Summary
Background
There is ongoing uncertainty about whether cannabis use increases the risk of developing an anxiety disorder. In this study we estimated the risk of having an incident healthcare visit for an anxiety disorder following an emergency department (ED) visit for cannabis use and explored factors associated with increased risk.
Methods
We used health administrative data to perform a population-based cohort study of all individuals aged 10–105 years with no previous healthcare visits for anxiety disorders in Ontario, Canada, between January 2008 and March 2019. We compared the risk of having an incident healthcare visit for an anxiety disorder in the ED or hospital (primary analysis) or additionally in an outpatient setting (secondary analysis) for individuals with an incident ED visit for cannabis to members of the general population using cumulative incidence functions and cause-specific hazard models adjusted for relevant confounders.
Findings
Our study included 12,099,144 individuals aged 10–105 without prior care for an anxiety disorder in the ED or hospital, of which 34,822 (0.29%) had an incident ED visit due to cannabis. Within 3-years of an incident ED visit due to cannabis, 12.3% (n = 4294) of individuals had an incident ED visit or hospitalization for an anxiety disorder—a 3.7-fold (adjusted Hazard Ratio [aHR] 3.69 95% CI 3.57–3.82) increased risk relative to the general population (1.2%). In secondary analysis, further excluding individuals with prior outpatient care for anxiety disorders, 23.6% of individuals with an ED visit due to cannabis had an incident outpatient visit, ED visit, or hospitalization for an anxiety disorder within 3-years compared to 5.6% of individuals in the general population (aHR 3.88 95% CI 3.77–2.99). The risk of having an incident healthcare visit for an anxiety disorder was higher in individuals with ED visits for cannabis use compared to the general population across all age and sex strata. However, younger males with ED visits for cannabis use (aHR 5.67 95% CI 5.19–6.21) had a greater risk relative to the general population than younger women with cannabis use (aHR 3.22 95% CI 2.95–3.52).
Interpretation
ED visits for cannabis use were associated with an increased risk of having an incident healthcare visit for an anxiety disorder, particularly in young males. These findings have important clinical and policy implications given the increasing use of cannabis over time and trend towards legalization of cannabis.
Funding
Canadian Institutes for Health Research.
Keywords: Cannabis, Cannabis use disorder, Anxiety, Anxiety disorder, Cohort study, Health administrative data
Research in context.
Evidence before this study
We searched PubMed for studies published up to October 2, 2023, for scientific papers that examined cannabis use as a risk factor for the development of anxiety. The search terms used were “anxiety”, “anxiety disorders”, “marijuana”, “cannabis”, with no limits applied to language or publication date. Our search identified three meta-analyses and one systematic review which examined the relationship between cannabis use and anxiety. Most studies investigated the cross–sectional association between cannabis use and anxiety and reported an increased prevalence of cannabis use in individuals with anxiety and anxiety disorders. In a subset of studies examining only studies with a longitudinal design, there was mixed evidence about whether cannabis use was significantly associated with an increased risk of being diagnosed with an anxiety disorder, for both the general population and adolescents.
Much of the evidence on the association between cannabis use and anxiety comes from small studies using random samples of the general population or youth and young adults. Across all studies in the systematic reviews, there were just over 100,000 individuals. Included studies had large variations in measures of cannabis use ranging from lifetime use to meeting criteria for a cannabis use disorder. Similarly, definitions of anxiety varied considerably, and anxiety symptoms and severity were determined by self-report rather than diagnosis by a health care provider. We found no studies using health administrative data at the population-level to examine the longitudinal association between healthcare visits for cannabis use and the future development of an anxiety disorder.
Added value of this study
Using linked health administrative data capturing all healthcare use for over 12 million individuals residing in the province of Ontario, Canada, we completed the largest assessment of the longitudinal relationship between cannabis use and anxiety in the literature. We used physician-based identification of emergency department (ED) care for cannabis use and outpatient, ED, and hospital-based care for anxiety disorders. We found that individuals with an ED visit for cannabis use were at over 3-fold increased risk of having an incident ED visit, hospitalization or outpatient visit for an anxiety disorder within 3-years of their visit relative to the general population. In a sensitivity analysis excluding all individuals with prior healthcare for any mental health or substance use disorders, an ED visit for cannabis use was associated with over a 9-fold increased risk of having an incident healthcare visit for an anxiety disorder relative to the general population. These elevations in risk were consistent across the lifecycle but greatest for younger men.
Implications of all the available evidence
Our study extends the existing literature on the association between cannabis use and anxiety disorders, which to date has used self-report for both exposures and outcomes and relied on small samples and survey-based designs. Our results suggest that individuals with cannabis use requiring ED treatment may be at increased risk of developing an anxiety disorder or experiencing worsening anxiety symptoms. These findings have important implications for clinical practice and policymaking, considering the growing prevalence of cannabis use and the ongoing trend toward liberalization of cannabis policy.
Introduction
Cannabis use is increasing globally, and is the third most commonly used drug after alcohol and nicotine.1 At the same time, the potency of cannabis (i.e., tetrahydrocannabinol [THC] concentration) has also increased markedly.2 There is concern that legalization in countries such as Canada (the site of this study) and particularly commercialization of cannabis—allowing widespread retail access and promotion to cannabis–may result in further increases in cannabis use and associated harms.3, 4, 5 Cannabis use is associated with reductions in certain cognitive domains and the development of several major psychiatric illnesses, with the largest body of evidence being for psychosis2,6, 7, 8 Increasing evidence also suggests an association between cannabis use and mood disorders and self-harm and suicidality.2,9,10 Importantly, while cannabis use has long been hypothesized as a risk factor for the development of problems with anxiety and anxiety disorders, evidence on this topic is limited and mixed.
