Abstract
Background:
Handoff miscommunications are a leading source of medical errors. Harmful medical errors decreased in pediatric academic hospitals following implementation of the I-PASS handoff improvement program. However, implementation across specialties has not been assessed.
Objective:
To determine if I-PASS implementation across diverse settings would be associated with improvements in patient safety and communication.
Design:
Prospective Type 2 Hybrid effectiveness implementation study.
Settings and Participants:
Residents from diverse specialties across 32 hospitals (12 community, 20 academic).
Intervention:
External teams provided longitudinal coaching over 18 months to facilitate implementation of an enhanced I-PASS program and monthly metric reviews.
Main Outcome and Measures:
Systematic surveillance surveys assessed rates of resident-reported adverse events. Validated direct observation tools measured verbal and written handoff quality.
Results:
2735 resident physicians and 760 faculty champions from multiple specialties (16 internal medicine, 13 pediatric, 3 other) participated. 1942 error surveillance reports were collected. Major and minor handoff-related reported adverse events decreased 47% following implementation, from 1.7 to 0.9 major events/person-year (p < .05) and 17.5 to 9.3 minor events/person-year (p < .001). Implementation was associated with increased inclusion of all five key handoff data elements in verbal (20% vs. 66%, p < .001, n = 4812) and written (10% vs. 74%, p < .001, n = 1787) handoffs, as well as increased frequency of handoffs with high quality verbal (39% vs. 81% p < .001) and written (29% vs. 78%, p < .001) patient summaries, verbal (29% vs. 78%, p < .001) and written (24% vs. 73%, p < .001) contingency plans, and verbal receiver syntheses (31% vs. 83%, p < .001). Improvement was similar across provider types (adult vs. pediatric) and settings (community vs. academic).
INTRODUCTION
The Joint Commission has identified communication errors as a contributing cause in approximately two out of every three “sentinel events”—the most serious adverse events in hospitals.1,2 The “handoff,” or transfer of patient information and responsibility between health care providers, is a critical point of vulnerability to a communication error. Several studies have found that there is often little standardization in the process or content of handoffs3–5 and that most resident physicians receive inadequate formal handoff training despite the emphasis on its importance from the National Academy of Medicine, ACGME, and others.6,7 Omissions of critical information, or the provision of outdated or erroneous information, occur very frequently.8 Several developments in health care systems have exacerbated handoff problems, including increasing patient complexity and work hour reductions.9–11 Because handoffs are highly vulnerable to errors and occur very frequently, they represent an important, understudied target for patient safety improvements.12–14
To address this vulnerability, our group began developing a bundle of handoff improvement interventions over a decade ago with an initial focus on pediatric resident physician end-of-shift handoffs. A successful single-center intervention15 served as the foundation for the I-PASS Handoff Program—a multifaceted verbal and written handoff communication improvement program organized around the mnemonic I-PASS (Illness severity, Patient summary, Action list, Situational awareness, and contingency planning, and Synthesis by receiver), that included handoff training, verbal and written handoff process improvements, faculty development and observations, and a sustainability campaign.16–18
After implementing this program in nine pediatric academic residency programs, preventable adverse events (harmful medical errors) decreased by 30%. However, it remained unclear whether the I-PASS program could be successfully implemented without the intensive oversight of a clinical trial, in specialties beyond pediatrics, or in community hospitals.
We, therefore, carried out a multicenter Type 2 Hybrid effectiveness implementation study to simultaneously determine if implementation of an enhanced I-PASS program across diverse settings would be associated with improvements in patient safety and communication.
METHODS
We conducted a 32-hospital project to implement the I-PASS program in inpatient teaching services caring for adults and children at tertiary care and community hospitals. The project was carried out in two 17-month long waves of implementation (16 hospitals in each wave) between 2015 and 2017 (Wave 1: April 2015 to August 2016; Wave 2: April 2016 to August 2017). This project was approved by the Boston Children’s Hospital Institutional Review Board (IRB). They determined that this was primarily a quality improvement (QI) project at the level of each participating hospital, but that IRB oversight was required for central data analysis. All participating sites received either local IRB approval or a QI waiver.
Participating hospitals
Interested hospitals completed a 32-item application that assessed institutional support, team strength, program size, geographical location, and a priori-defined characteristics of hospital type and specialty following a review of the 80 applications, a 10-member review committee selected 20 academic and 12 community hospitals to participate. Selected hospitals identified 1–2 units of a single specialty for the implementation where care was provided by resident-physicians in pediatrics (n = 13), internal medicine (n = 16), family medicine (n = 1), obstetrics and gynecology (n = 1), or medicine and pediatrics (n = 1). A mean of 87 resident physicians (ranging from a minimum of 13 to a maximum of 274 per site) and 25 faculty champions (ranging from a minimum of 3 to a maximum of 98 per site) participated as study subjects across the 32 hospitals.
