Abstract
Background:
Increased posterior tibial slope (PTS) leads to a relative anterior translation of the tibia on the femur. This is thought to decrease the stress on posterior cruciate ligament (PCL) reconstruction (PCLR) grafts.
Purpose/Hypothesis:
The purpose of this study was to analyze the effect of PTS on knee laxity, graft failure, and patient-reported outcome (PRO) scores after PCLR without concomitant anterior cruciate ligament reconstruction (ACLR). It was hypothesized that patients with higher PTS would have less knee laxity, fewer graft failures, and better PROs compared with patients with lower PTS.
Study Design:
Case-control study; Level of evidence, 3.
Methods:
All patients who underwent PCLR between 2001 and 2020 at a single institution were identified. Patients were excluded if they underwent concomitant or prior ACLR or proximal tibial osteotomy, were younger than 18 years, had <2 years of in-person clinical follow-up, and did not have documented PRO scores (Lysholm score and International Knee Documentation Committee [IKDC] score). Data were collected retrospectively from a prospectively gathered database. PTS measurements were recorded from perioperative lateral knee radiographs. A linear regression model was created to analyze PTS in relation to PRO scores. Patients with a grade 1 (1-5 mm) or higher posterior drawer were compared with those who had a negative posterior drawer.
Results:
A total of 37 knees met inclusion criterion; the mean age was 30.7 years at the time of surgery. The mean clinical follow-up was 5.8 years. No significant correlation was found between either the Lysholm score or the IKDC score and the PTS. Twelve knees (32.4%) had a positive posterior drawer at final follow-up. The mean PTS in knees with a positive posterior drawer was 6.2°, whereas that for knees with a negative posterior drawer was 8.3° (P = .08). No significant differences in PRO scores were identified for knees with versus knees without a positive posterior drawer. No documented graft failures or revisions were found.
Conclusion:
No significant differences were found in PROs or graft failure rates based on PTS at a mean of 5.8 years after PCLR. Increased tibial slope trended toward being protective against a positive posterior drawer, although this did not reach statistical significance.
Keywords: posterior cruciate ligament, posterior tibial slope, patient-reported outcomes
Posterior cruciate ligament (PCL) injuries are relatively uncommon and are usually associated with high-energy collisions involving a posterior-directed force to the proximal tibia.32,35 More than half of PCL injuries are combined with other ligamentous knee injuries, most commonly involving the anterior cruciate ligament (ACL) or posterolateral corner (PLC). 32 PCL injuries can additionally occur at the time of knee dislocation and may be associated with neurovascular injury. 21 Cadaveric studies have shown that an increased posterior tibial slope (PTS) leads to a relative anterior translation of the tibia on the femur.12,13 This anterior shift of the tibia brings the PCL insertion on the tibia closer to its origin on the femur and decreases graft forces after PCL reconstruction (PCLR).2,4 Associated ligamentous injuries and bony anatomic features such as the PTS may play a role in determining outcomes after PCLR. 31
In the ACL literature, several studies have demonstrated increased stress on the ACL in patients with an increased PTS, predisposing patients to ACL rupture and graft failure.5,8,9,24,25,29,38 Therefore, altering the PTS via osteotomy may reduce the risk of graft failure after ligament reconstruction.3,15,31,33 The outcomes of slope-altering osteotomy combined with PCLR remain unclear. A recent study evaluated concomitant high tibial osteotomy and ACL reconstruction (ACLR) or PCLR, but the study group included patients with primarily varus malalignment, predominantly medial compartment osteoarthritis symptoms, and no definitive history of a cruciate ligament injury. 15 A paucity of data are available analyzing patient-reported outcomes (PROs) and knee laxity after PCLR in relation to PTS. A recent study failed to demonstrate a statistically significant relationship between PTS and PROs after PCLR, although 48% of the patients in the cohort underwent concomitant ACLR. 36 Outcomes were not reported in relation to PTS for patients without concomitant ACLR. Concomitant ACLR may affect PRO scores, because less tension can be applied to the PCL graft during ACLR and PCLR procedures in order to avoid anterior overreduction of the tibiofemoral joint.
The purpose of our study was to analyze the effect of PTS on knee laxity, graft failure, and PRO scores after PCLR without concomitant ACLR. We hypothesized that patients with higher PTS would have less knee laxity, fewer graft failures, and better PROs after PCLR compared with patients who had lower PTS.
Methods
After receiving institutional review board approval for the study protocol, we identified all patients who underwent PCLR at our institution between 2001 and 2020. Patients who underwent concomitant reconstruction of the lateral collateral ligament (LCL) and posterolateral corner (PLC) or the medial collateral ligament (MCL) and posteromedial corner (PMC) were included. Patients were excluded if they underwent concomitant or prior ACLR, underwent a proximal tibial osteotomy before or after their PCL injury, were younger than 18 years, had <2 years of in-person clinical follow-up, did not have documented PRO scores including Lysholm and International Knee Documentation Committee (IKDC) scores, or did not provide preoperative research consent.
