Abstract
Aims
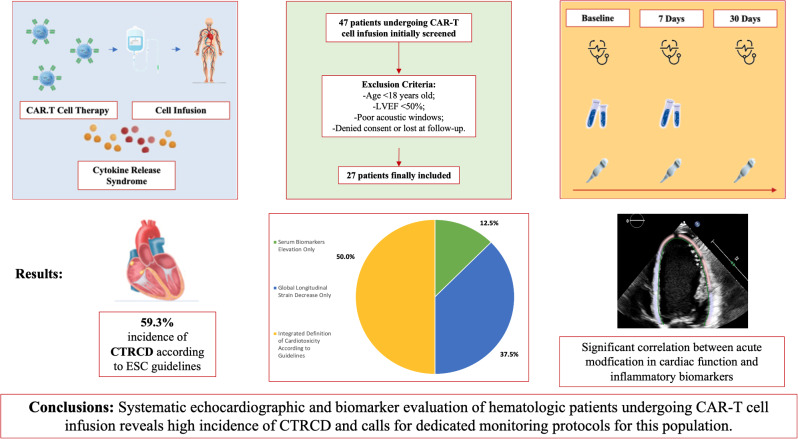
Chimeric Antigen Receptor-T (CAR-T) cell infusion is a rapidly evolving antitumor therapy; however, cardiovascular (CV) complications, likely associated with cytokine release syndrome (CRS) and systemic inflammation, have been reported to occur. The CARdio-Tox study aimed at elucidating incidence and determinants of cardiotoxicity related to CAR-T cell therapy.
Methods
Patients with blood malignancies candidate to CAR-T cells were prospectively evaluated by echocardiography at baseline and 7 and 30 days after infusion. The study endpoints were i) incidence of cancer therapy-related cardiac dysfunction (CTRCD), CTRCD were also balanced for any grade CRS, but CTRCD occurred of Cardiology Guidelines on Cardio-Oncology (decrements of left ventricular ejection fraction (LVEF) or global longitudinal strain (GLS) and/or elevations of cardiac biomarkers (high sensitivity troponin I, natriuretic peptides) and ii), correlations of echocardiographic metrics with inflammatory biomarkers.
Results
Incidence of CTRCD was high at 7 days (59,3%), particularly in subjects with CRS. The integrated definition of CTRCD allowed the identification of the majority of cases (50%). Moreover, early LVEF and GLS decrements were inversely correlated with fibrinogen and interleukin-2 receptor levels (p always ≤ 0.01).
Conclusions
There is a high incidence of early CTRCD in patients treated with CAR-T cells, and a link between CTRCD and inflammation can be demonstrated. Dedicated patient monitoring protocols are advised.
Graphical Abstract
Supplementary Information
The online version contains supplementary material available at 10.1186/s40959-024-00218-0.
Keywords: Chimeric antigen receptor-T cells, Inflammation, Cardiotoxicity, Echocardiography, Cardio-Oncology, Hematological malignancies
Introduction
Chimeric antigen receptor (CAR)-T cell therapy represents an effective therapeutic opportunity for patients with advanced hematological malignancies, delivering a significant improvement in response rates [1–3]; however, data from clinical trials and real-word reports show that numerous adverse events may occur [4, 5]. The main CAR-T cell toxicity is represented by the cytokine release syndrome (CRS), a subtype of systemic inflammatory response syndrome [6] which is characterized by an excessive systemic inflammatory response secondary to the interaction between the engineered T-cells, immune effectors and the tumor microenvironment [7]. Clinical presentation of CRS ranges from mild flu-like symptoms to life-threatening multiorgan dysfunction [7]. These manifestations do not spare the cardiovascular (CV) system, as denoted by cases of severe cardiac dysfunction, arrhythmias, and cardiovascular death [8–10].
Cause-and-effect relations between CRS severity and CV toxicity have been hypothesized [8–10], but prospective studies that probed optimal modalities for detecting and monitoring inflammation and CV toxicity in this unique patient population are scarce [11]. The CARdio-TOX study is a single center, prospective, proof-of-concept study of adult patients affected by refractory or relapsed (R/R) hematologic malignancies and treated with CAR-T cells. We recently reported that patients recruited in CARdio-TOX exhibited impaired left ventricle ejection fraction (LVEF) and global longitudinal strain (GLS) as early as 7 days after CAR-T cells infusion, with concomitant changes of several exploratory diastolic metrics occurring at the same time point [12]. Patient re-evaluation at 30 days showed an incomplete recovery of systolic and diastolic parameters, possibly denoting that acute myocardial damage may or may not resolve over time and pave the road to chronic toxicity and late clinical outcomes.
In the present study, we aimed at elucidating both the incidence of Cancer therapy-related cardiac dysfunction (CTRCD), defined as an aggregate of echocardiographic and biomarker abnormalities, and correlations between imaging alterations and bio-humoral indexes of inflammation.
Patients and methods
Study design and patient characteristics
CARdio-TOX is a non-profit, investigator-initiated, prospective, single center, real-life study conducted at the Department of Cardiovascular Medicine of Fondazione Policlinico Universitario A. Gemelli IRCCS, Rome, Italy, between April 2022 and April 2023. Adult patients eligible to CAR-T cell therapy underwent clinical, electrocardiographic and echocardiographic evaluations at baseline and then at 7 and 30 days after CAR-T cell administration. Three anti CD19 CAR-T cell preparations were used according to clinicians’ indications: Axicabtagene Ciloleucel (Yescarta, Kite Pharmaceuticals, Santa Monica, California), Tisagenlecleucel (Kymriah, Novartis Pharmaceuticals, East Hanover, New Jersey), Brexucabtagene Autoleucel (Tecartus, Kite Pharma EU B.V.). Inclusion criteria were age > 18, years, LVEF ≥ 50% and a confirmed diagnosis of R/R CD19+ B-cell malignancy (lymphoma or acute lymphoblastic leukemia) with two or more prior systemic therapies. Exclusion criteria were age < 18 years and left ventricular ejection fraction (LVEF) < 50% or poor acoustic window at baseline echocardiography. The following information was extracted from patient medical records: prior CV events, CV risk factors (arterial hypertension, smoking, diabetes mellitus, dyslipidemia), history of potentially cardiotoxic therapies (chemotherapy, immunotherapy, left chest radiation therapy, autologous hematopoietic stem cell transplantation [HSCT].