Intervention development
Through a process of expert panel review, stakeholder input, and group consensus, we revised all of our previously developed, pediatric-focused I-PASS curricular and implementation materials to be applicable for adult medical providers as well as pediatric providers. We developed a robust implementation guide that extensively detailed key implementation steps and milestones, which has been published previously.19 We focused on eight key areas of implementation: (1) Establishing team structure and institutional support; (2) Conducting a needs assessment and developing process maps describing baseline and ideal handoff states; (3) Training of resident physicians; (4) Engagement of I-PASS Champions (faculty) in live observations of handoffs including training how to complete standardized handoff assessments and deliver effective feedback20; (5) Development of standardized data collection procedures; (6) Revision of existing computerized and/or written handoff tools to fit an I-PASS format; (7) Implementation of a campaign to help promote and sustain I-PASS tailored to the local environment, and (8) Development of strategies to motivate ongoing involvement of I-PASS Champions over time. In order to reach a wide range of learners (e.g., resident physicians, attending physicians, hospital leaders), we developed a series of training materials (suggested duration and facilitation instructions described in the implementation guide19) including a self-study video module,21 in-person workshops for front line residents,21 faculty,20 and institutional leaders, and printed campaign materials and worksheets.22
Implementation process
We adapted the mentored implementation process developed previously by the SHM23–26 to facilitate multicenter dissemination of our initiative. We assigned each site an external mentorship team consisting of two physicians with prior I-PASS implementation experience, a central program coordinator, and a data analyst. Participating mentors on average oversaw two sites per wave and were compensated as consultants. Participating sites were eligible to receive $500 of incentive funds upon completion of key milestones but no additional funding was provided to support local administrative or faculty efforts. Each site identified 1–3 individuals who served as site leads. Mentors worked with site leads to develop an organizational chart that facilitated the development of a local team of key stakeholders (e.g., residency program directors, electronic medical record champions, etc.) and other individuals who participated in program implementation.19
Implementation consisted of three phases: (1) a 4–6-month “baseline” period that involved planning and training, a needs assessment and handoff process mapping to adapt I-PASS to local needs and workflow, and collection of pre-intervention data; (2) a 6-month “peri-intervention” phase following an initial “go-live” date, during which regular feedback of data led to development of Plan-Do-Study-Act (PDSA) cycles to improve program adoption; and (3) a 6-month “post-intervention” period during which focus shifted towards maintenance of the program. During each phase, mentors conducted monthly conference calls with local site leads and helped ensure sites met standard implementation process milestones. Site leads were trained by their mentors and via program-wide curriculum webinars to use and ensure all sites implemented the resident-physician and faculty training materials described above. Mentors conducted a 1-day site visit during the peri-intervention phase. During the site visit, mentors reviewed the status of implementation milestones and challenges with key stakeholders and team leaders and built institutional support through activities such as delivering grand rounds and meeting with local institutional leaders. Both the peri- and postintervention phases involved a monthly review of data reports that included updated run charts displaying the site-specific status of all outcome and process measures (described in detail below) as compared with the aggregated data from across sites. During monthly 1-h-long conference calls in these phases, mentors provided coaching to facilitate the development of iterative improvement cycles designed to increase adoption of the I-PASS handoff method. Site leads and mentors also participated in program-wide quarterly collaborative calls where individual sites shared their implementation experiences, successes, and challenges.
Main outcome measures
Each site collected data on the inclusion of key data elements in written and verbal handoffs, as well as ratings of handoff quality through direct observation of a sample of handoffs (suggested 30-min minimum duration) by faculty members. During a handoff observation, faculty members observed multiple patients being handed off using an adapted version of a previously validated assessment tool.27 Faculty members were instructed on the use of the assessment tool during a 1-h training session that reviewed how to give feedback for verbal (individual-level) and written (team-based) handoffs. The handoff assessment tool measured the frequency with which each of several key handoff elements (Illness severity statement, Patient summary, Action list, Situational awareness, and contingency planning, and Synthesis by receiver) were included in verbal and written handoffs, measured on 5-point frequency scales (Never, Rarely, Sometimes, Usually, Always). Our primary process measure was the percentage of observed handoff sessions in which the giver and receiver of the handoff usually or always adhered to all five structural elements during verbal and written handoffs. Observers also assessed the quality of the verbal and written patient summary and the verbal synthesis by the receiver on 5-point quality scales (Poor, Fair, Good, Very Good, Excellent) and assessed the frequency of “high-quality contingency plans with clear if/then format” on a 5-point frequency scale (Never, Rarely, Sometimes, Usually, Always). For analysis, we calculated the percentage of observations in which each quality measure was rated as very good or excellent.
To assess the rate of handoff-related adverse events, we conducted systematic surveillance via a survey19 (independent of any hospital voluntary reporting systems) of resident physicians working on the implementation units each month, asking them to report the number of patients during their most recent period of service (typically 2–4 weeks) who experienced minor or major harm as a result of a problematic handoff.28 Minor harm was defined as a limited clinical consequence such as a need for more frequent monitoring or transient discomfort, without prolongation of hospitalization, significant organ dysfunction or worsening of clinical condition. Major Harm was defined as significant clinical consequences such as deterioration in clinical status, organ dysfunction, prolonged hospitalization, disability beyond discharge, or death. The reported adverse event rate was calculated as the number of major or minor handoff-related harms per person (i.e., resident-physician)-year to normalize for the duration of time each resident-physician spent on service.
Statistical analysis
For analysis, we grouped data into baseline (typically 1–3 month duration), peri-intervention (1–6 months following launch of the intervention), and postintervention (7–12 months following intervention launch) periods. We applied mixed-effects logistic regression models to assess the frequency that handoffs included key data elements and ratings of the quality of handoff elements over time. A mixed-effects Poisson regression model was used to assess changes in reported adverse event rates across time periods. All models included random intercepts to control for hospital clustering.
While our main analyses looked at changes in measures across all sites combined from baseline to the postimplementation period, we also conducted secondary analyses comparing metrics of handoff quality baseline vs. postimplementation for certain a priori identified hospital and resident characteristics. These included stratified analyses of the hospitals in the two different waves of participation, academic versus community hospitals, adult versus pediatric patients, and interns versus senior level resident-physicians. These secondary analyses were conducted with mixed-effects logistic regression models that include the main effects of the time period and hospital/resident characteristics and an interaction term between the two. Of note, because resident physicians of multiple years worked collaboratively on the same written handoff document, we did not conduct stratified analyses of interns versus senior-level resident-physicians when examining the quality and content of written handoff assessments. All statistical analyses were performed using SAS version 9.4 (SAS Institute), and two-sided p < .05 were considered statistically significant. To ensure objectivity, all data were analyzed via a statistical team who did not have a role in development or implementation of the intervention.
RESULTS
Handoff observation frequency
To assess how often key elements were included in handoff and rate handoff quality, 3798 individuals were observed giving handoff (n = 431 baseline, 1859 peri-intervention, and 1508 postintervention) and 3429 were observed receiving handoff (n = 202 baseline, 1467 peri-intervention, and 1121 postintervention); 1620 printed handoff documents (n = 143 baseline, 715 peri-intervention, and 762 post-intervention) were reviewed. A mean of 9.7 observations of verbal handoffs per site per month and 5.4 printed handoff observations per site per month were completed.
Handoff quality
Implementation of the I-PASS Handoff Program across all 32 sites was associated with a marked improvement in the percentage of handoffs that usually or always included all key handoff elements (Figure 1). At baseline, 20.0% (95% confidence interval [CI]: 15.0%, 26.2%) of verbal handoffs included all five key elements, versus 51.9% (45.1%, 58.5%) peri-intervention and 66.3% (59.8%, 72.1%) postintervention. Similarly, written handoff communications included all five key elements 10.4% (5.8%, 17.7%) at baseline, 46.9% (36.1%, 58.1%) peri-intervention, and 73.5% (63.8%, 81.4%) postintervention.
FIGURE 1.
