SUMMARY
Chronic spontaneous urticaria (CSU) is a dermatological disorder accompanied by itching that greatly affects the quality of life and quality of sleep. Therefore, it is assumed that CSU patients consequently experience reduced melatonin secretion and lower values of serum or salivary melatonin. This pilot study included 20 patients with CSU (chronic urticaria of unknown etiology that lasts for more than 6 weeks) and 10 healthy controls. All subjects were examined by a dermatovenereologist-allergist, as well as an oral pathologist, to exclude oral pathological conditions. Salivary melatonin levels were determined by ELISA and all subjects completed a standardized Dermatology Life Quality Index questionnaire and Pittsburgh Sleep Quality Index on the same day they gave a saliva sample for analysis. According to our results, 86% of CSU patients had decreased values of salivary melatonin, and lower salivary melatonin values significantly correlated with a reduced quality of life in CSU patients. This study was the first to analyze melatonin in CSU patients, also suggesting a possible new therapeutic option for the treatment of CSU.
Key words: Melatonin, Salivary melatonin, Chronic spontaneous urticaria, Sleep disorder, Therapeutic options
Melatonin (N-acetyl-5-methoxytryptamine), a hormone produced mainly by the pineal gland, regulates circadian rhythm and sleep cycle. It improves the onset/duration/quality of sleep, and is centrally involved in antioxidation, circadian rhythmicity maintenance, sleep regulation, and neuronal survival (1). It is synthesized from the amino acid tryptophan and released only at night. Thus, concentrations in the blood are low during the day and begin increasing at dusk; peak secretion occurs between 11 P.M. and 3 A.M. Melatonin diffuses easily from the pineal gland into the blood and cerebrospinal fluid (it is soluble in lipids) (1, 2). According to research literature, melatonin secretion is mostly impaired in sleep disorders, various neuropsychiatric disorders such as depression, anxiety disorder, anorexia and other eating disorders, as well as in malignant diseases, immune disorders, oral disorders, and some dermatological diseases such as atopic dermatitis (AD) and psoriasis (3, 4). Chronic spontaneous urticaria (CSU) is a dermatological disorder accompanied by itching that greatly affects the quality of life and quality of sleep (5). Therefore, it is assumed that, consequently, CSU patients experience reduced melatonin secretion and lower values of melatonin. Since serum melatonin is partially excreted in urine or saliva, urinary or salivary melatonin is a valuable indicator of melatonin level.
This pilot study included 20 patients with CSU (chronic urticaria of unknown etiology that lasts for more than 6 weeks) and 10 healthy controls. The research was conducted at the Department of Dermatology and Venereology, Sestre milosrdnice University Hospital Center and at School of Dental Medicine in Zagreb, with permission from the institutional Ethics Committee (003-06/21-03/030) and with signed consent forms from all study participants. Written informed consent for publication of this article was obtained from all study patients. The study was performed in accordance with the Declaration of Helsinki.
We included adults ≥18 years of age, both men and women, in whom the disease lasted for more than 6 weeks with no obvious cause. We excluded subjects with drug-induced urticaria or angioedema, acute spontaneous urticaria, chronic urticaria of known cause, hereditary angioedema, urticarial vasculitis, periodontal disease, oral infections or other inflammatory processes, oral ulcers and carcinoma, xerostomia, malignant diseases, mental disorders, and pregnant women. The first 20 patients from our clinic who met the criteria were included in the study. Control group included healthy subjects who did not suffer from skin, malignant or psychiatric diseases. All subjects completed the standardized Dermatology Life Quality Index (DLQI) questionnaire and Pittsburgh Sleep Quality Index (PSQI) on the same day they gave a saliva sample for analysis. CSU patients also completed questionnaires on disease activity (Urticaria Activity Score, UAS) and control test (Urticaria Control Test, UCT). All participants were given instructions on proper saliva collection and on consumption of food, beverages, alcohol, smoking, and proper hygiene prior to saliva collection. Also, all subjects were examined by a dermatovenereologist-allergist, as well as by an oral pathologist, to exclude oral pathological conditions. Salivary melatonin levels were determined by the enzyme-linked immunosorbent assay (ELISA) at the Clinical Department of Chemistry using appropriate reagents (BÜHLMANN Laboratories AG, Schönenbuch, Switzerland). Saliva sampling was performed in the evening (10 P.M.-12 A.M.) using the indirect method of saliva collection with Salivette® (KemoLab d.o.o., Zagreb, Croatia) commercial saliva collection tubes (6, 7). The samples were stored in a refrigerator at 4 °C for a maximum of 72 hours and then stored in a specialized refrigerator at -80 °C, where they were stored until analysis. Melatonin values were recorded as reduced or normal (a reduced value was considered to be lower than 4.2 pg/mL). The t-test, Pearson correlation coefficient and linear regression were used on statistical analysis.
