Abstract
This report provides historical context and rationale for coordinated, systematic, and evidence-based public health emergency preparedness and response (EPR) activities to address the needs of women of reproductive age. Needs of pregnant and postpartum women, and infants—before, during, and after public health emergencies—are highlighted. Four focus areas and related activities are described: (1) public health science; (2) clinical guidance; (3) partnerships, communication, and outreach; and (4) workforce development. Finally, the report summarizes major activities of the Division of Reproductive Health’s EPR Team at the Centers for Disease Control and Prevention.
Keywords: maternal and infant health, emergency preparedness and response, maternal health
Introduction
Public health emergencies—including severe weather and natural disasters, infectious disease outbreaks, and man-made disasters—disrupt individual lives, families, and communities.1 Disasters may affect access to medical and social services,2 and may be associated with poor reproductive health outcomes such as pregnancy loss, preterm birth, and congenital anomalies.3–5 The Pandemic and All-Hazards Preparedness and Advancing Innovation Act of 2019 identifies pregnant and postpartum (P/PP) women and infants as populations with special clinical needs during public health emergencies.6 Therefore, women of reproductive age (WRA), 15–44 years, are a population of special interest in emergency preparedness and response (EPR).
The Centers for Disease Control and Prevention (CDC) Division of Reproductive Health (DRH) has been active in EPR since 2004. The inclusion of a maternal health team in CDC emergency operations during the 2009–2010 H1N1 Influenza Pandemic marked the beginning of enhanced collaborations between DRH in the National Center for Chronic Disease Prevention and Health Promotion (NCCDPHP) and the National Center on Birth Defects and Developmental Disabilities (NCBDDD). The team identified that pregnant women with H1N1 influenza had a disproportionately high risk of mortality due to 2009 influenza A (H1N1).7
After the H1N1 influenza pandemic, DRH progressively formalized its work in emergency response capacity building by establishing an EPR activity in 2011 followed by a dedicated EPR team in 2018. The EPR team’s mission is to advance public health science and build the capacity of the public health system and workforce to optimize reproductive and infant health before, during, and after public health emergencies.
For the past decade, the public health and medical communities have faced natural disasters and complex unprecedented infectious disease outbreaks. Since 2011, DRH participated in CDC’s public health emergency responses to Ebola in West Africa, Zika virus in the Americas, U.S. hurricane responses, and the coronavirus disease 2019 (COVID-19) response.8 These public health emergencies warranted continued coordination and multidisciplinary approaches to maternal and infant health (MIH).
DRH collaborated across CDC to conduct surveillance and research, respond to inquiries, develop clinical and public health guidance, and develop communication messages and other media products. Moreover, DRH collaborates with public health partners, including medical or professional organizations, and academia to identify gaps in knowledge, capacity building needs, and concerns relevant to EPR. These collaborations have elevated attention to MIH needs during public health emergencies and informed the development of preparedness tools and response-related resources.
Activities to build capacity for addressing reproductive health in emergencies fall into four focus areas: (1) public health science; (2) clinical guidance; (3) partnerships, communication, and outreach; and (4) workforce development.
Public health science
Public health science includes activities for advancing reproductive health before, during, and after public health emergencies. DRH has led or contributed to >100 surveillance activities, analytical studies, or guidance documents focused on emergency preparedness, infectious disease outbreaks, and CDC responses from 2011 to 2021. Examples include developing or leveraging existing surveillance to collect data about WRA and infants.
To enhance EPR MIH surveillance, survey questions on general emergency preparedness are now available for well-established surveillance systems such as the Behavioral Risk Factor Surveillance System (BRFSS)9 and the Pregnancy Risk Assessment and Monitoring System (PRAMS).10 In 2016, an optional eight-part question was made available as a PRAMS standard question to assess family disaster preparedness planning.11 Data for Hawaii12 and Tennessee were assessed in collaboration with the respective states’ PRAMS program and health department. Established surveillance systems such as BRFSS and PRAMS have also been leveraged during emergency responses.
During the Puerto Rico Zika response, the BRFSS was leveraged to assess prevalence of contraceptive use and other Zika virus prevention measures among WRA.13 PRAMS was similarly leveraged in Puerto Rico and used to conduct a hospital-based survey among women with a recent live birth about their concerns, behaviors, and experiences related to Zika virus exposure.14,15
The U.S. Zika Pregnancy and Infant Registry was developed as a partnership between CDC’s DRH and NCBDDD and state, local, and territorial health departments. The Registry was established to rapidly collect data on pregnant women with Zika virus infection and their infants,16 and became NCBDDD’s Surveillance for Emerging Threats to Mothers and Babies Network (SET-NET) after the Zika virus response ended17; SET-NET is a system that collects information on emerging health threats to pregnant women and their children through the first 3 years of life.
