Abstract
The pterygomandibular raphe (PMR) is a tendinous structure connecting the bucinator and the superior pharyngeal constrictor muscles. With its implications in the spread of oral cancer, the proper treatment of obstructive sleep apnea, and dental procedures, it is important to obtain a thorough understanding of the PMR. We reviewed the existing literature to compile the published information regarding its anatomy, embryology, imaging, variations, functions, pathologies, and clinical relevance of the pterygomandibular raphe.
Keywords: Anatomy, Tendons, Embryology, Anatomic variation, Oral
Introduction
The pterygomandibular raphe (PMR) is classically described as a tendon joining the maxilla and mandible [1]. Through the years, it has been referred to as the ligamentum pterygomandibulare [2, 3], ligamentum intermaxillaire [3, 4], aponeurose buccinatopharyngée [3, 5], and raphe buccipharyngica [3, 6]. Serving as an aponeurotic connection between the bucinator muscle (“bucinator” muscle is adopted in the second edition of Terminologia Anatomica [7]) and the superior pharyngeal constrictor muscle (SPC), the PMR has been reasoned to be crucial in the distinct swallowing and chewing functions of the two muscles [1]. From treating obstructive sleep apnea (OSA) to affecting the spread of various carcinomas, the PMR plays an important clinical role [8-15]. Thus, a proper understanding of this structure is necessary for effective clinical care.
Review
Ethical statement
The present study was performed in accordance with the requirements of the Declaration of Helsinki (64th WMA General Assembly, Fortaleza, Brazil, October 2013). The authors wish to sincerely thank those who donated their bodies to science so that anatomical research could be performed. Results from such research can potentially improve patient care and increase mankind’s overall knowledge. Therefore, these donors and their families deserve our highest gratitude.
Anatomy
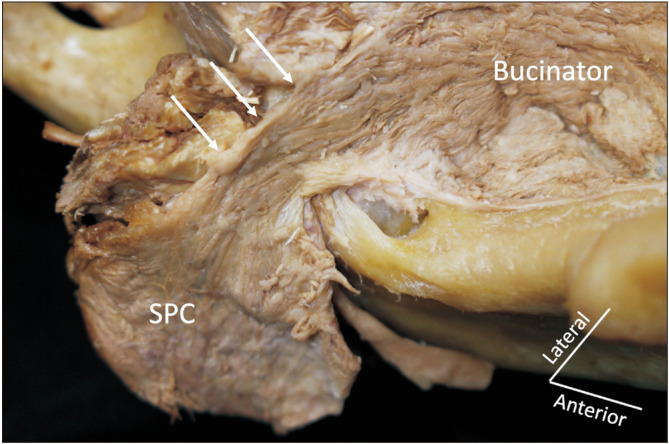
The PMR serves as a confluence of the oropharynx, nasopharynx, and the oral cavity itself through its various insertion points [16]. It is a muscular and fibrous structure that runs superiorly from the hamulus of the medial plate to its inferior attachment- the posterior mylohyoid ridge of the mandibular cortex or the posterior edge of the retromolar trigone (RMT) of the mandible [3, 13]. The anterior border of the PMR attaches to the bucinator, while the posterior border attaches to the SPC [13]. Covered by mucosa, it forms, on average, a 25–30 mm long pterygomandibular fold (PMF) right behind the third molar (Fig. 1) [3, 17]. The SPC is also reported to have continuous fiber to the soft palate and the root of the tongue [18, 19].
Fig. 1.
Pterygomandibular fold (arrowheads) right behind the mandibular last molar.
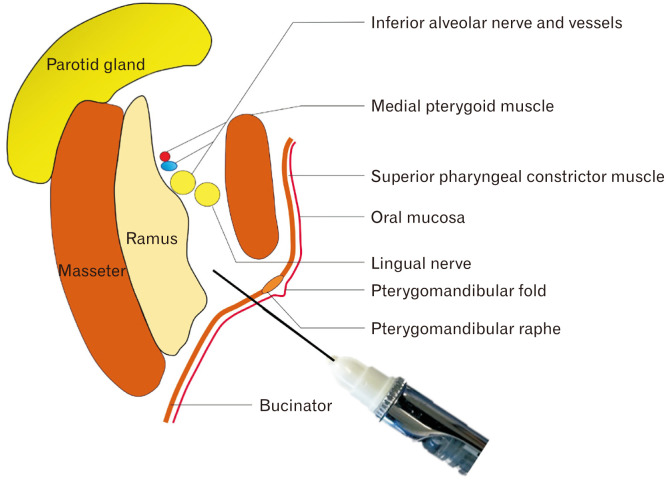
The PMR forms the anterior wall of the pterygomandibular space, an important cavity containing the inferior alveolar nerve, artery and vein, the lingual nerve, the nerve to mylohyoid, and the sphenomandibular ligament [20, 21]. Medial to the prestyloid compartment, the PMR’s medial surface is covered by oral mucosa [1, 9]. The lateral surface, however, is disconnected from the ramus of the mandible by a layer of buccal fat pad-derived adipose tissue [1].
