Abstract
Introduction
Sedentary behavior (including prolonged sitting) is a form of physical inactivity that has a negative impact on health, possibly including musculoskeletal complaints (MSCs). The purpose of this study was to determine the extent to which time spent sitting at work is associated with the one-year prevalence of MSCs in the neck, shoulder, upper back/thoracic spine, and lower back among workers from the Study of Mental Health in the Workplace (S-MGA). In addition, the study also examined whether leisure time, physical activity, and sex modify the relationship between occupational sitting and MSCs.
Methods
For this analysis, we used the S-MGA, a 5-year prospective study in Germany. The S-MGA is a nationwide representative employee cohort study with a baseline survey in 2012 and a follow-up survey in 2017. Sitting at work was measured using a question asked at baseline. The Nordic Musculoskeletal Questionnaire was used to determine the one-year prevalence of MSCs in the neck, shoulder, upper back, and lower back pain (yes/no). The assessment of MSCs was only conducted at the 2017 follow-up. Adjusted Poisson regression models were used to determine the association of baseline level of weekly hours spent sitting at work with MSCs during follow-up. In addition to unadjusted models, models were adjusted for demographic (age, sex, body mass index and occupational skill level), occupational (heavy lifting at work), psychological disorders and lifestyle factors (smoking status and leisure time physical activity), as well as preexisting musculoskeletal conditions reported at baseline. To examine whether the relationship between sitting time and pain was modified by sex and leisure time physical activity, the models were stratified for both these variables.
Results
Among the participants analyzed (n = 2,082), 49.8% were male, while 50.2% were female, and more than 60% of the study population spent over half of their working hours in a sitting position. Exposure to increased sitting at work reported at baseline was not consistently associated with 12-month prevalence of MSCs in the upper body at follow-up. However, differences in the association between occupational sitting and MSCs were dependent on the intensity of leisure time physical activity. Prevalence ratios (PRs) indicated an increased prevalence of MSC in the neck (PR = 1.46; 95% CI = 1.18–1.80) and shoulder (PR = 1.30; 95% CI = 1.03–1.64) in workers without leisure time physical activity who spent 25 to < 35 weekly working hours sitting.
Discussion
These findings suggest that leisure time physical activity interacts with the relationship between sitting at work and MSCs. The relationship between sitting at work and musculoskeletal pain needs further investigation, but we found indications that leisure time physical activity may counter the effects of sitting at work.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12995-024-00408-7.
Keywords: Occupational sitting, Longitudinal studies, Musculoskeletal, Pain, Physical work, Sedentary
Introduction
In industrially developed countries, musculoskeletal disorders are a leading cause of disability and incur high costs [1–3]. Work-related musculoskeletal disorders are defined as damage or diseases of muscles, nerves, tendons, joints, and cartilage or intervertebral discs due to risk factors in the work environment [4]. Work-related musculoskeletal disorders and complaints, such as neck and low back pain, remain frequent and are also a common cause of work disability [2, 5–7]. Musculoskeletal complaints (MSCs) have also been identified by the International Labor Organization (ILO) and the World Health Organization (WHO) as an occupational epidemic [8]. While heavy physical workload is known to increase the risk of developing MSCs [9, 10], prolonged sitting has also been suggested as a potential risk factor for work-related musculoskeletal disorders [11].
Sitting occupies a significant portion of our daily waking time. Globally, adults spend an average of 6.4 h per day sitting, and studies with objective measurements have shown that 50% of the European population sits more than 6 h per day [10–12]. Epidemiologic studies suggest that higher levels of sedentary work could be associated with several musculoskeletal conditions, including back and neck/shoulder pain [12]. For example, Celik et al. [13] found that among office workers, prolonged sitting at a desk, poor ergonomic working conditions/body position, work stress and lack of regular exercise were associated with lower back, upper back, shoulder, neck, arm or foot pain. However, studies examining the association between sitting time and neck and shoulder symptoms in office workers are inconsistent [12, 14–16]. Some cross-sectional studies have documented a positive association between occupational sitting and neck/shoulder pain and low back pain [17, 18]. However, longitudinal studies are sparse and show conflicting results [15, 19]. Thus, systematic reviews of longitudinal cohort and case-control studies find no association between sedentary time and the prevalence of musculoskeletal disorders [20–25]. Regarding musculoskeletal pain, systematic reviews report either positive [20, 26] or negative [27] associations between sitting time and musculoskeletal pain intensity. On the other hand, a dose-response relationship between the number of hours worked at a computer workstation and the risk of MSCs, particularly shoulder/neck, back, and upper limb pain and symptoms, has been reported by systematic reviews [28, 29].
The conflicting results may in part reflect inherent challenges in studying the association between sitting at work and MSCs. That is, well-established work-related risk-factors for MSCs, such as awkward body postures and heavy lifting at work [30] are likely to be negatively associated with sedentary work. Also, Sattar and Preiss [31] report that causality between sedentary behavior and MSCs is difficult to establish because pain and chronic disease may predispose to excessive sedentary behavior. The mixed results described above may also be due to a compensating effect of leisure time physical activities. There are studies indicating that workers with higher occupational sitting time sit less in their leisure time, i.e., workers with mostly sitting jobs were significantly more likely to be active during their leisure time than workers with more active jobs [32, 33]. Further complicating things, engaging in both a low and a high level of physical activity was associated with an increase of low back pain in a cross-sectional analysis [34]. Therefore, it seems important to consider leisure time physical activity when assessing the association between occupational sitting and MSCs.
The aim of the present study was to investigate the association between sedentary time at work and the one-year prevalence of MSCs using from the first two waves of the Study of Mental Health at Work (S-MGA). The S-MGA is prospective study of workers from across Germany designed to examine the connection between working conditions, mental health and functional ability in 5-year intervals [35]. We hypothesize that the increasing duration of sedentary behavior at work is associated with the prevalence of MSCs at follow-up, and that this relationship is modified by sex as well as leisure time physical activity.
Materials and methods
Study population
The data used in this study is from S-MGA, a nationally representative employee cohort study with a baseline survey in 2012 and a follow-up survey in 2017. The baseline measurements conducted in 2012 included questions about work experiences, health-related behaviors, and health status, and the follow-up survey in 2017 used the same internationally established instruments as the baseline survey [35].
The S-MGA sampling was based on the German Integrated Employment Biographies (IEB), which combines data from various sources of the German Federal Employment Agency [36]. The IEB captures employees subject to social security contributions in Germany, which accounted for more than 80% of all employees in Germany on the sampling date (December 31, 2010) [37]. The S-MGA used a two-stage cluster sampling procedure, with a random selection of 206 municipalities in the first stage and a random selection of individuals within municipalities in the second stage. At the outset (year 2012), the target population was defined as all employees subject to social security contributions in Germany born between 1951 and 1980. Civil servants, the self-employed and freelancers are not subject to social security contributions and were not included in the study [35].
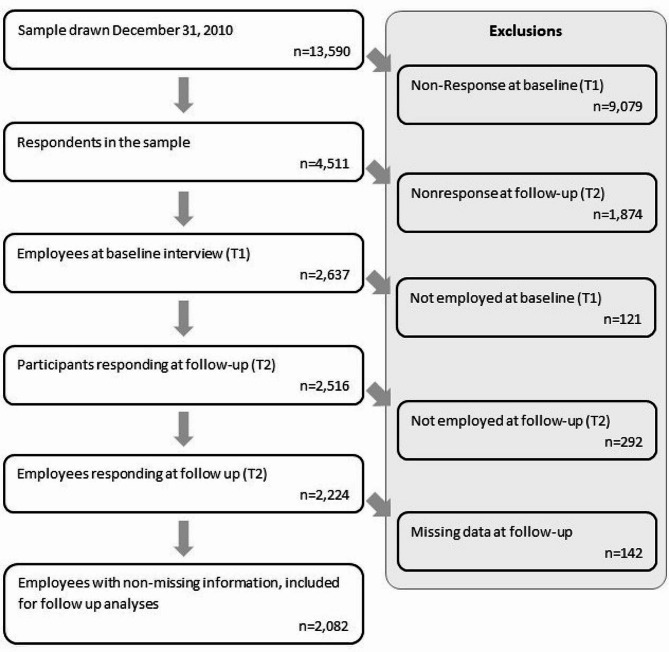
A total of 13,590 individuals were randomly selected and then sent a letter with information on the study about a week prior to the first attempt at an in-person interview [35]. Of the 4,511 respondents who took part at baseline (response: 33%), 2,637 also took part in the follow-up interviews (follow-up: 58%) (Fig. 1). Of these, 2,224 were employed at baseline and follow-up. The study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the ethics committee of the German Federal Institute for Occupational Safety and Health [38]. All information was obtained through computer-assisted personal interviews at the respondents’ home and all participants gave informed consent to participate in the study prior to enrollment [35].
Fig. 1.
Flow of participation in S-MGA
For this analysis, we conducted a complete case analysis and excluded 142 participants with missing information on sex, age, occupational skill level, smoking, musculoskeletal diseases, leisure time physical activity, psychological conditions, working hours per week, sitting, and lifting at the workplace, and body mass index (BMI), or MSCs symptoms (neck, shoulder, upper back, and lower back) at follow-up. Included in the number of excluded participants with missing information were two persons reporting more than 90 working hours per week and 86 persons reporting highly fluctuating or irregular working hours. Application of these exclusion criteria resulted in a final sample of 2,082 participants.
The data of the first two waves of the S-MGA are available as a Scientific Use File (SUF) for scientific research projects. Access was provided by the Research Data Center of the Federal Institute for Occupational Safety and Health (FDZ-BAuA) [39].
Variables
Outcome
To determine which body regions were affected by musculoskeletal symptoms in the 12-months preceding the survey, an adaptation of the Nordic Musculoskeletal Questionnaire was used [40]. The questions cover nine body regions (neck, shoulder, elbow, wrists/hands, upper back/thoracic spine, lower back (low back), hips/thighs, knees, ankles/feet) and ask: “Have you had any discomfort or pain in the following areas of your body at any time during the past 12 months?” with two response categories “yes/no”. These questions were only asked at the follow-up in 2017. The current study focused on the four upper-body regions as the dependent variables, namely, the neck, shoulders, upper back, and lower back. Studies show that upper extremities are often associated with MSC in office workers [29, 41]. The outcome in this study was the presence of MSCs in any of these four body regions during the last 12 months prior to the follow-up [40].
