Abstract
BACKGROUND:
In 2009, the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) revised its food packages to align with updated nutrition science. Understanding how these revisions may impact current consumption patterns could be important.
METHODS:
Dietary data from the 2011–2014 NHANES were used to estimate the percentage of children who were aged 12 to 23 months consuming selected food and beverage categories on any given day by age and WIC status (children who were on WIC, those who were eligible for but not receiving WIC benefits, and those who were not eligible for WIC).
RESULTS:
Consumption of food and beverage categories differed by WIC status. On a given day, a lower percentage of children who were eligible for but did not receive WIC benefits consumed vegetables (excluding white potatoes; 42.3%) and grains (76.5%) compared with children who were participating in WIC (vegetables [excluding white potatoes]: 60.4%; grains: 85.5%) and those who were not eligible for WIC benefits (vegetables [excluding white potatoes]: 58.1%; grains: 87.2%; P < .05). A lower percentage of both children who were eligible for but not receiving WIC benefits and those who were participating in WIC consumed fruits (57.6% and 70.6%, respectively) and snacks (45.9% and 48.5%, respectively) than those who were not eligible for WIC (fruits: 86.4%; snacks: 69.1%; P < .05). A lower percentage of children who were receiving WIC consumed dairy than children who were not eligible for WIC (91.7% and 97.2%, respectively; P < .05). A higher percentage of those who were receiving WIC consumed 100% juice (70.6%) than children who were eligible for but not receiving WIC (51.6%) and children who were not eligible for WIC (50.8%; P < .05).
CONCLUSIONS:
Improving early WIC participation and retention could positively impact some diet-related disparities among young children who are eligible for WIC.
The US Department of Agriculture (USDA) Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) provides nutrition education and counseling, nutritious supplemental foods, and referrals to health care and other social services for women who have low income and are pregnant or postpartum, including those who are breastfeeding or nonbreastfeeding and children ≤5 years of age who are at nutritional risk.1 In 2014, approximately one-half of all infants and slightly greater than one-quarter of all 1- to 4-year-olds in the United States participated in WIC.2
As part of the WIC Program, participants receive food benefits at no cost through a WIC food package. Before 2009, authorized food packages had not been comprehensively updated since 1980.3 However, the USDA issued an interim rule in 2007 to change the WIC food packages,4 and WIC state agencies implemented these revised food packages by October 1, 2009. The revised food packages were later codified in a subsequent final rule published on March 4, 2014, and this final rule contained minimal additional changes from the interim rule.3,5 Compared with the pre-2009 food packages, the revised WIC food packages include lower amounts of 100% juice, new cash-value vouchers for purchasing fresh fruits and vegetables, increased amounts of whole grains, and a standard issuance of lower-fat milk to women and children ages ≥24 months.6
Researchers in several studies have assessed the impacts of the WIC food package changes, which includes 1 study among children aged 2 to 4 years that revealed improvements in dietary quality and increased availability of healthy foods and beverages.7 However, to the knowledge of the authors, no published studies have assessed the dietary patterns of children 12 to 23 months of age in WIC after the interim rule by participation in WIC (ie, WIC status), including children who are eligible for WIC but not participating. Therefore, our objective in this study is to describe the consumption of selected food and beverage categories among a nationally representative sample of US toddlers aged 12 to 23 months by WIC status. These data may provide WIC educators with insights into food and beverage category consumption that align with current program aims as well as those categories that may need additional emphasis through nutrition education.
METHODS
The NHANES
The NHANES is an ongoing, nationally representative survey of the noninstitutionalized civilian US population and includes a stratified multistage probability design.8 Information on the study design and methods have been published elsewhere.9,10 The survey includes a household interview and a physical examination that is conducted in a mobile examination center (MEC). All participants provide written informed consent, with parents or guardians providing consent for minors to participate. Data are released in 2-year cycles. This analysis includes data from 2011 to 2012 and 2013 to 2014. NHANES protocol was approved by the National Center for Health Statistics Research Ethics Review Board. Response rates for children who were aged 1 to 5 years and underwent the physical examination were 77.6% in 2011–2012 and 74.6% in 2013–2014.11
Dietary Intake and Food-Group Categorization
The NHANES includes 2 24-hour dietary recalls, with the first recall collected in-person in the MEC and the second via telephone 3 to 10 days later. For this analysis, the first dietary recall was used, representing a given day’s intake for the population. Dietary information was collected in a standardized format by using the USDA Automated Multiple Pass Method,12 which helps ensure that all foods and beverages are reported in a 24-hour period, including breast milk. A proxy (generally a parent) who is most familiar with the child’s intake completes the dietary recall.
