Abstract
Background
Significant advances in managing congenital heart disease (CHD) have occurred over the past few decades, resulting in a fast-growing adult patient population with distinct needs requiring urgent attention. Research has recently highlighted the prevalence of neurocognitive differences among adults living with CHD. Yet, there is a lack of knowledge about the perspectives of people living with CHD and family members/caregivers on brain health. We sought to explore their perspectives to guide future research and clinical endeavours.
Methods
Using the principles of integrated knowledge translation and qualitative interpretive description, we conducted 2 focus groups with 7 individuals with CHD and their family members as part of a virtual forum on brain health in CHD. Data analysis followed the principles of interpretive description.
Results
A lack of understanding about overall brain health and neurocognitive differences in adult CHD was identified. To increase overall knowledge about brain health, initiatives should (1) focus on the individual living with CHD, involving family members and peers; (2) use social media and health care encounters for knowledge exchange; and (3) ensure a “balancing act” in the information provided to avoid feelings of worry and uncertainty about the future while simultaneously empowering people living with CHD.
Conclusions
There is a pressing need for better education about brain health among individuals living with CHD. Our findings can guide clinicians in developing programmes of care and (re)design health services that address the brain-heart axis and neurocognitive differences in CHD.
Résumé
Contexte
Des progrès significatifs ont été réalisés au cours des dernières décennies dans la prise en charge des cardiopathies congénitales, et il en résulte une croissance rapide de la population des patients adultes dont les besoins distincts requièrent une attention urgente. Des études récentes ont mis en évidence la prévalence des différences neurocognitives chez les adultes atteints de cardiopathies congénitales (CC). À ce jour, les connaissances sur les points de vue des personnes qui vivent avec la CC, des membres de leurs familles et de leurs aidants au sujet de la santé du cerveau sont insuffisantes. Notre objectif était d’explorer ces points de vue afin d’orienter les recherches à venir et les initiatives cliniques.
Méthodologie
En nous basant sur les approches d’application des connaissances intégrées et de description interprétative (DI) qualitative, nous avons organisé deux groupes de discussion avec 7 personnes atteintes de CC et les membres de leur famille, dans le cadre d’un forum virtuel sur la santé du cerveau dans les CC. L’analyse des données a été réalisée selon les principes de la DI.
Résultats
Un manque de connaissances au sujet de la santé du cerveau en général et des différences neurocognitives chez les personnes atteintes de CC a été observé. Afin d’améliorer le niveau des connaissances générales sur la santé du cerveau, les initiatives doivent : (1) être centrées sur les personnes qui vivent avec la CC, avec la participation des membres de leur famille et d’autres patients; (2) tirer profit des médias sociaux et des rencontres en contexte de soins de santé pour le partage de connaissances; et (3) veiller à maintenir un équilibre, puisqu’il convient d’outiller les personnes atteintes de CC sans toutefois causer de sentiment d’inquiétude ou d’incertitude quant à l’avenir.
Conclusions
Nous avons constaté le besoin urgent d’améliorer les connaissances des personnes qui vivent avec une CC au sujet de la santé du cerveau. Les résultats obtenus pourront guider les cliniciens dans l’élaboration de programmes de soins et la conception (ou la refonte) de services de soins de santé qui intègrent l’axe cerveau-cœur et les différences neurocognitives associées aux CC.
Over the last 2 decades, the prevalence of children with congenital heart disease (CHD) surviving into adulthood has increased by 63% due to improved survival in response to medical and surgical advancements.1 As a result, adults with CHD comprise a larger component of adult practice, creating an urgent need for the development of health services that meet lifelong care needs for these individuals. In Canada, increased numbers of hospitalizations of adults with CHD have mirrored similar trends across the world.2 This “demographic tsunami”3 of aging individuals with CHD has caused a paradigm shift among clinicians and researchers, who have recognized the personal, social, and economic implications for people living longer with CHD. Therefore, understanding the experiences of individuals living with CHD is paramount to developing specialized health services that meet the long-term care needs of this subpopulation and improve their quality of life.
Complications that develop in adult CHD (ACHD) related to brain health deserve special attention. Beyond cardiac issues, neurologic issues may begin in early life.4 Approximately 10% of those with CHD have a genetic syndrome that may include neurologic morbidity. In addition, dysmyelination and slower brain growth and development have been identified in neonates with critical CHD in the context of hypoxia and hypoperfusion in utero.4 Neurologic injury may be subsequently compounded by repeat surgeries and procedures in childhood. These issues, coupled with educational disruption related to hospitalizations as well as adverse social determinants of health more common in families affected by CHD, may impact neurocognition. Neurocognitive differences have been documented in children5 and cross-sectionally in adults with CHD.6,7 Further, health services research suggests that individuals living with CHD are at increased risk for early-onset dementia. However, mechanisms for these differences in later life are not well characterized. Atop the predisposition that may be conferred from early life insults, sit additional risks that may arise in later life. In adulthood, people with CHD are at higher risk of stroke (a well-defined risk factor for cognitive decline and dementia in other groups8) than age-matched peers without CHD.9, 10, 11, 12, 13, 14, 15 Other known risk factors for cognitive decline such as depression, impaired glucose tolerance or diabetes, hypertension, and low educational attainment are also present in people with CHD.16 Given the risk for neurocognitive differences in individuals living with CHD, and the additional threats to brain health due to stroke, and vascular and social risk factors, educational and preventative strategies aimed at preserving brain health are a priority.