Independent variables
All independent variables used were collected at the baseline survey.
Occupational sitting
In the questionnaire, sitting at work was measured with a scale adapted from the BiBB/BAuA employment study [42]: “How often do you have to sit at work?” with answer choices of “never”, “up to 1/4 of the time”, “up to half of the time”, “up to 3/4 of the time”, “more than three quarters (almost all of the time)”. The assessment was performed at both baseline and at the 5-year follow-up. Only the baseline occupational sitting was considered. This information was combined with weekly working hours to obtain categories of the hours spent sitting at work per week. Weekly working time was collected with the following two questions: “How many hours a week do you normally work, including regular overtime, overtime, etc.?” and for people with a second job(s) “How many hours do you usually work there each week?”. All participants reported the sum of time (hours, minutes) they spent sitting at work on a usual working week. The hours worked were multiplied by the proportion of time spent sitting at work. Proportions equidistant from the upper and lower limits of each category, using 100% as the upper limit of the highest category were used (e.g., 0 for never and 12.5% for the category “up to 1/4 of the time”). Finally, the weekly sitting time at work were categorized as, “under 5 hours/week “, “5 to < 15 hours/week “, “15 to < 25 hours/week”, “25 to < 35 hours/week” “35 or more hours/week”.
Covariates
Individual factors were chosen a priori as potential confounders based on previous literature and theoretical assumptions concerning their possible influence on sitting behaviors and MSCs. Numerous studies have shown that working long hours increases the risk of pain or discomfort in the back, knees, hips, feet, hands, arms, neck and shoulders [43]. Sitting time at work also increases with working hours [18]. Therefore, to account for the fact that occupational sitting time is increased with increased working time, “working hours per week” was integrated into the exposure variable.
There are studies indicating a relationship between workplace sitting and age, sex [44], occupational skill level [45], working hours [46], BMI [47], smoking [18], musculoskeletal diseases [48], psychological disorders and leisure time physical activity [20, 49]. There are also studies indicating a causal relationship between MSCs and the above-mentioned factors [50–54], making them likely confounders. The DAGitty tool was used to evaluate potential confounders using directed acyclic graphs (DAG) [55]. Based on the DAGs (online supplement), we adjusted for the baseline values of age, sex, occupational level, BMI, smoking, musculoskeletal diseases, psychological disorders, lifting/carrying heavy loads at work and leisure time physical activity.
Lifting and carrying at work was assessed with a question based on a question used in the BiBB/BAuA employment study: “Lifting and/or carrying heavy loads (women more than 10 kg/ men more than 20 kg), with the answer categories “never”, “up to 1/4 of the time”, “up to half of the time”, “up to 3/4 of the time”, “more than three quarters (almost all of the time)” [42]. We adjusted for lifting and carrying because physical work done in combination with periods of sitting may be more strongly associated with MSCs. Thus, we used the variable for lifting/carrying as a proxy for more physical work.
The presence of musculoskeletal diseases at baseline was assessed using a question from the Work Ability Index (WAI): “Has a doctor ever diagnosed you with any of the diseases or health conditions listed here?” with two response categories (‘yes’ or ‘no’) [56]. A list of medical conditions including “musculoskeletal diseases of the back, limbs or other parts of the body (e.g. repeated pain in joints or muscles, sciatica, rheumatism, spinal disorders)” was shown during the personal interviews.
For sex, participants had the option of assigning themselves to “female” or “male”. Age (years) at baseline was categorized by birth year as follows: 1951-55, 1956-60, 1961-65, 1966-70, 1971-75, 1976-80. BMI was calculated using self-reported weight (kg) and height (cm) and categorized into underweight (< 18.5 kg/m2), normal weight (18.5–24.9 kg/m2), overweight (25.0–29.9 kg/m2), and obesity (≥ 30.0 kg/m2) [57, 58].
Smoking status was asked with the response options “never”, “used to smoke”, “stopped in the last twelve months”, “occasionally”, and “daily”.
Occupational skill level of work was operationalized via the respondents’ occupations, which were coded manually according to the International Standard Classification of Occupations (ISCO 08) and categorized into four groups based on skill levels: unskilled workers, skilled workers, semi-professionals, academics/managers [59].
Psychological disorders (i.e., depression, anxiety, chronic insomnia, burnout) were assessed with the above mentioned list of the WAI questionnaire used to assess musculoskeletal diseases [56]. This list also included an item for “Psychological disorders (e.g. depression, anxiety, chronic insomnia, burnout syndrome)”.
Based on the 2020 WHO guidelines on physical activity and sedentary behavior, all adults should undertake regular physical activity. Adults should do at least 150–300 min of moderate-intensity aerobic physical activity, or at least 75–150 min of vigorous-intensity aerobic physical activity, or an equivalent combination of moderate-intensity and vigorous-intensity activity throughout the week for substantial health benefits. Adults should also do muscle-strengthening activities at moderate or greater intensity that involve all major muscle groups on two or more days a week, as these provide additional health benefits [60]. In this study, we examined a single item on leisure time physical activity: “How often do you practice in activities involving more physical exertion: e.g., heavy gardening in your free time?”. The response options were “(almost) daily”, “several times a week”, “once a week”, “less often”, “never”. These variables were measured via self-reported questionnaires at baseline. We combined responses for physical activity to obtain three categories:
mostly/all of the time = “(almost) daily” and “several times a week”,
some/little of the time = “once a week” and “less often”, and
none of the time = “never”.
Statistical analyses
Descriptive statistical procedures were performed, and inferential analysis of associations were conducted with regression analyses. Descriptive data are presented as mean and standard deviation (SD), or as frequency and percentage, where appropriate. The methods and measurement tools used are described in detail below.
Robust Poisson regression models were calculated to answer the research questions with prevalence ratios (PR) and 95% confidence intervals (95% CI). In the regression models, weekly sitting hours at work was used as the primary independent variable, with “under 5 hours/week” as the reference category. The presence of each MSC in one of the four regions of the MSCs at follow-up were the dependent variables (outcomes) and were treated separately for each outcome as binomial variables (yes/no) in all models.
Three adjustment sets were used:
Model 1: unadjusted model.
Model 2: an adjustment set of Model 1 with independent variables age, sex, and occupational skill level.
Model 3: an adjustment set of Model 2 with BMI, smoking, musculoskeletal diseases at baseline, psychological disorders, lifting/carrying heavy loads at work and leisure time physical activity.
Three different models were conducted in this study; however, the main focus is the fully adjusted model (Model 3), which will be comprehensively presented in the results and discussion.
To test whether sex and leisure time physical activity modifies the effect of occupational sitting on MSCs, two two-way interaction terms (occupational sitting × sex and occupational sitting × leisure time physical activity) were included in the adjusted models. The difference in the model-fit of models with or without the two-way interaction term were tested to determine if the interaction made a statistically significant improvement to the model-fit. This would indicate effect modification. Additionally, to determine whether sex and leisure time physical activity modify the effects of prolonged sitting on MSCs risk, stratification of these models for sex (women or men) and leisure time physical activity (mostly/always, little/sometime, or never) were also performed.
The significance level was set at α = 0.05 and statistical analysis was performed syntax-based using Stata 14 [61].
Results
Among the participants, 1036 individuals (49.8%) were male, while 1046 (50.2%) were female. The proportion of age and musculoskeletal system disease was similar between men and women. The mean working hours per week was recorded as 43.1 (SD 9.0) hours in men and 31.8 (SD 13.2) hours per week in women. Sex-related variations were evident when examining the percentage of participants meeting the WHO definition for being overweight, with 55.0% of men exceeding this threshold compared to 30.7% of women. Similarly, the prevalence of obesity among participants also exhibited sex disparities, with 19.7% of men surpassing the WHO-defined threshold as opposed to 15.6% of women.
Among both men and women participants, skilled workers accounted for 44.4% of men and 35.9% of women. Regarding psychological disorders (e.g., depression, anxiety, chronic insomnia, burnout), the minority of participants (9.2% of men and 18.0% of women) reported diagnoses at baseline. A total of 61.9% of men and 50.2% of women reported infrequent leisure time physical activity with greater physical exertion, some while approximately 9.2% of men and 5.7% of women reported leisure time physical activity with greater physical exertion more than once a week.
In terms of workplace-related factors, a considerable proportion of the sample (83.2%) reported being exposed to sitting during work. Male employees were more likely to have load lifting during working time than female employees.
In general, the proportion of MSCs (neck, shoulders, and upper back) in women was greater than that in men (64.4%, 57.7% and 35.8%, respectively). The proportion of complaint of lower back was similar between men and women (56.1% and 57.0%). These and further population characteristics are shown in Table 1.
Table 1.