An all-inside PCLR technique using a quadrupled peroneus longus, Achilles, or tibialis anterior allograft with both tibial and femoral suspensory fixation was performed. This technique was developed by the senior authors (B.A.L. and M.J.S.) and was initially described in 2015.1,11,22,23,28,34 In patients with combined injuries, reconstruction rather than repair was performed for the LCL/PLC and MCL/PMC.17,19,20 Postoperatively, patients were allowed to be toe-touch weightbearing in extension for 3 weeks, followed by 25% weightbearing with the brace unlocked after 3 weeks. Range of motion (ROM) was limited to 0° to 90° of passive motion in the prone position for the first 2 weeks. After 2 weeks, passive ROM was permitted as tolerated in the supine or prone position. Weightbearing as tolerated began at 6 weeks, and the brace was weaned beginning at 12 weeks. Return to running was permitted at 16 weeks if quadriceps strength was >80% symmetric and the ratio of hamstring to quadriceps strength was 50%. Full activity was permitted at 20 weeks if quadriceps strength was >85% symmetric and the ratio of hamstring to quadriceps strength was >60%.
Demographic, surgical, and outcomes data were collected retrospectively from our prospectively gathered multiligament knee injury database. Patient demographic data documented in the registry at the time of care included sex, age at the time of PCLR, laterality, body mass index (BMI), tobacco use, and diabetes. Time from injury to surgery was recorded as well as the presence or absence of a knee dislocation at the time of injury. Because we excluded patients with ACL injuries, all knee dislocations were, by definition, Schenck knee dislocation (KD) grade 1 (single cruciate). Surgical data documented in the registry at the time of care included primary or revision PCLR, concomitant procedures on the menisci or cartilage, concomitant LCL/PLC or MCL/PMC reconstruction, and PCL graft type. PRO data included Lysholm and IKDC scores, which were filled out by patients at regular intervals (ie, 1, 2, 5, and 10 years after surgery).
Additional details not otherwise contained within the registry were obtained via individual review of the electronic medical record. At the time of data review, PTS measurements were recorded from perioperative lateral knee radiographs using a previously described method. 10
Routine postoperative follow-up included in-person visits at a minimum of 2 weeks, 3 months, 6 months, 1 year, and 2 years. Many patients were seen in clinic further out than 2 years. Physical examination data for this study were obtained from the most recent in-person follow-up visit and were documented by the surgeon. All patients received PRO questionnaires either at their in-person follow-up visits or via USPS mail at regular intervals as described above. These scores were recorded in the registry prospectively.
Primary outcome measures were tibial slope in relation to Lysholm and IKDC scores and the presence or absence of a positive posterior drawer. For posterior drawer testing, grade 0 was defined as no posterior translation, grade 1 as 1 to 5 mm, grade 2 as 6 to 10 mm, and grade 3 as >10 mm. A positive posterior drawer was defined as grade ≥1. PCLR failure was defined as a grade 2 or 3 posterior drawer in the presence of symptomatic instability or complete graft disruption requiring revision PCLR. Secondary outcomes included complications and reoperations.
A linear regression model was created to analyze PTS in relation to PRO scores. Additionally, patients who were found to have a positive posterior drawer (grade ≥1) were compared with those who had a negative posterior drawer. Continuous variables were compared using the Student t test, whereas categorical variables were compared using the chi-square test. Statistical significance was set as P < .05. All analysis was conducted using SAS Version 9.4M6 (SAS Institute Inc).
Results
Of the 216 knees initially identified from the institutional database, 156 knees were excluded because they had concomitant ACLR, 1 knee had a prior ACLR, 4 knees had proximal tibial osteotomies as part of their surgical management, 4 knees were from patients younger than 18 years, 13 knees did not have PRO scores available, and 1 knee was from a patient who declined to participate in research studies. Therefore, 37 knees in 37 patients were included in the study.
Demographic and surgical data are shown in Table 1. The sample included 29 men (78%), and the mean age at the time of surgery was 30.7 years. The mean time from initial injury to PCLR was 16 months (range, 0-96 months). The mean clinical follow-up was 5.8 years. The mean PTS for the total cohort was 7.7°.
Table 1.
Patient Demographic and Surgical Characteristics (N = 37) a
| Variable | Value |
|---|---|
| Follow-up, y | 5.8 ± 3.5 |
| Posterior tibial slope, deg | 7.7 ± 3.2 |
| Age, y | 30.7 ± 10.5 |
| Male sex | 29 (78.3) |
| Right knee affected | 17 (45.9) |
| Body mass index, kg/m2 | 29.8 ± 5.4 |
| Tobacco use | 12 (32.4) |
| Diabetes | 1 (2.7) |
| Knee dislocation | 12 (32.4) |
| Vascular injury | 1 (2.7) |
| Neurologic injury | 3 (8.1) |
| Revision PCLR | 3 (8.1) |
| PCL graft type | |
| Achilles allograft | 16 (43.2) |
| Tibialis anterior allograft | 15 (40.5) |
| Peroneus longus allograft | 6 (16.2) |
| Isolated PCLR | 12 (32.4) |
| Combined PCLR | 25 (67.5) |
| PCL + MCL/PMC | 3 (8.1) |
| PCL + LCL/PLC | 19 (51.3) |
| PCL + MCL/PMC + LCL/PLC | 3 (8.1) |
| Concomitant meniscal procedures | 8 (21.6) |
| Medial only | 4 (10.8) |
| Lateral only | 2 (5.4) |
| Medial and lateral | 2 (5.4) |
| Concomitant cartilage procedures | 11 (29.7) |
| MFC chondroplasty | 6 (16.2) |
| Patellar chondroplasty | 5 (13.5) |
| Lateral tibial plateau chondroplasty | 2 (5.4) |
| MFC osteochondral autograft transfer | 1 (2.7) |
Data are reported as mean ± SD or n (% of the total). LCL, lateral collateral ligament; MCL, medial collateral ligament; MFC, medial femoral condyle; PCL, posterior cruciate ligament; PCLR, posterior cruciate ligament reconstruction; PLC, posterolateral corner; PMC, posteromedial corner.
