SUMMARY
Background:
Social determinants of health (SDoH) are consistently associated with SLE outcomes; however, SDoH are typically measured with conventional socioeconomic status (SES) factors such as income or education. We assessed the association of economic insecurities (food, housing, healthcare, and financial insecurity) with patient-reported outcomes (PROs), over and above conventional SES measures, in an SLE cohort.
Methods:
Data were derived from the California Lupus Epidemiology Study (CLUES; n=252). Food, housing, healthcare, and financial economic insecurities were assessed by validated screening tools. PROs were obtained via PROMIS, Neuro-QoL, Patient Health Questionnaire (PHQ)-8, and General Anxiety Disorder (GAD)-7 instruments. Poverty was defined as household income ≤125% of the federal poverty limit. Lower education was defined as less than college-graduate education. The association of economic insecurities with PROs was assessed by multivariable linear regression models adjusting for demographics, lupus characteristics, and comorbidities. We tested for interactions of insecurities with poverty and education.
Findings:
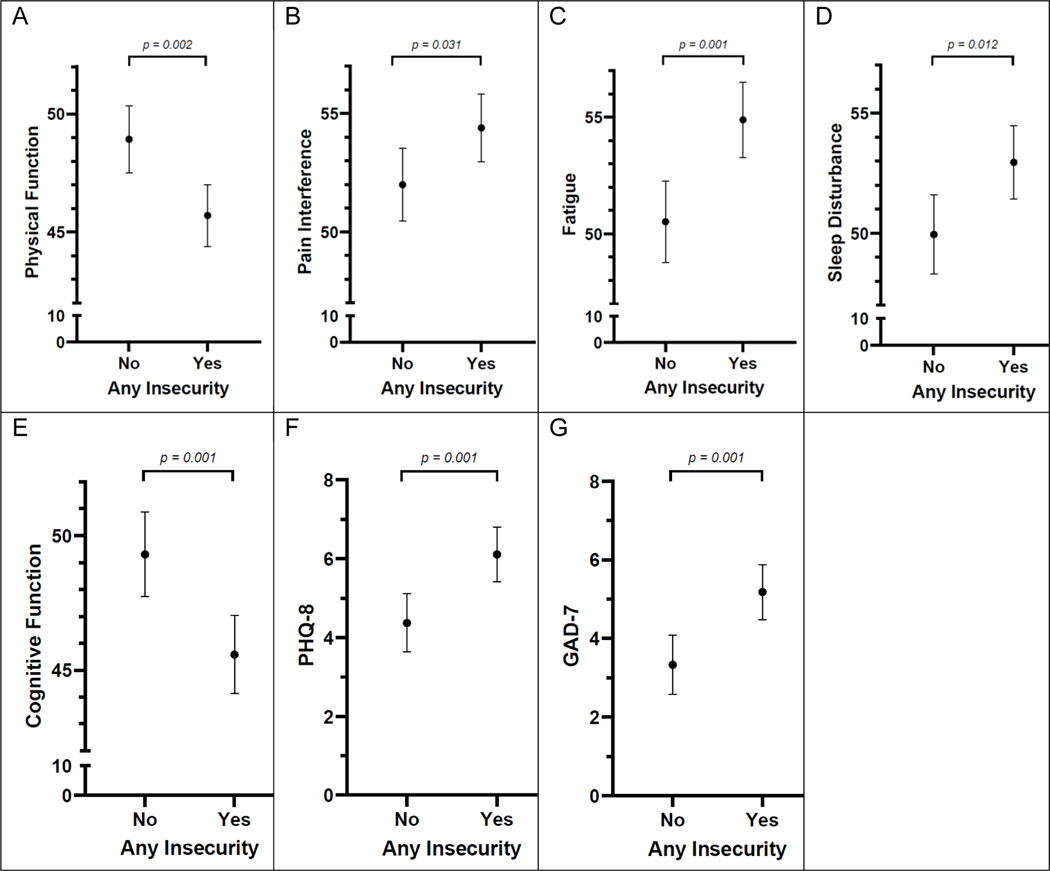
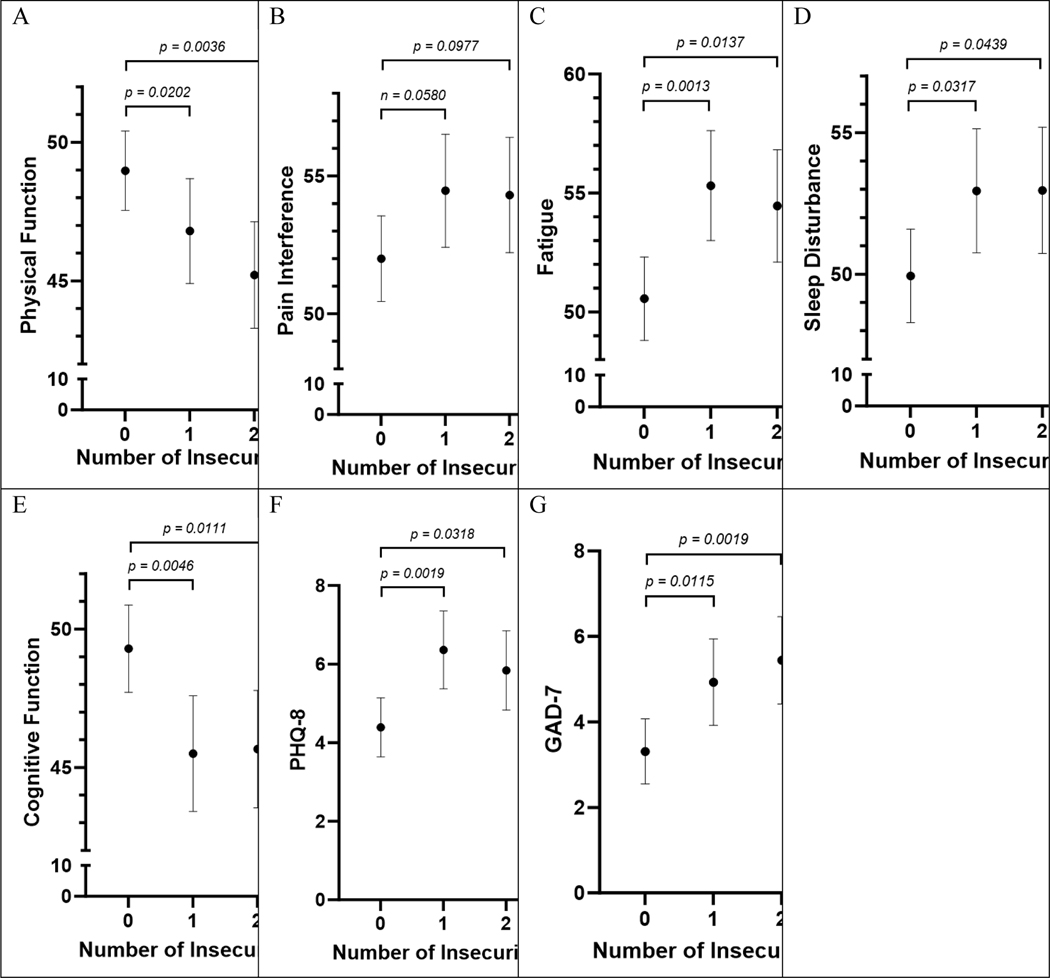
Mean age was 49·7 ±13.4 years, and 91% (228/252) were female. 32% (80/252) self-identified as Asian, 10% (26/252) as Black, 40% (101/252) as White, 3% (8/252) as mixed race, and 14% (36/252) as other race. About a quarter (59/252) self-identified as Hispanic. 54% (135/252) had at least one insecurity. Insecurities were highly prevalent, and more common in those with poverty and lower education. Adjusted multivariate analyses revealed that participants with any insecurity had significantly worse scores across all PROs measured: Physical Function, no insecurity 48·9 (47·5, 50·3) vs. any insecurity 45·7 (44·3, 47·0); Pain Interference, 52·0 (50·5, 53·5) vs. 54·4 (53·0, 55·8); Fatigue, 50·5 (48·8, 52·3) vs. 54·9 (53·3, 56·5); Sleep Disturbance, 49·9 (48·3, 51·6) vs. 52·9 (51·4, 54·5); Cognitive Function, 49·3 (47·7, 50·9) vs. 45.6 (44·1, 47·0); PHQ-8, 4.4 (3·6, 5·1) vs. 6.1 (5·4, 6·8); and GAD-7, 3·3 (2·6, 4·1) vs. 5·2 (4·5, 5·9). Individuals with more insecurities exhibited worse PROs. There were no statistically significant interactions between insecurities and poverty or education.
Interpretation:
Having any economic insecurity was associated with worse outcomes for people with SLE regardless of poverty or education. Findings provide insight into the relationship between economic insecurities and SLE outcomes and underscore the need to study whether interventions that directly address these insecurities can reduce health disparities in this disease.
Introduction
Systemic lupus erythematosus (SLE) is a chronic autoimmune disease with a prevalence of approximately 73 per 100,000 person-years in North America.1 Research suggests a genetic component to SLE onset but that the course and severity of SLE are often driven by social determinants of health (SDoH),2 defined as the “conditions in which people are born, grow, live, work, and age.”3 While SDoH encompass a wide range of social risk factors, only a select few have been examined in SLE, such as income, education level, and health insurance status. These factors have been associated with disease activity, damage accrual, and mortality.4,5
