Dear Editor,
Aquagenic palmoplantar keratoderma (APK) is a rare skin condition that primarily affects young adult females. It is characterized by the involvement of eccrine secretory coil and acrosyringium, leading to burning and oedema in the palms after water immersion. Hereditary papulotranslucent acrokeratoderma (HPA) is the closest differential diagnosis to APK. However, this case report presents an unusual case of APK with overlapping clinical features with HPA in a young man.
A 25-year-old male complained of skin thickening on the medial edge of his hands for two years. He also complained of skin becoming more wrinkled after brief water submersion. But the changes resolved within 5–10 minutes without discomfort, pruritis, or burning. He had no history of hyperhidrosis, drug use, atopic symptoms, respiratory problems, or any relevant family history. On examination, there were numerous tiny papules coalescing to form a hyperkeratotic, hyperpigmented plaque along the medial border of the bilateral palms, which became easily distinguishable and oedematous on immersion in water [Figure 1a and b]. On dermoscopy, there were numerous skin-colored to yellow-colored, well-defined coalescing globules, sparing the dermatoglyphics [Figure 2]. Aquagenic palmoplantar keratoderma and HPA were the differential diagnoses that were considered.
Figure 1.
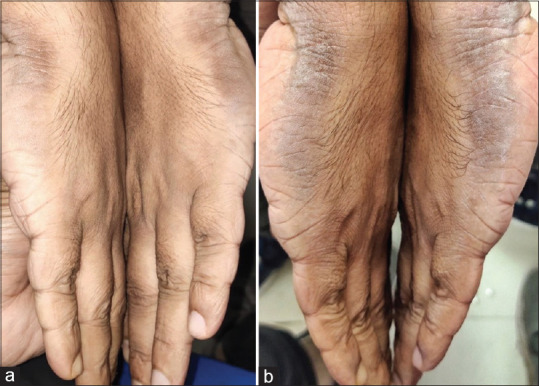
(a) Numerous tiny papules coalescing to form a hyperkeratotic hyperpigmented plaque along the medial border of bilateral palms. (b) Multiple translucent papules became easily distinguishable and the plaque became oedematous after immersion in water
Figure 2.
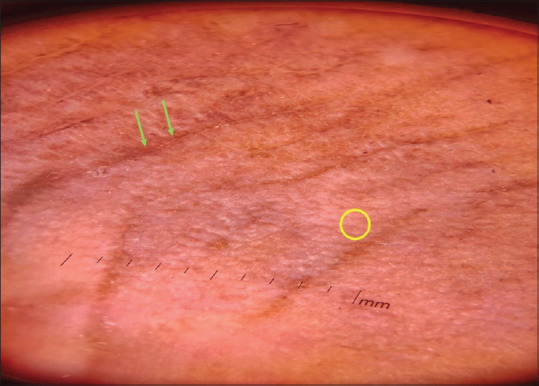
Numerous skin-colored to yellow-colored, well-defined coalescing globules (yellow circle), sparing the dermatoglyphics (green arrow) (DermLite DL3N, dry, contact, polarized, x10)
Just after immersing the hand in the water, a punch biopsy specimen was sent for histopathological examination. This showed spongiotic changes in the stratum corneum, multiple dilated eccrine ducts, and mild perivascular lymphocytic infiltration in the upper dermis [Figure 3]. Acquired aquagenic localized palmar keratoderma was established as the final diagnosis. Treatment was initiated with a 20% alcohol solution of aluminum chloride hexahydrate applied once daily at night. After a month of therapy, there was a significant improvement.
Figure 3.