Characteristics of the sample of male and female employees
| Characteristics | No. participants n (%) | Male n (%) | Female n (%) |
|---|---|---|---|
| Total | n = 2082 | n = 1036 | n = 1046 |
| Age (years) | |||
| 31–35 | 193 (9.3) | 108 (10.4) | 85 (8.1) |
| 36–40 | 310 (14.9) | 153 (14.8) | 157 (15.0) |
| 41–45 | 449 (21.6) | 221 (21.3) | 228 (21.8) |
| 46–50 | 491 (23.6) | 240 (23.2) | 251 (24.0) |
| 51–55 | 421 (20.2) | 206 (19.9) | 215 (20.6) |
| 56–60 | 218 (10.4) | 108 (10.4) | 110 (10.5) |
| BMI | |||
| Underweight - BMI under 18.5 kg/m² | 25 (1.2) | 2 (0.2) | 23 (2.2) |
| Normal weight - BMI greater than or equal to 18.5 to 24.9 kg/m² | 799 (38.4) | 260 (25.1) | 539 (51.5) |
| Overweight - BMI greater than or equal to 25 to 29.9 kg/m² | 891 (42.8) | 570 (55.0) | 321 (30.7) |
| Obesity - BMI greater than or equal to 30 kg/m² | 367 (17.6) | 204 (19.7) | 163 (15.6) |
| Occupational level | |||
| unskilled workers | 121 (5.8) | 39 (3.8) | 82 (7.8) |
| skilled workers | 835 (40.1) | 460 (44.4) | 375 (35.9) |
| semi-professionals | 580 (27.9) | 235 (22.7) | 345 (32.9) |
| academics/managers | 546 (26.2) | 302 (29.1) | 244 (23.3) |
| Psychological conditions | |||
| Yes | 283 (13.6) | 95 (9.2) | 188 (18.0) |
| No | 1799 (86.4) | 941 (90.8) | 858 (82.0) |
| Leisure time physical activity | |||
| mostly/all the time | 155 (7.4) | 95 (9.2) | 60 (5.7) |
| some/little of the time | 1166 (56.0) | 641 (61.9) | 525 (50.2) |
| None of the time | 761 (36.6) | 300 (29.0) | 441 (44.1) |
| Smoking | |||
| Never | 852 (40.9) | 390 (37.6) | 462 (44.2) |
| In the past | 622 (29.9) | 337 (32.5) | 285 (27.3) |
| Stopped in the last 12 months | 37 (1.8) | 24 (2.3) | 13 (1.2) |
| Sometimes | 134 (6.4) | 66 (6.4) | 68 (6.5) |
| Every day | 437 (20.99) | 219 (21.1) | 218 (20.8) |
| Musculoskeletal disease | |||
| Yes | 1,141 (54.8) | 572 (55.2) | 569 (54.4) |
| No | 941 (45.2) | 464 (44.8) | 477 (45.6) |
| Sitting at work | |||
| Never | 350 (16.8) | 182 (17.6) | 168 (16.1) |
| up to ¼ of the time | 422 (20.3) | 204 (19.7) | 218 (20.8) |
| up to ½ of the time | 344 (16.5) | 177 (17.1) | 167 (16.0) |
| up to ¾ of the time | 346 (16.6) | 173 (29.0) | 173 (16.5) |
| more than ¾ the time, almost always | 620 (29.8) | 300 (29.0) | 320 (30.6) |
| Sitting at work (hours/week) | |||
| Under 5 h/week | 570 (27.4) | 243 (23.5) | 327 (31.3) |
| 5 to < 15 h/week | 557 (20.4) | 194 (18.7) | 231 (22.1) |
| 15 to < 25 h/week | 365 (17.5) | 161 (15.5) | 204 (19.5) |
| 25 to < 35 h/week | 334 (16.0) | 171 (16.5) | 163 (15.6) |
| 35 or more hours/week | 388 (18.6) | 267 (25.8) | 121 (11.6) |
| Heavy lifting at workplace | |||
| never | 1,165 (56.0) | 551 (53.2) | 614 (58.7) |
| up to ¼ of the time | 593 (28.5) | 314 (30.3) | 279 (26.7) |
| up to ½ of the time | 171 (8.2) | 94 (9.1) | 77 (7.4) |
| up to ¾ of the time | 64 (3.1) | 27 (2.6) | 37 (3.5) |
| more than ¾ the time, almost always | 89 (4.3) | 50 (4.8) | 39 (3.7) |
working hours per week (
 , SD)
, SD)
|
37.4 (12.6) | 43.1 (9.0) | 31.8 (13.2) |
| Musculoskeletal symptoms at follow-up, in 2017 | |||
| Neck | |||
| Yes | 1137 (54.6) | 463 (44.7) | 674 (64.4) |
| No | 945 (45.4) | 573 (55.3) | 372 (35.6) |
| Shoulders | |||
| Yes | 1102 (52.9) | 498 (48.1) | 604 (57.7) |
| No | 980 (47.1) | 538 (51.9) | 442 (42.3) |
| Upper back | |||
| Yes | 635 (30.5) | 261 (25.2) | 374 (35.8) |
| No | 1447 (69.5) | 775 (74.8) | 672 (64.2) |
| Lower back | |||
| Yes | 1177 (56.5) | 581 (56.1) | 596 (57.0) |
| No | 905 (43.5) | 455 (43.9) | 450 (43.0) |
n: number;  : mean; SD: standard deviation
: mean; SD: standard deviation
Associations between sitting at work and MSCs
Table 2 shows the association of all four regions of the musculoskeletal system at follow-up and baseline sitting at work. Increased weekly sitting times at work at baseline were rarely statistically significantly associated with MSCs at follow-up among the total population. PRs for the 12-month prevalence of neck, shoulder and lower back complaints were lower in highest sitting categories (model 3) compared with the moderate sitting categories, which may either suggest an inverse U-shaped relationship between sitting at work and neck and lower back pain or is an indication of selection bias (e.g., healthy worker effect).
Table 2.
Associations between baseline workplace sitting in 2012 and complaints of neck, shoulder, upper back, and lower back pain in the last 12 months in 2017 (yes/no) among 2,082 employees aged 31–60 years in Germany. Poisson regressions. Prevalence Ratios (PR).
| Exposure | 12-month prevalence of complaints in different regions of the musculoskeletal system at follow-up | |||||||
|---|---|---|---|---|---|---|---|---|
| Occupational sitting 2012 | Neck n = 1137 | Shoulder n = 1102 | Upper back n = 635 | Lower back n = 1177 | ||||
| PR | 95% CI | PR | 95% CI | PR | 95% CI | PR | 95% CI | |
| Model 1 | ||||||||
| Under 5 h/week | 1 | (Ref) | 1 | (Ref) | 1 | (Ref) | 1 | (Ref) |
| 5 to < 15 h/week | 0.99 | 0.88–1.11 | 0.98 | 0.88–1.10 | 0.99 | 0.82–1.18 | 0.95 | 0.85–1.05 |
| 15 to < 25 h/week | 1.08 | 0.96–1.20 | 0.95 | 0.84–1.07 | 1.02 | 0.85–1.22 | 0.98 | 0.88–1.10 |
| 25 to < 35 h/week | 1.11 | 0.99–1.24 | 0.92 | 0.81–1.04 | 0.90 | 0.74–1.11 | 0.91 | 0.81–1.02 |
| 35 or more hours/week | 0.95 | 0.84–1.08 | 0.87 | 0.76–0.99 | 0.73 | 0.59–0.91 | 0.83 | 0.74–0.94 |
| Model 2 | ||||||||
| Under 5 h/week | 1 | (Ref) | 1 | (Ref) | 1 | (Ref) | 1 | (Ref) |
| 5 to < 15 h/week | 0.98 | 0.87–1.10 | 0.98 | 0.87–1.10 | 1.02 | 0.84–1.22 | 0.98 | 0.88–1.09 |
| 15 to < 25 h/week | 1.07 | 0.95–1.20 | 0.95 | 0.84–1.07 | 1.07 | 0.88–1.29 | 1.04 | 0.93–1.17 |
| 25 to < 35 h/week | 1.10 | 0.97–1.24 | 0.92 | 0.81–1.06 | 0.96 | 0.77–1.19 | 0.97 | 0.86–1.11 |
| 35 or more hours/week | 0.95 | 0.83–1.09 | 0.88 | 0.76–1.01 | 0.78 | 0.62–0.99 | 0.90 | 0.79–1.03 |
| Model 3 | ||||||||
| Under 5 h/week | 1 | (Ref) | 1 | (Ref) | 1 | (Ref) | 1 | (Ref) |
| 5 to < 15 h/week | 1.01 | 0.90–1.13 | 1.03 | 0.92–1.15 | 1.10 | 0.92–1.32 | 1.02 | 0.92–1.14 |
| 15 to < 25 h/week | 1.11 | 0.98–1.25 | 1.03 | 0.91–1.17 | 1.21 | 0.99–1.48 | 1.13 | 1.01–1.27 |
| 25 to < 35 h/week | 1.14 | 1.00-1.31 | 1.02 | 0.88–1.17 | 1.11 | 0.88–1.39 | 1.09 | 0.95–1.24 |
| 35 or more hours/week | 0.99 | 0.86–1.15 | 0.97 | 0.84–1.13 | 0.92 | 0.72–1.18 | 1.01 | 0.88–1.16 |
Model 1: unadjusted
Model 2: adjusted for sex, age, and occupational level
Model 3: adjusted for the covariates in model 2 and BMI, smoking, musculoskeletal diseases at baseline, psychological disorders, lifting/carrying heavy loads at work and leisure time physical activity
PR: prevalence ratio, Ref: reference category
Regression analyses stratified by sex
Interaction tests revealed that sex did not significantly modify the associations between occupational sitting and MSCs (p > 0.05). However, stratifying by categories of sex showed mixed findings. The fully adjusted regression analyses of occupational sitting times at baseline and MSCs at follow-up (model 3) stratified by sex are shown in Tables 3 and 4, using “under 5 hours/week” of sitting at work as the reference category.
Table 3.
Associations between baseline workplace sitting in 2012 and complaints of neck and shoulder pain in the last 12 months in 2017 (yes/no) stratified by sex to baseline among 2,082 employees aged 31–60 years in Germany. Poisson regressions. Prevalence Ration (PR).
| Exposure | Strata defined by sex prior to baseline | |||||||
|---|---|---|---|---|---|---|---|---|
| Occupational sitting 2012 | Neck, n = 1137 | Shoulder, n = 1102 | ||||||
| Men | Women | Men | Women | |||||
| PR | 95% CI | PR | 95% CI | PR | 95% CI | PR | 95% CI | |
| Model 3 | ||||||||
| Under 5 h/week | 1 | (Ref) | 1 | (Ref) | 1 | (Ref) | 1 | (Ref) |
| 5 to < 15 h/week | 0.84 | 0.67–1.06 | 1.12 | 0.98–1.27 | 0.99 | 0.83–1.19 | 1.05 | 0.90–1.21 |
| 15 to < 25 h/week | 1.12 | 0.89–1.42 | 1.10 | 0.96–1.26 | 0.99 | 0.79–1.23 | 1.05 | 0.89–1.22 |
| 25 to < 35 h/week | 1.26 | 1.00-1.60 | 1.06 | 0.91–1.24 | 1.00 | 0.80–1.26 | 1.01 | 0.84–1.22 |
| 35 or more hours/week | 1.02 | 0.79–1.30 | 0.97 | 0.81–1.16 | 0.93 | 0.74–1.17 | 1.01 | 0.83–1.23 |
Model 3: adjusted for age, occupational level, BMI, smoking, musculoskeletal diseases at baseline, psychological disorders, lifting/carrying heavy loads at work and leisure time physical activity
PR: prevalence ratio, Ref: reference category
Table 4.
