Abstract
Candidate foot-and-mouth disease (FMD) DNA vaccines designed to produce viral capsids lacking infectious viral nucleic acid were evaluated. Plasmid DNAs containing a portion of the FMDV genome coding for the capsid precursor protein (P1-2A) and wild-type or mutant viral proteinase 3C (plasmids P12X3C or P12X3C-mut, respectively) were constructed. Cell-free translation reactions programmed with pP12X3C (wild-type 3C) and pP12X3C-mut produced a capsid precursor, but only the reactions programmed with the plasmid encoding the functional proteinase resulted in P1-2A processing and capsid formation. Baby hamster kidney (BHK) cells also produced viral capsid proteins when transfected with these plasmids. Plasmid P12X3C was administered to mice by intramuscular, intradermal, and epithelial (gene gun) inoculations. Anti-FMD virus (FMDV) antibodies were detected by radioimmunoprecipitation (RIP) and plaque reduction neutralization assays only in sera of mice inoculated by using a gene gun. When pP12X3C and pP12X3C-mut were inoculated into mice by using a gene gun, both plasmids elicited an antibody response detectable by RIP but only pP12X3C elicited a neutralizing antibody response. These results suggest that capsid formation in situ is required for effective immunization. Expression and stimulation of an immune response was enhanced by addition of an intron sequence upstream of the coding region, while addition of the FMDV internal ribosome entry site or leader proteinase (L) coding region either had no effect or reduced the immune response.
Foot-and-mouth disease (FMD) is a highly contagious viral disease of cloven-hoofed animals, including pigs and cattle. Current FMD vaccines based on inactivated virus are effective (7), but outbreaks of FMD have been directly associated with incomplete inactivation of virus or the escape of virus from vaccine manufacturing facilities (4, 20). In addition, animals given these vaccines exhibit serotype-specific immunity and short-term protection from challenge (2). Alternative formats have been investigated by laboratories worldwide to develop new FMD vaccines which are both safe and effective.
In FMD virus (FMDV)-infected cells, a polyprotein is synthesized from genomic RNA and processed by viral proteinases into four primary cleavage products, leader (L) proteinase, P1-2A, P2, and P3 (33, 35). Concomitantly, myristoylation at the amino terminus of P1-2A, which is essential for efficient capsid assembly, occurs (1, 22). Viral proteinase 3C subsequently processes the structural protein precursor P1-2A into capsid proteins VP0, VP3, and VP1 and nonstructural peptide 2A (35). Capsid assembly is accompanied by production of other structures, including pentamers, which contain five copies of VP0, VP3, and VP1, and empty capsids, which contain 60 copies of each protein but lack viral RNA. Noninfectious provirions consist of RNA, VP0, VP1, and VP3, and cleavage of VP0 to VP4 and VP2, by an unknown mechanism, results in conversion of provirions to mature virions (21, 33). Immunological studies have identified linear and conformational sites that are present on both empty capsids and virions (13, 18, 32), and antisera raised against empty capsids have serological specificity which is indistinguishable from that of sera prepared against virions (34).
This information has led to efforts to develop subunit vaccines based on cDNA constructs containing the P1-2A and 3C regions of the viral genome (1, 23). We have shown that three out of four swine inoculated with extracts from Escherichia coli transformed with a construct containing P1-2A and 3C coding regions were protected from challenge by contact with an FMDV-infected animal (17). However, E. coli does not have the enzyme required for protein myristoylation (14) and the 3C proteinase is toxic for cells in this and other systems (1, 23, 31), making it difficult to produce large amounts of processed capsid structures.
To overcome these problems, we have developed a DNA inoculation-based strategy designed to produce capsids in inoculated animals. The P12X3C cassette, which contains FMDV serotype A12 sequences, including the complete P1, 2A, and 3C coding regions and partial 2B and 3B coding regions flanked by AUG and UAG codons, was cloned into pcDNA3 (Invitrogen, La Jolla, Calif.) downstream of the cytomegalovirus and T7 promoters. Plasmid P12X3C-mut was constructed by replacing a portion of the 3C coding region of pP12X3C with cDNA containing a mutation at the active site of 3C (cysteine to glycine at amino acid 163 [C163G]), from plasmid pT7-3CC163G (19). Plasmid pcDNA3-β-gal, which contains the complete β-galactosidase coding region, was provided by Brad Bissell and was used as a control plasmid.
