Abstract
BACKGROUND
The prognostic value of coronary collateral circulation (CC) in patients undergoing chronic total occlusion (CTO) percutaneous coronary intervention (PCI) is underdetermined. The purpose of the study was to assess the prognostic value of current two CC grading systems and their association with long-term outcomes in patients with CTO underwent PCI.
METHODS
We consecutively enrolled patients with single-vessel CTO underwent PCI between January 2010 and December 2013. All patients were categorized into well-developed or poor-developed collaterals group according to angiographic Werner’s CC (grade 2 vs. grade 0–1) or Rentrop (grade 3 vs. grade 0–2) grading system. The primary endpoint was 5-year cardiac death.
RESULTS
Of 2452 enrolled patients, the overall technical success rate was 74.1%. Well-developed collaterals were present in 686 patients (28.0%) defined by Werner’s CC grade 2, and in 1145 patients (46.7%) by Rentrop grade 3. According to Werner’s CC grading system, patients with well-developed collaterals had a lower rate of 5-year cardiac death compared with those with poor-developed collaterals (1.6% vs. 3.3%, P = 0.02), those with suboptimal recanalization was associated with higher rate of 5-year cardiac death compared with optimal recanalization (4.7% vs. 0.8%, P = 0.01) and failure patients (4.7% vs. 1.6%, P = 0.12). However, the similar effect was not shown in Rentrop grading system.
CONCLUSIONS
In patients with the single-vessel CTO underwent PCI, well-developed collaterals by Werner’s CC definition were associated with lower rate of 5-year cardiac death. Werner’s CC grading system had a greater prognostic value than Rentrop grading system in patients with CTO underwent PCI.
Coronary chronic total occlusions (CTOs) are presented in 20%–30% of patients with coronary artery disease, which defined as lesions with thrombolysis in myocardial infarction (TIMI) grade 0 flow for more than three months.[1] The rate of success percutaneous coronary intervention (PCI) for CTOs has improved in recent years, but it remains one of the most challenging procedures for interventional cardiologists.
Majority of CTO patients develop coronary collateral circulation (CC) to supply the downstream post-obstruction arterial segment.[2] Well-developed CCs provide invaluable perfusion to the region of myocardium distal to the occlusion. The collateral arteries connected with the receiving vessel could also be used as a possible route to access CTOs in some complex cases.[3]
There are 2 predominantly employed grading methods to assess the extent of CC, Rentrop grading system[4] and Werner’s CC grading system.[5] The Rentrop grading is based on the level of CC in filling the occluded arterial segment,[4] while the Werner’s CC system primarily depends on the size of collateral arteries.[5] Previous studies on the association between CC and the prognosis of CTO were mostly based on Rentrop grading system. A study in acute myocardial infarction patients with a CTO concluded that the presence of well-developed collaterals to the CTO is associated with improved survival.[6] However, whether the degree of collaterals affects prognosis in CTO patients is uncertain. A systematic review and meta-analysis[7] showed that the presence of robust collaterals based on Rentrop grading system is not associated with lower rates of acute myocardial infarction or mortality in patients with a CTO. However, there is lack of study to assess the association between the extent of CC and prognosis of CTO based on Werner’s CC grading system. The aim of the current study was to assess the prognostic value of current two CC grading systems and their association with long-term outcomes in patients with CTO underwent PCI in a large cohort of consecutive patients.
METHODS
Study Population
Between January 2010 and December 2013 in Fuwai Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China, we enrolled patients with single-vessel CTO who had undergone the PCI consecutively. A CTO was defined as 100% occlusion of a native coronary artery with TIMI grade 0 flow for at least three months. Lesions with bridging collaterals but unknown occlusion duration were also regarded as CTO lesions. The inclusion criteria of this study were as follows: (1) single-vessel CTO detected on diagnostic coronary angiography; and (2) the lesions were suitable for elective PCI. The exclusion criteria included: (1) target CTO lesions ≥ 2; and (2) acute myocardial infarction. The study was approved by the Institutional Review Board of Fuwai Hospital (No.2020-1256), Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China. All eligible patients gave electronic consent through either a telephone interview or a clinical visit during follow-up.
Intervention and Medication
Standard strategy and techniques were employed to carry out PCI through femoral or radial artery access. Antegrade wiring was commonly used in the present cohort, while retrograde approach and antegrade dissection reentry technique were still during an early stage of learning at that time and mainly performed by certified specialists. The devices as guide catheter, stent type and intravascular imaging utilization were selected by the operators. All patients were prescribed aspirin (100 mg daily) and clopidogrel (75 mg daily) for at least six days prior to the procedure, or a loading dose of aspirin (300 mg) or clopidogrel (600 mg) before the procedure. The patients were treated with medical therapy before PCI and after discharge, including beta-blocker, nitrate, and statins at the discretion of treating physicians. Most patients on antiplatelet therapies were typically given aspirin (100 mg once daily) for an indefinite period, and clopidogrel (75 mg once daily) for at least one year.