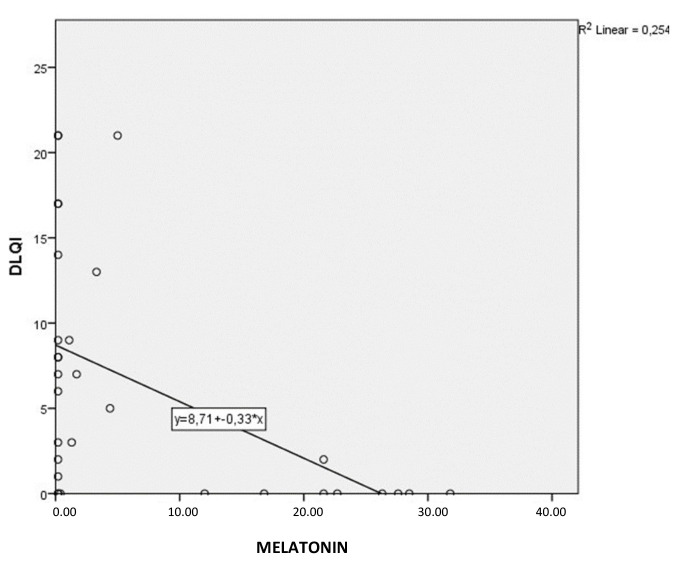
According to our results, 86% of CSU patients and 20% of healthy subjects had decreased values of salivary melatonin. Salivary melatonin values significantly correlated with a reduced quality of life. This correlation was moderate, linear and negative (r=-0.504; p≤0.045, Pearson correlation), meaning that as melatonin values increased, DLQI scores decreased. A scatter diagram shows that the relationship may be more exponential than linear, but the exponential function did not better define the relationship (Fig. 1). According to linear regression, for each 1 pg/mL increase in melatonin, the DLQI decreased by 0.3 scalar points. Melatonin did not correlate with gender or age, either in the total sample or in the patient sample alone, or with disease duration. There were no significant gender differences, although patients were slightly older than healthy controls (44±14 vs. 33±12 years; p=0.036).
Fig. 1.
Correlation and line of linear regression with prediction equation (y is the origin on the abscissa, and the value on x indicates the rate of change of DLQI with increasing melatonin). DLQI = Dermatology Life Quality Index
For total sample, melatonin did not correlate with PSQI scores, but results were near the threshold of significance, meaning that analysis of a larger sample could reveal a correlation. DLQI and PSQI were significantly, positively and linearly interrelated. In CSU patients, the correlation between melatonin and UAS score was not significant. The multiple regression model for melatonin (controlling for all predictors) was not statistically significant, although DLQI was significant.
Our results of melatonin analysis support the existing data that CSU patient impaired quality of life is particularly affected by reduced sleep quality, most often due to itching (8). The most common sleep disturbances included difficulty falling asleep, waking up too early and feeling tired, which impairs daily functioning, consequently leading to limitations in the patient social life (5). In addition, CSU patients are also more prone to the development of mental disorders (5). According to research literature, among psychological/psychiatric disorders in chronic urticaria patients, most common are sleep disorders (36.7%), followed by anxiety disorders (30.6%), mood disorders (29.4%), post-traumatic stress disorder (17.3%), and psychosomatic disorders (17.2%) (9).
Currently, the only meaningful literature data on melatonin values for diseases similar to CSU, in which itch impairs sleep and quality of life, are related to atopic dermatitis patients. In atopic dermatitis, multiple causes contribute to sleep disturbances, including learned scratching behavior and increased monoamines. There are studies that showed lower melatonin levels, as well as an attempt at melatonin supplementation due to disturbed sleep quality caused by intense itching in these patients (10). Furthermore, recent research (results of experimental and clinical studies) found that lower serum melatonin correlated with more severe atopic dermatitis and that melatonin supplementation improved sleep quality. If melatonin is administered at an adequate dose, increased melatonin levels in the body can reduce disease severity (3, 11). Since CSU and atopic dermatitis patients have similar issues, these results could be useful for CSU patients as well. It should also be mentioned that, due to significantly increased sleep disturbances and common psychiatric disorders in CSU patients, a multidisciplinary approach is necessary to treat them appropriately, including collaboration with clinical psychologists and psychiatrists, as well as attempts to design new therapeutic options.
Currently, exogenous melatonin is recommended for patients with sleep disorders as a possible pharmacotherapeutic option, e.g., for frequent insomnia and circadian rhythm disorders, as melatonin has both sleep-promoting and chronobiotic effects (12). According to recent guidelines, published in Frontiers Psychiatry (International Expert Opinions and Recommendations), insomnia can be treated with 2-10 mg of slow release melatonin one to two hours before sleeping time (12). Many studies with melatonin administration demonstrated it to improve the quality of sleep in various disorders (12-16). Concerning patients with chronic skin diseases (e.g., atopic dermatitis and CSU), it is very important not to forget their disturbed sleep and impaired quality of life.