Variations
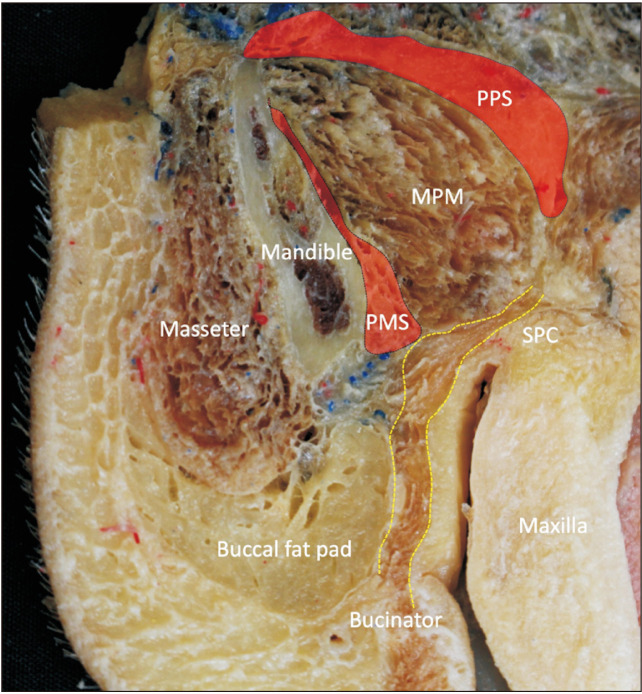
The presence and characteristics of the PMR have been the subject of conflicting reports. While some deny its existence, others support it (Figs. 2, 3) [3, 8, 9, 22-24]. After studying 50 hemiheads, Gaughran [25] concluded that the PMR was an anatomical artifact, citing the continuous nature of the bucinator and the SPC in all specimens. Various other studies support this view [22, 23]. In their study of the tendons of the temporalis muscle, Harn and Shackelford [22] describe the fascial-tendinous complex of the temporalis muscle as the functional equivalent to the PMR. They go on to claim lack of musculature within the PMF, mentioning the occasional ligamentous structure forming, but not the PMR [22].
Fig. 2.
The absence of the pterygomandibular raphe (arrows). SPC, superior pharyngeal constrictor muscle.
Fig. 3.
Axial section of the right bucinator and SPC shown with yellow dotted lines. There is no clear border between two muscles. MPM, medial pterygoid muscle; PMS, pterygomandibular space; PPS, parapharyngeal space; SPC, superior pharyngeal constrictor muscle.
Contrastingly, in a recent description of this buccotemporal fascia, researchers describe it inserting anterior to the PTM [24]. This existence of the PMR is supported by various other studies as well [8, 9, 17]. Subsequent studies done by Shimada and Gasser [3] detail the existence of various forms of the PMR. In his original study of 57 Japanese specimens, Shimada and Gasser [3] describes five morphologies of the PMR-type A–E: Type A was found in 41.5% of specimens and was a broad, triangular structure only in the upper portion of the PMR. Type B, found in 24.7% of specimens, was a broad triangular structure that narrowed inferiorly to the mandible. Type C, found in 11.7% of specimens, was a broad fascial region that separated the bucinator and superior constrictor muscles. Type D, found in 9.1% of specimens, was a narrow vertical band that separated the two muscles, consistent with most anatomical texts. Finally, type E, found in 13% of specimens, was an absent PMR with complete continuity of the two adjacent muscles [3]. However, in his following study of European descendants and African American individuals, Shimada and Gasser [3] found that types B and D were not present, and instead described the existence of only three types of PMRs—type A (28%), B (36%), and C (36%)—which were equivalent to the original type A, C, and E, respectively. Therefore, there seems to be wide variation of the PMR based on characteristics such as race. However, there were not significant differences within the types when compared based on side, sex, and age [3].