The primary objective was the incidence of CTRCD at 7 days after CAR-T cell infusion. CTRCD was defined according to 2022 European Society of Cardiology (ESC) Cardio-Oncology guidelines (LVEF reduction by ≥ 10% points to an LVEF of 40–49%, or LVEF reduction by < 10% points to an LVEF of 40– 49%, or a decline of global longitudinal strain (GLS) by ≥ 15% from baseline, or increases in cardiac biomarkers such as troponin or B-type natriuretic peptide) [13]. Indexes of LV dysfunction (LVEF, GLS) were then correlated with serum inflammatory biomarkers such as C-reactive protein (CRP), fibrinogen, ferritin, soluble interleukin 2 receptor (sIL-2r), interleukin 6 (IL-6).
The study was approved by the Institutional Ethic Committee. No extramural funding supported this work. The authors are solely responsible for study design and conduct, study analyses, drafting and editing of the paper, as well as its final content.
Echocardiographic evaluation
Transthoracic 2D echocardiography (TTE) was performed using Philips EPIQ7C (Philips Medical Systems, Andover, Massachusetts, USA). Colour, pulsed-wave and continuous wave Doppler images were acquired from the parasternal, apical and subcostal views [14, 15]. All images were digitally stored for offline analyses by an experienced operator (L.M.). 2D-Strain (2D-ST) analysis was determined from views acquired during three consecutive cardiac cycles, using a TomTec-Arena TM software (TomTec Imaging Systems, Unterschleissheim, Germany). LV-GLS was calculated from the average values of four-chamber, two-chamber, and three-chamber curves. LV dimension, LA volume with strain analysis and right ventricle (RV) longitudinal function were measured according to recommendations by the European Association of Cardiovascular Imaging (EACVI) and the American Society of Echocardiography (ASE) [14–16]. LV diastolic function, non-invasive estimation of LV filling pressures, and valvular heart diseases were evaluated according to current recommendations [17, 18]. Intra-observer and inter-observer variability assessment and values for our echocardiographic laboratory have been previously described [19].
Cardiac and inflammatory biomarkers
Blood samples for cardiac and inflammatory biomarkers were drawn before and 7 days after CAR-T cell infusion. High-sensitivity troponin I (hsTnI), soluble protein ST2 (sST2) and the aminoterminal fragment of prohormone BNP (Nt-proBNP) were used as cardiac biomarkers; IL6, sIL2r, ferritin and fibrinogen were used as inflammatory biomarkers as per institutional clinical practice. All biomarkers were measured according to validated protocols of the institutional Medicinal Chemistry department. CRS grade and any required treatment for CRS management were in accordance to the American Society for Transplantation and Cellular Therapy (ASTCT) consensus [20].
Statistical analyses
Dichotomous variables were expressed as counts (percentage). The distribution of continuous variables was tested using Kolmogorov–Smirnov test. Mean ± standard deviation was used to express continuous variables with normal distribution, while median (interquartile range) was used for variables with non-normal distribution. Continuous variables were compared using an unpaired Student’s t test or Mann–Whitney U test. Categorical data were evaluated using the χ2 test or Fisher exact test, as appropriate.
Differences in each continuous echocardiographic parameter and inflammatory biomarker between day 7 and baseline were expressed as ∆:100*(day 7 minus baseline)/baseline.
All tests were two-sided, and statistical significance was set at P < 0.05. All analyses were performed using SPSS (SPSS version 23, Inc., Chicago, IL, USA) statistical software.
Results
Patient characteristics and CTRCD incidence
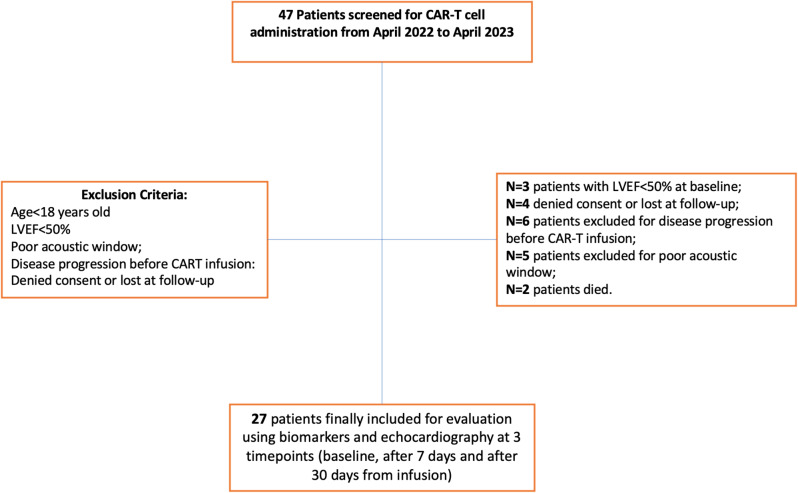
Forty-seven patients candidate for CAR-T cell therapy were screened, of whom 27 were eventually enrolled (Fig. 1).Sixteen patients (59,3% of the study population) were diagnosed CTRCD as per guidelines definition [13]. Patients with or without CTRCD were balanced for age, oncologic characteristics, common comorbidities and risk factors (hypertension, diabetes, smoking), as well as baseline laboratory and imaging findings; however, cardiotoxicity occurred more frequently in females (p = 0.042). CRS occurred in a total of 24 patients (88.8%) and the anti IL6 receptor antibody, tocilizumab, was used in 19 (70.4%) patients. Patients with or without CTRCD were also balanced for any grade CRS, but CTRCD occurred more often in patients with grade > 2 CRS [20]. Fever and usage of tocilizumab were therefore more frequent in patients with CTRCD (see also Table 1). As for CV events, we recorded only one case of non-fatal cardiac arrest in the context of severe CRS, a case of acute heart failure and a case of paroxysmal atrial fibrillation.
Fig. 1.
Study Flowchart. Abbreviations CAR-T = Chimeric Antigen Receptor-T; LVEF = left ventricular ejection fraction
Table 1.
