, 29, 30 MRI also proved to be helpful for diagnosis, with the added benefit of an increased sensitivity in sensing meniscal tears.31, 32, 33 Assessment of the shape and stability of a symptomatic discoid meniscus should be the foundation for determining treatment and assessed using arthroscopic evaluation. Partial meniscectomy—with or without tear repair—and preservation of the peripheral rim done arthroscopically should be the treatment of choice for persistently symptomatic non-Wrisberg discoid menisci in children.12,22,23 In addition, it is important to note that partial meniscectomy with suturing has been suggested to have fewer complications (such as decreased incidence of mediolateral instability and joint laxity) and better outcomes than total meniscectomy.10,11 We decided to use the KOOS-Child self-questionnaire due to its simple language that allows children to easily understand the questions with minimal assistance from their guardian, along with that we also found the content to be easily translated to Georgian language without loss of context. The main limiting factor in arthroscopic discoid meniscus repair is high technical demand required for a successful surgery.24 Surgical repair of the posterior capsular attachment of the posterior horn of the meniscus can be used as treatment and may play an important role in protecting the re-rupture due to abnormal shear forces.34, 35, 36 In addition, a potential complication of saucerization and partial resection is osteochondritis dissecans of the lateral femoral condyle31; future larger-scale trials should be conducted. Our study indicates that discoid lateral meniscus more commonly affects female patients more than male patients and more often presents symptomatically at a younger age (the average age for female patients was 8.2 years, whereas the average age for male patients was 9.4 years), as is consistent with previous studies.4,37, 38, 39
Limitations
The main limiting factors of this study was the smaller sample size and shorter follow-up time, in some cases. Another limiting factor was the fact that this was a retrospective study, not a randomized study, without a control group. In addition, several variables were not obtainable postoperatively such as postoperative MRIs, body mass index, and alignment. Due to the lack of a centralized MRI storage system in our country, patients were asked to bring their preoperative MRI discs on most recent follow-up; however, due to the nature of the longer follow-up times, the patients have either lost them or forgot to get them.
Conclusions
Arthroscopic saucerization of symptomatic non-Wrisberg discoid lateral meniscus, with additional repair as indicated, results in excellent or good outcomes in children younger than 12 years of age.
Disclosure
All authors (G.A.R., L.N., V.G., M.A.M., T.T., I.K., M.Z.) report no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
References
- 1.Young R.B. In: Cleland J., MacKay J.Y., Young R.B., editors. Vol. 1. Williams and Norgate; London: 1889. The external semilunar cartilage as a complete disc; p. 179. (Memoirs and memoranda in anatomy). [Google Scholar]
- 2.Watson-Jones R. Specimen of internal semilunar cartilage as a complete disc. Proc R Soc Med. 1930;23:588. doi: 10.1177/003591573002301141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cave E.F., Staples O.S. Congenital discoid meniscus of cause of internal derangement of the knee. Am J Surg. 1941;54:371–376. [Google Scholar]
- 4.Davidson D., Letts M., Glasgow R. Discoid meniscus in children: Treatment and outcome. Can J Surg. 2003;46:350–358. [PMC free article] [PubMed] [Google Scholar]
- 5.Watanabe M., Takeda S., Ikeuchi H. 3rd ed. Igaku-Shoin; Tokyo: 1979. Atlas of arthroscopy; pp. 75–130. [Google Scholar]
