Abstract
Tuberculous dactylitis is infrequently seen after the age of 6 years. The index and middle fingers are the most common sites. Early diagnosis is essential to eradicate the infection. Delay in diagnosis and management leads to extensive involvement which may require surgical intervention. The current literature reveals conservative management gives satisfactory results in early stages. Though surgical intervention in Tuberculous dactylitis is seldom required, delay in diagnosis and management leads to extensive involvement of the bone and sequestration which does not respond to Anti Tubercular Therapy and needs staged surgical interventions. We report a case of an 11-year-old girl who presented to us after extensive involvement of 2nd and 3rd metacarpals and failed to respond to ATT even after 1.5 years of medication. She required staged surgeries to eradicate the infection which led to loss of 2nd and 3rd metacarpals. Complex reconstructive procedures of hand were required in stages and the bone loss was managed with non-vascularized Fibular strut graft. At 2 years of follow up, there is complete incorporation of the graft, and the patient has satisfactory functions of the hand and can carry out activities of daily living with ease.
Keywords: Tuberculosis, Dactilytis, Metacarpal Loss, Reconstruction
Introduction
Extrapulmonary Tuberculosis (TB) is less prevalent than Pulmonary Tuberculosis with an incidence of 10 percent [1]. Tuberculous dactylitis is much more infrequent especially after the age of 6 years [2]. The index and middle fingers are the most common sites to be involved [3, 4]. TB of the metacarpals and phalanges is difficult to diagnose in the early stages of disease [5]. It should be a presumptive diagnosis in cases of long-standing pain, swelling and discharging sinus of the metacarpals which does not subside with oral antibiotics.
The current literature regarding the management of TB dactylitis reveals that conservative management gives satisfactory results without the need for surgical intervention [5, 6]. Surgical intervention is required only when there is complete destruction of the bone leading to sequestrum formation which does not respond to Anti Tuberculous Therapy (ATT).
We report a case of an 11-year-old girl with Tuberculous dactylitis which failed to respond to anti tuberculous medication and required extensive debridement and complex reconstruction of the hand. The patient and her parents gave consent for giving their details for this case report.
Case Report
An 11-year-old girl presented to us with pain, swelling and discharging sinuses in the left hand for 1.5 years. Initially patient complained of pain in the middle finger. There was no history of trauma. Pain was insidious in onset and gradually progressed and led to swelling of the left hand. She was managed at another center by incision and drainage and oral Cephalosporins. As there was no improvement in symptoms debridement was done again. The tissue fluid was positive for Cartridge- based nucleic acid amplification test (GeneXpert) and the histopathological examination revealed granulomas consistent with Tuberculosis. Anti Tuberculous therapy (ATT) with four-drug regimen was initiated. The sinuses were active and there was persistent discharge even after receiving ATT for 1.5 years.
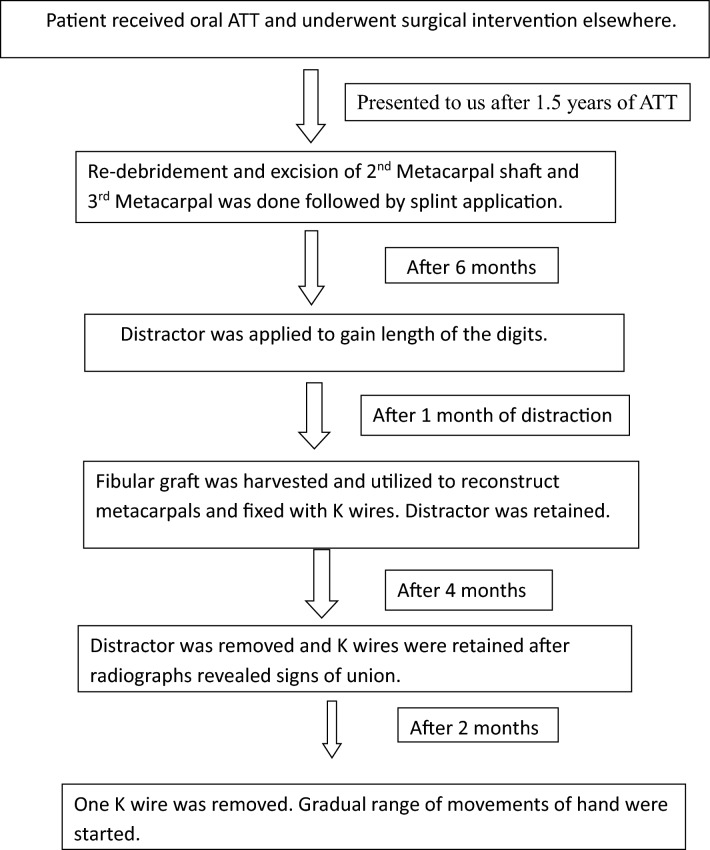