Similar to a previous study,13 food groups were identified by using the USDA What We Eat in America (WWEIA) categories14 that describe foods as they are consumed (eg, pizza and sandwiches) rather than individual components of foods. WWEIA categories are composed of mutually exclusive, large food categories that are further divided into smaller subcategories. The WWEIA categories are updated with new food codes for every NHANES dietary data release.15–17 The subcategories and the associated WWEIA food codes were used to develop 18 food and beverage categories for the current study (see Supplemental Table 2). All food and beverage categories that were reported for the current study are mutually exclusive, with the exception of total milk and dairy. Total milk includes 3 smaller subcategories (whole milk, reduced or low- or nonfat milk, and flavored milk or milk substitutes). Dairy includes both total milk and cheese and yogurt.
Analytic Sample
We limited our analyses to children who were 12 to 23 months of age at the time of the physical examination (n = 468). Children were excluded if they did not complete the dietary interview (n = 31), if the dietary intake record was coded as not reliable (n = 12), or if the children were missing information on variables that were required to determine WIC status (n = 7). This left a final sample size of 418 children who were 12 to 23 months of age.
Covariates
The analytic sample is described by WIC status. WIC status was defined as currently receiving WIC benefits. Children who were eligible for but not receiving WIC benefits were defined as children who did not report currently receiving WIC and (1) whose family income/poverty ratio was ≤1.85; (2) who reported receiving Medicaid; or (3) who reported receiving benefits from the Supplemental Nutrition Assistance Program (SNAP), which were previously called food stamps. Children who were not eligible for WIC were defined as those children who did not meet any of the previously described WIC eligibility criteria. Race and Hispanic origin were reported as non-Hispanic white, non-Hispanic African American, or Hispanic. Analyses include children who were identified as being of another race (including multiracial), but they are not shown as a separate group because of small sample sizes.
Statistical Analyses
As was done previously,13 we estimated the percentage of children who reported consuming any amount of a food or beverage in predefined food or beverage categories in the previous 24 hours. Children were classified as having any consumption or no consumption of specific food or beverage categories on a given day; however, the amount consumed was not quantified. Estimates and 95% confidence intervals (CIs) were calculated by using the Wald method for all children by WIC status. We used t tests (a priori pairwise comparisons were done by WIC status) to determine if food consumption frequencies differed by WIC status.
SPSS Complex Samples version 23.0 (IBM SPSS Statistics, IBM Corporation) was used in all analyses to account for the complex survey design. Analyses were weighted by using day-1 dietary weights, which adjust for oversampling, nonresponse, noncoverage, and day of the week.18 All percentages that are presented are weighted.
RESULTS
Among US children aged 12 to 23 months, 38.1% currently receive WIC benefits, 19.6% were eligible for but not receiving WIC benefits, and 42.2% were not eligible. There were no significant differences in WIC status by sex, but there were significant differences by race and Hispanic origin (P < .001). For example, among children who were currently receiving WIC benefits, a higher percentage were Hispanic (49.0%), followed by non-Hispanic white (24.6%) and non-Hispanic African American (16.7%).
In Table 1, the weighted percentage of US children who were 12 to 23 months of age and consumed select beverage categories on any given day by WIC status is presented. There were no statistically significant differences in consumption of whole, reduced-fat, low-fat, nonfat, or total milk or sugar-sweetened beverages on any given day by WIC status. A higher percentage of children who were receiving WIC benefits consumed 100% juice on a given day (70.6%) compared with both children who were eligible for but not receiving WIC benefits (51.6%) and children who were not eligible for WIC benefits (50.8%; P < .01). A lower percentage of children who were eligible for but not receiving WIC benefits consumed water on a given day (67.6%) compared with children who were not eligible for WIC benefits (82.6%; P < .05). Estimates of the percentage of children who were consuming breast milk, formula, or flavored milk or milk substitutes are not presented because of unstable estimates. However, flavored milk or milk substitutes are included as part of the total milk category.