Angiographic Imaging Analysis
An independent imaging core laboratory (Interventional Cardiovascular Imaging Core Laboratory, National Center for Cardiovascular Disease, Beijing, China) retrospectively evaluated angiographic and procedural characteristics. The angiographic intricacy of coronary disease was gauged by the SYNTAX (Synergy between Percutaneous Coronary Intervention with Taxus and Cardiac Surgery) score.[8] The complexity of CTO lesions was assessed by J-CTO (Multicenter CTO Registry in Japan) score[9] and PROGRESS (Prospective Global Registry for the Study of Chronic Total Occlusion Intervention) score.[10]
Procedural acute results were defined as three levels: optimal recanalization was defined as reperfusion of occluded vessel and its side branch (if any) with TIMI grade 3 flow recovery. Suboptimal recanalization was defined as reperfusion of occluded main vessel, and any of the following: (1) the existence of significant side branch occlusion; (2) final TIMI grade 1 or 2 flow; or (3) residual percentage diameter stenosis more than 30%. A significant side branch occlusion was defined as final TIMI grade 0 or 1 flow in branches ≥ 1.5 mm in diameter. Procedural failure was defined as failure to cross a lesion with a balloon catheter.
Collateral Circulation Assessment
The extent of coronary CC supplying the vascular territory of the CTO was assessed and graded according to the Rentrop grading system and the Werner’s CC grading system. Rentrop grading was scored as: grade 0 (no contrast filling of any collateral channel); grade 1 (filling of collaterals without epicardial filling of the CTO artery); grade 2 (partial filling of the epicardial vessel of the CTO artery); and grade 3 (complete epicardial filling of the CTO artery).[4] Werner’s CC grading was scored as: grade 0 (no visible connection between donor and recipient artery); grade 1 (thread-like connection); and grade 2 (continued side branch-like connection).[5] The representative imaging of collaterals defined by Werner’s CC and Rentrop grading system presented in Figure 1. All included patients were categorized into well-developed collateral group (Rentrop grade 3 or Werner’s CC grade 2) and poor-developed collateral group (Rentrop grade < 0–2 or Werner’s CC grade < 0–1).
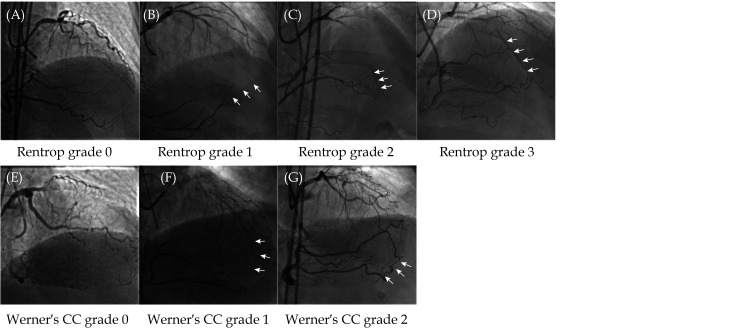
Figure 1.
Representative imaging of collaterals defined by Werner’s CC grading system and Rentrop grading system.
(A): Rentrop grade 0: no contrast filling of any collateral channel; (B): Rentrop grade 1: filling of collaterals without epicardial filling of the CTO artery (arrow); (C): Rentrop grade 2: partial filling of the epicardial vessel of the CTO artery (arrows); (D): Rentrop grade 3: complete epicardial filling of the CTO artery (arrows); (E): Werner’s CC grade 0: no visible connection between donor and recipient artery; (F): Werner’s CC grade 1: thread-like connection (arrow); and (G): Werner’s CC grade 2: continued side branch-like connection (arrows). CC: collateral circulation; CTO: chronic total occlusion.
Endpoints and Follow-up
The primary endpoint was cardiac death at five years. Secondary endpoints included 5-year spontaneous myocardial infarction (MI), all-cause death, ischemia-driven (ID) target vessel revascularization (TVR), and rehospitalization for heart failure. ID was defined as restenosis lesions with angiographic diameter ≥ 50% with ischemic evidence or ≥ 70% irrespective of the presence of ischemic evidence. TVR was defined as any repeat interventional or surgical revascularization of the treated CTO vessel. All adverse events were assessed by an independent clinical events committee.
A dedicated database was utilized to prospectively collect and record all baseline patient demographics, comorbidities, laboratory examinations, and procedural data. An independent office at Fuwai Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China conducted routinely clinical follow-ups at one month, six months, one year, and annually up to five years by outpatient visits or telephone contact.
Statistical Analysis
Counts (percentages) of categorical variables were evaluated by the Pearson’s chi-squared test or Fisher’s exact probability test, while mean ± SD of continuous data were compared with a two-sample Student’s t-test. Statistical significance was set at P-value < 0.05. Logistic regression was used to obtain odds ratio for possible correlative of well-developed CC defined by Werner’s CC grading system. Variables with P-value < 0.1 on the univariable analysis were included in the multivariate analysis. Cox proportional regression with hazard ratios (HR) and 95% CI was used to compare clinical outcomes between groups. From the date of revascularization, the follow-up times were calculated, with all patients censored at their last observed follow-up. Kaplan-Meier estimates and a Cox regression model were used to construct five-year survival curves, and the log-rank test was then employed to contrast the distributions of the time to the initial event during follow-up. Statistical analyses were performed using SPSS 26.0 (SPSS Inc., IBM, Chicago, IL, USA).