Associations between baseline workplace sitting in 2012 and complaint of upper back and the lower back in the last 12 months in 2017 (yes/no) stratified by sex to baseline among 2,082 employees aged 31–60 years in Germany. Poisson regressions. Prevalence Ratios (PR).
| Exposure | Strata defined by sex prior to baseline | |||||||
|---|---|---|---|---|---|---|---|---|
| Occupational sitting 2012 | Upper back, n = 635 | Lower back, n = 1177 | ||||||
| Men | Women | Men | Women | |||||
| PR | 95% CI | PR | 95% CI | PR | 95% CI | PR | 95% CI | |
| Model 3 | ||||||||
| Under 5 h/week | 1 | (Ref) | 1 | (Ref) | 1 | (Ref) | 1 | (Ref) |
| 5 to < 15 h/week | 1.20 | 0.88–1.63 | 1.07 | 0.85–1.35 | 1.04 | 0.89–1.21 | 1.01 | 0.87–1.18 |
| 15 to < 25 h/week | 1.15 | 0.79–1.66 | 1.25 | 0.99–1.59 | 1.13 | 0.95–1.34 | 1.13 | 0.97–1.32 |
| 25 to < 35 h/week | 1.20 | 0.81–1.77 | 1.05 | 0.79–1.40 | 1.03 | 0.84–1.26 | 1.15 | 0.96–1.38 |
| 35 or more hours/week | 1.08 | 0.74–1.59 | 0.75 | 0.52–1.07 | 1.00 | 0.83–1.21 | 1.03 | 0.84–1.27 |
Model 3: adjusted for age, occupational level, BMI, smoking, musculoskeletal diseases at baseline, psychological disorders, lifting/carrying heavy loads at work and leisure time physical activity
PR: prevalence ratio, Ref: reference category
The results of the stratified analyses by sex demonstrated no discernible differences in the direction of the associations between occupational sitting at baseline and MSCs among men and women at follow up (Tables 3 and 4). We found indications of a difference between male and female workers for neck complaints at follow-up and between 25 and < 35 h/week of sitting at work, with men showing an increased prevalence of neck complaints that we did not observe for women. For shoulder complaints, no clear associations or patterns were observed for men or women (Table 3). However, there are differences in the peak PRs for the 12-month prevalence of upper back complaints between both women and men (Table 4). It is noteworthy that statistically significant PRs were not identified in any of the groups.
Leisure time physical activity stratification
Interaction tests revealed that leisure time physical activity did not significantly modify the associations between occupational sitting and MSCs (p > 0.05). However, stratifying by categories of physical activity showed mixed findings. The results from the regression analyses stratified by leisure time physical activity (models 1–3) are shown in Tables 5, 6, 7 and 8. For complaints of pain in the neck and shoulders, different frequencies of leisure time physical activity influenced the effect of sitting at work (Tables 5, 6, 7 and 8).
Table 5.
Associations between baseline workplace sitting in 2012 and neck complaints in the last 12 months in 2017 (yes/no) stratified by leisure time physical activity to baseline among 2,082 employees aged 31–60 years in Germany. Poisson regressions. Prevalence Ratios (PR).
| Exposure | Strata defined by leisure time physical activity prior to baseline | |||||
|---|---|---|---|---|---|---|
| Neck, n = 1137 | ||||||
| Occupational sitting 2012 | none of the time | little/some of the time | mostly/all the time | |||
| PR | 95% CI | PR | 95% CI | PR | 95% CI | |
| Model 3 | ||||||
| Under 5 h/week | 1 | (Ref) | 1 | (Ref) | 1 | (Ref) |
| 5 to < 15 h/week | 1.23 | 1.03–1.47 | 0.93 | 0.79–1.10 | 0.68 | 0.44–1.03 |
| 15 to < 25 h/week | 1.17 | 0.96–1.43 | 1.10 | 0.93–1.30 | 0.97 | 0.65–1.45 |
| 25 to < 35 h/week | 1.46 | 1.18–1.80 | 1.05 | 0.88–1.26 | 0.83 | 0.49–1.41 |
| 35 or more hours/week | 1.20 | 0.96–1.49 | 0.90 | 0.74–1.10 | 0.66 | 0.30–1.43 |
Model 3: adjusted for sex, age, occupational level, BMI, smoking, musculoskeletal diseases at baseline, psychological disorders and lifting/carrying heavy loads at work
PR: prevalence ratio, Ref: reference category
Table 6.
Associations between baseline workplace sitting in 2012 and shoulder complaints in the last 12 months in 2017 (yes/no) stratified by leisure time physical activity to baseline among 2,082 employees aged 31–60 years in Germany. Poisson regressions. Prevalence Ratios (PR)
| Exposure | Strata defined by leisure time physical activity prior to baseline | |||||
|---|---|---|---|---|---|---|
| Shoulder, n = 1102 | ||||||
| Occupational sitting 2012 | none of the time | little/some of the time | mostly/all the time | |||
| PR | 95% CI | PR | 95% CI | PR | 95% CI | |
| Model 3 | ||||||
| Under 5 h/week | 1 | (Ref) | 1 | (Ref) | 1 | (Ref) |
| 5 to < 15 h/week | 1.12 | 0.94–1.34 | 1.02 | 0.87–1.21 | 0.75 | 0.54–1.05 |
| 15 to < 25 h/week | 1.12 | 0.91–1.38 | 1.05 | 0.88–1.26 | 0.69 | 0.46–1.02 |
| 25 to < 35 h/week | 1.30 | 1.03–1.64 | 0.95 | 0.77–1.16 | 0.73 | 0.45–1.19 |
| 35 or more hours/week | 1.12 | 0.90–1.41 | 0.94 | 0.77–1.16 | 0.58 | 0.27–1.22 |
Model 3: adjusted for the sex, age, occupational level, BMI, smoking, musculoskeletal diseases at baseline, psychological disorders and lifting/carrying heavy loads at work
PR: prevalence ratio, Ref: reference category
Table 7.
Associations between baseline workplace sitting in 2012 and upper back complaints in the last 12 months in 2017 (yes/no) stratified by leisure time physical activity to baseline among 2,082 employees aged 31–60 years in Germany. Poisson regressions. Prevalence Rations (PR).
| Exposure | Strata defined by leisure time physical activity prior to baseline | |||||
|---|---|---|---|---|---|---|
| Upper back, n = 635 | ||||||
| Occupational sitting 2012 | none of the time | little/some of the time | mostly/all the time | |||
| PR | 95% CI | PR | 95% CI | PR | 95% CI | |
| Model 3 | ||||||
| Under 5 h/week | 1 | (Ref) | 1 | (Ref) | 1 | (Ref) |
| 5 to < 15 h/week | 1.24 | 0.92–1.66 | 1.11 | 0.85–1.44 | 0.70 | 0.37–1.32 |
| 15 to < 25 h/week | 1.25 | 0.88–1.76 | 1.28 | 0.97–1.69 | 1.07 | 0.61–1.90 |
| 25 to < 35 h/week | 1.20 | 0.81–1.78 | 1.14 | 0.84–1.56 | 1.03 | 0.46–2.32 |
| 35 or more hours/week | 1.04 | 0.72–1.52 | 0.93 | 0.66–1.30 | 0.28 | 0.04–1.96 |
Model 3: adjusted for sex, age, occupational level BMI, smoking, musculoskeletal diseases at baseline, psychological disorders and lifting/carrying heavy loads at work
PR: prevalence ratio, Ref.: reference category
Table 8.
Associations between baseline workplace sitting in 2012 and lower back complaints in the last 12 months in 2017 (yes/no) stratified by leisure time physical activity to baseline among 2,082 employees aged 31–60 years in Germany. Poisson regressions. Prevalence Rations (PR)
| Exposure | Strata defined by leisure time physical activity prior to baseline | |||||
|---|---|---|---|---|---|---|
| Lower back, n = 1177 | ||||||
| Occupational sitting 2012 | none of the time | little/some of the time | mostly/all the time | |||
| PR | 95% CI | PR | 95% CI | PR | 95% CI | |
| Model 3 | ||||||
| Under 5 h/week | 1 | (Ref) | 1 | (Ref) | 1 | (Ref) |
| 5 to < 15 h/week | 1.15 | 0.98–1.36 | 1.00 | 0.86–1.17 | 0.71 | 0.50–1.01 |
| 15 to < 25 h/week | 1.22 | 1.01–1.47 | 1.13 | 0.96–1.33 | 0.80 | 0.57–1.12 |
| 25 to < 35 h/week | 1.32 | 1.07–1.63 | 1.03 | 0.85–1.24 | 0.88 | 0.54–1.41 |
| 35 or more hours/week | 1.08 | 0.87–1.43 | 1.03 | 0.85–1.25 | 0.66 | 0.34–1.29 |
Model 3: adjusted for sex, age, occupational level, BMI, smoking, musculoskeletal diseases at baseline, psychological disorders and lifting/carrying heavy loads at work
PR: prevalence ratio, Ref.: reference category
An association was observed between occupational sitting at baseline and the 12-month prevalence of neck, shoulder and lower back complaints among workers who did not engage in leisure time physical activity. Specifically, statistically significant increased PRs were observed for neck and shoulder complaints in association with 25 to < 35 h/week of occupational sitting among people reporting no strenuous leisure time physical activities. For lower back complaints, increased PRs were observed for both 15 to < 25 and 25 to < 35 h/week of occupational sitting (Table 8). However, other stratifications with little or some time, and mostly or all the time showed no increased risk.
Among workers with no leisure time physical activity, the highest PR was estimated for neck complaints for those sitting 25 to < 35 h/week at work after adjusting for all covariates (PR 1.46; 95% CI 1.18–1.80) (Table 5). Similar associations were not observed among groups of workers engaging in at least a little physical activity in their free time (little or some time, and mostly or all the time). Some indications of effect modifications were observed between physical activity category and occupational sitting for upper back complaints but these were not consistent and did not reach statistical significance (Table 7).
