Abstract
Objectives
The delays and challenges people encounter when seeking abortion are well-documented, but their psychological implications are understudied. Aiming to fill this gap, we explored the associations between experiences of delay-causing obstacles to abortion care and adverse mental health symptoms among individuals seeking abortion care.
Study design
In 2019, we surveyed 784 people (of 1092 approached) ages 15–45 accessing abortion care in four clinics in abortion-supportive states: California, Illinois, and New Mexico. We conducted multivariable Poisson regressions to examine associations between experiencing delay-causing obstacles to abortion care and stress, anxiety, and depression at the abortion appointment. We also used Poisson regression to examine whether some individuals are more likely to experience delay-causing obstacles than others.
Results
Three in five participants (58%) experienced delay-causing obstacles when accessing abortion care. The most prevalent obstacles were cost-related (45%), followed by access-related (43%), and travel time-related (35%) delays. In adjusted analyses, experiencing any type of delay-causing obstacle to abortion care was significantly associated with more symptoms of stress, anxiety, and depression and higher risk of anxiety and depressive disorders. Participants were more likely to experience delay-causing obstacles if they traveled from another state or over 100 miles to reach the clinic, sought abortion beyond 13 weeks gestation, lacked money for unexpected expenses, and found it difficult to pay for the abortion.
Conclusion
Abortion is a time-sensitive healthcare, but most individuals are forced to delay care due to various obstacles that may have a negative impact on their psychological well-being.
Implications
Obstacles causing delays in accessing abortion care may contribute to elevated symptoms of stress, anxiety, and depression and higher risk of anxiety and depressive disorders for abortion patients. As restrictive policies increase, delays are likely to worsen, potentially leading to psychological harm for people seeking abortion.
Keywords: Abortion access, Abortion delay, Burden, Delayed healthcare, Mental health, Psychological well-being
1. Introduction
Although abortion is a time-sensitive healthcare service, multiple systemic, logistical, and financial obstacles force pregnant individuals to delay care and receive abortion later in pregnancy [1], [2], [3], [4]. Abortions later in gestation can constrain patients’ care choices [5], [6], and while they are very safe, they carry a relatively higher risk of complications compared to those obtained earlier [7]. Furthermore, the more abortion care is delayed, the more inaccessible it becomes, as barriers accumulate with advancing gestation. Abortions later in pregnancy are not only more expensive, but also harder to obtain due to the limited number of providers offering such services, necessitating extended travel and additional expenses [8], [9], [10], [11], [12]. Restrictive abortion policies and gestational bans compel many to travel out of their state of residence [13], further complicating and prolonging the process of obtaining care. Navigating these complexities is particularly burdensome for individuals from vulnerable and marginalized groups, especially those living on lower incomes, who are disproportionately impacted by abortion restrictions and encounter more delays than their counterparts [2], [14]. Studies show that the duration of these delays can vary widely, ranging from several days to weeks [2], [5], potentially pushing pregnant individuals past gestational duration limits and making it impossible for them to obtain care at all [4].
While obstacles to abortion care have been well-documented, we know less about the associations between experiencing delays to care and people’s mental health. Although rigorous research has consistently shown that having an abortion does not increase the risk of mental health disorders [15], [16], [17], [18], psychological symptoms of depression, anxiety, and stress are higher before the abortion, compared to afterward [16], [19]. Nonetheless, most studies examining mental health and abortion have focused on factors associated with post-abortion mental health, leaving the source of these higher pre-abortion psychological symptoms less studied. Given the overwhelming challenges and considerable delays individuals face when seeking abortion care, these could be key determinants of negative mental health symptoms at the time of seeking an abortion.
A few qualitative studies have documented the emotional toll of delay-causing obstacles, including prolonged processes of referrals and Medicaid coverage application, lengthy appointment scheduling, time needed to raise funds to pay for the procedure, increased travel distances to reach a clinic, and multiple visits requirements [5], [20], [21], [22]. While these studies lay an important groundwork, more is needed to further understand the psychological burden of encountering delays when seeking abortion care. To our knowledge, no study has quantified the relationships between delay-causing obstacles and mental health symptoms pre-abortion. To address this critical literature gap, this analysis aims to answer the following research questions: (1) To what extent do individuals accessing abortion care in abortion-supportive states experience delay-causing obstacles? (2) Are certain groups of individuals more likely to experience delay-causing obstacles to abortion care? and (3) Is the experience of delay-causing obstacles to abortion care associated with adverse mental health symptoms at the time of the abortion seeking?
2. Methods
2.1. Study design
This analysis is based on cross-sectional survey data collected from individuals seeking abortion care as part of the Burden Study, which aimed to describe the psychosocial burden of seeking abortion in the United States [23]. Data was collected before the U.S. Supreme Court decision in Dobbs v. Jackson Women’s Health Organization in June 2022, eliminating the constitutional right to abortion [24]. As detailed elsewhere [23], between January and June 2019, we recruited participants from four abortion clinics in three states supportive of abortion (California, Illinois, and New Mexico). These states allowed abortions later in pregnancy, had no mandated waiting period laws, and bordered states with more restricted access. The selected recruitment sites served a diverse population of patients, including those traveling from other states to access care, enabling us to capture a variety of abortion-seeking experiences. To be eligible for the study, participants needed to be pregnant and seeking abortion services, aged 15 years or older, able to speak and read English or Spanish, and not pre-medicated with narcotics for a planned procedure. Research staff introduced the study to potential participants while they were waiting for their abortion appointment. After confirming eligibility and providing consent, participants completed a self-administered questionnaire on a tablet device in either English or Spanish, according to their preferences. Research staff were available to assist with any questions. Participants completed the questionnaire in approximately 20 minutes and received a $30 gift card as compensation for their time. The study was approved by the University of California, San Francisco Institutional Review Board.
