ABSTRACT
Background
Conservative care (CC) is a viable treatment option for some patients with kidney failure. Choosing between dialysis and CC can be a complex decision in which involvement of patients is desirable. Gaining insight into the experiences and preferences of patients regarding this decision-making process is an important initial step to improve care. We aimed to identify what is known about the perspective of patients regarding decision-making when considering CC.
Methods
PubMed, EMBASE and Cochrane databases were systematically searched on 23 February 2023 for qualitative and quantitative studies on patient-reported experiences on decision-making about CC. Data were analysed thematically.
Results
Twenty articles were included. We identified three major themes: creating awareness about disease and treatment choice, decision support and motivation to choose CC. Patients were often not aware of the option to choose CC. Patients felt supported by their loved ones during the decision-making process, although they perceived they made the final decision to choose CC themselves. Some patients felt pressured by their healthcare professional to choose dialysis. Reported reasons to choose CC were maintaining quality of life, treatment burden of dialysis, cost and the desire not to be a burden to others. In general, patients were satisfied with their decision for CC.
Conclusions
By focussing on the perspective of patients, we identified a wide range of patient experiences and preferences regarding the decision-making process. These findings can help to improve the complex decision-making process between dialysis and CC and to provide patient-centred care.
Keywords: dialysis, end-stage kidney disease, shared decision making, supportive care
 Watch the video of this contribution at https://academic.oup.com/ndt/pages/author_videos
Watch the video of this contribution at https://academic.oup.com/ndt/pages/author_videos
KEY LEARNING POINTS.
What was known:
Conservative care (CC) is increasingly recognised as a viable treatment option for older and frail patients with chronic kidney disease (CKD), for whom kidney transplantation is often not feasible and dialysis might yield limited survival benefit with potentially high treatment burden.
Although the perspective of healthcare professionals on this decisional process between dialysis and CC has been evaluated in several studies, an overview of the experiences and preferences of patients is lacking.
This study adds:
We identified a wide range of experiences, including the preference for a timely start of counselling about all treatment options and clear communication about the benefits and risks and prognosis of each treatment option.
The decision-making process is facilitated by involvement of loved ones. Patients appreciate the presentation of CC as a team-based and active approach.
The main barriers in decision making are limited awareness and knowledge about CKD and CC. Some patients feel persuaded by their healthcare professionals to choose dialysis and perceive a lack of choice.
Potential impact:
This scoping review provides comprehensive insights to improve the decision-making process by taking into account what is valued most by patients.
We emphasize the importance of timely education about CC in an understandable way and to invest in a trusting relationship between the healthcare professional and patient.
We developed a list of recommendations to improve the decisional process and to provide patient-centred care in order to support patients to choose a treatment option that fits their lives best.
INTRODUCTION
In general, patients with advanced chronic kidney disease (CKD) have three different treatment options when their kidney function deteriorates: kidney transplantation, dialysis and conservative care (CC). CC focusses on maintaining quality of life and treating symptoms, often combined with interventions to delay the progression of kidney disease and manage complications of kidney failure [1]. CC may especially suit older and frail patients for whom kidney transplantation is often not feasible and dialysis might yield limited survival benefit with potentially high treatment burden [2–4].
Choosing between dialysis and CC can be a complex decision, as there are multiple reasonable options, each with different potential benefits, risks and impacts on patients’ lives. This makes the decisional process ideally suited for shared decision making (SDM). Patient involvement during the process of selecting a treatment modality in advanced CKD is associated with increased treatment satisfaction [5, 6]. Although international guidelines recommend the use of SDM, its implementation in daily practice remains limited [1, 7, 8].
The perspective of healthcare professionals on decision making about dialysis or CC has been evaluated in previous studies, but an overview of patients’ perspectives is lacking [9, 10]. Gaining insights into the experiences and preferences of patients regarding the decision-making process is an important initial step to improve SDM. Therefore, we aimed to identify what is known about the perspective of patients regarding decision making when considering CC.
MATERIALS AND METHODS
We performed a scoping review, given the exploratory nature of the research question. Results were reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) extension for Scoping Reviews (Supplemental Table S1) [11].
Search strategy and selection criteria
The Cochrane Library, EMBASE and PubMed databases were searched for empirical studies using synonyms for ‘chronic kidney disease’, ‘conservative care’ and ‘decision making’. The full search strategy is provided in Supplement 2.
As we aimed to describe the perspective of patients in the decision-making process, we excluded articles that did not provide patient-reported data. Articles had to be on the subject of treatment modality decisions, either focussing solely on CC or CC and kidney replacement therapy (KRT) with the option of CC included. Articles reporting solely on advance care planning or dialysis withdrawal were excluded because we focussed on the initial treatment modality choice. Both qualitative and quantitative studies were eligible. Reviews were excluded after screening for additional references. After removing duplicates, titles and abstracts were screened for relevance in duplicate by two reviewers (M.J. and S.d.L.). After reaching consensus, full-text articles of relevant studies were assessed independently by the same two reviewers. Disagreements were resolved by discussion with a third reviewer (M.v.O.).
Data extraction and analysis
Data on the number of included patients, their characteristics (patient demographics, CKD stage) and study characteristics (study methodology, authors, country and year of publication) were extracted. Results on patient perspectives in the decision-making process were extracted from both qualitative and quantitative studies. Data from sources other than self-reported by patients (e.g. medical records or reports by healthcare professionals) were excluded. We performed a thematic synthesis with two independent reviewers (M.J. and S.d.L.) coding the text line by line, developing descriptive themes and subsequently analytic themes. Disagreements were resolved in consensus meetings. Due to the exploratory aim of this scoping review, we did not assess the methodological quality of included studies.