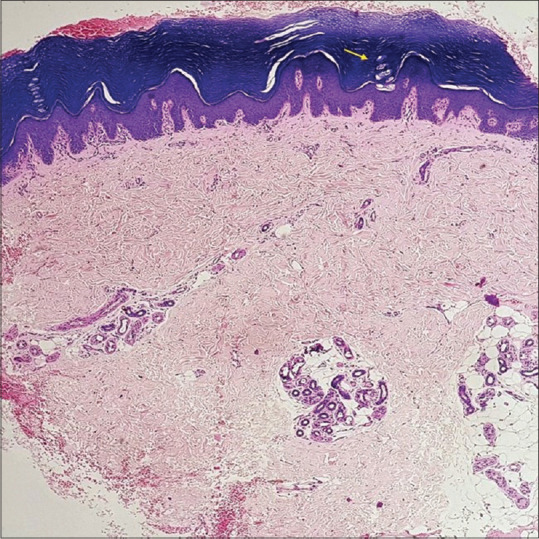
Dilated eccrine ducts (yellow arrow), mild perivascular lymphocytic infiltration in the upper dermis, and spongiotic changes in the stratum corneum (H and E; 10x)
English and McCollough originally identified APK in two sisters as an acquired disease characterized by burning and oedema affecting the palms following immersion in water.[1] Due to the resemblances between the lesions in hereditary papulotranslucent acrokeratoderma, they named it “transient reactive papulotranslucent acrokeratoderma.” Aquagenic palmoplantar keratoderma is also known as aquagenic syringeal acrokeratoderma due to its involvement of eccrine secretory coil and acrosyringium. The hallmark presentation includes papules and plaques with a burning sensation upon water immersion. Some patients demonstrate symptoms with a “hand-in-the-bucket” sign. Unusual presentations include localized and unilateral forms.[2] Aquagenic palmoplantar keratoderma is linked to cystic fibrosis, focal hyperhidrosis, and Raynaud’s syndrome. The pathophysiology is unclear, but theories suggest elevated aquaporin 5 expression or increased sympathetic fiber activity.[3] The distinctive histopathological findings involve spongiotic changes, orthohyperkeratosis with acanthosis, eccrine acrosyringia dilation, and perivascular inflammatory infiltration. Several treatment methods have been attempted, but there is currently no consensus on the best approach. Various therapies, including 20% aluminum chloride hexahydrate solution, corticosteroids, topically applied keratolytics, oral antihistamines, oral anticholinergics, botulinum toxin injection, and iontophoresis, have been discussed in the literature.[4]
The closest differential diagnosis to APK is HPA, which is characterized by asymptomatic yellowish-white translucent papules and plaques that become more prominent with water exposure. Hereditary papulotranslucent acrokeratoderma has an autosomal dominant inheritance and is associated with atopic diathesis.[5] Histopathology shows hyperkeratosis, hypergranulosis, and acanthosis with no inflammatory infiltrate in the dermis or abnormality in adnexal structures. Another differential diagnosis is palmoplantar keratoderma Bothnia type. It is a rare nonepidermolytic palmoplantar keratoderma characterized by diffuse thickening of the palms and soles, starting around age one. It is caused by gain-of-function mutations in the AQP5 gene, similar to APK. Bothnia type shares features with HPA, including autosomal dominant inheritance, familial clustering, and persistent lesions turning spongy following water immersion.[6]
Interestingly, this case showed overlapping clinical features with HPA, adding complexity to the diagnosis. There are not many documented cases of males with APK. Our patient also had localized involvement along the medial edges of both hands and did not experience burning when immersed in water. Lesions on our patient persisted and grew larger when they were immersed in water. Despite similarities, APK and HPA can be distinguished by their histologic features, suggesting they are variants of a wide spectrum of diseases.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.English JC, 3rd, McCollough ML. Transient reactive papulotranslucent acrokeratoderma. J Am Acad Dermatol. 1996;34:6867. doi: 10.1016/s0190-9622(96)80087-9. [DOI] [PubMed] [Google Scholar]
- 2.Dixit N, Sardana K, Tandon S, Singh Y. Atypical aquagenic keratoderma treated with oxybutynin chloride. An Bras Dermatol. 2018;93:308–9. doi: 10.1590/abd1806-4841.20187262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tchernev G, Semkova K, Cardoso JC, Ananiev JJ, Wollina U. Aquagenic keratoderma. Two new case reports and a new hypothesis. Indian Dermatol Online J. 2014;5:30–3. doi: 10.4103/2229-5178.126025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Medhus EJ, DeVore AC, DeVore K. Aquagenic palmoplantar keratoderma therapeutic response to topical glycopyrronium. JAAD Case Rep. 2021;13:17–9. doi: 10.1016/j.jdcr.2021.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim BJ, Kim J, Oh SH. Hereditary papulotranslucent acrokeratoderma: Prominent clinical presentation after water exposure. Ann Dermatol. 2019;31:S52–3. doi: 10.5021/ad.2019.31.S.S52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fertitta L, Charbit-Henrion F, Leclerc-Mercier S, Nguyen-Khoa T, Baran R, Alby C, et al. Bothnian palmoplantar keratoderma: Further delineation of the associated phenotype. Genes (Basel) 2022;13:2360. doi: 10.3390/genes13122360. [DOI] [PMC free article] [PubMed] [Google Scholar]