2.2. Outcome variables
We included three continuous mental health measures as dependent variables: symptoms of stress, anxiety, and depression. Stress was assessed using Cohen’s Perceived Stress Scale, which is the sum of four Likert-scaled items (e.g., “In the last month, how often have you felt that you were unable to control the important things in your life?”) with response options ranging from “never” to “very often” (α = 0.62, range 0–16) [25]. Anxiety was measured using the Generalized Anxiety Disorder (GAD-7) scale, consisting of the sum of seven Likert-scaled items (e.g., “Over the last two weeks, how often have you been bothered by being so restless that it is hard to sit still?”) with response options ranging from “not at all” to “nearly every day” (α = 0.94, range 0–21) [26]. Depression was assessed using the Patient Health Questionnaire-2 (PHQ-2), which sums two Likert-scaled items (e.g., “Over the last two weeks, how often have you been bothered by little interest or pleasure in doing things?”) with response options ranging from “not at all” to “nearly every day” (α = 0.86, range 0–6) [27]. We also created two dichotomous variables to assess whether people screened at risk of moderate to severe anxiety disorder, based on the GAD-7 recommended cutoff score of 10 or greater [26], and major depressive disorder, based on the PHQ-2 recommended cutoff score of 3 or greater [27].
2.3. Exposure variables
Our main independent variables of interest were delay-causing obstacles to accessing abortion. We asked participants to indicate if any of the following obstacles delayed them from obtaining care: (1) “Travel costs”, (2) “Procedure costs”, (3) “Insurance coverage”, (4) “Finding a place that does abortions”, (5) “Figuring out how to get to a clinic”, (6) “Not knowing where to go”, (7) “Finding a place to do the procedure this far along”, (8) “Travel time to obtain care to end this pregnancy”, and (9) “Needing multiple visits”. We grouped these responses by theme into three categories: cost-related delays (obstacles 1–3), access-related delays (obstacles 4–7), and travel time-related delays (obstacles 8–9).
2.4. Statistical analyses
To address research question 1, measuring the extent that participants accessing abortion care in abortion-supportive states experienced delay-causing obstacles, we performed descriptive statistics to describe the sample (Table 1) and the prevalence of delay-causing obstacles (Fig. 1). To answer research question 2 and assess the associations between participants’ characteristics and delay-causing obstacles, we ran Poisson regressions for each individual characteristic of interest. We included recruitment site as a covariate to account for the clustered nature of the data (Table 2). For research question 3, we conducted multivariable Poisson regressions to examine the associations between delay-causing obstacles and symptoms of anxiety, depression, and stress. Covariates were selected a-priori based on previous research [18] and on their association with delay-causing obstacles or mental health symptoms. We adjusted for socioeconomic characteristics (confidence in one’s ability to come up with $2000 if an unexpected need arose next month), current pregnancy characteristics (relationship with the man involved in the pregnancy and retrospective pregnancy intentions), and abortion seeking characteristics (gestational duration, seeking abortion due to fetal medical condition, maternal health concerns, or because pregnancy was the result of rape, and recruitment site). History of depression or anxiety, adverse childhood experiences, and problem substance use were also included (Table 3). We then estimated the marginal predictive mean symptoms of anxiety, depression, and stress by delay-causing obstacles using the margins command in Stata [28]. Lastly, we assessed the proportion of those screened at risk of moderate to severe anxiety or major depressive disorder by delay-causing obstacles. To address missing data, we employed multiple imputations using chained equations and dropped observations with missing outcome data prior to all regression analyses [29]. All analyses were performed using Stata version 17 (College Station, TX).
Table 1.