RESULTS
Study selection
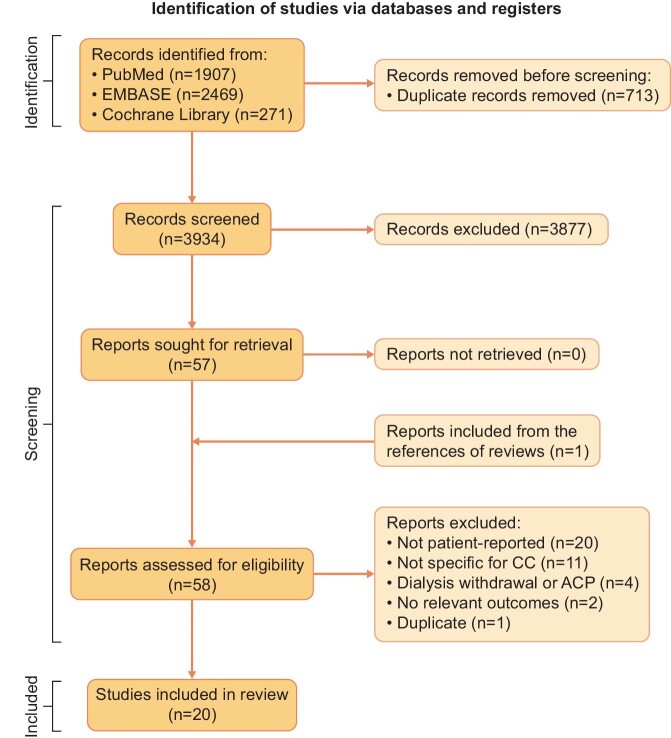
The literature search was conducted on 9 June 2022 and updated on 23 February 2023. This resulted in 3934 articles after duplicate removal. One relevant article was identified after checking the reference lists of reviews, which was published in a non-indexed journal. We assessed 58 full-text articles for eligibility, of which 38 were excluded because they did not provide data reported by patients (n = 20), did not specifically include information about CC (n = 11), focused on withdrawal from dialysis or advanced care planning (n = 4), had no relevant outcomes (n = 2) or were duplicates (n = 1). This led to the inclusion of 20 articles. An overview of the selection process is provided in Fig. 1.
Figure 1:
Study selection flow diagram [11]. ACP: advance care planning.
Study characteristics
Characteristics of the 20 included studies are described in Table 1. All articles were published after 2004 and were performed in the USA, UK, the Netherlands, France, Singapore and Australia. The majority (12/20) were qualitative studies using interviews. In addition, we included five cross-sectional survey studies, two randomised controlled trials (RCTs) and one pre-/post-intervention study that assessed an education tool. Eleven studies included patients who were facing the treatment decision. Overall, the studies included 2351 CKD patients, of whom only 94 had chosen CC; 135 had chosen dialysis and 2122 were yet to make their treatment decision. All studies except one reported the age of the participants, with a mean or median age of ≥65 years.
Table 1:
Characteristics of the included studies.
| Study population | Identified themes | ||||||
|---|---|---|---|---|---|---|---|
| First author, country, year | Study design | Number of participantsa | Age (years) | Stage CKD | Creating awareness | Decision support | Motivation to choose CC |
| Ashby [28], Australia, 2005 | Interviews | 7 patients who had chosen CC (4 dialysis withdrawal, 5 caregivers) | Range 57–89, median 77 | Stage 5b | X | X | |
| Eneanya [12], USA, 2020 | Interviews | 10 patients considering CC (16 healthcare professionals, 5 caregivers) | All ≥65, mean 73 | eGFR <20 ml/min/1.73 m2 | X | ||
| Eneanya [19], USA, 2020 | RCT | 100 patients before treatment decision | All ≥65, median 75 | Stage 4–5 | X | X | |
| Finkelstein [15], Singapore, 2018 | Survey | 151 patients before treatment decision | All ≥65 | Stage 3B–5 | X | X | X |
| Frazier [22], USA, 2022 | Survey | 350 patients before treatment decision | All ≥70, mean 78 | Stage 4 | X | X | X |
| Hamroun [18], France, 2022 | Survey | 1206 patients before treatment decision (137 healthcare professionals) | Mean 68 ± 13 | Stage 3–4 | X | ||
| Han [25], Singapore, 2019 | Interviews | 4 patients who had chosen CC (12 dialysis patients, 7 caregivers) | All ≥70 | Stage 5 | X | X | X |
| House [17], USA, 2022 | Interviews | 29 patients before treatment decision (10 healthcare professionals) | All ≥65, mean 73 | eGFR ≤20 ml/min/1.73 m2 | X | X | |
| Johnston [29], UK, 2012 | Interviews | 9 patients who had chosen CC | Range 74–96, mean 86 | Stage 5 | X | X | |
| Karlin [20], USA, 2019 | Interviews | 1 patient who had chosen CC, 5 considering CC (8 patients on dialysis, 6 caregivers) | All ≥65, mean 73.6 | eGFR ≤20 ml/min/1.73 m2 | X | X | X |
| Morton [31], Australia, 2012 | Survey | 105 patients before treatment decision (73 caregivers) | Median 67 | Stage 3–5 | X | ||
| Noble [30], UK, 2009 | Interviews | 30 patients considering CC (17 caregivers) | Unknown | Stage 4–5c | X | X | |
| Oestreich [13], USA, 2021 | Interviews | 14 patients before treatment decision (6 caregivers) | All ≥75, mean 79 | eGFR ≤20 ml/min/1.73 m2 | X | X | X |
| Seah [24], Singapore, 2015 | Interviews | 9 patients who had chosen CC | Range 61–84, median 81 | Stage 5 | X | X | X |
| Selman [14], UK, 2019 | Interviews | 20 patients who had chosen CC | Range 69–95, median 82 | Stage 5 | X | X | X |
| Tonkin-Crine [21], UK, 2018 | Interviews | 14 patients who had chosen CC (14 pre-dialysis patients, 14 on dialysis) | Range 74–92, mean 82 | Stage 5 | X | X | X |
| Verberne [23], Netherlands, 2019 | Survey | 24 patients who had chosen CC (75 patients on dialysis) | All ≥70, mean 84 | Stage 4–5 | X | X | X |
| Visser [27], Netherlands, 2009 | Interviews | 6 patients who had chosen CC (8 dialysis patients) | All ≥65, mean 82.5 | Stage 5b | X | X | |
| Wong [26], USA, 2023 | RCT | 92 patients considering CC (56 family members) | All ≥75, mean 82 ± 6 | Stage 4–5 | X | X | |
| Zimmerman [16], USA, 2020 | Pre/post study | 30 patients before treatment decision (16 healthcare professionals) | All ≥70, range 71–96 | eGFR <20 ml/min/1.73 m2 | X | X | |
ESRD: end-stage renal disease; RCT: randomised controlled trial.