Patient presented to us at this point for evaluation and further management. On examination, there was diffuse swelling of the hand and a non-healing ulcer of about 4*5 cm over the dorsum of left hand with surrounding discoloration,purulent discharge and sinuses of 1 × 1 cm on the dorsum and on the palmar aspect between middle and ring fingers (Fig. 1).There was local rise of temperature with diffuse tenderness in the dorsal and palmar aspect and movements of digits were painful. Radiographs revealed extensive involvement of 2nd, 3rd, 4th metacarpals and proximal phalanx of 3rd digit (Fig. 2) with medullary expansion, cortical erosion, periosteal reaction and sequestration of 2nd, 3rd, 4th metacarpals, loss of 3rd MCP joint space and destruction of articular margins. MRI of the hand revealed changes of acute on chronic osteomyelitis involving 2nd, 3rd, 4th metacarpals, base of 3rd proximal phalanx and Carpal bones with collection surrounding metacarpals and wrist joint suggestive of septic arthritis of MCP joints and wrist (Fig. 3). Blood investigations of the child revealed no immuno-compromised state.
Fig. 1.
Clinical pictures of the patient at presentation showing swelling in the dorsal and volar aspects of the hand with discoloration of the skin and discharging sinuses in the dorsum and in the palmar aspect of hand between middle and ring fingers
Fig. 2.
Radiographs at presentation showing soft tissue edema, with medullary expansion, cortical erosion, periosteal reaction and sequestration of 2nd, 3rd and 4th metacarpals. The 3rd MCP joint is involved in the disease process with loss of joint space and destruction of articular margins
Fig. 3.
T2-weighted images of MRI shows osteomyelitic changes in 2nd, 3rd and 4th metacarpals with edema and collection surrounding the metacarpals, MCP joints and wrist
Owing to the extensive nature of the disease, re-debridement was planned. Dorsal approach was utilized. Second and third metacarpals were extensively involved with sequestration and devitalized tissue surrounding them. Purulent discharge was seen around the metacarpals with osteomyelitic changes in the entire length of 3rd metacarpal and shaft of 2nd metacarpal. Thorough debridement of the granulation tissue and sinus tracts was performed. Shaft of 2nd metacarpal and the entire 3rd metacarpal were excised (Fig. 4). Only the head of the 2nd metacarpal was left in situ as it was not involved. As the bone quality did not allow application of external fixator at this stage, a below elbow splint was applied. The tissue and bone samples were sent for bacterial and histopathological examination. The reports were consistent with Tuberculous infection and negative for secondary bacterial infection. There was no antibiotic resistant. The patient improved clinically after this intervention and there was healing of all sinuses.
Fig. 4.

Intraoperative pictures of the excised 2nd and 3rd metacarpals suggestive of sequestration of the entire bone
After 6 months when the infection was quiescent, there was shortening of the 2nd and 3rd digits due to loss of intervening bone (Fig. 5a, b). To gain the length of the digits Universal Mini External Fixator (UMEX) with distractors was applied in this stage. Two distractors were applied, one for each digit. Proximal holding points were in the carpus with two Schanz pins in proximal carpus and two in distal carpal row. The distal holding points were in the proximal phalanges with two Schanz pins in each of 2nd and 3rd digits. All the Schanz pins were placed in anteroposterior plane. Distractors were connected to Schanz pins as two separate units to regain the length of the two digits (Fig. 6a, b). Distraction was started on the second post operative day at the rate of 0.5 mm twice a day.
