Abstract
Objective:
To estimate the marginal cost differences and care delivery process of a telerehabilitation versus outpatient session.
Design:
This study used a time-driven activity-based costing (TDABC) approach including 1) observation of rehabilitation sessions and creation of manual time stamps, 2) structured and recorded interviews with two occupational therapists familiar with outpatient therapy and two therapists familiar with telerehabilitation, 3) collection of standard wages for providers, and 4) the creation of an iterative flowchart of both an outpatient and telerehabilitation session care delivery process.
Setting:
Telerehabilitation and outpatient therapy evaluation.
Participants:
Three therapists familiar with care deliver for telerehabilitation or outpatient therapy.
Interventions:
Not applicable.
Main Outcome Measures:
Marginal cost difference between telerehabilitation and outpatient therapy evaluations.
Results:
Overall, telerehabilitation ($225.41) was more costly than outpatient therapy ($168.29) per session for a cost difference of $57.12. Primary time drivers of this finding were initial phone calls (0 mins for OP therapists versus 35 mins for TR) and post documentation (5 mins for OP versus 30 mins for TR) demands for telerehabilitation.
Conclusions:
Telerehabilitation is an emerging platform with the potential to reduce costs, improve healthcare inequities, and facilitate better patient outcomes. Improvements in documentation practices, staffing, technology, and reimbursement structuring would allow for a more successful translation.
Keywords: costs and cost analysis, telemedicine, physical rehabilitation, stroke
Access to stroke rehabilitation is limited for certain demographic groups including rural and low-income stroke survivors.1–5 The odds of receiving rehabilitation therapy for a stroke survivor are 1.2 times greater for urban than rural residents, with a 45% decreased odds for highly rural area where the population density is <7 per square mile.5 Early and high intensity therapy are necessary for maximal stroke recovery.6 Higher doses of therapy are correlated with better outcomes7, but traditional outpatient therapy is drastically underdosed with reduced effectiveness.6,8 Barriers to high dose therapy include cost, transportation, shortage of specialists in rural care, and patients’ poor adherence to home protocols.9
Telerehabilitation has the potential to overcome these barriers to care. Telerehabilitation involves the use of communication technologies such as telephones, videoconferencing, and remote tracking devices to deliver rehabilitation.10,11 Widespread use of telerehabilitation for stroke therapy could revolutionize occupational therapy (OT) delivery. Stroke care via telehealth has been shown to improve reach to rural communities 3. Additionally, when compared to traditional face-to-face therapy, telerehabilitation provides equal or greater benefits for stroke in areas of motor planning9, activities of daily living11, quality of life and depression12, caregiver training and burden13, and balance.14 Furthermore, telerehabilitation for stroke has demonstrated high levels of patient safety, satisfaction, and favorability.9
While there is growing support for telerehabilitation’s potential to improve patient access and positive therapy outcomes, little work has been done to compare its cost-effectiveness versus traditional in-person outpatient models of care .11,15 A 2022 systematic review revealed two telerehabilitation for stroke studies that considered costs.16 However, these studies were specific to a gaming intervention17 and a telephone follow-up protocol18 that are not necessarily reflective of general telerehabilitation. A third publication addressed costs for general telerehabilitation but specifically omitted indirect time costs such as the organization of care and documentation.19 Another systematic review concluded telerehabilitation has the potential be a cost-saving approach to care delivery.20
Cost analyses can identify costly variations in the care process that can be targeted for improvement There are three primary costing methods: 1) applying cost to charge ratio (CCR) to billing data, 2) using published relative value units (RVU), and 3) assessing actual patient visit flow using activity-based costing (ABC).21 The disadvantage with these traditional costing methods is they make it difficult to identify variations in the care process that may be significant drivers of costs and potential targets for improvement.22 Traditional billing lumps all rehabilitation costs into one number without any detailed information about work flow. Without a deep understanding of the care processes, it is difficult to find opportunities to improve efficiency.
In contrast, ABC starts with a bottom-up approach to build to an upstream aggregate cost. By examining the actual activities that make up a therapy session and who performs them, it is possible to clearly define processes and reduce costs of workflow and care delivery. Additionally, changing who performs certain activities can reduce aggregate costs. For example, costs can be reduced by having certified occupational therapy assistants (COTAs) rather than OTs provide some interventions or aides rather than therapy staff address administrative tasks. Traditional ABC, however, is limited by a lack of a time component. For billed services, an OT and a COTA are going to spend the same amount of time treating a patient with different levels of salary. However, costs for nonbillable time such as patient scheduling, non-point of service documentation, and equipment setup are difficult to calculate with traditional ABC methods.
