Abstract
Objective
This paper explores sociodemographic determinants and geographic disparities in COVID-19 booster uptake among fully vaccinated adults in Nueces County, Texas, USA with a population of over 353,000.
Methods
A logistic generalized additive model was applied to analyze 184,252 official vaccination records of fully vaccinated adults over the period between December 2020 and August 2022. An individual's odds in receiving a booster shot were estimated with a host of sociodemographic characteristics as predictors.
Results
Model estimation results reveal that male (odds ratio 0.836, 95% confidence interval 0.835–0.836, p < 0.001) and Hispanic residents (odds ratio 0.944, 95% confidence interval 0.943–0.945, p < 0.001) in the county were less likely to take a booster shot. Between the ages of 25 and 75, booster uptake increased with age (age 75 vs. 45 odd ratio 3.058, 95% confidence interval 3.052–3.063, p < 0.001). Booster uptake was lower in rural areas (odds ratio 0.804, 95% confidence interval 0.795–0.814, p < 0.001) and communities with high social vulnerability (highest vs. moderate vulnerability odd ratio 0.800, 95% confidence interval 0.767–0.836, p < 0.001).
Conclusion
Empirical results confirm that booster uptake varied across individuals and communities of different socioeconomic and demographic characteristics. To advance health equity, a more inclusive vaccine campaign should pay particular attention to those underserved populations.
Keywords: COVID-19 vaccine, Booster, Demographic and socioeconomic factors, Geographic disparities
1. Introduction
Vaccination has proven to be the most effective way to help protect people against COVID-19 infection, hospitalization, and death [1]. However, vaccine-induced immunity wanes over time [2,3]. Booster shots have become necessary for fully vaccinated people to provide optimal protection against the coronavirus [4,5]. In November 2021, the U.S. Centers for Disease Control and Prevention recommended a COVID-19 vaccine booster to all persons above the age of 18 [6].
Booster vaccine uptake refers to the population share that has received at least one booster dose of COVID-19 vaccine. Despite the wide availability of COVID-19 booster shots, only 48.6% of fully vaccinated Americans took a booster by August 2022 [7]. Strategies to target communities with low booster uptake would help more people stay protected [8,9].
A growing literature highlights the role that demographic and socioeconomic factors play in people's willingness to receive a vaccine [[10], [11], [12], [13], [14], [15]]. Such factors include age, gender, race/ethnicity, education, and income [10,11,[16], [17], [18], [19]]. Some studies [20,21] show a lower willingness to receive a booster vaccine among those with less education, lower socioeconomic status, or younger than 45. Such disparities in booster uptake-based demographic and socio-economic factors raise concerns about the fairness and equity of vaccine distribution and access, potentially rendering certain populations more vulnerable to the virus. Instead of assessing people's intentions based on survey data, this paper draws on official vaccination records to measure actual booster vaccine uptake.
As for the initial COVID-19 doses [10], the booster uptake rate has been found to vary geographically. By August 2022, the fully vaccinated population with at least one booster dose ranged from 28.7% in North Carolina to 63.3% in Vermont [7]. Even within a city, vaccination rates varied remarkably across neighborhoods [11]. Such disparities highlight, among others, a potential lack of a standardized approach to vaccination campaigns, leaving certain regions or communities more susceptible to the coronavirus. Communities with low vaccination rates motivate an in-depth assessment of their contributing factors. A better understanding of disparities in booster vaccine uptake, especially across communities and demographic groups, would help design appropriate interventions [22,23].
The objective of this paper is to explore disparities in booster uptake. The geographic area of our study is Nueces County in the state of Texas, USA. According to the 2021 American Community Survey, the county's population is 353,079 and 72% of that population is 18 years or older. Hispanic or Latino is the ethnic majority group, making up 62% of the county population. In October 2021, the Nueces County Public Health District began offering free COVID-19 booster shots to residents. More than 100 vaccination sites were opened across the county. By August 2022, 60% of county residents were fully vaccinated, but the adult population share with at least one booster shot was only 26%—considerably lower than the 38.7% national average [7]. Our case study reveals a significant gap between the fully vaccinated population and those with at least one booster shot. This highlights a potential breakdown in the continuum of care and follow-up for individuals who initially received the COVID-19 vaccine.
A study reports that the initial COVID-19 vaccine uptake in that region was lower among neighborhoods with lower socioeconomic status [11]. It is interesting to look at the booster uptake among fully vaccinated residents. In addition to sociodemographic factors, we examine potentially different booster uptakes between people living in rural as opposed to urban areas. This is motivated by the literature that highlights disparities in people's attitudes or beliefs toward vaccination between the two geographic settings [[24], [25], [26]].