However, after accounting for SDoH like poverty, education, and health insurance status, there are still variations in SLE outcomes that may be related to additional SDoH. Recently, some researchers have investigated the concept of economic insecurity, including difficulty paying for food, medications, or housing and found strong associations with several chronic disease outcomes.3 These measures may be particularly salient in the case of a complex chronic disease like SLE, a condition that requires significant out-of-pocket costs even among patients with health insurance.6 Indeed, a recent qualitative study reported that low-income and non-low-income respondents had similar experiences accessing care and having a treatment plan, and that both groups were affected by traditional stressors for persons with SLE (e.g., sun exposure, daily hassles).7 However, the groups differed in their experience of economic insecurity, with low-income respondents reporting more concerns about housing, food, and medical costs. In addition to these chronic stressors, low-income respondents highlighted how these concerns caused them to relegate dealing with SLE to times of severe illness or distress, rather than chronic disease management that focused on prevention of disease exacerbations.
We built on this work by assessing the relationship between measures of economic insecurity and SLE patient-reported outcomes (PROs) in the California Lupus Epidemiology Study (CLUES). Our analyses were guided by the comprehensive SDoH conceptual framework developed by the World Health Organization (WHO) in which material circumstances such as housing and financial means to buy food are viewed as intermediary determinants of health outcomes, separate from, but causally related to, structural SDoH such as education and income.8 In the WHO framework, these intermediary factors constitute an important mechanism through which socioeconomic position generates health inequities.
In this paper, we examined the hypothesis that such intermediary SDoH, which we conceptualize here as economic insecurity, are associated with worse patient-reported outcomes (PROs) in SLE even after accounting for conventional measures of SES. CLUES offers a unique opportunity to understand how economic insecurity may exert an effect beyond health insurance as all participants in the cohort have access to care through private insurance, universal health insurance in San Francisco, or the Medicaid expansion in California.9 We also evaluated whether poverty or education modified the association between economic insecurity and SLE outcomes, hypothesizing that economic insecurity may exacerbate the negative impact of low income and low educational attainment on PROs.
Methods
Subjects
All subjects were enrolled in CLUES, a cohort of racially and ethnically diverse participants that were recruited from the California Lupus Surveillance Project10 with additional recruitment from academic and community rheumatology clinics throughout the nine San Francisco Bay Area counties between February 2015 and January 2018. Inclusion criteria were Bay Area residency; ≥18 years of age; oral fluency in English, Spanish, Cantonese, or Mandarin; and ability to provide informed consent. All study procedures were approved by the UCSF Institutional Review Board, and all participants provided signed informed consent.
Study procedures involved an in-person research clinic visit, including collection and review of medical records prior to the visit; a history and physical examination conducted by a physician specializing in lupus; collection of biospecimens; and completion of a structured interview administered by an experienced research assistant. All SLE diagnoses were confirmed by study physicians based upon one of the following definitions used in prior California Lupus Surveillance Project and CLUES articles:10 (a) meeting ≥ 4 of the 11 American College of Rheumatology (ACR) revised criteria for the classification of SLE as defined in 1982 and updated in 1997,11 (b) meeting 3 of the 11 ACR criteria plus a documented rheumatologist’s diagnosis of SLE, or (c) a confirmed diagnosis of lupus nephritis, defined as fulfilling the ACR renal classification criterion (>0·5 grams of proteinuria per day or 3 + protein on urine dipstick analysis) or having evidence of lupus nephritis on kidney biopsy.