All of the PCL grafts used were allografts, including 16 (43.2%) Achilles, 15 (40.5%) tibialis anterior, and 6 (16.2%) peroneus longus. Isolated PCLR was performed in 12 knees, with additional ligaments reconstructed in 25 knees. Of the 25 multiligament knee reconstruction procedures, 19 of 25 (76%) were PCL + LCL/PLC, 3 of 25 (12%) were PCL + MCL/PMC, and 3 of 25 (12%) were PCL + MCL/PMC + LCL/PLC. Concomitant meniscectomy or meniscal repair was performed in 21.6% of patients, and cartilage procedures were performed in 29.7%. None of these variables met statistical significance for PROs or graft failure rate.
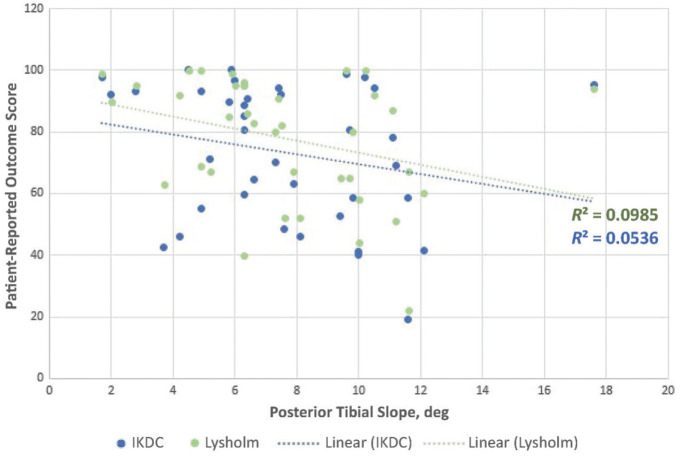
No statistically significant correlation was found for Lysholm or IKDC scores in relation to the PTS (Figure 1). Twelve patients (32.4%) had a positive posterior drawer at final follow-up, with 11 patients having grade 1 laxity and 1 patient having grade 2 laxity (Table 2). The mean PTS in patients with a positive posterior drawer was 6.4°, whereas that for patients with a negative posterior drawer was 8.3° (P = .08). No differences were found in age, sex, BMI, graft type, or isolated/combined PCLR for patients with a positive or negative posterior drawer. However, all 3 patients undergoing revision of a prior PCLR had a positive posterior drawer at the most recent follow-up. These 3 patients had a mean PTS of 6.6°. One patient had 2 prior revision PCLRs for persistent instability prior to presentation to our center. The second patient had a prior PCLR and subsequent PCL tunnel bone grafting performed at an outside institution. The third patient had a complete graft disruption after a prior PCLR at an outside institution. The reasons for graft failure in these 3 patients were not completely clear at the time of revision.
Figure 1.
Results of linear regression analysis of International Knee Documentation Committee (IKDC) and Lysholm scores based on posterior tibial slope.
Table 2.
Comparison of Patient Demographic and Surgical Data Based on Presence or Absence of a Posterior Drawer a
| Variable | Positive Posterior Drawer
b
(n = 12) |
Negative Posterior Drawer (n = 25) |
P |
|---|---|---|---|
| Posterior tibial slope, deg | 6.4 ± 2.2 | 8.3 ± 3.4 | .08 |
| Age, y | 30.0 ± 8.6 | 31.1 ± 11.4 | .77 |
| Male sex | 9 (75.0) | 20 (80.0) | .73 |
| Body mass index, kg/m2 | 29.7 ± 6.2 | 29.8 ± 5.1 | .97 |
| Tobacco use | 4 (33.3) | 7 (28.0) | .74 |
| Diabetes | 1 (8.3) | 0 (0.0) | NA |
| Revision PCLR | 3 (25.0) | 0 (0.0) | NA |
| PCL graft type | |||
| Achilles allograft | 5 (41.6) | 11 (44.0) | .89 |
| Tibialis anterior allograft | 6 (50.0) | 10 (40.0) | .56 |
| Peroneus longus allograft | 2 (16.7) | 4 (16.0) | .96 |
| Combined PCLR | 8 (66.7) | 17 (68.0) | .93 |
| PCL + MCL/PMC | 0 (0.0) | 3 (12.0) | NA |
| PCL + LCL/PLC | 8 (66.7) | 11 (44.0) | .19 |
| PCL + MCL/PMC + LCL/PLC | 0 (0.0) | 3 (12.0) | NA |
Data are reported as mean ± SD or n (%). LCL, lateral collateral ligament; MCL, medial collateral ligament; NA, not applicable; PLC, posterolateral corner; PMC, posteromedial corner.