Patient baseline characteristics (overall and according to the occurrence of cancer therapy-related cardiac dysfunction)
| Overall population 27 patients (100%) |
CTRCD 16 patients (59,3%) |
No CTRCD 11 patients (40,7%) |
P value | |
|---|---|---|---|---|
| Demographics | ||||
| Age, years [mean ± standard deviation] | 60.5 ± 10.4 | 58.8 ± 11.7 | 63.1 ± 7.9 | 0.260 |
| Female sex [n, (%)] | 9 (33.3) | 8 (88) | 1 [11] | 0.042 |
| Cardiovascular risk factors | ||||
| Hypertension [n, (%)] | 20 (74.1) | 10 (62.5) | 10 (90.1) | 0.183 |
| Diabetes [n, (%)] | 4 (14.8) | 2 (12.5) | 2 (18.2) | 1,000 |
| Smoking [n, (%)] | 12 (44.4) | 6 (37.5) | 6 (54.5) | 0,452 |
| Dyslipidemia [n, (%)] | 4 (14.8) | 3 (18.8) | 2 (18.2) | 1,000 |
| Previous history of IHD [n, (%)] | 0 (0) | 0 (0) | 0 (0) | |
| Electrocardiographic parameters | ||||
| Heart rate, bpm [mean ± standard deviation] | 84.1 ± 16.5 | 86.1 ± 13.6 | 80.5 ± 21.8 | 0.586 |
| PR duration, milliseconds [mean ± standard deviation] | 156.0 ± 32.8 | 155.0 ± 29.6 | 141.0 ± 41.6 | 0.939 |
| QRS duration, milliseconds [mean ± standard deviation] | 91.6 ± 8.6 | 90.7 ± 8.0 | 93.5 ± 10.2 | 0.567 |
| Complete left bundle branch block, [n, (%)] | 0 (0) | 0 (0) | 0 (0) | |
| Complete right bundle branch block, [n, (%)] | 0 (0) | 0 (0) | 0 (0) | |
| Medications | ||||
| Beta-blockers [n, (%)] | 8 (29.6) | 4 (25.0) | 4 (36.4) | 0.675 |
| ACE inhibitors/ARBs | 10 (37.0) | 5 (31.3) | 5 (45.5) | 0.687 |
| MRA [n, (%)] | 0 (0) | 0 (0) | 0 (0) | |
|
Prior Oncologic Therapies Anthracycline cumulative dose, mg/m2 [median (IQR)] |
585.0(566.0-1019.0) | 579.0 (561.0-888.0) | 600.0 (574.0-1034.0) | 0.562 |
| Previous Autologous HSCT [n, (%)] | 14 (51.9%) | 9 (56.3) | 5 (45.5) | 0.704 |
| Number of Previous Chemotherapy Lines mean ± standard deviation] | 2.79 ± 1.29 | 2.94 ± 1.61 | 2.55 ± 0.69 | 0.456 |
| CAR-T cell formulation | ||||
| Axicabtagene Ciloleucel [n, (%)] | 10 (37.1) | 7 (43.8) | 3 (27.3) | 0.448 |
| Tisagenlecleucel [n, (%)] | 9 (33.3) | 4 (25.9) | 5 (45.4) | 0.411 |
| Brexucabtagene Autoleucel [n, (%)] | 8 (29.6) | 5 (31.3) | 3 (27.3) | 1.000 |
| Laboratory data | ||||
| PLT x103/L [median (IQR)] | 154.0 (97.0-186.5) | 157.0(100.5-216.3) | 137.0(95.5–157) | 0.267 |
| Serum creatinine, mg/dL [mean ± standard deviation] | 0.9 ± 0.3 | 0.9 ± 0.3 | 1.0 ± 0.2 | 0.320 |
| Fibrinogen, mg/dL [median (IQR)] | 387.0 (297.0-466.0) | 409.0 (296.0-556.0) | 374.0 (310.0-387.0) | 0.208 |
| D-Dimer [median (IQR)] | 997.0 (754.0-1573.0) | 1078.0 (751.0-1804.0) | 997.0 (915.0-1323.0) | 0.981 |
| Ferritin, ng/mL [median (IQR)] | 193.0 (129.0-479.0) | 195.0 (134.0-531.0) | 193.0 (132.0-479.0) | 0.981 |
| Partial thromboplastin time, seconds [mean ± standard deviation] | 30.3 ± 4.4 | 29.7 ± 4.6 | 31.3 ± 4.2 | 0.364 |
| Antithrombin-III, % [mean ± standard deviation] | 99.0 ± 11.5 | 97.5 ± 11.3 | 101.0 ± 11.9 | 0.431 |
| VIII Factor, % [median (IQR)] | 193.0 (154.0-225.0) | 195.0 (157.0-223.0) | 193.0 (150.0-221.0) | 1.000 |
| Von Willebrand Factor, % [median (IQR)] | 207.0 (180.0-260.0) | 207.0 (182.0-253.0) | 220.0 (177.0-284.0) | 0.827 |
| Cardiac biomarkers | ||||
| hs-Troponin T, ng/mL [median (IQR)] | 5.0 (4.0–6.0) | 5.0 (3.8-5.0) | 5.0 (5.0–7.0) | 0.179 |
| NT-proBNP, pg/mL [median (IQR)] | 30.5 (15.5–124.0) | 57.0 (22.0-142.0) | 16.0 (12.0-111.0) | 0.121 |
| sST2, ng/mL [median (IQR)] | 27.0 (21.5–42.8) | 27.0 (18.5–36.3) | 27.0 (22.3–52.8) | 0.470 |
| Inflammatory biomarkers | ||||
| Interleukin 2 receptor, UI/L [median (IQR)] | 1416.0 (1113.0-2378.0) | 1334.0 (1160.0-1930.0) | 1540.0 (1084.0-2378.0) | 0.923 |
| Interleukin 6, ng/L [median (IQR)] | 23.6 (12.3–86.9) | 31.9 (11.3–155.0) | 19.6 (13.4–28.6) | 0.633 |
| Echocardiographic parameters | ||||