RESULTS
Baseline Characteristics
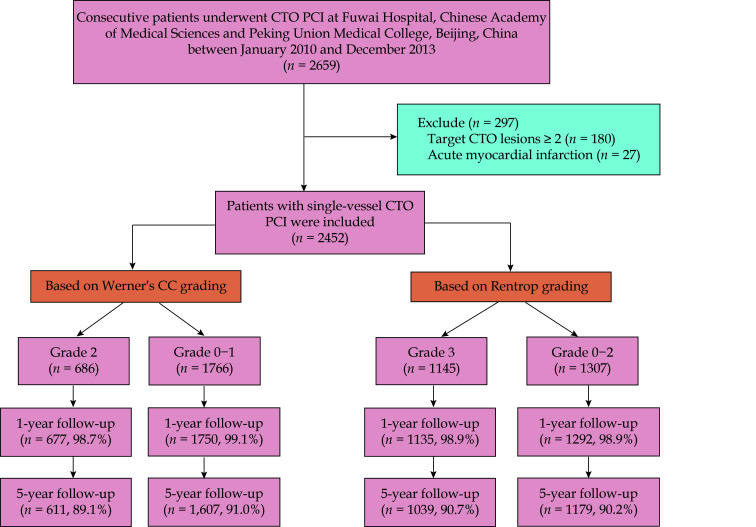
A total of 2452 patients with 2452 CTO lesions were finally enrolled (Figure 2), of whom 83.1% of patients were male and 31.7% of patients with diabetes mellitus. Mean age was 57.3 ± 10.4 years, overall technical success rate was 74.1%, including 59.6% of optimal recanalization and 14.4% of suboptimal recanalization. Well-developed collaterals were present in 686 patients (28.0%) defined by Werner’s CC grading, and in 1145 patients (46.7%) defined by Rentrop grading (Figure 3). Patients with well-developed collaterals were less prior MI (34.7% vs. 42.8%, P < 0.001, by Werner’s CC grade; 33.6% vs. 46.4%, P < 0.001, by Rentrop grade), with a higher left ventricular ejection fraction (61.5% ± 7.5% vs. 60.2% ± 8.1%, P < 0.001, by Werner’s CC grade; 61.5% ± 7.4% vs. 59.7% ± 8.3%, P < 0.001, by Rentrop grade) compared with patients with poor-developed collaterals (Table 1).
Figure 2.
Flow chart.
CC: collateral circulation; CTO: chronic total occlusion; PCI: percutaneous coronary intervention.
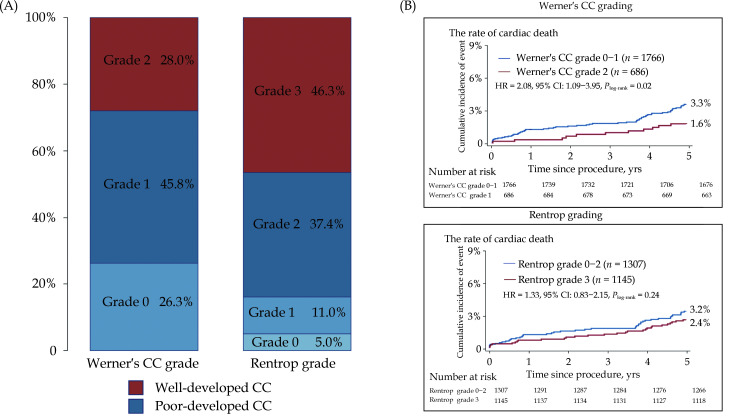
Figure 3.
Distribution of CC development (A) and Kaplan-Meier curves (B) for 5-year cardia death.
CC: collateral circulation.
Table 1. Patient characteristics among different collateral grading.
