Abstract
The new 2023 update of the International Federation of Gynecology and Obstetrics (FIGO) staging system for endometrial cancer incorporates the advances made in the understanding of the pathology and molecular classifications into the staging system. While the new staging system aids in precision medicine and may lead to better documentation of prognostic risk categories of endometrial cancer, it is complex and calls for an integrated approach and better communication between multiple disciplines involved in the management of endometrial cancer. In this review article, we address how the referral patterns to imaging services might change considering the updated staging system for endometrial cancer. We also discuss the practical aspects and nuances involved in the radiology service delivery and reporting practices as we adopt the new FIGO staging system for managing endometrial cancer patients.
Keywords: FIGO endometrial cancer staging, imaging, staging, endometrial cancer, uterus
Introduction
The endometrial cancer staging system was updated in 2023 by the International Federation of Gynecology and Obstetrics (FIGO) Women's Cancer subcommittee on Endometrial Cancer Staging. 1 Since 2009, there has been a significant improvement in understanding the different histological types, tumor patterns, and molecular classifications of carcinoma endometrium. 2 In each of the four stages, new subclassifications have been proposed and modified according to the new molecular and histological categorization. The primary purpose of the new FIGO staging system was to provide evidence-based context for treatment recommendations and to improve data-collection pertaining to patient outcomes in the future.
Uterine cancer was previously thought to be a disease of the developed world. However, there is a rising trend in the incidence of endometrial cancer in developing countries due to an increase in the risk factors. The risk factors for endometrial cancer include conditions associated with unopposed estrogen exposure (early menarche, nulliparity, late menopause, estrogen-only hormonal therapy, and polycystic ovarian syndrome), diabetes, obesity, tamoxifen therapy, previous pelvic irradiation and familial cancer syndromes like Lynch syndrome and Cowden syndrome. The burden of endometrial cancer in India is increasing and the National Cancer Registry of India has projected a cumulative risk of 1 in 190 and an estimated 5-year prevalence of 6.56 per 100,000 women. 3 Thus, developing an understanding of the new FIGO update is relevant in our context. In this review, we present the 2023 FIGO update for endometrial cancer and the role of imaging. We also present the implications of the new FIGO staging system on the use of imaging services for the management of patients with endometrial cancer.
Comparison of the 2023 version and 2009 version of the FIGO Staging System/2017 AJCC Eighth Edition
The new 2023 FIGO staging system for endometrial cancer has been tabulated in Table 1 . Carcinoma endometrium is surgically staged and pathologically examined. The molecular and histological classification and the essential points relevant to understanding of the staging system have been summarized in Table 2 and 3 . The 2023 staging system includes major revisions in each stage, and they are summarized below.
Table 1. New 2023 FIGO staging system of carcinoma of the endometrium (adapted from Berek et al) 1 .
| FIGO Stage | Carcinoma endometrium descriptors |
|---|---|
| Stage I | Lesion confined to the body of uterus and the ovary |
| IA | Disease limited only to the endometrium/a nonaggressive histological type (low-grade endometroid carcinoma), with invasion of <50% myometrium with no or focal LVSI/a good prognosis disease IA1: Nonaggressive histological type limited to an endometrial polyp/confined to endometrium only IA2: Nonaggressive histological types involving <50% myometrium with no or focal LVSI IA3: Low-grade endometrioid carcinomas limited to uterus and ovary (good prognosis disease) |
| IB | Nonaggressive histological types with invasion of ≥ 50% of the myometrium, and with either no or only focal LVSI |
| IC | Aggressive histological types limited to a polyp or lesion confined to the endometrium |
| Stage II | Nonaggressive histological types with invasion of cervical stroma without extrauterine extension/with substantial LVSI OR an aggressive histological type with myometrial invasion |
| IIA | Nonaggressive histological types with invasion of the cervical stroma |
| IIB | Nonaggressive histological types with substantial LVSI |
| IIC | Aggressive histological types with any degree of myometrial involvement |
| Stage III | Tumor of any histological subtype with local and/or regional spread |
| IIIA | Invasion of uterine serosa or adnexa or both; either by direct extension or metastasis IIIA1: Spread to ovary/fallopian tube (except when meeting criteria of stage IA3) IIIA2: Involvement of uterine subserosa/spread through uterine serosa |
| IIIB | Metastasis or direct spread to vagina and/or to parametria or the pelvic peritoneum IIIB1: Metastasis or direct spread to vagina and/or parametria IIIB2: Metastasis to pelvic peritoneum |
| IIIC | Metastasis to pelvic/para-aortic lymph nodes or to both IIIC1: Metastasis to pelvic lymph nodes IIIC1i: Micrometastasis IIIC1ii: Macrometastasis IIIC2 Metastasis to the para-aortic lymph nodes up to level of renal vessels, with or without metastasis to pelvic lymph nodes IIIC2i: Micrometastasis IIIC2ii: Macrometastasis |
| Stage IV | Spread to bladder mucosa and/or to intestinal mucosa and/or evidence of distance metastasis |
| IVA | Invasion of bladder mucosa and/or intestinal/bowel mucosa |
| IVB | Abdominal peritoneal metastasis beyond pelvis |
| IVC | Distant metastasis, which includes metastasis to any extra- or intra-abdominal lymph nodes above the renal vessels, lungs, liver, brain, or bone |
Abbreviations: FIGO, International Federation of Gynecology and Obstetrics; LVSI, lymphovascular space involvement.
Table 2. Grade and histological subtype relevant to staging of carcinoma endometrium 1 .
| • Nonaggressive histological types: low-grade (grades 1 and 2) endometrioid carcinoma (EEC) • Aggressive histological types: high-grade EECs (grade 3), serous carcinoma (SC), clear cell carcinoma (CCC), mixed carcinoma (MC), undifferentiated carcinoma (UC), carcinosarcoma (CS), and other unusual types like mesonephric-like and gastrointestinal type mucinous carcinomas. • Grade of EEC (based upon the proportion of solid areas): ○ Low grade ▪ Grade 1 (≤5%) ▪ Grade 2 (6%–50%) ○ High grade ▪ Grade 3 (>50%) ○ Nuclear atypia excessive for the grade raises the grade of grade 1 or 2 tumor by one • High-grade EECs (grade 3): prognostically, clinically, and molecularly heterogenous disease and needs molecular classification (to differentiate an excellent prognosis group (POLEmut in early-stage disease) from a bad prognosis group (p53 abnormal) |
Table 3. Key points about FIGO 2023 staging system for carcinoma endometrium 1 .
| • Carcinoma endometrium is surgically staged and pathologically examined • Grades, histological type, and LVSI should always be recorded • Wherever available molecular classification testing (POLE mut , MMRd, NSMP, p53abn) is advisable for prognostic risk-group stratification and as treatment influencing factors • LVSI 4 : negative (0 vessels); focal (<5 vessels); extensive/substantial (≥5 vessels involved) • SLN biopsy increases the detection of low-volume disease in lymph nodes and is considered a suitable alternative to systematic lymphadenectomy for staging proposes • It is essential to distinguish low-grade endometrioid carcinomas involving both the endometrium and ovaries (stage IA3) from extensive spread of carcinoma endometrium to the ovary (stage IIIA1) • Macro metastases are >2 mm in size whereas micro metastases are 0.2–2 mm and/or >200 cells and micro metastases are also considered to be metastatic involvement (pN1 (mi). 5 ITC are ≥0.2 mm and ≤200 cells, prognostic significance of which is unclear |
Abbreviations: FIGO, International Federation of Gynecology and Obstetrics; ITC, isolated tumor cell; LVSI, lymphovascular space invasion; MMRd, mismatch repair deficiency; NSMP, nonspecific molecular profile; POLEmut, POLE mutation; SLN, sentinel lymph node.