| LVEDV, ml [mean ± standard deviation] | 94.5 ± 19.5 | 91.6 ± 21.4 | 98.6 ± 16.3 | 0.344 |
| LVESV, ml [median (IQR)] | 39.0 (30.0-47.5) | 34.5 (29.0-44.5) | 40 (35.5–47.5) | 0.387 |
| LV Simpson Biplane EF, % [median (IQR)] | 60.0 (56.0-61.5) | 60.0 (55.0-62.3) | 60.0 (56.5–60.0) | 0.765 |
| LV GLS, % [mean ± standard deviation] | -18.2 ± 2.2 | -17.9 ± 2.6 | -18.8 ± 1.6 | 0.260 |
| Medial mitral S’ velocity, cm/s [mean ± standard deviation] | 9.4 ± 1.8 | 9.1 ± 2.0 | 9.9 ± 1.4 | 0.276 |
| E/A ratio [median (IQR)] | 0.8 (0.7-1.0) | 0.8 (0.7-1.0) | 0.8 (0.7–1.1) | 0.708 |
| E/e’ ratio, units [median (IQR)] | 6.0 (5.0-8.5) | 5.5 (4.0–7.0) | 9.0 (6.0-10.5) | 0.011 |
| LAV max, ml [mean ± standard deviation] | 47.6 ± 12.6 | 44.9 ± 12.5 | 51.4 ± 12.2 | 0.197 |
| LA Reservoir Strain, % [mean ± standard deviation] | 22.3 ± 5.4 | 21.6 ± 6.3 | 23.4 ± 4.1 | 0.392 |
| TAPSE, mm [median (IQR)] | 21.0 (18.0-23.5) | 20.5 (18.0–23.0) | 22.0 (20.0-24.5) | 0.485 |
| S’ RV, cm/s [mean ± standard deviation] | 12.8 ± 2.4 | 12.4 ± 2.4 | 13.3 ± 2.5 | 0.398 |
| Cytokine release syndrome | 24 (88,8) | 16 (100) | 8 (72.7) | 0.057 |
| Cytokine Release Syndrome grade ≥ 2, [n, (%)] | 19 (70.4) | 15 (93.8) | 4 (36.4) | 0.002 |
| Neurotoxicity, [n, (%)] | 10 (37.0) | 5 (31.3) | 5 (45.5) | 0.687 |
| Fever, [n, (%)] | 23 (85.2) | 16 (100) | 7 (63.6) | 0.019 |
| Hypotension, [n, (%)] | 14 (51.8) | 10 (62.5) | 4 (36.4) | 0.252 |
| Tocilizumab Use, [n, (%)] | 19 (70.4) | 15 (93.8) | 4 (36.4) | 0.002 |
| Corticosteroid Use, [n, (%)] | 10 (37.0) | 6 (37.5) | 4 (36.4) | 1.000 |
CAR-T: chimeric antigen receptor- T cells; CTRCD = cancer therapy-related cardiac dysfunction; CVD = cardiovascular disease; EDV = end-diastolic volume; EF = ejection fraction; ESV = end-systolic volume; GLS = global longitudinal strain; Hb = haemoglobin; HSCT = hematopoietic stem cell transplantation; IQR = interquartile range; LA = left atrial; LAEF = Left Atrial Emptying Fraction; LAV = left atrial volume; LV = left ventricular; MRA = mineralocorticoid receptor antagonist; NT-proBNP = N-terminal pro-brain natriuretic peptide; PLTs = platelets; RV = right ventricle; TAPSE = tricuspid annulus plane systolic excursion; WBC = white blood cells
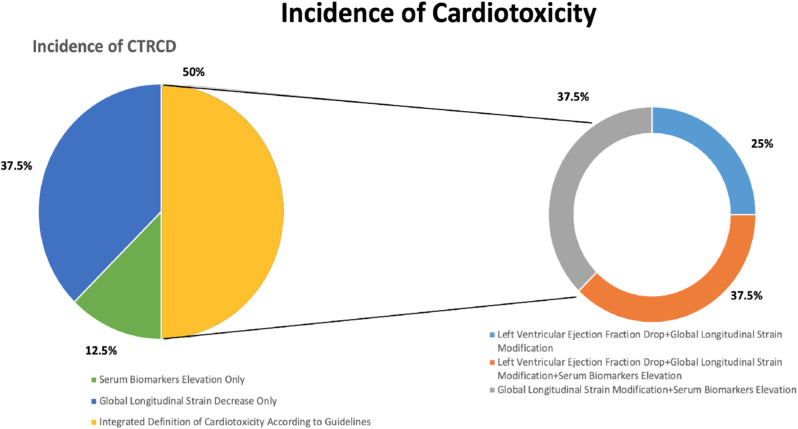
Patterns of CTRCD
Out of 16 patients diagnosed with CTRCD, 2 (12,5%) were characterized by only elevations of hsTnI or NT-proBNP, 6 (37,5%) were characterized by GLS decline ≥ 15% from baseline, and 8 (50%) were characterized by a composite of biomarkers and GLS with or without LVEF decrements (Fig. 2). Overall, GLS decrements were observed in 14 of 16 cardiotoxicity cases, followed by serum biomarkers elevations and LVEF decrements (9 and 5 of 16 cases, respectively). Patterns of LVEF and GLS changes are shown in Fig. 3, while a complete description of echocardiographic findings is reported in Table 1, Supplementary Materials.
Fig. 2.
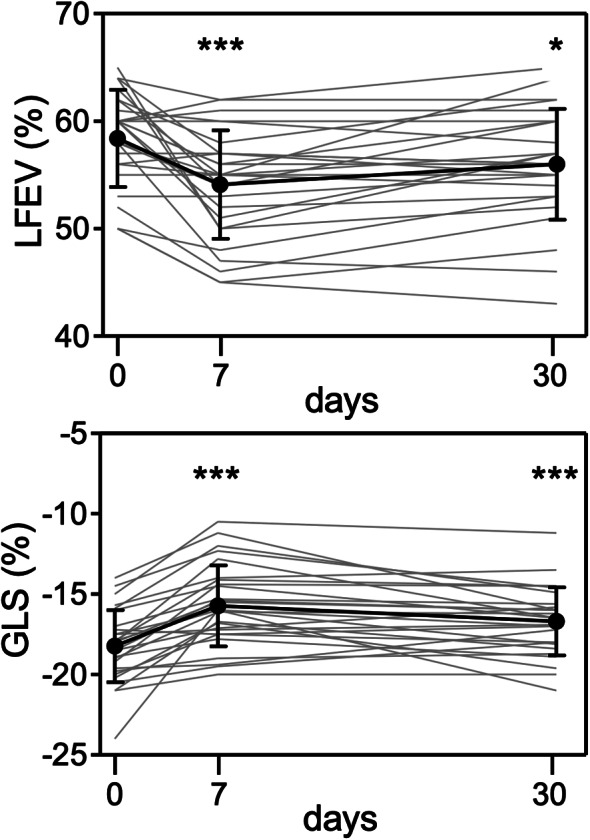
Temporal trends of LVEF and GLS in patients treated with CAR-T cells. Each panel shows individual data and means ± SD (at baseline and 7 and 30 days after CAR-T cells). Single or triple asterisks indicate P < 0.05 or P < 0.001 for LVEF and GLS at day 7 or 30 versus baseline. Abbreviations GLS = global longitudinal strain; LVEF = left ventricular ejection fraction
Fig. 3.
Graphical distribution of cancer therapy-related cardiac dysfunction (CTRCD) according to the definition used
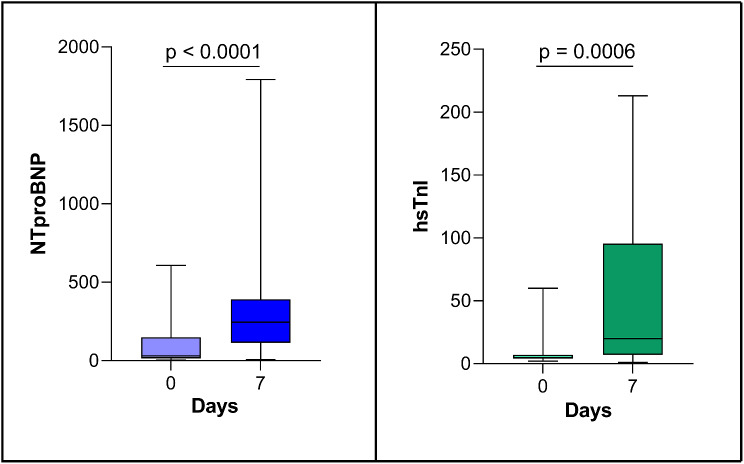
Changes in serum cardiac biomarkers at day 7 after CAR-T cell therapy are reported in Table 2; Fig. 4. In addition to significant elevations of hsTnI and NT-proBNP, there was a significant increase of sST2, marker of myocardial fibrosis (see also Table 2).