Demographic, socioeconomic, pregnancy, abortion seeking, and mental health characteristics of people seeking abortion in 2019 in four clinics in California, Illinois, and New Mexico (N = 784)
| Participants’ characteristics | N (%) |
|---|---|
| Demographic characteristics | |
| Age group (years) | |
| 15-17 | 38 (5) |
| 18-19 | 59 (7) |
| 20-24 | 199 (26) |
| 25-29 | 230 (29) |
| 30-39 | 234 (30) |
| 40-45 | 24 (3) |
| Self-reported race/ethnicity | |
| White, non-Hispanic | 208 (27) |
| Black, non-Hispanic | 208 (27) |
| Hispanic/Latina/Latinx | 179 (23) |
| Asian, Native Hawaiian, Pacific Islander, non-Hispanic | 46 (6) |
| Mixed race or other race/ethnicity | 86 (11) |
| Missing | 57 (6) |
| Socioeconomic characteristics | |
| Confidence in ability to come up with $2000 if an unexpected need arose next month | |
| Not at all confident | 356 (45) |
| Only slightly confident | 155 (20) |
| Somewhat confident | 121 (15) |
| Very confident | 79 (11) |
| Missing | 73 (9) |
| Has health insurance | 564 (72) |
| Difficulty finding money to pay to for abortion | |
| Not at all difficult | 346 (44) |
| A little bit difficult | 132 (17) |
| Somewhat difficult | 152 (19) |
| Very difficult | 146 (19) |
| Missing | 8 (1) |
| Current pregnancy characteristics | |
| Current relationship with the man involved in the pregnancy | |
| Very committed intimate relationship | 373 (48) |
| Somewhat committed intimate relationship | 103 (13) |
| Friends with benefits | 48 (6) |
| In contact but not in intimate relationship | 77 (10) |
| Not in contact/no relationship | 114 (14) |
| Other | 3 (1) |
| Missing | 66 (8) |
| Retrospective pregnancy intentions of current pregnancy | |
| Mistimed (wanted pregnancy sooner/later) | 270 (34) |
| Pregnancy wanted | 33 (4) |
| Wanted pregnancy never | 326 (42) |
| Not sure what wanted | 152 (19) |
| Missing | 3 (1) |
| Abortion seeking characteristics | |
| Gestational duration at the time of abortion (weeks) | |
| ≤12 | 548 (70) |
| 13-19 | 112 (14) |
| ≥20 | 113 (14) |
| Missing | 11 (2) |
| Seeking abortion due to fetal medical condition | 30 (4) |
| Seeking abortion due to maternal health concerns | 120 (15) |
| Seeking abortion because pregnancy is result of rape or sexual assault | 14 (2) |
| Traveled out-of-state to abortion clinic | 257 (33) |
| One-way distance traveled to abortion clinic (miles) | |
| ≤25 | 396 (51) |
| 26-50 | 101 (13) |
| 51-75 | 43 (5) |
| 76-100 | 39 (5) |
| >100 | 205 (26) |
| Recruitment site | |
| Clinic A | 248 (32) |
| Clinic B | 214 (27) |
| Clinic C | 212 (27) |
| Clinic D | 110 (14) |
| Mental health, childhood adversity, and substance use history | |
| History of depression or anxiety diagnosis | 196 (25) |
| History of adverse childhood experiences, any of following: | 265 (34) |
| Lived with someone who had a drinking problem | 178 (23) |
| Witnessed violence in the neighborhood | 173 (22) |
| Lived with someone who was mentally ill or depressed | 125 (16) |
| Lived with someone who served time in jail or prison | 126 (16) |
| Felt unsupported, unloved, or unprotected at home | 122 (15) |
| Missing | 49 (6) |
| History of problem substance use in the past year | 266 (34) |
| Monthly, weekly, or daily use of any illicit or street drugs or prescription drugs for recreational use | 99 (13) |
| Monthly, weekly, or daily use of four or more alcoholic drinks on one occasion | 233 (30) |
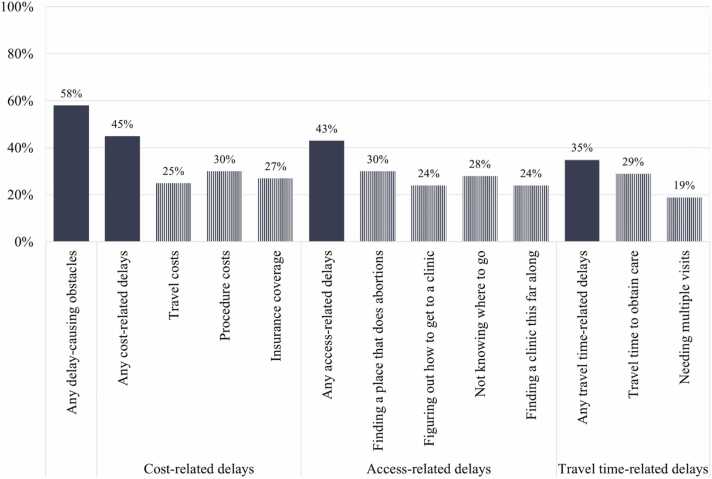
Fig. 1.
Unadjusted prevalence of delay-causing obstacles to abortion care among people seeking abortion in 2019 in four clinics in California, Illinois, and New Mexico (N = 784).
Table 2.