Despite an increase in the number of individuals living with CHD and the risk of neurocognitive differences in these individuals, systems and processes of care have been slow to adapt to these changes and patients lack specific counselling related to the awareness of brain health and preventative strategies.17 In Canada, some provinces have lacked overall clear processes of care for ACHD.18 In addition, persons living with CHD do not receive routine cognitive assessments or neurologic evaluations.4 Although it has been argued that there is a need for resources focusing on risk assessment and treatment for adults with CHD who have neurocognitive impairment,19 the patient and caregiver perspectives have not been explored in detail. It is not known what persons with ACHD and their family members know about neurocognitive decline, the overall brain-heart connection, what resources may be needed, and how information should be delivered.
An improved understanding of the gaps in knowledge about the brain-heart connection, including neurocognition, among people living with CHD can inform practice and clarify areas for health care service improvement. Therefore, in this study, we initially sought to identify gaps in knowledge associated with brain health in ACHD through facilitated discussions with individuals living with CHD and their family members. However, during data analysis, we identified a lack of general awareness and familiarity from participants regarding brain health and neurocognitive differences in CHD. Thus, the research question focused instead on what could be learned from people living with CHD to inform future initiatives that improve knowledge about brain health in CHD. Our results have the potential to answer some of the research priorities identified for ACHD,5,20 to help clinicians develop programmes of care for ACHD that address the brain-heart axis and neurocognition, and to (re)design health services for people living with CHD. The manuscript writing was guided by the COREQ21 checklist for reporting qualitative research.
Methods
Approach and design
We used the principles of integrated knowledge translation (IKT) and qualitative interpretive description (ID) to guide this study. IKT is an umbrella term used in approaches to research projects centred on active collaboration between researchers and knowledge partners (ie, researchers, policy makers, clinicians, organizations, people with lived or living experience, and family members/caregivers).22,23 Within health research, IKT or other cocreation approaches have been widely used24, 25, 26, 27, 28 and can ensure a more fulsome implementation of the research findings.24,29 Combined with IKT, we used ID, an analytic, inductive, qualitative research methodology for developing knowledge that informs practice in the applied disciplines in a new meaningful way, going beyond what was already known.30, 31, 32, 33, 34 Consequently, this knowledge augments health services design and interventions that consider the unique needs of individuals.
Setting
An advisory committee was established in 2020 with a diverse and representative group of knowledge partners (Fig. 1). Health care professionals (HCPs) had between 6 and 22 years of experience, with 2 of the HCPs with a clinical practice focused specifically on CHD. The advisory committee created a space for 2-way communication between the researchers and those who would benefit from the research results,35 and bidirectional engagement directly benefitted and shaped the research design.36 Members of the advisory committee with living experience of CHD received compensation for their time.
Figure 1.
Advisory committee.
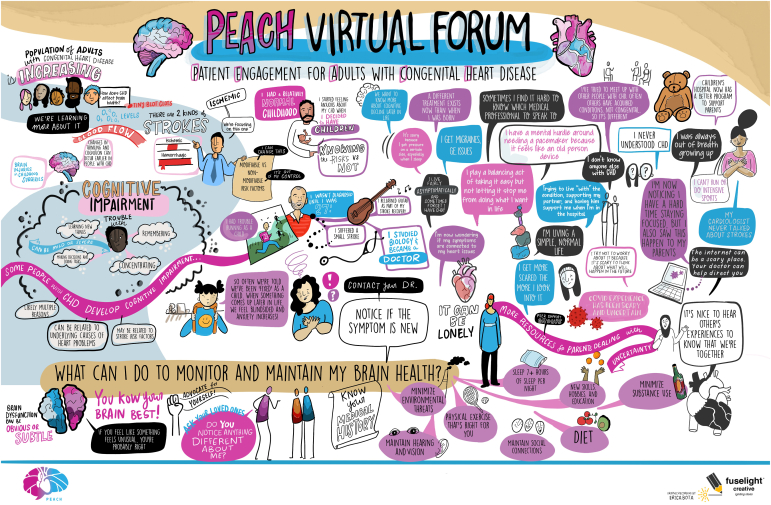
A 3-hour virtual forum planned and led by the advisory committee was held in September 2021 over Zoom to ensure the safety of the research team and participants during the COVID-19 pandemic and increase access to people with living experience (PWLE) of CHD across British Columbia. The virtual forum included 1 breakout room session that acted as a focus group (Table 1). Due to the nature of the topics explored and the potential for psychological distress, we created an additional breakout room to act as “quiet rooms” for participants and for a research team member to support those experiencing psychological distress. A graphic artist created an illustration of the virtual forum (Fig. 2), which was considered a secondary data source.
Table 1.
PEACH virtual forum agenda
| 09:00 AM | Introductions and icebreakers |
| 09:10 AM | Overview of brain health and congenital heart disease |
| 09:25 AM | Patient partner living experience |
| 09:40 AM | Break |
| 10:00 AM | Breakout rooms/focus groups |
| 11:00 AM | Discussion debrief |
| 11:15 AM | Break |
| 11:30 AM | Brain health and prevention Frequently asked questions |
| 11:45 AM | Wrap-up/closing |
Figure 2.
Graphic recording.
Sampling and recruitment
After approval by the Clinical Research Ethics Board, we used purposive sampling to recruit people between 18 and 49 years old diagnosed with moderate-to-severe CHD and fluent in English to attend the virtual forum and participate in the breakout session/focus group. Caregivers/family members of people living with CHD were also invited. A poster disseminated through the Yasmin & Amir Virani Provincial Adult Congenital Heart (VPACH) programme Facebook group was used to invite people living with CHD to participate in the virtual forum. Invitations were also disseminated to patients and families through the Canadian Congenital Heart Alliance website and listserv email. A purposive sample of participants already enrolled in the SEARCH (StrokE and vAscular Risk factors contributing to neuroCognitive decline in adult congenital Heart disease) study, a longitudinal study examining cognition and neuroimaging in adults with moderate-severe complexity CHD, were also invited to participate in the virtual forum. Consent was sought electronically. Forum participants were offered a CAD$100 gift card thanking them for their time.