TABLE 1.
Percentage of US Children Who Were 12 to 23 Months of Age and Consuming Any Beverages by WIC Status (NHANES 2011–2014)
| Eligible for but Not Receiving (n = 84), % (95% CI) | WIC (n = 202), % (95% CI) | Not Eligible (n = 132), % (95% CI) | |
|---|---|---|---|
|
| |||
| Milk and milk substitutes | |||
| Whole milk | 63.5 (48.0–76.7) | 65.0 (57.2–72.0) | 66.3 (54.9–76.1) |
| Reduced or low- or nonfat milk | 23.9 (13.9–38.0) | 20.0 (13.6–28.4) | 22.4 (12.9–35.9) |
| Total milk | 91.1 (80.3–96.3) | 85.7 (79.7–90.2) | 87.9 (77.0–94.0) |
| Other beverages | |||
| 100% juice | 51.6 (40.1 –63.0)a | 70.6 (61 2–78.6)b | 50.8 (39.3–62.1) |
| Sugar-sweetened beverages | 26.6 (15.5–41.6) | 31.1 (24.2–39.0) | 24.4 (14.8–37.6) |
| Water | 67.6 (56.1 —77.4)b | 74.8 (65.7–82.2) | 82.6 (71.6–89.9) |
Age is presented in months at the time of examination in a MEC. Beverages contained in the whole milk category include whole milk. Beverages contained in the reduced-fat or low- or nonfat milk category include reduced-fat, low-fat, or nonfat milk. Beverages contained in the total milk category include whole milk, reduced-fat milk, low-fat milk, nonfat milk, flavored milk, and/or milk substitutes (whole-fat flavored milk, reduced-fat flavored milk, low-fat flavored milk, nonfat flavored milk, milkshakes, or other dairy drinks). Beverages contained in the 100% juice category include citrus juice, apple juice, other fruit juice, vegetable juice, and baby juice. Beverages contained in the sugar-sweetened beverages category include soft drinks, fruit drinks, sports and energy drinks, nutritional beverages, smoothies and grain drinks, and flavored or enhanced water. Beverages contained in the water category include tap water, plain water, and baby water. WIC status is defined as children who are currently receiving WIC benefits. Eligible for but not receiving WIC benefits is defined as children who are eligible for WIC benefits on the basis of family income/poverty ratio, receipt of Medicaid, or receipt of SNAP benefits (previously called food stamps). Not eligible is defined as children who do not meet WIC eligibility criteria.
Indicates results that are significantly different from those of WIC participants (t test; P < .05).
Indicates results that are significantly different from those of children who are not eligible (t test; P < .05).
In Fig 1, the weighted percentage of US children who were 12 to 23 months of age and consuming different food categories by WIC status is presented (Supplemental Table 3 displays point estimates and 95% CIs). Significant findings are highlighted. Compared with children who were receiving WIC benefits, a lower percentage of children who were eligible for but not receiving WIC benefits consumed vegetables (excluding white potatoes; 60.4% and 42.3%, respectively) and grains (85.5% and 76.5%, respectively; P < .05; Fig 1). Compared with children who were receiving WIC benefits, a higher percentage of children who were not eligible for WIC benefits consumed fruit (70.6% and 86.4%, respectively), protein foods (80.5% and 90.0%, respectively), dairy (91.7% and 97.2%, respectively), and snacks (48.5% and 69.1%, respectively; P < .05). Compared with children who were eligible for but not receiving WIC benefits, a higher percentage of children who were not eligible for WIC benefits consumed fruit (57.6% and 86.4%, respectively), vegetables (excluding white potatoes; 42.3% and 58.1%, respectively), grains (76.5% and 87.2%, respectively), and snacks (45.9% and 69.1%, respectively; P < .05).
FIGURE 1.