Poisson regression analyses assessing associations between selected characteristics of people seeking abortion in 2019 in four clinics in California, Illinois, and New Mexico, and delay-causing obstacles to abortion care, adjusted for recruitment site (N = 784)
| Delay-causing obstacles to abortion care |
||||
|---|---|---|---|---|
| Any delay-causing obstacles | Cost-related delays | Access-related delays | Travel time-related delays | |
| %, Adjusted prevalence ratio (95% CI)a | %, Adjusted prevalence ratio (95% CI)a | %, Adjusted prevalence ratio (95% CI)a | %, Adjusted prevalence ratio (95% CI)a | |
| Demographic characteristics | ||||
| Age group (years) | ||||
| 15-17 | 55%, 0.88 (0.55-1.40) | 42%, 0.83 (0.48-1.41) | 53%, 1.03 (0.63-1.67) | 32%, 0.76 (0.41-1.40) |
| 18-19 | 61%, 0.91 (0.63-1.33) | 54%, 1.02 (0.68-1.53) | 53%, 0.98 (0.65-1.48) | 47%, 1.12 (0.72-1.74) |
| 20-24 (reference) | 61%, 1.00 | 48%, 1.00 | 46%, 1.00 | 36%, 1.00 |
| 25-29 | 53%, 0.90 (0.70-1.16) | 39%, 0.85 (0.64-1.14) | 39%, 0.86 (0.64-1.16) | 32%, 0.97 (0.70-1.35) |
| 30-39 | 53%, 0.87 (0.68-1.12) | 41%, 0.87 (0.65-1.16) | 34%, 0.74 (0.55-0.01) | 29%, 0.84 (0.60-1.18) |
| 40-45 | 37%, 0.57 (0.29-.13) | 17%, 0.32 (0.12-0.89)* | 21%, 0.43 (0.17-1.06) | 12%, 0.33 (0.10-1.04) |
| Self-reported race/ethnicity | ||||
| White, non-Hispanic (reference) | 61%, 1.00 | 48%, 1.00 | 42%, 1.00 | 36%, 1.00 |
| Black, non-Hispanic | 49%, 0.86 (0.66-1.12) | 36%, 0.83 (0.61-1.12) | 37%, 0.98 (0.71-1.34) | 26%, 0.87 (0.61-1.25) |
| Hispanic/Latina/Latinx | 58%, 0.86 (0.66-1.13) | 43%, 0.78 (0.57-1.06) | 42%, 0.85 (0.62-1.17) | 36%, 0.79 (0.56-1.11) |
| Asian, Native Hawaiian, Pacific Islander, non-Hispanic | 65%, 1.02 (0.68-1.53) | 52%, 1.04 (0.66-1.64) | 52%, 1.17 (0.73-1.85) | 43%, 1.17 (0.71-1.94) |
| Mixed race or other race/ethnicity | 70%, 1.09 (0.80-1.48) | 55%, 1.06 (0.75-1.50) | 51%, 1.13 (0.78-1.62) | 44%, 1.09 (0.74-1.61) |
| Socioeconomic characteristics | ||||
| Confidence in ability to come up with $2000 for unexpected needs next month | ||||
| Not at all confident | 65%, 1.86 (1.25-2.77)** | 53%, 2.93 (1.69-5.05)*** | 48%, 1.83 (1.15-2.91)** | 39%, 1.81 (1.08-3.03)* |
| Only slightly confident | 60%, 1.64 (1.07-2.53)** | 48%, 2.49 (1.40-4.42)** | 41%, 1.49 (0.90-2.47) | 33%, 1.42 (0.81-2.48) |
| Somewhat confident | 58%, 1.64 (1.05-2.56)** | 37%, 2.05 (1.12-3.75)* | 42%, 1.59 (0.94-2.69) | 36%, 1.70 (0.96-3.00) |
| Very confident (reference) | 34%, 1.00 | 18%, 1.00 | 25%, 1.00 | 20%, 1.00 |
| Has health insurance | ||||
| Yes (reference) | 56%, 1.00 | 41%, 1.00 | 42%, 1.00 | 34%, 1.00 |
| No | 66%, 1.20 (0.96-1.49) | 56%, 1.43 (1.12-1.82)** | 45%, 1.14 (0.87-1.48) | 36%, 1.12 (0.84-1.50) |
| Difficulty finding money to pay for abortion | ||||
| Not at all difficult (reference) | 40%, 1.00 | 21%, 1.00 | 27%, 1.00 | 20%, 1.00 |
| A little bit difficult | 58%, 1.54 (1.16-2.05)** | 42%, 2.07 (1.45-2.94)*** | 37%, 1.41 (1.00-2.00)* | 33%, 1.71 (1.17-2.51)** |
| Somewhat difficult | 66%, 1.77 (1.37-2.30)*** | 58%, 2.86 (2.09-3.91)*** | 47%, 1.80 (1.32-2.45)*** | 41%, 2.12 (1.50-3.00)*** |
| Very difficult | 80%, 2.08 (1.61-2.69)*** | 77%, 3.63 (2.68-4.91)*** | 67%, 2.42 (1.81-3.24)*** | 55%, 2.51 (1.80-3.51)*** |
| Current pregnancy characteristics | ||||
| Retrospective pregnancy intentions of current pregnancy | ||||
| Mistimed (wanted pregnancy sooner/later) | 58%, 1.08 (0.65-1.80) | 45%, 1.82 (0.89-3.73) | 43%, 1.27 (0.68-2.37) | 34%, 0.95 (0.52-1.73) |
| Pregnancy wanted (reference) | 51%, 1.00 | 24%, 1.00 | 33%, 1.00 | 36%, 1.00 |
| Wanted pregnancy never | 57%, 1.06 (0.64-1.74) | 44%, 1.77 (0.87-3.62) | 40%, 1.17 (0.63-2.16) | 35%, 0.95 (0.52-1.73) |
| Not sure what wanted | 50%, 0.88 (0.52-1.49) | 37%, 1.41 (0.67-2.96) | 39%, 1.07 (0.56-2.04) | 25%, 0.63 (3.33-1.22) |
| Abortion seeking characteristics | ||||
| Gestational duration at the time of abortion (weeks) | ||||
| ≤12 (reference) | 47%, 1.00 | 34%, 1.00 | 30%, 1.00 | 24%, 1.00 |
| 13-19 | 70%, 1.33 (1.01-1.75)* | 56%, 1.43 (1.05-1.94)* | 59%, 1.72 (1.26-2.34)*** | 48%, 1.56 (1.11-2.19)** |