Data collection
Participants attending the virtual forum were allocated randomly to a Zoom breakout room/focus group by the research team. Given the number of participants, we held 2 separate breakout rooms/focus groups. Data were collected during these breakout room sessions/focus groups. A semistructured interview guide (Supplemental Data) was cocreated by members of the advisory committee during the planning phase of the virtual forum. We used the term “cognitive impairment” during the virtual forum and breakout room/focus groups with participants to refer to “trouble with remembering, learning new things, concentrating, making decisions or carrying out tasks in everyday life; cognitive impairment can be anywhere from mild to very severe.” Two members of the advisory committee with CHD (AC and YEK) led the breakout room/focus groups. Both had discussed their stories of living with CHD in the first part of the virtual forum, and therefore, participants could be more open to sharing their experiences. Our intent with this approach was also to reduce existing power differentials between researchers and participants, in line with the principles of IKT. Two clinicians (JMCS and EMEL) supported the interviewers in each breakout room/focus group, and a brief primer by the investigator with experience in qualitative research methodology was provided before data collection. Two research staff members (MS and RHP) observed the breakout rooms/focus groups and acted as note-takers, developing a summary of the main points discussed. Breakout rooms/focus groups, lasted approximately 60 minutes, were audio-recorded and transcribed. Transcripts were deidentified and anonymized, with each participant given a code. A research team member (IDS) reviewed the transcripts for accuracy before uploading them to NVivo (released in March 2020) for analysis.
Data analysis
The first author (IDS), with knowledge and skills in qualitative research, was responsible for data analysis. Her background was in stroke care; therefore, she had no prior relationship with participants. Guided by the principles of ID and the study’s objectives, a set of questions was developed to facilitate the iterative data analysis. The investigator read each transcript to deconstruct the data and began an in-depth, inductive analysis using broad-based inductive coding. Subsequently, each broad-based coding was analysed, and constant comparison methods were used to identify patterns, similarities, and differences within and across the 2 focus groups. This process resulted in new codes and others being refined. The investigator then read the notes developed by the 2 research staff members who observed the focus groups and analysed the graphic recording (Fig. 2) in order to triangulate and generate new perspectives on the data. During data analysis, it became clear that the research question we sought to answer about the knowledge gaps related to brain health among people living with CHD could not be derived from this study due to a prior lack of awareness from participants that such connection existed. Thus, we explored what we could learn from individuals living with CHD to inform initiatives about brain health in CHD that could improve knowledge about brain health in this subpopulation.
After revising the research question, codes were revisited, themes were developed, and a narrative account using a higher level of interpretation that could be meaningful for practice was constructed. The advisory committee discussed the themes and narrative account during a group meeting, ensuring that the findings were representative of participants’ experiences. Findings were disseminated to cardiologists and the nursing team from the VPACH programme to gather meaningful input. This triangulation of perspectives confirmed that this was an important and underexplored topic in CHD, thus enhancing the trustworthiness of the analysis. Reflexivity was maintained throughout the analysis through a reflexive diary capturing impressions and thoughts about the data and how the researcher’s values and beliefs influenced the analysis.
Results
A total of 7 participants attended the virtual forum, including 1 family member, and participated in the breakout rooms/focus groups. The only family member present, a parent, attended the same focus group as their adult child. Most participants had English as their first language and lived primarily in urban areas in British Columbia. Although the sample size was appropriate given the philosophies of inquiry that underpin qualitative research, risks to participants’ anonymity could occur, which preclude sharing demographic characteristics.
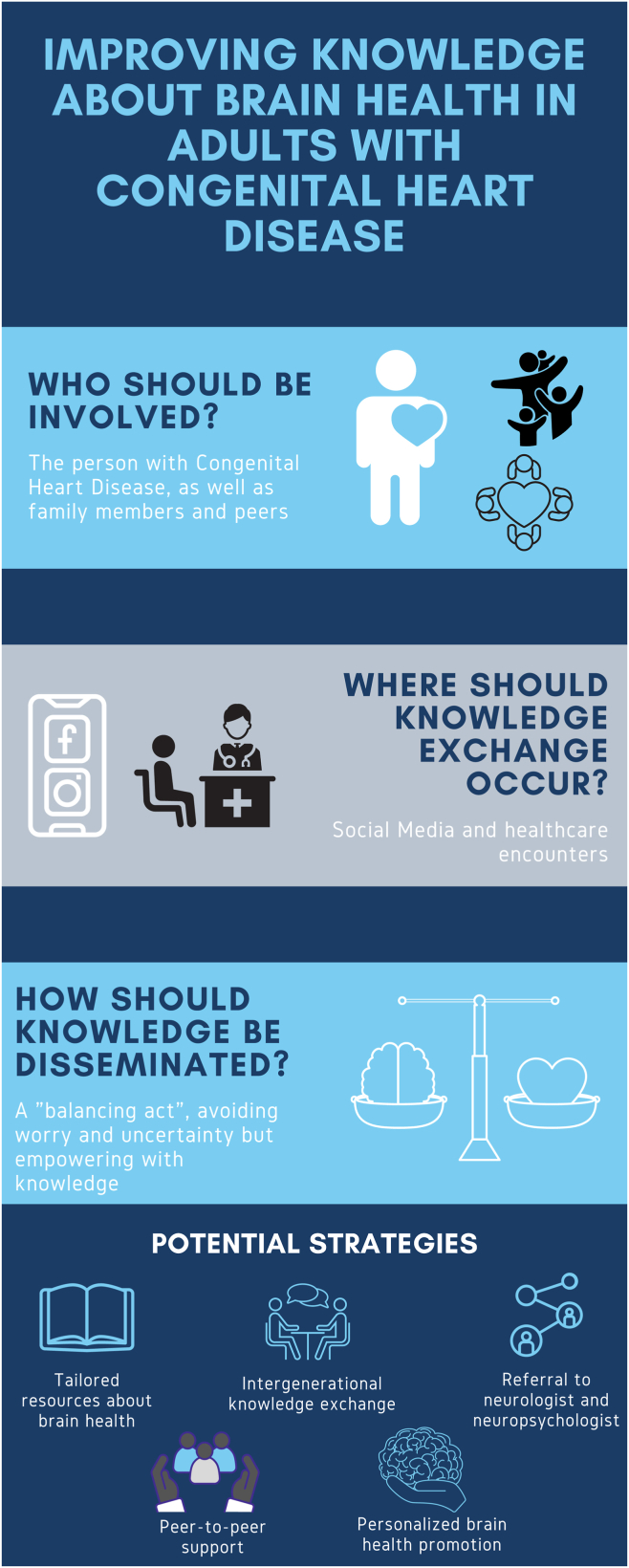
A key theme in our findings was the lack of understanding about overall brain health and neurocognitive differences in CHD, an area most identified as not explored during health care encounters. This contrasted with sound knowledge of adults living with CHD about their congenital heart lesion type and diagnosis. “We have dealt with so much. There’s more coming?” accurately represents participants’ reports of a lifetime’s experience of concerns related to their health and uncertainty about the future, and thus, the idea of facing further adversities was difficult to overcome. In fact, for some participants, the virtual forum was the first time they were made aware of the connection between the brain and heart and a motivating factor for attending the event. As a result of the lack of knowledge about overall brain health in CHD and to offer findings that can be applied to practice, our analysis identifies who should be involved in knowledge translation (KT) initiatives about brain health in ACHD, where KT initiatives should occur and how (Fig. 3). Our findings revealed that KT initiatives should (1) focus on the person living with CHD, involving family members and peers (who); (2) use social media and health care encounters for knowledge exchange (where); and (3) be a “balancing act” between avoiding feelings of worry about the future’s uncertainty and empowering people living with CHD (how).