Histology
Recent anatomical and histological study by Fukino et al. [26] has shown that the absence of the PMR in all examined specimens. The SPC joins the bucinator without clear border. The bucinator attaches the deep temporalis tendon that might reinforce the bucinator posteriorly. The variable bucinator/deep temporalis tendon/superior pharyngeal constrictor muscle complex (the muscles and their confluence) might have been recognized as a PMR. Fukino et al. [26] also described reasonable answers why the existence of the PMR has been believed for a long time.
Embryology
The bucinator muscle is innervated by the facial nerve, which is derived from the second pharyngeal arch. The SPC, on the other hand, is innervated by the pharyngeal plexus i.e., glossopharyngeal and vagus nerves and is associated with the third and fourth pharyngeal arch, respectively [27, 28]. The PMR is of embryological interest as it is a junction between these two arches’ derivatives [16]. In Shimada’s initial study of the PMR, the existence of a broad fascial separation between the bucinator and the SPC was confirmed in all 50 fetuses studied. Thus, any variation found in the PMR was deemed to develop postnatally [3, 29].
At gestational age (GA) 10 weeks, the bucinator is far anterior to the SPC. However, during this point in time, the palatopharyngeus begins pulling the SPC anteriorly. At GA 11–13 weeks, it meets with the bucinator and forms its connection. It is thought the PMR may contain the degenerated fibers of the SPC after movement of the muscles during further development [30].
Imaging
Magnetic resonance imaging (MRI) is generally considered the best way to visualize the PMR [8, 9, 13, 31]. Contrast-enhanced computed tomography could be used, but dental amalgam artifacts seem to create far too much degradation of the image [13]. Many studies use a combination of tendon-identifying techniques and location inference based on the relationship of the PMR to the bucinator and the SPC [8, 9, 13]. However, reliably localizing the PMR using MRI can be challenging due to the limited resolution of the technique. Additionally, the presence of other ligaments running inferoanteriorly in similar regions of the skull further might reduce the reliability of PMR imaging, which could be differentiate from the PMR by its location [13, 31].
Function
While the exact function of the PMR remains unknown, there are various theories about the role of the PMR [8]. Studies on OSA treatment have led to the discovery of certain findings, such as the PMR’s ability to stabilize the mandible and temporomandibular joint [8, 31]. Additionally, mandibular advancement has been found to result in more lateral than anterior-posterior movement, which is believed to be related to the function of the PMR [17]. Shimada reasoned that, without the PMR, the separate functions of the bucinator and SPC would be challenging. Without the PMR functioning as an anchor, he postulated it would be tough for the two muscles to separately assist in chewing or swallowing [3]. While this may not be the case due to its absence in some individuals, the location and tendinous nature of the PMR begs the question of how its presence changes the function of the various head and neck muscles of the region. The SPC has been also reported to have function of retrusive movement of the human adult tongue by connecting to transverse muscle of the tongue [32].
Pathology
Ossification and rigidity of the PMR have been reported [1, 33]. Reasoned to be due to the retention of embryonic ossification in the PMR, ossification of the structure was found in the past as a cause of the pharyngeal pain relieved through surgical removal [1]. Additionally, it seems that rigidity of the PMR could result in trismus and right mandibular displacement during mouth opening. It is reasoned that this is due to age-related fibrosis of the oral mucosa [33].
Clinical applications
The PMR has proven to be useful in many different clinical practices. One of these is the treatment of OSA [8-11, 34]. From mandibular advancement splint (MAS) to suspension palatoplasty to barbed reposition pharyngoplasty, the PMR plays an important role in various OSA procedures. A proper understanding of this structure will allow for informed decision making when deciding on a course of action for OSA treatment.
MASs work by decreasing airway collapsibility through fixing the mandible in an anterior position, thereby increasing the lateral dimension of the airway. However, they are only effective in 50% of users [35]. After observing the lateral dimension change occurring at the convergence of the bucinator and SPC, researchers believed the presence of the tendinous raphe would elicit a positive response to MAS. However, testing this hypothesis revealed that the presence of the PMR actually caused a worse response to the treatment, possibly due to its added ability to stabilize the temporomandibular joint [8]. Other treatments for OSA include suspension palatoplasty and barbed reposition pharyngoplasty. Their aim is to anchor the soft palate to more robust fascia in the oral cavity [10]. In many cases, this attachment point is the PMR [9-11]. While these two treatments have small differences, their efficacy as OSA treatment is notable.