Multiple studies have found that cannabis use and withdrawal can induce acute anxiety symptoms.11 However, the relationship between cannabis use and the development of anxiety disorders is less clear. A meta-analysis found an increased prevalence of cannabis use in individuals with anxiety and anxiety disorder.12 A systematic review of modifiable causes of anxiety did not support cannabis as a risk factor.13 A meta-analysis including 10 longitudinal studies found mixed results on studies with an overall weak positive association between cannabis use and self-reported severity of anxiety symptoms.14 A meta-analysis of three studies specific to adolescence found no relationship between cannabis use and future risk of anxiety during adulthood. The current literature has a number of important limitations, including; non-population-based studies, the use of a wide variety of measures for cannabis use which may have less clinical relevance (e.g., self-reported lifetime cannabis use), and defining anxiety symptoms and severity by self-report rather than diagnosis by a health care provider. In addition, while several prior studies have examined differences by age groups (e.g., adolescents vs adults) few studies have examined differences by sex or considered age–sex interactions. Collectively, despite the high prevalence of cannabis use in people with anxiety, there continue to be large gaps in the understanding of the underlying mechanism and direction of this relationship (e.g., does cannabis cause anxiety disorders, do individuals with anxiety disorders self-medicate with cannabis, are there common risk factors for both).12, 13, 14, 15, 16, 17
This study aimed to examine whether individuals with an emergency department (ED) visit for cannabis use were at increased risk of having healthcare visits for anxiety disorders. Specifically, our objectives were to: 1) estimate the future risk of incident healthcare visits for anxiety disorders in individuals with an ED visit for cannabis compared to individuals without an ED visit for cannabis, hereafter referred to the general population. 2) compare the risk having an incident healthcare visit for an anxiety disorder across age and sex strata. We investigated these aims using a longitudinal population-based cohort study in Ontario, Canada.
Methods
Study design
We conducted a retrospective cohort study using routinely collected health administrative data from the province of Ontario, Canada. The cohort included all Ontario residents aged 10–105 years between January 1, 2008 and March 31, 2019 (with follow-up until March 31, 2022) who were eligible for the province's single-payer health system (the Ontario Health Insurance Plan [OHIP]), which covers all ED visits, hospitalizations, and outpatient physician visits for an estimated 97% of the population of Ontario.18 We excluded individuals who were a) not residents of Ontario at index (incident ED visit due to cannabis, or pseudo index date for the general population), b) not eligible for OHIP at index or continually in the three prior years to maximize capture of recent prior healthcare for anxiety, and c) had one or more ED visits or hospitalizations due to cannabis in the three years prior to index (since our exposure was an incident ED visits or hospitalizations due to cannabis). We excluded all individuals with one or more healthcare visits for an anxiety disorder (in a hospital or ED setting for our primary outcome and in a hospital, ED or outpatient setting for our secondary outcome) at index or in the three years before the index date (incident ED visit due to cannabis, or pseudo-index date for the general population). Our study followed the STROBE reporting guidelines for reporting observational studies, see Appendix B.19,20
Data sources
We used six individual-level databases, linked and analyzed at ICES (formerly the Institute for Clinical Evaluative Science), to capture all ED visits, hospitalizations, and essential physician services in Ontario along with sociodemographic characteristics; see online Supplement Methods S1 for details on databases. These datasets were linked using unique encoded identifiers and analyzed at ICES.
Ethics statement
This project was approved by the privacy office at ICES, which is an independent, non-profit research institute. ICES is authorized under section 45 of Ontario's Personal Health Information Protection Act (PHIPA) to collect and analyze personal health information without consent for health system management, evaluation, monitoring, or planning and approved research projects.
Exposures
We compared individuals with an incident ED visit due to cannabis use—defined as a visit where International Classification of Diseases (ICD) 10th revision code F12.X (Mental and behavioural disorders due to use of cannabinoids) were the main or contributing reason for the visit—to all other individuals without an incident ED visit due to cannabis. Incident visits were defined as an ED visit due to cannabis, with no ED visits or hospitalizations due to cannabis in the prior three years. We identified hospitalizations using ICD-10 codes for acute care hospitalizations and ICD-9- and ICD-10-CM cannabis for adult mental health hospital admissions through the Ontario Mental Health Reporting System (OMHRS). These codes are from the Canadian Institute for Health Information indicator “Hospital Stays for Harm Caused by Substance Use” which is widely used for mental health system performance and evaluation in Canada.21 As a sensitivity analysis, we defined incident ED visits where the ICD-10 cannabis code was listed only as the main reason for the visit.
Outcomes
The primary outcome was an incident ED visit or hospitalization for an anxiety disorder. We included panic disorders, phobic disorders, generalized anxiety disorders, and anxiety disorders not otherwise specified our primary outcome. Anxiety disorders with organic causes, obsessive-compulsive disorders, and adjustment disorders/post-traumatic stress disorders were not included in the primary outcome. See online Supplement Methods S2 for a complete list of ICD-10 and DSM codes for anxiety disorders.