To advance public health science, DRH staff used existing data and developed tools for identification, measurement, and preparedness for the unique needs of WRA, especially P/PP women and infants during public health emergencies. One such tool is a collection of postdisaster health indicators and measures as well as example questions to guide assessment and surveillance. These indicators were developed in collaboration with expert partners across the United States to promote uniformity of measures and data collected, and can be used to inform and prioritize public health interventions and policies.18 Another tool is the pregnancy estimator tool, which estimates the number of pregnant women in a U.S. jurisdiction at any given time.
The pregnancy estimator can be used for preparedness and response efforts. DRH has also produced analytic reports for assessing potential impacts of public health emergencies on WRA. Examples include a report examining population-level changes in birth rates, birth outcomes, and pregnancy risk factors among women giving birth after a natural disaster,19 a systematic review on methodological issues in studies of disaster-related effects on reproductive health outcomes in the United States,3 and a report outlining the evidence for contraception availability to prevent unintended pregnancies during emergency situations.20
During the 2009–2010 H1N1 influenza pandemic response, the importance of studying influenza related to pregnant women and infants emerged.21 Therefore, in 2015, DRH formally developed a set of all-hazards focused questions called Guiding Principles (Fig. 1) to assess potential and emerging threats to WRA, especially P/PP women, and infants due to maternal exposure. The question format was used to prepare for biological events22 and for the Ebola response.23 Recommendations to guide investigation of direct infant exposures and to inform delivery of pediatric care were considered beyond the scope of the Guiding Principles. Clinical professional organizations, including the American Academy of Pediatrics, have provided focused pediatric recommendations and have outlined the complexity of infant care in such settings.24,25
FIG. 1.
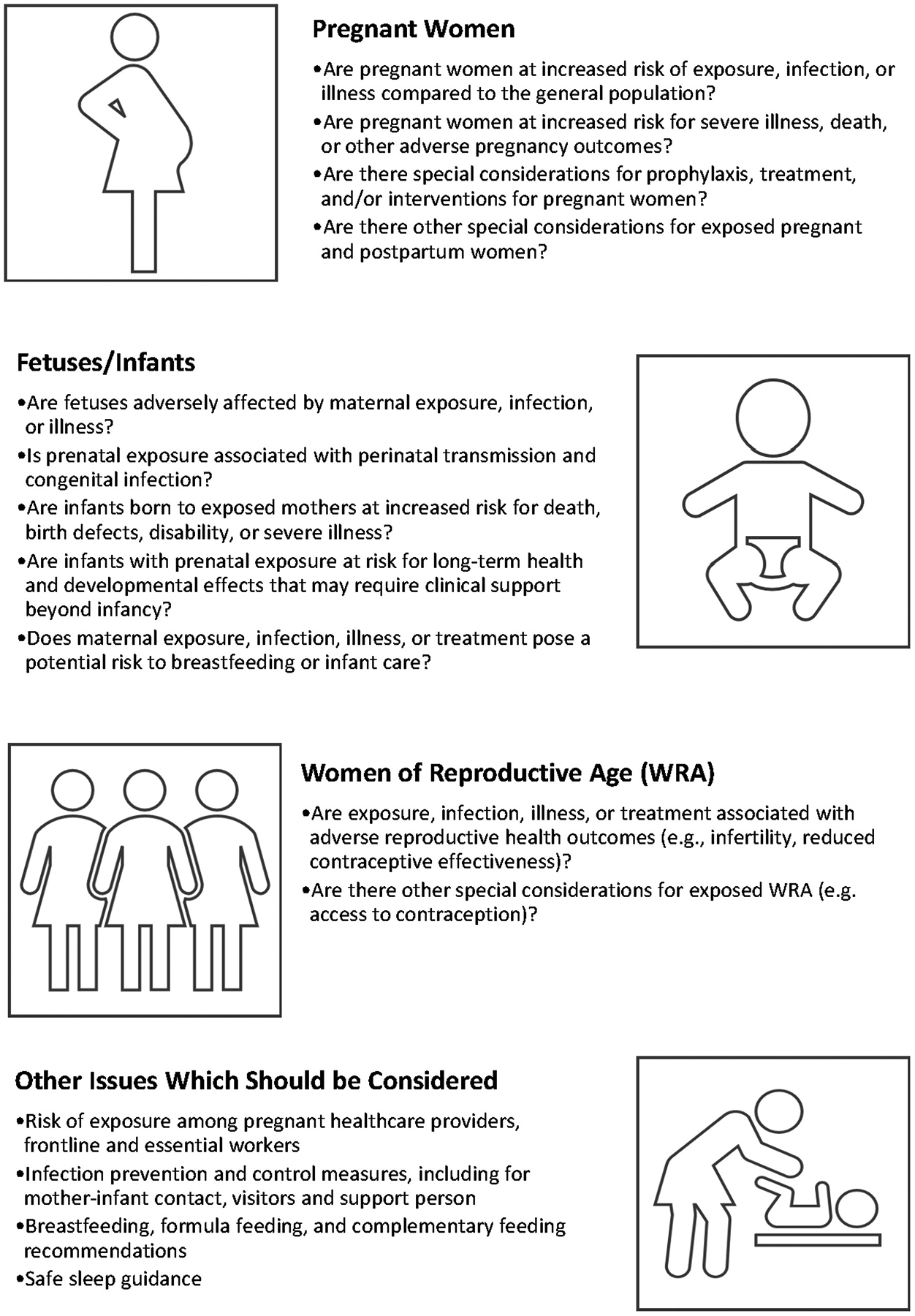
Guiding principles for assessing potential and emerging threats to WRA and infants during emergencies. WRA, women of reproductive age.
Clinical guidance
Knowledge gained from public health science has been used in both response and preparedness settings to inform clinical guidance for WRA. DRH and partners have worked closely to ensure that clinical recommendations and guidance are both timely and evidence driven. As a result of these efforts, recommendations and guidance documents and the related tools for health care providers may undergo multiple updates to keep pace with the speed of emerging science and evolving response needs. For example, from 2011 to 2021, DRH and its partners developed and updated 27 clinical guidance documents for obstetric and infant care settings during recent public health emergencies, including the H1N1 Influenza Pandemic (n = 9),8 the 2016 Zika virus outbreak (n = 11),26 the 2014 Ebola outbreak (n = 2),8 and the COVID-19 pandemic (n = 5).27