Stage I
In the new FIGO staging system, stage 1 tumors are nonaggressive histological types with absence of substantial or extensive lymphovascular space invasion (LVSI) and confined to the uterine corpus or aggressive histological types limited to a polyp or have no myometrial invasion. 1 However, there is a subset of patients with low-grade endometrioid carcinoma that synchronously arise from the endometrium and the ovaries that are classified as stage IA3. Stage 1A3 endometrial cancers are associated with a good prognosis and no adjuvant treatment is recommended. 6 This must be differentiated from extensive spread of the endometrial carcinoma to the ovaries that is classified as stage IIIA1. The following criteria are proposed by the new FIGO system to identify stage IA3: endometrial tumors with less than 50% myometrial invasion; absence of extensive/substantial LVSI, absence of additional metastases and the ovarian tumor is unilateral and confined to the ovary, without evidence of capsular invasion or rupture (equivalent to pT1a ovarian cancer).
Stage II
The new FIGO staging system subclassifies stage II disease into three subclasses such as IIA, IIB, and IIC based on histological type, LVSI, and anatomical extent. The presence of cervical stromal invasion is only applicable for nonaggressive histological subtypes. In these patients, the presence of cervical stromal invasion is staged as FIGO IIA when there is no or focal LVSI and those with substantial or extensive LVSI are FIGO IIB. LVSI has been shown to be a strong and independent prognostic factor for the recurrence of endometrial carcinoma and lymph node metastases and is associated with decreased survival. 7 On the other hand, aggressive histological types with any myometrial involvement are considered as FIGO IIC. This later change in the new staging system will increase the number of patients with stage II endometrial cancers since all patients who were previously staged as FIGO IA and IB would now be staged as IIC based on aggressive histology.
Stage III
In stage III, the tumor has spread outside of the uterus, but confined to the pelvis. The new subclassifications of stage III disease better reflects the prognosis. Stage IIIA1 is adnexal involvement and IIIA2 is uterine serosa infiltration. As detailed earlier, stage IIIA1 should be differentiated from stage IA3 that has disease limited to the uterus and a single ovary. Stage IIIB is now subdivided into two substages: Stage IIIB1 (like the previous stage IIIB) is characterized by involvement of vagina and/or parametria. However, the involvement of pelvic peritoneum is now subclassified as stage IIIB2 (which was previously stage IV). Stage IIIC includes metastases to pelvic or paraaortic lymph nodes or both and is further subdivided into micrometastasis (IIIC1i, IIIC2i) and macrometastasis to the lymph nodes (IIIC1ii, IIIC2ii). The isolated tumor cells are not included as metastatic and are considered as pN0(i + ). There is increasing utilization of sentinel lymph node sampling and ultra staging of lymph nodes to identify small volume disease including micro metastasis which has a better prognosis. 8
Stage IV
Stage IVA is unchanged as the local invasion of bladder and/or bowel mucosa. Stage IVB is a new substage for extra-pelvic peritoneal metastasis and is to be distinguished from stage IIIB2 that is localized pelvic peritoneal infiltration. Distant metastases, including intra-abdominal lymph nodes above the renal vessels or any extra-abdominal lymph nodes or to the liver, lungs, bone, or brain, are now classified as stage IVC.
The risk stratification of endometrial cancer patients based on molecular profiling has been the most significant advance in the management of endometrial cancer. Molecular markers identified by The Cancer Genome Atlas (TCGA) have been added to staging system in the new update. 9 The FIGO 2023 update recommends molecular profiling of endometrial tumor whenever feasible and classifies endometrial cancer based on prognostic groups recommended by TCGA as follows: good prognostic group with pathogenic POLE mutation (POL mut ); intermediate prognostic group with microsatellite instability or mismatch repair deficiency (MMRd) and nonspecific molecular profile (NSMP); and poor prognostic group with p53 abnormality. Based on these molecular prognostic groups early-stage endometrial cancers (stage I and II) are down staged to stage 1A irrespective of histological type and LVSI status if associated with POL mut and upstaged to stage IIC if associated with p53 abnormality. 1 Staging is not affected by intermediate risk molecular profile and molecular profile does not change the stages in advanced endometrial cancers (stages III and IV). 1
Management Algorithm for Endometrial Cancer
Endometrial cancer is confirmed with biopsy or surgical histopathology. Imaging helps in informed decision making in patients being considered for fertility sparing treatment options, acts as baseline prior to deciding on adjuvant treatment options in patients with incomplete surgical staging, and is an important tool for post-treatment surveillance. Early endometrial cancer patients benefit from sentinel lymph node sampling and ultra-staging. Imaging has a role in identifying advanced endometrial cancer patients and those with high-risk features who will benefit from systematic lymphadenectomy. Depending on the risk categories based on histological type and grade of tumor, molecular profile and anatomical extent of spread, adjuvant treatment options range from vaginal brachytherapy, external beam radiotherapy with or without chemotherapy. The flowchart in Fig. 1 summarizes the management of endometrial cancer. The new FIGO staging system recommends molecular profiling of all endometrial cancer patients whenever feasible. In our setting, p53 is likely to have wider adaptability than other markers due to the need for more aggressive treatment in this subset and less cost (500 INR). Moreover, there are previous reports on the incidence of p53 mutation and its association with prognosis among esophageal and cervical cancer patients in India. 10 11 POL mut helps de-escalation of treatment. But it is expensive (polymerase epsilon; 3,000 INR by polymerase chain reaction; 10,000 INR by next-generation sequencing). Also, the facilities and the expertise needed to perform molecular profiling are not widely available in India.
Fig. 1.
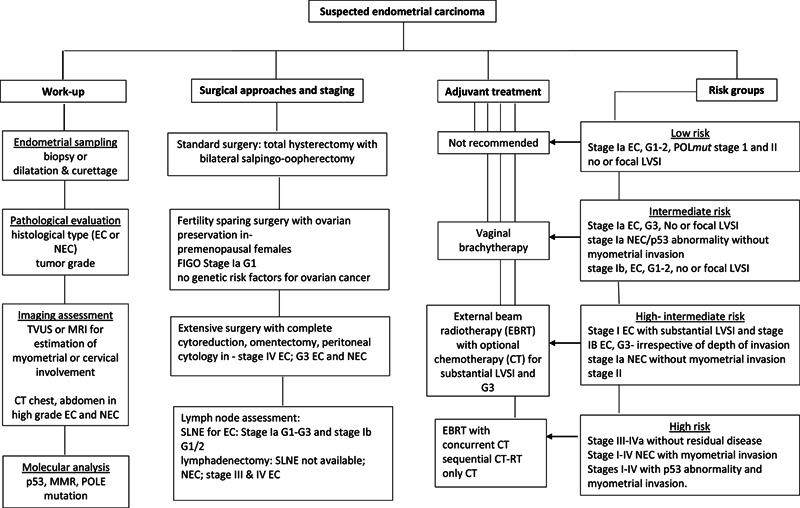
Flowchart showing the management of patients with endometrial cancer. G1/2/3, grade 1/2/3; EC, endometroid-type endometrial carcinoma; LVSI, lymphovascular space invasion; NEC, nonendometroid cancers like serous endometrial carcinoma, carcinosarcoma, and undifferentiated carcinoma; MMR, mismatch repair; POLE, polymerase Epsilon; TVS, transvaginal sonography; SLNE, sentinel lymph node excision; Stage, As per New FIGO staging system for endometrial cancer, version 2023.
Effect of New FIGO Staging System on Referrals to Imaging Services
The revised FIGO staging for endometrial cancer does not call for major changes in the imaging referral guidelines. Instead, there is a call for a more integrated approach to endometrial cancer care where the clinical inputs between the disciplines such as gynecology, gynae-oncology, pathology, radiology, radiation oncology, and medical oncology, and timely and optimal communications between these disciplines are essential to achieve the best possible staging accuracy, prognostic risk stratification and for making optimal and informed treatment-related decisions. The imaging modalities used in the management of endometrial cancer, their indications, strengths, weaknesses are summarized in Table 4 . Table 5 provides the imaging referral guidelines for use by both radiologists and clinical referrers in different clinical scenarios.