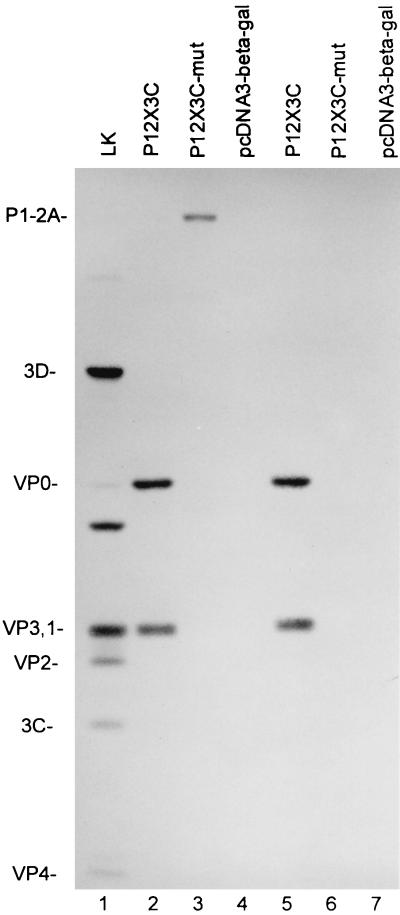
Plasmids were transcribed and translated in a T7 RNA polymerase TNT cell-free system (Promega, Madison, Wis.), and the products were examined by sodium dodecyl sulfate (SDS)-polyacrylamide gel electrophoresis or immunoprecipitated prior to gel analysis. Proteolytic processing of P1 to VP0, VP3, and VP1 and synthesis of mature 3C were detected in extracts programmed with pP12X3C (data not shown). The assembly of these antigens was also confirmed, since all three capsid proteins were immunoprecipitated by VP1-specific monoclonal antibodies (MAbs) 6FF5.1.3 and 6EE2.1.2 (Fig. 1, lanes 2 and 5). In extracts programmed with pP12X3C-mut, processed capsid proteins were not detected; however, a 91-kDa product equivalent to the size expected of an unprocessed P1-2A precursor was immunoprecipitated by MAb 6FF5.1.3, which recognizes an epitope within the G-H loop of VP1 (Fig. 1, lane 3), but not by MAb 6EE2.1.2, which recognizes an epitope at the carboxy terminus of VP1 (Fig. 1, lane 6) (3, 30). Although the autoradiograms prepared from the immunoprecipitated products show that more radiolabeled capsid antigen was recovered from reactions programmed with pP12X3C, quantitation of the FMDV products present in transcription-translation reactions resolved on SDS-containing gels (analyzed by using an image quantitation program [ImageQuant version 3.3; Molecular Dynamics, San Jose, Calif.]) showed that both plasmids were as efficient at producing viral antigen. Expression of the FMDV cassettes driven by the cytomegalovirus promoter was tested by transfecting BHK cells with Lipofectin (Life Technologies, Gaithersburg, Md.). Viral antigens were detected by immunoperoxidase staining using MAb 6FF5.1.3 in similar numbers of cells transfected with either pP12X3C or pP12X3C-mut but were detected by immunoperoxidase staining using MAb 6EE2.1.2 only in cells transfected with pP12X3C (data not shown).
FIG. 1.
Autoradiogram showing viral proteins immunoprecipitated from pP12X3C, pP12X3C-mut, and pcDNA3-β-gal programmed cell-free reaction mixtures. The [35S]methionine-labeled antigens were immunoprecipitated with MAb 6FF5.1.3 (lanes 2 to 4) or with MAb 6EE2.1.2 (lanes 5 to 7). Lane 1, immunoprecipitation of [35S]methionine-labeled FMDV-infected lamb kidney cell cytoplasmic extract with convalescent serum from an FMDV-infected bovine. The products were resolved by SDS-polyacrylamide gel electrophoresis on a 15% gel.