The study included 431 participants at baseline. Follow-up interviews have been conducted annually. All data for these analyses are from Year 5 interviews (February 2020 – March 2021), the first year in which information regarding economic insecurities was collected, unless noted below. Annual follow-up interview retention averaged 86%; however, between baseline and Year 5, 179 participants were lost to follow-up (including 14 deaths and all 21 Mandarin- and Cantonese-speaking participants, due to loss of language-concordant interviewer), leaving a sample size of 252 for these analyses. At the timepoint for these analyses, 10% (n=26) of the cohort self-identified as Black, 32% (n=80) as Asian, 14% (n=36) as Other, 3% (n=8) as Mixed race; 23% (n=59) self-identified as Hispanic, including all who self-identified as Other race.
Variables
Primary Predictors.
Our primary predictors were insecurities related to food, housing, general financial status, and ability to afford care for SLE. Housing insecurity was assessed with the 2013 Behavioral Risk Factor Surveillance System question “How often in the past 12 months would you say you were worried or stressed about having enough money to pay your rent/mortgage?”12 Answer options were never, rarely, sometimes, or always, with the latter two responses considered housing insecurity.
A validated brief assessment that asked how often the following statements were true assessed food insecurity: “Within the past 12 months we worried whether our food would run out before we got money to buy more,” and “Within the past 12 months the food we bought just didn’t last and we didn’t have money to get more.”13 Participants who answered either “always true” or “sometimes true” to either or both statements were classified as food insecure.
Financial insecurity was assessed with three questions.14 Participants rated their likelihood of experiencing actual hardships, having to reduce their standard of living to the bare necessities in the next two months, and their current difficulty living on their household income. Participants were characterized as financially insecure if they answered, “likely” or “somewhat” to any of the three items.
Inability to afford SLE care was assessed with the question, “How worried are you now that you may not be able to afford the care you need for your lupus in the next one to two years?” Response options were “not at all worried,” “somewhat worried,” and “very worried.” Participants were classified as SLE care insecure if they responded “somewhat” or “very worried.”
Covariates.
Covariates for multivariable regression analyses included demographic and SLE-specific variables. Basic demographic characteristics such as age, self-identified sex, and self-identified race and ethnicity were drawn from the baseline interview. SDoH covariates included poverty status (household income < or ≥125% of the federal poverty level based on household size), and education (< or ≥college-graduate education) collected in Year 5 and health literacy (dichotomized as limited or not limited15) collected at baseline. Number of major comorbid conditions (including cardiovascular disease, asthma, cancer, and diabetes, and obesity (defined as baseline body mass index kg/m2 ≥30) and SLE-specific clinical data, including SLE disease duration, moderate or high dose oral glucocorticoid use (prednisone ≥7·5mg/day or equivalent glucocorticoid), immunosuppressive medication use (yes/no), and hydroxychloroquine use (yes/no). were also collected from Year 5. At Year 4, accumulated SLE damage was assessed by the Brief Index of Lupus Damage (BILD), a validated patient-reported proxy for the Systemic Lupus International Collaborating Clinics/American College of Rheumatology Damage Index (SDI). Higher BILD scores indicate worse disease damage.
Outcomes.
We assessed the effect of economic insecurities on seven patient-reported outcomes. Four Patient Reported Outcomes Measurement Information System (PROMIS) short forms were administered to assess symptoms relevant to SLE — Physical Function, Pain Interference, Fatigue, and Sleep Disturbance.16 Minimally meaningful differences for these PROMIS scores have been estimated at ~2 points in SLE.17 The Neuro-QoL Cognitive Function short form was used to assess cognitive symptoms that are commonly reported in patients with SLE.18 All PROMIS and Neuro-QoL scales were scored as recommended and converted to T-scores with a population mean of 50 and standard deviation of 10, using PROMIS scoring documentation.
We also examined measures of depression and anxiety. The Patient Health Questionnaire (PHQ)-8 is an 8-item measure of depressive symptoms, scores >10 correspond with clinical diagnoses of depression. 19 The Generalized Anxiety Disorder (GAD)-7 is a validated 7-item screener for generalized anxiety disorder and can assess the severity of anxiety symptoms.20 For pain interference, fatigue, sleep disturbance, depression and anxiety, higher scores reflect worse health outcomes, whereas higher scores for physical function and cognitive function reflect better health outcomes.
All measures were available in English and Spanish.
Statistical Analysis.
We characterized the demographic and clinical characteristics of our cohort using means and standard deviations, median and interquartile range, or frequencies and proportions, as appropriate. The distribution of economic insecurities was calculated three ways: (1) binary indicator of any insecurity, (2) count of the number of insecurities experienced, and (3) stratification of our binary indicator by poverty and education. Differences in the distribution of PROs across these categories were tested for differences using independent-sample t-tests or one-way analyses of variance with Tukey post-hoc means tests, as appropriate. Missingness for all analytic variables and how it was handled is shown in Supplemental Table 1. Listwise deletion was performed for three observations for PROMIS Fatigue and one observation for other PROs.
Interactions between economic insecurities and poverty and education were operationalized using the cross-classification of our binary insecurity measure with our binary measures for poverty and education. Unadjusted differences in PROs by group were examined with analyses of variance with Tukey post-hoc means tests.
Differences in PROs were then examined in multivariable linear regression models, controlling for age, sex, race and ethnicity, poverty status, education, marital status, obesity, disease duration, disease damage (via BILD), comorbidities, and use of oral steroid, immunosuppressives, and hydroxychloroquine, and marginal adjusted means were calculated. To examine whether there was an interaction between insecurities and poverty status, the cross-classified measures of the binary insecurity measure with the binary poverty status measure were added to another set of regression analyses. We conducted a sensitivity analysis stratifying annual household income as < or ≥$60,000/year. A similar strategy was used to examine an interaction between insecurities and education. Sensitivity analyses assessed associations between individual insecurities and outcomes utilizing both unadjusted and adjusted models.
To ensure the appropriateness of models, we performed regression diagnostics for influential data, normality of residuals, homoscedasticity of residuals, multicollinearity, and non-linearity. All variance inflations factors (VIF) were <3, indicating lack of multicollinearity.
All analyses used Stata SE 17.0 software (StataCorp LLC, College Station, Texas). P-values ≤ 0.05 were considered statistically significant. Our study conforms to the STROBE (strengthening the reporting of observational studies in epidemiology) checklist for observational studies.