| Werner’s CC grading | Rentrop grading | ||||||
| Grade 2 (n = 686) |
Grade 0–1 (n = 1766) |
P-value | Grade 3 (n = 1145) |
Grade 0–2 (n = 1307) |
P-value | ||
| Data are presented as means ± SD or n (%). CC: collateral circulation. | |||||||
| Age, yrs | 56.9 ± 10.4 | 57.5 ± 10.4 | 0.21 | 57.3 ± 10.3 | 57.3 ± 10.5 | 0.87 | |
| Male | 573 (83.5%) | 1464 (82.9%) | 0.60 | 959 (83.8%) | 1078 (82.5%) | 0.42 | |
| Body mass index, kg/m2 | 26.6 ± 3.3 | 26.4 ± 3.3 | 0.44 | 26.4 ± 3.1 | 26.5 ± 3.4 | 0.71 | |
| Hypertension | 440 (64.1%) | 1160 (65.7%) | 0.48 | 744 (65.0%) | 856 (65.5%) | 0.80 | |
| Diabetes mellitus | 199 (29.0%) | 579 (32.8%) | 0.07 | 355 (31.0%) | 423 (32.4%) | 0.49 | |
| Hypercholesterolemia | 586 (85.4%) | 1485 (84.1%) | 0.46 | 954 (83.3%) | 1117 (85.5%) | 0.15 | |
| Prior myocardial infarction | 238 (34.7%) | 755 (42.8%) | < 0.001 | 385 (33.6%) | 608 (46.4%) | < 0.001 | |
| Prior percutaneous coronary intervention | 56 (8.2%) | 178 (10.1%) | 0.17 | 82 (7.2%) | 152 (11.6%) | < 0.001 | |
| Prior coronary artery bypass grafting | 17 (2.5%) | 58 (3.3%) | 0.36 | 19 (1.7%) | 56 (4.3%) | < 0.001 | |
| Current smoker | 308 (44.9%) | 689 (39.0%) | 0.008 | 459 (40.1%) | 538 (41.2%) | 0.59 | |
| Family history of coronary artery disease | 93 (13.6%) | 200 (11.3%) | 0.13 | 126 (11.0%) | 167 (12.8%) | 0.19 | |
| History of stoke | 48 (7.0%) | 154 (8.7%) | 0.19 | 94 (8.2%) | 108 (8.3%) | 1.00 | |
| Creatinine clearance < 60 mL/min | 53 (8.0%) | 164 (9.6%) | 0.24 | 100 (9.0%) | 117 (9.3%) | 0.78 | |
| Left ventricular ejection fraction, % | 61.5 ± 7.5 | 60.2 ± 8.1 | < 0.001 | 61.5 ± 7.4 | 59.7 ± 8.3 | < 0.001 | |
| ≤ 40% | 21 (3.1%) | 62 (3.5%) | 0.62 | 30 (2.6%) | 53 (4.1%) | 0.06 | |
Angiographic and Procedural Characteristics
For both two grading methods, patients with well-developed collaterals had larger reference vessel diameter (3.1 ± 0.4 mm vs. 2.9 ± 0.4 mm, P < 0.001, by Werner’s CC grade; 3.0 ± 0.4 mm vs. 2.9 ± 0.4 mm, P < 0.001, by Rentrop grade) and lower PROGRESS score (0.6 ± 0.6 vs. 1.2 ± 0.9, P < 0.001, by Werner’s CC grade; 0.8 ± 0.8 vs. 1.2 ± 0.9, P < 0.001, by Rentrop grade). For the Werner’s CC grading, patients with well-developed collaterals had longer CTO length (18.4 ± 11.4 mm vs. 17.3 ± 12.6 mm, P = 0.03) and lower SYNTAX score (18.0 ± 7.8 vs. 19.4 ± 8.4, P < 0.001), whereas for the Rentrop grading, patients with well-developed collaterals had shorter occluded length (16.5 ± 11.0 mm vs. 18.5 ± 13.2 mm, P < 0.001) and higher SYNTAX score (19.8 ± 8.1 vs. 18.3 ± 8.3, P < 0.001), compared with poor-developed collaterals. PCI acute procedural results were not associated with collateral level regardless of grading methods (Table 2). A multivariable analysis showed that the absence of prior history of MI, current smoker and larger reference vessel diameter were independently associated with well-developed CC defined by Werner’s CC grading (Table 3).
Table 2. Lesion characteristic among different collateral grading.
| Werner’s CC grading | Rentrop grading | ||||||
| Grade 2 (n = 686) |
Grade 0–1 (n = 1766) |
P-value | Grade 3 (n = 1145) |
Grade 0–2 (n = 1307) |
P-value | ||
| Data are presented as means ± SD or n (%). CC: collateral circulation; CTO: chronic total occlusion; PCI: percutaneous coronary intervention. | |||||||
| Target vessel | < 0.001 | 0.023 | |||||
| Left main artery | 1 (0.1%) | 3 (0.2%) | 3 (0.3%) | 1 (0.1%) | |||
| Left anterior descending | 249 (36.1%) | 697 (38.9%) | 448 (39.1%) | 483 (37.0%) | |||
| Left circumflex artery | 55 (8.0%) | 308 (17.2%) | 143 (12.5%) | 217 (16.6%) | |||
| Right coronary artery | 384 (55.7%) | 773 (43.8%) | 551 (48.1%) | 606 (46.4%) | |||
| Reference vessel diameter, mm | 3.1 ± 0.4 | 2.9 ± 0.4 | < 0.001 | 3.0 ± 0.4 | 2.9 ± 0.4 | < 0.001 | |
| CTO length, mm | 18.4 ± 11.4 | 17.3 ± 12.6 | 0.029 | 16.5 ± 11.0 | 18.5 ± 13.2 | < 0.001 | |
| Blunt stump | 292 (42.6%) | 722 (40.9%) | 0.47 | 451 (39.4%) | 563 (43.1%) | 0.07 | |
| Moderate or severe calcification | 98 (14.3%) | 224 (14.7%) | 0.29 | 140 (12.2%) | 182 (13.9%) | 0.23 | |
| Moderate or severe tortuosity | 336 (49.0%) | 737 (41.7%) | 0.001 | 507 (44.3%) | 566 (43.3%) | 0.65 | |
| In-stent | 54 (7.9%) | 148 (8.4%) | 0.74 | 68 (5.9%) | 134 (10.3%) | < 0.001 | |
| Retry PCI | 21 (3.1%) | 59 (3.3%) | 0.80 | 40 (3.5%) | 40 (3.1%) | 0.57 | |
| J-CTO score | 1.5 ± 1.0 | 1.4 ± 1.0 | < 0.001 | 1.4 ± 1.0 | 1.4 ± 1.0 | 0.10 | |
| PROGRESS score | 0.6 ± 0.6 | 1.2 ± 0.9 | < 0.001 | 0.8 ± 0.8 | 1.2 ± 0.9 | < 0.001 | |
| SYNTAX score | 18.0 ± 7.8 | 19.4 ± 8.4 | < 0.001 | 19.8 ± 8.1 | 18.3 ± 8.3 | < 0.001 | |
| PCI acute result | 0.18 | 0.25 | |||||
| Optimal success | 389 (56.7%) | 1073 (60.8%) | 699 (61.0%) | 763 (58.4%) | |||
| Sub-optimal success | 107 (15.6%) | 247 (14.0%) | 152 (13.3%) | 202 (15.5%) | |||
| Failure | 190 (27.7%) | 446 (25.3%) | 294 (25.7%) | 342 (26.2%) | |||
Table 3. Correlative factors of well-developed collaterals defined by Werner’s CC grading.