Figure 3.
Summary of key findings and potential strategies to improve knowledge about brain health in adult congenital heart disease.
Focusing on the person living with CHD but involving family members and peers
Individuals living with CHD recognized themselves as the main driver in seeking knowledge about CHD, whereas family members and peers were part of their support system. When confronted with questions about their condition, participants relied significantly on their own efforts to find answers. As one participant depicted: “You have to seek it out if you’re interested. Or if you’re not interested, you just kind of bury your head in the sand and just pretend like everything’s good” (participant C). The overall lack of resources for people living with CHD was one of the factors behind the belief that they had to rely on themselves. Being proactive about seeking further information also meant that people living with CHD sometimes initiated discussions about specific topics with their care provider.
Family members, especially parents, were important sources of knowledge for individuals with CHD during childhood. As a result, our participants could recount, in detail, the conditions of their childhood diagnosis, the succession of events, and any other medical events related to their condition. However, during adulthood, parents did not hold such a prominent role for individuals living with CHD. For some, other family members, such as partners, have taken up a continued supporting role instead. This change in supporting roles between childhood and adulthood might explain the presence of only 1 parent during the virtual forum. As one participant asked us: “How can I still be supportive of my husband while he’s being supportive of me in the hospital, or things like that?” (participant D). Partners also seemed to have a prominent role in identifying subtle cognitive differences that persons living with CHD might not have recognized immediately or had ignored.
Peers with CHD played an important role for people living with CHD. Given the heterogeneous nature of CHD and the need for individual treatment and management approaches, loneliness during childhood was common among participants. However, these feelings were also carried forward into adulthood. As a result, adults with CHD sought to connect with others living with CHD, whom they recognized as fundamental sources of knowledge throughout their patient journey. Those who had found that a community of peers with CHD welcomed the ability to share resources talk about shared experiences or other ways of socializing: “We have the VPACH group where some people do ask for advice, or you can talk to other people... Through the VPACH clinic, there is actually a group of us that have met up a couple of times just for coffee. And so that has been really nice to talk about common experiences” (participant C). Although it was difficult for some participants to find people with similar symptoms due to the heterogeneity of congenital heart lesions, these encounters with others living with CHD triggered, at times, changes in how participants viewed themselves and their diagnosis. As one participant stated, “As a child, you figure that you’re the only one. But you’re not” (participant I).
Surprisingly, an essential facet of peer-to-peer support was intergenerational learning. Participants highlighted the importance of learning from the experiences of older adults with CHD, mainly that “it gave [them] comfort to know that people in their 70s [had] survived” (participant I). Intergenerational peer-to-peer learning was also evident when one participant proposed that a connection between adults living with CHD and children with CHD should be created, as this would bring benefits for parents: “making some sort of connection where we could go into the children’s hospital or Zoom with parents and answer some of their questions and say to parents ‘look, I grew up on a farm and I rode horses and I snowboarded and I’ve seen and done all these things. You don’t have to keep your kids in a bubble.’ Just having that conversation with parents, I think, would be really helpful” (participant D).
When confronted with uncertainties or questions about CHD, persons living with CHD proactively sought resources and information about their condition. They relied on family members, such as partners and other individuals living with CHD, as sources of knowledge and support. The connection with peers via existing community groups and intergenerationally offered a shared learning opportunity.
Using social media and health care encounters
Persons living with CHD sought knowledge in social media and during health care encounters. Social media was an important place where our participants learned about CHD and connected with peers, particularly those with similar conditions. Some participants told us about existing local and international Facebook groups for people with CHD and other gender-specific groups. One participant described connecting via one of these groups: “I found those Facebook groups and I connected with a lady with the same defect in Australia. And we’ve been messaging, but she’s not local, of course, so I can’t just visit. But it’s still fun to talk to her and see her experience” (participant D). The same participant highlighted the need for more group platforms, which is unsurprising considering that peer-to-peer connection was a source of knowledge identified during our data analysis for some people living with CHD.