The positioning of the PMR slightly deep to the RMT at the junction of the oral cavity and the oropharynx allows it to act as a framework for tumor growth [13]. Around 7% of oral tumors begin in the RMT, and the PMR can allow them to spread to the masticator, the buccal space, and the buccal fat behind the maxillary sinus [12, 13]. As these tumors may spread submucosally, clinical examination alone is often not enough to detect them, making proper imaging of the PMR essential [13]. Additionally, the PMR is a common route of spreading for buccal squamous cell carcinomas [36, 37]. The PMR is also used for endoscopic resection of benign infratemporal fossa tumors. Surgeons are able to use a trans-lateral PMR or trans-medial PMR approach depending on the location of the tumor and its relation to the internal carotid artery [14]. Of course, the PMR also has a role in precancerous treatment [15]. More specifically, it is the site of treatment for oral submucous fibrosis generally associated with rigidity and inability to open the mouth fully. It is commonly treated with a combination of triamcinolone acetonide and hyaluronidase injected into the PMR [15]. The superior pharyngeal constrictor syndrome is also known caused by the SPC [38]. This syndrome can be associated with the bucinator muscle’s disfunction as PMR should connect two muscles.
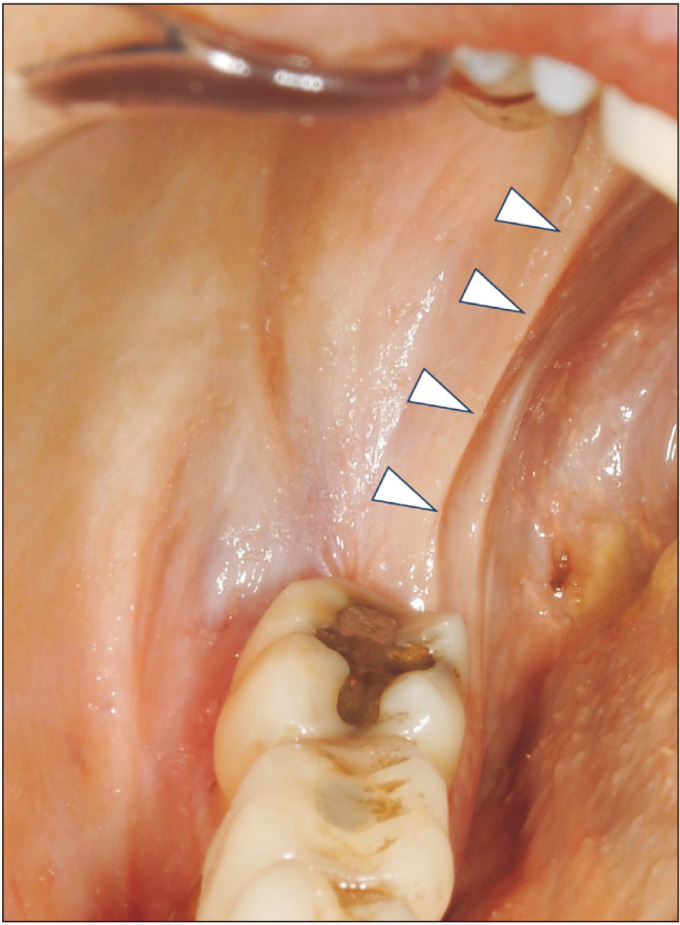
The PMR also influences various dental procedures. Dentists and other oral proceduralists must be wary of the PMR prior to creating a treatment plan, whether it be piercing it for the proper administration of an inferior alveolar nerve block in the pterygomandibular space or dictating proper fixation of lower dentures (Fig. 4) [3, 20].
Fig. 4.
Inferior alveolar nerve block in the pterygomandibular space (the level of the mandibular foramen).
Pterygomandibular raphe and fold
However, before utilizing the PMR as a landmark for clinical procedure, we need to consider the difference between the PMR and PMF. Many textbooks even research papers use the term PMR incorrectly. The PMR is not visualized in the oral cavity but the PMF is as it is a superficial mucosal fold. We do not really observe the PMR during the dental/surgical procedure because it is defined as the submucosal structure. In fact, most of the clinical studies which discussed “PMR” are the studies on “PMF.” The tendinous structure which is observed in MRI imaging should be the deep temporalis tendon (medial crus), not PMR, as the deep temporalis tendon always run supero-inferior direction posterior to the bucinator/SPC. Thus, the clinical/surgical description of the PMR can lead misunderstanding.