As a secondary outcome, we broadened our primary outcome definition to additionally include two or more outpatient visits for an anxiety disorder (DSM code 300x) to a psychiatrist, or general practitioner within 12 months of each other. We considered this a secondary outcome as outpatient diagnostic codes for anxiety disorders in Ontario are highly sensitive for detecting a mental health disorder but have less specificity for anxiety.22,23
Covariates
On index, we obtained sociodemographic details including age, sex, rural residence, and neighborhood income quintile. We obtained information on health care use in the three years prior to index, (available from 2005 onwards), including outpatient mental health visits and ED visits and hospitalizations for substance use (alcohol, cannabis, opioids, and other) and mental health conditions (mood disorder, schizophrenia and psychosis, self-harm, and other)22,24 Urban or rural residence and neighbourhood income level quintiles were defined using Statistics Canada census data.25
Statistical analyses
We presented descriptive statistics on the characteristics of individuals with an incident ED visit due to cannabis and the general population and compared them using standardized mean differences.26 We evaluated the risk of having a healthcare visit for an anxiety disorder for both groups using cumulative incidence functions and cause-specific Cox proportional hazards to compare risk. Members of the general population were assigned a pseudo-index date that matched the distribution of index dates for individuals with an ED visit due to cannabis; see online Supplement Methods S3 for details.
We present unadjusted and adjusted Cox models, with adjustments depending on the outcome and sensitivity analysis. For our main analysis of the primary outcome, we adjusted for age, sex, neighbourhood income quintile, rurality, outpatient mental health service use in the past three years (family medicine visit for anxiety yes/no, family medicine visit for cause other than anxiety yes/no, psychiatry visit for anxiety yes/no, psychiatry visit for cause other than anxiety yes/no), past three years acute care substance use (alcohol yes/no, opioids use yes/no, stimulants yes/no, other substance use yes/no), and past three years acute care mental health use (depression yes/no, psychosis yes/no, self-harm yes/no, and other mental health condition yes/no). For our main analysis of the secondary outcome, we excluded all individuals with prior outpatient anxiety care and adjusted for the same factors as the main analysis of the primary outcome, excluding outpatient anxiety.
We completed sensitivity analyses of the risk of an incident healthcare visit for anxiety (using both our primary and secondary outcomes), which included only individuals who had no outpatient, ED or hospital-based case for a mental health condition or substance use disorder in the three years before index. In these analyses, our Cox models were adjusted for age, sex, neighbourhood income quintile, and rurality. All data in ICES are complete except for rural residence or neighbourhood income-quintile (<0.2% missing); we included individuals with missing data in models with an additional category indicating missing. Given differences in the diagnosis of anxiety disorders by age, we complete subgroup analyses that examined age and sex strata separately.27 Proportional hazards were verified through visual inspection of log–log plots. All analyses were conducted using SAS Enterprise Guide 8.3 (SAS Institute, Cary, NC).
Role of funding source
The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Results
Our study population for our primary analysis consisted of 12,099,144 individuals without prior care for an anxiety disorder in the ED or hospital setting, of whom 34,822 (0.29%) had an ED visit due to cannabis, see online Supplemental Figure S1 for cohort flow. Compared to the general population, individuals with an ED for cannabis use were younger (mean age 27.6 vs 44.9 years, Standardized mean difference [SMD] 1.02), more likely to be male (66.7% vs 49.1%, SMD 0.36), and reside in the lowest-income quintile neighbourhood (28.8% vs 19.3%, SMD 0.22). They were also likely to have had prior outpatient mental health visits (59.8% vs 26.0%, SMD 0.73), ED visits or hospitalizations for non-cannabis substance use (14.1% vs 0.8%, SMD 0.52) or a mental health condition other than anxiety (19.0% vs 1.0%, SMD 0.63) in the past three years compared to the general population. Our study population for our secondary analysis, excluding all individuals with prior outpatient or ED, or hospital-based care for anxiety disorders, consisted of 19,460 (63.9%) individuals with an ED visit for cannabis use and 9,771,533 (81.0%) members of the general population. Our study population for our secondary analysis, excluding all individuals with any prior outpatient or ED, or hospital-based care for a mental health condition or substance use disorder, consisted of 12,587 (36.1%) individuals with an ED visit due to cannabis and 8,875,946 (73.6%) members of the general population, see Table 1.
Table 1.
Characteristics of individuals with an incident Emergency Department (ED) visit due to cannabis and the general population with no baseline anxiety disordera between January 2008 and March 2019.