To evaluate methods of DNA delivery, groups of five mice were inoculated with pP12X3C and pcDNA3-β-gal twice, at 3-week intervals, by the intradermal (i.d.) or intramuscular (i.m.) route or once or twice by using a gene gun (g.g.). One hundred micrograms of plasmid in 50 μl of phosphate-buffered saline was used for each i.d. or i.m. inoculation. Each g.g. inoculation consisted of two shots containing a total of 1 μg of DNA coupled to gold particles and was delivered by the PowderJect-XR delivery system as described previously (29). An antibody response, assayed by plaque reduction neutralization (PRN) assay and radioimmunoprecipitation (RIP), was detected only in mice inoculated twice with pP12X3C by g.g. (Table 1, groups 1 to 4 and 7 to 10).
TABLE 1.
Antibody response to DNA vaccination
| Group no. | DNA vaccinationa
|
Group PRN50 (individuals)b | Group RIP (individuals)c | ||
|---|---|---|---|---|---|
| Route | Plasmid | No. | |||
| 1 | i.d. | pcDNA3-βgal | 2× | − | − |
| 2 | i.m. | pcDNA3-βgal | 2× | − | − |
| 3 | g.g. | pcDNA3-βgal | 1× | − | − |
| 4 | g.g. | pcDNA3-βgal | 2× | − | − |
| 5 | g.g. | pP12X3C-mut | 1× | − | − |
| 6 | g.g. | pP12X3C-mut | 2× | − (−, −, −, −, −) | + (+, −, −, −, +) |
| 7 | i.d. | pP12X3C | 2× | − | − |
| 8 | i.m. | pP12X3C | 2× | − | − |
| 9 | g.g. | pP12X3C | 1× | − | − |
| 10 | g.g. | pP12X3C | 2× | 1.9 (2.5, 2.2, −, −, 1.9) | + (+, +, +, −, +) |
| 11 | g.g. | piP12X3C | 1× | − (−, −, −d, −e, −) | + (−, +, −, +, −) |
| 12 | g.g. | piP12X3C | 2× | 2.5 (2.6, −, 2.2, 2.6, 2.5) | + (+, −, +, +, +) |
| 13 | g.g. | pIRESP12X3C | 1× | − | − |
| 14 | g.g. | pIRESP12X3C | 2× | − (−, −, −, −, −) | + (+, −, −, +, −) |
| 15 | g.g. | piIRESP12X3C | 1× | − (−, −, −, −, −f) | + (+, +, −, −, −) |
| 16 | g.g. | piIRESP12X3C | 2× | 1.9 (2.2, 2.2, −, >2.8, 2.3) | + (+, +, −, +, +) |
| 17 | g.g. | pIRESLP12X3C | 1× | − | − |
| 18 | g.g. | pIRESLP12X3C | 2× | − | − |
| 19 | g.g. | piIRESLP12X3C | 1× | − | − |
| 20 | g.g. | piIRESLP12X3C | 2× | − | − |
Groups of five mice were inoculated once (1×) or twice (2×) i.d., i.m., or epithelially (g.g.) with the indicated plasmid.
Log of PRN50. Serum samples were tested at a 1:4 starting dilution for pooled samples (1:20 for each individual) and at a 1:20 starting dilution for individual samples. −, no neutralization was detected at the highest concentration tested.
Tested at a 1:4 dilution for pooled samples (1:20 for each individual in pool) and at a 1:20 dilution for individual samples. +, viral proteins visible on autoradiogram; −, no viral proteins visible on autoradiogram.
Starting dilution, 1:200.
Starting dilution, 1:25.
Starting dilution, 1:62.
Comparisons of the immune response achieved following inoculation with pP12X3C or pP12X3C-mut by g.g. revealed that both plasmids were capable of inducing an antibody response as determined by RIP (Table 1), although responses to pP12X3C were stronger in most animals that seroconverted after inoculation with this plasmid (data not shown). Interestingly, only the plasmid encoding a functional 3C proteinase was able to elicit antibodies that neutralize the virus (Table 1, groups 6 and 10). These findings, in conjunction with the results from cell-free translation and BHK cell transfection, which show that both plasmids express similar quantities of protein, suggest that the antigen responsible for stimulating a neutralizing antibody response in pP12X3C-inoculated animals consists of capsids. Nevertheless, we cannot exclude the possibility that differences in stability or processing of these two antigens in vivo could account for the observed differences in immunogenicity.