2. Materials and methods
2.1. Data sources
Our primary data source is the Nueces County Public Health District's vaccination records. The dataset consists of vaccination records for adults (aged 18 and older) from December 2020 through the end of August 2022. The records contain residents' name, home address, age, gender, and race/ethnicity, along with the dates and names of all coronavirus vaccine doses they received. Because the study involves personal information, the data compilation process was reviewed and subsequently approved by Texas A&M University – Corpus Christi Institutional Review Board (IRB Number:TAMU–CC–IRB-2022-0448).
After excluding individuals without all of the above personal information, our sample consists of 184,252 fully vaccinated individuals aged 18 years and older. Residents were considered fully vaccinated when they received two shots (initial doses) of the Pfizer and Moderna vaccines or one shot of Johnson and Johnson by February 2022. This sample represents 72% of the total adult population in Nueces County. According to data from the Texas Department of State Health Services, a total of 203,720 people of all ages, or 57% of the population, in Nueces County were fully vaccinated [27].
Numerous studies [10,11,24] have reported disparate COVID-19 vaccine uptakes among different socioeconomic groups. Because our official vaccination records do not contain socioeconomic information of individuals, we supplemented our empirical work with community-level data. Following [11], we incorporated the CDC's Social Vulnerability Index (SVI) data [28] as measures of a neighborhood's various socioeconomic and demographic characteristics.
The SVI dataset was developed using 2018 Census data to help communities prepare for and recover from public health emergencies. For each individual in our sample, we identified the SVI value of the census tract based on his/her home address. A higher SVI value indicates more potential negative effects on human health in a community caused by external stresses, such as natural disasters and disease outbreaks. The overall SVI index is derived from 15 sociodemographic and economic indicators, ranging from poverty and unemployment to vehicular access and housing conditions. Those indicators are grouped into four themes: a) socioeconomic status (below poverty level, unemployed, per capita income, and no high school diploma); b) household composition and disability (age 65 or older, age 17 or younger, and single parents); c) minority status and language (minority population, low English proficiency); and d) housing type and transportation (multi-unit structures, mobile homes, crowding, households without a vehicle, and institutional group quarters). Our empirical work involved those four broad social vulnerability indicators in addition to the composite index.
Other than socioeconomic and demographic factors, we explore different booster uptakes between rural and urban areas. The classification between urban and rural community settings for each census tract in our sample was derived from the Census Bureau, which delineated urban and rural areas by population density and land use characteristics [29]. As for the SVI, we identified an individual's urban or rural census tract by the home address.
2.2. Regression model
In our empirical model, the dependent variable is whether a fully vaccinated individual received the first booster shot or not. A booster is an additional dose given to individuals who have completed their initial vaccine series: the first two doses for the Pfizer or Moderna COVID-19 vaccine, or one shot of Johnson and Johnson. The dependent variable equals one for an individual who received a booster during the study period. The predictors are age, gender, race and ethnicity, rural vs. urban community, and the SVI indicators as community-level measures of socioeconomic and demographic characteristics. To estimate the binary outcome variable, we applied a logistic generalized additive model (GAM) [[30], [31]]:
where and p is the probability of taking a booster shot. Coefficients and smoothing functions are parameters to be estimated. Because Age and SVI are continuous variables with numerical data, we applied nonlinear smooth functions as depicted by and , respectively, based on the panelized regression splines [30]. Race is a categorical variable that falls into the following six categories: White persons, Black/African American persons, Asian persons, American Indian/Alaska Native persons, Pacific Islander/Hawaiian persons, and persons of More Than One Race. The variable equals 1 for males and 0 for females.
The logistic GAM estimations were conducted with the “gam” package using the R software, version 4.2.2. The empirical work began with exploratory regression analyses for potential predictors. A backward selection of regressors with a statistical significance level of 10% or better was employed to determine the final model specifications. As a result, is represented by Hispanic persons vs. otherwise, regardless of race. Estimation results for specific race/ethnicity combinations, such as Black-Hispanic residents, are not statistically meaningful. Therefore, the results were not included in the final regressions as reported in Section 3 below.
In addition to the composite SVI, we report estimation results for two of its constituent components, namely socioeconomic status and housing/transportation. The other two components are highly correlated with the other demographic variables in the model. Intuitively, the “household composition” indicator is related to the variable, and the “minority status” indicator is related to and .
3. Empirical results
3.1. Vaccination data
Table 1 displays the sample broken down by demographic characteristics included in model estimations. Out of the sample of 184,252 fully vaccinated adult residents in Nueces County, 43% had received a booster by August 2022. Out of those with a booster, approximately 5% were in the age group of 18–25 years, 20% in 25–45 years, 60% in 45–75 years, and another 15% older than 75. Relatively more males than females did not receive a booster. The majority of the fully vaccinated population was White residents, followed by those belonging to more than one race. By comparison, Hispanic residents made up 55% of the sample without a booster and 49% with a booster. A total of 14,016 adult residents (7.6% of the county population) lived in a rural community setting.
Table 1.