A positive posterior drawer was defined as grade 1 or higher.
No statistically significant differences in PRO scores were identified for patients with versus without a positive posterior drawer (Table 3). No documented graft failures or revisions occurred in our cohort. Other complications included patellar clunk (n = 1), arthrofibrosis (n = 2), painful hardware (n = 1), and a superficial wound dehiscence (n = 1). The single patient with a grade 2 posterior drawer did not have symptomatic instability and therefore did not meet our criteria for PCL graft failure. His tibial slope measurement was 4.9°. This patient was last seen in follow-up at 84.9 months postoperatively, at which time he was able to run without difficulty and did not have giving-way symptoms. He had a grade 2 posterior sag and drawer with a firm endpoint. Monitoring was recommended, and he did not go on to develop symptomatic instability. IKDC and Lysholm scores were 93.1 and 100, respectively, 10 years postoperatively. He is now >15 years out from surgery.
Table 3.
Comparison of Outcomes Based on Presence or Absence of a Posterior Drawer a
| Outcome | Positive Posterior Drawer
b
(n = 12) |
Negative Posterior Drawer (n = 25) |
P |
|---|---|---|---|
| Length of PRO follow-up, y | 5.7 ± 3.3 | 5.9 ± 3.7 | .86 |
| IKDC score | 76.4 ± 23.1 | 72.5 ± 22.5 | .63 |
| Lysholm score | 78.7 ± 21.3 | 77.8 ± 20.4 | .89 |
| Complications | 2 (16.7) | 3 (12.0) | .69 |
| Reoperations | 2 (16.7) | 3 (12.0) | .69 |
Data are reported as mean ± SD or n (%). IKDC, International Knee Documentation Committee; PRO, patient-reported outcome.
A positive posterior drawer was defined as grade 1 or higher.
Table 4 demonstrates patient characteristics and outcomes for those undergoing isolated PCLR versus PCLR combined with medial and/or lateral ligament reconstructions. Patients who underwent isolated PCLR had significantly higher PTS compared with those who had combined ligament reconstructions (10.1° vs 6.6°, respectively; P = .001) and were younger (25.7 vs 33.2 years, respectively; P = .04), but no difference was found between groups for PRO scores, the presence or absence of a posterior drawer, complications, or reoperations.
Table 4.
Comparison of Patient Demographic and Outcomes Data Based on Isolated Versus Combined PCLR a
| Variable | Isolated PCLR (n = 12) |
Combined PCLR
b
(n = 25) |
P |
|---|---|---|---|
| Posterior tibial slope, deg | 10.1 ± 2.9 | 6.6 ± 2.8 | .001 |
| Age, y | 25.7 ± 33.2 | 33.2 ± 11.4 | .04 |
| Male sex | 7 (58.3) | 16 (64.0) | .11 |
| Body mass index, kg/m2 | 30.7 ± 7.3 | 29.2 ± 4.3 | .46 |
| Length of PRO follow-up, y | 6.5 ± 5.1 | 5.5 ± 2.6 | .42 |
| IKDC score | 69.9 ± 20.0 | 75.7 ± 23.7 | .47 |
| Lysholm score | 70.4 ± 21.3 | 81.8 ± 19.3 | .11 |
| Complications | 2 (16.7) | 3 (12.0) | .69 |
| Reoperations | 2 (16.7) | 3 (12.0) | .69 |
| Posterior drawer | 4 (33.3) | 6 (24.0) | .55 |
Data are reported as mean ± SD or n (%). Boldface P values indicate statistically significant difference between groups (P < .05). IKDC, International Knee Documentation Committee; PCLR, posterior cruciate ligament reconstruction; PRO, patient-reported outcome.
PCLR combined with medial and/or lateral ligament reconstructions.
Discussion
At mean follow-up of 5.8 years, we failed to demonstrate a statistically significant difference in PROs or graft failure rates based on PTS. A recent study by Winkler et al 36 similarly failed to demonstrate a statistically significant relationship between PTS and PROs after PCLR, although 48% of the patients in their cohort underwent concomitant ACLR. Outcomes were not reported in relation to PTS for patients without concomitant ACLR. The ACL literature has described the deleterious effect of increasing PTS on ACLR grafts and ACLR failure rates.5,8,9,24,25,29,38 Because of the opposite effect of PTS on ACL and PCL graft forces,2,4,12,13 inclusion of patients with concomitant ACLR may confound conclusions specific to outcomes for PCLR based on tibial slope. Therefore, we excluded all patients with concomitant ACLR in the current study. Winkler et al demonstrated a lower PTS in patients with PCL graft failure and additionally reported that each 1° reduction in PTS led to a 1.3-fold increase in the odds of PCL graft failure. Although our study did not demonstrate a difference in graft failure rates based on PTS, we did not have any cases of graft failure for analysis. Future studies including patients with graft failure may further elucidate a potential association between graft failure and PTS.