Table 4. Imaging modalities for evaluation of endometrial malignancies.
| Imaging Modalities | Indications | Strength | Weaknesses |
|---|---|---|---|
| Transvaginal sonography | First line of imaging investigation for evaluating women with postmenopausal bleeding; intermenstrual or abnormal uterine bleeding in premenopausal women Used for screening patients on hormonal therapy and breast cancer patients on tamoxifen |
Easily available Low cost High negative predictive value in postmenopausal women 12 |
Interobserver variation. Low sensitivity and specificity for depth of myometrial invasion, nodal assessment, and parametrial invasion. |
| CECT scan (thorax + abdomen +pelvis) | Locally advanced endometrial carcinoma High-grade endometroid or serous type of endometrial carcinoma Recurrent/metastatic endometrial carcinoma for response evaluation |
Faster and easily available than PET-CT for distant nodal and distant metastatic workup | Poor soft tissue contrast and spatial resolution. Lower sensitivity and accuracy for locoregional staging in comparison to MRI and in detection of nodal metastasis. |
| MRI (pelvis) | Histological proven endometrial cancer, sonographically suspected endometrial cancer, and vaginal stenosis (when biopsy inaccessible) ESMO and NCCN recommends MRI preoperative workup of endometrial cancer 13 14 |
Best method to delineate endometrial tumor >10 mm. Excellent soft tissue contrast resolution. Facilitates accurate anatomical extent of disease. The diagnostic accuracy for predicting depth of myometrial invasion and cervical stromal invasion improves with dynamic post-contrast MRI. 12 15 16 17 18 19 20 21 Differentiates post-treatment fibrosis and local recurrence. |
Limits the visualization of anatomical details beyond the uterus and pelvis structures. Limited availability of MRI scanner, expertise for image interpretation, and long scan time. Lower sensitivity in evaluation of metastatic pelvic nodes. Motion/metallic implant artifacts from pelvic bones/Hip joints limits anatomical details of pelvis and makes locoregional extension evaluation more difficult. |
| PET-CT | Locoregionally advanced endometrial cancers. Equivocal/indeterminate nodal/distant metastatic lesions on CECT scan. Follow-up imaging of locally advanced endometrial cancers. Evaluation of recurrent disease. |
Detects nodal metastasis with sensitivity (53–73%) specificity (90–97%).
15
16
17
Superior in evaluation of distant metastatic spread and recurrent disease. |
Limited spatial resolution can mask small volume peritoneal disease and small lymph nodes. Physiological uptake in endometrium may mimic cancer, over/underestimate the depth of myometrial invasion. Necrotic/mucinous lesions may show less metabolic activity. |
Abbreviations: CECT, contrast-enhanced computed tomography; ESMO, European Society of Medical Oncology; MRI, magnetic resonance imaging; NCCN, National comprehensive cancer Network; PET-CT, positron emission tomography-computed tomography.
Table 5. Imaging referral guidelines for endometrial cancer.
| Clinical background a | Imaging referral guidelines |
|---|---|
| Scenario 1: Biopsy report available before imaging | |
| Nonaggressive histology | MRI pelvis with contrast Chest radiograph CECT of the thorax, abdomen, and pelvis if MRI pelvis shows FIGO stage III and above |
| Aggressive histology | CECT of the thorax, abdomen, and pelvis Or Whole body PET-CT |
| Scenario 2: Concurrent biopsy and imaging | |
| Biopsy not available | MRI pelvis with contrast to assess the local extent. Chest radiograph |
| Scenario 3: Suspected endometrial cancer on ultrasound or CT | |
| Biopsy not available | Advise gynecology referral, endometrial sampling for further evaluation. |
| Biopsy not feasible as in vaginal stenosis | MRI pelvis with contrast for diagnosis and local staging. |
| Scenario 4: Incidental diagnosis on surgical histopathology and seeking imaging care to decide on a further treatment plan | |
| Early-stage non-aggressive histology (stage 1A) Any stage I/II with POLE mutation |
No further imaging evaluation. Clinical follow-up. |
| Early-stage nonaggressive histology (stage IB,1C, II) and negative sentinel lymph node biopsy | MRI pelvis is recommended for planning vaginal brachytherapy. |
| Early-stage nonaggressive histology (stage IB,1C, II) without lymph node sampling | MRI pelvis is recommended for planning vaginal brachytherapy. CECT of the thorax, abdomen, and pelvis for restaging prior to adjuvant treatment. |
| Late-stage nonaggressive histology (stage III and above). | CECT of the thorax, abdomen, and pelvis as a baseline prior to adjuvant treatment. RT planning CT can be considered if external beam RT is being planned. |
| Aggressive histology (any type of surgery with myometrial invasion) | CECT of the thorax, abdomen, and pelvis as a baseline prior to adjuvant treatment. PET-CT is not recommended until 6 weeks after initial surgery due to metabolically active postoperative bed. |
| All histology types with myometrial invasion and p53 abnormality. | CECT of the thorax, abdomen, and pelvis as a baseline prior to adjuvant treatment. |
| Scenario 5: Being considered for fertility-sparing treatment options | |
| Biopsy is available and shows nonaggressive histology. When the molecular profile is available, exclude p53 abnormality. |
MRI pelvis with contrast for local staging. CECT of the thorax, abdomen, and pelvis to exclude metastases. |
| Scenario 6: Seeking imaging care for surveillance | |
| Surgical histopathology is available and nonaggressive histology | Early stage and baseline imaging when available: The clinical examination findings will dictate the need for imaging. Late stage: CECT thorax, abdomen, and pelvis to reassess disease status. PET-CT may be an alternative imaging modality. |
| Surgical histopathology is available and aggressive histology | CECT thorax, abdomen, and pelvis to reassess disease status. PET-CT may be an alternative imaging modality. |
| Surgical histopathology is not available | CECT thorax, abdomen, and pelvis to reassess disease status. PET-CT may be an alternative imaging modality. |
Abbreviations: CECT, contrast-enhanced computed tomography; FIGO, International Federation of Gynecology and Obstetrics; MRI, magnetic resonance imaging; PET-CT, positron emission tomography-computed tomography.
If there is clinical suspicion of Lynch syndrome due to prior cancer history or significant family history breast screening with bilateral mammograms and breast ultrasound and colon screening is appropriate.
Imaging Findings and the Implications of New FIGO Staging System on Radiology Reporting Practices
Before providing radiology reports along the line of the new FIGO staging system for endometrial cancer, version 2023, radiologists must consider if they have information pertaining to age, clinical presentation, histopathological type of uterine corpus neoplasm, and if fertility-sparing is being considered. Knowledge of how the diagnosis was made, and past surgical and treatment history are also useful considerations in image interpretation especially while reporting postoperative and surveillance imaging.
Radiologists could be in one of the following situations while interpreting imaging of patients with endometrial cancer:
-
a) Biopsy report is available while reporting staging magnetic resonance imaging (MRI): Accurate local staging is possible when information related to pelvic organ infiltration is combined with the histopathological type of the tumor. Table 6 provides the MRI protocol for staging endometrial cancer and Fig. 2 shows the optimal plane of oblique axial and coronal images that must be perpendicular and parallel to the long axis of the uterus. Depth of myometrial invasion is best determined using a combination of axial oblique T2-weighted, diffusion-weighted imaging (DWI) and post-contrast images obtained 2 minutes 30 seconds following the injection of contrast when there is maximum differential enhancement between the tumor and the myometrium. 23 Combination of T2 and DWI has comparable diagnostic accuracy to post-contrast images for determining the depth of invasion and can be used in resource-constrained settings. 24 25 Uninterrupted T2 hypointense junctional zone and early phase subendometrial enhancement are imaging signs of intact myometrium ( Fig. 3 ). 26 27 The depth of myometrial invasion is measured from the expected inner margin of the myometrium to the outermost edge of the tumor infiltrating the myometrium and compared with the full thickness of myometrium and is reported as invasion of less than or more than 50% of myometrial thickness. 17 22 Figs. 3 4 5 show the imaging findings of early endometrial cancer and demonstrate the value of knowing the histopathological type of endometrial cancer for accurate staging according to the updated staging system. Cervical stromal invasion is best determined on T2-weighted sagittal and axial images and 4 minutes delayed post-contrast images and is seen as replacement of T2 hypointense cervical stroma by iso to mildly hyperintense tumor ( Fig. 5 ). 17 20 22
We may see a subset of patients with biopsy diagnosis of endometrial cancer and an ultrasound report of US O-RADS 4/5 adnexal mass. The new FIGO staging system emphases the importance of identifying synchronous early stage endometrial and ovarian cancers (stage 1A3) from contiguous infiltration of ovaries by advanced endometrial cancer (stage IIIA1) and has laid guidelines for differentiating the two. 1 In patients with early endometrial cancer with less than 50% myometrial infiltration, a unilateral malignant ovarian mass without features of ascites, peritoneal disease, or other metastases corresponding to FIGO stage 1a ovarian cancer can be reported as stage 1A3 ( Fig. 6 ). On the other hand, ovarian masses due to contiguous infiltration in advanced endometrial cancer are staged as IIIA1 endometrial cancer ( Fig. 7 ). However, in patients with synchronous endometrial and ovarian cancer with more advanced stages of one of the two cancers, there will be dilemma in both the choice of imaging modality and in providing staging information. Contrast-enhanced computed tomography (CT) of the thorax, abdomen, and pelvis is appropriate in these patients and can be advised for completion of staging.