Examining the cost of care delivery broken down into a minute-by-minute flowchart will allow for the comparison of different approaches to therapy and discover possible areas for improvement. Time-driven activity-based costing (TDABC) is a technique used to improve efficiency in healthcare workflow by measuring costs required to deliver healthcare processes while adding a time variable.21 It combines techniques from accounting and industrial engineering to identify potential areas of cost reduction.23 This is typically done within the context of a specific type of patient visit. The element of time enables researchers and decision makers to understand how shifting clinic responsibilities or documentation processing may influence overall cost. For example, an occupational therapy aid spending 5 minutes to set up equipment allows occupational therapists to focus more effort on billable treatment time for high level rehabilitation. A TDABC consists of a multiple step process that is resource intensive utilizing expert interviews for short and inexpensive activities and observation for longer and complex activities.24 Recently, a modified TDABC process was developed and applied to telehealth.25 This approach has demonstrated feasibility, requires less research resources, and utilizes a structured qualitative approach to have expert providers describe workflows to be used to estimate resources used to deliver care. Workflow resource costs are then calculated for use as cost weights in economic evaluations.25
The aim of this project is to use time-driven activity-based costing (TDABC) to define the care delivery process and marginal cost differences for delivery of an initial OT assessment visit using telehealth compared to an in-person approach. Given the inherent reduction in patient travel time and cost-saving predictions from the literature20, we hypothesize telerehabilitation will be less costly than outpatient therapy as a care delivery process. We also hope this project will help define the care delivery process for telerehabilitation and assist therapists and administrators by providing them with potential areas of cost reduction.
2. Methods
We examined the costs of providing a stroke rehabilitation session via telerehabilitation versus traditional outpatient therapy using TDABC. This TDABC approach24,25 included: 1) observation of rehabilitation sessions and creation of manual time stamps, 2) structured and recorded interviews with two occupational therapists familiar with outpatient therapy and two therapists familiar with telerehabilitation, 3) collection of standard wages for providers, and 4) the creation of an iterative flowchart of both an outpatient and telerehabilitation session care delivery process. This study followed the reporting guidelines to ensure a standardization for TDABC research.26 This study was deemed a quality improvement project by the Institutional Review Board at the Medical University of South Carolina.
2.1. Site descriptions
For this TDABC analysis, we observed three therapy sites within the United States. Sites were chosen based on their established integration of telerehabilitation. The first was a large, hospital-based outpatient clinic in a metropolitan area focused on neurorehabilitation. The second was a private company offering telerehabilitation to rural school-aged patients with neurological deficits. The third site was a nationwide healthcare system experimenting with telerehabilitation for patients with neurological deficits using an in-house developed videoconferencing platform. While the focus of this project was on care delivery for stroke rehabilitation, we felt the care delivery process would not differ significantly with other neurological conditions. To increase our number of sessions, we also observed patient conditions included multiple sclerosis, brain injury, and cerebral palsy.
2.2. Observation of rehabilitation sessions and creation of manual time stamps
The first step in the TDABC process consisted of one author observing 19 neuro-telerehabilitation sessions to better understand the care delivery process. The researcher recorded descriptions of tasks completed during the therapy session, the flow of tasks, and time spent on all tasks for each session. Time was kept via a stopwatch and rounded to the nearest minute. Additionally, actors (all personnel) involved in the care delivery process were recorded. Based on these recordings, basic care delivery flowcharts were drafted. After the 19 sessions, no new information was emerging as saturation had likely been achieved.
2.3. Interview process
The second step involved researchers administering semi-structured interviews with therapists familiar with telerehabilitation or outpatient neurorehabilitation.24 Probing questions were asked to improve the depth of understanding of the care delivery process. Therapists assigned appropriate actors and approximate minutes spent on each task of their respective flowcharts. Previously collected timestamps and respective flowcharts were also presented to therapists for comparison and validation. Additionally, therapists provided information for actors and tasks done outside of the session but that are still directly related to the care delivery (ex. phone calls to schedule appointments and extra documentation time at the end of a workday). Handwritten flowcharts were updated with therapist feedback.
After the draft of the flowchart was updated, therapists were re-consulted to individually validate the flowcharts where suggestions for changes were discussed. This iterative process was continued until a consensus was reached among therapists as to the average process flow.