Table 2.
Temporal Trends of biomarkers evaluated at two timepoints (baseline before chimeric antigen receptor-T cell infusion and 7 days after administration)
| Baseline | 7 days | p-value | ||
|---|---|---|---|---|
| Cardiac Biomarkers | ||||
| hs-Troponin T, ng/mL [median (IQR)] | 5.0 (4.0–6.0) | 20.0 (7.0-94.5) | < 0,001 | |
| NT-proBNP, pg/mL [median (IQR)] | 30.5 (15.5–124.0) | 245.0 (152.0–363.0) | < 0,001 | |
| sST2, ng/mL [median (IQR)] | 27.0 (21.5–42.8) | 54.0 (24.5–140.0) | 0.032 | |
hs = high sensitivity; NT-proBNP = N-terminal prohormone of brain natriuretic peptide; sST2 = soluble ST2
Fig. 4.
Early modifications (7 days after infusion to baseline) of serum cardiac biomarkers. Abbreviations hsTnI = high sensitivity troponin I; NTproBNP = N-terminal pro b-type natriuretic peptide
Correlations between left ventricular systolic function and inflammatory markers
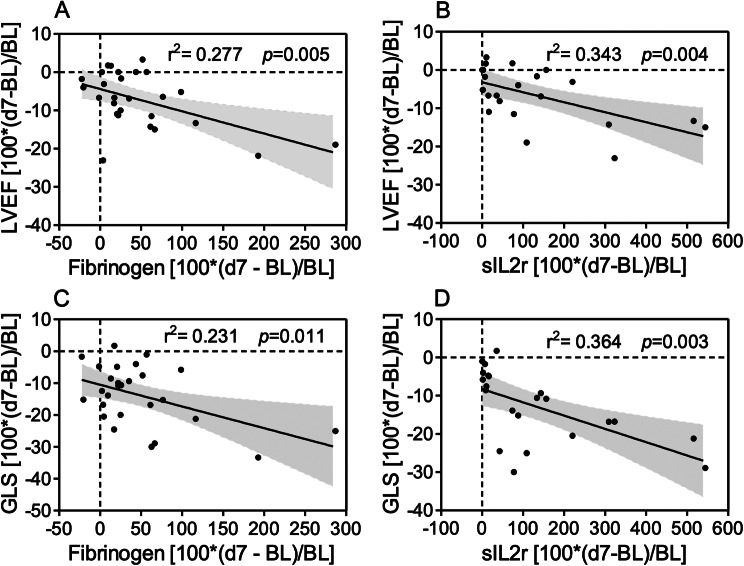
We characterized whether day 7 changes of LVEF and GLS, parameters of systolic function reported in ESC guidelines definition of CTRCD [13], correlated with changes of inflammatory biomarkers at the same time point. A statistically significant inverse correlation occurred between changes of LVEF or GLS and sIL2r or fibrinogen (Fig. 5). No correlation was observed with CRP, IL6, ferritin (not shown).
Fig. 5.
Significant Inverse Correlations between Early Changes in Echocardiographic Parameters and Inflammatory Indexes. Data were linear regression analyses with 95% confidence intervals of percentage differences of echocardiographic parameters versus inflammatory indexes, all expressed as 100*(day 7 minus baseline)/baseline. Panel A, LVEF versus fibrinogen; Panel B, LVEF versus sIL2r; panel C, GLS versus fibrinogen; panel D, GLS versus sIL2r. Similar results were obtained by non-parametric two-tailed correlation (p = 0.052, 0.005, 0.062 and 0.0001 in panels A, B, C and D, respectively). Abbreviations GLS = left ventricular global longitudinal strain; sIL2r = soluble interleukin 2 receptor; LVEF = left ventricular ejection fraction; d7 = day 7; BL, baseline
Discussion
Uncertainties remain around the actual incidence of CTRCD in patients treated with CAR-T cells [21–27]. A study of 137 patients found that 5.8% of them developed a significant drop in LVEF (defined as a decrease of at least 10% points to a value below 50%), mainly associated with the occurrence of grade ≥ 2 CRS [22]. Other studies showed that a reduction of LVEF below 50% or > 10% from baseline during index hospitalization occurred in 10.3% of 116 patients, with a decline in median LVEF from 58 to 37% at ∼ 12 days from CAR T-cell infusion [23]. Again, most of patients diagnosed with CTRCD had grade ≥ 2 CRS, further highlighting possible cause-and-effect relations between systemic inflammation and cardiotoxicity. On the other hand, the recently released ESC Cardio-Oncology guidelines recommend a definition of CTRCD that integrates abnormalities of imaging parameters and serum biomarkers, such as LVEF, GLS, troponin and natriuretic peptide [13]. In accordance with this definition, we were able to diagnose CTRCD in as many as 16 patients treated with CAR-T cells. Had we defined CTRCD only on the basis of LVEF decrements, its incidence would have been 18,5% (5 cases out of 27 patients).
The high incidence of CTRCD observed in our study warrants further considerations. Our patients received serial echocardiographic and biomarkers evaluations, which were done prospectively at pre-specified time points. This approach likely avoided the risk of underestimating CTRCD, that otherwise would bias studies in which imaging and laboratory evaluations were event-driven. In this context, it was not until recently when Lefebvre et al. prospectively evaluated 44 patients prior to and 2 days, 1 week, 1 month, and 6 months after CAR-T cell infusion [11]. No significant changes in LVEF were noticed across study visits and only a modest decrease in GLS was shown to occur at the early time points. Interestingly, only 52% of subjects developed CRS as opposed to at least 70% in previous reports and 89% in our present study; moreover, CRS was of a low grade in 95% of cases [11]. Lower incidence and severity of CRS may help to explain the milder cardiovascular manifestations observed by Lefebvre et al. compared to our study.
