Abstract
In this work, the case of a 70-year-old Caucasian woman affected by cryptogenic stroke is reported. After discarding other sources of embolism, a transesophageal echocardiogram was performed, which revealed the presence of a double interatrial septum associated with a left-sided atrial pouch. The persistent interatrial space was identified as the most probable source of thrombus.
Key Words: atrial septal pouch, cardioembolic ictus, case report, cryptogenic stroke, double interatrial septum
Graphical abstract
History of Presentation
A 70-year-old Caucasian woman fell at work with no loss of consciousness but with progressive blindness in her right eye, difficulty speaking, and strength deficit in her right limbs. On arrival in the emergency department, her symptoms progressed to severe right hemiparesis with aphasia and vomiting.
Learning Objectives
-
•
To understand the role of transesophageal echocardiography in the diagnosis of DIAS.
-
•
To be able to make a differential diagnosis of cryptogenic stroke with transesophageal echocardiography.
-
•
To raise awareness of the potential association of DIAS and atrial septal pouches with stroke.
Past Medical History
The patient never suffered cardiovascular or cerebrovascular events and had well-controlled hypertension on pharmacologic treatment. Her past medical history only included cervical conization 4 years before with a negative follow-up.
Differential Diagnosis
Stroke can be hemorrhagic or ischemic, with the latter involving thrombosis, embolism, and decreased perfusion as potential mechanisms.
Investigations
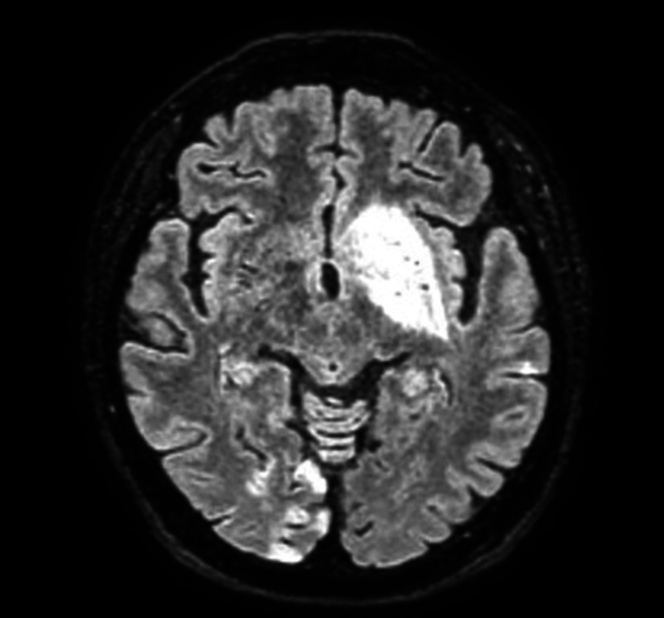
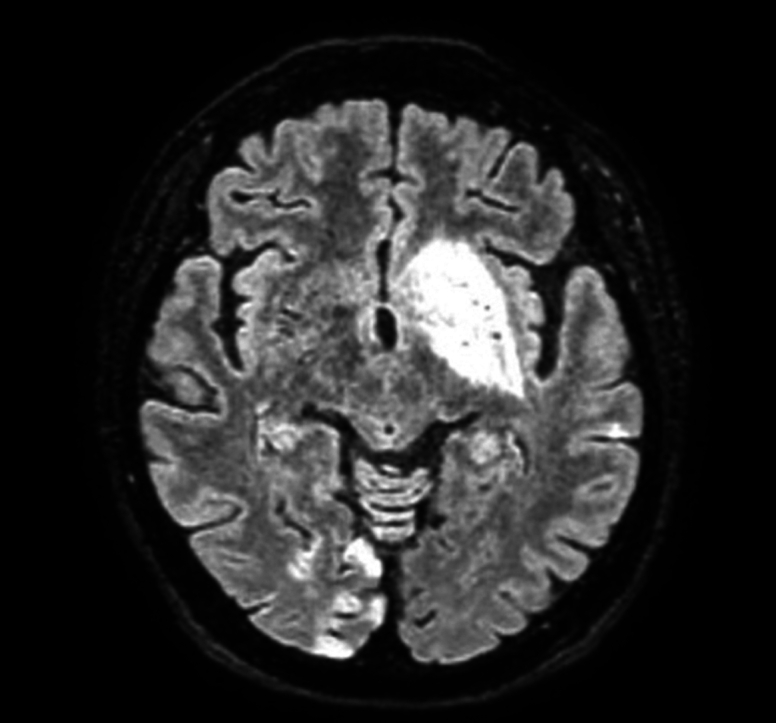
Emergency cranial computed tomography angiography revealed no opacification of the internal carotid artery with occlusion of the left carotid siphon to the M1 tract of the middle cerebral artery. The 24-hour brain computed tomography scan revealed hypodensity of the left anterior capsulolenticular area with no hemorrhagic transformation and hypodense areolae in the right inferior cerebellar hemispheric site, both of subacute ischemic nature. Brain magnetic resonance imaging (Figure 1) showed multiple ischemic lesions at the left lenticulocapsular site, the left hemispheric cortico-subcortical site, the right temporo-occipito-parietal cortico-subcortical site, the right inferior cerebellar hemispheric corticosubcortical site, and to a lesser extent at the left inferior cerebellar hemispheric site. Computed tomography angiography of supra-aortic trunks and intracranial vessels showed no hemodynamically significant stenosis.