2.4. Labor wage calculations
Labor statistics were gathered from the 2020 U.S. Bureau of Labor Statistics and included median hourly salary for all actors identified in the interviews.27 All currency reported in this study are in 2020 US dollars (USD). Medians were used instead of means so the assigned cost weights would not be skewed right by extremely high outliers. Median annual salaries were determined by median hourly wages multiplied by an assumed 40 hours per week for 52 weeks. A median loaded salary was calculated by adding 35% to the median annual salary to include fringe benefits (i.e., health insurance).28 Median costs per minute were then calculated by dividing the median loaded salary by 2080 yearly hours then further divided by 60 minutes. Per minute costs are essential for TDABC as they provide an estimated cost per actor for each phase of the care delivery flowchart. This resulted in data to compare costs and improve care delivery efficiency. All descriptive statistics were computed with Microsoft Excel.
2.5. Flowchart mapping and cost comparison
The final care delivery flowcharts for evaluations for both outpatient and telerehabilitation sessions (Figures 1 and 2) were mapped with LucidChart software (Lucid Software Inc.; South Jordan, Utah). Actors are differentiated in flowcharts by different colors for improved readability. Total costs for both flowcharts were calculated and compared to define cost differences between outpatient and telerehabilitation services. Tasks, minutes, and actors’ per-minute costs for both telerehabilitation and outpatient sessions were compiled into a table. Minutes spent for each task were multiplied by actors’ per-minute costs and summed to estimate total cost for each session type. Marginal cost was calculated as the total cost of a telerehabilitation visit minus the total cost of a traditional outpatient rehabilitation.
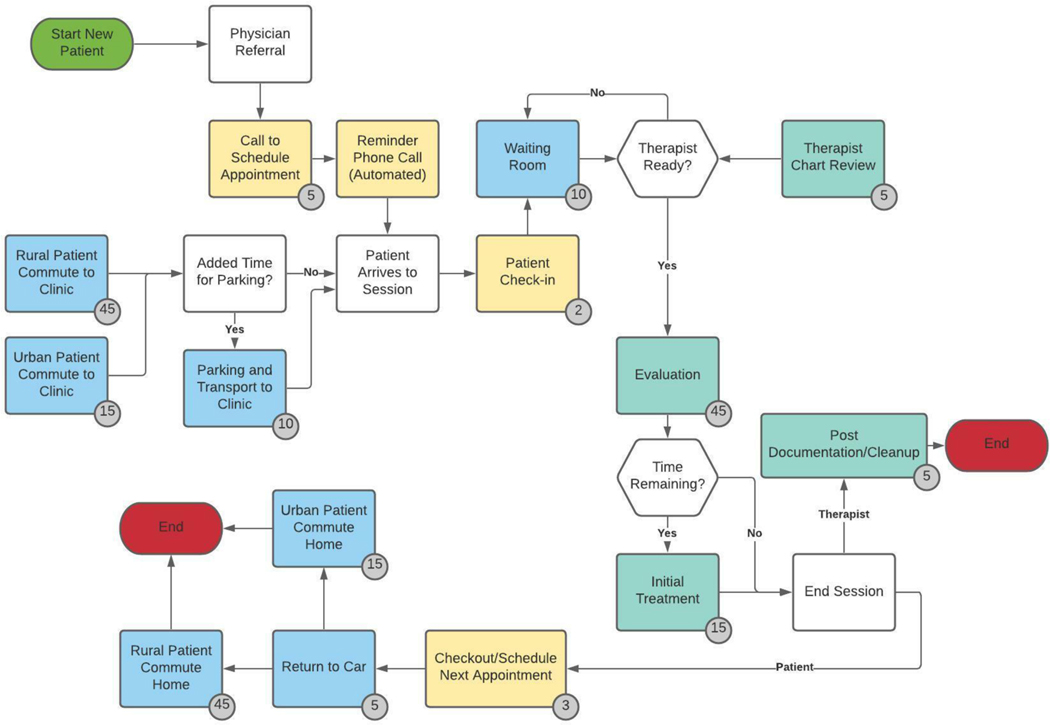
Figure 1:
TDABC flowchart of an outpatient therapy evaluation: Arrows indicate the flow of the care delivery process. Boxes are color coordinated to represent actors. Yellow boxes represent a clerical/patient interaction. Blue boxes represent only patient time. Green boxes represent therapist time.