Having said that the high incidence of CTRCD observed in our study originates from the updated definition of CTRCD released by ESC [13], largely based on subclinical indexes like GLS and serum biomarkers, we believe that detecting such early manifestations might be important for improving CV outcomes in the cancer patient. A multicenter registry of 202 CART-cell patients receiving anti-CD19 therapies aimed at assessing a composite endpoint of heart failure, cardiogenic shock, or myocardial infarction [25]. Sixteen percent of subjects experienced severe cardiac events, which were independently associated with overall mortality (hazard ratio 2.8). In analyzing determinants of event occurrence the authors identified a role for CV risk factors, in particular hypertension and history of atrial fibrillation or heart failure; interestingly, however, there was no information on clinical usage of anti-IL6 medications to mitigate CRS in these patients [25]. Post-marketing analyses similarly showed a fatality rate of CV and pulmonary adverse events, including late-occurring cardiomyopathy, tachyarrhythmias, pleural and pericardial effusions, as high as 30.9% [26]. None of our patients presented at treatment with a history of heart failure, ischemic heart disease, or arrhythmias, which probably explains why we did not record a significant incidence of fatal CV events after CAR-T cell therapy. However, the high incidence of CTRCD that we characterized as early as 7 days after CAR-T cell infusion, serves a rationale to intensify CV surveillance in high-risk patients with a potentially worse CV outcome. The ESC cardio-oncology guidelines advocate intensive surveillance in cases of signs and symptoms of congestion or high-grade CRS, but they do not clarify how often and how long patients should be surveilled [13].
There are further differences, as well as similarities, between our study and previously published reports. Older age, dyslipidemia and coronary artery disease were reported to increase the risk of cardiomyopathy after CAR-T cell therapy [22]. As already mentioned, our study did not recruit patients with a history of ischemic heart disease but hypertension, diabetes and smoking were equally represented among patients with or without CTRCD. On a different note, but in agreement with others [22, 23], we also found that neither the number of prior lines of therapy nor the cumulative anthracycline dose were significantly different among patients with or without CTRCD. This latter finding denotes the distinct nature of CAR-T cells cardiotoxicity, as previous treatment with anthracyclines usually aggravates the risk of cardiotoxicity upon patient’s exposure to subsequent cancer therapies.
Limitations
We acknowledge this was a single institution study, with a small sample size. The lack of a control arm in which patients with the same oncologic diagnosis received treatments with other drugs, possibly including newly developed bispecific antibodies that also cause some degree of CRS, preclude further considerations on the actual risk:benefit of CAR-T cells in terms of CV liability. Furthermore, the very low incidence of major CV events in our study population, likely reflecting the extensive use of anti-IL6 medication and short-follow-up, does not allow us to approximate how well such events would have been predicted by the imaging and bio-humoral markers we used to define CTRCD. Finally, the majority of subjects enrolled were males, preventing generalization of findings to females.
Strengths
In addition to denoting the value of integrating echocardiographic parameters with serum biomarkers, this study provides novel information on the relations between inflammation and CTRCD. We in fact confirmed a higher incidence of CTRCD in patients with grade ≥ 2 CRS, but we also investigated, for the first time in adult patients [27], on the association between changes in LVEF or GLS and inflammatory biomarkers. We did not find correlations with CRP, IL6 and ferritin, as tocilizumab interferes with IL6 assay [28] and reduces both CRP [29] and ferritin levels [30]; however, we found significant correlations with sIL2R, whose levels are relatively stable after tocilizumab initiation [31], and with fibrinogen, which shows longer half-life than ferritin [32, 33] and thus attains circulating levels more suitable for correlation analyses once tocilizumab has been started. These findings strengthen a causative link between inflammation and CAR-T cells cardiotoxicity, paving the road to further studies in these settings [34].
In addition, besides conventional cardiac biomarkers such as hsTnI and NT-proBNP, we characterized early changes of sST2, currently considered as an index of myocardial remodeling and fibrosis [35]. sST2 significantly increased at day 7, similar to hsTnI and Nt-proBNP (Table 2). As the ST2 gene is upregulated in the setting of myocardial stretch, these findings raise one more research issue in the settings of CAR-T cells cardiotoxicity [35].
Conclusions
This prospective study shows, for the first time, that a large proportion of patients treated with anti CD19 CAR-T cells may experience acute CTRCD, as defined by recent Cardio-Oncology guidelines. Moreover, a remarkable association of CTRCD with an inflammatory primum movens is confirmed by more direct correlations than in previous studies [36]. We therefore propose a systematic approach of clinical surveillance and comprehensive evaluation of patients undergoing CAR-T cell therapy, including both imaging and laboratory indexes as suggested by cardio-oncology guidelines. Early monitoring would remarkably assist the identification of patients at risk of developing severe cardiomyopathy. An extended follow-up, which was beyond the aims of this proof-of-concept study, would in turn elucidate the size effect of acute cardiotoxicity on late clinical outcomes.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
Not applicable.
Abbreviations
- CAR-T
chimeric antigen receptor-T
- CRP
c-reactive protein
- CRS
cytokine release syndrome
- CTRCD
cancer therapy-related cardiac dysfunction
- CV
cardiovascular
- IL
interleukin
- LA
left atrium
- LVEF
left ventricular ejection fraction
- LVGLS
left ventricular global longitudinal strain
Biographies
Massimiliano Camilli
is MD and Cardiologist at IRCSS Fondazione Policlinico Universitario Agostino Gemelli in Rome; he is a PhD student at Catholic University of the Sacred Heart, Rome. Principal fields of interest are Cardio-Oncology, Heart Failure and applied imaging.
Marcello Viscovo
is Hematologist and PhD student at IRCSS Fondazione Policlinico Universitario Agostino Gemelli in Rome. Principal fields of interest are cardiotoxicity and CAR-T cells.
Tamara Felici
is Cardiologist with principal interests in cardio-oncology and cardiovascular imaging.
Luca Maggio
is Cardiology resident at Catholic University of the Sacred Heart in Rome with main interest in cardio-oncology and cardiovascular imaging.
Federico Ballacci
is Cardiology resident at Catholic University of the Sacred Heart in Rome with main interest in epidemiology and statistics.
Giacomo Carella
is Cardiology resident at Humanitas research Hospital Milan with main focus in cardio-oncology.
Alice Bonanni
is biologist at Policlinico Universitario Agostino Gemelli with main interest in inflammation and cardiovascular diseases.
Priscilla Lamendola
is Cardiologist with principal interests in cardio-oncology and cardiovascular imaging.
Lorenzo Tinti
is Cardiology resident at Catholic University of the Sacred Heart in Rome with main interest in cardio-oncology and cardiovascular imaging.
Antonio Di Renzo
is Cardiology resident at Catholic University of the Sacred Heart in Rome with main interest in cardio-oncology and cardiovascular imaging.
Giulia Coarelli
is Cardiologist in Rome with main interests in cardio-oncology and cardiovascular imaging.
Eugenio Galli
is Hematologist and PhD student at IRCSS Fondazione Policlinico Universitario Agostino Gemelli in Rome. Principal fields of interest are cardiotoxicity and CAR-T cells.