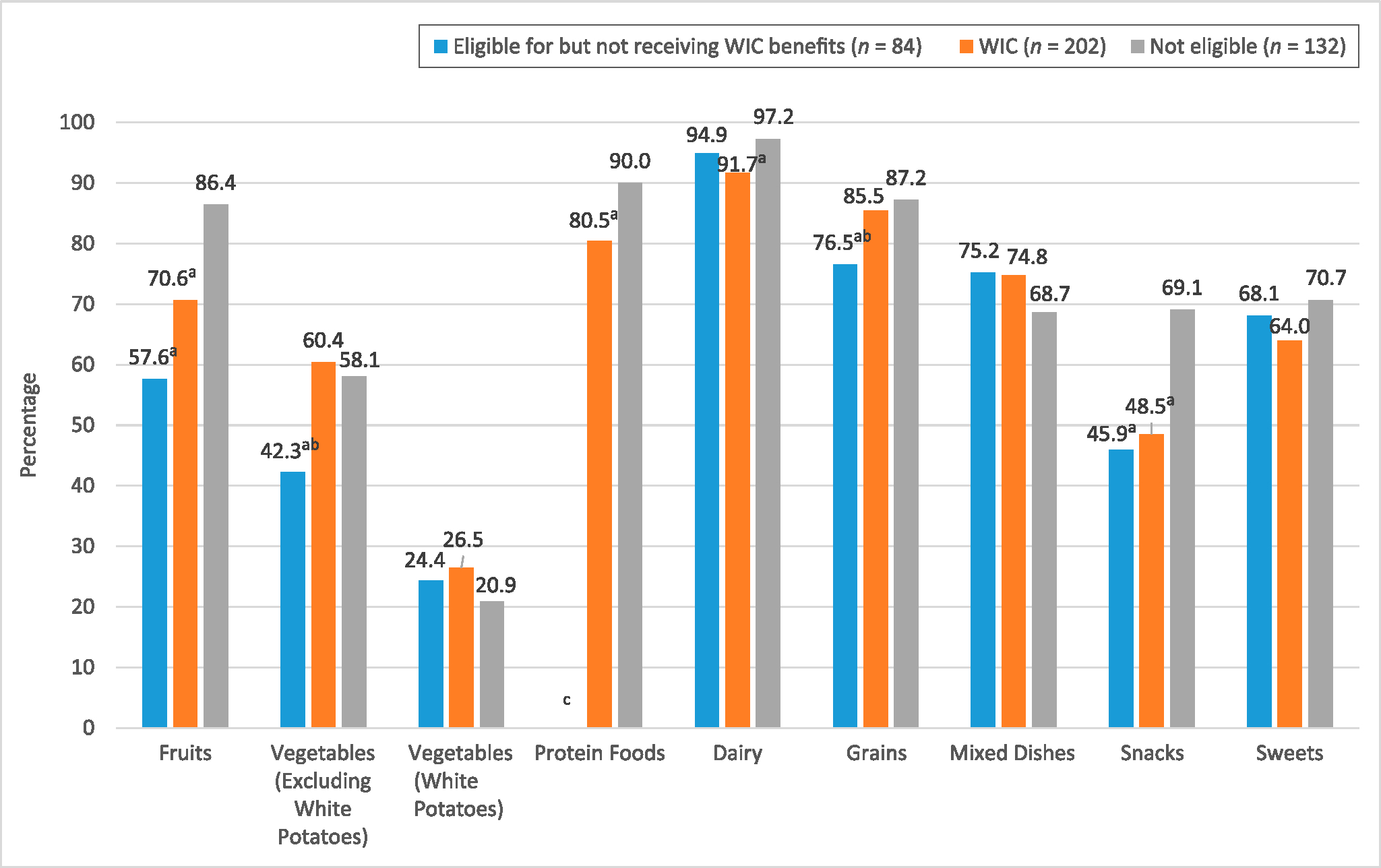
Percentage of US children who were 12 to 23 months of age and consuming different food categories by WIC status (NHANES 2011–2014). Age is presented in months at the time of examination in a MEC. Foods contained in the fruit category include apples, bananas, grapes, peaches and nectarines, berries, citrus fruits, melons, dried fruits, other fruits and fruit salad, and baby food fruit. Foods contained in the vegetables (excluding white potatoes) category include tomatoes, carrots, other red and orange vegetables, dark-green and leafy vegetables, lettuce and lettuce salads, legumes, string beans, onions, mixed vegetables, vegetable mixed dishes, corn, other starchy vegetables, and baby food vegetables. Foods contained in the vegetables (white potatoes) category include baked or boiled potatoes, French fries and other fried white potatoes, and mashed and white potato mixture. Foods contained in the protein foods category include meats, poultry, seafood, eggs and omelets, cured meats and poultry, nuts, seeds, processed soy products, baby food yogurt, cheese, and yogurt. Foods contained in the grains category include baby food cereals, ready-to-eat cereals, cooked cereals, breads, rolls, tortillas, quick breads and bread products, and cooked grains. Foods contained in the mixed-dishes category include meat, poultry, and seafood mixed dishes; rice, pasta, and other grain-based mixed dishes; pizza; burgers and sandwiches; and soup. Foods contained in the snacks category include savory snacks, crackers, and snack and/or meal bars. Foods contained in the sweets category include sweet bakery products, candy and sugar, and other desserts. WIC status is defined as children who are currently receiving WIC benefits. Eligible for but not receiving WIC benefits is defined as children who are eligible on the basis of family income/poverty ratio, receipt of Medicaid, or receipt of SNAP benefits (previously called food stamps). Not eligible is defined as children who do not meet WIC eligibility criteria. a Indicates results that are significantly different from those of children who are not eligible. b Indicates results that are significantly different from those of WIC participants (t test; P < .05). c Indicates that the estimate did not meet the National Center for Health Statistics criteria for data presentation. Although degrees of freedom and the relative CI were in compliance with data-presentation standards, the absolute CI was slightly >0.3.
DISCUSSION
Evidence suggests that early dietary patterns can contribute to those later in life and have lasting impacts.19 Programs such as WIC support families with low income by providing young children with healthy foods through its supplemental food package and nutrition education and counseling. Changes to the WIC food package align more closely with updated nutrition science, promote and support breastfeeding, and provide a wider variety of food.5 Indeed, these changes have resulted in WIC programs reporting a number of positive findings, including increases in the relative percent of the consumption of fruits, vegetables, and whole grains20; increased consumption of lower-fat milk21; and an overall improvement in dietary quality and alignment with the USDA Dietary Guidelines for Americans, 2010.22