Role of the funding source:
The funder had no role in study design, data collection, data analysis, data interpretation, or the decision to submit this manuscript for publication. KB and KG, both employees of the funder, reviewed drafts of the manuscript.
Results
The average age of the cohort at Year 5 was 49·7±13.4 years, with average SLE duration of 22·4±10.7 years, and 90% (n=228) of the cohort self-identified as women (Table 1). Approximately 12% (n=29) reported household incomes below poverty, and approximately 16% reported education less than college (n=39). Individuals who had been lost to follow-up prior to Year 5 were older (48 ±15 years vs. 45 ±13 years) and more commonly had incomes below poverty (27%; n=42 vs. 14%; n=33), but there were no significant differences at baseline in sex, race, comorbid conditions, SLE disease activity or damage, or the PROs (Supplemental Table 2).
Table 1:
Participant characteristics (n = 252)
| Mean ± SD or % (n) | |
|---|---|
| Sociodemographic characteristics | |
| Age, years· | 49·7 ± 13·4 |
| Female | 91 (228) |
| Male | 9 (24) |
| Race | |
| Asian | 32 (80) |
| Black | 10 (26) |
| White | 40 (101) |
| Mixed | 3 (8) |
| Other | 14 (36) |
| Hispanic ethnicity | 23 (59) |
| Income below poverty | 12 (29) |
| Education | |
| Less than high school | 5 (12) |
| High school degree | 11 (27) |
| Some college | 15 (38) |
| Associate degree, trade school | 14 (36) |
| College/university degree | 31 (78) |
| Post-graduate, professional | 24 (60) |
| Married | 57 (143) |
| Patient-reported outcomes (PROs) | |
| PROMIS Physical Function | 47·2 ± 9·8 |
| PROMIS Pain Interference | 53·3 ± 9·7 |
| PROMIS Fatigue | 52·9 ± 10·6 |
| PROMIS Sleep Disturbance | 51·2 ± 9·2 |
| NeuroQoL Cognitive Function | 47·3 ± 9·7 |
| PHQ-8 (depressive symptoms) Median (IQR) |
5·3 ± 4·5 5 (2, 8) |
| GAD-7 (anxiety) Median (IQR) |
4·3 ± 4·4 3 (1, 6) |
| General health characteristics | |
| Number of comorbid conditions Median (IQR) |
2·0 ± 1·7 2 (1,3) |
| Obesity (BMI ≥30) | 25 (63) |
| SLE-related | |
| SLE disease duration (years) | 22·4 ± 10·7 |
| SLE disease damage (BILD) Median (IQR) |
2·5 ± 2·4 1 (0, 3) |
| Medications | |
| High-dose glucocorticoids | 14 (35) |
| Hydroxychloroquine | 65 (163) |
| Immunosuppressives | 51 (129) |
Race and ethnicity categories are mutually exclusive.
BILD= Brief Index of Lupus Damage: BMI= body mass index; GAD-7= General Anxiety Disorder-7; PHQ-8= Patient Health Questionnaire-8; PROMIS= Patient-reported Outcomes Measurement Information System; SLE= systemic lupus erythematosus
Frequency of economic insecurities.
Housing insecurity was reported by 23% (57/252) of the cohort, food insecurity by 17% (43/252), financial insecurity by 21% (53/252), and worry about paying for SLE care by 42% (106/252) (Table 2). Over half (54%,135/252) of the respondents reported experiencing at least one insecurity, and over one quarter (72/252) reported two or more. Insecurities were significantly more common among individuals with poverty-level income (79% [23/29] of participants below poverty compared to 49% [100/206] of participants above poverty reported any insecurity) and lower education (72% [81/113] compared to 39% [54/138] with higher education). Worry about paying for SLE care did not differ by poverty status with 40% (82/206) of participants above poverty and 48% (14/29) below poverty worried about paying for the SLE care.
Table 2:
Frequency of reports of economic insecurities, total and by income and education
| Poverty | Lower education (<college degree) | ||||||
|---|---|---|---|---|---|---|---|
| Insecurities | Total % (n) | No (n = 206) % (n) | Yes (n = 29) % (n) | p* | No (n = 138) % (n) | Yes (n = 113) % (n) | p* |
| Housing | 23 (57) | 19 (39) | 41 (12) | 0·0060 | 12 (16) | 36 (41) | <0·0001 |
| Financial | 21 (53) | 16 (32) | 55 (16) | <0·0001 | 11 (15) | 34 (38) | <0·0001 |
| Food | 17 (43) | 12 (25) | 45 (13) | <0·0001 | 9 (12) | 27 (31) | <0·0001 |
| SLE care | 42 (106) | 40 (82) | 48 (14) | 0·42 | 31 (43) | 56 (63) | <0·0001 |
| Any of the above | 55 (135) | 49 (100) | 79 (23) | 0·0019 | 39 (54) | 72 (81) | <0·0001 |
| Number of insecurities | |||||||
| 0 | 46 (117) | 52 (106) | 21 (6) | 0·0002 | 61 (84) | 28 (32) | <0·0001 |
| 1 | 25 (63) | 26 (53) | 21 (6) | 24 (33) | 27 (30) | ||
| ≥ 2 | 29 (72) | 23 (47) | 59 (17) | 15 (21) | 45 (51) | ||
SLE=systemic lupus erythematosus·
p-values from chi-square analyses
Unadjusted analyses of PROs.
Unadjusted analyses examining the relationships between economic insecurities and PROs revealed significant differences between those with and without any economic insecurity and by the number of insecurities for all PROs. In all cases, economic insecurities were significantly associated with worse self-reported health outcomes. Across PROs the magnitude of the differences between none and any insecurity generally exceeded minimally meaningful differences for each scale. When considering the number of insecurities, differences were even larger. Examining the point estimates in analyses based on the number of insecurities, there appeared to be a stepwise effect with the worst outcomes among the group experiencing two or more economic insecurities (Table 3). In contrast, the only statistically significant differences by poverty status were for physical function and pain interference. Results of sensitivity analyses using income instead of poverty status (Supplemental Table 4) were not substantially different. Significant differences were also noted by education, with the lower education group having worse scores on all PROs. Differences in PROs by the individual insecurity measures are shown in Supplemental Table 5. Nearly all PROs were significantly worse for participants with each of the individual insecurities.