Giovanna Liuzzo
is MD, PhD, Professor of Cardiology at Catholic University of the Sacred Heart in Rome and head of the cardiovascular science laboratory.
Francesco Burzotta
is MD, Phd and Professor of Cardiology at Catholic University of the Sacred Heart.
Rocco Antonio Montone
is MD, PhD and Cardiologist at IRCSS Fondazione Policlinico Universitario Agostino Gemelli in Rome; fields of interest are pathophysiology of acute myocardial infarction and cardiovascular pharmacotherapy.
Federica Sorà
is Hematologist at IRCSS Fondazione Policlinico Universitario Agostino Gemelli in Rome. Principal fields of interest are Chronic Lymphocytic Leukemia and CAR-T cells therapy.
Simona Sica
is Professor of Hematology at IRCSS Fondazione Policlinico Universitario Agostino Gemelli in Rome. Principal fields of interest are CAR-T cells therapy and hematopoietic stem cell transplantation.
Stefan Hohaus
is Professor of Hematology at IRCSS Fondazione Policlinico Universitario Agostino Gemelli in Rome. Principal fields of interest are CAR-T cells therapy and lymphomas.
Gaetano Antonio Lanza
is MD and Professor of Cardiology at Catholic University of the Sacred Heart, Rome. He is chief of the non-invasive cardiology unit at IRCSS Fondazione Policlinico Universitario Agostino Gemelli in Rome.
Filippo Crea
is MD, Cardiologist and Full Professor of Cardiology at Catholic University of the Sacred Heart, Rome; he is editor-in-chief of European Heart Journal.
Antonella Lombardo
is MD and Professor of Cardiology at Catholic University of the Sacred Heart, Rome. She is chief of the echocardiography unit and cardio-oncology outpatient service at IRCSS Fondazione Policlinico Universitario Agostino Gemelli in Rome.
Giorgio Minotti
is MD and oncologist, Full Professor of Pharmacology and Clinical Pharmacology at the School of Medicine of Campus Bio-Medico University of Rome. His work mostly focuses on pharmacokinetic determinants and clinical correlates of cardiovascular events induced by oncologic therapies.
Author contributions
MC, MV, TF, LM, FB, GC, AB, PL, LT, ADR, GC, EG: idealization, statistical analysis and writing. GL, FB, RAM, FS, SS, SH, GAL, FC: supervision. AL, GM: idealization, writing and supervision. All authors read and approved the final manuscript.
Funding
Not applicable.
Data availability
The datasets used and analysed in this study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Ethics approval was obtained for the present study by Policlinico Universitario Agostino Gemelli IRCSS, Rome (ID6000).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Antonella Lombardo and Giorgio Minotti share senior co-authorship.
References
- 1.Jain T, Bar M, Kansagra AJ, et al. Use of Chimeric Antigen Receptor T Cell Therapy in clinical practice for Relapsed/Refractory aggressive B cell Non-hodgkin Lymphoma: an Expert Panel Opinion from the American Society for Transplantation and Cellular Therapy. Biol Blood Marrow Transpl. 2019;25:2305–21. doi: 10.1016/j.bbmt.2019.08.015. [DOI] [PubMed] [Google Scholar]
- 2.Kansagra AJ, Frey NV, Bar M, et al. Clinical Utilization of Chimeric Antigen Receptor T Cells in B Cell Acute Lymphoblastic Leukemia: An Expert Opinion from the European Society for Blood and Marrow Transplantation and the American Society for Blood and marrow transplantation. Biol Blood Marrow Transpl. 2019;25:e76–85. doi: 10.1016/j.bbmt.2018.12.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tang HKC, Wang B, Tan HX, et al. CAR T-Cell therapy for Cancer: latest updates and challenges, with a focus on B-Lymphoid malignancies and selected solid tumours. Cells. 2023;12:1586. doi: 10.3390/cells12121586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mucha SR, Rajendram P. Management and Prevention of Cellular-Therapy-related toxicity: early and late complications. Curr Oncol. 2023;30:5003–23. doi: 10.3390/curroncol30050378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brudno JN, Kochenderfer JN. Recent advances in CAR T-cell toxicity: mechanisms, manifestations and management. Blood Rev. 2019;34:45–55. doi: 10.1016/j.blre.2018.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lee DW, Gardner R, Porter DL, Louis CU, Ahmed N, Jensen M, Grupp SA, Mackall CL. Current concepts in the diagnosis and management of cytokine release syndrome. Blood. 2014;124(2):188–95. doi: 10.1182/blood-2014-05-552729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shah D, Soper B, Shopland L. Cytokine release syndrome and cancer immunotherapies - historical challenges and promising futures. Front Immunol. 2023;14:1190379. doi: 10.3389/fimmu.2023.1190379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Strati P, Gregory T, Majhail NS, Jain N. Chimeric Antigen receptor T-Cell therapy for hematologic malignancies: a practical review. JCO Oncol Pract. 2023;OP2200819. 10.1200/OP.22.00819. [DOI] [PubMed]
- 9.Marar RI, Abbasi MA, Prathivadhi-Bhayankaram S, et al. Cardiotoxicities of Novel therapies in Hematologic malignancies: chimeric Antigen receptor T-Cell therapy and bispecific T-Cell Engager Therapy. JCO Oncol Pract. 2023;19:331–42. doi: 10.1200/OP.22.00713. [DOI] [PubMed] [Google Scholar]
- 10.Ganatra S, Dani SS, Yang EH, Zaha VG, Nohria A. Cardiotoxicity of T-Cell antineoplastic therapies: JACC: CardioOncology primer. JACC CardioOncol. 2022;4:616–23. doi: 10.1016/j.jaccao.2022.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lefebvre B, Kang Y, Smith AM, Frey NV, Carver JR, Scherrer-Crosbie M. Cardiovascular effects of CAR T Cell Therapy: a retrospective study. JACC CardioOncol. 2020;2(2):193–203. doi: 10.1016/j.jaccao.2020.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Camilli M, Lombardo A, Crea F, Minotti G. Temporal Patterns of Left Ventricular Systolic and Diastolic Metrics Changes in Adult Patients with Hematological Malignancies Treated With Chimeric Antigen Receptor (CAR)-T Cells: Results from the CARdio-Tox Prospective Study. Eur Heart J Cardiovasc Imaging. In press10.1093/ehjci/jead317. [DOI] [PubMed]
- 13.Lyon AR, López-Fernández T, Couch LS, ESC Scientific Document Group. 2022 ESC Guidelines on cardio-oncology developed in collaboration with the European Hematology Association (EHA), the European Society for Therapeutic Radiology and Oncology (ESTRO) and the International Cardio-Oncology Society (IC-OS). Eur Heart J. 2022;43:4229–4361. 10.1093/eurheartj/ehac244. [DOI] [PubMed]