Number of participants who either had chosen CC, are considering CC or with unknown preference for treatment modality (before treatment decision). In parentheses is the participants in the study who are not included in this review.
In the study mentioned as ESKD.
cIn the study mentioned as advanced CKD.
Synthesis
Three major themes and 10 subthemes were identified. The major themes were creating awareness about disease and treatment choice, decision support and motivation to choose CC.
Theme 1: creating awareness about disease and treatment choice
The first theme described the process of creating awareness among patients regarding their kidney disease, prognosis and the treatment decision that eventually had to be made. It comprised three subthemes: knowledge about disease progression and prognosis, awareness of treatment choice and timing of introduction of treatment choice. These subthemes were addressed in 15 articles [12–26].
Knowledge about disease progression and prognosis
Patients missed information on disease progression and wanted more open conversations about their individual prognosis [12–14]. In a study among 151 pre-dialysis patients, 43% did not know the expected survival with dialysis or CC or whether survival would differ between these treatment options [15]. If the prognosis was uncertain, patients preferred that healthcare professionals share this uncertainty [13, 14]. Other patients preferred that prognostic information regarding their kidney disease was shared with them sooner, before the choice between treatment modalities was presented [16]. On the other hand, patients described that knowledge about disease progression caused stress and did not change their lifestyle [14, 17].
Awareness of treatment choice
Many patients did not remember whether they had been informed about CC as a treatment option. In a study among 1206 CKD patients, only 56 patients (4.6%) were aware of CC. This number increased with age (21% of patients >75 years of age) [18]. In another study among 151 pre-dialysis patients ≥75 years of age, 40% were unaware of CC as a treatment option [15]. Eight other studies assessed patients’ awareness about CC with similar results [12, 13, 17, 19–22, 26].
Timing of introduction of choice
In a study among 24 patients >70 years of age who had chosen CC, education about treatment options was initiated when the estimated glomerular filtration rate (eGFR) decreased below 20 ml/min/1.73 m2. A total of 93% of these patients were satisfied with the timing of counselling. No other studies specified when counselling about treatment options was initiated. In another study, 17 of 20 patients who had chosen CC felt well-informed at the time of choosing a treatment [14]. However, some preferred earlier counselling than they received from their healthcare professional. In other studies, a few participants felt counselling was initiated too soon, either because they immediately rejected dialysis and did not need extensive deliberation, or because it caused them stress [23, 24]. Others took time to weigh the perceived benefits and risks of treatment options, shaped by their personal values in life [25].
Theme 2: decision support
The second major theme we identified was decision support. Support during the decision-making process helps patients deliberate on the benefits and potential risks of treatment options. We identified three subthemes: sources and content of information, communication style and terminology used and the roles of patients, loved ones and healthcare professionals in the decision-making process. Seventeen studies reported about this theme [13–17, 19–30].
Sources and content of information
Patients received information about CC from nephrologists and kidney nurses, supplemented with leaflets and education sessions [14]. Others gained information through friends, family or media before seeing their healthcare professional [24]. This often resulted in negative impressions about dialysis, considering dialysis as painful and burdensome and believing others died due to dialysis [24, 25, 28]. One study addressed the role of fellow patients, but none of the patients felt that peer support would have been helpful [29].
Three studies evaluated the effect of educational programs and a patient decision aid (PtDA) [16,19,26]. One of these studies implemented a scenario tool that employs best- and worst-case scenarios to illustrate the treatment options. Patients appreciated the clarity of the prognostic information included in the aid. Some were startled by the confronting prognostic information or were frustrated that their healthcare professional had not shared this information with them earlier [16]. An RCT assessed whether a video-based education tool improved knowledge of CC compared with verbal education. Although knowledge increased significantly after education, no differences between the groups were found in knowledge or preference for treatment modality. The participants found the video helpful, appreciated the content and would recommend it to others [19]. Another RCT tested whether the use of a PtDA on CC aided the discussion about CC between patients and their healthcare professionals. Patients >75 years of age were randomised between standard education and education supplemented with the PtDA. Of the patients who received the PtDA, 26% discussed CC with their healthcare professionals, compared with 3% of controls [26].