Discussion
Main results
The aim of this study was to examine the relationship between occupational sitting and the 12-month prevalence of neck, shoulder, upper back, and low back complaints among German workers. To the best of our knowledge, this is the only prospective study examining the association between sedentary working times and MSCs in a representative population of German workers. More than 60% of the study population self-reported spending over half of their working hours in a sitting position. Using an estimation of the weekly working hours spent sitting, our findings indicated that sitting at baseline was associated with an increased 12-month prevalence of neck, shoulder and low back complaints at follow-up if workers did not report any strenuous leisure time physical activities at baseline. Otherwise, we did not observe clear dose-response patterns between sitting time and MSC, with PRs sometimes even sinking below 1 for the highest exposure category. When analyzing the data separately for men and women, no clear differences between men and women were observed, but men with an estimated weekly occupational sitting time of 25 to < 35 h/week had an increased prevalence of neck complaints (PR 1.26, 95% CI 1.00-1.60) that we did not observe for women (PR 1.06, 95% CI 0.91–1.24). However, this could be a chance finding.
Comparison to other studies
From our findings, we cannot conclusively determine whether sitting per se is a direct risk factor for MSCs, or if sitting (as it was asked here) serves as a proxy for other unaddressed risk factors, such as seated restricted/awkward body postures (e.g., bent forward over work or microscope). Systematic reviews that focused on longitudinal studies investigating occupational risk factors for neck-shoulder complaints found strong evidence supporting a causal relationship between awkward body postures and neck-shoulder pain [10, 62]. However, the evidence regarding sitting as a risk factor was considered insufficient in those reviews. Some longitudinal studies show a negative association between sitting time and MSCs [63, 64]. However, prospective studies specifically examining occupational sitting and complaints related to the neck, shoulder, upper back, and lower back are limited and have yielded conflicting results [65, 66], leaving the role of sitting time in MSCs not entirely clear.
Our findings regarding the association between occupational sitting time and neck/shoulder complaints, differ some from the results of the studies by Grooten et al. [63] and Picavet et al. [64]. Grooten et al. [63] assessed the sitting duration of 803 workers through self-reporting and found that sitting for more than 75% of working hours was associated with a higher likelihood of being free of neck/shoulder pain after 5 years. We observed increased PRs for neck complaints at the 5-year follow-up that approached but did not reach statistically significance. Similarly, Picavet et al. [64] reported that increased self-reported time spent sitting at work was associated with reduced upper extremity pain over a 15-year period. However, Hallman et al. found an inverse U-shaped relationship but no significant association between objectively measured sitting time at work and neck/shoulder complaints among blue-collar workers in their study [18]. They suggested that this finding might be attributed to a healthy worker effect, indicating that workers experiencing severe pain may have shifted to work tasks involving less prolonged sitting. On the other hand, our findings are in line with the study conducted by Ariëns et al. [66] using video observations to estimate PRs for sitting time and neck pain for a sample of 977 workers from various occupations. They discovered that sitting for more than 95% of working hours increased the risk of reporting regular or persistent neck pain three years later, compared to those who engaged in very little sitting.
Cervical disc disorders (ICD-10: M50), a relatively clearly definable disease presenting with neck pain may also be associated with occupational sitting. In fact, a case-control study of 226 participants conducted by Elsner and colleagues found an increased odds of cervical disc prolapse associated with computer work for categories of cumulative hours of computer work up to 4,945 h and between 4,945 and < 13,883 h versus no computer work [67]. Further research of long-term cumulative exposures to computer work and the ergonomic characteristics of computer work are needed to confirm these results.
As for upper back complaints, we observed some increased PRs for categories of sitting times, albeit not statistically significant and without any clear trends. Our observations differ from those of Hossain et al. [68], who examined the prevalence of work-related musculoskeletal disorders among readymade garment workers in Bangladesh, and found a significant association between work-related sitting and upper back disorders. This difference may be due to the use of different types of instruments to measure risk factors between studies. In particular, Hossain et al. used the Quick Exposure Check instrument to assess work-related ergonomic risk factors and symptoms by body region, such as upper back pain.
In terms of low back complaints, a cross-sectional analysis in the ‘New method for Objective Measurements of physical Activity in Daily living (NOMAD)’ in Denmark study revealed a significant positive association between total sitting time (per hour) and the intensity of low back pain (odds ratio; OR = 1.43, 95%CI = 1.15–1.77) [69]. Our study also found a statistically significant increased PR for low back complaints, but only in the category of 15 to < 25 h/week of occupational sitting. However, we did considered only the prevalence of complaints and not the intensity of pain.
Although we did not detect any discernible disparities between men and women in our findings, it is important to underscore a discovery made in previous studies. A cross-sectional study in four age groups by Spittaels et al. [70] unveiled sex-dependent variations in sedentary time and levels of physical activity across different age groups. Specifically, their results depicted a linear relationship among men, where sedentary behavior increased and physical activity decreased with age, culminating in a peak of 59% time spent sedentary in adults. This avenue of investigation may shed further light on the reasons behind the varying effects of prolonged sitting across different contexts, such as work and leisure, and among distinct sexes. For instance, Toomingas et al. [71] observed that women spent an average of 11% of their workday engaged in uninterrupted sitting for more than an hour, whereas men spent only 4.6% of their workday in such long sitting bouts (p = 0.013).
When stratifying for leisure time physical activity, we observed differences in the association between sitting at work and the 12-month prevalence of shoulder and neck pain among workers who do not engage in leisure time physical activity in their free time and those who are physically active during their leisure time. This is similar to findings of a study examining full-time workers in Brisbane, Australia and Daegu, South Korea, which found that increased physical activity and less time sitting had a beneficial effect on reducing the development of neck pain [72]. A longitudinal study of asymptomatic office workers also found that for every 1,000 steps of walking, the risk of neck pain reduced by 14% [73]. However, these differences were not evident for lower back complaints. These results support previous findings from the systematic reviews conducted by Kwon et al. [74] and Swain et al. [75].
Occupational and leisure physical activity/sedentary time have divergent impacts on health. A survey of Danish workers found sedentary workers were more likely to have low back pain if they did not participate in sports, and workers with high physical workloads had more complaints in the lower-extremities if they did not participate in sports [76]. Holtermann et al. [77] also describe a paradox where the risk of long-term sickness absences increases with occupational physical activity and decreases with leisure time physical activity.
Strengths and weaknesses
The strengths of this study include the S-MGA’s the utilization of the Federal Employment Agency’s register as a comprehensive sampling framework. The use of the register provides a clear and unambiguous definition of the population under study, and the population-based registry contains the complete records of all workers included in the Germany social security system [35]. This helped ensure a representative study population.
One of the other strengths of this study was the adjustment of individual and work-related risk factors as potential confounders of MSCs. We also adjusted for lifting/carrying of heavy objects as a risk factor for MSCs. Nevertheless, it is still plausible that other unadjusted factors at work or during leisure may have influenced the association between sitting and MSCs, such as socioeconomic status and awkward body postures [45, 65, 78].
Although we had longitudinal data, we could not assess incident MSCs, because prevalent MSC at baseline could not be excluded from the analysis. However, MSCs vary over time, making it difficult to consider their incidence. Nevertheless, we attempted to mitigate any potential reverse causality by using baseline exposure and covariate data, and by adjusting for pre-existing musculoskeletal conditions.
In addition, while information on awkward body postures were available, we chose not to adjust for it because the question did not adequately differentiate between seated restricted/awkward positions (bent forward) and other awkward positions, such as reaching behind the head and twisting at the waist. Furthermore, based on the results from a systematic review [25], there was no evidence of an association between awkward occupational postures and LBP. It is possible that awkward occupational postures while sitting are independently causative of LBP in the populations of workers studied [25]. Nevertheless, the addition of neck and arm posture measurements could provide valuable insights into whether sitting posture primarily represents postural restriction or if it genuinely acts as a risk factor for MSCs [18]. Future studies should simultaneously record both sitting and arm postures and incorporate both variables into a model aiming to explain the risk of MSCs. These models could also explore the possibility of an interaction between sitting posture and arm postures.
Selection bias may also be a limitation of our analysis. For one, the only suitable sampling frame available for finding a rather representative German working population is the social security system. However, civil servants, the self-employed and freelancers are exempt from the social security system in Germany. Thus, these workers were not included in the S-MGA. Also, the S-MGA did not comprise workers older than 60 years at baseline because persons over 60 would reach retirement age of 65 before the first follow-up. We also excluded those who were retired or were otherwise not employed at follow-up, which may have introduced healthy work bias, as health problems can lead to unemployment or early retirement [79]. Although this may introduce some healthy-worker bias, we focused on those who were still working because sitting at work may have more of an acute or more immediate effect on the prevalence of MSCs. We found a strong correlation between baseline and follow-up values of sitting at work (Spearman’s rho = 0.8, P < 0.001) and a moderate correlation for working hours (Spearman’s rho = 0.7, P < 0.001).
One potential reason for the inconsistent findings among studies could be the use of self-reported measurements of sitting duration, which may be subject to inaccuracies and biases, possibly influenced by factors such as musculoskeletal complaints [69, 80]. Although sitting time is a prevalent behavior that can be easily recalled in interviews [81], it has been suggested that self-reported measures of sedentary behavior may be less reliable and valid than objective measures [82]. Objective data on sitting would have also allowed for a consideration of sitting in relation to standing or movements at work.
Furthermore, self-reported sitting time is prone to underestimation [83]. A further limitation is the self-reported information on physical activity. Self-reported assessments have been shown to correlate poorly with objective measures, and discrepancies seem to increase with the intensity of the physical activity being assessed [84]. This may have influenced our results as we used a variable describing activities with increased physical exertion. While measurement errors are likely, they would more likely be non-differential, which may bias the risk estimate towards null effect. If there is non-differential exposure misclassification, the true association between sitting time and MSCs might be even stronger than shown in our study.
Another limitation was that the S-MGA faced challenges in achieving the targeted response rate of 50%, despite considerable efforts made (e.g., reminder letters, incentives). The actual response at baseline and follow-up was about 37.5% and 59%, respectively. This low response might have implications for the internal as well as external validity of the study, as respondents might be less representative of the general population compared to the baseline cohort. Attrition over time further exacerbates this issue, potentially leading to selection effects.