Outside of response settings, DRH has worked with partners to develop guidance for medical countermeasures to public health threats such as bioterrorism events to increase preparedness. These efforts involve rigorous review of existing data and considerations of the impacts of disease, treatment, and preventive measures for WRA and infants. Examples include DRH’s systematic review of worldwide anthrax cases among pregnant women that informed clinical guidance,28 a review of antimicrobial safety profiles for prophylaxis and treatment of anthrax in pregnant women,29 a task force report outlining resource needs for neonatal and pediatric emergency mass critical care,30 and an expert meeting report summarizing clinical considerations for anthrax prophylaxis and treatment of P/PP women.31
Partnerships, communication, and outreach
Partnerships, communication, and outreach involve (1) leveraging partnerships within CDC as well as with health departments, MIH partners, medical professionals, and academic institutions to increase reach of emergency response efforts; (2) strengthening communication strategies with national MIH partners and clinicians; and (3) communicating findings and increasing awareness of EPR in reproductive health through planned peer exchange activities.
Strategic partnerships within CDC and with local, territorial, state health departments, MIH partner organizations, and academic institutions have been crucial to increasing reach of EPR efforts. For example, in collaboration with the University of North Carolina at Chapel Hill, DRH developed the Reproductive Health After Disaster Toolkit to guide health departments in the postdisaster assessment of WRA and their health needs.32 Universities and local and state public health agencies have used the toolkit after hurricanes, tornadoes, and flooding in several southern states.33,34 DRH is updating this toolkit in partnership with the Council of State and Territorial Epidemiologist (CSTE). The updated toolkit will support jurisdictions in making immediate and interim decisions to address the reproductive health needs of women and infants before, during, and after disasters.
DRH provided technical assistance to the CDC Foundation to establish the Zika Contraception Access Network (Z-CAN), a network of trained health care providers aimed at preventing Zika-related birth defects through rapid implementation of reversible contraceptive services in Puerto Rico. The network provided client-centered contraceptive counseling and same day access to contraceptive methods to >21,000 women between May 2016 and mid-August 2017.35 The program included a communications and marketing campaign called “Ante La Duda, Pregunta” to increase awareness of Z-CAN services.36 The program also developed the “Increasing Access to Contraception: A Toolkit for Program Development, Implementation, and Evaluation,” a suite of tools, and partnership and outreach strategies for adapting and implementing Z-CAN.