Figure 1.
Brain Magnetic Resonance Imaging
The presence of multiple ischemic lesions at the left lenticulocapsular site, the left hemispheric cortico-subcortical site, the right temporo-occipito-parietal cortico-subcortical site, the right inferior cerebellar hemispheric cortico-subcortical site, and to a lesser extent the left inferior cerebellar hemispheric site.
Continuous electrocardiography monitoring was performed during the whole hospitalization to exclude a cardioembolic genesis. In addition, dynamic Holter electrocardiography was performed showing no atrial fibrillation or other emboligenic arrhythmias. A loop recorder was implanted and was negative after 3 months.
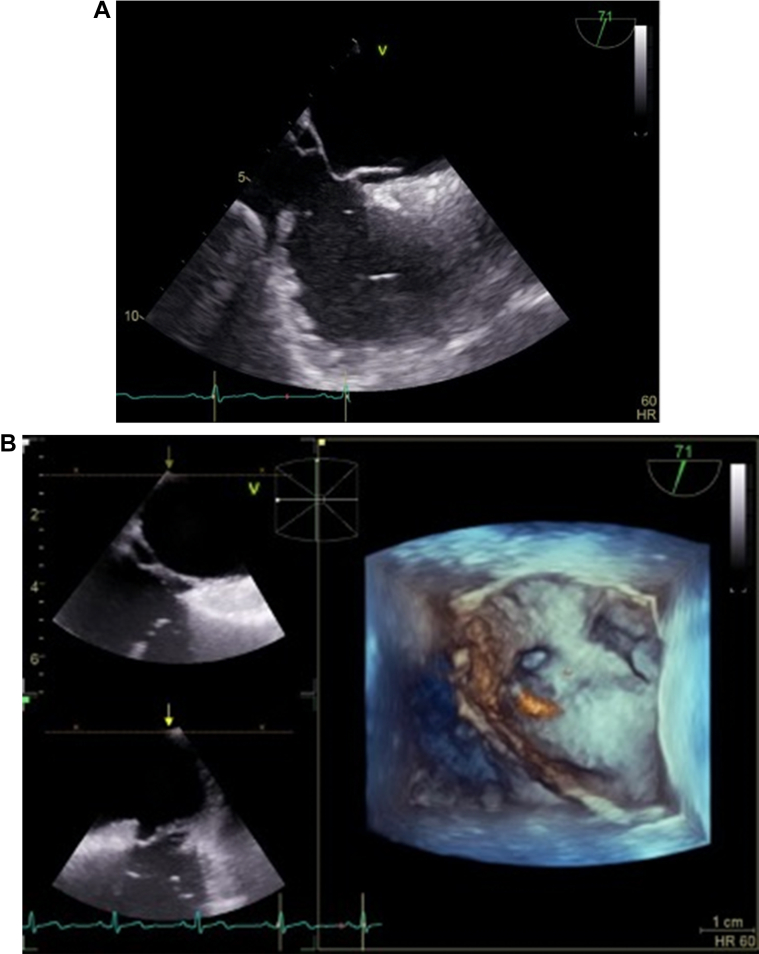
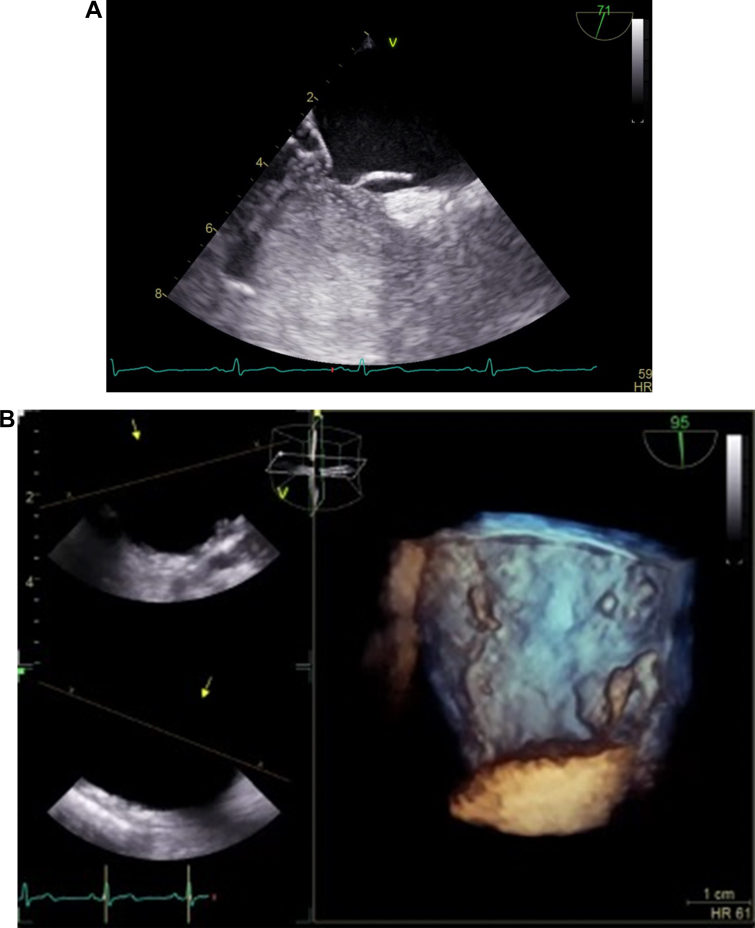
A transesophageal echocardiogram and transthoracic echocardiogram were performed with 2-dimensional and 3-dimensional methods, and the following findings were documented. The atrial septum showed a double contour morphology in its posterior cranial portion (Video 1). The presence of 2 parallel interatrial septa, between which a clear echocardiographic lucent chamber was present, was clearly referable to a double interatrial septum (DIAS). On the left side of the atrial septum, a left-side atrial pouch (length = 13 mm, width = 16 mm, and orifice separation = 2 mm) was well visualized (Figures 2A and 2B). The fossa ovalis, which was spared, appeared mobile but without spontaneous separations; in basal conditions and after the Valsalva maneuver, there were no interatrial shunt signs (Figure 3).