-
b) Biopsy report not available during the reporting session: The information pertaining to the type of uterine neoplasm may not be available during the reporting session when the findings are unsuspected. For example, endometrial cancer or malignant uterine mass can be detected on transvaginal ultrasound in patients with postmenopausal bleeding; contrast-enhanced CT or MRI pelvis or MRI lumbosacral spine performed for other unrelated indications. Also, in clinical situations where imaging and biopsy are performed in parallel for logistic reasons, in patients with vaginal stenosis where biopsy is not feasible, and accessibility to histopathology reports will affect availability of biopsy reports to the reporting radiologists. In these situations, staging is not possible.
In symptomatic postmenopausal women with endometrial thickening more than or equal to 5 mm on transvaginal scan, endometrial sampling is advised for further evaluation. 28 In asymptomatic and premenopausal women, the referral guidelines are unclear and further management decisions are taken by gynecologists based on the clinical assessment and review of risk factors. 29 Similarly, in patients with unsuspected endometrial thickening on CT performed for other reasons it is best to advise transvaginal ultrasound for further evaluation since small hydrometra, hematometra and changes through the menstrual cycle can affect the appearance endometrium may mimic pathological endometrial thickening. 30
If an MRI of the pelvis is being reported and biopsy details are not available, the next best practice would be to report the involvement of certain key anatomical structures that can help the clinical referrer with accurate staging. These include reporting the location of the tumor ( Fig. 8 ), the depth of myometrial infiltration, cervical stromal infiltration; adnexal, uterine serosal, vaginal, parametrial ( Figs. 7 and 8 ), and pelvic peritoneal infiltration; and infiltration of the adjacent structures like the bladder and the bowel; lymph nodes, and if there are suprarenal nodes; and hydroureter. These findings can aid informed decision-making and surgical planning. Further evaluation with contrast-enhanced CT of the thorax, abdomen, and pelvis can be advised depending on the findings noted on the MRI.
c) Fertility sparing: Imaging plays an important role in excluding contraindications to fertility-sparing treatment options in young women with Grade 1 endometroid endometrial cancer. 31 Contrast-enhanced MRI of the pelvis is the imaging modality of choice for excluding any myometrial and deep cervical stromal invasion, skip lesions or metastases vagina or parametrium, synchronous ovarian malignancy, and pelvic lymph node metastases ( Figs. 9 and 10 ). In patients with intermediate (MMRd and NSMP) and high-risk (p53 abnormality) molecular profiles, contrast-enhanced CT of the thorax, abdomen, and pelvis is a useful addition for excluding distant metastases. 22
d) Reporting of postoperative or surveillance imaging: Depending on the local practice, postoperative imaging that follows incomplete surgical staging could be a combination of MRI pelvis and chest radiograph or contrast-enhanced CT of the thorax, abdomen, and pelvis. The purpose of imaging in this setting is to reassess the tumor burden and decide on the type of adjuvant treatment, which can either be external beam radiotherapy and/or chemotherapy. Thus, considering the type and the extent of surgery is useful for reporting. A residual tumor in the pelvis is seen as asymmetrical or enhancing nodular soft tissue thickening in the vaginal vault ( Fig. 11A ). Assessing the imaging appearance of the surgical bed and locating significant pelvic lymph nodes is useful for planning radiation therapy. Lymphatic collections or postoperative seromas are common following pelvic lymphadenectomy 32 and are seen as loculated fluid density collections along the pelvic side walls and may persist for several months ( Fig. 11B ). Comparison with previous imaging and taking note of surgical details is key to recognizing these collections in the pelvis. Postoperative inflammatory changes in the surgical bed are FDG avid on positron emission tomography-computed tomography (PET-CT) for 8 to 12 weeks and image interpretation can be challenging during this period. 16 33 34 However, during post-treatment surveillance, PET-CT can be considered in symptomatic patients to exclude recurrence in the lymph nodes and distant metastases when routine imaging surveillance with CT is negative. 35 36
Table 6. MRI protocol for endometrial carcinoma 12 15 17 20 22 .
| Mandatory sequences | Imaging planes |
|---|---|
| Large FOV—T2WI | Axial and coronal |
| Small FOV high-resolution T2W | Sagittal T2W of the pelvis Oblique coronal and oblique axial, angled parallel and perpendicular to endometrial cavity respectively. |
| EPI diffusion-weighted imaging | Oblique axial or sagittal plane as T2W Two b values (b = 0, b = 800 or 1000) |
| T1WI (FS 3D GRE) DCE | T1FS (3D GRE) weighted gradient echo volumetric interpolated breath hold images in oblique axial or sagittal planes obtained in: Early phase (30–60 s) Equilibrium phase (120–180 s) Delayed phase (post 4 min) |
Abbreviations: 3D, three-dimensional; EPI, echo-planar imaging; FOV, field of view; FS, fat-suppressed; GRE, gradient echo; MRI, magnetic resonance imaging; T2W, T2-weighted.
Fig. 2.
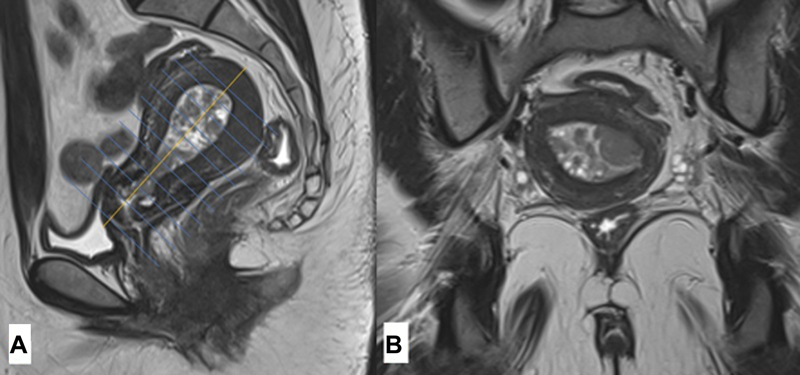
Recommended planes of imaging for accurate estimation of depth of myometrial invasion and cervical stromal invasion. ( A ) Midline sagittal image showing the long axis of the endometrial cavity and oblique axial image ( B ) is planned perpendicular to the long axis of the endometrial cavity.
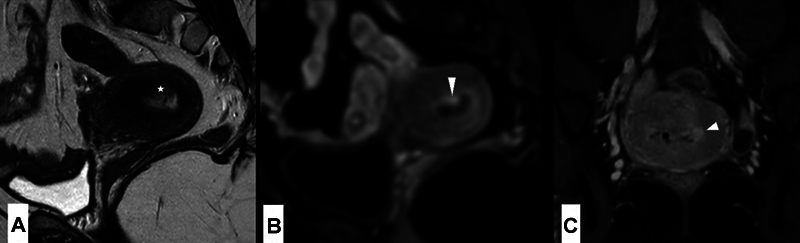
Fig. 3.