Collaboration with external partners through outreach is critical to building EPR capacity nationwide. In September 2018, CityMatCH conducted a maternal child health (MCH) EPR capacity assessment with its members. Results were communicated to national, state, and local MCH experts and ongoing needs were discussed at a stakeholder meeting. City and local health department (LHD) staff shared that because MCH staff were not involved in planning, the MCH population’s needs were not sufficiently addressed in EPR plans. To address this concern, in 2019, DRH partnered with the CSTE to conduct a nationwide epidemiology capacity assessment to understand MCH EPR capacity within state and territorial public health departments.
Key findings from responding jurisdictions showed that MCH epidemiologists had adequate support during normal operations, but a substantial proportion (34.4%) faced unique challenges in conducting surveillance, accessing and collecting data, or responding to the needs of WRA and infants specifically during an emergency.37 More than half of MCH Epidemiologists were not considered “essential personnel” and only 10% indicated routine or frequent collaboration between MCH and EPR staff.37 Findings from this assessment illustrate the importance of including MIH into EPR activities and the need for MIH EPR collaboration at the jurisdictional level.
To promote collaboration and build EPR capacity for MIH, DRH partnered with the Association of Maternal and Child Health Programs (AMCHP) in an action learning collaborative (ALC). The ALC included an annual cohort of multidisciplinary state and territory teams with five to seven members representing MIH and Public Health Emergency Preparedness. Sixteen states and four territories participated in three cohorts from 2018–2021 (Cohort #1: Hawaii, New Jersey, Texas; Cohort #2: Arizona, Georgia, Missouri, Nevada, Rhode Island, South Carolina, West Virginia, Puerto Rico; Cohort #3: California, Indiana, Maine, Ohio, Wisconsin, Wyoming, America Samoa, Commonwealth of the Northern Mariana Islands, Guam).
Each cohort enhanced their jurisdictional EPR frameworks to specifically address emergency needs of WRA (especially P/PP) and infants by providing feedback on a preparedness checklist, and developing or implementing action plans for checklist components. The preparedness checklist is available for health professionals, epidemiologists, emergency preparedness personnel, and other public health staff interested in reproductive health and EPR.38
With the goal of further expanding capacity building opportunities, DRH is actively working with the National Association of City and County Health Officials (NACCHO) to increase LHD capacity to prioritize the needs of MCH populations during emergencies. Select LHDs are provided technical assistance through a virtual learning collaborative to strengthen MCH and EPR collaboration. In addition, NACCHO conducting a multimedia assessment to identify needs, concerns, and health-seeking behaviors of expectant parents amid the COVID-19 pandemic. NACCHO will develop outreach and health promotion materials tailored to WRA, especially P/PP women based on the assessment findings.
Communication and outreach strategies include preparing and disseminating action-oriented messages to partners, health care providers, and the public. DRH collaborates with external and internal colleagues to disseminate scientific findings and EPR information for general, professional, and clinical audiences. Examples of emergency risk communication materials include the development of electronic resources with disaster planning messages such as “Safety Messages for Pregnant, Postpartum, and Breastfeeding Women During Disasters,”39 and a CDC Feature: “Disaster Safety for Expecting and New Parents,”40 which are articles written by subject matter experts and health communicators to emphasize strong call-to-action messages for general audiences. DRH also made plain language messaging more accessible by translating these resources to Spanish.
DRH’s communication and outreach efforts have included disseminating the latest scientific findings, recommendations, and resources through presentations, such as nationwide webinars/conferences, partner updates, networking and peer exchange, as well as through social media. The dissemination of scientific information is accomplished through peer-review journal publications, Morbidity and Mortality Weekly Report publications, technical presentations, and numerous other timely social media and partner updates to internal and external partners. DRH fosters frequent communications and exchanges with collaborators to ensure partners have access to tools and resources, and to encourage widespread awareness of resources to prepare for and respond to the needs of WRA and infants during public health emergencies.
Workforce development
Workforce development includes (1) developing and maintaining subject matter expertise, (2) creating DRH all hazards preparedness plans to address MIH during emergencies, and (3) identifying training needs and developing educational curricula for internal CDC staff. One example of a workforce development activity was the creation of the EPR operational plan and infrastructure to support DRH staff readiness and response. This document became the foundation for a broader CDC MIH internal operational plan developed collaboratively with the NCBDDD’s Children’s Preparedness Unit; Division of Birth Defects and Infant Disorders; the Division of Nutrition, Physical Activity and Obesity; and the Center for Preparedness and Response.