| Variables | Odds ratio (95% CI) | P-value |
| CC: collateral circulation. | ||
| Diabetes mellitus | 1.159 (0.950–1.414) | 0.15 |
| Occlusion myocardial infarction | 1.408 (1.140–1.739) | 0.002 |
| Current smoker | 0.803 (0.668–0.996) | 0.02 |
| Left ventricular ejection fraction | 1.012 (0.998–1.025) | 0.09 |
| Reference vessel diameter | 2.139 (1.728–2.647) | < 0.001 |
| Chronic total occlusion length | 1.001 (0.993–1.008) | 0.85 |
| Moderate or severe tortuosity | 0.932 (0.760–1.142) | 0.50 |
| Target vessel | ||
| Left anterior descending | 0.577 (0.058–5.759) | 0.64 |
| Left circumflex artery | 0.935 (0.092–9.509) | 0.94 |
| Right coronary artery | 0.414 (0.041–4.144) | 0.41 |
Outcomes
According to Werner’s CC definition, patients with well-developed collaterals had a lower rate of 5-year cardiac death compared with those with poor-developed collaterals (1.6% vs. 3.3%, HR = 2.08, 95% CI: 1.09–3.95, P = 0.02); but the difference was not significant by Rentrop grading (2.4% vs. 3.2%, HR = 1.33, 95% CI: 0.83–2.15, P = 0.24) (Table 4). Time-to-event curves also showed persist significant lower incidence of cardiac death (log-rank P = 0.02) in well-developed collaterals by Werner’s CC grading, but not significant (log-rank P = 0.24) by Rentrop grading (Figure 3). There was no statistical difference between well-developed CC and poor-developed CC for secondary endpoints as all-cause death, MI, ID-TVR and rehospitalization for heart failure at 5-year cardiac death, regardless of collateral grading system (Table 4).
Table 4. Long-term outcomes among different collateral grading.
| Werner’s CC grading | Rentrop grading | ||||||||
| Grade 2 (n = 686) |
Grade 0–1 (n = 1766) |
HR (95% CI) | P-value | Grade 3 (n = 1145) |
Grade 0–2 (n = 1307) |
HR (95% CI) | P-value | ||
| CC: collateral circulation. | |||||||||
| Primary endpoint | |||||||||
| Cardiac death | 11 (1.6%) | 59 (3.3%) | 2.08 (1.09–3.95) | 0.03 | 28 (2.4%) | 42 (3.2%) | 1.33 (0.825–2.146) | 0.24 | |
| Secondary endpoints | |||||||||
| All-cause death | 23 (3.4%) | 93 (5.3%) | 1.56 (0.99–2.47) | 0.05 | 49 (4.3%) | 67 (5.1%) | 1.21 (0.84–1.75) | 0.30 | |
| Spontaneous myocardial infarction | 30 (4.4%) | 106 (6.0%) | 1.36 (0.91–2.05) | 0.12 | 61 (5.3%) | 75 (5.7%) | 1.09 (0.78–1.53) | 0.62 | |
| Rehospitalization for heart failure | 20 (2.8%) | 62 (3.4%) | 1.08 (0.63–1.85) | 0.77 | 32 (2.7%) | 50 (3.6%) | 1.38 (0.85–2.24) | 0.19 | |
| Ischemia-driven target vessel re- vascularization |
85 (12.4%) | 190 (10.8%) | 0.85 (0.66–1.09) | 0.20 | 142 (12.4%) | 133 (10.2%) | 0.81 (0.64–1.03) | 0.09 | |
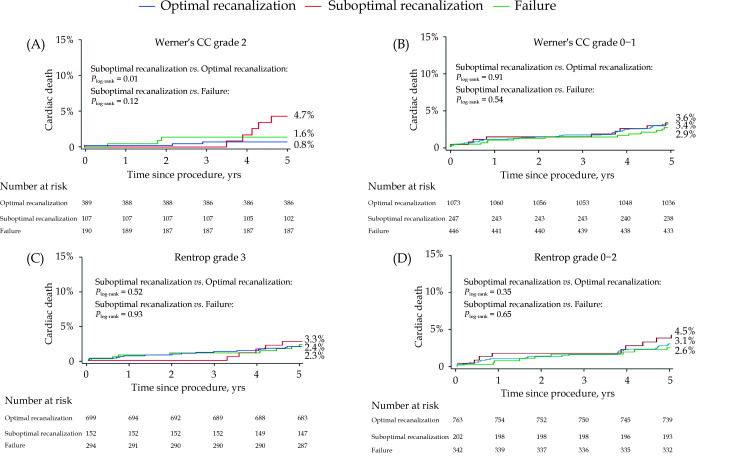
In patients with well-developed collateral arteries by Werner’s CC grading, 5-year cardiac death in suboptimal recanalization was significantly higher than in the optimal recanalization group (4.7% vs. 0.8%, log-rank P = 0.01), numerically higher than that in failure group without statistical significance (4.7% vs. 1.6%, log-rank P = 0.12). However, there was no significant association between 5-year cardiac death and acute procedural results in well-developed CC by Rentrop grading system and poor-developed collaterals regardless of collateral grading methods (Figure 4).
Figure 4.
Kaplan–Meier curves for 5-year cardiac death according to acute procedural results by Werner’s CC grading (A & B) and Rentrop grading (C & D).
CC: collateral circulation.
DISCUSSION
In this large-scale CTO-PCI cohort with prolonged follow-up duration, the main findings were: (1) well-developed collaterals were present in the 686 patients (28.0%) defined by Werner’s CC grading, while in 1145 patients (46.7%) defined by Rentrop grading; (2) absence of prior history of MI, current smoker and larger reference vessel diameter were independently associated with well-developed CC defined by Werner’s CC grading; (3) well-developed collaterals by Werner’s CC definition were associated with superior long-term outcomes, and suboptimal recanalization was associated with higher rate of 5-year cardiac death in these patients; and (4) there was no association between Rentrop grading system and the prognostic of CTO underwent PCI.