Conclusion
The PMR has been considered the tendinous structure which links the bucinator and the SPC. However, many studies misunderstood the definition of the PMR. The most recent study of the PMR has clearly shown that the PMR does not exist by three-dimensional analysis which focused on the relationship of surrounding structures which the authors of the present review do believe. However, the PMF still exists as an important superficial landmark, and proper understanding of its various pathologies and functions will allow clinicians to effectively address oral carcinomas, OSA, and other population-spanning maladies.
Acknowledgements
The authors sincerely thank those who donated their bodies to science so that anatomical research could be performed. Results from such research can potentially increase mankind’s overall knowledge and thus improve patient care. Therefore, these donors and their families deserve our highest gratitude [39].
Funding Statement
Funding None.
Footnotes
Author Contributions
Conceptualization: JI. Data acquisition: NK, KF, RST. Data analysis or interpretation: RV, KF, JI. Drafting of the manuscript: RV. Critical revision of the manuscript: NK, KF, RST, JI. Approval of the final version of the manuscript: all authors.
Conflicts of Interest
No potential conflict of interest relevant to this article was reported.
References
- 1.Griffin WL., Jr Symptomatic ossification of the pterygomandibular raphe. Arch Otolaryngol. 1978;104:298–9. doi: 10.1001/archotol.1978.00790050064016. [DOI] [PubMed] [Google Scholar]
- 2.Macalister A. A text-book of human anatomy: systematic and topographical, including the embryology, histology and morphology of man, with special reference to the requirements of practical surgery and medicine. Griffin; 1889. [Google Scholar]
- 3.Shimada K, Gasser RF. Morphology of the pterygomandibular raphe in human fetuses and adults. Anat Rec. 1989;224:117–22. doi: 10.1002/ar.1092240115. [DOI] [PubMed] [Google Scholar]
- 4.Hollstein L. In: [Textbook of human anatomy] Verlag von E.H, editor. Schroeder; 1873. p. 279. German. [Google Scholar]
- 5.Poirier P, Charpy A. [Treatise on human anatomy] 2nd-3rd ed. Masson; 1901. pp. 355–7. French. [Google Scholar]
- 6.Rauber A, Kopsch F. [Rauber-Kopsch textbook and atlas of human anatomy] Georg Thieme; 1952. p. 521. German. [Google Scholar]
- 7.FIPAT, author. Terminologia Anatomica. 2nd ed. Federative International Programme for Anatomical Terminology; 2019. [Google Scholar]
- 8.Brown EC, Jugé L, Knapman FL, Burke PGR, Ngiam J, Sutherland K, Butler JE, Eckert DJ, Cistulli PA, Bilston LE. Mandibular advancement splint response is associated with the pterygomandibular raphe. Sleep. 2021;44:zsaa222. doi: 10.1093/sleep/zsaa222. [DOI] [PubMed] [Google Scholar]
- 9.Garaycochea O, Baptista P, Calvo-Imirizaldu M, Terrasa D, Moffa A, Casale M, Alcalde J, O'Connor-Reina C, Plaza G, Fernández S. Surgical anatomy of the lingual nerve for palate surgery: where is located and how to avoid it. Eur Arch Otorhinolaryngol. 2022;279:5347–53. doi: 10.1007/s00405-022-07432-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li HY, Lee LA, Kezirian EJ, Nakayama M. Suspension palatoplasty for obstructive sleep apnea- a preliminary study. Sci Rep. 2018;8:4224. doi: 10.1038/s41598-018-22710-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vicini C, Hendawy E, Campanini A, Eesa M, Bahgat A, AlGhamdi S, Meccariello G, DeVito A, Montevecchi F, Mantovani M. Barbed reposition pharyngoplasty (BRP) for OSAHS: a feasibility, safety, efficacy and teachability pilot study. "We are on the giant's shoulders". Eur Arch Otorhinolaryngol. 2015;272:3065–70. doi: 10.1007/s00405-015-3628-3. [DOI] [PubMed] [Google Scholar]