Health care encounters also represented an optimal way to disseminate knowledge. All participants described having at least yearly contact with an HCP (a cardiologist, family physician, or nurse practitioner). Few reported seeing a neurologist. For participants, seeing different HCPs and specialists was common and often highlighted as problematic because of the disjointed care experienced with health care providers who often had differing opinions and approaches to care. Yet, there was no consensus on which HCPs could best disseminate knowledge regarding brain-heart health. In fact, some participants felt that the responsibility should be shared among the health care team and disseminated by the health care provider whom individuals living with CHD see most frequently. For example, the only parent who attended our virtual forum said: “I would like [my daughter’s] GP to be aware of the special risk factors to be watching in her. She sees [the GP] much more often than the VPACH clinic. The VPACH clinic sees her once every two years or so. So I would like, I would feel better if I had confidence that there was information being shared between the cardiologist and the GP” (participant F). In contrast, other persons living with CHD preferred to receive new knowledge about the brain-heart connection at each appointment with an HCP with expertise in the area and able to direct them to further resources: “I feel I also would like to hear from my cardiologist. Having a discussion with cardiologists like ‘this is all the risk factors that you have’ could be overwhelming. But at some point, having it shared that there are these risk factors maybe at each appointment you have with the cardiologist, like one new risk factor comes up or something. I think also personally, I would like to hear from a cardiologist and being given the resources or direction on where to do the research, do a little bit of research on my own” (participant G).
When faced with questions or lack of knowledge about their condition, people living with CHD have sought responses in social media groups. However, they still recognized the importance of acquiring knowledge during their health care encounters, even when these were less frequent.
A “balancing act”: Avoiding worry and uncertainty but empowering with knowledge
Participants noted that information about brain and heart health should be a “balancing act” between avoiding feelings of worry about the future’s uncertainty and empowering persons living with CHD. This dichotomy was characteristic of our participants’ approach to living with CHD. On the one hand, adults living with CHD reported an attitude of “just living with it,” avoiding remembering what it means to live with CHD or even, at times, forgetting their diagnosis. As one participant told us: “to be honest, I forget about it until I get the message: ‘it’s time for your checkup’ at the VPACH clinic. I just forget about it in my case” (participant B). As a result of this approach to living with CHD, participants expressed uncertainty about wanting to know what to expect in the future. Avoiding this information could prevent any worrisome feelings triggered by being unexpectedly told about future problems when, in the past, adults living with CHD had been told their condition had been “fixed.”
On the other hand, people living with CHD also recognized the need to empower people living with CHD with knowledge about the brain-heart connection: “I think it’s a fine line between being overwhelmed with the information and worried about the future, compared to being educated and empowered. Ok, I have the information, I have options, things may or may not happen” (participant C). For some participants, learning that there were still uncertainties about developing neurocognitive differences in the future offered some reassurance.
Therefore, knowledge transmitted to people living with CHD about brain-heart health should strike a balance between providing information that offers foundational knowledge about brain-heart health while avoiding triggering feelings of worry and overwhelmedness.
Discussion
The value of KT and partnerships between researchers and PWLE to optimize health outcomes and improve health services in cardiovascular disease has been discussed recently.37 Centring the voices of adults with CHD throughout the study, our findings offer considerations to clinicians for developing ACHD programmes and health services (re)design that address the brain-heart axis (Fig. 3). Specifically, KT initiatives to improve knowledge about brain health should (1) focus on the person living with CHD, including their families and peers; (2) be disseminated via social media and all health care encounters; and (3) be offered in a way that avoids worry among adults with CHD while simultaneously empowering them.
Our study identified that participants were not well informed about the brain-heart connection and neurocognitive differences. This lack of knowledge was a motivating factor for attending the virtual forum and demonstrated that adults living with CHD often seek information about their condition when it is not readily available, a point consistent with the literature.38 Therefore, appropriate and tailored resources for adults living with CHD that target the individual with the condition and ensure a good balance between empowering with information and minimizing worry about the future are needed. Such resources should also seek to inform family members and peers, whom our findings identified as support systems for adults with CHD. The vital role of family members and peers in the patient trajectory of those living with CHD is consistent with previous studies on the psychological impact of living with CHD.38 Similar to children with CHD, adults with CHD continue to see their family members as a good source of support. However, family members’ roles might change during adulthood. For instance, in children with CHD, parents have a much more prominent role in the child’s life, whereas in adulthood, they assume the role of a spectator.39 Our findings supported this and suggested that other family members, such as partners, may be a substitute for the parents and play a more active role, including identifying subtle neurocognitive differences that may not be evident for adults with CHD. Exploring the role that partners play in the lives of adults with CHD may highlight further considerations for KT initiatives in brain-heart health.
Peers with CHD were also identified as necessary anchors for adults living with CHD. Support from others with living experience of CHD allows adults living with CHD to seek advice, share resources, and discuss their experiences. In particular, the value of intergenerational knowledge exchange, where participants were encouraged and informed by the health span and longevity of older peers living with CHD, was highlighted. Peer-to-peer support and opportunities for adults with CHD to connect are of value and should be available in specialized CHD centres, as well as virtually for those living more remotely. Our participants illuminated strategies for optimizing peer support, such as opportunities for interpersonal connection through intergenerational learning among adults living with CHD, as well as for children living with CHD and their parents. These might also be appropriate strategies for disseminating information about the connection between the brain and heart. Parents of children living with CHD face uncertainties around their child’s future, sometimes alongside overwhelming negative feelings and thoughts that can hinder parents’ ability to come to terms with their child’s diagnosis.40 Thus, an intergenerational knowledge exchange programme has the potential to offer parents the opportunity to gain knowledge and advice about practical tips, emotional support, and a sense of connectedness, as well as sharing information about preventative measures for brain-heart health. This uncertainty about one’s future health can extend into adulthood.38 Therefore, for younger individuals, the opportunities for intergenerational learning with middle and older adults living with CHD who have had similar journeys might offer a sense of hope and reassurance about health span, lifespan, and quality of life.