Descriptive characteristics of the data sample (total sample size: 184,252).
| Variable | Level | Booster |
Non-booster |
||
|---|---|---|---|---|---|
| N = 78822 | % | N = 105430 | % | ||
| Age | 18–25 | 3934 | 5.0 | 14928 | 12.5 |
| 25–45 | 15539 | 19.7 | 39806 | 38.5 | |
| 45–75 | 47572 | 60.4 | 43677 | 42.2 | |
| 75+ | 11777 | 14.5 | 7019 | 6.8 | |
| Gender | Female | 44383 | 56.3 | 54221 | 51.4 |
| Male | 34431 | 43.7 | 51154 | 48.6 | |
| Race | White | 44425 | 56.4 | 66520 | 63.1 |
| Black/African American | 1512 | 1.9 | 2556 | 2.4 | |
| Asian | 1312 | 1.7 | 2611 | 2.5 | |
| American Indian/Alaska Native | 159 | 0.2 | 389 | 0.4 | |
| Pacific islander or Hawaiian | 34 | 0.0 | 155 | 0.1 | |
| More than one race | 31380 | 39.8 | 33199 | 31.5 | |
| Ethnicity | Non-Hispanic | 40418 | 51.3 | 47902 | 45.4 |
| Hispanic | 38404 | 48.7 | 57527 | 54.6 | |
| Urban | Urban | 73491 | 93.2 | 96745 | 91.8 |
| Rural | 5331 | 6.8 | 8685 | 8.1 | |
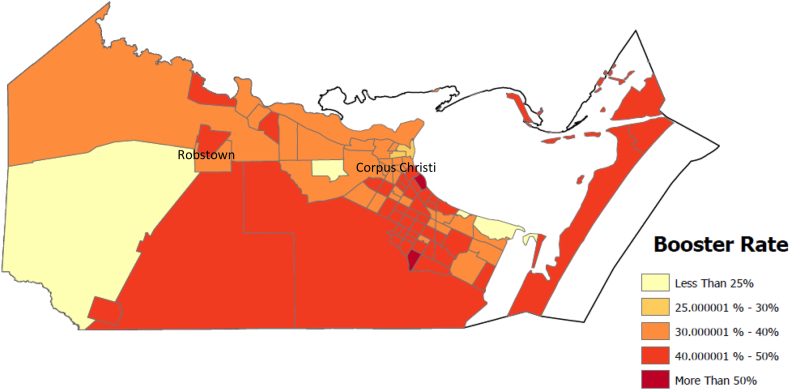
3.2. Spatial pattern of booster vaccination rate
The booster vaccine uptake in Nueces County varied remarkably across different neighborhoods. Fig. 1 is a map of the county and its 82 census tracts each indicating the population share of adults with a booster. Booster uptake appears to be lower in the northern portion of the county, especially near the downtown area of the city of Corpus Christi. On the contrary, the share of the boosted population is the highest among neighborhoods in the Southside district of the city. Residents in the Southside census tracts tend to be more affluent and educated than those in the downtown area [11].
Fig. 1.
Map of adults with a booster as a percentage of the fully vaccinated population in each census tract in Nueces County, Texas.
3.3. Model estimation results
Table 2 presents the results of the GAM regression described in Section 2.2 above. All alternative model specifications include individuals’ demographics, namely age, gender, race and ethnicity, along with the rural vs. urban environment. Variables without estimates represent the reference groups or baselines. The results are odds ratios (ORs) with corresponding confidence intervals. Most coefficient estimates are statistically significant. An odds ratio above (below) one suggests that the odds of taking a booster are higher (lower) for the predictor than for the corresponding benchmark group.
Table 2.
Sociodemographic and neighborhood factors on booster uptake (N = 184,252).