Although researchers in studies have assessed dietary changes among WIC participants since the initial WIC food package changes that were instituted in 2009, we found no studies in which researchers specifically compared the consumption of different food and beverage categories between children who were WIC participants, those who were eligible for but not receiving WIC benefits, or those who were not eligible for WIC benefits, particularly among young children. Therefore, our findings are unique. Our data suggest that WIC participation may have an impact on reducing diet-related disparities for certain food categories as compared with children who are not eligible for WIC. The receipt of WIC benefits eliminated the disparity for 2 food categories (vegetables [excluding white potatoes] and grains), yet disparities remained for some food categories. Given the recent changes in the WIC food package, these observations suggest that WIC could be playing an important role in the foods young children are eating.
Evidence from longitudinal studies has revealed the importance of early dietary patterns on later dietary behaviors and health outcomes.23–28 For example, young children who had infrequent consumption of fruits and vegetables at 11 months of age continued to have infrequent consumption 6 years later.24 A 2015 American Academy of Pediatrics Clinical Report calls on pediatricians to play an active role in obesity prevention with a focus on starting before 2 years of age.29 These recommendations include the promotion of a diet that is rich in fruits, vegetables, whole grains, low-fat dairy products, and lean proteins and one that is limited in foods with high caloric density.29 Given that 12.3% of children who were 3 to 23 months of age and participating in WIC in 2014 had a high weight for length,30 there is a need for a continued focus on healthy dietary patterns beginning in the early years. Our data suggest that participation in WIC may help reduce disparities in the consumption of certain food categories on a given day, specifically vegetables (excluding white potatoes) and grains. Therefore, efforts to identify children who are eligible for WIC and to engage or retain them in the program may be beneficial and could have positive impacts on their later dietary behaviors and health outcomes. Pediatricians are a trusted source of information and may be able to help encourage participation or continued participation in programs such as WIC. This may be especially important because participation in WIC decreases precipitously between the time period of the first and second birthdays.2
This study has several limitations. First, “any consumption” on a given day does not represent habitual intake and may over- or underrepresent episodically consumed foods. The amount of foods or beverages consumed was not assessed. Therefore, for example, children who were receiving WIC benefits may have consumed a larger or smaller amount of fruits or vegetables as compared with children who were eligible for but not receiving WIC benefits or those who were not eligible for WIC benefits. However, the results do include information on the consumption of food and beverage categories by WIC status, and future analyses could be used to address this gap.