Implications
Our study suggests that even moderate physical activity can help alleviate the negative impact of prolonged sitting on the risk of MSCs. This implies that promoting physical activity or integrating movement-based tasks into work activities could serve as effective methods for primary prevention of MSCs. In a recent systematic review conducted by Sundstrup et al. on workplace interventions to address musculoskeletal disorders among employees engaged in physically demanding work, they underscored the significance of implementing physical exercise at the workplace to reduce MSCs, particularly if it aligns with the job context [85]. Additionally, in a review focusing on workplace interventions for preventing upper extremity musculoskeletal disorders and symptoms, Eerd and colleagues found that stretching exercise programs, vibration feedback on mouse use, and workstation forearm supports demonstrated a moderate level of evidence for positively affecting the prevention of upper extremity MSCs. They further recommend the incorporation of workplace-based resistance training exercise programs to prevent and manage symptoms and disorders related to upper extremity MSCs [86].
One aspect that requires further investigation is how changes to working conditions following the pandemic may have changed the relationship between sedentary work and MSCs. This should be possible when the next wave of S-MGA data is available.
Moreover, studies by Gupta et al. [69] and Nourbakhsh et al. [87] have indicated that occupational sitting, leisure time sitting, and total sitting may be correlated. Hence, it may be important either to perform a combined analysis of occupational and leisure time sitting or to mutually adjust for these variables when investigating their independent association with MSCs. Another reason for differentiating between work and leisure time sitting is the potential variation in temporal patterns of sitting, which can be relevant for both metabolic [88] and musculoskeletal symptoms [89]. Additionally, MSCs often coexist with multiple health issues and morbidities [8, 90] and are becoming increasingly common comorbidities in chronic diseases like type 2 diabetes [91, 92].
Conclusion
These findings suggest a complex and multifactorial relationship between occupational sitting and MSCs, potentially involving interactions with other leisure time physical activity. While providing valuable insights, our study emphasizes the necessity for further research to fully elucidate mechanisms and establish a definitive causal relationship. It is crucial to either conduct a combined analysis of occupational and leisure time sitting or mutually adjust for these variables to explore their independent association with MSCs.
Furthermore, our results suggest that even infrequent physical activity may be an effective intervention or prevention strategy against sitting-related MSC in workers. However, further research is needed on the intensity, frequency and duration that may be beneficial for prevention. The study illuminates intricate associations between workplace sitting and various types of pain, hinting at potential protective effects within specific subgroups. These findings underscore the need for comprehensive research to understand these relationships better and identify preventive measures for workplace-related pain complaints. Future studies should delve into additional factors and utilize more objective measures of sitting and leisure time physical activity to enhance result validity and uncover underlying mechanisms. Addressing these knowledge gaps will enable the development of targeted interventions promoting musculoskeletal health and overall well-being in work environments.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We are grateful to the Research Data Center of the Federal Institute for Occupational Safety and Health (BAuA), Germany (FDZ-BAUA) for making the Scientific Use File available. We are also grateful for the valuable comments by Dr. Ulrike Rösler from the BAuA. Thank you also to Uwe Rose for answering our questions regarding the S-MGA study.
Author contributions
All authors critically revised the manuscript for important intellectual content. THAD conducted the analyses and wrote the first draft with JH. THAD and KRS were also involved in the data management and analysis. All authors critically revised and commented on the manuscript drafts.
Funding
Open Access funding enabled and organized by Projekt DEAL. This study was partially funded by the Federal Institute for Occupational Safety and Health (F 2384).
Open Access funding enabled and organized by Projekt DEAL.
Data availability
A file called the Scientific Use File (SUF), which includes both wave 1 and wave 2 of the cohort, is accessible at the Research Data Centre of the Federal Institute of Occupational Safety and Health (FDZ-BAuA). Research teams interested in analyzing data from the S-MGA study can request access through the FDZ-BAuA (https://www.baua.de/DE/Forschung/Forschungsdaten/Forschungsdaten_node.html).
Declarations
Ethics approval and consent to participate
This study was conducted according to the guidelines of the Declaration of Helsinki and was approved by the Ethics Committee of the Federal Institute for Occupational Safety and Health (BAuA; approval number 006_2016_Müller, 6 March 2016).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Blyth FM, Briggs AM, Schneider CH, Hoy DG, March LM. The Global Burden of Musculoskeletal Pain-where to from Here? Am J Public Health. 2019;109(1):35–40. doi: 10.2105/AJPH.2018.304747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.James SL, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the global burden of Disease Study 2017. Lancet. 2018;392(10159):1789–858. doi: 10.1016/S0140-6736(18)32279-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Punnett L. Musculoskeletal disorders and occupational exposures: how should we judge the evidence concerning the causal association? Scand J Public Health. 2014;42(13suppl):49–58. doi: 10.1177/1403494813517324. [DOI] [PubMed] [Google Scholar]
- 4.Korhan O, Ahmed Memon A. Introductory Chapter: Work-Related Musculoskeletal Disorders [Internet]. Work-related Musculoskeletal Disorders: IntechOpen; 2019. [Google Scholar]
- 5.Barmer BARMERG. 2022 2022 [Available from: https://www.bifg.de/publikationen/reporte/gesundheitsreport%2D2022]. [Accessed: 04 March 2024].
- 6.TK. Gesundheitsreporte nach Jahren| Die Techniker - Firmenkunden 2022 [Available from: https://www.tk.de/firmenkunden/service/gesund-arbeiten/gesundheitsberichterstattung/archiv-gesundheitsreporte/gesundheitsreporte-nach-jahren-2034298]. [Accessed: 2022/11/27/11:04:19].
- 7.Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the global burden of Disease Study 2010. Lancet (London England). 2012;380(9859):2163–96. [DOI] [PMC free article] [PubMed]
- 8.Briggs AM, Woolf AD, Dreinhöfer K, Homb N, Hoy DG, Kopansky-Giles D, et al. Reducing the global burden of musculoskeletal conditions. Bull World Health Organ. 2018;96(5):366–8. doi: 10.2471/BLT.17.204891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.da Costa BR, Vieira ER. Risk factors for work-related musculoskeletal disorders: a systematic review of recent longitudinal studies. Am J Ind Med. 2010;53(3):285–323. doi: 10.1002/ajim.20750. [DOI] [PubMed] [Google Scholar]
- 10.Mayer J, Kraus T, Ochsmann E. Longitudinal evidence for the association between work-related physical exposures and neck and/or shoulder complaints: a systematic review. Int Arch Occup Environ Health. 2012;85(6):587–603. doi: 10.1007/s00420-011-0701-0. [DOI] [PubMed] [Google Scholar]
- 11.Sharma G, Ahmad S, Mallick Z, Khan ZA, James AT, Asjad M, et al. Risk factors Assessment of Musculoskeletal disorders among Professional Vehicle drivers in India using an Ordinal Priority Approach. Mathematics. 2022;10(23):4492. doi: 10.3390/math10234492. [DOI] [Google Scholar]
- 12.Dzakpasu FQS, Carver A, Brakenridge CJ, Cicuttini F, Urquhart DM, Owen N, Dunstan DW. Musculoskeletal pain and sedentary behaviour in occupational and non-occupational settings: a systematic review with meta-analysis. Int J Behav Nutr Phys Act. 2021;18(1):159. doi: 10.1186/s12966-021-01191-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Celik S, Celik K, Dirimese E, Taşdemir N, Arik T, Büyükkara İ. Determination of pain in musculoskeletal system reported by office workers and the pain risk factors. Int J Occup Med Environ Health. 2018;31(1):91–111. doi: 10.13075/ijomeh.1896.00901. [DOI] [PubMed] [Google Scholar]
- 14.Davis KG, Kotowski SE. Postural variability: an effective way to reduce musculoskeletal discomfort in office work. Hum Factors. 2014;56(7):1249–61. doi: 10.1177/0018720814528003. [DOI] [PubMed] [Google Scholar]
- 15.Lee S-H, Son C, Yeo S, Ha I-H. Cross-sectional analysis of self-reported sedentary behaviors and chronic knee pain among South Korean adults over 50 years of age in KNHANES 2013–2015. BMC Public Health. 2019;19:1375. doi: 10.1186/s12889-019-7653-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Waersted M, Hanvold TN, Veiersted KB. Computer work and musculoskeletal disorders of the neck and upper extremity: a systematic review. BMC Musculoskelet Disord. 2010;11:79. doi: 10.1186/1471-2474-11-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yue P, Liu F, Li L. Neck/shoulder pain and low back pain among school teachers in China, prevalence and risk factors. BMC Public Health. 2012;12(1):789. doi: 10.1186/1471-2458-12-789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hallman DM, Gupta N, Mathiassen SE, Holtermann A. Association between objectively measured sitting time and neck-shoulder pain among blue-collar workers. Int Arch Occup Environ Health. 2015;88(8):1031–42. doi: 10.1007/s00420-015-1031-4. [DOI] [PubMed] [Google Scholar]