The plan provides general guidance for coordinating, developing, and maintaining maternal health activities during an emergency response. This plan and previous experiences building collaborative relationships within CDC have been beneficial to support collaboration while working remotely during the COVID-19 response. The plan enabled a strategic and coordinated MIH response within CDC during the pandemic.
To develop and maintain subject matter expertise, DRH continuously participates in the planning and execution of agency-wide and interagency emergency preparedness activities such as drills, tabletop exercises, and full-scale exercises on topics such as pandemic influenza, smallpox, anthrax, and nuclear/radiation incidents. Participation in these exercises optimizes DRH staff capacity to respond to public health emergencies. Activities include training about specific hazards for WRA, planning mock emergency response situations about reproductive health, and creating and adapting standard operating procedures, communication materials, and other supporting materials. Exercises such as these foster federal cross-agency collaboration and strengthen relationships within CDC for enhanced MIH EPR capacity.
To help build EPR workforce capacity of the public health system, DRH developed the “Reproductive Health in Emergency Preparedness and Response” course for public health and medical professionals in the United States.41 Of 828 public health and medical professionals who completed the online course, 758 unique learners (91.5%) received continuing education credits (66% for nurses or physicians, 32% for nonphysicians, and 2% for volunteers who completed pilot testing). As previously mentioned, the course is currently being updated in collaboration with AMCHP. The revised course will highlight preparedness and response resources and tools to support action planning and prioritization and EPR capacity of U.S. jurisdictions.
CDC’s MIH Emergency Response to COVID-19
As part of the COVID-19 response, the four focus areas remain a priority. DRH EPR team staff co-lead the Pregnancy and Infant Linked Outcomes Team (PILOT), a cross-division and cross-center multidisciplinary team supporting CDC response efforts to collect and analyze data to understand the impact of COVID-19 on pregnant women and infants. Public health science related to the COVID-19 response has included rapid data collection to inform response actions and preparing and sharing evidence-based resources and tools for health care professionals, health departments, and other partners.
In early 2020, DRH staff rapidly conducted a systematic review of case reports of Middle East respiratory syndrome coronavirus, severe acute respiratory syndrome coronavirus (SARS-CoV), and SARS-CoV-2 infections during pregnancy to inform the developing COVID-19 outbreak, using the Guiding Principles to inform key questions.42 As the outbreak response continues to evolve, the Guiding Principles serve as a framework to assess the impact of COVID-19 during pregnancy, and inform clinical guidance for WRA and infants.
Building on previous work from CDC’s responses and subsequent preparedness planning exercises, the team was able to use national COVID-19 case surveillance data to determine that pregnancy is associated with increased risk of severe illness from COVID-19, including death.43,44 DRH also worked collaboratively with NCBDDD to adapt the SET-NET for COVID-19 at the beginning of the response, and continues to collect longitudinally linked surveillance data to understand how infection during pregnancy affects pregnant women and their infants.17,45
In addition, DRH used the existing PRAMS infrastructure to implement two supplements to collect data on (1) prenatal care, delivery, postpartum care, and infant care during the pandemic, and (2) COVID-19 vaccination. Data collected as part of these efforts have been used to help direct public health action, communication, and outreach efforts and inform clinical guidance for obstetric and infant care settings. Because the SARS-CoV-2 virus is novel, its direct effects as well as the broader impact of the pandemic on P/PP women and infants were unknown, but knowledge continues to advance.42,44,46
Clinical guidance activities involve providing leadership and subject matter expertise in the development of guidance documents for health care professionals who care for pregnant patients with COVID-19 and who treat neonates with suspected or confirmed SARS-CoV-2 infection. DRH continuously provides clinical and epidemiological expertise to address maternal health inquiries related to COVID-19 medical care, diagnostic and management approaches from health care providers, public health professionals, and the public.
The emergence of COVID-19 has highlighted the importance of intentional, respectful, and established partnerships during a complex response to rapidly investigate the impact of infectious diseases during pregnancy. Strategies include strengthening collaborations with partners, identifying communication and outreach approaches, and disseminating scientific findings and information to general, public health professionals, and clinical audiences.47
Close collaborations within CDC included response and task force leadership, as well as other MIH subject matter experts from multiple centers across the agency. Although internal partnerships evolve during a response, they are necessary for ensuring that MIH matters are adequately addressed. Collaborations with health departments, MCH partners, and medical professionals have also been critical to increase effectiveness of emergency response efforts and widespread awareness of SARS-CoV-2 infection in pregnancy.