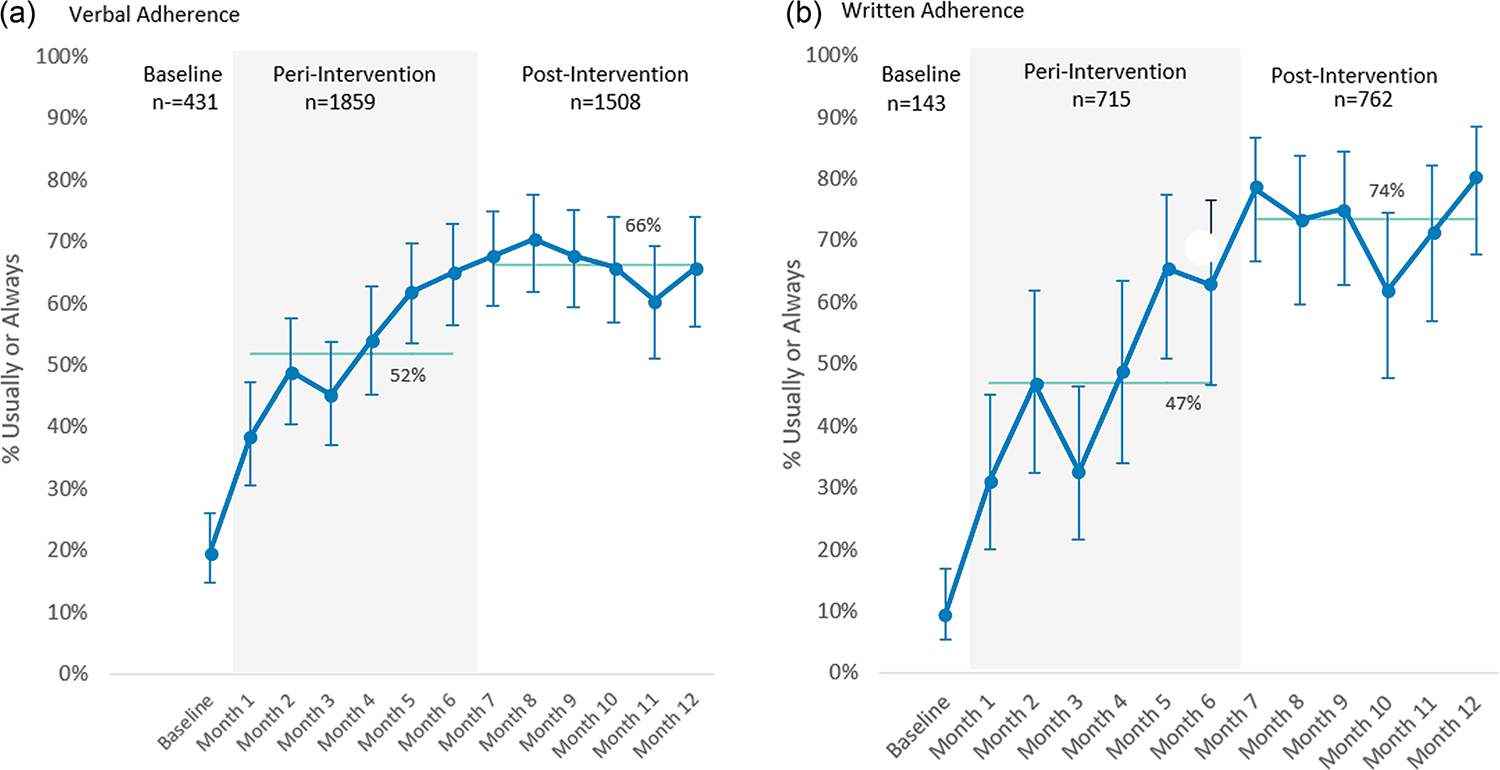
Adherence to (a) all 5 verbal I-PASS elements and (b) all five written I-PASS elements. For both figures, to account for clustering by site, proportions estimated from mixed effects models. Vertical lines represent 95% confidence intervals. Horizontal lines reflect peri-intervention and postintervention overall adherence rates.
From the baseline to the postintervention period there were also significant improvements in the percentage of verbal and written handoffs that included very good or excellent patient summaries (38.7%–80.9% verbal; 29.1%–78.1% written), that usually or always included high-quality contingency plans (28.9%–77.8% verbal; 24.1%–72.6% written), and that included very good or excellent syntheses by the receiving physician (31.4%–83.1%) (Figure 2, p < .001 for all comparisons).
FIGURE 2.