- 6.Barthel T., Pesch R., Lippert M.J., Lutz G. Arthroskopische Behandlung des lateralen Scheibenmeniskus. Arthroskopie. 1995;8:12–18. [in German] [Google Scholar]
- 7.Ikeuchi H. Arthroscopic treatment of the discoid lateral meniscus: technique and long-term results. Clin Orthop. 1982;167:19–28. [PubMed] [Google Scholar]
- 8.Clark C.R., Ogden J.A. Development of the menisci of the human knee joint. Morphologic changes and their potential role in childhood meniscal injuries. J Bone Joint Surg Am. 1983;65:538–547. [PubMed] [Google Scholar]
- 9.Nathan P.A., Cole S.C. Discoid meniscus: A clinical and pathological study. Clin Orthop. 1969;64:107–113. [PubMed] [Google Scholar]
- 10.Kim S.J., Kim D.W., Min B.H. Discoid lateral meniscus associated with anomalous insertion of the medial meniscus. Clin Orthop. 1995;315:234–237. [PubMed] [Google Scholar]
- 11.Hede A., Larsen E., Sandberg H. Partial versus total meniscectomy. A prospective, randomised study with long-term follow-up. J Bone Joint Surg Br. 1992;74:118–121. doi: 10.1302/0301-620X.74B1.1732238. [DOI] [PubMed] [Google Scholar]
- 12.Ozeki N., Koga H., Nakamura T., et al. Surgical repair of symptomatic Wrisberg variant discoid lateral mensicus with pull-out repair and capsulodesis. Arthrosc Tech. 2021;11:e61–e68. doi: 10.1016/j.eats.2021.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Barnes C.L., McCarthy R.E., Vanderschilden J.L., McConnell J.R., Nusbickel F.R. Discoid lateral meniscus in a young child: Case report and review of the literature. J Pediatr Orthop. 1988;8:707–709. doi: 10.1097/01241398-198811000-00016. [DOI] [PubMed] [Google Scholar]
- 14.Chen Y.C. Arthroscopic meniscectomy of the discoid meniscus. Arthroscopy. 1988;4:131–135. [Google Scholar]
- 15.Okazaki K., Miura H., Matsuda S., Hashizume M., Iwamoto Y. Arthroscopic resection of the discoid lateral meniscus: long-term follow-up for 16 years. Arthroscopy. 2006;22:967–971. doi: 10.1016/j.arthro.2006.04.107. [DOI] [PubMed] [Google Scholar]
- 16.Raber D.A., Friederich N.F., Hefti F. Discoid lateral meniscus in children: Long-term follow-up after total meniscectomy. J Bone Joint Surg Am. 1998;80:1579–2586. doi: 10.2106/00004623-199811000-00003. [DOI] [PubMed] [Google Scholar]
- 17.Hayashi L.K., Yamaga H., Ida K., Miura T. Arthroscopic meniscectomy for discoid lateral meniscus in children. J Bone Joint Surg Am. 1988;70:1495–1500. [PubMed] [Google Scholar]
- 18.Ahn J.H., Lee S.H., Yoo J.C., Lee Y.S., Ha H.C. Arthroscopic partial meniscectomy with repair of the peripheral tear for symptomatic discoid lateral meniscus in children: results of minimum 2 years of follow-up. Arthroscopy. 2008;24:888–898. doi: 10.1016/j.arthro.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 19.Ahn J.H., Kim K.I., Wang J.H., Jeon J.W., Cho Y.C., Lee S.H. Long-term results of arthroscopic reshaping for symptomatic discoid lateral meniscus in children. Arthroscopy. 2015:867–873. doi: 10.1016/j.arthro.2014.12.012. [DOI] [PubMed] [Google Scholar]
- 20.Yoo W.J., Jang W.Y., Park M.S., et al. Arthroscopic treatment for symptomatic discoid meniscus in children: Midterm outcomes and prognostic factors. Arthroscopy. 2015;31:2327–2334. doi: 10.1016/j.arthro.2015.06.032. [DOI] [PubMed] [Google Scholar]
- 21.Yoo W.J., Lee K., Moon H.J., et al. Meniscal morphologic changes on magnetic resonance imaging are associated with symptomatic discoid lateral meniscal tear in children. Arthroscopy. 2012;28:330–336. doi: 10.1016/j.arthro.2011.08.300. [DOI] [PubMed] [Google Scholar]