Health care encounters were also identified as a key pathway to transmit knowledge about brain-heart health and neurocognitive differences to adults living with CHD and their families. Although there was no consensus on the most appropriate health care provider to offer information about brain-heart health and neurocognition, we recognize that being prescriptive about who is best positioned to carry responsibilities ignores the nuances differentiating health care systems, and patients’ specific circumstances. For instance, living in rural areas in British Columbia, the family physician or nurse practitioner may be the first point of contact and whom they see most often. The same may not apply in urban areas closer to specialized CHD centres where a cardiologist follows adults living with CHD with complex needs. Specialized ACHD centres should ensure that appropriate educational resources and care pathways for people living with CHD with neurocognitive differences are disseminated and tailored for use in primary care.
Given, however, that risk factor management may help to prevent neurocognitive decline,16 preventative strategies may be optimized by providing personalized health promotion interventions for nurse-led ACHD care. Specialist nurses, registered nurses (RNs), and advanced practice nurses (APNs) are in an optimal position to advise adults with CHD on risk factor prevention, assessment, and potential referral to clinicians with expertise in neurorehabilitation. The scope of practice of RNs and APNs specialized in CHD can encompass assessing learning needs, readiness for and barriers to learning, and developing and implementing individualized teaching plans. Moreover, RNs and APNs may already support adults with CHD, coordinating and managing their care.41 As a result, brain health and neurocognition could be included as a discussion point, respecting the decision-making capacity of individuals about the level and depth of information about brain-heart health and neurocognitive differences. This can offer an appropriate balance of information without increasing fear and uncertainty about the future. Implementing these processes of care would address the lack of knowledge about neurocognitive differences and optimize brain health. Furthermore, it could tackle the lack of structured education available for adults with CHD42 in some settings.
Prevention and management of neurocognitive differences could also be strengthened during health care encounters with cardiologists and in primary care.3 Recognizing the implications of cognitive impairment on the quality of life of adults living with CHD and the need for referrals to specialists,19 clinicians could develop rapid guides to aid in screening for neurocognitive differences in people living with CHD17 and subsequent referral to neurologists and neuropsychologists, who at present are not part of specialized ACHD teams.17,43 Developing close partnerships with clinicians with expertise in neurology and neurocognition as core elements of the multidisciplinary team will be key in developing integrated systems and pathways that routinely address brain health as part of CHD care.
Social media emerged as an essential route for providing information about brain-heart health to people living with CHD. Participants found that Facebook groups offered peer connection and learning opportunities about CHD through sharing experiences. In a study by Jacobs et al,44 Facebook groups related to congenital anomalies, including CHD, were identified as essential for PWLE to understand their condition, make friends, and receive advice and recommendations about day-to-day management, medications, treatments, research, and emotional support. The same study noted that most PWLE of congenital defects wanted HCPs, particularly specialist nurses, to interact with them online.44 Therefore, leveraging social media groups for KT initiatives about brain health among adults living with CHD is crucial, including disseminating information about neurocognitive differences, prevention, and management. By bringing awareness to brain health and neurocognition in these social groups, there is a benefit of mutual and reciprocal learning between HCPs and PWLE, and among PWLE. Moreover, although not mentioned by participants in our study, we recognize the role of patient advocacy websites, such as the Canadian Congenital Heart Alliance, and the possible opportunities to develop and implement resources about brain-heart health, neurocognitive differences, prevention, and management that can be accessible by all.
Limitations
Study limitations should be considered when interpreting our findings. Participants in our study were mostly young and middle-aged adults living primarily in urban areas in British Columbia, who spoke English as their first language. Thus, their experiences may not reflect the experiences of other individuals living with CHD living in rural areas or other provinces. In addition, we did not consider the implications for KT among adults with CHD from different racial/ethnic, sex, gender, and socioeconomic axes. A wide variation in participant demographics with attention to their intersecting experiences could provide further insights into KT initiatives on brain health and neurocognition in people living with CHD and remains a priority for future work.
Conclusion
This study identified a need for better education about brain health among people with ACHD. The findings point out that initiatives to improve brain health in people living with CHD should (1) focus on the person living with CHD, involving family members and peers; (2) use both social media and health care encounters for knowledge exchange; and (3) ensure a “balancing act” in the information provided to avoid feelings of worry and uncertainty about the future while simultaneously empowering people living with CHD. Also emerging was the need for opportunities for intergenerational learning between individuals with CHD. Our findings can guide clinicians in developing programmes of care for ACHD and (re)design health services that address the brain-heart axis and neurocognitive differences informed by the perspectives of individuals with ACHD.
Acknowledgements
We would like to thank our participants for their engagement in the forum and the VPACH programme for their ongoing support. We also extend our thanks to Mina Shahsavar, one of our patient partners, and the staff from Fuselight who helped facilitate the virtual forum.
Ethics Statement
This study was conducted after approval by the Clinical Research Ethics Board at the University of British Columbia.
Patient Consent
The authors confirm that a patient consent form(s) has been obtained for this article.
Funding Sources
This work was supported by the Vancouver Coastal Health Research Institute Patient-Oriented Research Award (VCH POR—F19-05501) and Heart and Stroke Foundation Grant-in-Aid (HSF GIA—G-19-0026367).
Disclosures
The authors have no conflicts of interest to disclose.