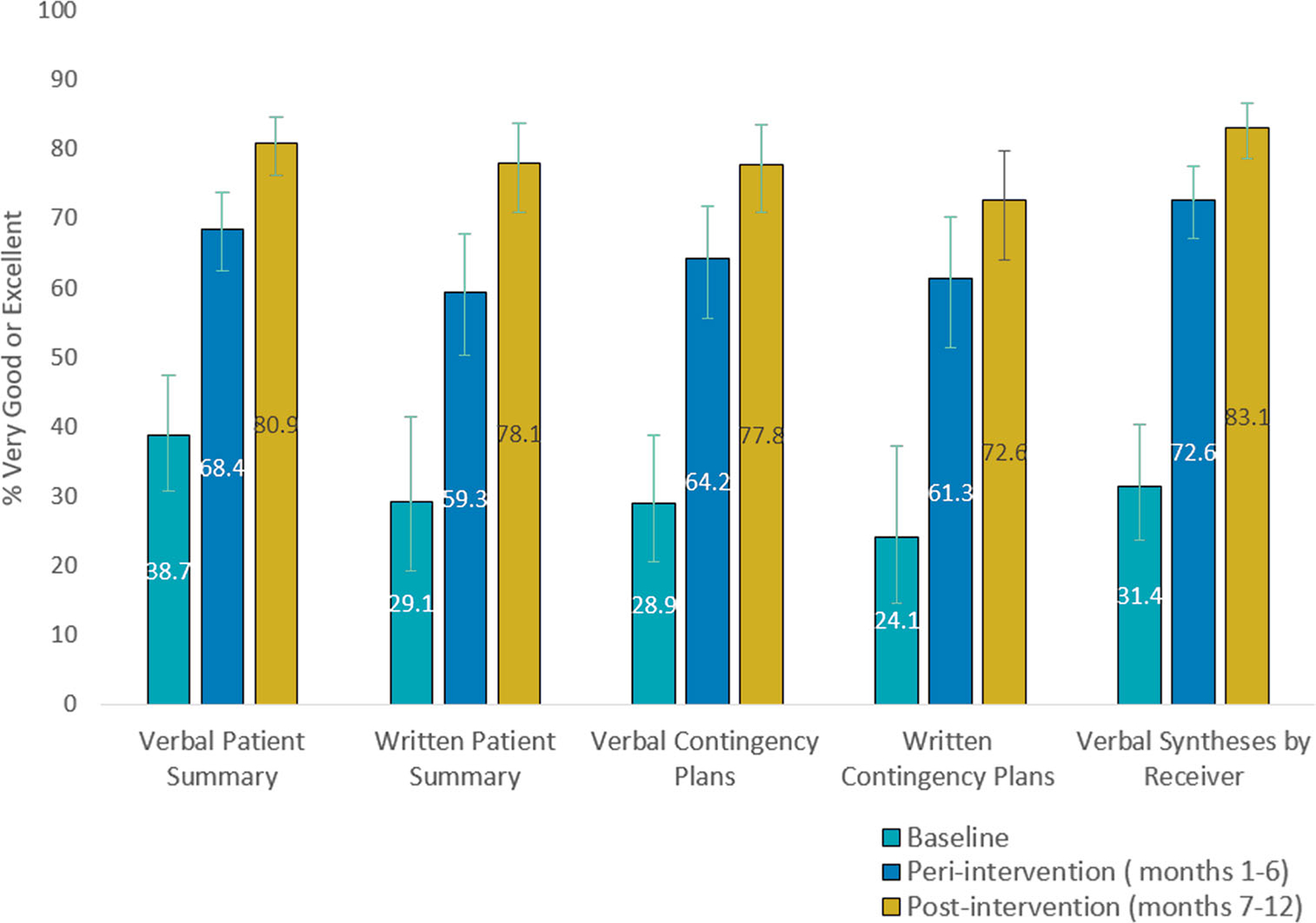
Quality of verbal and written handoff communication. To account for clustering by site, proportions estimated from mixed effects models. Vertical lines represent 95% confidence intervals. Improvement from baseline to postintervention for all comparisons (p < .001).
Handoff-related reported adverse events
A total of 1942 standardized surveillance reports (n = 245 baseline, 869 peri-intervention, and 828 postintervention) of the frequency of handoff-related adverse events were collected from the resident end-of-rotation survey (response rate 58.6%). Across all sites combined, mentored implementation of the I-PASS Handoff Program was associated with a 47.1% reduction in the frequency of handoff-related reported major adverse events (1.7 vs. 0.9 events per person-year, p < .05), as well as a 46.9% reduction in handoff-related, reported minor harm events (17.5 vs. 9.3 events per person-year, p < .001) (Table 1).
TABLE 1.
Handoff‐related, resident‐physician reported adverse event rate by intervention time period
| Events/person year (95% CI) |
p Value (baseline vs. postintervention) | |||
|---|---|---|---|---|
| Baseline (n = 245) | Peri‐intervention (1–6 months, n = 869) | Postintervention (7–12 months, n = 828) | ||
| Any adverse event | 19.7 | 12.7 | 10.5 | <.001 |
| (16.9, 22.9) | (11.3, 14.3) | (9.3, 11.9) | ||
| Minor event | 17.5 | 11.8 | 9.3 | <.001 |
| (15.1, 20.3) | (10.6, 13.1) | (8.2, 10.4) | ||
| Major event | 1.7 | 0.9 | 0.9 | .03 |
| (1.1, 2.7) | (0.7, 1.3) | (0.7, 1.3) | ||
Abbreviation: CI, confidence interval.
Subgroup analyses
Differences existed in how often certain subgroups included key data elements at baseline (Figures 3 and 4). However, there were no significant differences in the extent to which adherence to the I-PASS structure for verbal or written handoffs was attained during the postintervention period when comparing the characteristics of study wave, community versus academic setting, specialty, or level of training (Figures 3 and 4). There were significant tests of