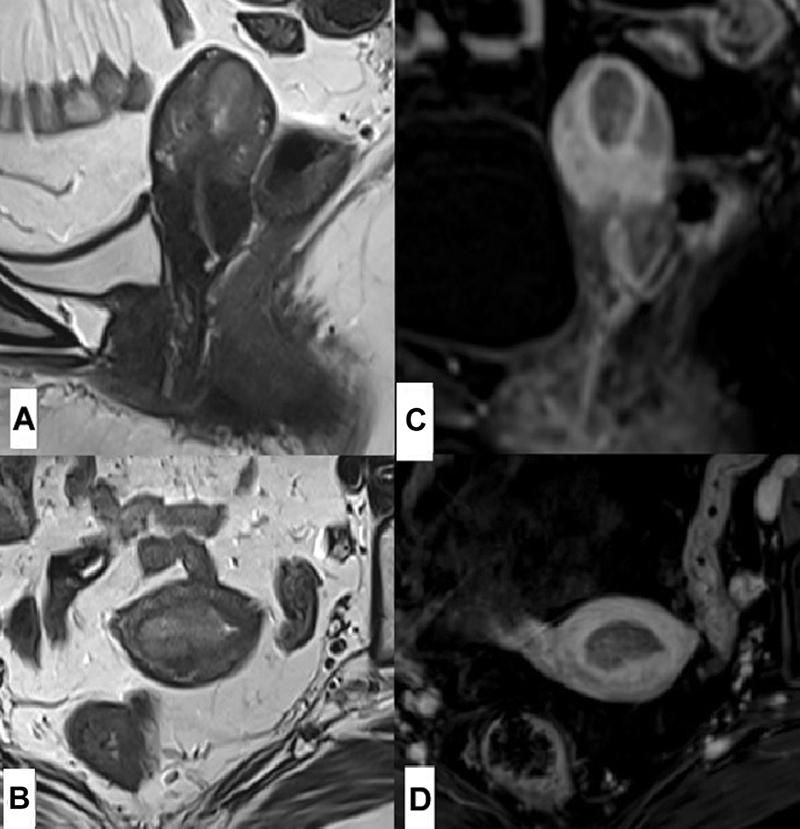
Endometrial biopsy of a 57-year-old female with postmenopausal bleeding showed grade 1 endometroid endometrial carcinoma. Magnetic resonance imaging high-resolution T2 weighted ( A ) sagittal and ( B ) axial images showed intermediate signal intensity mass in the endometrial cavity in the fundus region with the intact T2 hypointense junctional zone. ( C, D ) Sagittal and axial early post-contrast images show uninterrupted smooth sub-endometrial enhancement consistent with tumor confined to the endometrial cavity. In line with the new staging system, this would be staged 1A1 endometrial cancer.
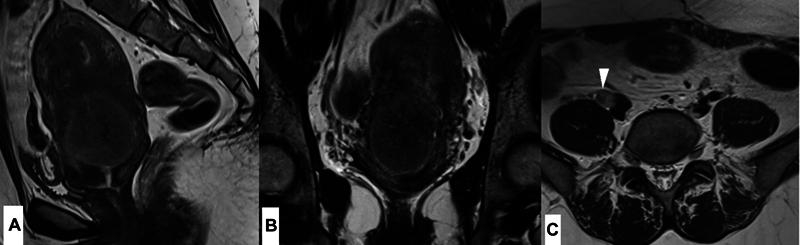
Fig. 4.
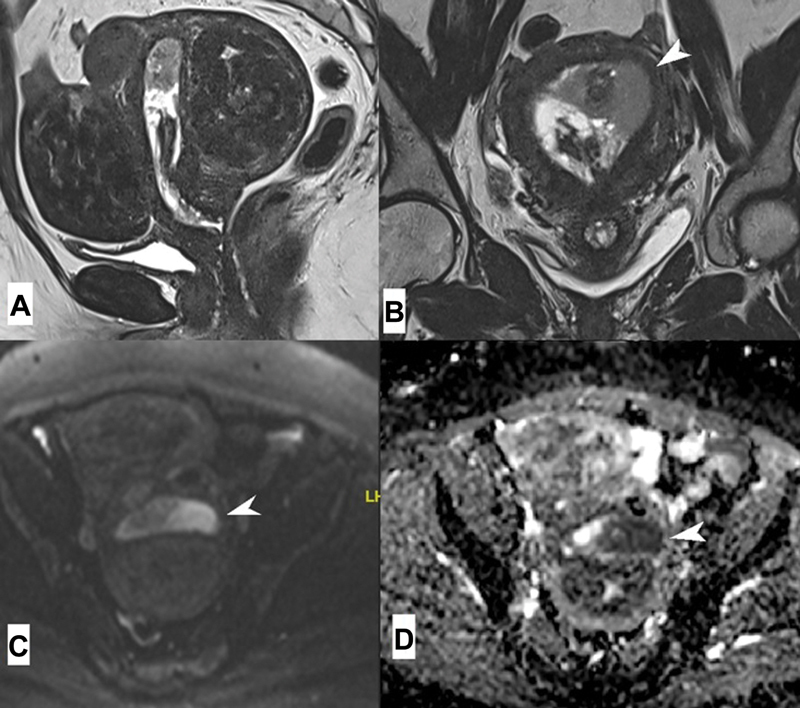
Endometrial biopsy of a 61-year-old female with postmenopausal bleeding showed high-grade serous carcinoma. Magnetic resonance imaging (MRI) high-resolution T2 weighted ( A ) sagittal and ( B ) coronal and ( C, D ) diffusion-weighted imaging showed a heterogeneous diffusion restricting growth within the endometrial cavity infiltrating less than 50% of the myometrial thickness in the left side of the fundus of the uterus (arrowheads in b,c,d). MRI was reported as International Federation of Gynecology and Obstetrics (FIGO) 1A endometrial cancer according to the 2009 FIGO staging system. Given the nonendometroid or an aggressive histological type and myometrial infiltration, according to the new 2023 FIGO staging system, this patient would be staged as FIGO IIC endometrial carcinoma. Also, note the multiple classical intramural fibroids.
Fig. 5.
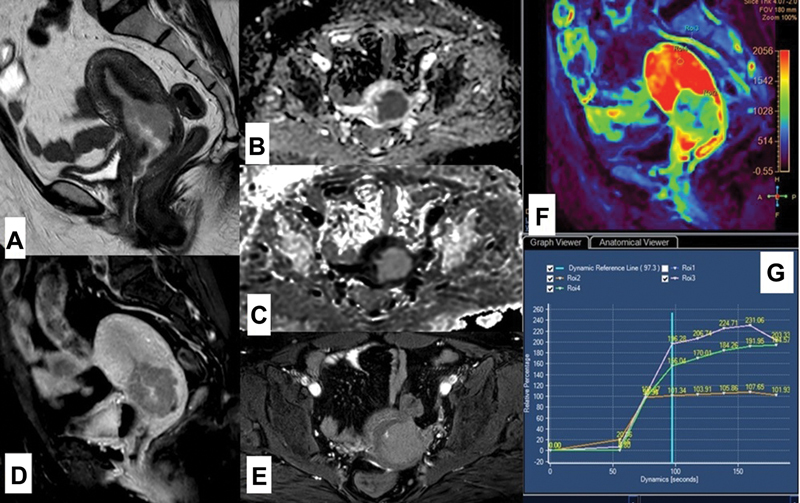
A 45-year-old female with grade 3 endometrioid and serous endometrial adenocarcinoma underwent magnetic resonance imaging (MRI) pelvis with contrast for staging. ( A ) T2-weighted sagittal image and ( B, C ) diffusion-weighted imaging with apparent diffusion coefficient map show T2 intermediate signal diffusion restricting growth in the endometrial cavity (*) and endocervical region with myometrial and posterior cervical stromal infiltration. ( D ) Post-contrast sagittal image showing poor enhancement of the endometrial mass in comparison with the myometrium. ( E ) Delayed axial post-contrast image shows persistent enhancement. ( F ) Color map showing prominent differentiation of the perfusion hue. ( G ) Kinetic curves of dynamic contrast-enhanced MRI compared contrast enhancement kinetics of the external iliac artery (top pink curve) with rapid and steep curve, myometrium with steep early wash-in (green curve) and the mass in the endometrium and endocervix showing slower and stunted wash-in (orange curve) and persistent plateau. This patient was staged as IIC endometrial cancer.