Table 3:
Unadjusted differences in PROs by insecurities, income, and education
| Physical Functiona | Pain Interferenceb | Fatigueb | Sleep Disturbanceb | Cognitive Functiona | Depressionb | Anxietyb | |
|---|---|---|---|---|---|---|---|
|
| |||||||
| Any insecurity | |||||||
| No (n=117) | 50·4 ± 0·7 | 50·7 ± 9·2 | 49·5 ± 10·0 | 49·4 ± 9·0 | 50·2 ± 8·9 | 3·9 ± 4·0 | 2·9 ± 3·6 |
| Yes (n=135) | 44·4 ± 8·9 | 55·5 ± 9·5 | 55·8 ± 10·2 | 53·3 ± 9·1 | 44·8 ± 8·8 | 6·5 ± 4·6 | 5·5 ± 4·7 |
| p | <0·0001 | <0·0001 | <0·0001 | 0·0008 | <0·0001 | <0·0001 | <0·0001 |
| Number of insecurities | |||||||
| 0 (n = 117) | 50·4 ± 0·7 | 50·7 ± 9·2 | 49·5 ± 10·0 | 49·4 ± 9·0 | 50·2 ± 8·9 | 3·9 ± 4·0 | 2·9 ± 3·6 |
| 1 (n = 63) | *46·1 ± 9·3 | *54·6 ± 9·5 | *55·1 ± 10·8 | 52·6 ± 9·2 | *46·0 ± 9·9 | *6·2 ± 4·6 | *4·7 ± 4·1 |
| ≥2 (n = 72) | *42·9 ± 8·4 | *56·3 ± 9·6 | *56·3 ± 9·7 | *54·0 ± 9·0 | *43·8 ± 7·8 | *6·8 ± 4·6 | *6·2 ± 5·1 |
| p | <0·0001 | 0·0002 | <0·0001 | 0·0024 | <0·0001 | <0·0001 | <0·0001 |
| Poverty | |||||||
| No (n = 206) | 48·0 ± 9·7 | 52·7 ± 9·5 | 52·3 ± 10·7 | 51·2 ± 8·9 | 47·8 ± 9·3 | 5·1 ± 4·4 | 4·2 ± 4·3 |
| Yes (n = 29) | 42·1 ± 8·6 | 57·0 ± 10·1 | 55·3 ± 10·6 | 52·2 ± 11·3 | 44·8 ± 9·6 | 6·2 ± 5·5 | 5·2 ± 4·9 |
| p | 0·002 | 0·02 | 0·17 | 0·59 | 0·097 | 0·24 | 0·26 |
| Lower education (<college degree) | |||||||
| No (n = 138) | 49·5 ± 9·5 | 51·4 ± 9·5 | 51·6 ± 10·6 | 50·6 ± 8·4 | 48·3 ± 9·2 | 4·7 ± 4·2 | 3·7 ± 4·1 |
| Yes (n = 113) | 44·3 ± 9·3 | 55·6 ± 9·4 | 54·6 ± 10·4 | 52·8 ± 10·0 | 46·0 ± 9·3 | 6·1 ± 4·8 | 5·0 ± 4·7 |
| p | <0·0001 | 0·0005 | 0·026 | 0·056 | 0·042 | 0·012 | 0·020 |
| Any insecurity x income | |||||||
| No insecurity + no poverty (n = 111) | 50·9 ± 9·5 | 50·3 ± 8·9 | 49·1 ± 9·9 | 49·7 ± 8·8 | 50·4 ± 8·8 | 3·7 ± 3·6 | 2·9 ± 3·6 |
| No insecurity + poverty (n = 6) | 41·9 ± 10·6 | 58·6 ± 11·5 | 56·4 ± 10·2 | 45·3 ± 13·2 | 45·9 ± 10·7 | 8·2 ± 8·3 | 2·8 ± 3·8 |
| Insecurity + no poverty (n = 112) | *44·9 ± 9·0 | *55·3 ± 9·5 | *55·9 ± 10·1 | *53·2 ± 8·8 | *44·9 ± 8·7 | *6·7 ± 4·6 | *5·5 ± 4·6 |
| Insecurity + poverty (n = 23) | *42·1 ± 8·2 | *56·7 ± 10·0 | 55·0 ± 10·9 | 54·0 ± 10·4 | *44·5 ± 9·6 | 5·6 ± 4·6 | *5·8 ± 5·1 |
| p | <0·0001 | <0·0001 | <0·0001 | 0·0018 | <0·0001 | <0·0001 | <0·0001 |
| Any insecurity x education | |||||||
| No insecurity + higher education (n = 84) | 51·8 ± 9·2 | 49·6 ± 8·9 | 49·1 ± 9·9 | 49·9 ± 8·5 | 50·6 ± 9·1 | 3·8 ± 3·8 | 3·0 ± 3·7 |
| No insecurity + lower education (n = 32) | *46·5 ± 10·1 | 53·8 ± 9·4 | 50·7 ± 10·6 | 48·5 ± 10·5 | 48·9 ± 8·7 | 4·3 ± 4·8 | 2·8 ± 3·4 |
| Insecurity + higher education (n = 54) | *45·8 ± 9·0 | *54·2 ± 9·7 | *55·3 ± 10·7 | 51·6 ± 8·4 | *44·8 ± 8·3 | *6·1 ± 4·5 | *4·9 ± 4·4 |
| Insecurity + lower education (n = 81) | *43·4 ± 8·9 | *56·4 ± 9·4 | *56·0 ± 9·9 | *54·5 ± 9·4 | *44·8 ± 9·3 | *6·8 ± 4·7 | *5·9 ± 4·9 |
| p | <0·0001 | <0·0001 | <0·0001 | 0·0020 | <0·0001 | <0·0001 | <0·0001 |
Data are mean ± SD· Differences in group means were tested with t-tests or analyses of variance.·
Significantly different from “No insecurity, income>poverty/high education” group based on post-hoc means test·
Higher scores reflect better outcomes
Higher scores reflect worse outcomes
In unadjusted models of the insecurity–poverty groups, overall significant differences between groups were noted for each PRO. In each case, the post-hoc means test indicated differences between one or both insecurity groups (either “insecurity+no poverty” or “insecurity+poverty”) and the “no insecurity+no poverty” group. Similar results were noted for the insecurity–education group analysis. These results are contrary to our hypothesis that poverty and low education would exacerbate effects of insecurities on outcomes. Rather, we see an effect of economic insecurity regardless of low SES (either poverty or low education).
Adjusted analyses.