interaction for the degree of improvement in handoff adherence over time and several hospital and participant characteristics (Figures 3 and 4), driven largely by differences in baseline rates. Reported adverse event rates decreased significantly from baseline to postintervention for all comparisons (p < .001) except for community hospital (p = .069) (Supporting Information: Appendix 2).
FIGURE 3.
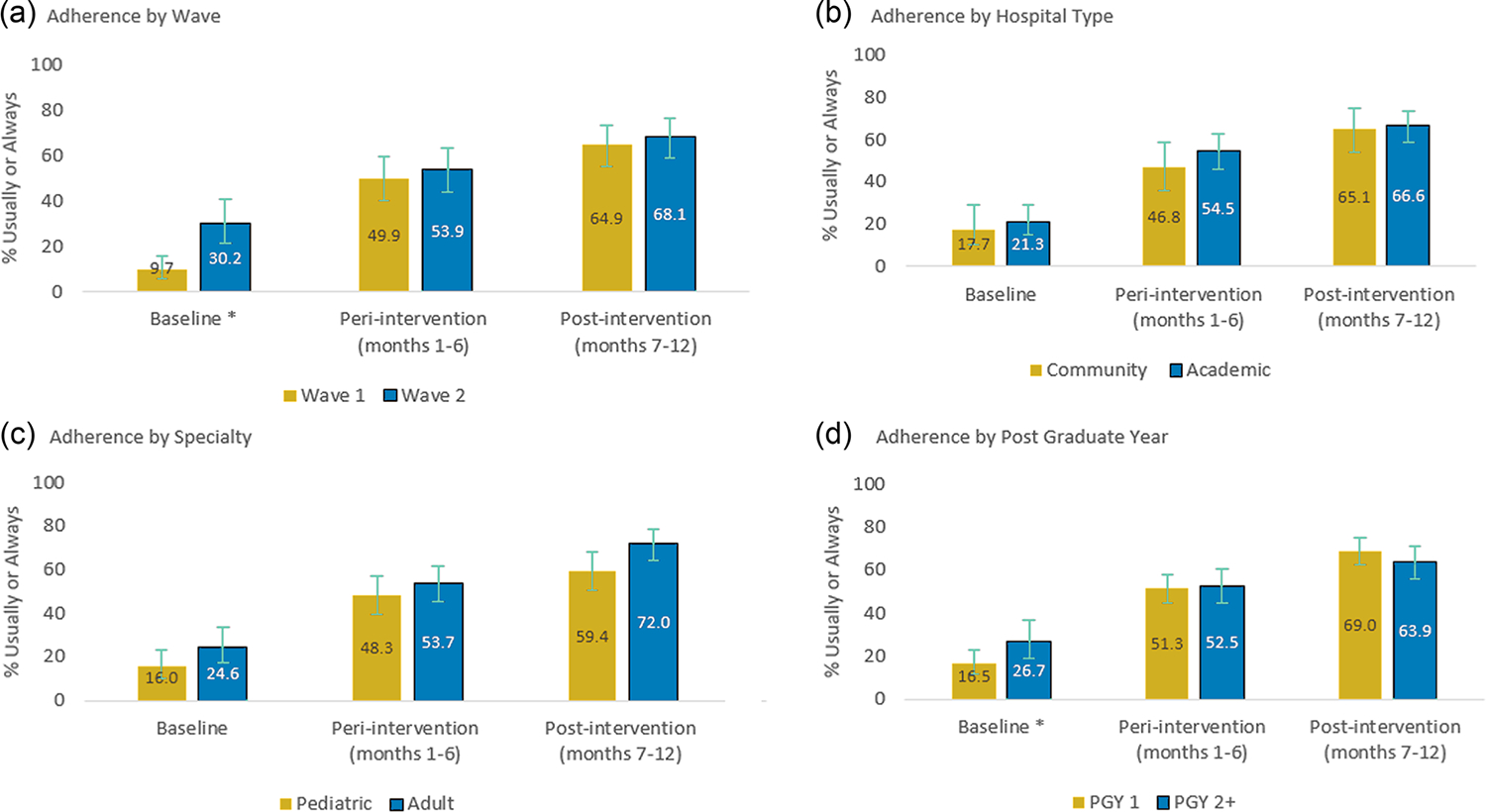
Verbal adherence to I-PASS by hospital and resident characteristics of (a) wave, (b) hospital type, (c) specialty, and (d) post graduateyear. For all figures, to account for clustering by site, proportions estimated from mixed effects models. Vertical lines represent 95% confidence intervals. Improvement from baseline to postintervention for all comparisons (p < .001). *Difference at baseline across wave (p < .001) and postgraduate year (p < .05). The test of interaction between time (baseline to postintervention) and hospital characteristic was significant for wave (p < .001) and postgraduate year (0.011) but not for hospital type (p = .325) or specialty (p = .070). There were no significant differences in adherence in the postintervention period by wave, hospital type, specialty, or PGY year.
FIGURE 4.
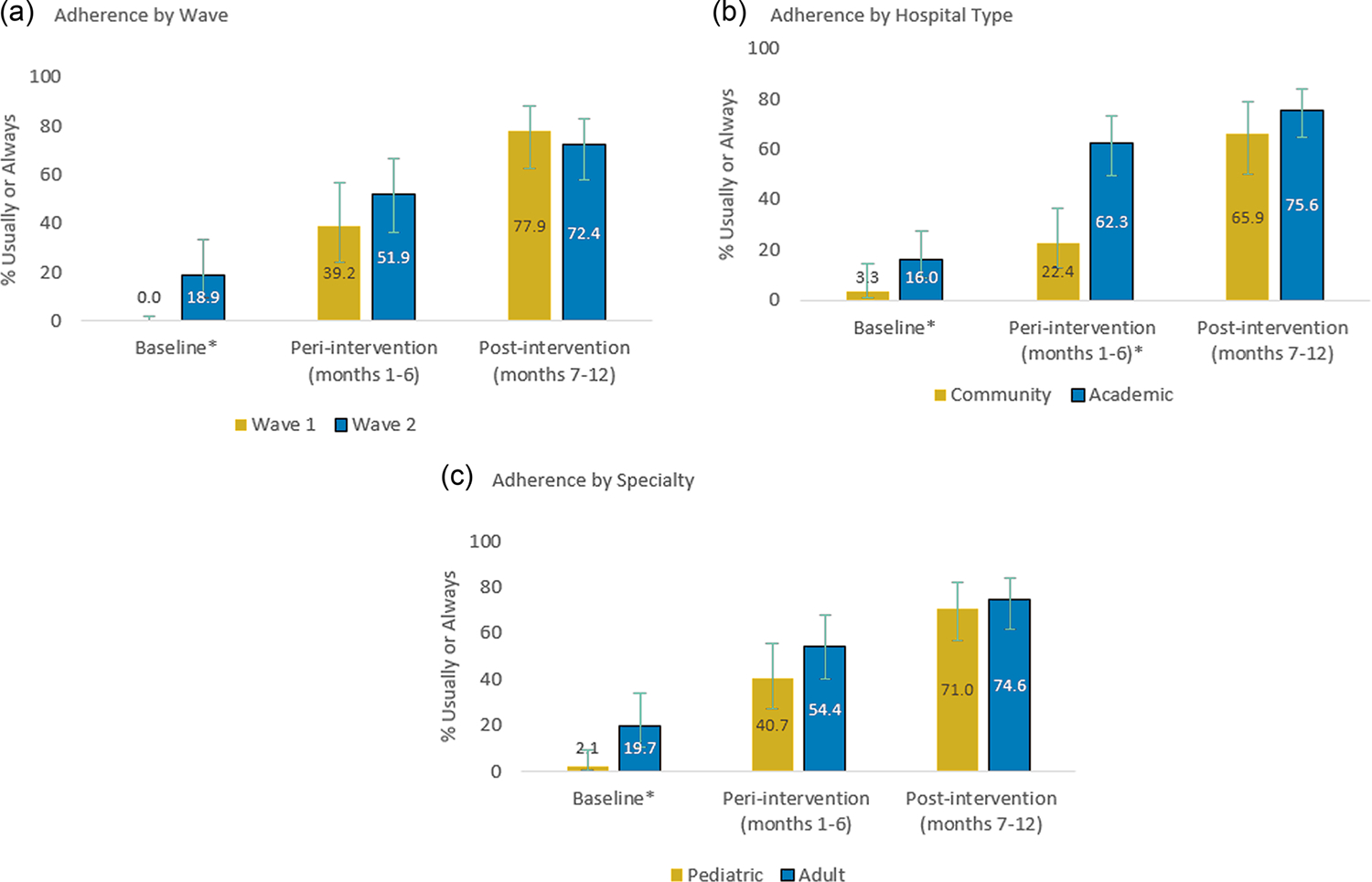
Written adherence to I-PASS by hospital characteristics of (a) wave of participation, (b) hospital type, and (c) specialty. For all figures, to account for clustering by site, proportions estimated from mixed effects models. Vertical lines represent 95% confidence intervals. Improvement from baseline to postintervention for all comparisons (p < .001). *p < .05 across wave, hospital type, and specialty at baseline. The test of interaction between time (baseline to postintervention) and hospital characteristic was significant for wave (p < .001), hospital type (p < .001), and specialty (p = .018), reflecting significant differences atbaseline. There were no signicant differences in adherence in the postintervention period by wave, hospital type, or specialty.