Footnotes
To access the supplementary material accompanying this article, visit CJC Pediatric and Congenital Heart Disease at https://www.cjcpc.ca// and at https://doi.org/10.1016/j.cjcpc.2023.10.010
Supplementary Material
References
- 1.Smith J.M.C., Andrade J.G., Human D., Field T.S. Adults with complex congenital heart disease: cerebrovascular considerations for the neurologist. Front Neurol. 2019;10:329. doi: 10.3389/fneur.2019.00329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Islam S., Yasui Y., Kaul P., Marelli A.J., Mackie A.S. Congenital heart disease hospitalizations in Canada: a 10-year experience. Can J Cardiol. 2016;32:197–203. doi: 10.1016/j.cjca.2015.05.022. [DOI] [PubMed] [Google Scholar]
- 3.Lapum J.L., Fredericks S., Bailey B., et al. Historical investigation of medical treatment for adult congenital heart disease: a Canadian perspective. Congenit Heart Dis. 2019;14:185–192. doi: 10.1111/chd.12716. [DOI] [PubMed] [Google Scholar]
- 4.Selvanathan T., Smith J.M.C., Miller S.P., Field T.S. Neurodevelopment and cognition across the lifespan in patients with single-ventricle physiology: abnormal brain maturation and accumulation of brain injuries. Can J Cardiol. 2022;38:977–987. doi: 10.1016/j.cjca.2022.02.009. [DOI] [PubMed] [Google Scholar]
- 5.Gurvitz M., Burns K.M., Brindis R., et al. Emerging research directions in adult congenital heart disease: a report from an NHLBI/ACHA working group. J Am Coll Cardiol. 2016;67:1956–1964. doi: 10.1016/j.jacc.2016.01.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Perrotta M.L., Saha P., Zawadzki R., et al. Adults with mild-to-moderate congenital heart disease demonstrate measurable neurocognitive deficits. J Am Heart Assoc. 2020;9 doi: 10.1161/JAHA.119.015379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Verrall C.E., Yang J.Y.M., Chen J., et al. Neurocognitive dysfunction and smaller brain volumes in adolescents and adults with a Fontan circulation. Circulation. 2021;143:878–891. doi: 10.1161/CIRCULATIONAHA.120.048202. [DOI] [PubMed] [Google Scholar]
- 8.Kalaria R.N., Akinyemi R., Ihara M. Stroke injury, cognitive impairment and vascular dementia. Biochim Biophys Acta. 2016;1862:915–925. doi: 10.1016/j.bbadis.2016.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Castro L.A., Shah A.H., Hiebert B., Tam J.W., Ducas R.A. Population and resource utilization among patients with adult congenital heart disease: a snapshot view of a moderate-size Canadian regional centre. CJC Open. 2021;3:1132–1138. doi: 10.1016/j.cjco.2021.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fedchenko M., Mandalenakis Z., Rosengren A., et al. Ischemic heart disease in children and young adults with congenital heart disease in Sweden. Int J Cardiol. 2017;248:143–148. doi: 10.1016/j.ijcard.2017.06.120. [DOI] [PubMed] [Google Scholar]
- 11.Lanz J., Brophy J.M., Therrien J., et al. Stroke in adults with congenital heart disease: incidence, cumulative risk, and predictors. Circulation. 2015;132:2385–2394. doi: 10.1161/CIRCULATIONAHA.115.011241. [DOI] [PubMed] [Google Scholar]
- 12.Rehan R., Kotchetkova I., Cordina R., Celermajer D. Adult congenital heart disease survivors at age 50 years: medical and psychosocial status. Heart Lung Circ. 2021;30:261–266. doi: 10.1016/j.hlc.2020.05.114. [DOI] [PubMed] [Google Scholar]
- 13.Giang K.W., Fedchenko M., Dellborg M., Eriksson P., Mandalenakis Z. Burden of ischemic stroke in patients with congenital heart disease: a nationwide, case-control study. J Am Heart Assoc. 2021;10 doi: 10.1161/JAHA.120.020939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pedersen M.G.B., Olsen M.S., Schmidt M., et al. Ischemic stroke in adults with congenital heart disease: a population-based cohort study. J Am Heart Assoc. 2019;8 doi: 10.1161/JAHA.118.011870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pickard S.S., Gauvreau K., Gurvitz M., et al. Stroke in adults with coarctation of the aorta: a national population-based study. J Am Heart Assoc. 2018;7 doi: 10.1161/JAHA.118.009072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Keir M., Ebert P., Kovacs A.H., et al. Neurocognition in adult congenital heart disease: how to monitor and prevent progressive decline. Can J Cardiol. 2019;35:1675–1685. doi: 10.1016/j.cjca.2019.06.020. [DOI] [PubMed] [Google Scholar]
- 17.Stout K.K., Daniels C.J., Aboulhosn J.A., et al. 2018 AHA/ACC guideline for the management of adults with congenital heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;139:e698–800. doi: 10.1161/CIR.0000000000000603. [DOI] [PubMed] [Google Scholar]
- 18.Keir M., Penner M., Dehghani P., et al. Barriers to care in ACHD: a study of young adults in Saskatchewan. CJC Open. 2020;2:439–446. doi: 10.1016/j.cjco.2020.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ilardi D., Ono K.E., McCartney R., Book W., Stringer A.Y. Neurocognitive functioning in adults with congenital heart disease. Congenit Heart Dis. 2017;12:166–173. doi: 10.1111/chd.12434. [DOI] [PubMed] [Google Scholar]
- 20.Goossens E., Fleck D., Canobbio M.M., Harrison J.L., Moons P. Development of an international research agenda for adult congenital heart disease nursing. Eur J Cardiovasc Nurs. 2013;12:7–16. doi: 10.1016/j.ejcnurse.2011.06.009. [DOI] [PubMed] [Google Scholar]
- 21.Tong A., Sainsbury P., Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19:349–357. doi: 10.1093/intqhc/mzm042. [DOI] [PubMed] [Google Scholar]