| ED visit for cannabis use (N = 34,822)b | General population (N = 12,064,322)c | Standardized mean difference | |
|---|---|---|---|
| N (%) | |||
| Sex | |||
| Female | 11,587 (33.3) | 6,136,802 (50.9) | 0.36 |
| Male | 23,235 (66.7) | 5,927,520 (49.1) | 0.36 |
| Age | |||
| Mean ± SD | 27.61 ± 12.72 | 44.90 ± 20.28 | 1.02 |
| 10–18 years | 8684 (24.9) | 1,390,334 (11.5) | 0.35 |
| 19–24 years | 10,590 (30.4) | 1,005,502 (8.3) | 0.58 |
| 25–44 years | 11,159 (32.0) | 3,543,486 (29.4) | 0.06 |
| 45–64 years | 3886 (11.2) | 3,910,659 (32.4) | 0.53 |
| 65+ years | 503 (1.4) | 2,214,341 (18.4) | 0.59 |
| Rurality | |||
| Urban | 31,164 (89.5) | 10,755,424 (89.2) | 0.01 |
| Rural | 3468 (10.0) | 1,286,487 (10.7) | 0.02 |
| Neighbourhood income quintile | |||
| 1 (Poorest) | 10,043 (28.8) | 2,329,924 (19.3) | 0.22 |
| 2 | 7235 (20.8) | 2,373,741 (19.7) | 0.03 |
| 3 | 6239 (17.9) | 2,406,412 (19.9) | 0.05 |
| 4 | 5698 (16.4) | 2,443,694 (20.3) | 0.10 |
| 5 (Richest) | 5342 (15.3) | 2,470,854 (20.5) | 0.13 |
| Substance use acute care visits in past 3 years | |||
| Any | 4907 (14.1) | 101,006 (0.8) | 0.52 |
| Alcohol | 2892 (8.3) | 80,382 (0.7) | 0.38 |
| Stimulants | 707 (2.0) | 5324 (0.0) | 0.20 |
| Opioids | 506 (1.5) | 7204 (0.1) | 0.16 |
| Other | 1951 (5.6) | 14,782 (0.1) | 0.33 |
| Mental health acute care visits in past 3 years | |||
| Any | 6616 (19.0) | 124,255 (1.0) | 0.63 |
| Mood disorder | 3376 (9.7) | 66,640 (0.6) | 0.42 |
| Psychosis | 2421 (7.0) | 16,512 (0.1) | 0.38 |
| Deliberate Self harm | 1637 (4.7) | 29,102 (0.2) | 0.29 |
| Other | 1428 (4.1) | 24,643 (0.2) | 0.27 |
| Outpatient mental health and substance use visits in past 3 years | |||
| Any | 20,835 (59.8) | 3,134,484 (26.0) | 0.73 |
| Any anxiety (300) | 15,362 (44.1) | 2,292,789 (19.0) | 0.56 |
| Family physician | 19,354 (55.6) | 2,973,652 (24.6) | 0.67 |
| Family anxiety (300) | 13,960 (40.1) | 2,179,506 (18.1) | 0.50 |
| Psychiatrist | 9486 (27.2) | 582,121 (4.8) | 0.64 |
| Psychiatrist anxiety (300) | 4412 (12.7) | 289,864 (2.4) | 0.40 |
| Any outpatient or acute mental health or substance use visits in past 3 years | |||
| Yes | 22,235 (63.9) | 3,188,376 (26.4) | 0.81 |
| No | 12,587 (36.1) | 8,875,946 (73.6) | 0.81 |
Baseline anxiety disorder defined as care for an anxiety disorder in an ED or hospital setting in the past 3-years.
Characteristics taken at time of incident ED visit.
Characteristics taken on pseudindex date matching distribution of incident cannabis ED visits.
Primary outcome: incident ED visit or hospitalization for anxiety disorder
Within 3-years, 12.3% of people with an ED visit for cannabis use had an incident ED visit or hospitalization for an anxiety disorder compared to 1.2% of members of the general population. After adjustment individuals with an ED visit for cannabis use had a 3.7-fold (adjusted hazard ratio [aHR] 3.69 95% CI 3.57–3.82) increased risk of having an incident ED visit or hospitalizations for an anxiety disorder relative to the general population. In our sensitivity analysis, were ED visits for cannabis use were limited to only ED visits with cannabis as the main reason for the visit (as opposed to main or contributing), individuals (n = 14,582) with an ED visit for cannabis use had a 9.2-fold (adjusted hazard ratio [aHR] 9.24 95% CI 8.82–9.69) increased risk relative to the general population (n = 12,064,322), see online Table S1. In our sensitivity analysis excluding all individuals with any prior healthcare for mental health conditions or substance use disorders, the risk of having an incident ED or hospitalization for an anxiety disorder within 3-years was 7.7% for individuals with an ED visit for cannabis use and 0.7% for the general population. This represented a 9.4-fold (aHR 9.37 95% CI 8.79–9.99) increased risk in the cannabis group relative to the general population, Table 2.
Table 2.
Risk of incident healthcare visit for an anxity disorder after an Emergency Department (ED) visit due to cannabis relative to the general population.
| Population at risk | Diagnosis in 1 year, no. (%) | Diagnosis in 3 years, no. (%) | Diagnosis in 5 years, no. (%) | Diagnosis, no. (%) | Incidence per 100,00 person yrsa | Unadjusted hazard ratioa (95% CI) | Fully adjusted hazard ratioa,f (95% CI) | |
|---|---|---|---|---|---|---|---|---|
| Primary analysis: no baseline anxiety disorderb | ||||||||
| Primary outcome:incident ED visit or hospitalization for an anxiety disorderc | ||||||||
| Cannabis | 34,822 | 2429 (6.98) | 4294 (12.33) | 5450 (15.65) | 6575 (18.88) | 4166.93 | 11.16 (10.83–11.51) | 3.69 (3.57–3.82) |
| General population | 12,064,322 | 49,577 (0.41) | 143,345 (1.19) | 214,655 (1.78) | 303,117 (2.51) | 403.87 | Ref | Ref |
| Secondary outcome:incident outpatient visit ED visit or hospitalization for an anxiety disorderd | ||||||||
| Cannabis | 19,460 | 3135 (16.11) | 5359 (27.54) | 6552 (33.67) | 7701 (39.57) | 9295.35 | 5.84 (5.69–6.00) | 3.88 (3.77–3.99) |
| General population | 9,771,533 | 163,334 (1.67) | 550,132 (5.63) | 845,655 (8.65) | 1,197,735 (12.26) | 1914.87 | Ref | Ref |
| Sensitivity analysis: no baseline mental health or substance use disorderse | ||||||||
| Primary outcome:incident ED visit or hospitalization for an anxiety disorderc | ||||||||
| Cannabis | 12,587 | 569 (4.52) | 966 (7.67) | 1240 (9.85) | 1514 (12.03) | 2582.76 | 11.02 (10.34–11.74) | 9.37 (8.79–9.99) |
| General population | 8,875,946 | 20,354 (0.23) | 64,351 (0.73) | 101,317 (1.14) | 150,467 (1.70) | 246.56 | Ref | Ref |
| Secondary outcome:incident outpatient visit ED visit or hospitalization for an anxiety disorderd | ||||||||
| Cannabis | 12,587 | 1746 (13.87) | 2975 (23.64) | 3636 (28.89) | 4316 (34.29) | 7954.15 | 5.47 (5.27–5.67) | 5.31 (5.12–5.50) |
| General population | 8,875,946 | 127,799 (1.44) | 443,646 (5.00) | 692,443 (7.80) | 998,249 (11.25) | 1699.83 | Ref | Ref |
Risk at 3-years.