| Variable | Level | (1) |
(2) |
(3) |
(4) |
|---|---|---|---|---|---|
| Odds Ratio [p-value] (95% CI) | Odds Ratio [p-value] (95% CI) | Odds Ratio [p-value] (95% CI) | Odds Ratio [p-value] (95% CI) | ||
| Gender | Female | – | – | – | – |
| Male | 0.836 [<0.001] (0.835–0.836) | 0.834 [<0.001] (0.834–0.834) | 0.835 [<0.001] (0.834–0.835) | 0.836 [<0.001] (0.835–0.836) | |
| Race | White | – | – | – | – |
| Black/African American | 0.893 [0.014] (0.860–0.929) | 0.890 [0.001] (0.860–0.923) | 0.870 [<0.001] (0.837–0.906) | 0.884 [<0.001] (0.855–0.914) | |
| Asian | 0.900 [0.004] (0.863–0.938) | 0.893 [0.002] (0.859–0.928) | 0.916 [0.015] (0.877–0.954) | 0.903 [0.005] (0.872–0.936) | |
| American Indian/Alaska Native | 0.725 [0.001] (0.616–0.854) | 0.726 [0.001] (0.618–0.852) | 0.727 [<0.001] (0.617–0.856) | 0.727 [0.001] (0.623–0.847) | |
| Pacific islander or Hawaiian | 0.450 [<0.001] (0.315–0.642) | 0.453 [<0.001] (0.319–0.645) | 0.463 [<0.001] (0.324–0.661) | 0.459 [<0.001] (0.345–0.648) | |
| More than one race | 1.328 [<0.001] (1.326–1.329) | 1.330 [<0.001] (1.328–1.331) | 1.327 [<0.001] (1.325–1.329) | 1.329 [<0.001] (1.328–1.330) | |
| Ethnicity | Non-Hispanic | – | – | – | – |
| Hispanic | 0.949 [<0.001] (0.947–0.950) | 0.953 [<0.001] (0.952–0.954) | 0.915 [<0.001] (0.9144–0.9157) | 0.944 [<0.001] (0.943–0.945) | |
| Rural | Urban | – | – | – | – |
| vs. urban | Rural | 0.806 [<0.001] (0.794–0.938) | 0.80 [<0.001] (0.789–0.811) | 0.794 [<0.001] (0.783–0.805) | 0.804 [<0.001] (0.795–0.814) |
| Age | 25 vs. 18 | 1.027 [0.002] (1.013–1.042) | 1.026 [0.003] (1.008–1.043) | 1.034 [0.001] (1.013–1.052) | 1.035 [<0.001] (1.013–1.044) |
| 45 vs. 25 | 2.239 [<0.001] (2.236–2.241) | 2.228 [<0.001] (2.225–2.235) | 2.226 [<0.001] (2.219–2.234) | 2.231 [<0.001] (2.222–2.234) | |
| 75 vs. 45 | 3.050 [<0.001] (3.043–3.061) | 3.051 [<0.001] (3.040–3.063) | 3.032[<0.001] (3.027–3.041) | 3.058 [<0.001] (3.052–3.063) | |
| 100 vs. 75 | 0.424 [<0.001] (0.361–0.492) | 0.415 [<0.001] (0.363–0.480) | 0.421 [<0.001] (0.363–0.491) | 0.422 [<0.001] (0.361–0.483) | |
| SVI Index | Moderate (7.140) vs. Lowest (2.00) | 3.834 [<0.001] (2.352–5.684) | |||
| Highest (12.000) vs. Moderate (7.140) | 0.800 [<0.001] (0.767–0.836) | ||||
| Socio-economic Status | Moderate (1.940) vs. Lowest (0) | 1.342 [<0.001] (1.214–1.483) | 1.387 [<0.001] (1.234–1.559) | ||
| Highest (3.820) vs. Moderate (1.940) | 0.908 [0.002] (0.873–0.945) | 0.934 [<0.001] (0.895–0.975) | |||
| Housing/Transport-ation | Moderate(2.110) vs. Lowest (0) | 0.773 [<0.001] (0.634–0.842) | 0.732 [<0.001] (0.620–0.865) | ||
| Highest (3.970) vs. Moderate (2.110) | 0.845 [<0.001] (0.818–0.872) | 0.895 [<0.001] (0.869–0.922) |
The first model specification indicates that the odds of fully vaccinated adults in Nueces County taking a booster shot were lower for males [OR 0.836, 95% CI 0.835–0.836, p < 0.001] than females. Hispanic residents had lower odds of taking a booster [OR 0.949, 95% CI 0.947–0.950, p < 0.001] than non-Hispanic residents, and residents living in a rural area had lower odds of taking a booster [OR 0.806, 95% CI 0.794–0.938, p < 0.001] than those living an urban area. Other things being equal, White residents were more likely to take a booster than all other races, except those belonging to more than one race.
Table 2 also shows the results for the relationship between age and the receipt of a booster through the odds ratios of selected ages (age 25 vs. 18, age 45 vs. 25, age 75 vs. 45, and age 100 vs. 75). The odds ratio for “age 25 vs. 18” is the ratio between the odds of receiving a booster for 25-year-old residents and the odds for 18-year-old residents. As shown in the first model specification, residents aged 25 had slightly higher odds than the odds of residents aged 18 [OR 1.027, 95% CI 1.013–1.042, p < 0.001]. The odds ratio increases at each subsequent age benchmark through 75 [e.g., age 75 vs. 45 OR 3.050, 95% CI 3.043–3.061, p < 0.001].
The four model specifications in Table 2 differ by the community-level social vulnerability variables included. The odds ratios for these variables are reported for comparing the median (moderate) against the minimum SVI score (low), and for comparing the maximum score (highest) against the median. The first specification includes the composite SVI. The SVI scores range between 0 and 12 with a median of 7.140. The odds for Nueces County residents in moderately vulnerable neighborhoods to take a booster were higher than those in the least vulnerable neighborhoods [OR 3.834, 95% CI 2.352–5.684, p < 0.001]. Those living in the most vulnerable neighborhoods had lower odds compared to those living in a moderately vulnerable neighborhood [OR 0.804, 95% CI 0.767–0.836, p < 0.001]. Nonetheless, these results are for comparison only, as the overall community vulnerability index encompasses some demographic factors captured by other predictors.