Workforce development response-related activities for COVID-19 include hosting internal information sharing and peer-exchange forums to keep staff up to date with response activities, learn about the experiences and deployment of responders, and help maintain readiness for deployment opportunities. DRH disseminates scientific findings and information on SARS-CoV-2 infection in pregnancy to internal, public health, and clinical audiences through Clinical Outreach and Communication Activity calls, COVID-19 Webinar and Partners Calls and technical presentations to build EPR-MIH capacity. DRH also contributes in the distribution of a literature review e-mail update to >60 individuals three times per week highlighting recent publications on COVID-19 and pregnancy to develop and maintain subject matter expertise.
Future Directions
DRH’s EPR work for WRA and infants reflect the value of a coordinated response to address MIH needs in public health emergency settings. Attention to MIH needs is critical for future EPR activities. Ongoing exchanges of subject matter expertise (e.g., workgroups), peer-exchange forums (e.g., conferences and webinars), and enhanced communication can encourage further strengthening of jurisdictional capacity to better optimize reproductive health during public health emergencies.
Improving facets of public health surveillance (such as collecting pregnancy and gestational status) and the need for data linkages (such as for mother infant dyads) are critical in any emergency where WRA and infants are impacted. DRH’s EPR priority is to optimize reproductive and infant health during emergencies through advancing public health science, informing clinical guidance, collaborating with partners, promoting communication and outreach efforts, and enhancing workforce development.
Acknowledgments
Members of Division of Reproductive Health Emergency Preparedness and Response Team: Karen Chang, PhD; L. Duane House, PhD; Jessica Meeker, PhD, Aspen Riser, MPH; Maria Rivera, MPH; Regina Simeone, MPH, MS; Ashley Smoots, MPH; Bailey Wallace, MPH.
Funding Information
No funding was received to assist with the preparation of this manuscript.
Footnotes
Disclaimer
Findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- 1.Nelson C, Lurie N, Wasserman J, Zakowski S. Conceptualizing and defining public health emergency preparedness. Am J Public Health 2007;97(Suppl_1): S9–S11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Callaghan WM, Rasmussen SA, Jamieson DJ, et al. Health concerns of women and infants in times of natural disasters: Lessons learned from hurricane Katrina. Matern Child Health J 2007;11:307–311. [DOI] [PubMed] [Google Scholar]
- 3.Zotti ME, Williams AM, Robertson M, Horney J, Hsia J. Post-disaster reproductive health outcomes. Matern Child Health J 2012;17:783–796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Harville E, Xiong X, Buekens P. Disasters and perinatal health:A systematic review. Obstet Gynecol Surv 2010;65: 713–728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cordero JF. The epidemiology of disasters and adverse reproductive outcomes: Lessons learned. Environ Health Perspect 1993;101(Suppl 2):131–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pandemic and All-Hazards Preparedness and Advancing Innovation Act of 2019, S. 1379, Congress, 116 sess (Sen. Burr RR-N 2019) 2019. Available at: https://www.govtrack.us/congress/bills/116/s1379/text Accessed January 9, 2019.
- 7.Siston AM, Rasmussen SA, Honein MA, et al. Pandemic 2009 influenza A (H1N1) virus illness among pregnant women in the United States. JAMA 2010;303:1517–1525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Division of Reproductive Health National Center for Chronic Disease Prevention and Health Promotion. Reproductive health in emergency preparedness and response. 2021. Available at: https://www.cdc.gov/reproductivehealth/emergency/index.html Accessed August 25, 2021.