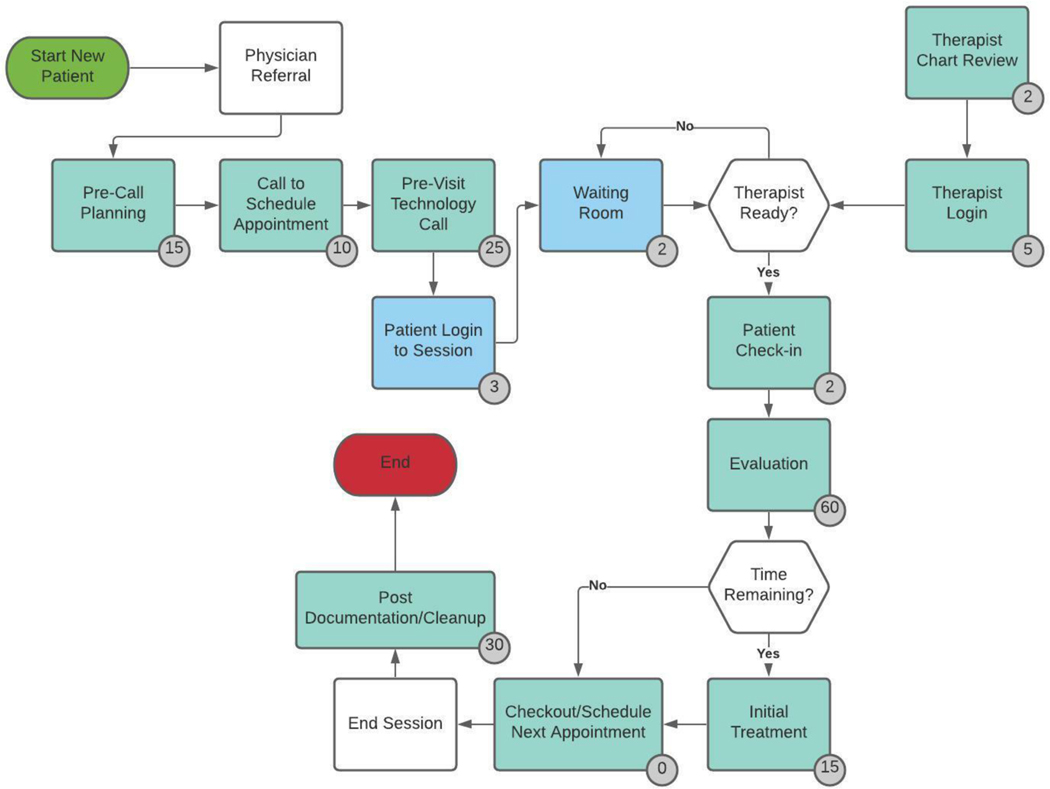
Figure 2:
TDABC flowchart of an outpatient therapy evaluation: Arrows indicate the flow of the care delivery process. Boxes are color coordinated to represent actors. Blue boxes represent only patient time. Green boxes represent therapist time.
3. Results
3.1. Actor identification
The purpose of this study was to define the care delivery process and estimate the marginal cost differences between a telerehabilitation versus outpatient session for stroke survivors. Observers and therapist interviewees identified the actors involved in the care delivery flow for outpatient therapy. These included occupational therapists (OTs), certified occupational therapy assistants (COTA), support staff (clerical), and the patient. Outpatient therapists also mentioned clerical staff. For telerehabilitation, all therapists mentioned they do not have a secretary and perform all clerical duties.
3.2. Wage calculations
The identification of all actors during session observations allowed for the calculation of specific labor wages. National data of labor wages for all actors were collected (Table 1).27 For therapists, base median hourly salaries were: OT ($41.48), and COTA ($30.26). Annual median salaries were OT ($86,278) and COTA ($62,940). With the addition of a 35% increase for fringe benefits, loaded salaries were: OT ($116,476) and COTA ($84,970) based on typical practice standards. Productivity standards were assumed to be 83% for OTs and 90% for COTAs. This number was multiplied by 2080 (assumed full-time hours for one year) to determine productive hours. Productive hours were then used to calculate per minute costs for each employee. Cost per minute for each therapist were: OT ($1.12) and COTA ($0.76).
Table 1.
Labor Wages
| Hourly | Annual | Minute | ||||
|---|---|---|---|---|---|---|
| Occupation Title | Median | Mean | Median | Fringe Benefits | Loaded Salary | Cost/Min |
| All Occupations | $20.17 | $27.07 | $41,953 | $14,684 | $56,637 | $0.57 |
| Occupational Therapists | $41.48 | $42.06 | $86,278 | $30,197 | $116,476 | $1.12 |
| Occupational Therapy Assistants |
$30.26 | $30.49 | $62,940 | $22,029 | $84,970 | $0.76 |
| Medical Secretaries | $17.96 | $18.75 | $37,356 | $13,075 | $50,432 | $0.51 |
| Computer User Support Specialists |
$25.33 | $27.40 | $52,686 | $18,440 | $71,127 | $0.71 |
Both clerical and patient hours were calculated at 80% productivity. Patients’ wages were calculated as the national average for all occupations. This came out for patients as: $20.17 (median hourly), $41,954 (median yearly), $56,637 (loaded salary), and $0.57 (cost per minute). Clerical staff wages were: $17.96 (median hourly), $37,356 (median yearly), $50,431 (loaded salary), and $0.51 (cost per minute).