The second model includes the SVI indicator for the socioeconomic status instead of the composite index. The odds ratios are reported for comparing the median SVI score (1.940) against the minimum (0) and for comparing the maximum (3.820) against the median. Accordingly, those living in a neighborhood with moderate socioeconomic vulnerability had higher odds compared to those living in a neighborhood with the lowest socioeconomic vulnerability [OR 1.342, 95% CI 1.214–1.483, p < 0.001]. However, those living in neighborhoods with the highest socioeconomic vulnerability had lower odds compared to those living in neighborhoods with moderate socioeconomic vulnerability [OR 0.908, 95% CI 0.873–0.945, p < 0.001].
The third model specification includes the housing/transportation component of SVI instead. Accordingly, those living in a neighborhood with a moderate housing/transportation vulnerability score of 2.110 had lower odds compared to those living in a neighborhood with the lowest housing/transportation vulnerability score of 0 [OR 0.773, 95% CI 0.634–0.842, p < 0.001]. Those living in neighborhoods with the highest housing/transportation vulnerability score of 3.970 had even lower odds than those living in neighborhoods with moderate housing/transportation vulnerability [OR 0.845, 95% CI 0.818–0.872, p < 0.001].
The final model specification includes the previous two constituent components of SVI. All coefficient estimates are close to their counterparts in the other specifications. This reflects the robustness of including both community-level social vulnerability variables in conjunction with the demographic variables. In addition, multicollinearity among predictors in the model is likely not a potential concern as their pairwise correlation coefficients are no higher than the conventional threshold of 0.5.
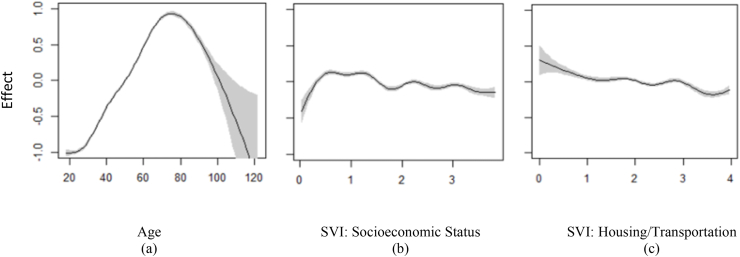
3.4. Age and social vulnerability
For the continuous variables representing age and two attributes of social vulnerability, Table 2 above presents the estimated odds ratios of some selected values of the predictors for illustration. The three plots in Fig. 2 further show the partial predictions corresponding to the full ranges of age, SVI socioeconomic status scores, and SVI housing/transportation scores, respectively, over the same vertical axis scale. Those plots essentially show estimates of the impacts of the three predictors along with the 95% confidence bands.
Fig. 2.
Estimated smoothing functions in GAM for booster uptake by age (a),social vulnerability – socioeconomic status (b), and social vulnerability – Housing/Transportation (c).
Fig. 2(a) shows a flat slope between ages 18 and 25 and then a positive slope through age 75. The slope is negative for ages above 75. This means that, for adults younger than 25 years, booster uptake does not change with age. For those between ages 25 and 75, booster uptake increases with each additional year. For those older than 75 years, booster uptake decreases with age. It is noteworthy that the estimates for most ages above 100 are indifferent from zero given the wide 95% confidence band, due in part to their considerably smaller sample sizes for these ages.
The other two panels of Fig. 2 show the impacts of social vulnerability conditions. According to Fig. 2(b), booster uptake increases with lower socioeconomic status among neighborhoods with the lowest socioeconomic vulnerability. Beyond those neighborhoods, however, booster uptake decreases with higher socioeconomic vulnerability. In Fig. 2(c)–a negative relationship between booster uptake and the social vulnerability condition also holds for the SVI indicator reflecting housing quality and transportation accessibility.
4. Discussion
This study contributes to a better understanding of the socioeconomic and demographic determinants for booster uptake using local official COVID-19 vaccination records of Nueces County in Texas, USA. There are several interesting findings. First, as well documented in the literature, booster uptake depended on individuals’ demographic characteristics [[9], [10], [11],20]. Among the fully vaccinated, Hispanic residents and most racial minorities were less likely to receive a booster shot. Seniors older than 75 were also less likely than the rest of the population to take the shot.
On the other hand, our finding of a higher booster uptake among females than males is at odds with the related literature. Paul and Fancourt [9] and Neely and Scacco [20] find no meaningful association between gender and the willingness to take a COVID-19 vaccine. Brownstein et al. [10] report a stronger intention among males than females, while Raman et al. [21] and Lee et al. [32] report the opposite results. Such discrepancies might be an outcome of differences in regional demographics. For instance, according to the 2020 Census data, 65% of the male population in Nueces County (67.6% nationwide) participates in the labor force, compared with 55.4% of females (58.7% nationwide). A lower booster uptake among males than females might stem from the interference of vaccination appointments with work schedules or concerns about the impact of potential side effects on work [32,33].