| ≥20 | 80%, 1.45 (1.09-1.92)** | 66%, 1.55 (1.13-2.12)** | 72%, 1.88 (1.37-2.58)*** | 58%, 1.59 (1.13-2.24)** |
| Seeking abortion due to fetal medical condition | ||||
| Yes | 57%, 0.87 (0.53-1.42) | 40%, 0.76 (0.42-1.36) | 37%, 0.68 (0.37-1.25) | 50%, 1.13 (0.66-1.92) |
| No (reference) | 55%, 1.00 | 42%, 1.00 | 41%, 1.00 | 32%, 1.00 |
| Traveled out-of-state to abortion clinic | ||||
| Yes | 59%, 1.48 (1.16-1.89)*** | 49%, 1.76 (1.34-2.32)*** | 46%, 1.77 (1.33-2.34)*** | 37%, 1.70 (1.26-2.30)*** |
| No (reference) | 54%, 1.00 | 39%, 1.00 | 38%, 1.00 | 31%, 1.00 |
| One-way distance traveled to abortion clinic (miles) | ||||
| ≤25 (reference) | 47%, 1.00 | 32%, 1.00 | 29%, 1.00 | 19%, 1.00 |
| 26-50 | 45%, 0.92 (0.67-1.27) | 36%, 1.05 (0.72-1.52) | 27%, 0.87 (0.57-1.33) | 25%, 1.17 (0.74-1.85) |
| 51-75 | 58%, 1.06 (0.69-1.63) | 40%, 1.03 (0.61-1.72) | 44%, 1.27 (0.77-2.08) | 35%, 1.37 (0.78-2.40) |
| 76-100 | 77%, 1.47 (1.98-2.22) | 44%, 1.16 (0.68-1.98) | 72%, 2.01 (1.29-3.14)** | 46%, 1.85 (1.07-3.19)* |
| >100 | 73%, 1.47 (1.15-1.88)** | 66%, 1.90 (1.44-2.51)*** | 63%, 1.99 (1.49-2.66)*** | 60%, 2.49 (1.79-3.44)*** |
p < 0.05.
p < 0.01.
p < 0.001.
Adjusted prevalence ratios derived from Poisson regression models using multiple imputation and adjusted for recruitment site.
Table 3.
Multivariable associations between delay-causing obstacles to abortion care and stress, anxiety and depression among people seeking abortion in 2019 in four clinics in California, Illinois, and New Mexico (N = 784)
| Stress | Anxiety |
Depression |
|||
|---|---|---|---|---|---|
| Symptoms (0-16) | Symptoms (0-21) | At risk of moderate to severe anxiety disorder | Symptoms (0-6) | At risk of major depressive disorder | |
| aPR (95% CI) | aPR (95% CI) | aPR (95% CI) | aPR (95% CI) | aPR (95% CI) | |
| Any delay-causing obstacles to abortion care | 1.18 (1.10-1.26)*** | 1.32 (1.24-1.40)*** | 1.40 (1.06-1.84)** | 1.33 (1.19-1.48)*** | 1.44 (1.09-1.90)** |
| Cost-related delays | 1.12 (1.05-1.19)*** | 1.25 (1.18-1.32)*** | 1.34 (1.03-1.74)* | 1.30 (1.17-1.45)*** | 1.49 (1.14-1.94)** |
| Access-related delays | 1.09 (1.02-1.16)** | 1.21 (1.14-1.29)*** | 1.29 (1.00-1.68)* | 1.19 (1.07-1.33)*** | 1.25 (0.96-1.62)* |
| Travel time-related delays | 1.10 (1.03-1.18)** | 1.30 (1.23-1.38)*** | 1.33 (1.02-1.74)* | 1.31 (1.17-1.46)*** | 1.41 (1.08-1.85)** |
aPR, adjusted prevalence ratio; CI, confidence interval.
All analyses are multivariable Poisson regression models using multiple imputation and adjust for ability to come up with $2000 for an unexpected need, relationship with man involved in the pregnancy, pregnancy intentions, gestational duration, seeking abortion due to fetal anomaly, maternal health concerns, or rape, recruitment site, history of depression or anxiety, history of ACEs, and history of problem substance use.
p < 0.001.
p < 0.01.
p < 0.05.
3. Results
Out of 1092 individuals approached by research staff, 846 (77%) agreed to participate and 824 (75%) were eligible and initiated the survey. Among them, 784 (95%) completed at least one-fifth of the questionnaire, constituting the multiple imputation sample for this analysis. Our sample characteristics closely resemble those of a national sample of abortion patients seeking clinic-based care in terms of age, gestational duration, and race/ethnicity [14]. Most participants (70%) obtained an abortion at 12 weeks gestation or earlier, with the majority being in their twenties (55%), and approximately one-quarter identified as non-Hispanic Black (27%), White (27%), or Hispanic/Latina (23%). While many participants had health insurance (72%), nearly two in five found it very difficult (19%) or somewhat difficult (19%) to find money to pay for their abortion, and about half (45%) were not at all confident in their ability to come up with $2000 for unexpected expenses. Half of the sample (49%) lived more than 25 miles from the clinic where they sought an abortion, and one-third (33%) lived in another state from the abortion clinic (Table 1).