Figure 2.
Transesophageal Echocardiogram
(A and B) The atrial septum showed a double contour morphology in its posterior cranial portion. On the left side of the atrial septum, there were images compatible with a left-sided atrial pouch (length = 13 mm, width = 16 mm, and orifice separation = 2 mm).
Figure 3.
Transesophageal Echocardiogram After Valsalva Maneuver
(A and B) There were no signs of shunt at the level of the interatrial septum.
Furthermore, other embolism sources were ruled out because the left ventricle global systolic function was normal with no segmental asynergies detectable, the left atrium was nondilated (33 mL/m2) and no thrombosis inside was detected, no thrombosis was found in “chicken-wing” morphology in the left auricula (its emptying maximum velocity was around 0.4 m/s), and the valvular structures seemed to be regular for morphology and dynamics with no plus images.
Management
On arrival in the emergency department, the patient underwent systemic thrombolysis and subsequent endovascular treatment of mechanical thrombectomy, resulting in recanalization of the carotid siphon and recanalization of both the M1 tract of the left middle cerebral artery and the A2 tract of the left anterior cerebral artery. After discarding other sources of embolism, the persistent interatrial space was identified as the most probable source of thrombus in this specific case. Anticoagulation (enoxaparin sodium) was the preferred therapy after a collective discussion.