- 9.Xu F, Mawokomatanda T, Flegel D, et al. Surveillance for certain health behaviors among states and selected local areas—Behavioral risk factor surveillance system, United States, 2011. MMWR Surveill Summ 2014;63:1–149. [PubMed] [Google Scholar]
- 10.Zilversmit L, Sappenfield O, Zotti M, McGehee MA. Preparedness planning for emergencies among postpartum women in Arkansas during 2009. J Women’s Health 2014; 24:e83–e88. [DOI] [PubMed] [Google Scholar]
- 11.Division of Reproductive Health National Center for Chronic Disease Prevention and Health Promotion. PRAMS Phase 8 Standard Questions. Centers for Disease Control and Prevention; 2016. [Google Scholar]
- 12.Strid P, Fok CCT, Zotti M, et al. Disaster preparedness among women with a recent live birth in Hawaii - Results from the pregnancy risk assessment monitoring system (PRAMS), 2016. Disaster Med Public Health Prep 2021:1–10. doi: 10.1017/dmp.2021.274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pazol K, Ellington SR, Fulton AC, et al. Contraceptive use among women at risk for unintended pregnancy in the context of public health emergencies—United States, 2016. MMWR Morb Mortal Wkly Rep 2018;67:898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.D’Angelo DV, Salvesen von Essen B, Lamias MJ, et al. Measures taken to prevent Zika virus infection during pregnancy—Puerto Rico, 2016. MMWR Morb Mortal Wkly Rep 2017;66:574–578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Division of Reproductive Health National Center for Chronic Disease Prevention and Health Promotion. PRAMS Zika Postpartum Emergency Response Survey (PRAMS-ZPER) in Puerto Rico. 2021. Available at: https://www.cdc.gov/prams/special-projects/zika/index.htm Accessed July 21, 2021.
- 16.Simeone RM, Shapiro-Mendoza CK, Meaney-Delman D, et al. Possible Zika virus infection among pregnant women—United States and Territories, May 2016. MMWR Morb Mortal Wkly Rep 2016;65:514–519. [DOI] [PubMed] [Google Scholar]
- 17.Woodworth KR, Reynolds MR, Burkel V, et al. A Preparedness model for mother–baby linked longitudinal surveillance for emerging threats. Matern Child Health J 2021;25:198–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zotti ME, Williams AM, Wako E. Post-disaster health indicators for pregnant and postpartum women and infants. Matern Child Health J 2015;19:1179–1188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tong VT, Zotti ME, Hsia J. Impact of the Red River catastrophic flood on women giving birth in North Dakota, 1994–2000. Matern Child Health J 2011;15:281–288. [DOI] [PubMed] [Google Scholar]
- 20.Ellington SR, Kourtis AP, Curtis KM, et al. Contraceptive availability during an emergency response in the United States. J Women’s Health 2013;22:189–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rasmussen SA, Kissin DM, Yeung LF, et al. Preparing for influenza after 2009 H1N1: Special considerations for pregnant women and newborns. Am J Obstet Gynecol 2011;204(6 Suppl 1):S13–S20. [DOI] [PubMed] [Google Scholar]
- 22.Watson AK, Ellington S, Nelson C, Treadwell T, Jamieson DJ, Meaney-Delman DM. Preparing for biological threats: Addressing the needs of pregnant women. Birth Defects Res 2017;109:391–398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ellington S, Perez M, Morof D, et al. Addressing maternal health during CDC’s Ebola response in the United States. J Women’s Health 2017;26:1141–1145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Faherty LJ, Rasmussen SA, Lurie N. Planning for research on children during public health emergencies. Pediatrics 2016;137:e20153611. [DOI] [PubMed] [Google Scholar]
- 25.Disaster Preparedness Advisory Council, Committee on Emergency Medicine. Ensuring the health of children in disasters. Pediatrics 2015;136:e1407–e1417. [DOI] [PubMed] [Google Scholar]
- 26.Centers for Disease Control and Prevention. MMWR Zika Reports. 2021. Available at: https://www.cdc.gov/mmwr/zika_reports.html Accessed August 25, 2021.
- 27.National Center for Immunization and Respiratory Diseases Division of Viral Diseases. Clinical care information for COVID-19. 2021. Available at: https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care.html Accessed August 25, 2021.