3.3. Phase identification, flowchart creation, and final cost comparisons
Next, observers and therapist interviewees identified the main task phases of the care delivery flow for telerehabilitation outpatient therapy (Table 2). The phases were identified in order as: call to schedule appointment; transportation/parking; check in/chart review; evaluation/treatment; schedule follow up, clean-up/documentation; and patient transportation home. Technical difficulties for patients and clinicians included internet connectivity, equipment (ex. webcam or microphone), or software failure (ex. program crashed). These were not included in the flowchart as they were inconsistent and occurred spontaneously during different times of the session. However, we tested this in a sensitivity analysis and the range goes from $225.41 with 0 technical problems to $231.64 with an average of 3.7 mins for technical problems.
Table 2.
Outpatient versus telerehabilitation evaluation cost comparison
| Outpatient | Telerehabilitation | |||||
|---|---|---|---|---|---|---|
| Phase | Description | OT | Clerical | Patient | OT | Patient |
| Phase 1 | Call to schedule initial/confirm next (minutes) | 0 | 5 | 5 | 50 | 35 |
| Phase 2 | Transportation/parking (minutes) | 0 | 0 | 42 | 0 | 0 |
| Phase 3 | Check in/chart review (minutes) | 5 | 2 | 2 | 9 | 7 |
| Phase 4 | Evaluation/treatment (billable) (minutes) | 45 | 0 | 45 | 60 | 60 |
| Phase 5 | Schedule follow up (minutes) | 0 | 3 | 3 | 0 | 0 |
| Phase 6 | Clean up/documentation (minutes) | 5 | 0 | 0 | 30 | 0 |
| Phase 7 | Transportation home (minutes) | 0 | 0 | 37 | 0 | 0 |
| Total mins/actor | 70 | 10 | 149 | 149 | 102 | |
| Cost/min | $1.12 | $0.51 | $0.57 | $1.12 | $0.57 | |
| Actor cost/session | $78.71 | $5.05 | $84.52 | $167.54 | 57.86 | |
| Technical difficulties time Cost |
0 $0.00 |
3.7 mins $6.23 |
||||
| Total cost/session | $168.29 | $231.64 | ||||
Final evaluation flowcharts can be found in Figures 1 and 2 for traditional rehabilitation therapy evaluation and telerehabilitation evaluation respectively. Overall, telerehabilitation ($231.64) was more costly than outpatient therapy ($168.29) per session, resulting in a marginal cost difference of $63.35. Primary time drivers of this finding were initial phone call (0 mins for outpatient therapists versus 35 mins for telerehabilitation) and post documentation (5 mins for outpatient versus 30 mins for telerehabilitation) demands for telerehabilitation (Table 2). Interviewees described a lack of electronic health record integration with telerehabilitation as one of the reasons for increased post-session documentation. Additionally, technical difficulties were responsible for a mean of 3.7 minutes (SD=4.6) lost per session for both patients and clinicians. When multiplied by the cost per minute of a computer user support specialist, this equates to an average of $6.23 per session.
4. Discussion
To our knowledge, this is the first attempt to define the care delivery process and compare the resulting marginal costs for telerehabilitation versus outpatient therapy. In contrast to our hypothesis and findings from other studies16,20, this project found that telerehabilitation was more costly than traditional outpatient therapy. It is likely that our results reflect that outpatient therapy, as a longstanding traditional standard of practice model, has been streamlined, while in contrast, telerehabilitation is new and without standards of practice. At this time, outpatient therapy may be less costly because therapist work time is maximized in reimbursable activities. However, telerehabilitation is an emerging platform with the potential to reduce costs, improve healthcare inequities, and increase therapy intensity to facilitate better patient outcomes given opportunities for system learning toward improvements in process efficiency. To advance telerehabilitation efficiency, the results of this project stress 3 potential areas of improvement: 1) documentation practices, 2) staffing, and 3) technology.