The related literature also underscores the role that age plays in vaccine uptake. Paul and Fancourt [9] report that those least willing to receive a COVID-19 vaccine are youth between 18 and 29 years old, and seniors older than 60 are most willing to receive a shot. On the contrary, Neely and Scacco [20] find that adults within the age group of 25–44 express more vaccine hesitancy than the younger age group of 18–24. Still, Raman et al. [21] find that older Americans are more likely to be fully vaccinated but then they are less likely to receive a booster. In this paper, the logistic GAM model has allowed us to visualize booster uptake among adults across the entire age spectrum. Interestingly, booster uptake is positively associated with age only between 25 and 75 years. Young adults might be more likely to have a false sense of confidence about their safety as they tend to be less severely affected by the coronavirus disease [34]. The elderly might be more concerned about side effects [33].
Our findings concerning the impact of socioeconomic disparities on vaccine uptake align with the existing literature [11,35,36]. Neely and Scacco [20] and Caspi et al. [35] find that Hispanic persons are more likely than non-Hispanic persons to express concerns and unwillingness to take COVID-19 shots. Lee et al. [32] attribute Hispanic persons’ particular vaccine hesitancy to their cultural beliefs. Our findings of lower booster uptake among socially vulnerable and rural neighborhoods align with the literature on vaccine hesitancy [37]. Sparks et al. [38] attribute a lack of vaccine uptake in rural areas to limited access to healthcare facilities. Taken together, empirical evidence on disparities in booster uptake raises questions about the equity of vaccine distribution and access, potentially leaving certain sociodemographic groups more vulnerable to the virus.
Nonetheless, it is important to note some limitations of our empirical work with local official records of a local public health district for a comprehensive understanding of vaccine behavior. Our dataset only includes adults who were fully vaccinated by February 2022, potentially limiting the generalizability of findings to a broader population, while raising concerns about the exclusion of later vaccinations, among others. Similarly, the exclusion of individuals without complete personal information might introduce selection bias, as those individuals may have different socioeconomic or demographic characteristics.
Furthermore, our dataset does not contain information about certain characteristics of individuals that might have affected vaccination outcomes. For instance, first, the social vulnerability indicators at the community level that we considered in model estimations may not fully capture the diverse socioeconomic attributes of individuals, such as their income levels and employment status. Second, our dataset lacks information about individuals with COVID-19 infection during the study period. This would potentially affect their likelihood of taking a booster. Third, the period spanning almost two years potentially leads to measurement errors due to migration, particularly those who moved out of the county after taking the initial COVID-19 vaccines. According to the Current Population Survey's database, Nueces County's annual out-migration was historically 4% of the total population [39]. The potential effects of these and similar factors on our empirical results should be taken into consideration.
5. Conclusions
We have studied COVID-19 booster uptake using official vaccination records of Nueces County in the state of Texas, USA, with a diverse population. Overall, the empirical results confirm that booster uptake varied across individuals of different socioeconomic and demographic characteristics. Male and Hispanic residents were less likely to receive a booster shot. Booster uptake was positively associated with age between 25 and 75. Those living in a rural area or socially vulnerable community were also less likely to take a booster. To advance health equity in Nueces County, a more inclusive vaccine campaign would involve targeting those traditionally underserved communities.
While the study provides a better understanding of sociodemographic and geographic disparities in a region, it remains unclear whether the findings from one county in Texas fully represent the entire nation and beyond. From this perspective, more fruitful research would extend the study area to other regions with different sociodemographic makeups.
Ethics statement
The study protocol was approved by Texas A&M University – Corpus Christi Institutional Review Board (IRB Number:TAMU–CC–IRB-2022-0448), and informed consent was waived due to the retrospective study design.
Data availability statement
The data that has been used is confidential.
CRediT authorship contribution statement
Yuxia Huang: Writing – review & editing, Writing – original draft, Validation, Software, Methodology, Investigation, Formal analysis, Conceptualization. Jim Lee: Writing – review & editing, Writing – original draft, Investigation, Formal analysis. Lei Jin: Methodology, Investigation. Md Mahabubur Rahman: Visualization, Formal analysis. Ana Guerrero: Investigation, Formal analysis. Meng Zhao: Resources, Data curation. Kyoung Lee: Resources, Data curation.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
This study was funded by the Natural Science Foundation (Grant No. 2112631).
Contributor Information
Yuxia Huang, Email: lucy.huang@tamucc.edu.
Jim Lee, Email: jim.lee@tamucc.edu.
Lei Jin, Email: lei.jin@tamucc.edu.
Md Mahabubur Rahman, Email: mahabubur.rahman@tamucc.edu.
Ana Guerrero, Email: aguerrero32@islander.tamucc.edu.