Three in five participants (58%) reported experiencing delay-causing obstacles when accessing abortion care. Delays related to cost were the most common type (45%), followed by access-related delays (43%), and travel time-related delays (35%) (Fig. 1). According to Poisson regression analyses examining the association between participant characteristics and delay-causing obstacles, adjusted for recruitment site, participants who traveled from another state (adjusted Prevalence Ratio [aPR] 1.48, 95% confidence interval [CI] 1.16–1.89) or over 100 miles to reach the abortion clinic (aPR 1.47, 95% CI 1.15–1.88) were significantly more likely to experience any type of delay-causing obstacles compared to their counterparts. Those who obtained their abortion at 13 to 19 weeks gestation (aPR 1.33, 95% CI 1.01–1.75) or beyond 20 weeks gestation (aPR 1.45, 95% CI 1.09–1.92) were also significantly more likely to have experienced delay-causing obstacles compared to those with a gestational duration of 12 weeks or less. Additionally, participants who lacked money for unexpected expenses (aPR 1.86, 95% CI 1.25–2.77), and those who found it very difficult to find money to pay for their abortion (aPR 2.08, 95% CI 1.61–2.69) were significantly more likely to experience all types of delay-causing obstacles compared to their counterparts (Table 2).
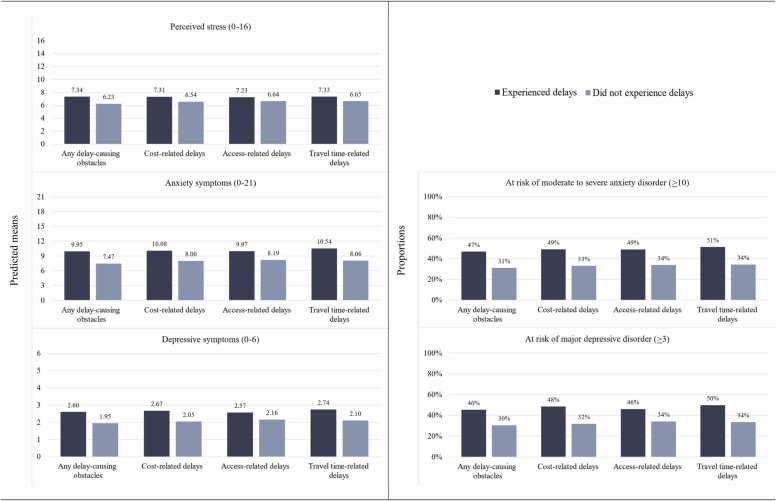
In multivariable Poisson regression analyses adjusting for participant characteristics and recruitment site, experiencing any type of delay-causing obstacles, including cost-related, access-related, and travel-time related obstacles to abortion care, was significantly associated (p < 0.05) with more symptoms of stress, anxiety, and depression, and higher risk of moderate to severe anxiety disorder and major depressive disorder (Table 3). Predicted mean symptoms of stress, anxiety, and depression and proportion of those screened at risk of anxiety and depressive disorders by delay-causing obstacles are presented in Figure 2.
Fig. 2.
Predicted mean adverse mental health symptoms and proportion screening at risk of anxiety and depressive disorders by delay-causing obstacles to abortion care among people seeking abortion in 2019 in four clinics in California, Illinois, and New Mexico (N = 784).
4. Discussion
The present study sought to explore the psychological implications of encountering delay-causing obstacles in accessing abortion care. We found that a substantial proportion of individuals seeking abortion services – three in five – experienced delays to care due to various obstacles. In the current post-Dobbs context and in more restrictive settings, delays are likely to be even more pronounced [30]. Importantly, we found that experiences of delay-causing obstacles corresponded with significantly higher levels of stress, anxiety, and depression symptoms and greater risk of moderate to severe anxiety disorder and major depressive disorder. To the best of our knowledge, our study is the first to provide such evidence about the quantitative relationships between delay-causing obstacles to abortion care and people’s mental health. These novel results reinforce qualitative research that focuses on the emotional burden of seeking abortion in the U.S. [5], [20], [21], [22]. They also suggest that policies that restrict access and lead to delays, such as mandated waiting period laws and gestational limits, may be negatively associated with the psychological well-being of people trying to obtain abortion care [23].
Our findings underscore the crucial role that financial constraints play in individuals’ ability to access timely abortion care. Cost-related delays were the most frequently reported type of obstacle among our participants. The groups of people more likely to experience delays included individuals lacking money for unexpected expenses and people who found it very difficult to procure funds for the procedure. These results echo the existing literature showing that the cost of abortion and related expenses are major barriers for individuals seeking abortion in the U.S. [2], [4], [11] and that people living on lower incomes face lengthier abortion-seeking processes compared to their counterparts [2], [14]. People may be caught in a cycle: raising funds to pay for the abortion could cause substantial delays, which can then lead to additional expenses, since abortion price rises with advancing gestation [8], [11]. Furthermore, over one-quarter of our participants experienced delays related to insurance costs. This aligns with studies indicating that even in states where Medicaid coverage is available, eligible abortion patients do not necessarily have their procedure paid for by the program, due to complex reimbursement processes [8], [11]. Qualitative studies have similarly described the negative emotional impact on abortion patients when they could not use insurance or had to rely on financial aid to secure the necessary funds [9], [31]. Also consistent with previous research [13], [32], [33], we found that delay-causing obstacles were more likely to be experienced by individuals who lived far from the clinic or had to cross state lines to reach care. This emphasizes the uneven geographical distribution of clinics in the country that forces people to travel considerably long distances to obtain care, while managing multiple financial and logistical challenges such as transportation, accommodation, and lost wages [9], [34]. Our results corroborate this work and expand on this knowledge, demonstrating that obstacles not only extend the process of seeking care but may also contribute to worse psychological outcomes for those in need of these services.