In previous reported post-hoc studies, the prevalence of CC was observed in 58% of recent occlusions, and up to 96% when CTOs were present.[2] In a study of Werner, et al.[5] collateral connection grade CC2 was observed in 35% of patients with CTO, while Rentrop grade 3 in 78% of patients with CTO. In the present study, CCs were present in 95% of patients with CTO defined by Rentrop grading and 73.7% of patients with CTO defined by Werner’s CC grading. Well-developed CCs were present in 46.7% of patients defined by Rentrop grading, however in those patients, only 48.1% of patients was concordant with Werner’s CC defined well-developed collaterals. It suggested that Werner’s CC grading system might provide a better discrimination for the formation of collateral vessels in CTOs.
Our study showed that absence of prior history of MI, current smoker and larger reference vessel diameter were independently associated with well-developed CC defined by Werner’s CC grading. CTOs without prior MI usually detected long after vessel occlusion, and always based on severer coronary stenosis. Previous study has found that patients with robust CC were associated with a greater degree of luminal stenosis and a longer ischemia time.[11] Therefore, CTOs without previous MI were associated with robust CC, because of the prolonged ischemia time and more critical stenosis. Arteriogenesis is a form of CCs growth, which is related to increased shear forces.[12] And the arterial diameter is shown to increase in response to an increase in wall shear stress,[13] so larger reference vessel diameter was associated with well-developed CC might related the increased shear forces. Interestingly, current smoker was found to be a factor with well-developed CC in our study, which consistent with results of the SMART study.[14] The possible explanation is that nicotine was identified as a potent angiogenic agent and may also promote arteriogenesis by activation of endothelial-monocyte interactions.[15]
We found that well-developed collaterals by Werner’s CC definition were associated with superior long-term outcomes, but the similar effect was not shown in Rentrop grading system. Possible explanation was the well-developed collaterals defined by CC grading as continued side “branch-like connection” is more sharply defined and might provide more sufficient perfusion to donor vessels, compared with Rentrop grading as “complete” epicardial filling. Werner’s CC grade was reported be associated with invasive parameters of collateral function, such as collateral resistance index independently.[5] Werner’s CC2 collaterals preserved regional left ventricular function better than did CC1 collaterals. In contrast, the Rentrop grading shows only a weak correlation with invasive parameters of collateral function, which could explain the results of present study and previous meta-analysis that the presence of well-developed collaterals defined by Rentrop classification was not associated with lower rates of MI or mortality.[7]
Collateral vessels can be classified broadly into two groups: one is “capillary-sized” collaterals lacking vascular smooth muscle, the other is much larger “side branch size” collaterals with a muscular vessel wall.[16] Based on the definition, Werner’s CC grade 2 were angiographically visible collaterals with continued side branch-like connections which always above 0.4 mm and have well-developed structure of vessel wall,[12] whereas Rentrop grade 3 might include both “capillary-sized” and “side branch size” collaterals. An analysis by Rockstroh, et al.[17] indicated that the flow of collaterals was largely related to vessel diameter, and 2 or 3 largest connections in the angiographically visible collateral spectrum carried majority of flow. We therefore speculated that a well-developed CC with “side branch size” might be the critical factor for the favorable prognosis.