- 28.Meaney-Delman D, Zotti ME, Rasmussen SA, et al. Anthrax cases in pregnant and postpartum women: A systematic review. Obstet Gynecol 2012;120:1439–1449. [DOI] [PubMed] [Google Scholar]
- 29.Meaney-Delman D, Rasmussen SA, Beigi RH, et al. Prophylaxis and treatment of anthrax in pregnant women: A systematic review of antibiotics. Obstet Gynecol 2013;122:885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Barfield WD, Krug SE, Kanter RK, et al. Neonatal and pediatric regionalized systems in pediatric emergency mass critical care. Pediatr Crit Care Med 2011;12(6 Suppl): S128–S134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Meaney-Delman D, Zotti ME, Creanga AA, et al. Special considerations for prophylaxis for and treatment of anthrax in pregnant and postpartum women. Emerg Infect Dis 2014;20:e130611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zotti ME, Williams AM. Reproductive health assessment after disaster: Introduction to the RHAD toolkit. J Women’s Health 2011;20:1123–1127. [DOI] [PubMed] [Google Scholar]
- 33.Arosemena FA, Fox L, Lichtveld MY. Reproductive health assessment after disasters: Embedding a toolkit within the disaster management workforce to address health inequalities among gulf-coast women. J Health Care Poor Under-served 2013;24:17–28. [DOI] [PubMed] [Google Scholar]
- 34.Association of Maternal and Child Health Programs. Reproductive Health Assessment After Disaster Toolkit (RHAD Toolkit). Sharing Best Practices in Maternal & Child Health. 2013. Available at: http://www.amchp.org/programsandtopics/BestPractices/InnovationStation/ISDocs/RHAD_2015.pdf [Google Scholar]
- 35.Lathrop E, Romero L, Hurst S, et al. The Zika Contraception Access Network: A feasibility programme to increase access to contraception in Puerto Rico during the 2016–2017 Zika virus outbreak. Lancet Public Health 2018;3:e91–e99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Powell R, Rosenthal J, August EM, et al. Ante La Duda, Pregunta: A social marketing campaign to improve contraceptive access during a public health emergency. Health Commun 2020:1–8. doi: 10.1080/10410236.2020.1828534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Council of State and Territorial Epidemiologists. Maternal and child health epidemiology and emergency preparedness and response: Capacity assessment and key informant interview analysis report. 2021. https://cdn.ymaws.com/www.cste.org/resource/resmgr/mch/MCHE_Report20_final.pdf
- 38.Association of Maternal and Child Health Programs. Public health emergency preparedness and response checklist for maternal and infant health during public health emergencies. 2019;2021. http://www.amchp.org/programsandtopics/WorkforceDevelopment/Documents/EPR%20ALC/DRAFT%20Preparedness%20Checklist%20of%20State%20Capabilities%20for%202019-20%20updated%2010-22-19.pdf
- 39.Division of Reproductive Health National Center for Chronic Disease Prevention and Health Promotion. Safety messages for pregnant, postpartum, and breastfeeding women during natural disasters and severe weather. Centers for Disease Control and Prevention. 2020. Available at: https://www.cdc.gov/reproductivehealth/emergency/safety-messages.htm Accessed August 25, 2021. [Google Scholar]
- 40.Promotion DoRHNCfCDPaH. Disaster safety for expecting and new parents. Centers for Disease Control and Prevention. 2021. Available at: https://www.cdc.gov/reproductivehealth/features/disaster-planning-parents/index.html Accessed August 25, 2021 [Google Scholar]
- 41.Zotti ME, Ellington SR, Perez M. CDC Online course: Reproductive health in emergency preparedness and response. J Women’s Health 2016;25:861–864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Galang RR, Chang K, Strid P, et al. Severe coronavirus infections in pregnancy: A systematic review. Obstet Gynecol 2020;136:262–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zambrano LD, Ellington S, Strid P, et al. Update: Characteristics of symptomatic women of reproductive age with laboratory-confirmed SARS-CoV-2 infection by pregnancy status—United States, January 22–October 3, 2020. MMWR Morb Mortal Wkly Rep 2020;69:1641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ellington S, Strid P, Tong VT, et al. Characteristics of women of reproductive age with laboratory-confirmed SARS-CoV-2 infection by pregnancy status—United States, January 22–June 7, 2020. MMWR Morbid Mortal Wkly Rep 2020;69:769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Woodworth KR, Olsen EO, Neelam V, et al. Birth and infant outcomes following laboratory-confirmed SARS-CoV-2 infection in pregnancy - SET-NET, 16 Jurisdictions, March 29–October 14, 2020. MMWR Morb Mortal Wkly Rep 2020;69:1635–1640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Delahoy MJ, Whitaker M, O’Halloran A, et al. Characteristics and maternal and birth outcomes of hospitalized pregnant women with laboratory-confirmed COVID-19—COVID-NET, 13 states, March 1–August 22, 2020. MMWR Morb Mortal Wkly Rep 2020;69:1347–1354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Division of Viral Diseases National Center for Immunizations and Respiratory Diseases. Investigating the impact of COVID-19 during pregnancy. Centers for Disease Control and Prevention. 2021. Available at: https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/special-populations/pregnancy-data-on-covid-19/what-cdc-is-doing.html Accessed March 10, 2021. [Google Scholar]