Individuals with no anxiety visits at index or in past 3 years (primary outcome: no ED visits or Hospitalizations, secondary outcome: additionally, no outpatient visits).
Defined as 1 or more ED visits or hospitalizations for an anxiety disorder.
Defined as 1 or more ED visits or hospitalizations for an anxiety disorder or 2 or more outpatient visits for anxiety.
Individuals with no outpatient visits, ED visits or Hospitalizations for any mental health or substance use disorder in past 3 years.
Adjusted for age, sex, neighbourhood income quintile and rurality in all models. Further adjusted in no baseline anxiety disorder models for past three years outpatient mental health service use (anxiety visit family medicine visit yes/no, psychiatry yes/no and non-anxiety family medicine visit yes/no, psychiatry yes/no), past three years acute care substance use (alcohol yes/no, opioids use yes/no, stimulants yes/no, other substance use yes/no), and past three years acute care mental health use (depression yes/no, schizophrenia yes/no, self-harm yes/no, and other mental health condition yes/no).
Secondary outcome: incident ED visit, hospitalization or outpatient visit for an anxiety disorder
Within 3-years, 27.5% of people with an ED visit for cannabis use has an incident outpatient, ED or hospitalization for an anxiety disorder compared to 5.6% of members of the general population. After adjustment individuals with an ED visit for cannabis use had a 3.9-fold (adjusted hazard ratio [aHR] 3.88 95% CI 3.77–3.99) increased risk relative to the general population. In our sensitivity analysis excluding all individuals with any baseline mental health conditions or substance use disorders, the risk of an incident outpatient, ED visit or hospitalization for an anxiety disorder within 3-years was 23.6% for individuals with an ED visit for cannabis use and 5.0% for the general population. This represented a 5.3-fold (aHR 5.31 95% CI 5.37–5.50) increased risk in the cannabis group relative to the general population), Table 2.
Cumulative incidence functions for the risk of the primary and secondary outcome following an incident ED visit due to cannabis and in the general population are presented in Fig. 1. Individuals with an ED visit due to cannabis had an immediate increase in both the primary and secondary outcomes relative to the general population, which continued over 5-years of follow-up.
Fig. 1.
Cumulative incidence function curves comparing incident healthcare visits for an anxiety disorder following an ED visit due to cannabis compared to the general population over 5-years. The primary outcome (left column) is an incident ED visit or hospitalization for an anxiety disorder, the secondary outcome (right column) is an incident outpatient, ED or hospitalizaiton for an anxiety disorder. In the sensitivity analysis (bottom row), those with any prior care for a mental health or substance use disorder were excluded. MH/SUD = mental health or substance use disorder.
Subgroup analyses
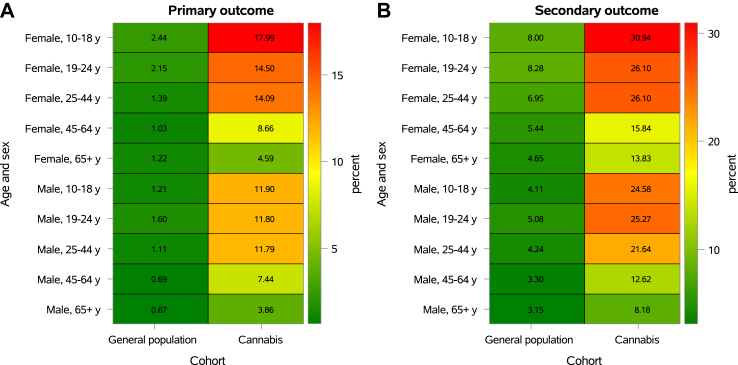
Fig. 2 shows the risk of having an incident healthcare visit for an anxiety disorder (primary and secondary outcomes for the no anxiety at baseline groups) within three years based on age, sex, and having had an ED visit due to cannabis. The absolute risk of incident anxiety disorder visits varied considerably by age and sex for individuals with higher rates in youth and women for individuals with an ED visit for cannabis use and the general population. There was an increase in the risk incident anxiety disorder visits in the cannabis group relative to the general population across all age and sex strata. However, the relative increase in risk was greater for younger individuals, particularly for males. For example, amongst individuals aged 10–18 years, the increased risk of incident outpatient visit, ED visit, or hospitalization for an anxiety disorder (secondary outcome definition) in individuals with an ED visit to cannabis relative to the general population was almost double in men (aHR 5.67 95% CI 5.19–6.21) compared to women (aHR 3.22 95% CI 2.95–3.52), see online Table S2 for age and sex-specific hazard ratios.
Fig. 2.
Visual representation of crude percent of individuals diagnosed with an anxiety disorder in the ED or hospital within 3-years of an ED visit due to cannabis and the general population by age and sex. Panel A shows the primary outcome (incident ED visit or hospitalization for an anxiety disorder), and Panel B shows the secondary outcome (incident outpatient visit, ED visit or hospitalization for an anxiety disorder). In Panel A and Panel B individuals have no prior care for an anxiety disorders.