DISCUSSION
We found that implementation of the I-PASS Handoff Program in a wide range of pediatric and adult settings was associated with major improvements in handoff communications and a 47% reduction in handoff-related adverse events. Importantly, across provider types (adult vs. pediatric), settings (community vs. academic), and level of training (PGY1 vs. PGY2+), similarly high levels of handoff quality and reported adverse event reduction rates were achieved post-implementation. Taken together, these findings indicate that the I-PASS Handoff Program can be successfully implemented in diverse specialties and hospitals, and could potentially promote widespread improvements in patient safety.
In our prior nine-center pediatric study, preventable adverse events decreased by 30% after implementation of I-PASS. In the current effectiveness implementation study, we extended this work by adapting and implementing I-PASS for adult patients and resident physicians in academic and community hospital settings. By design, we rolled the program out without the robust funding for personnel and data collection efforts that supported our prior clinical trial, to determine if sites could successfully implement it with more limited financial support, though the study did provide external coaching and infrastructure. Additionally, sites were primarily responsible for rolling the intervention out locally and for funding their personnel.
Since the completion of our prior pediatric I-PASS Study, literature has emerged suggesting that I-PASS might be adapted for use by nurses29 and medical students,6,30 as well as psychiatrists,31 Emergency Department physicians,32,33 and other provider34–36 or handoff types.37,38 While these studies reported improved outcomes and handoff quality following implementation, they typically had a less comprehensive implementation approach, reported fewer outcomes without a focus on process measures as well as adverse events and were typically conducted in only one or two units at a time within a single institution. A larger hospital-wide study by Shahian et al.39 likewise suggested that I-PASS could be rolled out to nurses and physicians across care areas, but this effort was limited by a number of identified implementation barriers, and data describing outcomes were limited; importantly, patient safety was not measured. To our knowledge, no studies have evaluated the implementation of any handoff program in as many diverse settings as did the current study.
To assess adverse event rates, we relied on a novel approach of systematic surveillance of resident physicians through monthly systematic surveys. While this approach is considerably more robust than hospitals’ typical voluntary event reporting systems, it was less comprehensive than the methodology used in our prior work.16 We chose to capture data in this manner to improve the feasibility and sustainability of program evaluation, but it is likely that this methodology captures only a subset of the errors that would be captured using more comprehensive surveillance. Of note, however, the degree of reduction in adverse events we observed using this methodology was of similar magnitude to that seen in our prior studies using more intensive methods that incorporated detailed medical record review as well as more detailed provider and/or patient reporting.15,16
Our project has several limitations. First, we focused on resident-physician end-of-shift handoffs, with a primary focus on general pediatric and internal medicine units, and the extent to which the I-PASS approach is generalizable to additional handoff or provider types is unclear. While the I-PASS structure is potentially adaptable to more complex handoffs (e.g., intrafacility or interfacility transfers, inpatient to outpatient transitions, and transitions involving ambulatory care), each of these multi-stakeholder communications involves nuances that warrant further study of the adaptation and implementation process. Second, although we gave explicit instructions on how to measure the inclusion of data elements and the quality of handoff documentation, those measuring these processes or reporting adverse event frequency could not be blinded to intervention status, which might have introduced bias. The concordance between multiple process measures by raters and the adverse events reported by resident physicians themselves, however, is reassuring. Additionally, as with any survey the adverse event reporting by resident physicians may be subject to recall bias although our systematic surveillance approach was intended to minimize the impact of this limitation over the course of the study. Third, while the degree of support and infrastructure we provided to each site in the project was much less than that of what we previously provided in our clinical trial, substantial site mentor and study team effort was expended to facilitate the successful implementation of the program. The degree to which hospitals might be successful in implementing I-PASS without such an investment of resources remains unclear. Fourth, while our response rate of 58% was relatively strong for a pragmatic study of resident physicians, nonresponse bias could have affected our estimates of adverse event rates and other measures. Given the magnitude of the effect size observed in this study, however, we believe it highly unlikely that nonresponse bias could have occurred differentially in the different phases of the study to a degree that would have substantively changed our main findings. Lastly, though our selected sites were diverse, other sites might not experience the same degree of improvement observed here. Based on our collective experiences, we believe sites must be fully committed to a QI project in order for it to succeed, with the needed infrastructure in place to carry it out.
CONCLUSIONS
We found that implementation of the I-PASS Handoff Program in 32 hospitals was associated with increased inclusion of key handoff data elements, improvements in the quality of handoff communication, and a significant reduction in reported rates of handoff-related adverse events. A wide variety of provider types across diverse adult and pediatric settings were able to achieve similarly high levels of achievement using I-PASS. At a policy level, we believe that our findings provide evidence that substantiates the ongoing focus of the ACGME and Joint Commission on handoffs. Moreover, as studies have consistently demonstrated the critical importance of high-quality, multifaceted handoff programs, we believe that policies should evolve to reflect these data, more strongly incentivizing adoption of high-quality handoff programs that have been demonstrated to substantially advance patient safety.
Supplementary Material
ACKNOWLEDGMENTS
The authors would like to express their sincere appreciation to the resident physicians, faculty, patients, and families who participated in the project as well as to the Pediatric Research in Inpatient Settings (PRIS) Network and the Society for Hospital Medicine for their support in facilitating the project. The SHM I-PASS Study was supported by a grant from the Agency for Healthcare Research and Quality (AHRQ, R18 HS23291-01).