In an attempt to increase the expression level of FMDV capsid proteins and enhance the immune response in animals, plasmid P12X3C was modified to include an intron and the FMDV internal ribosome entry site (IRES) upstream of the P1 coding region. The addition of an intron has been shown to increase the expression level of plasmids in mammalian cells, presumably by facilitating the movement of mRNA from nucleus to cytoplasm (9, 28). The FMDV IRES was added to the construct to determine if cap-independent translation directed by the IRES would result in higher levels of protein expression. The IRES was added to the construct with or without the L coding region. The L proteinase shuts off host cell mRNA translation (12), which could result in enhanced expression of the FMDV cassette regulated by the IRES. A chimeric intron obtained from plasmid pCI (Promega) was inserted upstream of the P1 coding region of pP12X3C to produce piP12X3C. The IRES of FMDV type A12 with or without the L coding region was placed upstream of the P1 coding region of pP12X3C or between the intron and P1 coding region of piP12X3C to produce pIRESLP12X3C or pIRESP12X3C and piIRESLP12X3C or piIRESP12X3C, respectively.
All modified plasmids, including piP12X3C, pIRESP12X3C, piIRESP12X3C, pIRESLP12X3C, and piIRESLP12X3C, expressed FMDV proteins as demonstrated by cell-free transcription-translation and BHK cell transfection (data not shown). Interestingly, immunoperoxidase staining showed that cells transfected with plasmids carrying the L coding region (pIRESLP12X3C and piIRESLP12X3C) exhibited cytopathic effects. This phenomenon is consistent with the expected cytotoxicity of the L proteinase, which shuts off host mRNA translation by cleavage of the translation initiation factor eIF-4G in transfected cells (12).
The results from g.g. inoculation of these plasmids in mice demonstrated that the addition of an intron to the plasmids resulted in an enhanced antibody response. Mice inoculated with pP12X3C carrying an intron (piP12X3C) developed RIP antibodies after only one inoculation, although two inoculations were required for the development of neutralizing antibodies (Table 1, groups 11 and 12). Addition of the IRES alone appeared to negatively affect the performance of pP12X3C (Table 1, groups 10 and 14) and had little effect on piP12X3C (Table 1, groups 11, 12, 15, and 16), suggesting that in this context internal initiation of translation was not superior to scanning from the 5′ end of mRNA. The presence of the L coding region in any of the plasmids was detrimental to the induction of an immune response (Table 1, groups 17 to 20). We hypothesize that the cytotoxic effect of the L proteinase on transfected cells (as seen in cell culture) resulted in both decreased protein production and duration of antigen presentation in animals.
This study has demonstrated that delivery of an FMDV cDNA construct containing the P1-2A and 3C coding regions as a DNA vaccine results in the assembly of FMDV capsid structures and that these plasmids are capable of inducing a neutralizing antibody response in mice. These results support immunological studies demonstrating the broad serological specificity of cell culture-derived empty capsids (13, 18, 32) and encourage the continued development of this approach as a potentially viable alternative to inactivated virus vaccines. Introduction of the P1-2A and 3C cassettes directly into animals appears to avoid observed problems of 3C cytotoxicity which have hampered other empty-capsid approaches (see above). However, the toxicity of 3C could adversely affect antigen production from transfected cells of vaccinated animals as well.
We have recently shown that a fundamentally different type of DNA vaccine, based on production of attenuated full-length viral genomes in inoculated animals can also stimulate an anti-FMDV immune response (36). The DNA vaccine candidate presented here has some safety advantages over the construct developed by Ward et al. (36), since only empty viral particles are synthesized in vaccinated animals. In addition, animals inoculated with piP12X3C, which lacks the coding regions for several nonstructural viral proteins, can be distinguished from virus-infected animals, which show immune responses to these antigens (5, 24). DNA vaccines of both types have the advantage that they can be readily altered to include the P1 coding region of new field isolates. This allows production of updated vaccines without the requirement for cell culture-adaptation, which is needed to produce traditional vaccines from field isolates and which is known to result in production of antigenic variants (6, 16).