Discussion
In this population-based study of over 12 million people, we found that within three years of an ED visit for cannabis use 12.3% of individuals had an incident ED visit or hospitalization for an anxiety disorder and 27.5% of individuals had an incident outpatient visit, ED visit or hospitalization for an anxiety disorder. After adjustment, rates were over 3-fold higher than the risk in the unexposed general population of 1.2% (ED visit or hospitalizations) and 5.6% (outpatient visit, ED visit, or hospitalization). Males and females of all ages with an ED visit due to cannabis were at increased risk of incident healthcare visits for an anxiety disorder relative to the general population. However, adolescent10, 11, 12, 13, 14, 15, 16, 17, 18 males experienced the largest relative increase in risk from cannabis use.
Our findings add to the literature about the relationship between cannabis use and anxiety disorders and suggest both an association between cannabis use and the risk of anxiety disorders as well as with the severity of anxiety symptoms leading to the need for ED visits or hospitalization. The increased risk of our primary outcome (incident ED visit or hospitalization for an anxiety disorder) captures severe initial presentations or worsening of pre-existing anxiety disorders. The increased risk of our secondary outcome (incident outpatient visit, ED visit or hospitalization for an anxiety disorder) in individuals with ED visit for cannabis likely captures new diagnoses of an anxiety disorder. Previous studies have presented mixed findings with a 2021 meta-analysis of 10 longitudinal studies containing 49,273 individuals reported that cannabis use was associated with a slightly increased risk of developing any anxiety condition (OR = 1.25 95% CI 1.01–1.54).14 Critically, studies to date have generally had small sample sizes, incomplete adjustment for confounders, and generally relied on self-reported cannabis use rather than health records for identification of exposure to cannabis. Our findings of over a 3-fold increase in the risk incident healthcare visit for an anxiety disorder following an ED visit due to cannabis use compared to much more modest increases in prior work may be related to both the nature of our study design and greater severity of exposure (e.g., cannabis use requiring care in the ED vs self-reported lifetime or past year cannabis use). Our study cannot isolate the causal relationship between cannabis use and the development of anxiety disorders. While our findings raise concern that heavy cannabis use may cause anxiety disorders, there are two alternative explanations for our findings.12 First, individuals with an anxiety disorder who have not yet presented for care may have been self-medicating with cannabis in an attempt to alleviate symptoms. Our sensitivity analysis, excluding all individuals with any mental health or substance use history, continued to find a positive association, reducing the likelihood of this first explanation. Second, common risk factors such as genetic predisposition or adverse life experiences may increase the risk of both severe cannabis use and anxiety disorders. While there is increasing evidence of alterations by cannabis on neurocognition, including processes linked to anxiety disorders, further research in this area is indicated.
Cannabis use is increasing globally, and emerging data from Canada and the United States suggests that higher-risk cannabis use (e.g., regular use and use of higher potency products) and associated healthcare encounters may have accelerated following non-medical cannabis legalization and commercialization.5,28, 29, 30, 31 Our findings highlight that cannabis use that requires care in the ED is associated with an increased risk of being diagnosed with an anxiety disorder. Given accumulating evidence of the association of cannabis use with severe psychiatric disease, further public education and interventions are indicated. For countries proceeding with the legalization of medical and non-medical cannabis public-health-oriented regulation based on best practices from alcohol and tobacco along with emerging cannabis-specific evidence may be indicated to avoid potential increases in anxiety disorders.32 In the interim ongoing monitoring of changes in anxiety disorders following legalization are needed.
Our study has several limitations. First, while the use of health administrative data has several advantages (large cohorts with reduced risk of selection bias) it captures care for cannabis use rather than cannabis use itself. Consequently, while our study supports that cannabis use requiring ED care is associated with an increased risk of anxiety disorders, the findings have reduced inference for the relationship between less frequent or heavy cannabis use and anxiety. In addition, individuals in Ontario with higher risk (e.g., frequent) or disordered cannabis use who have not received care in ED settings would be classified in the general population, which would bias our findings towards the null. Second, our primary outcome, an incident ED visit or hospitalization for an anxiety disorder, is specific for anxiety but captures both severe initial presentations of anxiety and potential worsening of pre-existing anxiety disorders previously managed in outpatient settings. While our secondary outcome, which included incident outpatient visits for anxiety disorders, is more likely to be capturing new anxiety disorders, outpatient codes have not been validated specifically for anxiety disorders in Ontario. Third, health administrative data lacks information on patterns of cannabis use (frequency of use, type and potency of products) which may be relevant for the relationship between cannabis use and anxiety disorders. Finally, while our study design, which excluded prior healthcare visits for anxiety disorders, reduces the possibility of reverse causality, some individuals with incident ED visits for cannabis use may have already had anxiety but not yet been diagnosed with an anxiety disorder or received treatment.10 Regardless of causality, the finding suggests that individuals with cannabis use requiring treatment in the ED or hospital setting are at a high risk of anxiety disorders and may benefit from further assessment and intervention.
This cohort study found having an ED visit due to cannabis use was associated with an increased risk of requiring hospital-based care for anxiety and being diagnosed with an incident anxiety disorder. The elevated risk was present for all age groups and in men in women but was particularly pronounced for younger men. These findings have important implications given global increases in cannabis use and potency, along with increasing trends toward the legalization and commercialization of medical and non-medical cannabis.
Contributors
Dr Myran and Mr Pugliese had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: All Authors. Acquisition, analysis, or interpretation of data: All author. Drafting of the manuscript: Myran. Critical revision of the manuscript for important intellectual content: All Authors. Statistical analysis: Myran, Pugliese, Harrison. Obtained funding: Myran, Tanuseputro. Administrative, technical, or material support: Myran, Harrison. Supervision: Myran.