While our study provides valuable insights, it is not without limitations. The cross-sectional design restricts us from drawing causal conclusions. Our sample only represents individuals seeking clinic-based abortion care, and our recruitment sites were located in abortion-supportive states pre-Dobbs, limiting generalizability. Furthermore, although we accounted for clustering by including a fixed effect for site, as suggested for small number of clusters [35], this approach may reduce statistical power, limiting our ability to detect true effects. Additionally, variations in state drug policies may have impacted the validity of our pre-pregnancy illicit drug use measure; for instance, cannabis was legal in California and Illinois but not in New Mexico during our study and people’s responses may have varied by state of residence. Future prospective research in more diverse regions post-Dobbs and among individuals obtaining abortion outside of the healthcare system is necessary to fully understand the impact of barriers and delays on mental health.
Nonetheless, this study offers a robust analysis, and in light of the recent changes to abortion access, it gains even greater importance. With the overturning of Roe v. Wade and increased restrictions and bans on abortion, delays in care are likely to become more prevalent and consequential [30]. As pregnant individuals struggle with accessing the healthcare they need and are forced to navigate complex legal risks and longer distances to reach these time-sensitive services, the accompanying psychological symptoms may intensify, potentially leading to further harm.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Declaration of interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Funding: This work was supported by a Resource Allocation Program Award from the UCSF Clinical and Translational Science Institute’s Pilot Awards Program, and an Advancing New Standards in Reproductive Health Core grant. The first author is supported by the Society of Family Planning Research Fund, Emerging Scholars in Family Planning grant (SFPRF15-ES17). The second author is supported by a Eunice Kennedy Shriver National Institute of Child Health and Human Development, Office of Research on Women's Health, Building Interdisciplinary Research Careers in Women's Health grant (K12 HD052163). The funders had no role in the study design, data collection, analysis, interpretation, or publication.
References
- 1.Drey E.A., Foster D.G., Jackson R.A., et al. Risk factors associated with presenting for abortion in the second trimester. Obstet Gynecol. 2006;107(1):128–135. doi: 10.1097/01.AOG.0000193608.14463.11. [DOI] [PubMed] [Google Scholar]
- 2.Finer L.B., Frohwirth L.F., Dauphinee L.A., et al. Timing of steps and reasons for delays in obtaining abortions in the United States. Contraception. 2006;74(4):334–344. doi: 10.1016/j.contraception.2006.04.010. [DOI] [PubMed] [Google Scholar]
- 3.French V., Anthony R., Souder C., et al. Influence of clinician referral on Nebraska women’s decision-to-abortion time. Contraception. 2016;93(3):236–243. doi: 10.1016/j.contraception.2015.10.006. [DOI] [PubMed] [Google Scholar]
- 4.Upadhyay U.D., Weitz T.A., Jones R.K., et al. Denial of abortion because of provider gestational age limits in the United States. Am J Pub Health. 2022;112(9):1305–1312. doi: 10.2105/AJPH.2022.310984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carpenter E., Gyuras H., Burke K.L., et al. Seeking abortion care in Ohio and Texas during the COVID-19 pandemic. Contraception. 2023;118 doi: 10.1016/j.contraception.2022.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wingo E., Ralph L.J., Kaller S., et al. Abortion method preference among people presenting for abortion care. Contraception. 2021;103(4):269–275. doi: 10.1016/j.contraception.2020.10.004. [DOI] [PubMed] [Google Scholar]
- 7.Bartlett L.A., Berg C.J., Shulman H.B., et al. Risk factors for legal induced abortion–related mortality in the United States. Obstet Gynecol. 2004;103(4):729–737. doi: 10.1097/01.AOG.0000116260.81570.60. [DOI] [PubMed] [Google Scholar]
- 8.Foster D.G., Kimport K. Who seeks abortions at or after 20 weeks? Perspect Sex Reprod Health. 2013;45(4):210–218. doi: 10.1363/4521013. [DOI] [PubMed] [Google Scholar]
- 9.Kimport K. Reducing the burdens of forced abortion travel: referrals, financial and emotional support, and opportunities for positive experiences in traveling for third-trimester abortion care. Soc Sci Med. 2022;293 doi: 10.1016/j.socscimed.2021.114667. [DOI] [PubMed] [Google Scholar]
- 10.Makleff S., Blaylock R., Ruggiero S., et al. Travel for later abortion in the USA: lived experiences, structural contributors and abortion fund support. Cult Health Sex. 2023:1–7. doi: 10.1080/13691058.2023.2033834. [DOI] [PubMed] [Google Scholar]
- 11.Roberts S.C., Gould H., Kimport K., et al. Out-of-pocket costs and insurance coverage for abortion in the United States. Women's Health Issues. 2014;24(2):e211–e218. doi: 10.1016/j.whi.2013.12.002. [DOI] [PubMed] [Google Scholar]
- 12.Witwer E., Jones R.K., Fuentes L., et al. Abortion service delivery in clinics by state policy climate in 2017. Contraception: X. 2020;2 doi: 10.1016/j.conx.2020.100043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Smith M.H., Muzyczka Z., Chakraborty P., et al. Abortion travel within the United States: an observational study of cross-state movement to obtain abortion care in 2017. Lancet Regional Health–Am. 2022:10. doi: 10.1016/j.lana.2022.100159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jones RK, Jerman J. Time to appointment and delays in accessing care among U.S. abortion patients. Guttmacher Institute, 2016.