Communication style and terminology used
Patients appreciated when healthcare professionals took time to explain the disease and treatment options and to answer their questions. They favoured straightforward communication [14]. Patients described straightforward communication as comprehensive and clear, without being insensitive. Others criticised the repetition of information about the management of their disease and the focus on laboratory results instead of an individualized approach [17]. Patients emphasised the importance of continuity of care to build a good relationship with their healthcare professionals [13, 14, 29].
Several patients had the impression that CC was an equivalent to ‘doing nothing’ and ‘imminent death’ [13, 20]. Patients appreciated CC more if it was presented as a team-based, whole-person, active approach with a focus on delaying disease progression [13]. In one study, some patients did not perceive CC as a reasonable treatment option, even if it aligned with their stated goals in life. The authors suggested that the participants either misunderstood what CC encompasses or equated it with death [20].
Roles of patients, loved ones and healthcare professionals in the decision-making process
Many patients perceived they had made the final choice for CC themselves [14, 23–25, 27, 29]. They valued their own treatment preferences as the most important opinion and expressed that they made an independent or self-directed decision [23, 25, 29]. At the same time, patients preferred to involve their loved ones and felt supported by them [14, 23–25]. Some patients determined their preference for treatment modality by themselves before involving their family [24]. Other patients felt persuaded by their family or healthcare professionals to choose dialysis [14, 17, 23, 25, 30].
Several studies described an asymmetrical relationship between patients and their healthcare professionals. Patients felt pushed to choose dialysis and considered themselves not in a position to question the healthcare professional's recommendation [17, 21, 25]. Others even avoided discussing the decision with their medical team, because they felt pressured to choose dialysis [24]. In a study among 151 pre-dialysis patients, half of the participants valued the healthcare professional's opinion about the best treatment modality as the most dominant factor in their decision. They would switch their choice for CC to dialysis or vice versa if their healthcare professional recommended them to [15]. Other patients perceived to have no choice to commence dialysis due to their comorbidities [29]. In other studies, patients felt supported in their decision by their healthcare professionals [23, 25, 30].
Theme 3: motivation to choose CC
The third and final theme on motivation to choose CC comprises four subthemes: quality of life and burden of dialysis treatment, burden to loved ones and the healthcare system, cost and decisional regret. Frequently mentioned reasons to choose CC are expressed in these topics. Fourteen studies reported on this theme [13–15, 20–25, 27–31].
Quality of life and burden of dialysis treatment
Quality of life and a sense of life completion were important reasons to choose CC. In particular, older participants said they had a fulfilled life and did not necessarily want to further prolong their life [13, 14, 21, 23–25, 28, 29]. Choosing CC was often a result of rejecting dialysis. Patients perceived dialysis as painful and burdensome and expected that dialysis would have interfere with their daily life. Without dialysis, patients expected to maintain autonomy in daily life, spend less time in the hospital and have more freedom to travel [14, 23–25, 27, 28, 30, 31]. Transport to the dialysis centre was also a major concern, as patients did not want to rely on hospital transportation or their loved ones [21, 27, 29]. Others believed that dialysis would result in a better quality of life and a prolonged life [20, 21, 27].
Burden to loved ones and the healthcare system
Patients often expressed that they wanted to avoid becoming a burden to their loved ones. Patients were concerned about becoming more dependent on their families and caregivers after starting dialysis. They mentioned increased caregiving responsibilities, financial burden and the time investment their caregivers would need to make [21, 23–25, 28, 29]. In some studies this was a major reason not to choose dialysis [25, 28]. Others mentioned giving priority to their loved ones’ well-being rather than prolonging their own life [24]. Additionally, some patients did not want to be a burden to the healthcare system [21, 28].
Cost
Three studies, all conducted in Singapore, reported cost as a decision-making factor. The additional financial burden of dialysis was an important reason to choose CC [15, 24, 25]. Although CC is less expensive than dialysis, some patients also worried about the expenses for consultations and medication [24].
Decisional regret
In general, patients were satisfied with their choice of CC [14, 23, 24, 27]. They were mostly satisfied with the information provided and stated they were adequately informed at the time of decision making [14, 23]. According to these patients, decision making could have been improved by providing information earlier on all reasonable treatment options earlier, tailored to an individual's situation [23]. Some patients who felt pressured to choose CC were unhappy at the time the treatment decision was made [14]. One study measured how patients perceived SDM during their choice of treatment modality using a validated questionnaire about the decision-making process. Higher levels of SDM were associated with being well-informed, greater satisfaction with medical care and greater decisional certainty [22]. In two studies, patients mentioned CC as a potentially temporary management strategy, with an option to change their decision and commence dialysis if personal goals and circumstances changed [13, 21].
DISCUSSION
This scoping review provides an overview of patient experiences and preferences during the decision-making process when choosing between dialysis and CC. To our knowledge, this is the first review focussing on the perspective of patients. We identified three main themes: creating awareness about disease and treatment choice, decision support and motivation to choose CC. A list of recommendations to improve the decision-making process based on the main findings of this review is provided in Table 2.