Footnotes
CONFLICT OF INTEREST
All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declare: all authors had financial support from the Agency for Healthcare Research and Quality for the submitted work. CPL, SJP, TCS, NDS, AJS, and DCW hold equity in the I-PASS Patient Safety Institute. RS works for Intermountain Healthcare, which holds equity in the I-PASS Patient Safety Institute. SC, JKO’T, and SJP hold stock options in the I-PASS Patient Safety Institute. SC, NK, CPL, JKO’T, SJP, GR, TCS, NDS, AJS, and DCW have consulted with the I-PASS Patient Safety Institute. The I-PASS Patient Safety Institute is a company that seeks to train institutions in best handoff practices and aid in their implementation. The current study was designed before the I-PASS Patient Safety Institute was conceived of as an entity and the I-PASS Patient Safety Institute was in no way involved in this study. Moreover, to ensure objectivity, all data were analyzed via a statistical team who do not have any involvement with the I-PASS Patient Safety Institute. All analyses were conducted by this statistical team. TCS, NDS, AJS, and DCW have received monetary awards, honoraria, and travel reimbursement from multiple academic and professional organizations for teaching and consulting on physician performance and handoffs. CPL and RS are supported in part by the Children’s Hospital Association for their work as executive council members of the Pediatric Research in Inpatient Settings (PRIS) network. RS has received monetary awards, honorariums, and travel reimbursement from multiple academic and professional organizations for talks about pediatric hospitalist research networks and quality of care. CPL has received monetary awards, honoraria, and travel reimbursement from multiple academic and professional organizations for teaching and consulting on sleep deprivation, physician performance, handoffs, and safety, and has served as an expert witness in cases regarding patient safety and sleep deprivation. JLS was the recipient of a grant from Mallinckrodt Pharmaceuticals to conduct an investigator-initiated study of opioid-related adverse drug events in surgical patients. All other authors have no conflict of interest to disclose at this time.
SUPPORTING INFORMATION
Additional supporting information can be found online in the Supporting Information section at the end of this article.
REFERENCES
- 1.The Joint Commission. Sentinel event statistics released for 2014. The Joint Commission Online. Accessed October 6, 2017. http://www.jointcommission.org/assets/1/23/jconline_April_29_15.pdf
- 2.Starmer AJ, Spector ND, West DC, Srivastava R, Sectish TC, Landrigan CP. Integrating research, quality improvement, and medical education for better handoffs and safer care: disseminating, adapting, and implementing the I-PASS program. Jt Comm J Qual Patient Saf. 2017;43(7):319–329. doi: 10.1016/j.jcjq.2017.04.001 [DOI] [PubMed] [Google Scholar]
- 3.Horwitz LI, Krumholz HM, Green ML, Huot SJ. Transfers of patient care between house staff on internal medicine wards: a national survey. Arch Intern Med. 2006;166(11):1173–1177. doi: 10.1001/archinte.166.11.1173 [DOI] [PubMed] [Google Scholar]
- 4.Solet DJ, Norvell JM, Rutan GH, Frankel RM. Lost in translation: challenges and opportunities in physician-to-physician communication during patient handoffs. Acad Med. 2005;80(12):1094–1099. [DOI] [PubMed] [Google Scholar]
- 5.Vidyarthi AR, Arora V, Schnipper JL, Wall SD, Wachter RM. Managing discontinuity in academic medical centers: strategies for a safe and effective resident sign-out. J Hosp Med. 2006;1(4):257–266. doi: 10.1002/jhm.103 [DOI] [PubMed] [Google Scholar]
- 6.O’toole JK, Stevenson AT, Good BP, et al. Closing the gap: a needs assessment of medical students and handoff training. J Pediatr. 2013;162(5):887–888. doi: 10.1016/j.jpeds.2013.01.045 [DOI] [PubMed] [Google Scholar]
- 7.Sectish TC, Starmer AJ, Landrigan CP, Spector ND, I-PASS Study Group. Establishing a multisite education and research project requires leadership, expertise, collaboration, and an important aim. Pediatrics. 2010;126(4):619–622. doi: 10.1542/peds.2010-1793 [DOI] [PubMed] [Google Scholar]
- 8.Mistry K, Landrigan C, Goldmann D, Bates D. Communication during post-operative patient hand-off in the pediatric intensive care unit. Presented at: Critical Care Medicine; 2005. [Google Scholar]
- 9.Landrigan CP, Rothschild JM, Cronin JW, et al. Effect of reducing interns’ work hours on serious medical errors in intensive care units. N Engl J Med. 2004;351(18):1838–1848. doi: 10.1056/NEJMoa041406 [DOI] [PubMed] [Google Scholar]
- 10.Berry J, Agrawal R, Kuo D. Characteristics of hospitalizations for patients who use a structured clinical care program for children with medical complexity. JAMA Pediatrics. 2011;159(2):284–290. doi: 10.1016/j.jpeds.2011.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Berry J, Agrawal RK, Cohen E, Kuo DZ. The landscape of medical care for children with Medical Complexity Children’s Hospital Association; 2018. Accessed March 10, 2018. https://www.childrenshospitals.org/issues-and-advocacy/children-with-medical-complexity/issue-briefs-and-reports/the-landscape-of-medical-care-for-children-with-medical-complexity
- 12.Abraham J, Kannampallil T, Patel VL. A systematic review of the literature on the evaluation of handoff tools: implications for research and practice. J Am Med Inform Assoc. 2014;21(1):154–162. doi: 10.1136/amiajnl-2012-001351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mardis M, Davis J, Benningfield B, et al. Shift-to-shift handoff effects on patient safety and outcomes: a systematic review. Am J Med Qual. 2017;32(1):34–42. doi: 10.1177/1062860615612923 [DOI] [PubMed] [Google Scholar]
- 14.Riesenberg LA, Leitzsch J, Massucci JL, et al. Residents’ and attending physicians’ handoffs: a systematic review of the literature. Acad Med. 2009;84(12):1775–1787. doi: 10.1097/ACM.0b013e3181bf51a6 [DOI] [PubMed] [Google Scholar]