As described previously,13 we categorized foods and beverages on the basis of WWEIA food codes, and the frequency of consumption could be a result of the number and types of foods and beverages within each category. These categorizations reflect food groups as a whole and not specific ingredients within each food and beverage item (eg, potatoes or tomatoes consumed in beef stew). A complete breakdown of how we categorized each food and beverage is provided in Supplemental Table 2. During the majority of the survey time period (2011–2014), the WIC food package interim rule was in effect; however, beginning in March 2014, the final rule went into effect.6 The final rule included slight modifications, including the provision that white potatoes were eligible as part of the cash-value vouchers (implemented by July 1, 2015),31 the provision that yogurt could be used as a partial substitute for dairy (implemented by April 1, 2015), and the provision that increased the cash-value voucher for fruits and vegetables (implemented by June 2, 2014).6 These changes may have resulted in a higher percentage of children who were receiving WIC benefits consuming specific food items (ie, those food items that were affected by the modifications in the final rule). This was not accounted for in our analysis. Thus, our results may not necessarily reflect dietary consumption of food and beverage categories under the current USDA rule.
Although we pooled multiple survey years together, we still had small sample sizes for the different groups, specifically children who were eligible for but not receiving WIC benefits. This may have impacted our ability to detect statistically significant differences between the different groups of children. In addition, we were not able to stratify by race and Hispanic origin and WIC status because of small sample sizes and unstable estimates. Additional survey years may be required to confirm our findings. An earlier study revealed certain differences in the percentage of children who were consuming different foods and beverages by race and Hispanic origin,13 and we cannot rule out that the differences reported here by WIC status were not a function of differences by race and Hispanic origin. Lastly, these data are cross-sectional, so we cannot infer causality.
Data for this study (eg, dietary intake, household income, and SNAP and Medicaid participation data) are self-reported and subject to systematic errors or bias because individuals may have over- or underestimated amounts, values, or participation.32,33 Because of the nature of this study (ie, secondary data analysis), no attempt was made to address these biases. Proxy respondents provided the information on foods and beverages that were consumed for children 12 to 23 months of age. However, proxy respondents may not be with the child for the entire day and may not know all food and beverage items a child consumed.
This study also has several strengths. NHANES is a nationally representative study with an adequate sample size to allow for the presentation of findings by WIC status (participating in WIC, eligible for but not participating in WIC, and not eligible). Many studies do not differentiate further than WIC versus non-WIC participants, which makes our study unique in that we could assess the potential impact WIC had on the consumption of different food and beverage categories on a given day. The dietary data that were collected in NHANES use a standardized methodology, which helps respondents remember foods and beverages consumed in a given day.12
CONCLUSIONS
Our findings describe the proportion of children who were consuming different food and beverage categories on any given day by WIC status using data collected after the 2009 WIC food package changes. We found that WIC participation may have contributed to reduced disparities in the consumption of grains and vegetables (excluding white potatoes), but this was not seen across all food categories.
Because over one-half of infants and 1-year-old children who are eligible for WIC participate in the program,2 WIC plays a pivotal role in shaping the nutrition and health status of US children. Pediatricians can help encourage their patients to participate or continue participating in programs such as WIC in an effort to reduce diet-related disparities between children who are eligible for WIC and those who are not eligible.
Supplementary Material
WHAT’S KNOWN ON THIS SUBJECT:
In 2009, the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) revised its child food package to align more closely with updated nutrition science. As a result, dietary improvements have been reported among program participants.
WHAT THIS STUDY ADDS:
Since the WIC food package changes, children who were aged 12 to 23 months and eligible for but not receiving WIC had the lowest percentage of consuming certain food groups compared with those who were not eligible for WIC and those who were receiving WIC. Our findings suggest WIC participation improves diet-related disparities.
ACKNOWLEDGMENT
We acknowledge Dr Eve Essery Stoody for her helpful review and comments on the article and data analysis.
ABBREVIATIONS
- CI
confidence interval
- MEC
mobile examination center
- NHANES
National Health and Nutrition Examination Survey
- SNAP
Supplemental Nutrition Assistance Program
- USDA
United States Department of Agriculture
- WIC
Special Supplemental Nutrition Program for Women, Infants, and Children
- WWEIA
What We Eat in America
Footnotes
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
Dr Casavale′s current affiliation is Center for Food Safety and Applied Nutrition, United States Food and Drug Administration, College Park, MD.