- 22.Kothari A., Wathen C.N. A critical second look at integrated knowledge translation. Health Policy. 2012;109:187–191. doi: 10.1016/j.healthpol.2012.11.004. [DOI] [PubMed] [Google Scholar]
- 23.Jull J., Giles A., Graham I.D. Community-based participatory research and integrated knowledge translation: advancing the co-creation of knowledge. Implement Sci. 2017;12:150. doi: 10.1186/s13012-017-0696-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cassidy C.E., Shin H.D., Ramage E., et al. Trainee-led research using an integrated knowledge translation or other research partnership approaches: a scoping reviews. Health Res Policy Syst. 2021;19:135. doi: 10.1186/s12961-021-00784-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jenkins E.K., Kothari A., Bungay V., Johnson J.L., Oliffe J.L. Strengthening population health interventions: developing the CollaboraKTion Framework for Community-Based Knowledge Translation. Health Res Policy Sys. 2016;14:65. doi: 10.1186/s12961-016-0138-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kitson A., Powell K., Hoon E., et al. Knowledge translation within a population health study: how do you do it? Implement Sci. 2013;8:54. doi: 10.1186/1748-5908-8-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Baumbusch J.L., Kirkham S.R., Khan K.B., et al. Pursuing common agendas: a collaborative model for knowledge translation between research and practice in clinical settings. Res Nurs Health. 2008;31:130–140. doi: 10.1002/nur.20242. [DOI] [PubMed] [Google Scholar]
- 28.Cluley V. Using photovoice to include people with profound and multiple learning disabilities in inclusive research. Br J Learn Disabil. 2016;45:39–46. [Google Scholar]
- 29.Gagliardi A.R., Berta W., Kothari A., Boyko J., Urquhart R. Integrated knowledge translation (IKT) in health care: a scoping review. Implement Sci. 2016;11:38. doi: 10.1186/s13012-016-0399-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Thorne S. 2nd ed. Routledge; New York: 2016. Interpretive Description. [Google Scholar]
- 31.Thorne S., Reimer-Kirkham S., MacDonald-Emes J. Interpretive description: a noncategorical qualitative alternative for developing nursing knowledge. Res Nurs Health. 1997;20:169–177. doi: 10.1002/(sici)1098-240x(199704)20:2<169::aid-nur9>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 32.Thorne S., Reimer-Kirkham S., O’Flynn-Magee K. The analytic challenge in interpretive description. Int J Qual Methods. 2004;3:1–11. [Google Scholar]
- 33.Thorne S. In: Routledge International Handbook of Qualitative Nursing Research. Beck C.T., editor. Taylor & Francis; New York: 2013. Interpretive description; pp. 295–306. [Google Scholar]
- 34.Thorne S. In: The Oxford Handbook of Qualitative Research. Leavy P., editor. Oxford University Press; 2014. Applied interpretive approaches. [Google Scholar]
- 35.Sharma A., Angel L., Bui Q. Patient advisory councils: giving patients a seat at the table. Fam Pract Manag. 2015;22:22–27. [PubMed] [Google Scholar]
- 36.Young K., Kaminstein D., Olivos A., et al. Patient involvement in medical research: what patients and physicians learn from each other. Orphanet J Rare Dis. 2019;14:21. doi: 10.1186/s13023-018-0969-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lauck SB, Saarijärvi M, De Sousa I, et al. Accelerating knowledge translation to improve cardiovascular outcomes and health services: opportunities for bridging science and clinical practice. Eur J Cardiovasc Nurs. 2023 doi: 10.1093/eurjcn/zvad077. https://doi.org/10.1093/eurjcn/zvad077 [e-pub ahead of print] [DOI] [PubMed] [Google Scholar]
- 38.Cornett L., Simms J. At the ‘heart’ of the matter: an exploration of the psychological impact of living with congenital heart disease in adulthood. J Health Psychol. 2014;19:393–406. doi: 10.1177/1359105312471569. [DOI] [PubMed] [Google Scholar]
- 39.de Hosson M., Goossens P.J.J., De Backer J., De Wolf D., Van Hecke A. Needs and experiences of adolescents with congenital heart disease and parents in the transitional process: a qualitative study. J Pediatr Nurs. 2021;61:90–95. doi: 10.1016/j.pedn.2021.03.016. [DOI] [PubMed] [Google Scholar]
- 40.Williams T.S., McDonald K.P., Roberts S.D., et al. From diagnoses to ongoing journey: parent experiences following congenital heart disease diagnoses. J Pediatr Psychol. 2019;44:924–936. doi: 10.1093/jpepsy/jsz055. [DOI] [PubMed] [Google Scholar]
- 41.Simpson M., Weingart E., Lewis J., et al. The role of the nurse in adult congenital heart disease: past, present and future. Br J Card Nurs. 2022;17:1–10. [Google Scholar]
- 42.Fredericks S., Lapum J., Graham J., et al. Continuity of care for adults living in the community who have been diagnosed with congenital heart disease. Primary Health Care. 2019;29:34–39. [Google Scholar]
- 43.Baumgartner H., De Backer J., Babu-Narayan S.V., et al. 2020 ESC Guidelines for the management of adult congenital heart disease. Eur Heart J. 2021;42:563–645. doi: 10.1093/eurheartj/ehaa554. [DOI] [PubMed] [Google Scholar]
- 44.Jacobs R., Boyd L., Brennan K., Sinha C.K., Giuliani S. The importance of social media for patients and families affected by congenital anomalies: a Facebook cross-sectional analysis and user survey. J Pediatr Surg. 2016;51:1766–1771. doi: 10.1016/j.jpedsurg.2016.07.008. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.