Fig. 6.
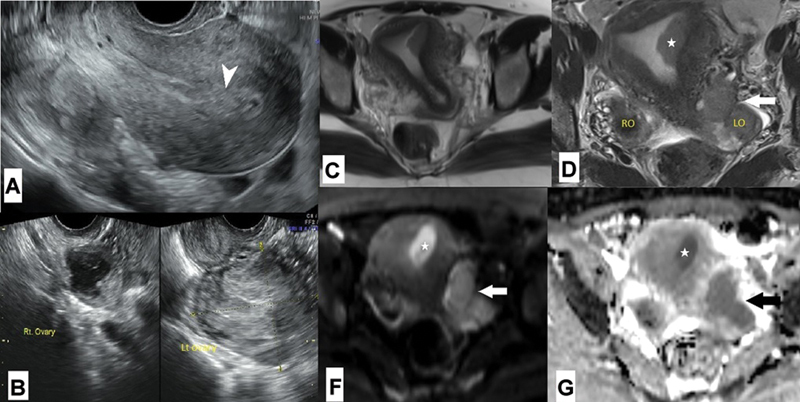
A 35-year-old who was being treated for primary infertility had ( A, B ) transvaginal ultrasound showing endometrial thickening (arrowhead) and US-O-RADS 4 left ovarian mass. Initial endometrial biopsy revealed endometrial hyperplasia. ( C, D ) Axial T2-weighted magnetic resonance imaging and ( E, F ) diffusion-weighted imaging with apparent diffusion coefficient map showed intermediate signal diffusion restricting eccentric soft tissue mass in the endometrial cavity near the left cornua of the uterus (*) with no myometrial invasion and an irregular lobulated predominantly solid diffusion restricting left ovarian mass (arrow) suggestive of malignant left ovarian mass. The right ovary was normal. There was no obvious peritoneal disease. The patient underwent total abdominal hysterectomy, bilateral salpingo-oophorectomy, omentectomy, and pelvic and para-aortic lymphadenectomy. Surgical histopathology revealed International Federation of Gynecology and Obstetrics (FIGO) 1A grade 1 endometroid endometrial carcinoma and FIGO 1C2 endometroid adenocarcinoma of the ovary. She was given adjuvant chemotherapy following the surgery.
Fig. 7.
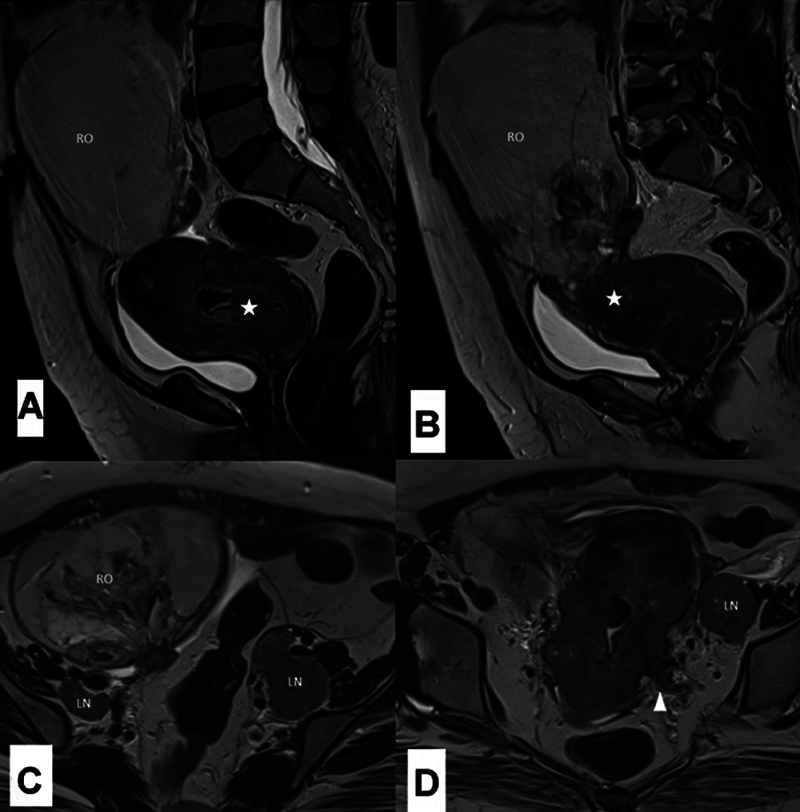
A 36-year-old female with advanced endometrial cancer underwent magnetic resonance imaging (MRI) pelvis. ( A, B ) T2 sagittal MRI showing a large ill-defined intermediate signal intensity endometrial mass (*) infiltrating full thickness of myometrium, uterine serosa, cervix, and the vagina. There is a large predominantly cystic mass with solid areas in the right ovary and appears contiguous with the uterine growth. ( C, D ) T2 axial MRI shows left parametrial infiltration (arrow in D) and bilateral multiple iliac lymph nodes. This is an example of new International Federation of Gynecology and Obstetrics IIIC1ii endometrial cancer.
Fig. 8.
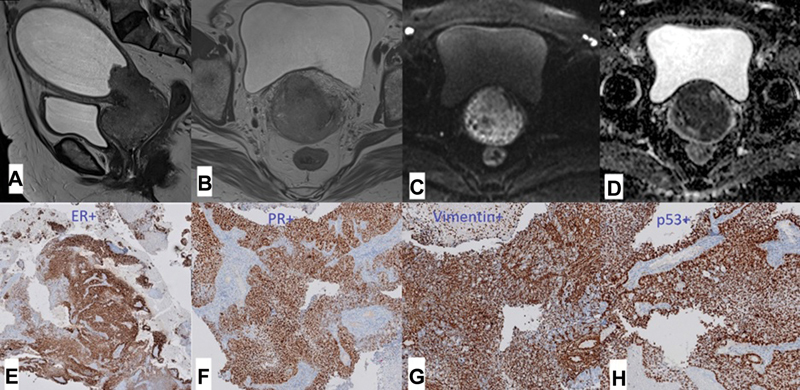
A 49-year-old with bleeding and fowl smelling vaginal discharge was referred with clinically suspected carcinoma cervix. Biopsy revealed grade 3 endometroid endometrial carcinoma and molecular profile showed p53 abnormality. Magnetic resonance imaging high-resolution T2 weighted ( A ) sagittal and ( B ) axial and ( C, D ) diffusion-weighted imaging images with apparent diffusion coefficient map showed polypoidal intermediate signal intensity growth lower uterus and cervix infiltrating the cervical stroma, vagina, and the left parametrium, and associated with a large hydrometra. There was no evidence of metastases on computed tomography (not shown). ( E – H ) Histopathology slides of immunohistochemistry tests show positive staining for ( E ) estrogen receptors, ( F ) progestin receptors and ( G ) vimentin, thus proving endometrial origin of the tumor and was also positive for p53 mutation ( H ). The patient underwent neoadjuvant chemotherapy followed by radical hysterectomy and adjuvant radiotherapy.
Fig. 9.
A 25-year-old young lady presented with irregular menstrual cycles. ( A ) A left para-sagittal image depicting a T2 isointense nodule projecting into the endometrial cavity (*). ( B ) An early dynamic post-contrast para-sagittal image and ( C ) a delayed post-contrast axial image. ( B and C ) Early and persistent nodular enhancement of the lesion detected in A (arrowhead in B and C). Histopathology is suggestive of grade 1 endometrioid adenocarcinoma with mucinous differentiation classified as stage IA1. She opted for uterine-preserving hormonal treatment for fertility planning.
Fig. 10.
A 33-year-old young lady was being evaluated for possible fertility-preserving treatment after biopsy of an endometrial polyp revealed grade 2 endometroid endometrial carcinoma. Magnetic resonance imaging pelvis ( A ) sagittal and ( B ) coronal T2 high-resolution images of the pelvis showed a large 4 cm sized intermediate signal polypoidal growth from the endometrium protruding into the endocervical canal with less than 50% myometrial invasion. ( C ) T2-weighted axial image showed a tumor signal intensity right common iliac node (arrowhead). No other metastases were found on computed tomography (not shown). Thus, fertility preserving treatment option was deferred. The patient underwent hysterectomy and systematic lymphadenectomy. Surgical histopathology showed International Federation of Gynecology and Obstetrics IIIC1 grade 2 EEC with metastatic right iliac node. She underwent adjuvant radiotherapy following surgery.