4.1. Documentation practices
Telerehabilitation therapist interviewees mentioned long periods of unbillable time required to complete post session documentation (Table 2). This may be very specific to the observed sites, but this lost time was due to the inefficient methodology of scoring clinical assessments in paper form and then spending the time to manually upload the forms into the electronic health records (EHR). In outpatient therapy, this lost productivity time has been reduced by improved clinical assessment integration into the EHR. Therapists can enter and sign assessment outcomes electronically to skip the unnecessary practice of printing and scanning these documents. This may become more commonly available as more rehabilitation assessments are validated for virtual use.29
4.2. Staffing
The telerehabilitation therapists in this project also mentioned spending nonbillable time that is traditionally not performed by therapists. Therapists’ time spent on scheduling appointments and teaching patients how to use telerehabilitation software and technology could be streamlined to lower paid personnel or through recorded instructions to improve therapist productivity and maximize cost savings.30 This finding is consistent with previous literature noting increases in consultation time with telerehabilitation approaches to care delivery.20 In contrast, outpatient rehabilitation utilizes clerical staff to schedule and handle administrative responsibilities which allows therapists to spend more time in reimbursable activities. Additionally, for therapy documents that are not integrated into the EHR, outpatient therapists have additional clerical staff support who can upload the documents so as not to reduce therapist productivity.
4.3. Technology
Technical difficulties and digital literacy must be considered to improve patient and therapist adoption. Limited access to technology and internet connectivity are major barriers to telehealth use.31 In particular, older patients consider the technical performance, user effort, and perceived digital privacy and security when deciding to use telehealth.32 Improved user interfaces and patient education on troubleshooting and increasing computer literacy may help to reduce the impact of these difficulties. By default, outpatient therapists do not have technology barriers with the delivery of a session. However, they also have clerical support to help troubleshoot issues with computers and rehabilitation equipment.
Additionally, examining technology and processes related to other successful uses of telerehabilitation that have been in use longer may help improve care delivery. For example, pediatric therapists have pioneered the use of telerehabilitation to improve access for school-aged patients.33,34 Learning from their success and struggles may help accelerate the adoption process and improve reimbursement.
Study Limitations
Some limitations of these project findings exist. Our focus was on improving the process of telerehabilitation for stroke survivors. Though some of the patients had other neurological disorders, the results may not be generalizable to other conditions. It is important to note that we did not assess the content of the evaluation/treatment for patients, just the care delivery process. For example, specific clinical assessments may differ for stroke survivors and patients with multiple sclerosis. However, it is the authors’ opinions that the logistics of the care delivery process (outside of billable time) such as transportation, appointment check in, and documentation time are not likely to vary between these populations. This general approach to assessing care delivery for multiple diagnoses has been done for outpatient clinics35 and pre-operative centers.36 Therapists interviewed were local to South Carolina and, therefore, results may not be generalizable to other clinics, regions of the United States, or other countries. Reimbursement for different tasks in the flowcharts may differ in other countries. This project was focused on individual sessions and aggregate costs may differ. Additionally, we feel that though evaluation and treatment approaches are much different for OT and PT, the logistical care delivery processes are not significantly different. Further research could examine this further to observe possible differences (i.e., documentation speed).
This project did not include overhead costing as our purpose was to help improve workflow efficiency. Future studies should compare overhead costs of telerehabilitation and outpatient therapy. Facility operations can vary greatly by region and size of practice. Additionally, telerehabilitation practice likely vary greatly depending on the types of software used and size of the company providing services. It is important to remember this research represents a simplification of reality for process improvement purposes; facility-specific analysis is recommended to compare local costs. Salaries are based on national averages but will vary significantly based on local salaries for both patients and staff. This study did not compare rural and urban patients, although costs for transportation time was not influential enough to make the telerehabilitation session less costly in this case. This study also did not include the costs of parking as this can be highly variable depending on the facility type and location nor did it include hotel accommodations for patients having to travel extra-long distances. This study did not account for missed visits, though this has been explored generally in telehealth previously37 and compliance with care has been previously reported as comparable.16 Finally, the cost of milage is $0.16 per mile for medical care which was also not included in this analysis as we were focused on time not distance.38 The relationship between time and distance driven would vary dramatically depending on if the outpatient facility is urban or rural.
Conclusions
Telerehabilitation is an emerging service delivery model for adult stroke survivors that has the potential to reduce social disparities and improve access to care. However, improvements in the delivery are necessary to advance efficiency and promote widespread adoption. Maximizing the time therapists spend with patients in therapy and minimizing nonbillable time will dramatically improve costs. Additional cost studies should be performed to examine alternative forms of telerehabilitation such as asynchronous training and group therapy as well as overhead cost differences.
Funding:
This publication was supported, in part, by the National Center for Advancing Translational Sciences of the National Institutes of Health under Grant Numbers TL1 TR001451 and the UL1 TR001450. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. This publication was supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) as part of the National Telehealth Center of Excellence Award (U66 RH31458-01-00). Data analytic support for the study was provided through the CEDAR core funded by the MUSC Office of the Provost and by the South Carolina Clinical and Translational Research (SCTR) Institute, with an academic home at the Medical University of South Carolina, through NIH grant number UL1 RR029882. The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement, by HRSA, HHS, or the U.S. Government.