After adjustment for covariables, including poverty status, education, and health literacy, individuals with any insecurity had significantly worse scores on all PROs: Physical Function, no insecurity 48·9 (47·5, 50·3) vs. any insecurity 45·7 (44·3, 47·0); Pain Interference, 52·0 (50·5, 53·5) vs. 54·4 (53·0, 55·8); Fatigue, 50·5 (48·8, 52·3) vs. 54·9 (53·3, 56·5); Sleep Disturbance, 49·9 (48·3, 51·6) vs. 52·9 (51·4, 54·5); Cognitive Function, 49·3 (47·7, 50·9) vs. 45·6 (44·1, 47·0); PHQ-8, 4·4 (3·6, 5·1) vs. 6·1 (5·4, 6·8); and GAD-7, 3·3 (2·6, 4·1) vs. 5·2 (4·5, 5·9). (Figure 1). The magnitude of the difference between groups now ranged from 2–4 points; while smaller than our unadjusted models, these are still meaningful differences (Supplemental Table 3). Differences by the number of insecurities showed significantly worse scores for individuals with one and ≥2 insecurities compared to individuals with no insecurities except for sleep disturbance (Figure 2). There was not a clear association between individual economic insecurities and PROs in adjusted analyses (Supplemental Table 5), although housing and financial insecurity were associated with worse physical functioning and anxiety symptoms. We did not find interactions between insecurities and either poverty status or education.
Figure 1: Adjusted marginal means from multivariable analysis, by any insecurity.
Adjusted means (95% confidence interval) calculated from multivariable linear regression analyses controlling for age, sex, race and ethnicity, marital status, education, income, health literacy, comorbid conditions, obesity, disease duration, disease damage, high glucocorticoid use, immunosuppressive use, and hydroxychloroquine use.·
P values from multivariable linear regression, compared to no insecurities group·
PHQ-8 = Patient Health Questionnaire, measure of depressive symptoms
GAD-7 = Generalized Anxiety Disorder questionnaire
Figure 2: Adjusted marginal means from multivariable analysis, by number of insecurities.
Adjusted means (95% confidence interval) calculated from multivariable linear regression analyses controlling for age, sex, race and ethnicity, marital status, education, income, health literacy, comorbid conditions, obesity, disease duration, disease damage, high glucocorticoid use, immunosuppressive use, and hydroxychloroquine use.·
P values from multivariable linear regression, compared to no insecurities group·
PHQ-8 = Patient Health Questionnaire, measure of depressive symptoms
GAD-7 = Generalized Anxiety Disorder questionnaire
Discussion
In this study of the relationship between economic insecurities – an important emerging concept in the SDoH literature – and patient-reported outcomes in a diverse group of individuals with SLE, we found that economic insecurities were highly prevalent, with over half of participants reporting at least one insecurity, such as concern about paying for food, housing, or SLE medical care. The presence of any insecurity was associated with worse PROs across a broad range of domains. These relationships were observed even after accounting for sociodemographic factors, poverty status, education, health literacy, comorbidities, SLE disease damage, and lupus medications.
This study expands the growing knowledge base regarding the relationship between social determinants of health and outcomes in SLE, a condition with significant health disparities. Previous studies have demonstrated that more commonly considered SDoH, such as poverty, lower educational attainment, or health insurance coverage, are associated with worse outcomes in SLE. Within a broader SDoH framework, we build on this previous work by examining several additional SDoH in the area of economic insecurity. Interestingly, we found that economic insecurities were not limited to individuals living in poverty; almost half of those with incomes above poverty reported at least one insecurity. Additionally, we did not find that a specific type of insecurity drove the association with outcomes; instead, we saw the strongest effects among those with the highest number of insecurities of any type. These results held after controlling for poverty, education level, health literacy, and a host of clinical indicators and indicate that economic insecurities are a unique risk factor for poor health outcomes in SLE.
Building on our previous qualitative study, we hypothesized that economic insecurities would exacerbate the deleterious effects of poverty and that higher education would ameliorate the effects of economic insecurities. We did not find support for either hypothesis: there was no significant direct effect of poverty on most of the PROs examined.21 While our sample size precluded examination of more granular income brackets and results need to be replicated in larger samples, we found that differences in outcomes were primarily due to insecurities, suggesting that traditional income thresholds do not adequately capture the total effect of low SES. Our study was conducted in the San Francisco Bay Area which has a high cost of living and may explain why economic insecurities have a stronger relationship with outcomes than poverty and educational achievement. There are likely factors at the macro, meso and micro level that may impact levels of economic insecurity including the housing supply, physical access to food, neighborhood characteristics, accessibility of transportation and disability status.22,23
We did, however, find strong direct effects for education, consistent with existing literature.21 The pattern of results for education and any insecurity suggests that the effect of education was confounded by economic insecurities rather than an interaction between the two. Respondents in the previous qualitative study narrated how social connections, a form of social support, via higher education helped them navigate the healthcare system.5 More direct measures of social support may modify the deleterious effects of economic insecurities and should be the subject of future investigations. In addition, work remains to establish the contexts in which economic insecurities have the strongest (or any) effect.5,22,23
The pattern of economic insecurities seen in this study is consistent with that observed in other chronic diseases, such as diabetes mellitus (DM). For example, in a study of the relationship between economic insecurities and diabetes, 19% of the study cohort reported food insecurity (compared to 17% in CLUES).24 For context, the total prevalence of adults living in households with food insecurity was markedly lower at 10% in 2021.25 Additionally, the association we found between insecurities and outcomes is consistent with findings from studies examining economic insecurities and diabetes management. For example, having food insecurity was associated with increased HbA1c and worse depression and anxiety symptoms.24,26
There are several mechanisms that may explain the association of SDoH with SLE outcomes. We found evidence for an additive effect of insecurities suggesting that studying interventions across the broad domains examined may be needed to improve SLE health outcomes. To illustrate, housing and financial insecurity can create difficulties with obtaining, storing, and regularly taking medications or accessing health care for chronic conditions such as SLE.27 Additionally, economic insecurities may be associated with both depression and anxiety symptoms via chronic stress. For example, in the context of diabetes, researchers observed that food insecurity increased stress and depression thereby worsening diabetes outcomes through impaired self-care practices.28 Whether the effects of these insecurities on psychological outcomes was modified in the presence of SLE warrants further study.