- 22.Tiftikçi U., Serbest S. Repair of isolated horizontal meniscal tears with all-inside suture materials using the overlock method: Outcome study with a minimum 2-year follow-up. J Orthop Surg Res. 2016;11:131. doi: 10.1186/s13018-016-0466-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Roos E.M., Roos H.P., Lohmander L.S., Ekdahl C., Beynnon B.D. Knee injury and osteoarthritis outcome score (KOOS)—development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28:88–96. doi: 10.2519/jospt.1998.28.2.88. [DOI] [PubMed] [Google Scholar]
- 24.Örtqvist M., Roos E.M., Broström E.W., Janarv P.M., Iversen M.D. Development of the Knee Injury and Osteoarthritis Outcome Score for children (KOOS-Child): Comprehensibility and content validity. Acta Orthop. 2012;83:666–673. doi: 10.3109/17453674.2012.747921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schiphof D., Boers M., Bierma-Zeinstra S.M. Differences in descriptions of Kellgren and Lawrence grades of knee osteoarthritis. Ann Rheum Dis. 2008;67:1034–1036. doi: 10.1136/ard.2007.079020. [DOI] [PubMed] [Google Scholar]
- 26.Silverman J.M., Mink J.H., Deutsch A.L. Discoid menisci of the knee: MR imaging appearance. Radiology. 1989;173:351–354. doi: 10.1148/radiology.173.2.2798867. [DOI] [PubMed] [Google Scholar]
- 27.Kaplan E.B. Discoid lateral meniscus of the knee joint. J Bone Joint Surg Am. 1957;39:77–80. [PubMed] [Google Scholar]
- 28.Aichroth P.M., Patel D., Marx C. Congenital discoid lateral meniscus in children: A follow-up study and evolution of management. J Bone Joint Surg Br. 1991;73:932–936. doi: 10.1302/0301-620X.73B6.1955439. [DOI] [PubMed] [Google Scholar]
- 29.Bellier G., DuPont J.Y., Larrain M., Caudron C., Carlioz H. Lateral discoid menisci in children. Arthroscopy. 1989;5:52–56. doi: 10.1016/0749-8063(89)90092-3. [DOI] [PubMed] [Google Scholar]
- 30.Bramson R.T., Staple T.W. Double contrast knee arthrography in children. AJR Am J Roentgenol. 1975;123:838–844. doi: 10.2214/ajr.123.4.838. [DOI] [PubMed] [Google Scholar]
- 31.Hall F.M. Arthrography of the discoid lateral meniscus. AJR Am J Roentgenol. 1977;218:993–1002. doi: 10.2214/ajr.128.6.993. [DOI] [PubMed] [Google Scholar]
- 32.Haveson S.B., Rein B.I. Lateral discoid meniscus of the knee: Arthrographic diagnosis. AJR Am J Roentgenol. 1970;109:581–585. doi: 10.2214/ajr.109.3.581. [DOI] [PubMed] [Google Scholar]
- 33.Blacksin M.F., Greene B., Bothelho G. Bilateral diskoid medial menisci diagnosed by magnetic resonance imaging: A case report. Clin Orthop. 1992;285:214–216. [PubMed] [Google Scholar]
- 34.Washington E.R., Root L., Liener U.C. Discoid lateral meniscus in children: Long-term follow-up after excision. J Bone Joint Surg Am. 1995;77:1357–1361. doi: 10.2106/00004623-199509000-00011. [DOI] [PubMed] [Google Scholar]
- 35.Campbell A.L., Pace J.L., Mandelbaum B.R. Discoid lateral meniscus. Curr Rev Musculoskelet Med. 2023;16:154–161. doi: 10.1007/s12178-023-09824-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Perkins C.A., Busch M.T., Christino M.A., Willimon S.C. Saucerization and repair of discoid lateral menisci with peripheral rim instability: Intermediate-term outcomes in children and adolescents. J Pediatr Orthop. 2021;41:23–27. doi: 10.1097/BPO.0000000000001695. [DOI] [PubMed] [Google Scholar]
- 37.Woods G.W., Whelan J.M. Discoid meniscus. Clin Sports Med. 1990;9:695–706. [PubMed] [Google Scholar]
- 38.Kelly B.T., Green D.W. Discoid lateral meniscus in children. Curr Opin Pediatr. 2002;14:54–61. doi: 10.1097/00008480-200202000-00010. [DOI] [PubMed] [Google Scholar]
- 39.Randhawa S., Tran E., Segovia N.A., Ganley T., Tompkins M., Ellis H., et al. Epidemiological study of the discoid meniscus: Investigating demographic-based predictors in large-scale claims database. Cureus. 2021;13 doi: 10.7759/cureus.20050. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.