Preliminary experiments in swine inoculated with plasmids encoding FMDV empty capsids have yielded variable results. In one experiment a swine was inoculated with pP12X3C by using a g.g. This swine seroconverted (serum dilution giving a 50% reduction in PFU [PRN50] = 1:80) after the first inoculation, and after four inoculations (PRN50 = 1:640) the animal was protected from contact challenge with an FMD-infected swine. In another experiment, piP12X3C and piIRESP12X3C were inoculated into swine (three swine/group) twice by g.g. Surprisingly, these swine did not seroconvert and were not protected from contact challenge. These results suggest that with our present constructs, more than two inoculations are required for protection.
It has been previously shown for inactivated FMD vaccines that there is a close association between virus-specific antibodies and protection (26) and that this response is probably T-helper-cell dependent (10, 11, 15). Furthermore, cytokines such as interleukin 1 and interleukin 2 can enhance the immune response to inactivated FMD vaccines (25). In addition, the isotype of induced antibodies may be important in the level of protection afforded vaccinated animals (8, 27). Thus, we are currently attempting to improve the immune response to our vaccine candidate, piP12X3C, by inclusion of cytokine genes which, upon expression, can direct and modulate the immune system.
Acknowledgments
We thank the Plum Island animal caretakers for assistance with the animals; Brad Bissell, PIADC, ARS, for pcDNA3-β-gal; Carol House, PIADC, FADDL, for lamb kidney cells; and the PowderJect Vaccines, Inc., Madison, Wis., for providing the PowderJect-XR delivery device, operational protocols, gold particles, and helpful discussions.
We also acknowledge the Binational Agriculture Research and Development Fund (grant US-2417-94, awarded to M. J. Grubman and Y. Stram, Kimron Veterinary Institute, Bet-Dagan, Israel) and the USDA Cooperative State Research, Education, and Extension Service (NRICGP proposal 9401720, awarded to P. W. Mason) for financial support.
REFERENCES
- 1.Abrams C C, King A M Q, Belsham G J. Assembly of foot-and-mouth disease virus empty capsids synthesized by a vaccinia virus expression system. J Gen Virol. 1995;76:3089–3098. doi: 10.1099/0022-1317-76-12-3089. [DOI] [PubMed] [Google Scholar]
- 2.Bachrach H L. Foot-and-mouth disease virus. Annu Rev Microbiol. 1968;22:201–244. doi: 10.1146/annurev.mi.22.100168.001221. [DOI] [PubMed] [Google Scholar]
- 3.Baxt B, Vakharia V, Moore D M, Franke A J, Morgan D O. Analysis of neutralizing antigenic sites on the surface of type A12 foot-and-mouth disease virus. J Virol. 1989;63:2143–2151. doi: 10.1128/jvi.63.5.2143-2151.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Beck E, Strohmaier K. Subtyping of European foot-and-mouth disease virus strains by nucleotide sequence determination. J Virol. 1987;61:1621–1629. doi: 10.1128/jvi.61.5.1621-1629.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Berger H-G, Straub O C, Ahl R, Tesar M, Marquardt O. Identification of foot-and-mouth disease virus replication in vaccinated cattle by antibodies to non-structural virus proteins. Vaccine. 1990;8:213–216. doi: 10.1016/0264-410x(90)90048-q. [DOI] [PubMed] [Google Scholar]
- 6.Bolwell C, Brown A L, Barnett P V, Campbell R O, Clarke B E, Parry N R, Ouldridge E J, Brown F, Rowlands D J. Host cell selection of antigenic variants of foot-and-mouth disease virus. J Gen Virol. 1989;70:45–57. doi: 10.1099/0022-1317-70-1-45. [DOI] [PubMed] [Google Scholar]
- 7.Brown F. New approaches to vaccination against foot-and-mouth disease. Vaccine. 1992;10:1022–1026. doi: 10.1016/0264-410x(92)90111-v. [DOI] [PubMed] [Google Scholar]