- 12.Crecco M, Vidiri A, Vigili MG, Angelone ML, Mattioli M, Marzetti F, Squillaci S. [The magnetic resonance estimation of the T parameter in the staging of tumors of the oral cavity and tongue. A correlation with postoperative data and preliminary echotomographic experience]. Radiol Med. 1994;87:452–9. Italian. [PubMed] [Google Scholar]
- 13.Rao D, Sandhu S, Ormsby C, Natter P, Haymes D, Cohen I, Jenson M. Review of the pterygomandibular raphe. Neurographics. 2017;7:121–5. doi: 10.3174/ng.2170196. [DOI] [Google Scholar]
- 14.Yu LG, Wang L, Zhao LJ, Zhang SN, Chen M, Cai L, Li N, Jiang Y. [Application of endoscopic resection of benign tumor in infratemporal fossa]. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2020;55:87–93. doi: 10.3760/cma.j.issn.1673-0860.2020.02.002. Chinese. [DOI] [PubMed] [Google Scholar]
- 15.Singh M, Niranjan HS, Mehrotra R, Sharma D, Gupta SC. Efficacy of hydrocortisone acetate/hyaluronidase vs triamcinolone acetonide/hyaluronidase in the treatment of oral submucous fibrosis. Indian J Med Res. 2010;131:665–9. [PubMed] [Google Scholar]
- 16.Mukherji SK, Pillsbury HR, Castillo M. Imaging squamous cell carcinomas of the upper aerodigestive tract: what clinicians need to know. Radiology. 1997;205:629–46. doi: 10.1148/radiology.205.3.9393513. [DOI] [PubMed] [Google Scholar]
- 17.Cuccia AM, Caradonna C, Caradonna D. Manual therapy of the mandibular accessory ligaments for the management of temporomandibular joint disorders. J Am Osteopath Assoc. 2011;111:102–12. [PubMed] [Google Scholar]
- 18.Tsumori N, Abe S, Agematsu H, Hashimoto M, Ide Y. Morphologic characteristics of the superior pharyngeal constrictor muscle in relation to the function during swallowing. Dysphagia. 2007;22:122–9. doi: 10.1007/s00455-006-9063-2. [DOI] [PubMed] [Google Scholar]
- 19.Fukino K, Tsutsumi M, Sanudo J, Ono T, Akita K. Anatomical significance of the spatial distribution of the palatopharyngeus with regard to velopharyngeal closure. Cleft Palate Craniofac J. 2019;56:744–50. doi: 10.1177/1055665618813082. [DOI] [PubMed] [Google Scholar]
- 20.Khoury JN, Mihailidis S, Ghabriel M, Townsend G. Applied anatomy of the pterygomandibular space: improving the success of inferior alveolar nerve blocks. Aust Dent J. 2011;56:112–21. doi: 10.1111/j.1834-7819.2011.01312.x. [DOI] [PubMed] [Google Scholar]
- 21.Iwanaga J, Tubbs RS. A new treatment for lingual nerve injury: an anatomical feasibility study for using a buccal nerve pedicle graft. Surg Radiol Anat. 2020;42:49–53. doi: 10.1007/s00276-019-02345-1. [DOI] [PubMed] [Google Scholar]
- 22.Harn SD, Shackelford LS. Further evaluation of the superficial and deep tendons of the human temporalis muscle. Anat Rec. 1982;202:537–48. doi: 10.1002/ar.1092020413. [DOI] [PubMed] [Google Scholar]
- 23.Okada R, Muro S, Eguchi K, Yagi K, Nasu H, Yamaguchi K, Miwa K, Akita K. The extended bundle of the tensor veli palatini: anatomic consideration of the dilating mechanism of the Eustachian tube. Auris Nasus Larynx. 2018;45:265–72. doi: 10.1016/j.anl.2017.05.014. [DOI] [PubMed] [Google Scholar]
- 24.Rusu MC, Hostiuc S, Jianu AM. A glimpse of past, the temporo-buccinator band of Hovelaque, or the buccotemporal fascia of Zenker. Morphologie. 2021;105:189–95. doi: 10.1016/j.morpho.2020.07.003. [DOI] [PubMed] [Google Scholar]
- 25.Gaughran G. The pterygomandibular raphe- anatomical artifact. Anat Rec. 1976;184:410. [Google Scholar]