Discussion
DIAS is a very rare condition, with only 8 cases reported in the literature so far.1 It is characterized by a double-layered atrial septum with a persistent interatrial space between the 2 atria. There are 2 theories that can explain the presence of 2 interatrial septa: the first is related to the abnormal development of the septum secundum, with failure of resorption of the superior portion of the septum primum in utero; according to the other theory, the additional septum is most likely to be a persistent left venous valve of the sinus venosus.2 This anomaly is of unknown significance. Thrombus formation between the septa with systemic embolization and in a case coronary embolization has already been reported.3
DIAS can be associated with other congenital heart defects (eg, ventricular septal defect, coarctation, and hypoplastic left heart).2 Differential diagnoses include aneurysm of the atrioventricular membranous septum, the atrial septal pouch, and the cor triatriatum, although Faletra et al4 assumed that features of DIAS are consistent with a large atrial septal pouch and both Thilenius et al5 and Bharati and Lev6 described this atrial septal anomaly as type C cor triatriatum. Certainly, DIAS presents a technical challenge in procedures requiring transseptal puncture. After discarding a persistent foramen ovale and other sources of embolism, anticoagulation is the preferred therapy.7
Follow-Up
At a subsequent follow-up at 6 months, the patient did not experience any new episodes of stroke or hemorrhagic events.
Conclusions
There is an important knowledge gap for stroke patients without an identifiable cause, so-called cryptogenic stroke, which is roughly one-quarter of all ischemic strokes. A left-sided atrial pouch is a new concept,8 whereas DIAS is still anecdotal. Both conditions may presumably promote blood stasis and thrombus formation, but still there are few certainties.9 In the present case, the 2 conditions coexisted. In the future, a systematic study of the atrial septum to identify atrial pouches and DIAS will clarify how often these anatomic abnormalities are associated with thromboembolic events.
Funding Support and Author Disclosures
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Appendix
For supplemental videos, please see the online version of this paper.
Appendix
The Atrial Septum Showed a Double Contour Morphology in Its Posterior Cranial Portion
References
- 1.Arunthamakun J., Wang H., Singh S. An atrial anomaly- a case of double interatrial septum. J Am Coll Cardiol. 2021;77(suppl 1):2626. [Google Scholar]
- 2.Roberson D.A., Javois A.J., Cui W., Madronero L.F., Cuneo B.F., Muangmingsuk S. Double atrial septum with persistent interatrial space: echocardiographic features of a rare atrial septal malformation. J Am Soc Echocardiogr. 2006;19:1175. doi: 10.1016/j.echo.2006.04.001. [DOI] [PubMed] [Google Scholar]
- 3.Breithardt O.A., Papavassiliu T., Borggrefe M. A coronary embolus originating from the interatrial septum. Eur Heart J. 2006;27(23):2745. doi: 10.1093/eurheartj/ehl051. [DOI] [PubMed] [Google Scholar]
- 4.Faletra F.F., Leo L.A., Paiocchi V.L., et al. Revisiting anatomy of the inter- atrial septum and its adjoining atrioventricular junction using noninvasive imaging techniques. J Am Soc Echocardiogr. 2019;32:580–592. doi: 10.1016/j.echo.2019.01.009. [DOI] [PubMed] [Google Scholar]
- 5.Thilenius O.G., Bharati S., Lev M. Subdivided left atrium: an expanded concept of cor triatriatum sinistrum. Am J Cardiol. 1976;37:743–752. doi: 10.1016/0002-9149(76)90369-6. [DOI] [PubMed] [Google Scholar]
- 6.Bharati S., Lev M. In: The Pathology of Congenital Heart Disease. Bharati S., editor. Futura; 1996. Cor triatriatum sinistrum (double left atrium) pp. 1285–1299. [Google Scholar]
- 7.Seyfert H., Bohlscheid V., Bauer B. Double atrial septum with persistent interatrial space and transient ischaemic attack. Eur J Echocardiogr. 2008;9(5):707–708. doi: 10.1093/ejechocard/jen161. [DOI] [PubMed] [Google Scholar]
- 8.Hołda M.K., Koziej M., Holda J., et al. Atrial septal pouch — morphological features and clinical considerations. Int J Cardiol. 2016;220:337–342. doi: 10.1016/j.ijcard.2016.06.141. [DOI] [PubMed] [Google Scholar]
- 9.Chandrashekhar Y., Narula J. LA septal pouch as a source of thromboembolism: innocent until proven guilty? J Am Coll Cardiol Img. 2010;3(12):1296–1298. doi: 10.1016/j.jcmg.2010.11.003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The Atrial Septum Showed a Double Contour Morphology in Its Posterior Cranial Portion