Fig. 5.
a Clinical images after stage 1 debridement show healing of the ulcer, short 2nd and 3rd digits. b Radiological image after debridement suggestive of quiescence of infection
Fig. 6.
a, b Clinical pictures and radiographs after stage 2 surgery show the configuration of the UMEX fixator which was applied to distract and regain the length of the 2nd and 3rd digits
After 1 month, appropriate length was achieved and fibular graft was harvested, and it was used to reconstruct the 2nd and 3rd metacarpals. As the 3rd metacarpal was completely excised, the fibular strut graft was placed aiming for arthrodesis of 3rd metacarpophalangeal joint in functional position. It was fixed with a transfixing K wire from proximal phalanx to carpus. As the head of the 2nd metacarpal was not involved, the strut graft was placed between the intact head and carpals. It was fixed with a horizontal K wire holding the 2 struts (Fig. 7). The distractor was retained for rotational stability.
Fig. 7.

Radiographs after stage 3 surgery showing placement of Fibular strut graft in the place of 2nd and 3rd metacarpal and fixation with K wires. One K wire was passed from proximal phalanx of 3rd digit to carpus and another K wire was passed horizontally to fix the two strut grafts
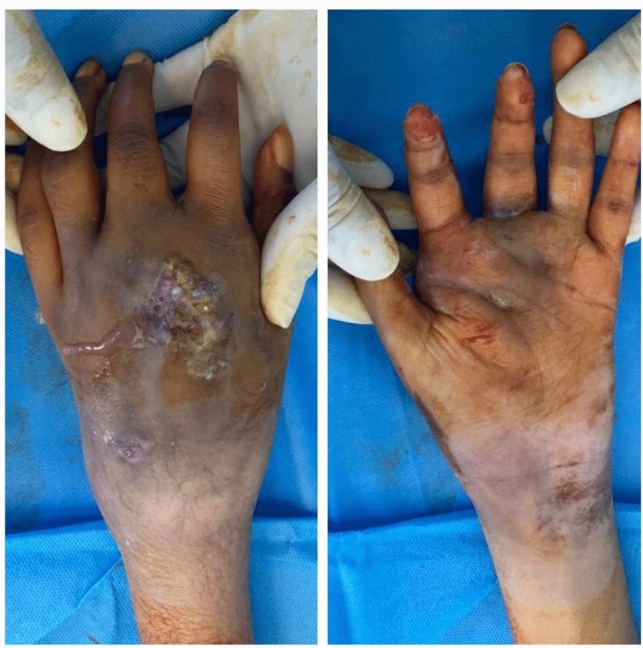
Her follow up radiographs revealed incorporation of the fibular graft at 4 months (Fig. 8). The distractor was removed then. After 2 months, vertical K wire passing through the 3rd digit was removed. Horizontal K wire was retained (Fig. 9, 10, 11). Below elbow splint was given and a gradual range of movements of the hand were started. The timeline of management (Fig. 12) reveals her entire duration of treatment.
Fig. 8.

At 4 months, post-stage 3 surgery the AP and Oblique radiographs reveal incorporation of the graft. The distractor was removed at this stage but the K wires were retained
Fig. 9.

Radiograph at 6 months follow up reveal incorporation of the Fibula strut graft which was placed in the place of 2nd metacarpal. The horizontal K wire was retained till complete incorporation
Fig. 10.

Radiographs at 2 years follow up show complete incorporation of both the strut grafts, arthrodesis of 3rd MCP joint and restoration of articular surface of 2nd MCP joint
Fig. 11.

a Clinical pictures at 2 years follow up showing well healed soft tissue and near normal restoration of the length of digits. b Clinical images of the patient carrying out activities of daily living with ease
Fig. 12.