In our cohort, 1 patient sustained both a peroneal nerve and a popliteal artery injury, whereas 2 patients had peroneal nerve injuries without a vascular injury. Previous studies have reported the effects of peroneal nerve injuries as well as vascular injuries on outcomes after ligament reconstruction.18,30 Patients with peroneal nerve injuries had no difference in Lysholm or IKDC scores compared with patients who did not have such injuries, whereas patients with popliteal artery injuries requiring bypass grafting had significantly lower functional scores. The patient in our cohort with both a nerve injury and a popliteal artery injury requiring reconstruction had an IKDC score of 78 and a Lysholm score of 87 at 5 years postoperatively. Both of these scores were greater than the mean scores of the overall cohort (74 and 78, respectively). The 2 patients with peroneal nerve injuries but no vascular injuries had IKDC scores of 80 and 92 and Lysholm scores of 95 and 82. We found no difference in tibial slope for patients with a vascular or nerve injury compared with patients who did not have such an injury (P = .75). The sample size for this analysis was very small, and the analysis is likely underpowered to determine a significant difference in PRO scores or tibial slope for this cohort of patients.
Prior studies have examined potential risk factors for PCL injury and poor outcomes after PCLR. Bernhardson et al 7 demonstrated a lower PTS in patients with PCL injuries (5.7°) compared with uninjured controls (8.6°). The mean PTS in our cohort with PCL injuries was slightly higher at 7.7°. Another study by Bernhardson et al 4 demonstrated increased PCL graft forces in cadaveric models with lower PTS. Although these 2 studies may point to an increased risk for graft failure in patients with decreased PTS, neither analyzed clinical outcomes after PCLR in living patients. Our clinical study failed to demonstrate any such relationship between PTS and graft failure. Noyes and Barber-Westin 26 reported risk factors for persistent pain and dysfunction after PCLR, including persistent posterolateral rotatory instability, femoral or tibial bone tunnel misplacement, and varus malalignment. The effect of PTS on graft failure and PROs was not analyzed by Noyes and Barber-Westin.
Few studies have reported the outcomes of revision PCLR. Woodmass et al 37 reported the outcomes of 23 patients undergoing revision multiligament knee reconstruction. These patients included many with ACLR. At final follow-up, a positive posterior drawer was found in 5 of the 23 patients: grade 1+ in 4 patients and grade 3+ in 1 patient. The mean IKDC score of the total cohort was 74.5 and Lysholm score was 79.4. A high-energy mechanism of injury and age at the time of revision were associated with worse PRO scores. Noyes and Barber-Westin 26 reported the outcomes of 15 revision PCLRs. The investigators demonstrated significant improvements in pain and function as well as radiographic posterior drawer measurements. Two of the 15 patients experienced failure of revision PCLR. For the 3 cases of revision PCLR included in our study, the mean age at time of revision was 31.6 years. All 3 patients underwent concomitant LCL/PLCR. Mean tibial slope was 6.6°. Mean IKDC score was 79.7 and Lysholm score was 79.0. All 3 patients had a grade 1 posterior drawer. One of the 3 patients had a superficial wound dehiscence requiring irrigation and debridement with revision wound closure, but there were no other complications.
King et al 16 compared the outcomes of multiligament knee reconstruction in patients with Schenck KD grade 3M (ACL/PCL/MCL) and KD grade 3L (ACL/PCL/LCL) knee dislocations. Their data demonstrated inferior Lysholm and IKDC scores in patients undergoing medial repair compared with medial reconstruction or lateral reconstruction or repair. Our study did not show a statistically significant difference in PROs based on combined medial versus lateral reconstructions (P = .94 for IKDC and P = .39 for Lysholm). We excluded patients who underwent ACLR, so it is possible that the difference shown by King et al was related to the ACLR. More data comparing combined PCL/MCL versus PCL/LCL reconstruction could further elucidate a potential difference in PROs between the 2 cohorts.
The present study demonstrated a trend toward a decreased PTS in patients with a persistent positive posterior drawer after PCLR, although this did not reach statistical significance. The current study also demonstrated no difference in outcomes based on isolated versus combined PCLR. Patients undergoing isolated PCLR had a significantly higher PTS compared with those undergoing combined PCLR (P = .001), but the reason for this and the clinical significance are unclear. The protective trend of increased PTS against a persistent posterior drawer is consistent with prior cadaveric studies. Giffin et al12,13 performed 2 cadaveric studies to analyze the effect of PTS on knee joint biomechanics. The investigators demonstrated an anterior shift of the tibia with respect to the femur in knees with an increased PTS. This reduced the posterior tibial sag and posterior tibial translation (PTT). However, the studies did not demonstrate a difference in the anterior-posterior translation of the tibia. The cadaveric study by Petrigliano et al 27 demonstrated a reduction in the posterior drawer after PTS-increasing osteotomies. Conversely, those investigators reported an increase in the posterior drawer after PTS-decreasing osteotomies. These cadaveric results suggest a biomechanical relationship between PTS and posterior drawer after PCLR. Our results suggest a similar trend, although the protective effect of an increased PTS on posterior drawer testing did not reach statistical significance. Although cadaveric studies have suggested a relationship between PTS and knee laxity, the clinic data are limited. Gwinner et al 14 measured PTS and side-to-side difference in PTT before and after PCLR and demonstrated an inverse correlation between PTS and PTT. However, Bernhardson et al 6 performed a similar study and reported no significant correlation between PTS and side-to-side difference in PTT after PCLR. Although our study failed to demonstrate a statistically significant correlation, the results suggest that an increased PTS may be protective against a persistent posterior drawer.