This study has limitations. We could not examine additional factors that may impact economic insecurities such as disability status, accessibility of transportation, physical access to food, housing supply, and neighborhood characteristics.22,23 Our measures of financial insecurity and SLE care insecurity asked about anticipated needs rather than an inability to pay for medications as others have.24 These are not fully equivalent, but we believe these measures still reflect the psychological aspect of these concerns and likely reflect at least partially an inability to pay for food, housing, or medications. Our measures also assessed insecurities over varying time frames. A portion of the original CLUES sample was lost to follow-up. Importantly, participants lost to follow-up were more likely to be below the poverty level, which may impact the internal and external validity of the study. As we collected our primary exposure (economic insecurities) at Year 5, we were unable to perform sensitivity analyses on this group as it is missing both exposure and outcome data (PROs). However, there were no significant differences in any of the other demographic characteristics or baseline PROs between individuals who were and were not lost to follow-up. Our cohort was based in California; the demographics and sociopolitical context of the area limits the generalizability of our findings outside this region. Our cohort was also relatively highly educated; in a cohort with greater diversity in educational attainment, our results may have differed. Other limitations of our study include unmeasured confounding, possible exposure-confounder feedback, and potential residual confounding secondary to measurement errors in confounders such as education and disease duration.
The study also has significant strengths, including our cohort’s universal access to healthcare via regional policy.9 Access to care is critical to proper management of SLE but access is not the same the ability to afford proper care for a complex chronic disease like SLE, particularly in the American healthcare system in which individuals with health insurance may still have large out-of-pocket costs. This unique characteristic of the CLUES cohort removed confounding between those with and without insurance and allowed us to examine the impact of economic insecurities on outcomes above and beyond the access to care afforded by health insurance. In this vein, our analyses found that SLE care insecurity did not correspond with poverty status. One potential reason for these findings is that Medicaid, the U.S. insurance program for those with low incomes, provides a drug low-income subsidy so that payment for expensive medications including biologics, is only a few dollars a month, unlike for individuals with other types of insurance where drug costs can run high.
Overall, this study provides one of the most comprehensive examinations of the relationship between an important subset of SDoH – economic insecurities – and SLE outcomes. Our findings suggest that economic insecurities are highly prevalent and impactful exposures for those living with SLE. Having any of the insecurities examined was associated with worse outcomes across a breadth of domains. Importantly, many of these economic insecurities are modifiable with the appropriate interventions, such as long-term rent subsidies, child tax credits, and food programs.29 Although likely challenging to conduct, studies examining the impact and cost-effectiveness of interventions that address economic insecurity are needed given the striking health disparities in SLE. Increased recognition of the importance of these social exposures and knowledge of available resources to provide for patients experiencing economic insecurity may have potential to improve outcomes for those living with SLE.
Supplementary Material
Research in context.
Evidence before this study.
We searched PubMed for observational studies of SLE from 2008 to the present using the search terms “poverty”, “socioeconomic”, and “systemic lupus erythematosus”. Pre-existing literature on the relationship between socioeconomic factors and SLE outcomes consisted of cross-sectional analyses of varying SLE cohorts including the California Lupus Surveillance Project, California Lupus Epidemiology Study and Lupus Outcomes Study. These studies demonstrate that low income, low educational attainment, and a lack of health insurance are among the social determinants of health (SDoH) associated with poorer SLE outcomes. However, there are additional SDoH, including economic insecurities, that may impact SLE patient-reported outcomes above and beyond income, education, and health insurance. A qualitative study revealed the self-reported impact of economic insecurities related to food, housing, medical care, and finances on patients’ management of SLE.
Added value of this study
In this cross-sectional SLE study, we demonstrated that economic insecurities related to food, housing, medical care, and finances, contribute to poor SLE outcomes, even after accounting for factors such as having health insurance, health literacy, poverty, and education. These results further our understanding of the relationship between SDoH and SLE outcomes, and identify economic insecurities as an area for further mechanistic investigation.
Implications of all the available evidence
Economic insecurity is an emerging concept in research examining SDoH and their relationship to disease outcomes. In this study, we show that economic insecurity with regard to food, housing, healthcare and finances is associated with worse outcomes for people with SLE regardless of poverty, education, health literacy, or health insurance status. Findings provide further insight into the relationship between economic insecurity and SLE outcomes and warrant further research into the mechanisms underpinning this association. From a clinical perspective, our study underscores the need to study whether interventions that directly address economic insecurities can reduce health disparities in this disease.
Funding:
Supported by the Centers for Disease Control (Grant 5U01DP005120 and Grant U48DP006374), NIH (National Institute of Arthritis and Musculoskeletal and Skin Diseases grants P30-AR-070155 and K24AR074534), Robert L. Kroc Chair and Alice Betts Chair in Rheumatic and Connective Tissue Diseases, and Russell/Engleman Medical Research Center for Arthritis.
Sources of funding
This study was funded by grants from the Centers for Disease Control and Prevention (U01DP006701 and U48DP006374) and a grant from the Rheumatology Research Foundation.
Disclosures:
Dr. Yazdany has received research grant funding from Gilead, Astra Zeneca, BMS Foundation, and Aurinia. She has performed consulting for Astra Zeneca, Pfizer and Aurinia. Dr Gordon has received consultancy fees from Alumis, Amgen, Astra-Zeneca, Sanofi, UCB (in the last 3 years).
Footnotes
CDC Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Declaration of interests
Mr. Sandoval-Heglund, Dr. Roberts, Mr. Park, Dr. Dall’Era, Dr. Lanata, Dr. Barbour, and Dr. Greenlund declare no actual or perceived conflicts of interest.
Dr. Gordon declares consulting fees from Amgen, UCB, Astra Zeneca, and Alumis.
Dr. Katz declares grant support for this manuscript from the following sources: CDC U01DP006701 and U48DP006374.
Dr. Yazdany declares grant support for this manuscript from the following sources: NIH/NIAMS K24 AR074534, CDC U01DP006701, and NIH/NIAMS P30 AR070155. She also declares research grants from the following: Gilead, Astra Zeneca, and BMS Foundation, and consulting fees from Astra Zeneca, Aurinia, Pfizer, and Adelphi Values. She is the research lead for the RISE registry for the American College of Rheumatology.
No individuals other than the listed authors contributed to this work.
Data sharing
Deidentified participant data that underlie these analyses and data codebooks will be made available to academic researchers upon request and in accordance with institutional data sharing guidelines, which will require a formal signed data access agreement. Study questionnaires used to collect data will also be available.
Data will be available beginning at the time of publication and ending 36 months following article publication.