Fig. 11.
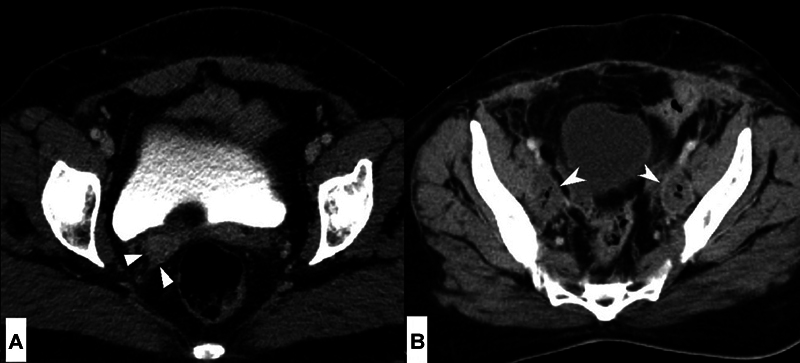
Computed tomography (CT) images through the pelvis of two different patients. ( A ) CT of a patient who underwent hysterectomy and bilateral salpingo oophorectomy for grade 2, International Federation of Gynecology and Obstetrics II endometroid endometrial cancer 9 months ago and received no adjuvant therapy showed a nodular soft tissue thickening in the right vaginal vault (arrowheads) suspicious for local recurrence. ( B ) Postoperative CT of another patient following hysterectomy and pelvic lymphadenectomy elsewhere for endometrial cancer showed bilateral thin-walled collections with air pockets along both the pelvic side walls (arrowheads) and fat stranding suggestive of postoperative lymphatic collections.
Table 7 provides the radiology reporting checklist for patients with endometrial cancer.
Table 7. Radiology reporting checklist for MRI/CT/PET-CT.
|
CLINICAL DETAILS:
Preoperative staging/AUB or postmenopausal bleeding/incidentally detected endometrial carcinoma post-hysterectomy for staging
HPE results—available/unavailable; If available, molecular profiling: Nonaggressive/aggressive/unknown Fertility preservation: yes/no FINDINGS: Uterus: If postop status, comment on the vaginal vault. (Elicit history of how many days postop). Uterus size: _____ x _______ x _______ cm Uterus position: anteverted/retroverted Hydrometra: absent/present Tumor epicenter: uterus/cervix; if uterus endometrium/myometrium Tumor size: _____ x _______ x _______ cm Extent of uterine involvement: Myometrial invasion: absent/present; if present < 50% or >50% Uterine serosa: not involved/involved. Cervical stromal invasion: absent/present Adnexa: Mass in the ovaries/fallopian tubes: absent/present If yes: contiguous/noncontiguous with the uterine mass Describe mass: appearance, extent Parametrium: not involved/involved, if involved contiguous/non-contiguous with the uterine mass Vagina: not involved/involved, if involved contiguous/non-contiguous with the uterine mass Bladder, distal ureters, rectum: not involved/involved, if involved contiguous/noncontiguous with the uterine mass Kidneys: hydronephrosis absent/present Peritoneum: a) Pelvic peritoneum: not involved/involved b) Extra-pelvic peritoneum: not involved/involved, if involved extent Ascites: absent/present; if present mild/moderate/large volume Lymph nodes: SAD mm a) internal iliac/external iliac/obturator b) Common iliac c) Para-aortic: infrarenal/suprarenal d) Omental/mesenteric e) Diaphragmatic f) Mediastinal/hilar g) Supraclavicular Other findings: Other organ metastases: Lungs/liver/bones/brain Co-existent malignancies check list: Stomach/bowel/breast/ovary and tubes IMPRESSION: If histology if available, provide FIGO stage If histology is not available, provide the following information in the impression: T-findings: Depth of myometrial invasion (< 50% or >50%); cervical stromal invasion; uterine serosal/adnexal infiltration/pelvic peritoneal infiltration/bladder or rectal infiltration. N-findings: M-findings: |
Abbreviations: CT, computed tomography; FIGO, International Federation of Gynecology and Obstetrics; MRI, magnetic resonance imaging; PET-CT, positron emission tomography-computed tomography.
Conclusion
As a radiologist delivering imaging care to endometrial cancer patients, it is important to develop an understanding of the management of endometrial cancer. Considering the complexity of the updated FIGO staging system for endometrial cancer, it is vital to ensure optimal inter-disciplinary communications and interpreting imaging studies of these patients along with surgical and treatment history, histopathology, and molecular profile whenever available for accurate staging and risk stratification. MRI pelvis with contrast is the imaging modality of choice for determining the local extent of disease and for identifying contraindications to fertility sparing treatment options. Contrast-enhanced CT of the thorax, abdomen and pelvis is the modality of choice for determining extra-pelvic extent of disease in patients with locally advanced uterine cancer. PET-CT may be considered in selected patients with negative CT but a strong clinical suspicion of recurrence.
Acknowledgements
We would like to thank Sherin Daniel, Department of Pathology, Christian Medical College, Vellore, for her inputs in pathology aspects of the manuscript.
Funding Statement
Funding None declared.
Conflict of Interest None declared.
Author Contributions
All authors contributed to the concept/design, a draft of the manuscript, and its editing. All authors read and approved the final manuscript. A.C. is the guarantor for the contents of the manuscript.
References
- 1.Endometrial Cancer Staging Subcommittee, FIGO Women's Cancer Committee . Berek J S, Matias-Guiu X, Creutzberg C et al. FIGO staging of endometrial cancer: 2023. Int J Gynaecol Obstet. 2023;162(02):383–394. doi: 10.1002/ijgo.14923. [DOI] [PubMed] [Google Scholar]
- 2.Höhn A K, Brambs C E, Hiller G GR, May D, Schmoeckel E, Horn L C. 2020 WHO classification of female genital tumors. Geburtshilfe Frauenheilkd. 2021;81(10):1145–1153. doi: 10.1055/a-1545-4279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.ICMR-NCDIR-NCRP Investigator Group . Mathur P, Sathishkumar K, Chaturvedi M et al. Cancer Statistics, 2020: report from National Cancer Registry Programme, India. JCO Glob Oncol. 2020;6:1063–1075. doi: 10.1200/GO.20.00122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barnes E A, Martell K, Parra-Herran C, Taggar A S, Donovan E, Leung E. Substantial lymphovascular space invasion predicts worse outcomes in early-stage endometrioid endometrial cancer. Brachytherapy. 2021;20(03):527–535. doi: 10.1016/j.brachy.2020.12.006. [DOI] [PubMed] [Google Scholar]
- 5.O'Sullivan B, Brierley J, Byrd D et al. The TNM classification of malignant tumours-towards common understanding and reasonable expectations. Lancet Oncol. 2017;18(07):849–851. doi: 10.1016/S1470-2045(17)30438-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Concin N, Creutzberg C L, Vergote I et al. ESGO/ESTRO/ESP Guidelines for the management of patients with endometrial carcinoma. Virchows Arch. 2021;478(02):153–190. doi: 10.1007/s00428-020-03007-z. [DOI] [PubMed] [Google Scholar]
- 7.Stålberg K, Bjurberg M, Borgfeldt C et al. Lymphovascular space invasion as a predictive factor for lymph node metastases and survival in endometrioid endometrial cancer - a Swedish Gynecologic Cancer Group (SweGCG) study. Acta Oncol. 2019;58(11):1628–1633. doi: 10.1080/0284186X.2019.1643036. [DOI] [PubMed] [Google Scholar]