Meng Zhao, Email: mzhao@ncat.edu.
Kyoung Lee, Email: klee2023@hawaii.edu.
References
- 1.CDC Benefits of getting a COVID-19 vaccine. 2022. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/vaccine-benefits.html
- 2.Cameroni E., et al. Broadly neutralizing antibodies overcome SARS-CoV-2 Omicron antigenic shift. Nature. 2021;602:664–670. doi: 10.1038/s41586-021-04386-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Planas D., Saunders N., Maes P., et al. Considerable escape of SARS-CoV-2 Omicron to antibody neutralization. Nature. 2022;602(7898):671–675. doi: 10.1038/s41586-021-04389-z. [DOI] [PubMed] [Google Scholar]
- 4.Chalkias S., Eder F., Essink B., et al. Safety, immunogenicity and antibody persistence of a bivalent Beta-containing booster vaccine against COVID-19: a phase 2/3 trial. Nat. Med. 2022;28(11):2388–2397. doi: 10.1038/s41591-022-02031-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Choi A., Koch M., Wu K., Chu L., et al. Safety and immunogenicity of SARS-CoV-2 variant mRNA vaccine boosters in healthy adults: an interim analysis. Nat. Med. 2021;27(11):2025–2031. doi: 10.1038/s41591-021-01527-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.CDC CDC expands booster shot eligibility and strengthens recommendations for 12-17 year olds. 2022. https://www.cdc.gov/media/releases/2022/s0105-Booster-Shot.html
- 7.CDC CDC COVID data tracker: vaccinations in the US. 2022. https://covid.cdc.gov/covid-data-tracker/#vaccinations_vacc-people-additional-dose-totalpop
- 8.Loubet P., Laureillard D., Martin A., et al. Why promoting a COVID-19 vaccine booster dose? Anesthesia Critical Care & Pain Medicine. 2021;40 doi: 10.1016/j.accpm.2021.100967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Paul E., Fancourt D. Predictors of uncertainty and unwillingness to receive the COVID-19 booster vaccine: an observational study of 22,139 fully vaccinated adults in the UK. The Lancet Regional Health – Europe. 2022;14 doi: 10.1016/j.lanepe.2022.100317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brownstein N.C., Harika R., Whiting J., et al. COVID-19 vaccine behaviors and intentions among a national sample of United States adults ages 18–45. Prev. Med. 2022;160 doi: 10.1016/j.ypmed.2022.107038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee J., Huang Y. COVID-19 vaccine hesitancy: the role of socioeconomic factors and spatial effects. Vaccines. 2022;10(3):352. doi: 10.3390/vaccines10030352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McKinnon B., Quach C., Dube E., Nguyen C.T., Zinszer K. Social inequalities in COVID-19 vaccine acceptance and uptake for children and adolescents in Montreal, Canada. Vaccine. 2022;39(49):7140–7145. doi: 10.1016/j.vaccine.2021.10.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Prickett K.C., Habibi H., Carr P.A. COVID-19 vaccine hesitancy and acceptance in a cohort of diverse New Zealanders. The Lancet Regional Health – Western Pacific. 2021;14 doi: 10.1016/j.lanwpc.2021.100241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Urrunaga-Pastor D., Guido B.Q., Guido H.A., et al. Cross-sectional analysis of COVID-19 vaccine intention, perceptions and hesitancy across Latin America and the Caribbean. Trav. Med. Infect. Dis. 2021;41 doi: 10.1016/j.tmaid.2021.102059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Valckx S., Crevecoeur J., Verelst F., et al. Individual factors influencing COVID-19 vaccine acceptance in between and during pandemic waves (July-December 2020) Vaccine. 2022;40(1):151–161. doi: 10.1016/j.vaccine.2021.10.073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Frisco M.L., van Hook J., Thomas K.J.A. Racial/ethnic and nativity disparities in U.S. Covid-19 vaccination hesitancy during vaccine rollout and factors that explain them. Soc. Sci. Med. 2022;307 doi: 10.1016/j.socscimed.2022.115183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mondal P., Sinharoy A., Su L. Sociodemographic predictors of COVID-19 vaccine acceptance: a nationwide US-based survey study. Publ. Health. 2021;198:252–259. doi: 10.1016/j.puhe.2021.07.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nino M., Hearne B., Cai T. Trajectories of COVID-19 vaccine intentions among US adults: the role of race and ethnicity. SSM-Population Health. 2021;15 doi: 10.1016/j.ssmph.2021.100824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Reiter P.I., Pennell M.I., Katz M.I. Acceptability of a COVID-19 vaccine among adults in the United States: how many people would get vaccinated? Vaccine. 2020;38(42):6500–6507. doi: 10.1016/j.vaccine.2020.08.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Neely S., Scacco J. Receptiveness of American adults to COVID-19 vaccine boosters: a survey analysis. PEC Innovation. 