Table 2:
Recommendations on improving decision making in the treatment of kidney failure, based on the main findings of the scoping review.
| 1. Create awareness about the disease and treatment options • Provide information about CKD including prognostic information • Create awareness about the future treatment decision well before the decision needs to be made • Assess patient's preferences regarding information provision and timing of education about treatment options • List all (reasonable) treatment options: kidney transplantation, dialysis and CC 2. Provide support during the decision-making process • Provide comprehensive information and use transparent and honest communication • Build a trusting relationship and offer continuity of care • Encourage patients to ask questions and to participate proactively in the decision-making process • Involve family members and caregivers in the decision-making process • Provide information about the benefits and risks of each treatment option • Regarding CC: note that patients appreciate when CC is framed as an active approach • Ask patients whether they use other sources of information in order to respond to information retrieved by the patient. Patients frequently have pre-existing opinions regarding treatment modalities, based on friends, family or media • Offer decision-making support, like information on paper, digital educational programs, PtDAs and peer support 3. Help patients to make a preference-based decision • Help patients to elucidate their motivation to choose a particular treatment modality. ○ Frequently mentioned reasons to choose CC are quality of life, autonomy and sense of life completion ○ Frequently mentioned reasons against dialysis are treatment burden, time investment, transportation to the hospital or dialysis centre, being a burden to loved ones or the healthcare system in terms of time and cost |
The first theme identified in our review addressed patients’ awareness about CKD and the treatment choice that has to be made. Many patients were not aware of CC as a treatment option, despite the older age of the participants in the included studies. We could not trace whether patients actually did receive information about CC, except for one study [20]. The authors stated that at least four of seven patients were informed about CC, but apparently patients did not perceive it as a treatment option for them. This suggests that counselling about CC is not sufficient, as information about CC might be lacking at all or is not offered in an understandable way. This can hamper SDM when CC is a reasonable option, as knowledge of all treatment options is crucial to be able to consider them and make a well-informed decision [32].
Previous studies found that healthcare professionals struggle with what information to provide about CKD and treatment options, due to the complexity of the disease, uncertainty about the disease course and the complexity and preference sensitivity of treatment modalities [10, 33]. Barriers identified among healthcare professionals regarding education about CC are hesitation on how to approach the topic, uncertainty whether a patient would benefit from CC, fear about the patient's response after suggesting CC as a reasonable treatment option and doubts about the patient’s capacity to understand the information [10, 32, 34]. Communication skills training for healthcare professionals, educational programs for patients and PtDAs can help to overcome these barriers [35, 36], complemented with increased awareness and knowledge about CC among healthcare professionals.
Patients had conflicting views about the optimal timing to initiate counselling about treatment modalities. Most patients would have preferred to have received this information earlier, although not all. Previous studies stressed the importance of a timely initiation of this discussion to provide sufficient time to elaborate on the options, prevent hasty decisions and have enough time left to prepare for the chosen modality [37, 38]. As patients’ preferences for the timing of counselling vary, we advise to inform patients in advance that there is a future decision to make when their kidney function deteriorates further and to assess patients’ preferences about the timing of education about these treatment options early on.
International guidelines recommend SDM when choosing a treatment modality for advanced CKD [1]. Key elements of SDM are the involvement of patients and reaching a joint decision that reflects patients’ values and preferences [39]. However, patients across the reviewed articles perceived a lack of choice due to an asymmetrical relationship with their healthcare professional. This power imbalance was also identified as a major barrier in several systematic reviews, which focused on the decision-making process for a KRT modality [38], commencing or withholding dialysis [40] and SDM in general [41]. Although the included studies mentioned a power imbalance as the main reason patients perceived to have no choice, other explanations exist. Healthcare professionals might steer decision-making unintentionally due to their own preference about which treatment suits the patient best. Previous research showed that implicit persuasion is common in the process of choosing a treatment modality [42]. Additionally, patient decision making might be driven by fear of death or might be further complicated due to cognitive impairment and uraemia [43].
In our review, many patients expressed that they made the decision for CC by themselves. The Dutch Kidney Patient Association has found that many patients look for lived experience stories or peer support. Surprisingly, the role of PtDAs was evaluated in only one of the studies included. Recently, an overview was provided of tools to support CKD patients in choosing a treatment modality [44]. Of 145 tools identified, only 26 addressed CC. In general, patients who had used these tools were more informed about treatment options and took a more active role in choosing a treatment compared with those who did not use these tools.
The third theme comprised the motivation to choose CC. Often-mentioned reasons to choose CC in our review were maintaining quality of life, a sense of life completion and the desire not to be a burden to loved ones. The choice of CC was often the result of rejecting dialysis because of perceived physical treatment burden, expected interference with daily life, concerns about transport to the dialysis centre and cost. These findings are in line with previous research [38, 40, 45]. We recommend to elicit patients’ values and goals in life during the decision-making process, aiming to help patients make a decision that fits their lives best.
In general, patients who had chosen CC were satisfied with their decision, most likely reflecting a well-informed and deliberate decision. Although decisional regret has not been compared head to head between dialysis and CC, patients more often switch their choice of dialysis to CC than vice versa [46]. In dialysis patients, higher decisional regret is associated with less involvement in decision making, insufficient information provision at the time of decision making and choosing dialysis over CC to please family members or healthcare professionals [47, 48].
The participants of the reviewed studies brought forward different views on CC. These differences must be seen in their respective time and cultural backgrounds. CC is an increasingly recognised treatment for advanced CKD kidney failure and implemented in nephrology care. This is also reflected by the fact that we did not find relevant articles published before 2005. Large disparities in access to KRT and perceptions on CC may be present across countries and over time [8, 49]. For example, patients in Singapore had additional cost motivations for choosing CC compared with patients in countries in which reimbursement of KRT is organised differently [24]. The extent to which CC is implemented in healthcare institutions also influences healthcare professionals’ views on CC [21]. Large differences are present within Europe in the establishment of CC, with the estimated proportion of patients receiving CC ranging from 0% in Slovenia to 15% in Hungary [49]. As the included studies were conducted in only six countries, the generalisability of our results to other countries is uncertain. The same applies for the implementation of SDM. Transferability of the results is highly dependent on the degree of SDM implementation.