Timeline of treatment
At 2 years follow up, the radiographs revealed complete incorporation of the graft (Fig. 10), and the patient has satisfactory functions of the hand and can carry out day to day activities with comfort (Fig. 11a, b).
QuickDASH score [7] was utilized to assess her hand function (Table 1). Her score improved to 9 from the preoperative score of 65.
Table 1.
QuickDASH score [7] {(sum of n responses/n)–1} × 25
| Parameter | Preoperative score | Postoperative- 2 years follow up score |
|---|---|---|
| Open a tight jar | 5 | 1 |
| Do heavy household chores | 5 | 3 |
| Carry shopping bag | 5 | 1 |
| Wash your bag | 5 | 1 |
| Use knife to cut | 5 | 2 |
| Impact on recreational activities | 2 | 2 |
| Interference with social activities | 4 | 1 |
| Limitation in work | 4 | 1 |
| Upper limb pain | 3 | 1 |
| Tingling | 2 | 1 |
| Difficulty in sleeping due to pain | 2 | 1 |
Discussion
Tuberculous dactylitis is more common in children. 85% of patients with TB in metacarpals and phalanges are reported in less than 6 years of age [2]. Concomitant active pulmonary tuberculosis is demonstrable in only one-third of patients [8]. TB of small bones of hand generally presents as a painless swelling which if not treated leads to discharging sinuses and eventually leads to destruction of the bone. Cystic expansion of the short tubular bones gives the appearance of “Spina Ventosa” on radiographs [8]. Early diagnosis is crucial in the management of these patients. Delay in diagnosis can jeopardize the functional outcome [9].
Subasi et al. [3] reported seven patients with an age range of 3 to 6 years who were diagnosed with TB dactylitis. All the patients were managed with ATT given for 1.5 years with complete subsidence of infection and satisfactory results. Our patient had no remission despite Anti Tuberculous drugs were given for 1.5 years. Her investigations revealed no drug resistance. The probable cause of unresponsiveness to the therapy could be a delay in the treatment and extensive sequestration of multiple metacarpals which could have hampered the drug penetration [10].
Ritz et al. [11] reviewed 37 cases of TB dactylitis in children and adolescents. They mentioned that though surgery has a limited role, it would play a supportive role in case of sequestrum formation which requires debridement. Bandyopadhyay et al. [9] report a case of TB dactylitis in a 2-year-old boy which was managed with excision of the 3rd metacarpal followed by strut graft from fibula [9]. Our patient required reconstruction of the two rays due to sequestration of two metacarpals. As per our knowledge, this is the first case report in literature where there was loss of two metacarpals which required reconstruction. Maini et al. described free metatarsal transfer for metacarpal loss. However they utilized if to manage a case of Giant Cell Tumor of metacarpal [12].There are also reports of the use of non-vascularized fibular graft after tumor excision leading to metacarpal loss [13, 14]. Our case also required Fibular strut graft to reconstruct the metacarpals. Non-vascularized fibular strut graft is easy to harvest and provides an excellent functional outcome when used as intercalary autograft in cases of bone loss [13, 14].
The challenges in our case were non- responsiveness of the disease secondary to extensive bony involvement, poor mineralization of bone at the outset which did not permit application of the external fixator in stage 1, shortening of the digits after debridement and complete loss of 3rd metacarpophalangeal joint. We managed all these issues in stages. Based on our experience, we recommend extensive debridement to eradicate the disease, gaining length of the digits followed by reconstruction with Fibular strut graft for such cases.
Conclusion
Tuberculous dactylitis is rarely encountered after the age of 6 years. Delay in diagnosis and failed response to oral Anti Tubercular drugs in TB dactylitis may warrant complex staged reconstructive procedures to provide good functional outcome.
Acknowledgements
We would like to acknowledge the contribution of Dr. Atul Bhaskar, Dr. Anil Agarwal, and Dr. Federico Canavese.
Data availability
Not applicable.
Declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standard statement
This article does not contain any studies with human or animal subjects performed by the any of the authors.