- 15.Charles V.E., Polis C.B., Sridhara S.K., et al. Abortion and long-term mental health outcomes: a systematic review of the evidence. Contraception. 2008;78(6):436–450. doi: 10.1016/j.contraception.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 16.Major B., Cozzarelli C., Cooper M.L., et al. Psychological responses of women after first-trimester abortion. Arch Gen Psychiatry. 2000;57(8):777–784. doi: 10.1001/archpsyc.57.8.777. [DOI] [PubMed] [Google Scholar]
- 17.Munk-Olsen T., Laursen T.M., Pedersen C.B., et al. Induced first-trimester abortion and risk of mental disorder. N Engl J Med. 2011;364(4):332–339. doi: 10.1056/NEJMoa0905882. [DOI] [PubMed] [Google Scholar]
- 18.Biggs M.A., Upadhyay U.D., McCulloch C.E., et al. Women’s mental health and well-being 5 years after receiving or being denied an abortion: a prospective, longitudinal cohort study. JAMA Psychiatry. 2017;74(2):169–178. doi: 10.1001/jamapsychiatry.2016.3478. [DOI] [PubMed] [Google Scholar]
- 19.Steinberg J.R., Tschann J.M., Furgerson D., et al. Psychosocial factors and pre-abortion psychological health: the significance of stigma. Soc Sci Med. 2016;150:67–75. doi: 10.1016/j.socscimed.2015.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jung C., Fiastro A., Cornell A., et al. Patient perspectives on barriers in obtaining timely abortion care in Los Angeles, California. Contraception. 2023;117:50–54. doi: 10.1016/j.contraception.2022.12.005. [DOI] [PubMed] [Google Scholar]
- 21.Kimport K., Rasidjan M.P. Exploring the emotional costs of abortion travel in the United States due to legal restriction. Contraception. 2023;120 doi: 10.1016/j.contraception.2022.12.004. [DOI] [PubMed] [Google Scholar]
- 22.Odum T., Heymann O., Turner A.N., et al. Assessing psychosocial costs: Ohio patients’ experiences seeking abortion care. Contraception. 2023;117:45–49. doi: 10.1016/j.contraception.2022.12.007. [DOI] [PubMed] [Google Scholar]
- 23.Biggs M.A., Neilands T.B., Kaller S., et al. Developing and validating the psychosocial burden among people seeking abortion scale (PB-SAS) PloS One. 2020;15(12) doi: 10.1371/journal.pone.0242463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.State Laws and Policies: an overview of abortion laws. Guttmacher Institute; 2023. 〈https://www.guttmacher.org/state-policy/explore/overview-abortion-laws〉 (accessed September 19, 2023).
- 25.Cohen S., Kamarck T., Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983:385–396. doi: 10.2307/2136404. [DOI] [PubMed] [Google Scholar]
- 26.Spitzer R.L., Kroenke K., Williams J.B., et al. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 27.Kroenke K., Spitzer R.L., Williams J.B. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care. 2003:1284–1292. doi: 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- 28.Williams R. Using the margins command to estimate and interpret adjusted predictions and marginal effects. Stata J. 2012;12(2):308–331. doi: 10.1177/1536867×1201200209. [DOI] [Google Scholar]
- 29.Von Hippel P.T. Regression with missing Ys: an improved strategy for analyzing multiply imputed data. Sociol Methodol. 2007;37(1):83–117. doi: 10.1111/j.1467-9531.2007.00180.x. [DOI] [Google Scholar]
- 30.Rader B., Upadhyay U.D., Sehgal N.K., et al. Estimated travel time and spatial access to abortion facilities in the US before and after the Dobbs v Jackson Women’s Health decision. JAMA. 2022;328(20):2041–2047. doi: 10.1001/jama.2022.16222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dennis A., Manski R., Blanchard K. Does Medicaid coverage matter?: a qualitative multi-state study of abortion affordability for low-income women. J Health Care Poor Underserved. 2014;25(4):1571–1585. doi: 10.1353/hpu.2014.0162. [DOI] [PubMed] [Google Scholar]
- 32.Brown B.P., Hebert L.E., Gilliam M., et al. Distance to an abortion provider and its association with the abortion rate: a multistate longitudinal analysis. Perspect Sex Reprod Health. 2020;52(4):227–234. doi: 10.1363/psrh.12101. [DOI] [PubMed] [Google Scholar]
- 33.Cartwright A.F., Karunaratne M., Barr-Walker J., et al. Identifying national availability of abortion care and distance from major US cities: systematic online search. J Med Internet Res. 2018;20(5) doi: 10.2196/jmir.9820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Barr-Walker J., Jayaweera R.T., Ramirez A.M., et al. Experiences of women who travel for abortion: a mixed methods systematic review. PloS One. 2019;14(4) doi: 10.1371/journal.pone.0209991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.McNeish D., Stapleton L.M. Modeling clustered data with very few clusters. Multivar Behav Res. 2016;51(4):495–518. doi: 10.1080/00273171.2016.1167008. [DOI] [PubMed] [Google Scholar]