Twenty studies met our inclusion criteria, with the majority of patients yet to make a decision. There has been limited evaluation of patients’ perspectives on the decision-making process between CC and dialysis, especially from patients who already had chosen CC. More knowledge should be gained about the impact of CC on patients’ lives, health-related quality of life and how patients evaluate their choice. Further studies should focus on improving awareness and education about CC. Future research may also focus on which patients benefit most from CC and the survival of patients receiving CC. This information is often lacking in the decision-making process and patients consider this information important [14, 15, 34].
Our scoping review has several strengths. By focusing on the input provided by patients, we were able to provide reliable and valuable insights regarding the preferences of patients themselves. Our elaborate search strategy and the inclusion of both qualitative and quantitative studies allowed us to create a comprehensive overview. The themes we identified are largely overlapping with core aspects of SDM in general [39], specific for treatment modality choice in advanced CKD [32] and the commonly used Three Talk Model [50].
The differences in designs of the included articles are a limitation of this review, as it was hard to compare results. We dealt with this issue by providing an overview of the methods used in the respective articles (Table 1). Comparison of results is further hampered by the heterogeneity of the study populations, with geographical and cultural differences. When applying the results of our study, healthcare professionals should always keep local issues or preferences in mind. By focussing our search on CC, we might have missed patients’ considerations about CC as part of studies primarily focussing on other treatment modalities.
CONCLUSIONS
We identified a wide range of experiences reflecting what patients consider important during treatment decision making in advanced CKD. Limited awareness and knowledge about CKD and CC, as well as a perceived lack of choice, were the main barriers for optimal decision making. Patients appreciated a timely start of counselling about treatment options, with comprehensive and clear communication and involvement of family members during the decision-making process. This scoping review resulted in a list of recommendations to help healthcare professionals support their patients to choose a treatment option that fits their lives best.
Supplementary Material
Contributor Information
Micha Jongejan, Department of Internal Medicine, Leiden University Medical Center, Leiden, The Netherlands.
Sanne de Lange, Department of Nephrology and Hypertension, University Medical Center Utrecht, Utrecht, The Netherlands.
Willem Jan W Bos, Department of Internal Medicine, Leiden University Medical Center, Leiden, The Netherlands; Department of Internal Medicine, St. Antonius Hospital, Nieuwegein, The Netherlands.
Arwen H Pieterse, Department of Biomedical Data Sciences, Leiden University Medical Center, Leiden, The Netherlands.
Wanda S Konijn, Dutch Kidney Patient Association (NVN), Bussum, The Netherlands.
Marjolijn van Buren, Department of Internal Medicine, Leiden University Medical Center, Leiden, The Netherlands; Department of Nephrology, Haga Hospital, The Hague, The Netherlands.
Alferso C Abrahams, Department of Nephrology and Hypertension, University Medical Center Utrecht, Utrecht, The Netherlands.
Mathijs van Oevelen, Department of Internal Medicine, Leiden University Medical Center, Leiden, The Netherlands.
FUNDING
None declared.
AUTHORS’ CONTRIBUTIONS
S.d.L., M.v.O., M.v.B. and A.A. designed the study. M.J., S.d.L. and M.v.O. performed the search, article selection, data extraction, coding of selected articles and the thematic synthesis and drafted the manuscript. M.v.O. provided guidance. W.K. provided input from the patients’ perspective. W.J.B., M.v.B., A.A., A.P. and W.K. critically reviewed the manuscript. All authors read and approved the final manuscript.
DATA AVAILABILITY STATEMENT
No new data were generated or analysed in support of this research.
CONFLICT OF INTEREST STATEMENT
The authors declare that they have no relevant financial interests. The results presented in this article have not been published previously in whole or part. M.v.B., A.A., W.J.B. and M.v.O. are conducting a prospective study to compare outcomes between CC and dialysis in older patients.