Limitations
Our study has some limitations, including the limitations inherent to a retrospective study. These include heterogeneity of surgical techniques and rehabilitation protocols, although these differences were minimal for the surgeons in the current study, as standardized rehabilitation protocols have been implemented for >15 years. Our study had a wide range of PRO follow-up times. The mean length of PRO follow-up was 5.8 years (range, 2-20 years). It is possible the PRO values used in our analysis would yield different results if they were obtained at different times in each patient's recovery. Another limitation is the lack of a graft failure and revision cohort. Future studies that include cases of graft failure and revision should further evaluate the relationship between PTS and these adverse outcomes. An additional limitation is that laxity was based on physical examination findings obtained by the surgeon, which exposes the data to potential bias. However, the long study period and retrospective nature of the study made it impossible to obtain kneeling stress radiographs on each patient. Another potential limitation is the exclusion of coronal plane evaluation, which was beyond the scope of the current study. However, varus malalignment is implicated in patients with medial compartment knee osteoarthritis, which would confound the results of our PRO outcomes. Finally, our sample size of 37 patients could have been a limiting factor for the observance of statistically significant outcomes. However, to our knowledge, this is the largest data set evaluating PROs in relation to PTS after PCLR while excluding ACLR.
Conclusion
We found no significant differences in PROs or graft failure rates based on PTS at a mean follow-up of 5.8 years after PCLR. Increased PTS trended toward being protective against a positive posterior drawer, although this did not reach statistical significance.
Footnotes
Final revision submitted August 24, 2023; accepted September 7, 2023.
One or more of the authors has declared the following potential conflict of interest or source of funding: A.J.K. has received grants from DJO; consulting fees from Arthrex, JRF Ortho, and Responsive Arthroscopy; nonconsulting fees from Arthrex; royalties from Arthrex; and honoraria from JRF Ortho and MTF Biologics. K.R.O. has received education payments from Gemini Medical, consulting fees from Arthrex and Smith & Nephew, and nonconsulting fees from Smith & Nephew. M.J.S. has received research support from Arthrex and Stryker, education payments from Arthrex, consulting fees from Arthrex, nonconsulting fees from Arthrex, and royalties from Arthrex. B.A.L. has received consulting fees from Arthrex and Smith & Nephew; nonconsulting fees from Arthrex, Smith & Nephew, and Linvatec; and royalties from Arthrex. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Mayo Clinic (ref No. PR07-004018-16).
References
- 1. Abreu FG, Freychet B, Vieira TD, et al. All-arthroscopic treatment of combined posterior cruciate ligament and posterolateral corner instability. Arthrosc Tech. 2022;11(6):e977-e982. doi: 10.1016/j.eats.2022.01.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ahmad R, Patel A, Mandalia V, Toms A. Posterior tibial slope: effect on, and interaction with, knee kinematics. JBJS Rev. 2016;4(4):e31-e36. doi: 10.2106/jbjs.Rvw.O.00057 [DOI] [PubMed] [Google Scholar]
- 3. Arthur A, LaPrade RF, Agel J. Proximal tibial opening wedge osteotomy as the initial treatment for chronic posterolateral corner deficiency in the varus knee: a prospective clinical study. Am J Sports Med. 2007;35(11):1844-1850. doi: 10.1177/0363546507304717 [DOI] [PubMed] [Google Scholar]
- 4. Bernhardson AS, Aman ZS, DePhillipo NN, et al. Tibial slope and its effect on graft force in posterior cruciate ligament reconstructions. Am J Sports Med. 2019;47(5):1168-1174. doi: 10.1177/0363546519827958 [DOI] [PubMed] [Google Scholar]
- 5. Bernhardson AS, Aman ZS, Dornan GJ, et al. Tibial slope and its effect on force in anterior cruciate ligament grafts: anterior cruciate ligament force increases linearly as posterior tibial slope increases. Am J Sports Med. 2019;47(2):296-302. doi: 10.1177/0363546518820302 [DOI] [PubMed] [Google Scholar]
- 6. Bernhardson AS, DePhillipo NN, Aman ZS, Kennedy MI, Dornan GJ, LaPrade RF. Decreased posterior tibial slope does not affect postoperative posterior knee laxity after double-bundle posterior cruciate ligament reconstruction. Am J Sports Med. 2019;47(2):318-323. doi: 10.1177/0363546518819786 [DOI] [PubMed] [Google Scholar]