Data sharing statement
The dataset from this study is held securely in coded form at ICES. While legal data sharing agreements between ICES and data providers (e.g., healthcare organizations and government) prohibit ICES from making the dataset publicly available, access may be granted to those who meet pre-specified criteria for confidential access, available at www.ices.on.ca/DAS (email: das@ices.on.ca). The full dataset creation plan and underlying analytic code are available from the authors upon request, understanding that the computer programs may rely upon coding templates or macros that are unique to ICES and are therefore either inaccessible or may require modification.
Declaration of interests
Marco Solmi has received honoraria/has been a consultant for AbbVie, Angelini, Lundbeck, Otsuka. Daniel Myran was supported by the Bruyère Research Institute and a Research Fellow Salary Award from the Canadian Institutes of Health Research and the University of Ottawa Department of Family Medicine. Peter Tanuseputro was supported by a PSI Graham Farquharson Knowledge Translation Fellowship. No other disclosures were reported.
Acknowledgements
This study was supported by the University of Ottawa site of ICES, which is funded by an annual grant from the Ontario Ministry of Health and Ministry of Long-Term Care. This study also received funding from Canadian Institutes for Health Research (grant No 452360).
The analyses, conclusions, opinions and statements expressed herein are solely those of the authors and do not reflect those of the funding or data sources; no endorsement is intended or should be inferred.
Parts of this material are based on data and/or information compiled and provided by the Canadian Institute for Health Information. Parts of this material are based on data and/or information compiled and provided by CIHI and the Ontario Ministry of Health. The analyses, conclusions, opinions and statements expressed herein are solely those of the authors and do not reflect those of the funding or data sources; no endorsement is intended or should be inferred. This document used data adapted from the Statistics Canada Postal CodeOM Conversion File, which is based on data licensed from Canada Post Corporation, and/or data adapted from the Ontario Ministry of Health Postal Code Conversion File, which contains data copied under license from ©Canada Post Corporation and Statistics Canada.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.eclinm.2024.102455.
Appendix A. Supplementary data
References
- 1.United Nations Office on Drugs and Crime World drug report 2022. 2022. https://www.unodc.org/unodc/en/data-and-analysis/world-drug-report-2022.html [cited 2023 Jul 27]. Available from:
- 2.Petrilli K., Ofori S., Hines L., Taylor G., Adams S., Freeman T.P. Association of cannabis potency with mental ill health and addiction: a systematic review. Lancet Psychiatry. 2022;9(9):736–750. doi: 10.1016/S2215-0366(22)00161-4. https://pubmed.ncbi.nlm.nih.gov/35901795/ [cited 2023 Feb 1] Available from: [DOI] [PubMed] [Google Scholar]
- 3.Hall W., Stjepanović D., Caulkins J., et al. Public health implications of legalising the production and sale of cannabis for medicinal and recreational use. Lancet. 2019;394(10208):1580–1590. doi: 10.1016/S0140-6736(19)31789-1. [DOI] [PubMed] [Google Scholar]
- 4.Murray R.M., Hall W. Will legalization and commercialization of cannabis use increase the incidence and prevalence of psychosis? JAMA Psychiatry. 2020;77(8):777–778. doi: 10.1001/jamapsychiatry.2020.0339. https://pubmed.ncbi.nlm.nih.gov/32267480/ [cited 2023 Jan 30] Available from: [DOI] [PubMed] [Google Scholar]
- 5.Myran D.T., Pugliese M., Tanuseputro P., Cantor N., Rhodes E., Taljaard M. The association between recreational cannabis legalization, commercialization and cannabis-attributable emergency department visits in Ontario, Canada: an interrupted time–series analysis. Addiction. 2022;117(7):1952–1960. doi: 10.1111/add.15834. https://onlinelibrary.wiley.com/doi/full/10.1111/add.15834 [cited 2022 Mar 3]; Available from: [DOI] [PubMed] [Google Scholar]
- 6.Marconi A., Di Forti M., Lewis C.M., Murray R.M., Vassos E. Meta-analysis of the association between the level of cannabis use and risk of psychosis. Schizophr Bull. 2016;42(5):1262–1269. doi: 10.1093/schbul/sbw003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Solmi M., De Toffol M., Kim J.Y., et al. Balancing risks and benefits of cannabis on humans: umbrella review of meta-analyses of randomized controlled trials and observational studies. BMJ. 2023;382 doi: 10.1136/bmj-2022-072348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Myran D.T., Harrison L.D., Pugliese M., et al. Transition to schizophrenia spectrum disorder following emergency department visits due to substance use with and without psychosis. JAMA Psychiatry. 2023;80(11):1169–1174. doi: 10.1001/jamapsychiatry.2023.3582. https://jamanetwork.com/journals/jamapsychiatry/fullarticle/2809870 [cited 2023 Nov 8] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Feingold D., Weinstein A. Cannabis and depression. Adv Exp Med Biol. 2021;1264:67–80. doi: 10.1007/978-3-030-57369-0_5. [DOI] [PubMed] [Google Scholar]