REFERENCES
- 1. Davison SN, Levin A, Moss AH et al. Executive summary of the KDIGO Controversies Conference on Supportive Care in Chronic Kidney Disease: developing a roadmap to improving quality care. Kidney Int 2015;88:447–59. 10.1038/ki.2015.110 [DOI] [PubMed] [Google Scholar]
- 2. Al-Mansouri A, Al-Ali FS, Hamad AI et al. Assessment of treatment burden and its impact on quality of life in dialysis-dependent and pre-dialysis chronic kidney disease patients. Res Soc Admin Pharm 2021;17:1937–44. 10.1016/j.sapharm.2021.02.010 [DOI] [PubMed] [Google Scholar]
- 3. Schoot TS, Goto NA, van Marum RJ et al. Dialysis or kidney transplantation in older adults? A systematic review summarizing functional, psychological, and quality of life-related outcomes after start of kidney replacement therapy. Int Urol Nephrol 2022;54:2891–900. 10.1007/s11255-022-03208-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Voorend CGN, van Oevelen M, Verberne WR et al. Survival of patients who opt for dialysis versus conservative care: a systematic review and meta-analysis. Nephrol Dial Transplant 2022;37:1529–44. 10.1093/ndt/gfac010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Robinski M, Mau W, Wienke A et al. The Choice of Renal Replacement Therapy (CORETH) project: dialysis patients’ psychosocial characteristics and treatment satisfaction. Nephrol Dial Transplant 2017;32:315–24. [DOI] [PubMed] [Google Scholar]
- 6. Van Biesen W, van der Veer SN, Murphey M et al. Patients’ perceptions of information and education for renal replacement therapy: an independent survey by the European Kidney Patients’ Federation on information and support on renal replacement therapy. PLoS One 2014;9:e103914. 10.1371/journal.pone.0103914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Galla JH. Clinical practice guideline on shared decision-making in the appropriate initiation of and withdrawal from dialysis. J Am Soc Nephrol 2000;11:1340–2. [DOI] [PubMed] [Google Scholar]
- 8. de Jong RW, Stel VS, Rahmel A et al. Patient-reported factors influencing the choice of their kidney replacement treatment modality. Nephrol Dial Transplant 2022;37:477–88. 10.1093/ndt/gfab059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Russell JSC, Oliverio A, Paulus A. Barriers to conservative management conversations: perceptions of nephrologists and fellows-in-training. J Palliat Med 2021;24:1497–504. 10.1089/jpm.2020.0690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ladin K, Pandya R, Kannam A et al. Discussing conservative management with older patients with CKD: an interview study of nephrologists. Am J Kidney Dis 2018;71:627–35. 10.1053/j.ajkd.2017.11.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Page MJ, McKenzie JE, Bossuyt PM et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Eneanya ND, Labbe AK, Stallings TL et al. Caring for older patients with advanced chronic kidney disease and considering their needs: a qualitative study. BMC Nephrol 2020;21:213. 10.1186/s12882-020-01870-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Oestreich T, Sayre G, O'Hare AM et al. Perspectives on conservative care in advanced kidney disease: a qualitative study of US patients and family members. Am J Kidney Dis 2021;77:355–64.e1. 10.1053/j.ajkd.2020.07.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Selman LE, Bristowe K, Higginson IJ et al. The views and experiences of older people with conservatively managed renal failure: a qualitative study of communication, information and decision-making. BMC Nephrol 2019;20:38. 10.1186/s12882-019-1230-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Finkelstein EA, Ozdemir S, Malhotra C et al. Understanding factors that influence the demand for dialysis among elderly in a multi-ethnic Asian society. Health Policy 2018;122:915–21. 10.1016/j.healthpol.2018.06.008 [DOI] [PubMed] [Google Scholar]
- 16. Zimmermann CJ, Jhagroo RA, Wakeen M et al. Opportunities to improve shared decision making in dialysis decisions for older adults with life-limiting kidney disease: a pilot study. J Palliat Med 2020;23:627–34. 10.1089/jpm.2019.0340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. House TR, Wightman A, Rosenberg AR et al. Challenges to shared decision making about treatment of advanced CKD: a qualitative study of patients and clinicians. Am J Kidney Dis 2022;79:657–66.e1. 10.1053/j.ajkd.2021.08.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hamroun A, Speyer E, Ayav C et al. Barriers to conservative care from patients’ and nephrologists’ perspectives: the CKD-REIN Study. Nephrol Dial Transplant 2022;37:2438–48. 10.1093/ndt/gfac009 [DOI] [PubMed] [Google Scholar]
- 19. Eneanya ND, Percy SG, Stallings TL et al. Use of a supportive kidney care video decision aid in older patients: a randomized controlled trial. Am J Nephrol 2020;51:736–44. 10.1159/000509711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Karlin J, Chesla CA, Grubbs V. Dialysis or death: a qualitative study of older patients’ and their families’ understanding of kidney failure treatment options in a US public hospital setting. Kidney Med 2019;1:124–30. 10.1016/j.xkme.2019.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Tonkin-Crine S, Okamoto I, Leydon GM et al. Understanding by older patients of dialysis and conservative management for chronic kidney failure. Am J Kidney Dis 2015;65:443–50. 10.1053/j.ajkd.2014.08.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Frazier R, Levine S, Porteny T et al. Shared decision making among older adults with advanced CKD. Am J Kidney Dis 2022;80:599–609. 10.1053/j.ajkd.2022.02.017 [DOI] [PubMed] [Google Scholar]
- 23. Verberne WR, Konijn WS, Prantl K et al. Older patients’ experiences with a shared decision-making process on choosing dialysis or conservative care for advanced chronic kidney disease: a survey study. BMC Nephrol 2019;20:264. 10.1186/s12882-019-1423-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Seah AS, Tan F, Srinivas S et al. Opting out of dialysis – exploring patients’ decisions to forego dialysis in favour of conservative non-dialytic management for end-stage renal disease. Health Expect 2015;18:1018–29. 10.1111/hex.12075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Han E, Haldane V, Koh JJK et al. Perspectives on decision making amongst older people with end-stage renal disease and caregivers in Singapore: a qualitative study. Health Expect 2019;22:1100–10. 10.1111/hex.12943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Wong SPY, Oestreich T, Prince DK et al. A patient decision aid about conservative kidney management in advanced kidney disease: a randomized pilot trial. Am J Kidney Dis 2023;82:179–88. 10.1053/j.ajkd.2022.12.007 [DOI] [PubMed] [Google Scholar]