This study was the first to analyze melatonin in CSU patients and our results showed these patients to have low melatonin values. Therefore, we recommend melatonin supplementation as a possible new therapeutic option for the treatment of sleep disturbances in CSU patients. Although this pilot study included a small number of patients, it may be useful as a basis for further studies.
References
- 1.Xie Z, Chen F, Li WA, Geng X, Li C, Meng X, et al. A review of sleep disorders and melatonin. Neurol Res. 2017;39:559–65. 10.1080/01616412.2017.1315864 [DOI] [PubMed] [Google Scholar]
- 2.Neubauer DN, Pandi-Perumal SR, Spence DW, et al. Pharmacotherapy for insomnia in adults. J Cent Nerv Syst Dis. 2018;10:1179573518770672. Published online 2018 Apr 19. https://www.uptodate.com/contents/pharmacotherapy-for-insomnia-in-adults 10.1177/1179573518770672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jaworek AK, Szepietowski JC, Hałubiec P, Wojas-Pelc A, Jaworek J. Melatonin as an antioxidant and immunomodulator in atopic dermatitis – a new look on an old story: a review. Antioxidants. 2021;10:1179. 10.3390/antiox10081179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kartha LB, Chandrashekar L, Rajappa M, Menon V, Thappa DM, Ananthanarayanan PH. Serum melatonin levels in psoriasis and associated depressive symptoms. Clin Chem Lab Med. 2014;52:e123–5. 10.1515/cclm-2013-0957 [DOI] [PubMed] [Google Scholar]
- 5.Maurer M, Giménez-Arnau A, Ensina LF, Chu CY, Jaumont X, Tassinari P. Chronic urticaria treatment patterns and changes in quality of life: AWARE study 2-year results. World Allergy Organ J. 2020;13:100460. 10.1016/j.waojou.2020.100460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Meštrović-Štefekov J, Lugović-Mihić L, Hanžek M, Bešlić I, Japundžić I, Karlović D. Salivary cortisol values and personality features of atopic dermatitis patients: a prospective study. Dermatitis. 2022. September-October;33(5):341–8. Epub 2022 Jan 28. 10.1097/DER.0000000000000834 [DOI] [PubMed] [Google Scholar]
- 7.Ćesić D, Lugović-Mihić L, Ferček I, Grginić Gverić A, Jelić M, Bešlić I, et al. Salivary microbiota is significantly less diverse in patients with chronic spontaneous urticaria compared to healthy controls: preliminary results. Life (Basel). 2021;11:1329. 10.3390/life11121329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Abdel Latif OM. Impact of severity of CSU on sleep, anxiety and depressive symptoms in adults. Eur Acad Res. 2017;2:1145–57. [Google Scholar]
- 9.Konstantinou GN, Konstantinou GN. Psychiatric comorbidity in chronic urticaria patients: a systematic review and meta-analysis. Clin Transl Allergy. 2019;9:42. 10.1186/s13601-019-0278-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hendricks AJ, Manivannan M, Shi VY. Clinical pearls on sleep management in atopic dermatitis. Dermatitis. 2019;30:287–93. 10.1097/DER.0000000000000523 [DOI] [PubMed] [Google Scholar]
- 11.Bertino L, Guarneri F, Cannavò SP, Casciaro M, Pioggia G, Gangemi S. Oxidative stress and atopic dermatitis. Antioxidants. 2020;9:196. 10.3390/antiox9030196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Palagini L, Manni R, Aguglia E, Amore M, Brugnoli R, Bioulac S, et al. International expert opinions and recommendations on the use of melatonin in the treatment of insomnia and circadian sleep disturbances in adult neuropsychiatric disorders. Front Psychiatry. 2021;12:688890. 10.3389/fpsyt.2021.688890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zambrelli E, Lividini A, Spadavecchia S, Turner K, Canevini MP. Effects of supplementation with antioxidant agents on sleep in autism spectrum disorder: a review. Front Psychiatry. 2021;28;12:689277. doi: 10.3389/fpsyt.2021.689277 10.3389/fpsyt.2021.689277 [DOI] [PMC free article] [PubMed]
- 14.Wang XQ, Wang DQ, Bao YP, Liu JJ, Chen J, Wu S, et al. Preliminary study on changes of sleep EEG power and plasma melatonin in male patients with major depressive disorder after 8 weeks treatment. Front Psychiatry. 2021;12:736318. 10.3389/fpsyt.2021.736318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yardimci A, Ozdede MR, Kelestimur H. Agomelatine, a potential multi-target treatment alternative for insomnia, depression, and osteoporosis in postmenopausal women: a hypothetical model. Front Psychiatry. 2021;12:654616. 10.3389/fpsyt.2021.654616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bešlić I, Lugović-Mihić L, Vrtarić A, Bešlić A, Škrinjar I, Hanžek M, et al. Melatonin in dermatologic allergic diseases and other skin conditions: current trends and reports. Int J Mol Sci. 2023;24:4039. 10.3390/ijms24044039 [DOI] [PMC free article] [PubMed] [Google Scholar]