Based on an analysis from the same cohort, Guan, et al.[18] demonstrated that suboptimal procedural results were associated with significantly higher long-term incidence of cardiac death and MI, compared with both optimal recanalization and procedural failure. In the current study, we verified the conclusion in patients with full-developed collaterals (Werner’s CC grade 2), but not poor-developed collaterals. In those suboptimal recanalizations with side branch occlusion, final TIMI flow grade 1 or 2, or residual stenosis > 30%, patients tend to have worse runoff after stent implantation, this effect is usually greater when originally well-developed collaterals were injured. The poor runoff was associated with restenosis and re-occlusion of the recanalized vessel.[19] It is widely recognized that collateral flow in CTOs were significantly decreased immediately after recanalization and would regress further in the next 3–5 months.[20,21] These collaterals remain recruitable when re-occlusion occurs,[22] but in case of collaterals being injured, the effect may be not enough.[23]
LIMITATIONS
There are several limitations must be noted. Firstly, this was a retrospective single-center study with potential selection bias. Secondly, the CTO PCI were performed six to nine years ago, contemporary devices and techniques such as retrograde or antegrade dissection re-entry were used in a small proportion of patients, the relatively lower success rate may influence the results. Thirdly, the lack of intravascular imaging and physiological assessment in the current study meant we could not provide detailed measurements of CTO lesions and functional status of both donor and acceptor vessels. Fourthly, there is a lack of imaging follow-up to evaluate the dynamic changes of collateral arteries. Last but not least, the viable myocardial viability was not fully evaluated before PCI. Future prospective studies using advanced techniques and devices with higher enough success rate are warranted to further clarify the association between CC and long-term outcomes after CTO recanalization.
CONCLUSIONS
In conclusions, in patients with single-vessel CTO underwent interventional recanalization, well-developed collaterals by Werner’s CC definition were associated with superior long-term outcomes, and suboptimal recanalization was associated with higher rate of 5-year cardiac death in these patients. Werner’s CC grading system had a greater prognostic value than Rentrop grading system in patients with CTO underwent PCI.
ACKNOWLEDGMENTS
All authors had no conflicts of interest to disclose. The authors thank all the nonauthor CTO-PCI operators of Department of Cardiology (Ji-Lin CHEN, Jun DAI, Zhan GAO, Feng-Huan HU, Chong-Jian LI, Jian-Jun LI, Hai-Bo LIU, Yi MAO, Chao-Wei MU, Hong QIU, Hong-Bing YAN, Min YAO, Meng-Yue YU, Hai-Tao ZHANG, Pei ZHANG, and Jing-Lin ZHAO), Fuwai Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China and other research personnel for their contributions to the study.
References
- 1.Werner GS The role of coronary collaterals in chronic total occlusions. Curr Cardiol Rev. 2014;10:57–64. doi: 10.2174/1573403X10666140311123814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zoll PM, Wessler S, Schlesinger MJ Interarterial coronary anastomoses in the human heart, with particular reference to anemia and relative cardiac anoxia. Circulation. 1951;4:797–815. doi: 10.1161/01.CIR.4.6.797. [DOI] [PubMed] [Google Scholar]
- 3.Rathore S, Katoh O, Matsuo H, et al Retrograde percutaneous recanalization of chronic total occlusion of the coronary arteries: procedural outcomes and predictors of success in contemporary practice. Circ Cardiovasc Interv. 2009;2:124–132. doi: 10.1161/CIRCINTERVENTIONS.108.838862. [DOI] [PubMed] [Google Scholar]
- 4.Rentrop KP, Cohen M, Blanke H, et al Changes in collateral channel filling immediately after controlled coronary artery occlusion by an angioplasty balloon in human subjects. J Am Coll Cardiol. 1985;5:587–592. doi: 10.1016/S0735-1097(85)80380-6. [DOI] [PubMed] [Google Scholar]
- 5.Werner GS, Ferrari M, Heinke S, et al Angiographic assessment of collateral connections in comparison with invasively determined collateral function in chronic coronary occlusions. Circulation. 2003;107:1972–1977. doi: 10.1161/01.CIR.0000061953.72662.3A. [DOI] [PubMed] [Google Scholar]