- 27. Visser A, Dijkstra GJ, Kuiper D et al. Accepting or declining dialysis: considerations taken into account by elderly patients with end-stage renal disease. J Nephrol 2009;22:794–9. [PubMed] [Google Scholar]
- 28. Ashby M, op't Hoog C, Kellehear A et al. Renal dialysis abatement: lessons from a social study. Palliat Med 2005;19:389–96. 10.1191/0269216305pm1043oa [DOI] [PubMed] [Google Scholar]
- 29. Johnston S, Noble H. Factors influencing patients with stage 5 chronic kidney disease to opt for conservative management: a practitioner research study. J Clin Nurs 2012;21:1215–22. 10.1111/j.1365-2702.2011.04001.x [DOI] [PubMed] [Google Scholar]
- 30. Noble H. Reasons renal patients give for deciding not to dialyze: a prospective qualitative interview study. Dial Transplant 2009;38:82–9. [Google Scholar]
- 31. Morton RL, Snelling P, Webster AC et al. Dialysis modality preference of patients with CKD and family caregivers: a discrete-choice study. Am J Kidney Dis 2012;60:102–11. 10.1053/j.ajkd.2011.12.030 [DOI] [PubMed] [Google Scholar]
- 32. Saeed F, Shah AY, Allen RJ et al. Communication principles and practices for making shared decisions about renal replacement therapy: a review of the literature. Curr Opin Nephrol Hypertens 2021;30:507–15. 10.1097/MNH.0000000000000731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Schell JO, Patel UD, Steinhauser KE et al. Discussions of the kidney disease trajectory by elderly patients and nephrologists: a qualitative study. Am J Kidney Dis 2012;59:495–503. 10.1053/j.ajkd.2011.11.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Parvez S, Abdel-Kader K, Pankratz VS et al. Provider knowledge, attitudes, and practices surrounding conservative management for patients with advanced CKD. Clin J Am Soc Nephrol 2016;11:812–20. 10.2215/CJN.07180715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Van den Bosch J, Warren DS, Rutherford PA. Review of predialysis education programs: a need for standardization. Patient Prefer Adherence 2015;9:1279–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Stacey D, Légaré F, Lewis K et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev 2017;4:CD001431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Harwood L, Clark AM. Understanding pre-dialysis modality decision-making: a meta-synthesis of qualitative studies. Int J Nurs Stud 2013;50:109–20. 10.1016/j.ijnurstu.2012.04.003 [DOI] [PubMed] [Google Scholar]
- 38. Morton RL, Tong A, Howard K et al. The views of patients and carers in treatment decision making for chronic kidney disease: systematic review and thematic synthesis of qualitative studies. BMJ 2010;340:c112. 10.1136/bmj.c112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Bomhof-Roordink H, Gärtner FR, Stiggelbout AM et al. Key components of shared decision making models: a systematic review. BMJ Open 2019;9:e031763. 10.1136/bmjopen-2019-031763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Hussain JA, Flemming K, Murtagh FE et al. Patient and health care professional decision-making to commence and withdraw from renal dialysis: a systematic review of qualitative research. Clin J Am Soc Nephrol 2015;10:1201–15. 10.2215/CJN.11091114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Joseph-Williams N, Elwyn G, Edwards A. Knowledge is not power for patients: a systematic review and thematic synthesis of patient-reported barriers and facilitators to shared decision making. Patient Educ Couns 2014;94:291–309. 10.1016/j.pec.2013.10.031 [DOI] [PubMed] [Google Scholar]
- 42. van Dulmen S, Peereboom E, Schulze L et al. The use of implicit persuasion in decision-making about treatment for end-stage kidney disease. Perit Dial Int 2022;42:377–86. 10.1177/08968608211027019 [DOI] [PubMed] [Google Scholar]
- 43. Noble H, Brazil K, Burns A et al. Clinician views of patient decisional conflict when deciding between dialysis and conservative management: qualitative findings from the PAlliative Care in chronic Kidney diSease (PACKS) study. Palliat Med 2017;31:921–31. 10.1177/0269216317704625 [DOI] [PubMed] [Google Scholar]
- 44. Engels N, de Graav GN, van der Nat P et al. Shared decision-making in advanced kidney disease: a scoping review. BMJ Open 2022;12:e055248. 10.1136/bmjopen-2021-055248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Ramer SJ, McCall NN, Robinson-Cohen C et al. Health outcome priorities of older adults with advanced CKD and concordance with their nephrology providers’ perceptions. J Am Soc Nephrol 2018;29:2870–8. 10.1681/ASN.2018060657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Voorend CGN, Verberne WR, van Oevelen M et al. Changing the choice from dialysis to conservative care or vice versa in older patients with advanced chronic kidney disease. Nephrol Dial Transplant 2021;36:1958–61. 10.1093/ndt/gfab162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Tan EGF, Teo I, Finkelstein EA et al. Determinants of regret in elderly dialysis patients. Nephrology 2019;24:622–9. 10.1111/nep.13400 [DOI] [PubMed] [Google Scholar]
- 48. Saeed F, Ladwig SA, Epstein RM et al. Dialysis regret: prevalence and correlates. Clin J Am Soc Nephrol 2020;15:957–63. 10.2215/CJN.13781119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Stel VS, de Jong RW, Kramer A et al. Supplemented ERA-EDTA Registry data evaluated the frequency of dialysis, kidney transplantation, and comprehensive conservative management for patients with kidney failure in Europe. Kidney Int 2021;100:182–95. 10.1016/j.kint.2020.12.010 [DOI] [PubMed] [Google Scholar]
- 50. Elwyn G, Durand MA, Song J et al. A three-talk model for shared decision making: multistage consultation process. BMJ 2017;359:j4891. 10.1136/bmj.j4891 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No new data were generated or analysed in support of this research.