Abbreviations
- TDABC
Time-driven activity-based costing
- OT
Occupational therapy
- CCR
cost to charge ratio
- ABC
activity-based costing
- RVU
relative value units
- COTAs
certified occupational therapy assistants
- USD
US dollars
Footnotes
Conflictions of Interest Statement: None of the authors report any conflicts of interest for this manuscript and project.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Nalleballe K, Brown A, Sharma R, et al. When Telestroke Programs Work, Hospital Size Really Does Not Matter. J Neurosci Rural Pract. 2020;11(3):403–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Harkey LC, Jung SM, Newton ER, Patterson A. Patient Satisfaction with Telehealth in Rural Settings: A Systematic Review. Int J Telerehabil. 2020;12(2):53–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Müller-Barna P, Hubert GJ, Boy S, et al. TeleStroke Units Serving as a Model of Care in Rural Areas. Stroke. 2014;45(9):2739–2744. [DOI] [PubMed] [Google Scholar]
- 4.Joubert J, Prentice LF, Moulin T, et al. Stroke in rural areas and small communities. Stroke. 2008;39(6):1920–1928. [DOI] [PubMed] [Google Scholar]
- 5.Jia H, Cowper DC, Tang Y, Litt E, Wilson L. Postacute stroke rehabilitation utilization: are there differences between rural-urban patients and taxonomies? J Rural Health. 2012;28(3):242–247. [DOI] [PubMed] [Google Scholar]
- 6.Lohse KR, Lang CE, Boyd LA. Is more better? Using metadata to explore dose-response relationships in stroke rehabilitation. Stroke. 2014;45(7):2053–2058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jeffers MS, Karthikeyan S, Gomez-Smith M, et al. Does Stroke Rehabilitation Really Matter? Part B: An Algorithm for Prescribing an Effective Intensity of Rehabilitation. Neurorehabil Neural Repair. 2018;32(1):73–83. [DOI] [PubMed] [Google Scholar]
- 8.Lang CE, Macdonald JR, Reisman DS, et al. Observation of amounts of movement practice provided during stroke rehabilitation. Arch Phys Med Rehabil. 2009;90(10):1692–1698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cramer SC, Dodakian L, Le V, et al. Efficacy of Home-Based Telerehabilitation vs In-Clinic Therapy for Adults After Stroke: A Randomized Clinical Trial. JAMA Neurol. 2019;76(9):1079–1087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Richmond T, Peterson C, Cason J, et al. American Telemedicine Association’s Principles for Delivering Telerehabilitation Services. Int J Telerehabil. 2017;9(2):63–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Laver KE, Adey-Wakeling Z, Crotty M, Lannin NA, George S, Sherrington C. Telerehabilitation services for stroke. Cochrane Database Syst Rev. 2020;1(1):Cd010255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Linder SM, Rosenfeldt AB, Bay RC, Sahu K, Wolf SL, Alberts JL. Improving Quality of Life and Depression After Stroke Through Telerehabilitation. Am J Occup Ther. 2015;69(2):6902290020p6902290021–6902290020p6902290010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tchero H, Tabue Teguo M, Lannuzel A, Rusch E. Telerehabilitation for Stroke Survivors: Systematic Review and Meta-Analysis. J Med Internet Res. 2018;20(10):e10867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Burgos PI, Lara O, Lavado A, et al. Exergames and Telerehabilitation on Smartphones to Improve Balance in Stroke Patients. Brain Sci. 2020;10(11). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Standing C, Standing S, McDermott M-L, Gururajan R, Kiani Mavi R. The Paradoxes of Telehealth: a Review of the Literature 2000–2015. Systems Research and Behavioral Science. 2018;35(1):90–101. [Google Scholar]
- 16.Howes S, Stephenson A, Murphy P, et al. Factors influencing the delivery of telerehabilitation for stroke: A systematic review. Physiotherapy. 2022;114:e90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lloréns R, Noé E, Colomer C, Alcañiz M. Effectiveness, usability, and cost-benefit of a virtual reality-based telerehabilitation program for balance recovery after stroke: a randomized controlled trial. Arch Phys Med Rehabil. 2015;96(3):418–425.e412. [DOI] [PubMed] [Google Scholar]