- 8.Capozzo A V, Periolo O H, Robiolo B, Seki C, LaTorre J L, Grigera P R. Total and isotype humoral responses in cattle vaccinated with foot-and-mouth disease virus (FMDV) immunogen produced either in bovine tongue tissue or in BHK-21 cell suspension cultures. Vaccine. 1997;15:624–630. doi: 10.1016/s0264-410x(96)00284-8. [DOI] [PubMed] [Google Scholar]
- 9.Choi T, Huang M, Gorman C, Jaenisch R. A generic intron increases gene expression in transgenic mice. Mol Cell Biol. 1991;11:3070–3074. doi: 10.1128/mcb.11.6.3070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Collen T, DiMarchi R, Doel T R. A T cell epitope in VP1 of foot-and-mouth disease virus is immunodominant for vaccinated cattle. J Immunol. 1991;146:749–755. [PubMed] [Google Scholar]
- 11.Collen T, Pullen L, Doel T R. T cell-dependent induction of antibody against foot-and-mouth disease virus in a mouse model. J Gen Virol. 1989;65:395–403. doi: 10.1099/0022-1317-70-2-395. [DOI] [PubMed] [Google Scholar]
- 12.Devaney M A, Vakharia V N, Lloyd R E, Ehrenfeld E, Grubman M J. Leader protein of foot-and-mouth disease virus is required for cleavage of the p220 component of the cap-binding protein complex. J Virol. 1988;62:4407–4409. doi: 10.1128/jvi.62.11.4407-4409.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Doel T R, Chong W K T. Comparative immunogenicity of 146S, 75S, and 12S particles of foot-and-mouth disease virus. Arch Virol. 1982;73:185–191. doi: 10.1007/BF01314726. [DOI] [PubMed] [Google Scholar]
- 14.Duronio R J, Jackson-Machelsky E, Heuckeroth R O, Olins P O, Devine C S, Yonemoto W, Slice L W, Taylor S S, Gordon J I. Protein N-myristoylation in Escherichia coli: reconstitution of a eukaryotic protein modification in bacteria. Proc Natl Acad Sci USA. 1990;87:1506–1510. doi: 10.1073/pnas.87.4.1506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Francis M J, Hastings G Z, Syred A D, McGinn B, Brown F, Rowlands D J. Non-responsiveness to a foot-and-mouth disease virus peptide overcome by addition of foreign helper T-cell determinants. Nature (London) 1987;330:168–170. doi: 10.1038/330168a0. [DOI] [PubMed] [Google Scholar]
- 16.Gonzalez M, Mateu M G, Martinez M A, Carillo C, Sobrino F. Comparison of capsid protein VP1 of the viruses used for the production and challenge of foot-and-mouth disease vaccines in Spain. Vaccine. 1992;10:731–734. doi: 10.1016/0264-410x(92)90504-d. [DOI] [PubMed] [Google Scholar]
- 17.Grubman M J, Lewis S A, Morgan D O. Protection of swine against foot-and-mouth disease with viral capsid proteins expressed in heterologous systems. Vaccine. 1993;11:825–829. doi: 10.1016/0264-410x(93)90357-4. [DOI] [PubMed] [Google Scholar]
- 18.Grubman M J, Morgan D O, Kendall J, Baxt B. Capsid intermediates assembled in a foot-and-mouth disease virus genome RNA-programmed cell-free translation system and in infected cells. J Virol. 1985;56:120–126. doi: 10.1128/jvi.56.1.120-126.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Grubman M J, Zellner M, Bablanian G, Mason P W, Piccone M E. Identification of the active-site residues of the 3C proteinase of foot-and-mouth disease virus. Virology. 1995;213:581–589. doi: 10.1006/viro.1995.0030. [DOI] [PubMed] [Google Scholar]
- 20.King A M Q, Underwood B O, McCahon D, Newman J W I, Brown F. Biochemical identification of viruses causing the 1981 outbreaks of foot-and-mouth disease in the UK. Nature. 1981;293:479–480. doi: 10.1038/293479a0. [DOI] [PubMed] [Google Scholar]