- 6.Elias J, Hoebers LPC, van Dongen IM, et al Impact of collateral circulation on survival in ST-segment elevation myocardial infarction patients undergoing primary percutaneous coronary intervention with a concomitant chronic total occlusion. JACC Cardiovasc Interv. 2017;10:906–914. doi: 10.1016/j.jcin.2017.01.026. [DOI] [PubMed] [Google Scholar]
- 7.Allahwala UK, Nour D, Bhatia K, et al Prognostic impact of collaterals in patients with a coronary chronic total occlusion: a meta-analysis of over 3000 patients. Catheter Cardiovasc Interv. 2021;97:E771–E777. doi: 10.1002/ccd.29348. [DOI] [PubMed] [Google Scholar]
- 8.Sianos G, Morel MA, Kappetein AP, et al The SYNTAX score: an angiographic tool grading the complexity of coronary artery disease. EuroIntervention. 2005;1:219–227. doi: 10.1182/blood-2006-09-048868. [DOI] [PubMed] [Google Scholar]
- 9.Morino Y, Abe M, Morimoto T, et al Predicting successful guidewire crossing through chronic total occlusion of native coronary lesions within 30 minutes: the J-CTO (Multicenter CTO Registry in Japan) score as a difficulty grading and time assessment tool. JACC Cardiovasc Interv. 2011;4:213–221. doi: 10.1016/j.jcin.2010.09.024. [DOI] [PubMed] [Google Scholar]
- 10.Christopoulos G, Kandzari DE, Yeh RW, et al Development and validation of a novel scoring system for predicting technical success of chronic total occlusion percutaneous coronary interventions: the PROGRESS CTO (Prospective Global Registry for the Study of Chronic Total Occlusion Intervention) score. JACC Cardiovasc Interv. 2016;9:1–9. doi: 10.1016/j.jcin.2015.09.022. [DOI] [PubMed] [Google Scholar]
- 11.Allahwala UK, Weaver JC, Nelson GI, et al Effect of recruitment of acute coronary collaterals on in-hospital mortality and on left ventricular function in patients presenting with ST-elevation myocardial infarction. Am J Cardiol. 2020;125:1455–1460. doi: 10.1016/j.amjcard.2020.02.023. [DOI] [PubMed] [Google Scholar]
- 12.Van Royen N, Piek JJ, Schaper W, et al Arteriogenesis: mechanisms and modulation of collateral artery development. J Nucl Cardiol. 2001;8:687–693. doi: 10.1067/mnc.2001.118924. [DOI] [PubMed] [Google Scholar]
- 13.Kamiya A, Togawa T Adaptive regulation of wall shear stress to flow change in the canine carotid artery. Am J Physiol. 1980;239:H14–H21. doi: 10.1152/ajpheart.1980.239.1.H14. [DOI] [PubMed] [Google Scholar]
- 14.Koerselman J, de Jaegere PP, Verhaar MC, et al Coronary collateral circulation: the effects of smoking and alcohol. Atherosclerosis. 2007;191:191–198. doi: 10.1016/j.atherosclerosis.2006.03.021. [DOI] [PubMed] [Google Scholar]
- 15.Heeschen C, Weis M, Cooke JP Nicotine promotes arteriogenesis. J Am Coll Cardiol. 2003;41:489–496. doi: 10.1016/s0735-1097(02)02818-8. [DOI] [PubMed] [Google Scholar]
- 16.Schaper W Collateral vessel growth in the human heart. Role of fibroblast growth factor-2. Circulation. 1996;94:600–601. doi: 10.1161/01.cir.94.4.600. [DOI] [PubMed] [Google Scholar]
- 17.Rockstroh J, Brown BG Coronary collateral size, flow capacity, and growth: estimates from the angiogram in patients with obstructive coronary disease. Circulation. 2002;105:168–173. doi: 10.1161/hc0202.102120. [DOI] [PubMed] [Google Scholar]
- 18.Guan C, Yang W, Song L, et al Association of acute procedural results with long-term outcomes after CTO PCI. JACC Cardiovasc Interv. 2021;14:278–288. doi: 10.1016/j.jcin.2020.10.003. [DOI] [PubMed] [Google Scholar]
- 19.Schumacher SP, Stuijfzand WJ, Opolski MP, et al Percutaneous coronary intervention of chronic total occlusions: when and how to treat. Cardiovasc Revasc Med. 2019;20:513–522. doi: 10.1016/j.carrev.2018.07.025. [DOI] [PubMed] [Google Scholar]
- 20.Seiler C The human coronary collateral circulation. Heart. 2003;89:1352–1357. doi: 10.1136/heart.89.11.1352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Keulards DCJ, Alsanjari O, Keeble TR, et al Changes in coronary collateral function after successful chronic total occlusion percutaneous coronary intervention. EuroIntervention. 2022;18:e920–e928. doi: 10.4244/EIJ-D-22-00118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Petronio AS, Baglini R, Limbruno U, et al Coronary collateral circulation behaviour and myocardial viability in chronic total occlusion treated with coronary angioplasty. Eur Heart J. 1998;19:1681–1687. doi: 10.1053/euhj.1998.1154. [DOI] [PubMed] [Google Scholar]
- 23.Choo GH Collateral circulation in chronic total occlusions: an interventional perspective. Curr Cardiol Rev. 2015;11:277–284. doi: 10.2174/1573403X11666150909112548. [DOI] [PMC free article] [PubMed] [Google Scholar]