- 8.Mueller J J, Pedra Nobre S, Braxton K et al. Incidence of pelvic lymph node metastasis using modern FIGO staging and sentinel lymph node mapping with ultrastaging in surgically staged patients with endometrioid and serous endometrial carcinoma. Gynecol Oncol. 2020;157(03):619–623. doi: 10.1016/j.ygyno.2020.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cancer Genome Atlas Research Network . Kandoth C, Schultz N, Cherniack A D et al. Integrated genomic characterization of endometrial carcinoma. Nature. 2013;497(7447):67–73. doi: 10.1038/nature12113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mir M M, Dar N A, Gochhait S, Zargar S A, Ahangar A G, Bamezai R N. p53 mutation profile of squamous cell carcinomas of the esophagus in Kashmir (India): a high-incidence area. Int J Cancer. 2005;116(01):62–68. doi: 10.1002/ijc.21002. [DOI] [PubMed] [Google Scholar]
- 11.Khan M A, Tiwari D, Dongre A et al. Exploring the p53 connection of cervical cancer pathogenesis involving north-east Indian patients. PLoS One. 2020;15(09):e0238500. doi: 10.1371/journal.pone.0238500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Maheshwari E, Nougaret S, Stein E B et al. Update on MRI in evaluation and treatment of endometrial cancer. Radiographics. 2022;42(07):2112–2130. doi: 10.1148/rg.220070. [DOI] [PubMed] [Google Scholar]
- 13.Abu-Rustum N, Yashar C, Arend R et al. Uterine neoplasms, version 1.2023, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2023;21(02):181–209. doi: 10.6004/jnccn.2023.0006. [DOI] [PubMed] [Google Scholar]
- 14.ESMO Guidelines Committee . Oaknin A, Bosse T J, Creutzberg C L et al. Endometrial cancer: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up. Ann Oncol. 2022;33(09):860–877. doi: 10.1016/j.annonc.2022.05.009. [DOI] [PubMed] [Google Scholar]
- 15.Otero-García M M, Mesa-Álvarez A, Nikolic O et al. Role of MRI in staging and follow-up of endometrial and cervical cancer: pitfalls and mimickers. Insights Imaging. 2019;10(01):19. doi: 10.1186/s13244-019-0696-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lakhani A, Khan S R, Bharwani N et al. FDG PET/CT pitfalls in gynecologic and genitourinary oncologic imaging. Radiographics. 2017;37(02):577–594. doi: 10.1148/rg.2017160059. [DOI] [PubMed] [Google Scholar]
- 17.Nougaret S, Horta M, Sala E et al. Endometrial cancer MRI staging: updated guidelines of the European Society of Urogenital Radiology. Eur Radiol. 2019;29(02):792–805. doi: 10.1007/s00330-018-5515-y. [DOI] [PubMed] [Google Scholar]
- 18.Haldorsen I S, Salvesen H B. What is the best preoperative imaging for endometrial cancer? Curr Oncol Rep. 2016;18(04):25. doi: 10.1007/s11912-016-0506-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Manchanda S, Subashree A B, Renganathan R et al. Imaging recommendations for diagnosis, staging, and management of uterine cancer. Indian J Med Paediatr Oncol. 2023;44(01):110–118. [Google Scholar]
- 20.Meissnitzer M, Forstner R. MRI of endometrium cancer - how we do it. Cancer Imaging. 2016;16:11. doi: 10.1186/s40644-016-0069-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nougaret S, Lakhman Y, Vargas H A et al. From staging to prognostication: achievements and challenges of MR imaging in the assessment of endometrial cancer. Magn Reson Imaging Clin N Am. 2017;25(03):611–633. doi: 10.1016/j.mric.2017.03.010. [DOI] [PubMed] [Google Scholar]
- 22.Sbarra M, Lupinelli M, Brook O R, Venkatesan A M, Nougaret S. Imaging of endometrial cancer. Radiol Clin North Am. 2023;61(04):609–625. doi: 10.1016/j.rcl.2023.02.007. [DOI] [PubMed] [Google Scholar]
- 23.Manfredi R, Mirk P, Maresca G et al. Local-regional staging of endometrial carcinoma: role of MR imaging in surgical planning. Radiology. 2004;231(02):372–378. doi: 10.1148/radiol.2312021184. [DOI] [PubMed] [Google Scholar]
- 24.Guo Y, Wang P, Wang P et al. Myometrial invasion and overall staging of endometrial carcinoma: assessment using fusion of T2-weighted magnetic resonance imaging and diffusion-weighted magnetic resonance imaging. OncoTargets Ther. 2017;10:5937–5943. doi: 10.2147/OTT.S145763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Takeuchi M, Matsuzaki K, Harada M. Evaluating myometrial invasion in endometrial cancer: comparison of reduced field-of-view diffusion-weighted imaging and dynamic contrast-enhanced MR imaging. Magn Reson Med Sci. 2018;17(01):28–34. doi: 10.2463/mrms.mp.2016-0128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fujii S, Kido A, Baba T et al. Subendometrial enhancement and peritumoral enhancement for assessing endometrial cancer on dynamic contrast enhanced MR imaging. Eur J Radiol. 2015;84(04):581–589. doi: 10.1016/j.ejrad.2015.01.004. [DOI] [PubMed] [Google Scholar]
- 27.Yamashita Y, Harada M, Sawada T, Takahashi M, Miyazaki K, Okamura H. Normal uterus and FIGO stage I endometrial carcinoma: dynamic gadolinium-enhanced MR imaging. Radiology. 1993;186(02):495–501. doi: 10.1148/radiology.186.2.8421757. [DOI] [PubMed] [Google Scholar]
- 28.Long B, Clarke M A, Morillo A DM, Wentzensen N, Bakkum-Gamez J N. Ultrasound detection of endometrial cancer in women with postmenopausal bleeding: systematic review and meta-analysis. Gynecol Oncol. 2020;157(03):624–633. doi: 10.1016/j.ygyno.2020.01.032. [DOI] [PubMed] [Google Scholar]
- 29.Jones E R, O'Flynn H, Njoku K, Crosbie E J. Detecting endometrial cancer. Obstet Gynaecol. 2021;23(02):103–112. [Google Scholar]
- 30.Yitta S, Hecht E M, Mausner E V, Bennett G L. Normal or abnormal? Demystifying uterine and cervical contrast enhancement at multidetector CT. Radiographics. 2011;31(03):647–661. doi: 10.1148/rg.313105057. [DOI] [PubMed] [Google Scholar]
- 31.McEvoy S H, Nougaret S, Abu-Rustum N R et al. Fertility-sparing for young patients with gynecologic cancer: How MRI can guide patient selection prior to conservative management. Abdom Radiol (NY) 2017;42(10):2488–2512. doi: 10.1007/s00261-017-1179-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ghezzi F, Uccella S, Cromi A et al. Lymphoceles, lymphorrhea, and lymphedema after laparoscopic and open endometrial cancer staging. Ann Surg Oncol. 2012;19(01):259–267. doi: 10.1245/s10434-011-1854-5. [DOI] [PubMed] [Google Scholar]
- 33.Dejanovic D, Hansen N L, Loft A. PET/CT variants and pitfalls in gynecological cancers. Semin Nucl Med. 2021;51(06):593–610. doi: 10.1053/j.semnuclmed.2021.06.006. [DOI] [PubMed] [Google Scholar]
- 34.Ulaner G A, Lyall A. Identifying and distinguishing treatment effects and complications from malignancy at FDG PET/CT. Radiographics. 2013;33(06):1817–1834. doi: 10.1148/rg.336125105. [DOI] [PubMed] [Google Scholar]
- 35.Sharma P, Kumar R, Singh H et al. Carcinoma endometrium: role of 18-FDG PET/CT for detection of suspected recurrence. Clin Nucl Med. 2012;37(07):649–655. doi: 10.1097/RLU.0b013e31824d24fa. [DOI] [PubMed] [Google Scholar]
- 36.Gholkar N S, Saha S C, Prasad G, Bhattacharya A, Srinivasan R, Suri V. The accuracy of integrated [(18)F] fluorodeoxyglucose-positron emission tomography/computed tomography in detection of pelvic and para-aortic nodal metastasis in patients with high risk endometrial cancer. World J Nucl Med. 2014;13(03):170–177. doi: 10.4103/1450-1147.144817. [DOI] [PMC free article] [PubMed] [Google Scholar]