Requestors must submit a formal request, including a proposal for analysis and variables requested. Proposals for new analyses and requests for data for meta-analyses will be considered. Requests will be reviewed by the CLUES executive committee.
Costs for any data preparation will be the responsibility of the requestor.
Datasets may be conveyed by email or other secure transmission method.
References
- 1.Izmirly P, Parton H, Wang L, et al. Prevlanece of systemic lupus erythematosus in the United States: estimates from a meta-analysis of the Centers for Disease Control and Prevention national lupus registries. Arthritis Rheumatol 2021; 73: 991–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.DeQuattro K, Yelin E. Socioeconomic status, health care, and outcomes in systemic lupus erythematosus. Rheum Dis Clin North Am 2020; 46(639–649). [DOI] [PubMed] [Google Scholar]
- 3.Artiga S, Hinton E. Beyond health care: the role of social determinants in promoting health and health equity. 2018. https://files.kff.org/attachment/issue-brief-beyond-health-care (accessed August 24, 2023. [Google Scholar]
- 4.Yelin E, Trupin L, Yazdany J. A prospective study of the impact of current poverty, history of poverty, and exiting poverty on accumulation of disease damage in systemic lupus erythematosus. Arthritis Rheumatol 2017; 69: 1612–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yelin E, Yazdany J, Trupin L. Relationship between poverty and mortality in systemic lupus erythematosus. Arthritis Care Res 2018; 70: 1101–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.González-Naranjo L, Ugarte-Gil M, Alarcón G. Socioeconomic aspects of systemic lupus erythematosus. In: Tsokos G, editor. Systemic Lupus Erythematosus. Cambridge, MA: Academic Press; 2016. p. 39–42. [Google Scholar]
- 7.Yelin E, Trupin L, Bunde J, Yazdany J. Poverty, neighborhoods, persistent stress, and SLE outcomes: a qualitative study of the patients’ perspective. Arthritis Care Res 2019; 71: 398–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization. A conceptual framework for action on the social determinants of health. . 2010. https://www.who.int/publications/i/item/9789241500852.
- 9.Jacobs K, Lucia L. Universal health care: lessons from San Francisco. Health Affairs 2018; 37: 1375–82. [DOI] [PubMed] [Google Scholar]
- 10.Dall’Era M, Cisternas M, Snipes K, Herrinton L, Gordon C, Helmick C. The incidence and prevalence of systemic lupus erythematosus in San Francisco County, California. Arthrits Rheum 2017; 69: 1996–2005. [DOI] [PubMed] [Google Scholar]
- 11.Hochberg MC. Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 1997; 40(9): 1725. [DOI] [PubMed] [Google Scholar]
- 12.Stahre M, VanEenwyk J, Siegel P, Njal R. Housing insecurity and the association with health outcomes and unhealthy behaviors, Washington State, 2011. Prev Chronic Dis 2015; 12: 140511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gunderson C, Engelhard E, Crumbaugh A, Seligman H. Brief assessment of food insecurity accurately identifies high-risk US adults. Public Health Nutr 2017; 20: 1367–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vinokur A, Price R, Caplan R. Hard times and hurtful partners: how financial strain affects depression and relationship satisfaction of unemployed persons and their spouses. J Pers Soc Psychol 1996; 71: 166–79. [DOI] [PubMed] [Google Scholar]
- 15.Katz P, Dall’Era M, Trupin L, et al. The impact of limited health literacy on patient-reported outcomes in systemic lupus erythematosus. Arthritis Care Res 2021; 73: 110–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cella D, Yount S, Rothrock N, et al. The Patient-Reported Outcomes Measurement Information System (PROMIS): progress of an NIH Roadmap cooperative group during its first two years. Med Care 2007; 45 (5 Suppl 1): S3–S11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Katz P, Pedro S, Alemao E, et al. Estimates of responsiveness, minimally important differenes, and patient acceptable symptoms state in five Patient-Reported outcomes Measurement Information System short forms in systemic lupus erythematosus. ACR Open Rheumatology 2020; 2: 53–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gershon R, Lai J, Bode R, et al. Neuro_QOL: quality of life item banks for adults with neurological disorders: item development and calibrations based upon clinical and general population testing. Qual Life Res 2012; 21: 475–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kroenke K, Strine T, Spitzer R, Williams J, Mokdad A. The PHQ-8 as a measure of current depression in the general population. J Affective Disorders 2009; 114: 163–73. [DOI] [PubMed] [Google Scholar]
- 20.Spitzer R, Kroenke K, Williams J, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 2006; 166: 1092–7. [DOI] [PubMed] [Google Scholar]
- 21.Astrike-Davis E, Cleveland R, Bridges S, Jonas B, Callahan L. Associations of socioeconomic status with disease progression in African Americans with early rheumatoid arthritis. Arthritis Care Res 2023; 75: 85–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ploeg M, Breneman V, Farrigan T, et. Access to affordable and nutritious food: measuring and understanding food deserts and their consequences: Report to Congress, 2009. [Google Scholar]
- 23.Zenk S, Schulz A, Israel B, James S, Bao S, Wilson M. Neighborhood racial composition, neighborhood poverty, and the spatial accessibility of supermarkets in metropolitan Detroit. Am J Public Health 2005; 95: 660–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Berkowitz S, Meigs J, DeWalt D, et al. Material need insecurities, control of disabetes mellitus, and use of health care resources: results of the measuring economic Insecurity in diabetes study. JAMA Intern Med 2015; 175: 257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Coleman-Jensen A, Rabbitt M, Gergory C, Singh A. Household food security in the United States in 2021: U.S. Department of Agriculture, Economic Research Service, 2022. [Google Scholar]
- 26.Leung C, Heisler M, Patel M. Multiple social risk factors are associated with diabetes management and psychosocial outcomes among adults with diabetes. Prev Med Rep 2022; 29: 101957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fernandez S, Lopez C, Ibarra C, Sheehan D, Ladner R, Trepka M. Examining barriers to medication adherence and retention in care among women living in HIV in the face of homelessness and unstable housing. Int J Environ Res Public Health 2022; 19: 11484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Walker R, Campbell J, Egede L. Differential impact of food insecurity, distress, and stress on self-care behaviors and glycemic control using path analysis. J Gen Intern Med 2019; 34: 2779–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Oronce C, Miake-Lye I, Begashaw M, Booth M, Shrank W, Shekelle P. Interventions to address food insecurity among adults in Canada and the US. JAMA Health Forum 2021; 2: e212001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.