- 15.Starmer AJ, Sectish TC, Simon DW, et al. Rates of medical errors and preventable adverse events among hospitalized children following implementation of a resident handoff bundle. JAMA. 2013;310(21):2262–2270. doi: 10.1001/jama.2013.281961 [DOI] [PubMed] [Google Scholar]
- 16.Starmer AJ, Spector ND, Srivastava R, et al. Changes in medical errors after implementation of a handoff program. N Engl J Med. 2014;371(19):1803–1812. doi: 10.1056/NEJMsa1405556 [DOI] [PubMed] [Google Scholar]
- 17.Starmer AJ, O’toole JK, Rosenbluth G, et al. Development, implementation, and dissemination of the I-PASS Handoff Curriculum: a multisite educational intervention to improve patient handoffs. Acad Med. 2014;89(6):876–884. [DOI] [PubMed] [Google Scholar]
- 18.Starmer AJ, Spector ND, Srivastava R, et al. I-PASS, a mnemonic to standardize verbal handoffs. Pediatrics. 2012;129(2):201–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.O’toole JK, Starmer AJ, Calaman S, et al. I-PASS mentored implementation handoff curriculum: implementation guide and resources. MedEdPORTAL. 2018;14(14):10736. doi: 10.15766/mep_2374-8265.10736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.O’toole JK, Starmer AJ, Calaman S, et al. I-PASS mentored implementation handoff curriculum: champion training materials. MedEdPORTAL. 2019;15(15):10794. doi: 10.15766/mep_2374-8265.10794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.O’toole JK, Hepps J, Starmer AJ, et al. I-PASS mentored implementation handoff curriculum: frontline provider training materials. MedEdPORTAL. 2020;16:10912. doi: 10.15766/mep_2374-8265.10912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rosenbluth G, Patel SJ, Destino LA, et al. I-PASS Handoff Curriculum: Campaign Toolkit. MedEdPORTAL. 9:9397. doi: 10.15766/mep_2374-8265.9397 [DOI] [Google Scholar]
- 23.Maynard GA, Budnitz TL, Nickel WK, et al. Mentored implementation: building leaders and achieving results through a collaborative improvement model. Innovation in patient safety and quality at the national level. Jt Comm J Qual Patient Saf. 2012;38(7):301–310. [DOI] [PubMed] [Google Scholar]
- 24.Li J, Hinami K, Hansen LO, Maynard G, Budnitz T, Williams MV. The physician mentored implementation model: a promising quality improvement framework for health care change. Acad Med. 2015;90(3):303–310. doi: 10.1097/ACM.0000000000000547 [DOI] [PubMed] [Google Scholar]
- 25.Schnipper JL, Mixon A, Stein J, et al. Effects of a multifaceted medication reconciliation quality improvement intervention on patient safety: final results of the MARQUIS study. BMJ Qual Saf. 2018;27(12):954–964. doi: 10.1136/bmjqs-2018-008233 [DOI] [PubMed] [Google Scholar]
- 26.Rogers KM, Childers DJ, Messler J, Nolan A, Nickel WK, Maynard GA. Glycemic control mentored implementation: creating a national network of shared information. Jt Comm J Qual Patient Saf. 2014;40(3):111–118. doi: 10.1016/s1553-7250(14)40014-x [DOI] [PubMed] [Google Scholar]
- 27.Starmer AJ, Landrigan C, Srivastava R, et al. I-PASS handoff curriculum: faculty observation tools. MedEdPORTAL. 2013;9:9570. doi: 10.15766/mep_2374-8265.9570 [DOI] [Google Scholar]
- 28.Kitch BT, Cooper JB, Zapol WM, et al. Handoffs causing patient harm: a survey of medical and surgical house staff. Jt Comm J Qual Patient Saf. 2008;34(10):563–570. doi: 10.1016/s1553-7250(08)34071-9 [DOI] [PubMed] [Google Scholar]
- 29.Starmer AJ, Schnock KO, Lyons A, et al. Effects of the I-PASS Nursing Handoff Bundle on communication quality and workflow. BMJ Qual Saf. 2017;26:949–957. doi: 10.1136/bmjqs-2016-006224 [DOI] [PubMed] [Google Scholar]
- 30.Sheng J, Manjunath S, Michael M, et al. Integrating handover curricula in medical school. Clin Teach. 2020;17(6):661–668. doi: 10.1111/tct.13181 [DOI] [PubMed] [Google Scholar]
- 31.Bowes MR, Santiago PN, Hepps JH, Hershey BR, Yu CE. Using I-PASS in psychiatry residency transitions of care. Acad Psychiatry. 2018;42(4):534–537. doi: 10.1007/s40596-017-0822-1 [DOI] [PubMed] [Google Scholar]
- 32.Heilman JA, Flanigan M, Nelson A, Johnson T, Yarris LM. Adapting the I-PASS handoff program for emergency department inter-shift handoffs. West J Emerg Med. 2016;17(6):756–761. doi: 10.5811/westjem.2016.9.30574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chladek MS, Doughty C, Patel B, et al. The standardisation of handoffs in a large academic paediatric emergency department using I-PASS. BMJ Open Qual. 2021;10(3):e001254. doi: 10.1136/bmjoq-2020-001254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fitzgerald KM, Banerjee TR, Starmer AJ, et al. Effect of a multispecialty faculty handoff initiative on safety culture and handoff quality. Pediatr Qual Saf. 2022;7(2):e539. doi: 10.1097/pq9.0000000000000539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wolinska JM, Lapidus-Krol E, Fallon EM, Kolivoshka Y, Fecteau A. I-PASS enhances effectiveness and accuracy of hand-off for pediatric general surgery patients. J Pediatr Surg. 2022;57(4):598–603. doi: 10.1016/j.jpedsurg.2021.11.015 [DOI] [PubMed] [Google Scholar]
- 36.Jorro-Barón F, Suarez-Anzorena I, Burgos-Pratx R, et al. Handoff improvement and adverse event reduction programme implementation in paediatric intensive care units in Argentina: a stepped-wedge trial. BMJ Qual Saf. 2021;30(10):782–791. doi: 10.1136/bmjqs-2020-012370 [DOI] [PubMed] [Google Scholar]
- 37.Blazin LJ, Sitthi-Amorn J, Hoffman JM, Burlison JD. Improving patient handoffs and transitions through adaptation and implementation of I-PASS across multiple handoff settings. Pediatr Qual Saf. 2020;5(4):e323. doi: 10.1097/pq9.0000000000000323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Huth K, Stack AM, Hatoun J, et al. Implementing receiver-driven handoffs to the emergency department to reduce miscommunication. BMJ Qual Saf. 2021;30(3):208–215. doi: 10.1136/bmjqs-2019-010540 [DOI] [PubMed] [Google Scholar]
- 39.Shahian DM, McEachern K, Rossi L, Chisari RG, Mort E. Large-scale implementation of the I-PASS handover system at an academic medical centre. BMJ Qual Saf. 2017;26(9):760–770. doi: 10.1136/bmjqs-2016-006195 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