- 14.Lang RM, Badano LP, Mor-Avi V et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015;28:1–39.e14. 10.1016/j.echo.2014.10.003. PMID: 25559473. [DOI] [PubMed]
- 15.Galderisi M, Cosyns B, Edvardsen T et al. 2016–2018 EACVI Scientific Documents Committee; 2016–2018 EACVI Scientific Documents Committee. Standardization of adult transthoracic echocardiography reporting in agreement with recent chamber quantification, diastolic function, and heart valve disease recommendations: an expert consensus document of the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2017;18:1301–1310. 10.1093/ehjci/jex244. PMID: 29045589. [DOI] [PubMed]
- 16.Badano LP, Kolias TJ, Muraru D, et al. Standardization of left atrial, right ventricular, and right atrial deformation imaging using two-dimensional speckle tracking echocardiography: a consensus document of the EACVI/ASE/Industry Task Force to standardize deformation imaging. Eur Heart J Cardiovasc Imaging. 2018;19:591–600. doi: 10.1093/ehjci/jey042. [DOI] [PubMed] [Google Scholar]
- 17.Nagueh SF, Smiseth OA, Appleton CP, et al. Recommendations for the evaluation of left ventricular diastolic function by Echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2016;29:277–314. doi: 10.1016/j.echo.2016.01.011. [DOI] [PubMed] [Google Scholar]
- 18.Vahanian A, Beyersdorf F, Praz F, ESC/EACTS Scientific Document Group et al. 2021 ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J. 2022;43:561–632. doi: 10.1093/eurheartj/ehab395. [DOI] [PubMed] [Google Scholar]
- 19.Camilli M, Iannaccone G, Russo M, et al. Early improvement of strain imaging parameters predicts long-term response to sacubitril/valsartan in patients with heart failure with reduced ejection fraction: an observational prospective study. Int J Cardiol. 2023;131110. 10.1016/j.ijcard.2023.06.001. [DOI] [PubMed]
- 20.Lee DW, Santomasso BD, Locke FL, et al. ASTCT Consensus Grading for Cytokine Release Syndrome and neurologic toxicity Associated with Immune Effector cells. Biol Blood Marrow Transpl. 2019;25:625–38. doi: 10.1016/j.bbmt.2018.12.758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Totzeck M, Anker MS, Rassaf T. CAR T-cell cancer therapies: do not forget the heart. Eur Heart J. 2023;44:2043–5. doi: 10.1093/eurheartj/ehad175. [DOI] [PubMed] [Google Scholar]
- 22.Alvi RM, Frigault MJ, Fradley MG, et al. Cardiovascular events among adults treated with chimeric Antigen receptor T-Cells (CAR-T) J Am Coll Cardiol. 2019;74:3099–108. doi: 10.1016/j.jacc.2019.10.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ganatra S, Redd R, Hayek SS, et al. Chimeric Antigen receptor T-Cell therapy-Associated Cardiomyopathy in patients with refractory or relapsed Non-hodgkin Lymphoma. Circulation. 2020;142:1687–90. doi: 10.1161/CIRCULATIONAHA.120.048100. [DOI] [PubMed] [Google Scholar]
- 24.Lefebvre B, Kang Y, Smith AM, Frey NV, Carver JR, Scherrer-Crosbie M. Cardiovascular effects of CAR T Cell Therapy: a retrospective study. JACC CardioOncol. 2020;2:193–203. doi: 10.1016/j.jaccao.2020.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mahmood SS, Riedell PA, Feldman S, et al. Biomarkers and cardiovascular outcomes in chimeric antigen receptor T-cell therapy recipients. Eur Heart J. 2023;44:2029–42. doi: 10.1093/eurheartj/ehad117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Goldman A, Maor E, Bomze D, et al. Adverse Cardiovascular and pulmonary events Associated with chimeric Antigen receptor T-Cell therapy. J Am Coll Cardiol. 2021;78:1800–13. doi: 10.1016/j.jacc.2021.08.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shalabi H, Sachdev V, Kulshreshtha A, et al. Impact of cytokine release syndrome on cardiac function following CD19 CAR-T cell therapy in children and young adults with hematological malignancies. J Immunother Cancer. 2020;8:e001159. doi: 10.1136/jitc-2020-001159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen F, Teachey DT, Pequignot E, et al. Measuring IL-6 and sIL-6R in serum from patients treated with tocilizumab and/or siltuximab following CAR T cell therapy. J Immunol Methods. 2016;434:1–8. doi: 10.1016/j.jim.2016.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Berman M, Berliner S, Bashouti N, Elkayam O, Ziv-Baran T. Reduced C-reactive protein level at hospital admission in patients treated with Tocilizumab - An attention may be required. Heliyon. 2023;9(6):e16665. doi: 10.1016/j.heliyon.2023.e16665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Guz D, Gafter-Gvili A, Lev N, Sahaf Levin G, Lev S. Tocilizumab Treatment Effect on Iron Homeostasis in severe COVID-19 patients. Acta Haematol. 2022;145(4):440–7. doi: 10.1159/000522307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Azmy V, Kaman K, Tang D, et al. Cytokine profiles before and after Immune Modulation in Hospitalized patients with COVID-19. J Clin Immunol. 2021;41(4):738–47. doi: 10.1007/s10875-020-00949-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Knovich MA, Storey JA, Coffman LG, Torti SV, Torti FM. Ferritin for the clinician. Blood Rev. 2009;23(3):95–104. doi: 10.1016/j.blre.2008.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Vilar R, Fish RJ, Casini A, Neerman-Arbez M. Fibrin(ogen) in human disease: both friend and foe. Haematologica. 2020;105(2):284–96. doi: 10.3324/haematol.2019.236901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Camilli M, Maggio L, Tinti L, et al. Chimeric antigen receptor-T cell therapy-related cardiotoxicity in adults and children cancer patients: a clinical appraisal. Front Cardiovasc Med. 2023;10:1090103. doi: 10.3389/fcvm.2023.1090103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Coglianese EE, Larson MG, Vasan RS, et al. Distribution and clinical correlates of the interleukin receptor family member soluble ST2 in the Framingham Heart Study. Clin Chem. 2012;58:1673–81. doi: 10.1373/clinchem.2012.192153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lee DH, Chandrasekhar S, Jain MD, et al. Cardiac and inflammatory biomarker differences in adverse cardiac events after chimeric antigen receptor T-Cell therapy: an exploratory study. Cardiooncology. 2023;9:18. doi: 10.1186/s40959-023-00170-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and analysed in this study are available from the corresponding author on reasonable request.