- 19.Stefansdottir R, Gudmundsdottir SL. Sedentary behavior and musculoskeletal pain: a five-year longitudinal Icelandic study. Public Health. 2017;149:71–3. doi: 10.1016/j.puhe.2017.04.019. [DOI] [PubMed] [Google Scholar]
- 20.Alzahrani H, Alshehri M, Attar WA, Alzhrani M. (320) The Association between Sedentary Behavior and Low Back Pain: A Systematic Review and Meta-Analysis of Longitudinal Studies The Journal of Pain. 2019;20(4, Supplement):S55. [DOI] [PMC free article] [PubMed]
- 21.Chen S-M, Liu M-F, Cook J, Bass S, Lo SK. Sedentary lifestyle as a risk factor for low back pain: a systematic review. Int Arch Occup Environ Health. 2009;82(7):797–806. doi: 10.1007/s00420-009-0410-0. [DOI] [PubMed] [Google Scholar]
- 22.Hartvigsen J, Leboeuf-Yde C, Lings S, Corder EH. Is sitting-while-at-work associated with low back pain? A systematic, critical literature review. Scand J Public Health. 2000;28(3):230–9. [PubMed] [Google Scholar]
- 23.Jun D, Zoe M, Johnston V, O’Leary S. Physical risk factors for developing non-specific neck pain in office workers: a systematic review and meta-analysis. Int Arch Occup Environ Health. 2017;90(5):373–410. doi: 10.1007/s00420-017-1205-3. [DOI] [PubMed] [Google Scholar]
- 24.Paksaichol A, Janwantanakul P, Purepong N, Pensri P, van der Beek AJ. Office workers’ risk factors for the development of non-specific neck pain: a systematic review of prospective cohort studies. Occup Environ Med. 2012;69(9):610–8. doi: 10.1136/oemed-2011-100459. [DOI] [PubMed] [Google Scholar]
- 25.Roffey DM, Wai EK, Bishop P, Kwon BK, Dagenais S. Causal assessment of occupational sitting and low back pain: results of a systematic review. Spine Journal: Official J North Am Spine Soc. 2010;10(3):252–61. doi: 10.1016/j.spinee.2009.12.005. [DOI] [PubMed] [Google Scholar]
- 26.De Carvalho DE, de Luca K, Funabashi M, Breen A, Wong AYL, Johansson MS, et al. Association of exposures to seated postures with Immediate increases in Back Pain: a systematic review of studies with objectively measured sitting time. J Manip Physiol Ther. 2020;43(1):1–12. doi: 10.1016/j.jmpt.2019.10.001. [DOI] [PubMed] [Google Scholar]
- 27.Øverås CK, Villumsen M, Axén I, Cabrita M, Leboeuf-Yde C, Hartvigsen J, Mork PJ. Association between objectively measured physical behaviour and neck- and/or low back pain: a systematic review. Eur J Pain. 2020;24(6):1007–22. doi: 10.1002/ejp.1551. [DOI] [PubMed] [Google Scholar]
- 28.Brewer S, Van Eerd D, Amick BC, Irvin E, Daum KM, Gerr F, et al. Workplace interventions to prevent musculoskeletal and visual symptoms and disorders among computer users: a systematic review. J Occup Rehabil. 2006;16(3):325–58. doi: 10.1007/s10926-006-9031-6. [DOI] [PubMed] [Google Scholar]
- 29.Ijmker S, Huysmans MA, Blatter BM, van der Beek AJ, van Mechelen W, Bongers PM. Should office workers spend fewer h at their computer? A systematic review of the literature. Occup Environ Med. 2007;64(4):211–22. doi: 10.1136/oem.2006.026468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Khan MR, Singh NK. Prevalence of musculoskeletal disorders among Indian railway sahayaks. Int J Occup Environ Health. 2018;24(1–2):27–37. doi: 10.1080/10773525.2018.1507187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sattar N, Preiss D. Reverse causality in Cardiovascular Epidemiological Research. More Common than Imagined? Circulation. 2017;135(24):2369–72. doi: 10.1161/CIRCULATIONAHA.117.028307. [DOI] [PubMed] [Google Scholar]
- 32.Chau JY, Grunseit A, Midthjell K, Holmen J, Holmen TL, Bauman AE, van der Ploeg HP. Cross-sectional associations of total sitting and leisure screen time with cardiometabolic risk in adults. Results from the HUNT study, Norway. J Sci Med Sport. 2014;17(1):78–84. doi: 10.1016/j.jsams.2013.03.004. [DOI] [PubMed] [Google Scholar]
- 33.Tigbe WW, Lean MEJ, Granat MH. A physically active occupation does not result in compensatory inactivity during out-of-work h. Prev Med. 2011;53(1):48–52. doi: 10.1016/j.ypmed.2011.04.018. [DOI] [PubMed] [Google Scholar]
- 34.Heneweer H, Picavet HSJ, Staes F, Kiers H, Vanhees L. Physical fitness, rather than self-reported physical activities, is more strongly associated with low back pain: evidence from a working population. Eur Spine J. 2012;21(7):1265–72. doi: 10.1007/s00586-011-2097-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rose U, Schiel S, Schröder H, Kleudgen M, Tophoven S, Rauch A, et al. The study on Mental Health at Work: design and sampling. Scand J Public Health. 2017;45(6):584–94. doi: 10.1177/1403494817707123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Oberschachtsiek D, Scioch P, Seysen C, Heining J. Integr Employ Biographies Sample. 2009(03):64. https://doku.iab.de/fdz/reporte/2009/DR_03-09-EN.pdf
- 37.Alda H, Bender S, Gartner H. The linked employer-employee dataset of the IAB (LIAB). 6/2005. 2012.
- 38.Schiel S, Sandbrink K, Aust F, Schumacher D. Mentale Gesundheit bei der Arbeit (S-MGA II). 2018. 10.21934/baua:bericht20180831
- 39.Pattloch D, Rose U, Menze L, Schöllgen I. Datendokumentation des Scientific Use File der Studie zur Mentalen Gesundheit bei der Arbeit (S-MGA), Wellen 1 und 2. 2021.
- 40.Kuorinka I, Jonsson B, Kilbom A, Vinterberg H, Biering-Sørensen F, Andersson G, Jørgensen K. Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Occup Med. 2007;57(4):300–1. doi: 10.1016/0003-6870(87)90010-X. [DOI] [PubMed] [Google Scholar]
- 41.Lu M-L, Lowe BD, Howard NL, Meyers AR, Fox RR, Dong RG, Baker BA. Work-related Musculoskeletal disorders. Mod Occup Dis Diagnosis. 2022:287–353.
- 42.Tynes T, Aagestad C, Thorsen SV, Andersen LL, Perkio-Makela M, García FJP, et al. Physical working conditions as covered in European monitoring questionnaires. BMC Public Health. 2017;17(1):544. doi: 10.1186/s12889-017-4465-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.CDC. Diseases and Long Hours (Continued), Musculoskeletal Disorders: Centers for Disease Control (CDC). 2020 [Available from: https://www.cdc.gov/niosh/work-hour-training-for-nurses/longh/mod3/24.htmlfiles/4365/24.html]. [Accessed: 2023/07/14/15:40:53].
- 44.Matthews CE, Chen KY, Freedson PS, Buchowski MS, Beech BM, Pate RR, Troiano RP. Amount of Time Spent in sedentary behaviors in the United States, 2003–2004. Am J Epidemiol. 2008;167(7):875–81. doi: 10.1093/aje/kwm390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Clark B, Kolbe-Alexander T, Duncan M, Brown W. Sitting time, physical activity and sleep by work type and pattern—the Australian longitudinal study on women’s Health. Int J Environ Res Public Health. 2017;14(3):290. doi: 10.3390/ijerph14030290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ervasti J, Pentti J, Nyberg ST, Shipley MJ, Leineweber C, Sørensen JK, et al. Long working hours and risk of 50 health conditions and mortality outcomes: a multicohort study in four European countries. Lancet Reg Health Europe. 2021;11:100212. doi: 10.1016/j.lanepe.2021.100212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lin T, Courtney TK, Lombardi DA, Verma SK. Association between sedentary work and BMI in a U.S. National Longitudinal Survey. Am J Prev Med. 2015;49(6):e117–23. doi: 10.1016/j.amepre.2015.07.024. [DOI] [PubMed] [Google Scholar]
- 48.Baker R, Coenen P, Howie E, Williamson A, Straker L. The Short Term Musculoskeletal and Cognitive effects of prolonged sitting during Office Computer Work. Int J Environ Res Public Health. 2018;15(8). [DOI] [PMC free article] [PubMed]
- 49.Alzahrani H, Alshehri MA, Alzhrani M, Alshehri YS, Al Attar WSA. The association between sedentary behavior and low back pain in adults: a systematic review and meta-analysis of longitudinal studies. PeerJ. 2022;10:e13127. doi: 10.7717/peerj.13127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.AlOmar RS, AlShamlan NA, Alawashiz S, Badawood Y, Ghwoidi BA, Abugad H. Musculoskeletal symptoms and their associated risk factors among Saudi office workers: a cross-sectional study. BMC Musculoskelet Disord. 2021;22(1):763. doi: 10.1186/s12891-021-04652-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hoy D, March L, Brooks P, Blyth F, Woolf A, Bain C, et al. The global burden of low back pain: estimates from the global burden of Disease 2010 study. Ann Rheum Dis. 2014;73(6):968–74. doi: 10.1136/annrheumdis-2013-204428. [DOI] [PubMed] [Google Scholar]
- 52.Robertson D, Kumbhare D, Nolet P, Srbely J, Newton G. Associations between low back pain and depression and somatization in a Canadian emerging adult population. J Can Chiropr Assoc. 2017;61(2):96–105. [PMC free article] [PubMed] [Google Scholar]
- 53.Shiri R, Karppinen J, Leino-Arjas P, Solovieva S, Viikari-Juntura E. The association between smoking and low back pain: a meta-analysis. Am J Med. 2010;123(1):e877–35. doi: 10.1016/j.amjmed.2009.05.028. [DOI] [PubMed] [Google Scholar]
- 54.Webb R, Brammah T, Lunt M, Urwin M, Allison T, Symmons D. Prevalence and predictors of intense, chronic, and disabling neck and back pain in the UK general population. Spine. 2003;28(11):1195–202. doi: 10.1097/01.BRS.0000067430.49169.01. [DOI] [PubMed] [Google Scholar]
- 55.Textor J, van der Zander B, Gilthorpe MS, Liskiewicz M, Ellison GT. Robust causal inference using directed acyclic graphs: the R package ‘dagitty’. Int J Epidemiol. 2016;45(6):1887–94. doi: 10.1093/ije/dyw341. [DOI] [PubMed] [Google Scholar]
- 56.Hasselhorn H-M, Freude G. Der Work-Ability-Index: Ein Leitfaden. Bremerhaven: Wirtschaftsverl. NW, Verl. für neue Wiss; 2007. p. 54.
- 57.Weir CB, Jan A. BMI classification percentile and cut off points. StatPearls. Treasure Island (FL): StatPearls Publishing; 2022. [PubMed] [Google Scholar]
- 58.WHO. The Asia-Pacific perspective: redefining obesity and its treatment. 2000.
- 59.Hagen F. Levels of education: relation between ISCO skill Level and ISCED Categories. In: telematic multidisciplinary assistive technology education. 2015.