- 7. Bernhardson AS, DePhillipo NN, Daney BT, Kennedy MI, Aman ZS, LaPrade RF. Posterior tibial slope and risk of posterior cruciate ligament injury. Am J Sports Med. 2019;47(2):312-317. doi: 10.1177/0363546518819176 [DOI] [PubMed] [Google Scholar]
- 8. Christensen JJ, Krych AJ, Engasser WM, Vanhees MK, Collins MS, Dahm DL. Lateral tibial posterior slope is increased in patients with early graft failure after anterior cruciate ligament reconstruction. Am J Sports Med. 2015;43(10):2510-2514. doi: 10.1177/0363546515597664 [DOI] [PubMed] [Google Scholar]
- 9. Cooper JD, Wang W, Prentice HA, Funahashi TT, Maletis GB. The association between tibial slope and revision anterior cruciate ligament reconstruction in patients ≤21 years old: a matched case-control study including 317 revisions. Am J Sports Med. 2019;47(14):3330-3338. doi: 10.1177/0363546519878436 [DOI] [PubMed] [Google Scholar]
- 10. Dean RS, DePhillipo NN, Chahla J, Larson CM, LaPrade RF. Posterior tibial slope measurements using the anatomic axis are significantly increased compared with those that use the mechanical axis. Arthroscopy. 2021;37(1):243-249. doi: 10.1016/j.arthro.2020.09.006 [DOI] [PubMed] [Google Scholar]
- 11. Freychet B, Desai VS, Sanders TL, et al. All-inside posterior cruciate ligament reconstruction: surgical technique and outcome. Clin Sports Med. 2019;38(2):285-295. doi: 10.1016/j.csm.2018.11.005 [DOI] [PubMed] [Google Scholar]
- 12. Giffin JR, Stabile KJ, Zantop T, Vogrin TM, Woo SL, Harner CD. Importance of tibial slope for stability of the posterior cruciate ligament deficient knee. Am J Sports Med. 2007;35(9):1443-1449. doi: 10.1177/0363546507304665 [DOI] [PubMed] [Google Scholar]
- 13. Giffin JR, Vogrin TM, Zantop T, Woo SL, Harner CD. Effects of increasing tibial slope on the biomechanics of the knee. Am J Sports Med. 2004;32(2):376-382. doi: 10.1177/0363546503258880 [DOI] [PubMed] [Google Scholar]
- 14. Gwinner C, Weiler A, Roider M, Schaefer FM, Jung TM. Tibial slope strongly influences knee stability after posterior cruciate ligament reconstruction: a prospective 5- to 15-year follow-up. Am J Sports Med. 2017;45(2):355-361. doi: 10.1177/0363546516666354 [DOI] [PubMed] [Google Scholar]
- 15. Kim JS, Park SB, Choi HG, Jeong HW, Shim SJ, Lee YS. Is there any benefit in the combined ligament reconstruction with osteotomy compared to ligament reconstruction or osteotomy alone? Comparative outcome analysis according to the degree of medial compartment osteoarthritis with anterior or posterior cruciate ligament insufficiency. Arch Orthop Trauma Surg. 2023;143(7):3677-3689. doi: 10.1007/s00402-022-04544-9 [DOI] [PubMed] [Google Scholar]
- 16. King AH, Krych AJ, Prince MR, Pareek A, Stuart MJ, Levy BA. Surgical outcomes of medial versus lateral multiligament-injured, dislocated knees. Arthroscopy. 2016;32(9):1814-1819. doi: 10.1016/j.arthro.2016.01.038 [DOI] [PubMed] [Google Scholar]
- 17. Kovachevich R, Shah JP, Arens AM, Stuart MJ, Dahm DL, Levy BA. Operative management of the medial collateral ligament in the multi-ligament injured knee: an evidence-based systematic review. Knee Surg Sports Traumatol Arthrosc. 2009;17(7):823-829. doi: 10.1007/s00167-009-0810-4 [DOI] [PubMed] [Google Scholar]
- 18. Krych AJ, Giuseffi SA, Kuzma SA, Stuart MJ, Levy BA. Is peroneal nerve injury associated with worse function after knee dislocation? Clin Orthop Relat Res. 2014;472(9):2630-2636. doi: 10.1007/s11999-014-3542-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Levy BA, Dajani KA, Morgan JA, Shah JP, Dahm DL, Stuart MJ. Repair versus reconstruction of the fibular collateral ligament and posterolateral corner in the multiligament-injured knee. Am J Sports Med. 2010;38(4):804-809. doi: 10.1177/0363546509352459 [DOI] [PubMed] [Google Scholar]
- 20. Levy BA, Dajani KA, Whelan DB, et al. Decision making in the multiligament-injured knee: an evidence-based systematic review. Arthroscopy. 2009;25(4):430-438. doi: 10.1016/j.arthro.2009.01.008 [DOI] [PubMed] [Google Scholar]
- 21. Levy BA, Fanelli GC, Whelan DB, et al. Controversies in the treatment of knee dislocations and multiligament reconstruction. J Am Acad Orthop Surg. 2009;17(4):197-206. doi: 10.5435/00124635-200904000-00001 [DOI] [PubMed] [Google Scholar]
- 22. Levy BA, Piepenbrink M, Stuart MJ, Wijdicks CA. Posterior cruciate ligament reconstruction with independent suture tape reinforcement: an in vitro biomechanical full construct study. Orthop J Sports Med. 2021;9(2):2325967120981875. doi: 10.1177/2325967120981875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Martin RK, Melugin HP, Freychet B, Krych AJ, Stuart MJ, Levy BA. Posterior cruciate ligament all-inside reconstruction. Sports Med Arthrosc Rev. 2020;28(1):18-22. doi: 10.1097/jsa.0000000000000249 [DOI] [PubMed] [Google Scholar]