Dr Hamner conceptualized and designed the study, conducted analyses, and drafted the initial manuscript; Dr Paolicelli, Dr Casavale, Ms Haake, and Ms Bartholomew provided substantial contributions to the design of the study and interpretation of the data and critically reviewed and revised the manuscript; and all authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
REFERENCES
- 1.US Department of Agriculture, Food and Nutrition Service. About WIC- WIC at a glance. 2017. Available at: https://www.fns.usda.gov/wic/about-wic-wic-glance. Accessed November 1, 2017
- 2.US Department of Agriculture, Food and Nutrition Service, Office of Policy Support. National- and State-Level Estimates of Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) Eligibles and Program Reach in 2014, and Updated Estimates for 2005–2013. Alexandria, VA: US Department of Agriculture; 2017 [Google Scholar]
- 3.US Department of Agriculture, Food and Nutrition Service. Background: revisions to the WIC food package. 2015. Available at: https://www.fns.usda.gov/wic/background-revisions-wic-food-package. Accessed November 1, 2017
- 4.US Department of Agriculture, Food and Nutrition Service. Special Supplemental Nutrition Program for Women, Infants and Children (WIC): revisions in the WIC food packages; interim rule. Fed Regist. 2007;72:68965–69032. Codified at 7 CFR §246 [Google Scholar]
- 5.US Department of Agriculture, Food and Nutrition Service. Final rule: revisions in the WIC food packages. 2017. Available at: https://www.fns.usda.gov/wic/final-rule-revisions-wic-food-packages. Accessed November 1, 2017
- 6.US Department of Agriculture, Food and Nutrition Service. Final rule: revisions in the WIC food package. Fed Regist. 2014;79:12273–12300. Codified at 7 CFR §246 [Google Scholar]
- 7.Schultz DJ, Byker Shanks C, Houghtaling B. The impact of the 2009 Special Supplemental Nutrition Program for Women, Infants, and Children food package revisions on participants: a systematic review [published correction appears in J Acad Nutr Diet. 2015;115(11):1886]. J Acad Nutr Diet. 2015;115(11):1832–1846 [DOI] [PubMed] [Google Scholar]
- 8.National Center for Health Statistics. About the National Health and Nutrition Examination Survey. Available at: www.cdc.gov/nchs/nhanes/about_nhanes.htm. Accessed March 14, 2016
- 9.Curtin LR, Mohadjer LK, Dohrmann SM, et al. National Health and Nutrition Examination Survey: sample design, 2007–2010. Vital Health Stat 2. 2013;(160):1–23 [PubMed] [Google Scholar]
- 10.Johnson CL, Dohrmann SM, Burt VL, Mohadjer LK. National Health and Nutrition Examination Survey: sample design, 2011–2014. Vital Health Stat 2. 2014;(162):1–33 [PubMed] [Google Scholar]
- 11.National Center for Health Statistics. NHANES response rates and population totals. 2015. Available at: https://wwwn.cdc.gov/nchs/nhanes/ResponseRates.aspx. Accessed October 28, 2016
- 12.Moshfegh AJ, Rhodes DG, Baer DJ, et al. The US Department of Agriculture automated multiple-pass method reduces bias in the collection of energy intakes. Am J Clin Nutr. 2008;88(2):324–332 [DOI] [PubMed] [Google Scholar]
- 13.Hamner HC, Perrine CG, Gupta PM, Herrick KA, Cogswell ME. Food consumption patterns among U.S. children from birth to 23 months of age, 2009–2014. Nutrients. 2017;9(9):E942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.US Department of Agriculture, Agriculture Research Service, Food Surveys Research Group. What We Eat in America food categories. 2015. Available at: https://www.ars.usda.gov/ARSUserFiles/80400530/pdf/1314/food_category_list.pdf. Accessed March 14, 2016
- 15.US Department of Agriculture, Agriculture Research Service, Food Surveys Research Group. What We Eat in America food categories 2009–2010. Available at: https://www.ars.usda.gov/ARSUserFiles/80400530/pdf/0910/Food_categories_2009-2010.pdf. Accessed May 22, 2017