- 60.Bull FC, Al-Ansari SS, Biddle S, Borodulin K, Buman MP, Cardon G, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54(24):1451–62. doi: 10.1136/bjsports-2020-102955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.StataCorp . Stata Statistical Software: Release MP/14. College Station. TX: StataCorp LLC; 2018. [Google Scholar]
- 62.SBU. Swedish Agency for Health Technology Assessment and Assessment of Social Services (SBU) Swedish Agency for Health Technology Assessment and Assessment of Social Services (SBU) copyright © 2022 by SBU–. Stockholm: Swedish Agency for Health Technology Assessment and Assessment of Social Services; 2022. SBU Systematic Review Summaries. Occupational exposures and complaints of neck, shoulder, arm, or hand: a systematic review. [PubMed] [Google Scholar]
- 63.Grooten WJ, Mulder M, Josephson M, Alfredsson L, Wiktorin C. The influence of work-related exposures on the prognosis of neck/shoulder pain. Eur Spine J. 2007;16(12):2083–91. doi: 10.1007/s00586-007-0481-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Picavet HSJ, Pas LW, Oostrom SHv P, HPvd, Verschuren WMM, Proper KI. The relation between Occupational sitting and Mental, Cardiometabolic, and Musculoskeletal Health over a period of 15 years– the Doetinchem Cohort Study. PLoS ONE. 2016;11(1):e0146639. doi: 10.1371/journal.pone.0146639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hallman DM, Gupta N, Heiden M, Mathiassen SE, Korshøj M, Jørgensen MB, Holtermann A. Is prolonged sitting at work associated with the time course of neck-shoulder pain? A prospective study in Danish blue-collar workers. BMJ open. 2016;6(11):e012689. doi: 10.1136/bmjopen-2016-012689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ariëns GM, Bongers PM, Douwes M, Miedema MC, Hoogendoorn WE, Wal Gvd, et al. Are neck flexion, neck rotation, and sitting at work risk factors for neck pain? Results of a prospective cohort study. Occup Environ Med. 2001;58(3):200–7. doi: 10.1136/oem.58.3.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Elsner G, Petereit-Haack G, Haerting J, Bergmann A, Bolm-Audorff U, Celik S, et al. Fall-Kontroll-Studie zu Bandscheibenvorfällen Der Halswirbelsäule durch berufliche Belastungen. Dortmund Berlin Dresden: BAuA; 2009. p. 104. [Google Scholar]
- 68.Hossain MD, Aftab A, Al Imam MH, Mahmud I, Chowdhury IA, Kabir RI, Sarker M. Prevalence of work related musculoskeletal disorders (WMSDs) and ergonomic risk assessment among readymade garment workers of Bangladesh: a cross sectional study. PLoS ONE. 2018;13(7):e0200122. doi: 10.1371/journal.pone.0200122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Gupta N, Christiansen CS, Hallman DM, Korshøj M, Carneiro IG, Holtermann A. Is objectively measured sitting Time Associated with Low Back Pain? A cross-sectional investigation in the NOMAD study. PLoS ONE. 2015;10(3):e0121159. doi: 10.1371/journal.pone.0121159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Spittaels H, Van Cauwenberghe E, Verbestel V, De Meester F, Van Dyck D, Verloigne M, et al. Objectively measured sedentary time and physical activity time across the lifespan: a cross-sectional study in four age groups. Int J Behav Nutr Phys Act. 2012;9:149. doi: 10.1186/1479-5868-9-149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Toomingas A, Forsman M, Mathiassen SE, Heiden M, Nilsson T. Variation between seated and standing/walking postures among male and female call centre operators. BMC Public Health. 2012;12:154. doi: 10.1186/1471-2458-12-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Jun D, Johnston V, McPhail SM, O’Leary S. A longitudinal evaluation of risk factors and interactions for the Development of Nonspecific Neck Pain in Office Workers in two cultures. Hum Factors. 2021;63(4):663–83. doi: 10.1177/0018720820904231. [DOI] [PubMed] [Google Scholar]
- 73.Sitthipornvorakul E, Janwantanakul P, Lohsoonthorn V. The effect of daily walking steps on preventing neck and low back pain in sedentary workers: a 1-year prospective cohort study. European Spine Journal: Official Publication of the European Spine Society, the European Spinal Deformity Society, and the European section of the cervical. Spine Res Soc. 2015;24(3):417–24. doi: 10.1007/s00586-014-3577-3. [DOI] [PubMed] [Google Scholar]
- 74.Kwon BK, Roffey DM, Bishop PB, Dagenais S, Wai EK. Systematic review: occupational physical activity and low back pain. Occup Med. 2011;61(8):541–8. doi: 10.1093/occmed/kqr092. [DOI] [PubMed] [Google Scholar]
- 75.Swain CTV, Pan F, Owen PJ, Schmidt H, Belavy DL. No consensus on causality of spine postures or physical exposure and low back pain: a systematic review of systematic reviews. J Biomech. 2020;102:109312. doi: 10.1016/j.jbiomech.2019.08.006. [DOI] [PubMed] [Google Scholar]
- 76.Hildebrandt VH, Bongers PM, Dul J, van Dijk FJ, Kemper HC. The relationship between leisure time, physical activities and musculoskeletal symptoms and disability in worker populations. Int Arch Occup Environ Health. 2000;73(8):507–18. doi: 10.1007/s004200000167. [DOI] [PubMed] [Google Scholar]
- 77.Holtermann A, Hansen JV, Burr H, Sogaard K, Sjogaard G. The health paradox of occupational and leisure-time physical activity. Br J Sports Med. 2012;46(4):291–5. doi: 10.1136/bjsm.2010.079582. [DOI] [PubMed] [Google Scholar]
- 78.Hallman DM, Mathiassen SE, Heiden M, Gupta N, Jørgensen MB, Holtermann A. Temporal patterns of sitting at work are associated with neck-shoulder pain in blue-collar workers: a cross-sectional analysis of accelerometer data in the DPHACTO study. Int Arch Occup Environ Health. 2016;89(5):823–33. doi: 10.1007/s00420-016-1123-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Pedersen J, Bjorner JB, Burr H, Christensen KB. Transitions between sickness absence, work, unemployment, and disability in Denmark 2004–2008. Scand J Work Environ Health. 2012;38(6):516–26. doi: 10.5271/sjweh.3293. [DOI] [PubMed] [Google Scholar]
- 80.Balogh I, Ørbaek P, Ohlsson K, Nordander C, Unge J, Winkel J, et al. Self-assessed and directly measured occupational physical activities–influence of musculoskeletal complaints, age and gender. Appl Ergon. 2004;35(1):49–56. doi: 10.1016/j.apergo.2003.06.001. [DOI] [PubMed] [Google Scholar]
- 81.Ribeiro AS, Pereira LC, Silva DRP, Santos Ld, Schoenfeld BJ, Teixeira DC, et al. Physical activity and sitting time are specifically Associated with multiple chronic diseases and Medicine Intake in Brazilian older adults. J Aging Phys Act. 2018;26(4):608–13. doi: 10.1123/japa.2017-0271. [DOI] [PubMed] [Google Scholar]
- 82.Lagersted-Olsen J, Korshøj M, Skotte J, Carneiro IG, Søgaard K, Holtermann A. Comparison of objectively measured and self-reported Time spent sitting. Int J Sports Med. 2014;35(6):534–40. doi: 10.1055/s-0033-1358467. [DOI] [PubMed] [Google Scholar]
- 83.Ryu S, Chang Y, Jung H-S, Yun KE, Kwon M-J, Choi Y, et al. Relationship of sitting time and physical activity with non-alcoholic fatty liver disease. J Hepatol. 2015;63(5):1229–37. doi: 10.1016/j.jhep.2015.07.010. [DOI] [PubMed] [Google Scholar]
- 84.Prince SA, Cardilli L, Reed JL, Saunders TJ, Kite C, Douillette K, et al. A comparison of self-reported and device measured sedentary behaviour in adults: a systematic review and meta-analysis. Int J Behav Nutr Phys Act. 2020;17(1):31. doi: 10.1186/s12966-020-00938-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Sundstrup E, Seeberg KGV, Bengtsen E, Andersen LL. A systematic review of Workplace interventions to Rehabilitate Musculoskeletal disorders among employees with physical demanding work. J Occup Rehabil. 2020;30(4):588–612. doi: 10.1007/s10926-020-09879-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Eerd DV, Munhall C, Irvin E, Rempel D, Brewer S, Beek AJ, et al. Effectiveness of workplace interventions in the prevention of upper extremity musculoskeletal disorders and symptoms: an update of the evidence. Occup Environ Med. 2016;73(1):62–70. doi: 10.1136/oemed-2015-102992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Nourbakhsh MR, Moussavi SJ, Salavati M. Effects of lifestyle and work-related physical activity on the degree of lumbar lordosis and chronic low back pain in a Middle East population. J Spinal Disord. 2001;14(4):283–92. doi: 10.1097/00002517-200108000-00002. [DOI] [PubMed] [Google Scholar]
- 88.Healy GN, Dunstan DW, Salmon J, Cerin E, Shaw JE, Zimmet PZ, Owen N. Breaks in sedentary time: beneficial associations with metabolic risk. Diabetes Care. 2008;31(4):661–6. doi: 10.2337/dc07-2046. [DOI] [PubMed] [Google Scholar]
- 89.Mathiassen SE. Diversity and variation in biomechanical exposure: what is it, and why would we like to know? Appl Ergon. 2006;37(4):419–27. doi: 10.1016/j.apergo.2006.04.006. [DOI] [PubMed] [Google Scholar]
- 90.GBD Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the global burden of Disease Study 2017. Lancet (London England) 2018;392(10159):1789–858. doi: 10.1016/S0140-6736(18)32279-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Sözen T, Başaran NÇ, Tınazlı M, Özışık L. Musculoskeletal problems in diabetes mellitus. Eur J Rheumatol. 2018;5(4):258–65. doi: 10.5152/eurjrheum.2018.18044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Williams MF, London DA, Husni EM, Navaneethan S, Kashyap SR. Type 2 diabetes and osteoarthritis: a systematic review and meta-analysis. J Diabetes Complicat. 2016;30(5):944–50. doi: 10.1016/j.jdiacomp.2016.02.016. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
A file called the Scientific Use File (SUF), which includes both wave 1 and wave 2 of the cohort, is accessible at the Research Data Centre of the Federal Institute of Occupational Safety and Health (FDZ-BAuA). Research teams interested in analyzing data from the S-MGA study can request access through the FDZ-BAuA (https://www.baua.de/DE/Forschung/Forschungsdaten/Forschungsdaten_node.html).