- 26.Fukino K, Iitsuka M, Kitagawa N, Tubbs RS, Akita K, Iwanaga J. Three-dimensional analysis of the muscles related to the so-called "pterygomandibular raphe": an anatomical and histological study. Dysphagia. 2024 Jan 10; doi: 10.1007/s00455-023-10645-3. [Epub]. https://doi.org/10.1007/s00455-023-10645-3 . [DOI] [PubMed] [Google Scholar]
- 27.Gutierrez S, Iwanaga J, Pekala P, Yilmaz E, Clifton WE, Dumont AS, Tubbs RS. The pharyngeal plexus: an anatomical review for better understanding postoperative dysphagia. Neurosurg Rev. 2021;44:763–72. doi: 10.1007/s10143-020-01303-5. [DOI] [PubMed] [Google Scholar]
- 28.Sakamoto Y. Classification of pharyngeal muscles based on innervations from glossopharyngeal and vagus nerves in human. Surg Radiol Anat. 2009;31:755–61. doi: 10.1007/s00276-009-0516-9. [DOI] [PubMed] [Google Scholar]
- 29.Shimada K. A study of the morphology of the raphe pterygomandibularis, part 1. The adults. Nihon Univ Dent J. 1979;53:998–1007. [Google Scholar]
- 30.Jin ZW, Kim JH, Yamamoto M, Katori Y, Abe H, Murakami G, Abe SI. Growth in fetuses of the constrictor pharyngis superior with special reference to its meeting with the buccinator: an embryological basis of adult variations in palatopharyngeal anatomy. Surg Radiol Anat. 2022;44:559–71. doi: 10.1007/s00276-022-02907-w. [DOI] [PubMed] [Google Scholar]
- 31.Brown EC, Cheng S, McKenzie DK, Butler JE, Gandevia SC, Bilston LE. Tongue and lateral upper airway movement with mandibular advancement. Sleep. 2013;36:397–404. doi: 10.5665/sleep.2458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Saigusa H, Yamashita K, Tanuma K, Saigusa M, Niimi S. Morphological studies for retrusive movement of the human adult tongue. Clin Anat. 2004;17:93–8. doi: 10.1002/ca.10156. [DOI] [PubMed] [Google Scholar]
- 33.Ouchi K, Ueno Y, Suzuki H, Jinnouchi A. Trismus caused by pterygomandibular raphe rigidity: a case report and systematic review. Oral Health Care. 2018;3:1–4. doi: 10.15761/OHC.1000146. [DOI] [Google Scholar]
- 34.Askar SM, Al-Hussain OH, Abd El-Badea A, Abou-Sharkh AA, Awad AM. Suspension-expansion pharyngoplasty: a modified technique for oropharyngeal collapse in obstructive sleep apnea. Eur Arch Otorhinolaryngol. 2023;280:1343–51. doi: 10.1007/s00405-022-07688-x. [DOI] [PubMed] [Google Scholar]
- 35.Mehta A, Qian J, Petocz P, Darendeliler MA, Cistulli PA. A randomized, controlled study of a mandibular advancement splint for obstructive sleep apnea. Am J Respir Crit Care Med. 2001;163:1457–61. doi: 10.1164/ajrccm.163.6.2004213. [DOI] [PubMed] [Google Scholar]
- 36.Xu SS, Li D, Zhou Y, Sheng B, Zeng C, Zhong SX. Pathways involved in the spread of buccal carcinoma on contrast-enhanced multislice CT. Dentomaxillofac Radiol. 2015;44:20140111. doi: 10.1259/dmfr.20140111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Otsuru M, Yanamoto S, Naruse T, Omori K, Morishita K, Sumi M, Umeda M. Surgical treatment and prognosis of posteriorly invading oral cancer: potential clinical significance of pterygomandibular raphe. J Dent Sci. 2023;18:81–6. doi: 10.1016/j.jds.2022.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shankland WE., 2nd Anterior throat pain syndromes: causes for undiagnosed craniofacial pain. Cranio. 2010;28:50–9. doi: 10.1179/crn.2010.007. [DOI] [PubMed] [Google Scholar]
- 39.Iwanaga J, Singh V, Ohtsuka A, Hwang Y, Kim HJ, Moryś J, Ravi KS, Ribatti D, Trainor PA, Sañudo JR, Apaydin N, Şengül G, Albertine KH, Walocha JA, Loukas M, Duparc F, Paulsen F, Del Sol M, Adds P, Hegazy A, Tubbs RS. Acknowledging the use of human cadaveric tissues in research papers: recommendations from anatomical journal editors. Clin Anat. 2021;34:2–4. doi: 10.1002/ca.23671. [DOI] [PubMed] [Google Scholar]