- 16.US Department of Agriculture, Agriculture Research Service, Food Surveys Research Group. What We Eat in America food categories 2011–2012. Available at: https://www.ars.usda.gov/ARSUserFiles/80400530/pdf/1112/Food_categories_2011-2012.pdf. Accessed May 22, 2017
- 17.US Department of Agriculture, Agriculture Research Service, Food Surveys Research Group. What We Eat in America food categories 2013–2014. Available at: https://www.ars.usda.gov/ARSUserFiles/80400530/pdf/1314/Food_categories_2013-2014.pdf. Accessed May 22, 2017
- 18.National Center for Health Statistics, Division of Health and Nutrition Examination Surveys. National Health and Nutrition Examination Survey: Analytic Guidelines, 2011–2012. Hyattsville, MD: Centers for Disease Control and Prevention; 2013 [Google Scholar]
- 19.Birch LL, Doub AE. Learning to eat: birth to age 2 y. Am J Clin Nutr. 2014;99(3):723S–728S [DOI] [PubMed] [Google Scholar]
- 20.Chiasson MA, Findley SE, Sekhobo JP, et al. Changing WIC changes what children eat. Obesity (Silver Spring). 2013;21(7):1423–1429 [DOI] [PubMed] [Google Scholar]
- 21.Whaley SE, Ritchie LD, Spector P, Gomez J. Revised WIC food package improves diets of WIC families. J Nutr Educ Behav. 2012;44(3):204–209 [DOI] [PubMed] [Google Scholar]
- 22.Tester JM, Leung CW, Crawford PB. Revised WIC food package and children’s diet quality. Pediatrics. 2016;137(5):e20153557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Perrine CG, Galuska DA, Thompson FE, Scanlon KS. Breastfeeding duration is associated with child diet at 6 years. Pediatrics. 2014;134(suppl 1):S50–S55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Grimm KA, Kim SA, Yaroch AL, ScanlonKS. Fruit and vegetable intake during infancy and early childhood. Pediatrics. 2014;134(suppl 1):S63–S69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sonneville KR, Long MW, Rifas-Shiman SL, Kleinman K, Gillman MW, Taveras EM. Juice and water intake in infancy and later beverage intake and adiposity: could juice be a gateway drink? Obesity (Silver Spring). 2015;23(1):170–176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rose CM, Savage JS, Birch LL. Patterns of early dietary exposures have implications for maternal and child weight outcomes. Obesity (Silver Spring). 2016;24(2):430–438 [DOI] [PubMed] [Google Scholar]
- 27.Hohman EE, Paul IM, Birch LL, Savage JS. INSIGHT responsive parenting intervention is associated with healthier patterns of dietary exposures in infants. Obesity (Silver Spring). 2017;25(1):185–191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rose CM, Birch LL, Savage JS. Dietary patterns in infancy are associated with child diet and weight outcomes at 6 years. Int J Obes (Lond). 2017;41(5):783–788 [DOI] [PubMed] [Google Scholar]
- 29.Daniels SR, Hassink SG; Committee on Nutrition. The role of the pediatrician in primary prevention of obesity. Pediatrics. 2015;136(1). Available at: www.pediatrics.org/cgi/content/full/136/1/e275 [DOI] [PubMed] [Google Scholar]
- 30.Freedman DS, Sharma AJ, Hamner HC, et al. Trends in weight-for-length among infants in WIC from 2000 to 2014. Pediatrics. 2017;139(1):e20162034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.US Department of Agriculture. WIC policy memorandum #2015–3: eligibility of white potatoes for purchase with the cash-value voucher. 2014. Available at: https://fns-prod.azureedge.net/sites/default/files/wic/WPM_2015-3-Eligibility_of_White_Potatoes_for_Cash_Value_Voucher.pdf. Accessed March 12, 2018
- 32.Burrows TL, Martin RJ, Collins CE. A systematic review of the validity of dietary assessment methods in children when compared with the method of doubly labeled water. J Am Diet Assoc. 2010;110(10):1501–1510 [DOI] [PubMed] [Google Scholar]
- 33.Subar AF, Freedman LS, Tooze JA, et al. Addressing current criticism regarding the value of self-report dietary data. J Nutr. 2015;145(12):2639–2645 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