- 18.Rodgers H, Howel D, Bhattarai N, et al. Evaluation of an Extended Stroke Rehabilitation Service (EXTRAS) A Randomized Controlled Trial and Economic Analysis. Stroke. 2019;50(12):3561–3568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tousignant M, Boissy P, Corriveau H, Moffet H. In home telerehabilitation for older adults after discharge from an acute hospital or rehabilitation unit: A proof-of-concept study and costs estimation. Disability and Rehabilitation: Assistive Technology. 2006;1(4):209–216. [DOI] [PubMed] [Google Scholar]
- 20.Kairy D, Lehoux P, Vincent C, Visintin M. A systematic review of clinical outcomes, clinical process, healthcare utilization and costs associated with telerehabilitation. Disabil Rehabil. 2009;31(6):427–447. [DOI] [PubMed] [Google Scholar]
- 21.Gapenski LC, Reiter KL. Healthcare finance : an introduction to accounting & financial management / Gapenski Louis C., Reiter Kristin L.. Sixth edition. ed. Chicago, Illinois;: Health Administration Press; 2016. [Google Scholar]
- 22.Keswani A, Sheikholeslami N, Bozic KJ. Value-based Healthcare: Applying Time-driven Activity-based Costing in Orthopaedics. Clinical Orthopaedics and Related Research®. 2018;476(12):2318–2321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kaplan RS, Witkowski M, Abbott M, et al. Using time-driven activity-based costing to identify value improvement opportunities in healthcare. J Healthc Manag. 2014;59(6):399–412. [PubMed] [Google Scholar]
- 24.Keel G, Savage C, Rafiq M, Mazzocato P. Time-driven activity-based costing in health care: A systematic review of the literature. Health Policy. 2017;121(7):755–763. [DOI] [PubMed] [Google Scholar]
- 25.Dooley M, Simpson A, Williams D, Cristaldi K, McElligot J, Nietert P, Simpson K A modification of time-driven activity-based costing for comparing cost of telehealth and in-person visits. Telemedicine and e-Health. 2021;In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Etges A, Polanczyk CA, Urman RD. A standardized framework to evaluate the quality of studies using TDABC in healthcare: the TDABC in Healthcare Consortium Consensus Statement. BMC Health Serv Res. 2020;20(1):1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Statistics UBoL. Occupational Employment and Wage Statistics. https://www.bls.gov/oes/current/oes_nat.htm. Accessed 01/05/2022.
- 28.Silvestre JH, Ulrich BT, Johnson T, Spector N, Blegen MA. A multisite study on a new graduate registered nurse transition to practice program: Return on investment. Nurs Econ. 2017;35(3):110. [Google Scholar]
- 29.Almubark BM, Majrashi N, Alghusun N, Alhammad M, Alhthifi F, Alyahya RSW. Telehealth Clinical Practice Guide for Occupational Therapy, Physical Therapy, and Speech and Language Pathology: A Saudi and Middle Eastern Guide. Telemed J E Health. 2021. [DOI] [PubMed] [Google Scholar]
- 30.Sperl T, Ptacek R, Trewn J. The Practical Lean Six Sigma Pocket Guide for Healthcare: Tools for the Elimination of Wastes in Hospitals, Clinics, and Physician Group Practices. MCS Media, Incorporated; 2013. [Google Scholar]
- 31.Unni EJ, Patel K, Beazer IR, Hung M. Telepharmacy during COVID-19: A Scoping Review. Pharmacy (Basel). 2021;9(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.van Houwelingen CT, Ettema RG, Antonietti MG, Kort HS. Understanding Older People’s Readiness for Receiving Telehealth: Mixed-Method Study. J Med Internet Res. 2018;20(4):e123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cason J Telehealth: a rapidly developing service delivery model for occupational therapy. Int J Telerehabil. 2014;6(1):29–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cason J Telehealth and Occupational Therapy: Integral to the Triple Aim of Health Care Reform. Am J Occup Ther. 2015;69(2):6902090010p6902090011–6902090010p6902090018. [DOI] [PubMed] [Google Scholar]
- 35.Demeere N, Stouthuysen K, Roodhooft F. Time-driven activity-based costing in an outpatient clinic environment: Development, relevance and managerial impact. Health Policy. 2009;92(2):296–304. [DOI] [PubMed] [Google Scholar]
- 36.French KE, Albright HW, Frenzel JC, et al. Measuring the value of process improvement initiatives in a preoperative assessment center using time-driven activity-based costing. Healthcare. 2013;1(3):136–142. [DOI] [PubMed] [Google Scholar]
- 37.Covert LT, Slevin JT, Hatterman J. The Effect of Telerehabilitation on Missed Appointment Rates. Int J Telerehabil. 2018;10(2):65–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Service IR. Standard Mileage Rates. Internal Revenue Service. Published 2021. Accessed 11/29/2021. [Google Scholar]