2022;1 doi: 10.1016/j.pecinn.2022.100019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Raman S., et al. Omicron and likelihood of receiving a COVID-19 vaccine booster: evidence from a randomized choice-based experiment. Soc. Sci. Med. 2022;310 doi: 10.1016/j.socscimed.2022.115277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Murewanhema G., Musuka G., Mukwenha S., et al. Hesitancy, ignorance or uncertainty? The need for effective communication strategies as Zimbabwe's uptake of COVID-19 vaccine booster doses remains poor. Public Health in Practice. 2022;2 doi: 10.1016/j.puhip.2022.100244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Smith C.D., Mennis J. Incorporating geographic information science and technology in response to the COVID-19 pandemic. Prev. Chronic Dis. 2020;17(E58) doi: 10.5888/pcd17.200246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bennet K., Pumkam C., Probst J. Rural-urban differences in the location of influenza vaccine administration. Vaccine. 2011;29:5970–5977. doi: 10.1016/j.vaccine.2011.06.038. [DOI] [PubMed] [Google Scholar]
- 25.Cuadros D., Branscum A., Mukandavire Z., Miller F., MacKinnon N. Dynamics of the COVID-19 epidemic in urban and rural areas in the United States. Ann. Epidemiol. 2021;59(2021):16–20. doi: 10.1016/j.annepidem.2021.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dobis E.A., McGranahan D. vol. 2021. U.S. Department of Agriculture; Washington, DC: 2021. https://www.ers.usda.gov/amber-waves/2021/february/rural-residents-appear-to-be-more-vulnerable-to-serious-infection-or-death-from-coronavirus-covid-19 (Rural Residents Appear to Be More Vulnerable to Serious Infection or Death from Coronavirus COVID-19). [Google Scholar]
- 27.Corpus Christi Caller-Times Nueces county COVID-19 vaccine tracker: 57% of people fully vaccinated. 2022. https://www.caller.com/story/news/2022/02/16/gda-covid-19-vaccine-doses-corpus-christi-tx-nueces-county/62948087007/
- 28.CDC/ATSDR CDC/ATSDR social vulnerability index 2018 database Texas. Centers for disease Control and prevention/agency for toxic substances and disease registry/geospatial research, analysis, and Services program. 2022. https://www.atsdr.cdc.gov/placeandhealth/svi/data_documentation_download.html
- 29.Census Bureau Urban and rural. 2022. https://www.census.gov/programs-surveys/geography/guidance/geo-areas/urban-rural.html
- 30.Hastie T., Tibshirani R. Chapman and Hall; London: 1990. Generalized Additive Models. [DOI] [PubMed] [Google Scholar]
- 31.Wood S.N. second ed. Chapman & Hall; New York: 2017. Generalized Additive Models: an Introduction with R. [Google Scholar]
- 32.Lee R., Hu H., Kawaguchi E., et al. COVID-19 booster vaccine attitudes and behaviors among university students and staff in the United States: the USC Trojan pandemic research Initiative. Preventive Medicine Reports. 2022;28 doi: 10.1016/j.pmedr.2022.101866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rzymski P., Poniedzialek B., Fai A. Willingness to receive the booster COVID-19 vaccine dose in Poland. Vaccines. 2021;9:1286. doi: 10.3390/vaccines9111286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Maragakis L.L. December 2. Johns Hopkins Medicine; 2020. https://www.hopkinsmedicine.org/health/conditions-and-diseases/coronavirus/coronavirus-and-covid-19-younger-adults-are-at-risk-too (Younger Adults Are at Risk). [Google Scholar]
- 35.Caspi G., Dayan A., Eshal Y., et al. Socioeconomic disparities and COVID-19 vaccination acceptance: a nationwide ecologic study. Clin. Microbiol. Infection. 2021;27(10):1502–1506. doi: 10.1016/j.cmi.2021.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gertz A., Rader B., Sewalk K., Brownstein J.S. Emerging socioeconomic disparities in COVID-19 vaccine second-dose completion rates in the United States. Vaccines. 2022;10:121. doi: 10.3390/vaccines10010121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Saelee R., Zell E., Murthy B.P., et al. Disparities in COVID-19 vaccination coverage between urban and rural Counties – United States, December 14, 2020–January 31, 2022. MMWR Morbidity and Mortality Weekly Report. 2022;71:335–340. doi: 10.15585/mmwr.mm7109a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sparks G., Hamel L., Kirzinger A., et al. vol. 2021. Kaiser Family Foundation; Oakland, CA: 2021. https://www.kff.org/coronavirus-covid-19/poll-finding/kff-covid-19-vaccine-monitor-vaccine-attitudes-rural-suburban-urban/ (KFF COVID-19 Vaccine Monitor: Differences in Vaccine Attitudes between Rural, Suburban, and Urban Areas). [Google Scholar]
- 39.Census Bureau CPS migration/geographic mobility data tables. 2021. https://www.census.gov/topics/population/migration/data/tables/cps.html
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that has been used is confidential.