- 10.Volkow N.D., Baler R.D., Compton W.M., Weiss S.R.B. Adverse health effects of marijuana use. N Engl J Med. 2014;370(23):2219–2227. doi: 10.1056/NEJMra1402309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sharpe L., Sinclair J., Kramer A., De Manincor M., Sarris J. Cannabis, a cause for anxiety? A critical appraisal of the anxiogenic and anxiolytic properties. J Transl Med. 2020;18(1):1–21. doi: 10.1186/s12967-020-02518-2. https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-020-02518-2 [cited 2023 Jul 6] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kedzior K.K., Laeber L.T. A positive association between anxiety disorders and cannabis use or cannabis use disorders in the general population--a meta-analysis of 31 studies. BMC Psychiatry. 2014;14:136. doi: 10.1186/1471-244X-14-136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zimmermann M., Chong A.K., Vechiu C., Papa A. Modifiable risk and protective factors for anxiety disorders among adults: a systematic review. Psychiatry Res. 2020;285 doi: 10.1016/j.psychres.2019.112705. [DOI] [PubMed] [Google Scholar]
- 14.Xue S., Husain M.I., Zhao H., Ravindran A.V. Cannabis use and prospective long-term association with Anxiety: a systematic review and meta-analysis of longitudinal studies: usage du cannabis et association prospective à long terme avec l’anxiété: une revue systématique et une méta-analyse d’études longitudinales. Can J Psychiatry. 2021;66(2):126–138. doi: 10.1177/0706743720952251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Onaemo V.N., Fawehinmi T.O., D'Arcy C. Comorbid cannabis use disorder with major depression and generalized anxiety disorder: a systematic review with meta-analysis of nationally representative epidemiological surveys. J Affect Disord. 2021;281:467–475. doi: 10.1016/j.jad.2020.12.043. [DOI] [PubMed] [Google Scholar]
- 16.Gobbi G., Atkin T., Zytynski T., et al. Association of cannabis use in adolescence and risk of depression, anxiety, and suicidality in young adulthood: a systematic review and meta-analysis. JAMA Psychiatry. 2019;76(4):426–434. doi: 10.1001/jamapsychiatry.2018.4500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Crippa J.A., Zuardi A.W., Martín-Santos R., et al. Cannabis and anxiety: a critical review of the evidence. Human Psychopharmacol. 2009;24(7):515–523. doi: 10.1002/hup.1048. [DOI] [PubMed] [Google Scholar]
- 18.Non-insured clients | Alliance for healthier communities. https://www.allianceon.org/Non-Insured-Clients [cited 2023 Jul 18]. Available from:
- 19.von Elm E., Altman D.G., Egger M., Pocock S.J., Gøtzsche P.C., Vandenbroucke J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370(9596):1453–1457. doi: 10.1016/S0140-6736(07)61602-X. [DOI] [PubMed] [Google Scholar]
- 20.Benchimol E.I., Smeeth L., Guttmann A., et al. The REporting of studies conducted using observational routinely-collected health data (RECORD) statement. PLoS Med. 2015;12(10) doi: 10.1371/journal.pmed.1001885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ministry of Health and Long-Term Care . ON; Toronto: 2011. Early psychosis intervention program standards. [Google Scholar]
- 22.MHASEF Research Team . Technical Appendix; Toronto, ON: 2018. Mental health and addictions system performance in Ontario: a baseline scorecard. [Google Scholar]
- 23.Chiu M., Guttmann A., Kurdyak P. Mental health and addictions system performance in Ontario: an updated scorecard, 2009-2017. Healthc Q. 2020;23(3):7–11. doi: 10.12927/hcq.2020.26340. https://pubmed.ncbi.nlm.nih.gov/33243359/ [cited 2023 Jan 31] Available from: [DOI] [PubMed] [Google Scholar]
- 24.Kurdyak P., Lin E., Green D., Vigod S. Validation of a population-based algorithm to detect chronic psychotic illness. Can J Psychiatry. 2015;60(8):362–368. doi: 10.1177/070674371506000805. https://pubmed.ncbi.nlm.nih.gov/26454558/ [cited 2023 Feb 1] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Statistics Canada . 2016. Population centre and rural area classification. [Google Scholar]
- 26.Austin P.C. Using the standardized difference to compare the prevalence of a binary variable between two groups in observational research. Commun Stat Simul Comput. 2009;38(6):1228–1234. [Google Scholar]
- 27.Altemus M., Sarvaiya N., Neill Epperson C. Sex differences in anxiety and depression clinical perspectives. Front Neuroendocrinol. 2014;35(3):320–330. doi: 10.1016/j.yfrne.2014.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Myran D.T., Pugliese M., Roberts R.L., et al. Association between non-medical cannabis legalization and emergency department visits for cannabis-induced psychosis. Mol Psychiatry. 2023 doi: 10.1038/s41380-023-02185-x. [cited 2023 Jul 31] Available from: [DOI] [PubMed] [Google Scholar]
- 29.Myran D.T., Gaudreault A., Konikoff L., Talarico R., Pacula R.L. Changes in cannabis-attributable hospitalizations following nonmedical cannabis legalization in Canada. JAMA Netw Open. 2023;6(10):e2336113. doi: 10.1001/jamanetworkopen.2023.36113. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2810194 [cited 2023 Oct 18] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cerdá M., Mauro C., Hamilton A., et al. Association between recreational marijuana legalization in the United States and changes in marijuana use and cannabis use disorder from 2008 to 2016. JAMA Psychiatry. 2020;77(2):165–171. doi: 10.1001/jamapsychiatry.2019.3254. https://jamanetwork.com/journals/jamapsychiatry/fullarticle/2755276 [cited 2023 Dec 11] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Imtiaz S., Nigatu Y.T., Ali F., et al. Cannabis legalization and cannabis use, daily cannabis use and cannabis-related problems among adults in Ontario, Canada (2001–2019) Drug Alcohol Depend. 2023;244 doi: 10.1016/j.drugalcdep.2023.109765. [DOI] [PubMed] [Google Scholar]
- 32.World Health Organization . World Health Organization; 2010. Global strategy to reduce the harmful use of alcohol; p. 38. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.