- 24. Nakazato K, Taketomi S, Inui H, Yamagami R, Kawaguchi K, Tanaka S. Lateral posterior tibial slope and length of the tendon within the tibial tunnel are independent factors to predict tibial tunnel widening following anatomic anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2021;29(11):3818-3824. doi: 10.1007/s00167-020-06419-1 [DOI] [PubMed] [Google Scholar]
- 25. Ni QK, Song GY, Zhang ZJ, et al. Steep posterior tibial slope and excessive anterior tibial translation are predictive risk factors of primary anterior cruciate ligament reconstruction failure: a case-control study with prospectively collected data. Am J Sports Med. 2020;48(12):2954-2961. doi: 10.1177/0363546520949212 [DOI] [PubMed] [Google Scholar]
- 26. Noyes FR, Barber-Westin SD. Posterior cruciate ligament revision reconstruction, part 1: causes of surgical failure in 52 consecutive operations. Am J Sports Med. 2005;33(5):646-654. doi: 10.1177/0363546504271210 [DOI] [PubMed] [Google Scholar]
- 27. Petrigliano FA, Suero EM, Voos JE, Pearle AD, Allen AA. The effect of proximal tibial slope on dynamic stability testing of the posterior cruciate ligament- and posterolateral corner-deficient knee. Am J Sports Med. 2012;40(6):1322-1328. doi: 10.1177/0363546512439180 [DOI] [PubMed] [Google Scholar]
- 28. Prince MR, Stuart MJ, King AH, Sousa PL, Levy BA. All-inside posterior cruciate ligament reconstruction: graftlink technique. Arthrosc Tech. 2015;4(5):e619-e624. doi: 10.1016/j.eats.2015.06.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Salmon LJ, Heath E, Akrawi H, Roe JP, Linklater J, Pinczewski LA. 20-Year outcomes of anterior cruciate ligament reconstruction with hamstring tendon autograft: the catastrophic effect of age and posterior tibial slope. Am J Sports Med. 2018;46(3):531-543. doi: 10.1177/0363546517741497 [DOI] [PubMed] [Google Scholar]
- 30. Sanders TL, Johnson NR, Levy NM, et al. Effect of vascular injury on functional outcome in knees with multi-ligament injury: a matched-cohort analysis. J Bone Joint Surg Am. 20 2017;99(18):1565-1571. doi: 10.2106/jbjs.16.01540 [DOI] [PubMed] [Google Scholar]
- 31. Savarese E, Bisicchia S, Romeo R, Amendola A. Role of high tibial osteotomy in chronic injuries of posterior cruciate ligament and posterolateral corner. J Orthop Traumatol. 2011;12(1):1-17. doi: 10.1007/s10195-010-0120-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Schulz MS, Russe K, Weiler A, Eichhorn HJ, Strobel MJ. Epidemiology of posterior cruciate ligament injuries. Arch Orthop Trauma Surg. 2003;123(4):186-191. doi: 10.1007/s00402-002-0471-y [DOI] [PubMed] [Google Scholar]
- 33. Song GY, Ni QK, Zheng T, Zhang ZJ, Feng H, Zhang H. Slope-reducing tibial osteotomy combined with primary anterior cruciate ligament reconstruction produces improved knee stability in patients with steep posterior tibial slope, excessive anterior tibial subluxation in extension, and chronic meniscal posterior horn tears. Am J Sports Med. 2020;48(14):3486-3494. doi: 10.1177/0363546520963083 [DOI] [PubMed] [Google Scholar]
- 34. Therrien E, Pareek A, Song BM, Wilbur RR, Stuart MJ, Levy BA. All-inside PCL reconstruction. J Knee Surg. 2021;34(5):472-477. doi: 10.1055/s-0040-1722313 [DOI] [PubMed] [Google Scholar]
- 35. Wilson SM, Mehta N, Do HT, Ghomrawi H, Lyman S, Marx RG. Epidemiology of multiligament knee reconstruction. Clin Orthop Relat Res. 2014;472(9):2603-2608. doi: 10.1007/s11999-014-3653-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Winkler PW, Wagala NN, Carrozzi S, et al. Low posterior tibial slope is associated with increased risk of PCL graft failure. Knee Surg Sports Traumatol Arthrosc. 2022;30(10):3277-3286. doi: 10.1007/s00167-021-06760-z [DOI] [PubMed] [Google Scholar]
- 37. Woodmass JM, O’Malley MP, Krych AJ, et al. Revision multiligament knee reconstruction: clinical outcomes and proposed treatment algorithm. Arthroscopy. 2018;34(3):736-744. doi: 10.1016/j.arthro.2017.09.022 [DOI] [PubMed] [Google Scholar]
- 38. Ziegler CG, DePhillipo NN, Kennedy MI, Dekker TJ, Dornan GJ, LaPrade RF. Beighton score, tibial slope, tibial subluxation, quadriceps circumference difference, and family history are risk factors for anterior cruciate ligament graft failure: a retrospective comparison of primary and revision anterior cruciate ligament reconstructions. Arthroscopy. 2021;37(1):195-205. doi: 10.1016/j.arthro.2020.08.031 [DOI] [PubMed] [Google Scholar]