Informed consent
For this type of study informed consent is not required.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Nguyen Ngoc S, Nguyen Thai H, Van Vu Q, Vu Tung L, Nguyen Ngoc R, Nguyen VH. Late discovering spina ventosa: a case report. Int Med Case Rep J. 2021;14:449–453. doi: 10.2147/IMCRJ.S318003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Salimpour R, Salimpour P. Picture of the month. Tuberculous dactylitis. Archives of Pediatrics and Adolescent Medicine Journal. 1997;151(8):851–852. doi: 10.1001/archpedi.1997.02170450101018. [DOI] [PubMed] [Google Scholar]
- 3.Subasi M, Bukte Y, Kapukaya A, Gurkan F. Tuberculosis of the metacarpals and phalanges of the hand. Annals of Plastic Surgery. 2004;53(5):469–472. doi: 10.1097/01.sap.0000130708.80606.6a. [DOI] [PubMed] [Google Scholar]
- 4.Fairag R, Hamdi A. Tuberculous dactylitis: case presentation and functional outcome. Journal of Orthopaedic Case Report. 2016;6(3):22–24. doi: 10.13107/jocr.2250-0685.484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Martini M, Benkeddache Y, Medjani Y, Gottesman H. Tuberculosis of the upper limb joints. International Orthopaedics. 1986;10(1):17–22. doi: 10.1007/BF00266268. [DOI] [PubMed] [Google Scholar]
- 6.Benkeddache Y, Gottesman H. Skeletal tuberculosis of the wrist and hand: A study of 27 cases. The Journal of Hand Surgery. 1982;7(6):593–600. doi: 10.1016/S0363-5023(82)80109-3. [DOI] [PubMed] [Google Scholar]
- 7.Beaton DE, Wright JG, Katz JN, Upper Extremity Collaborative Group Development of QuickDASH: comparison of three item-reduction approaches. The Journal of Bone Joint Surgery America. 2005;87(5):1038–1046. doi: 10.2106/JBJS.D.02060. [DOI] [PubMed] [Google Scholar]
- 8.Gyanshankar PM, Dhamgaye TM, Amol BF. Spina ventosa discharging tubercle bacilli–a case report. Indian Journal of Tuberculosis. 2009;56(2):100–103. [PubMed] [Google Scholar]
- 9.Ranadeb B, Arindam M, Rajib KM. Case report: “spina ventosa” tuberculous dactylitis in a 2-year-old boy - a very rare disease. The Open Orthopaedics Journal. 2012;6:118–120. doi: 10.2174/1874325001206010118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dhammi et al. Current Concepts in Diagnosis & Management Of Osteoarticular Tuberculosis, Orthopaedic Journal of M P Chapter. 2020. Vol. 26. Issue 1
- 11.Ritz N, Connell T, Tebruegge M, Johnstone B. Curtis N Tuberculous dactylitis-an easily missed diagnosis. European Journal of Clinical Microbiology & Infectious Diseases. 2011;30(11):1303–1310. doi: 10.1007/s10096-011-1239-5. [DOI] [PubMed] [Google Scholar]
- 12.Maini L, Cheema G, Yuvarajan P, Gautam V. Free osteoarticular metatarsal transfer for giant cell tumor of metacarpal—a surgical technique. Journal of hand and microsurgery. 2011;3:89–92. doi: 10.1007/s12593-011-0048-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Isma SP, Irsan II, Rahaditya IG, Huwae TE, Santoso AR. Free non-vascularized fibular graft reconstruction after resection of metacarpal unicameral bone cyst: A case report. Molecular and Clinical Oncology. 2019;103:339–342. doi: 10.3892/mco.2019.1803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dhatt S, Tripathy SK, Goyal T, et al. Aneurysmal bone cyst of fourth metacarpal bone in a child: excision and reconstruction with fibular strut graft—a case report and review of literature. European Journal of Orthopaedic Surgery & Traumatology. 2011;21:51–54. doi: 10.1007/s00590-010-0661-1. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.