- 21.Knipe T, Rieder E, Baxt B, Ward G, Mason P W. Characterization of synthetic foot-and-mouth disease virus provirions separates acid-mediated disassembly from infectivity. J Virol. 1997;71:2851–2856. doi: 10.1128/jvi.71.4.2851-2856.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Krausslich H-G, Holscher C, Reuer Q, Harber J, Wimmer E. Myristoylation of the poliovirus polyprotein is required for proteolytic processing of the capsid and for viral infectivity. J Virol. 1990;64:2433–2436. doi: 10.1128/jvi.64.5.2433-2436.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lewis S A, Morgan D O, Grubman M J. Expression, processing and assembly of foot-and-mouth disease virus capsid structures in heterologous systems: induction of a neutralizing antibody response in guinea pigs. J Virol. 1991;65:6572–6580. doi: 10.1128/jvi.65.12.6572-6580.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lubroth J, Brown F. Identification of native foot-and-mouth disease virus non-structural protein 2C as a serological indicator to differentiate infected from vaccinated livestock. Res Vet Sci. 1995;59:70–78. doi: 10.1016/0034-5288(95)90034-9. [DOI] [PubMed] [Google Scholar]
- 25.McCullough K C, Pullen L, Parkinson D. The immune response against foot-and-mouth disease virus: influence of the T lymphocyte growth factors IL-1 and IL-2 on the murine humoral response in vivo. Immunol Lett. 1991;31:41–46. doi: 10.1016/0165-2478(92)90008-c. [DOI] [PubMed] [Google Scholar]
- 26.McCullough K C, De Simone F, Brocchi E, Capucci L, Crowther J R, Kihm U. Protective immune response against foot-and-mouth disease. J Virol. 1992;66:1835–1840. doi: 10.1128/jvi.66.4.1835-1840.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mulcahy G, Gale C, Robertson P, Iyisan S, DiMarchi R D, Doel T R. Isotype responses of infected, virus-vaccinated and peptide-vaccinated cattle to foot-and-mouth disease virus. Vaccine. 1990;8:249–256. doi: 10.1016/0264-410x(90)90054-p. [DOI] [PubMed] [Google Scholar]
- 28.Palmiter R D, Sandgren E P, Avarbock M R, Allen D D, Brinster R L. Heterologous introns can enhance expression of transgenes in mice. Proc Natl Acad Sci USA. 1991;88:478–482. doi: 10.1073/pnas.88.2.478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pertmer T A, Roberts T R, Haynes J R. Influenza virus nucleoprotein-specific immunoglobulin G subclass and cytokine responses elicited by DNA vaccination are dependent on the route of vector DNA delivery. J Virol. 1996;70:6119–6125. doi: 10.1128/jvi.70.9.6119-6125.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Robertson B H, Morgan D O, Moore D M. Location of the neutralizing monoclonal antibodies generated against the outer capsid polypeptide, VP1, of foot-and-mouth disease virus A12. Virus Res. 1984;1:489–500. doi: 10.1016/0168-1702(84)90006-6. [DOI] [PubMed] [Google Scholar]
- 31.Roosien J, Belsham G J, Ryan M D, King A M Q, Vlak J M. Synthesis of foot-and-mouth disease virus capsid proteins in insect cells using baculovirus expression vectors. J Gen Virol. 1990;71:1703–1711. doi: 10.1099/0022-1317-71-8-1703. [DOI] [PubMed] [Google Scholar]
- 32.Rowlands D J, Sangar D V, Brown F. A comparative chemical and serological study of the full and empty particles of foot-and-mouth disease virus. J Gen Virol. 1975;26:227–238. doi: 10.1099/0022-1317-26-3-227. [DOI] [PubMed] [Google Scholar]
- 33.Rueckert R R. Picornaviridae: the viruses and their replication. In: Fields B N, Knipe D M, Howley P H, editors. Virology. Philadelphia, Pa: Lippincott-Raven Publishers; 1996. pp. 609–654. [Google Scholar]
- 34.Rweyemamu M M, Terry G, Pay T W F. Stability and immunogenicity of empty particles of foot-and-mouth disease virus. Arch Virol. 1979;59:69–79. doi: 10.1007/BF01317896. [DOI] [PubMed] [Google Scholar]
- 35.Vakharia V N, Devaney M A, Moore D M, Dunn J J, Grubman M J. Proteolytic processing of foot-and-mouth disease virus polyproteins expressed in a cell-free system from clone-derived transcripts. J Virol. 1987;61:3199–3207. doi: 10.1128/jvi.61.10.3199-3207.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ward G, Rieder E, Mason P W. Plasmid DNA encoding replicating foot-and-mouth disease virus genomes induces antiviral immune responses in swine. J Virol. 1997;71:7442–7447. doi: 10.1128/jvi.71.10.7442-7447.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]