Congenital abdominal wall hernias are common when they occur via anterior abdominal wall. However, these are extremely rare in the regions outside of it, including the lateral wall and the lumbar region. 1 These are different from classically described lumbar hernias, which include spigelian, Grynfeltt's (via superior lumbar triangle), and Petit's hernia (via inferior lumbar triangle).
We presented the case of a 1-day-old neonate brought to the pediatric outpatient department (OPD) by parents for on-and-off swelling in the right hypochondrium seen when the neonate cried ( Fig. 1 , Video 1 ). Ultrasound of the abdomen showed herniation of the right lobe of the liver via a defect in the right lateral abdominal wall. The defect was seen between the midaxillary line and anterior axillary line and located below the subcoastal margin, inferiorly limited by abdominal wall muscles ( Fig. 2 , Video S2 ). It was completely reducible and was diagnosed as an L4 (lumbar) lateral abdominal wall hernia (LAWH) according to the classification of the European Hernia Society ( Fig. 3A ). 2 No additional anomalies were detected. The skin site was marked at the site of hernia preoperatively and the patient underwent surgery. Intraoperatively, skin incision revealed a peritoneum lined hernial sac protruding via a 3 × 3 cm defect in the region between the mid and anterior axillary lines in the subcoastal location with the liver as the content of hernia and was easily reducible. All the muscle layers were defective at the site. Underlying colon and bowel loops were normal. The defect was closed using 3–0 absorbable sutures and redundant skin was removed. The patient's guardians were advised regarding surgical repair of defect preferably before the age of 1 year. The patient was discharged symptom free at day 4 postsurgery and was advised to follow up in the OPD.
Fig. 1.

Clinical still image demonstrating swelling in the lateral abdominal wall.
Fig. 2.
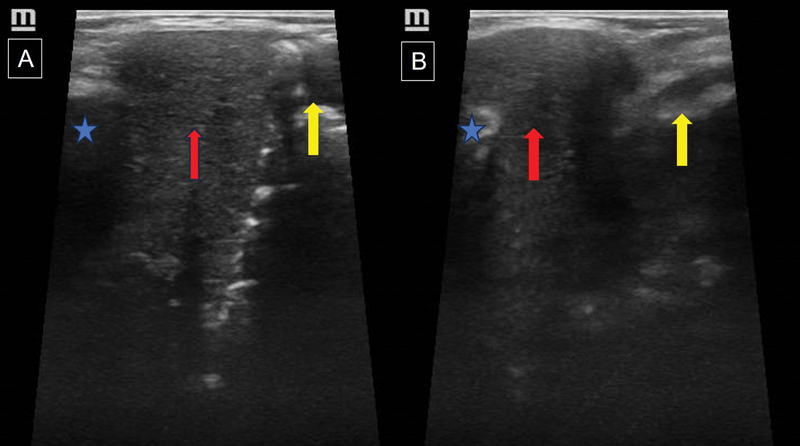
Ultrasound images in the sagittal plane with a linear probe show coastal margin ( blue star and arrow in A and B ) and the edge of the lateral abdominal wall muscles ( yellow arrow in A and B ) with herniation of the liver ( red arrow in A and B ). Note the increase in herniation of the liver in image ( B ) as the patient cries.
Fig. 3.
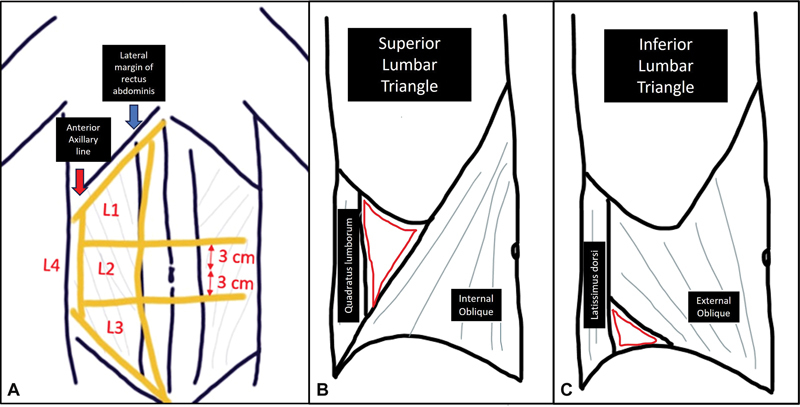
Illustration demonstrating the classification of ( A ) the European Hernia Society of lateral abdominal wall hernia (L1: subcoastal; L2: flank; L3: iliac; and L4: lumbar). Our case had a defect between the mid and anterior axillary lines making it an L4 hernia. ( B ) Anatomical landmarks of the superior lumbar triangle. ( C ) Anatomical landmarks of the superior lumbar triangle.
Video 1 Clinical video demonstrating swelling and its change in size when the patient cries.
Video 2 Video demonstrating herniation of the liver via a defect in the lateral abdominal wall in the subcoastal location.
The lumbar region is divided into superior and inferior triangles. The superior triangle is bounded by an inferior aspect of the last rib, the internal oblique anteriorly, and the quadratus lumborum posteriorly, while the inferior triangle is bounded by the origin of the external oblique anteriorly, latissimus dorsi posteriorly, and the iliac crest inferiorly ( Fig. 3B, C ). In our case, herniation was not seen from either of these locations and hence we classified it as a congenital lateral abdominal wall hernia.
Experience with congenital LAWH is limited, with only 60 cases reported in the literature. 3 4 The probable cause for development of LAWH includes insult during embryonic development causing defect in the germinal disk, defects in the amnion, defects in the ectodermal placode, and/or vascular defects. Nonvisualization of all the abdominal wall layers with maintained skin places the time of insult probably during embryogenesis, after the abdominal wall was formed with normal ectodermal development, related to a regional vascular problem.
The exact cause of hernia is not known. In our case, no other congenital anomaly or bony abnormality was seen. However, in the literature, these defects are reported with other associated skeletal malformations such as lumbo-costovertebral syndrome 5 6 and vertebral defects, anal atresia, cardiac defects, tracheoesophageal fistula, renal anomalies, and limb abnormalities (VACTERL) syndrome. Previous case reports mention associated dextrocardia and anorectal malformation in random and not as a part of VACTERL as at least three features should be present.
Cross-sectional imaging like computed tomography (CT) and magnetic resonance imaging (MRI) has a significant role in confirming the associated malformations with bony defects seen better on CT and organ anomalies on MRI. They are not required in all cases but in the cases where initial X-ray or ultrasound is suggestive of associated anomalies. A preoperative CT/MRI provides a preoperative roadmap for treatment of hernial defects and associated anomalies. There are no guidelines regarding the imaging protocol and case-based protocols should be followed. In our case, since X-rays and ultrasound revealed no other anomalies, CT and MRI were not done. Screening echocardiography revealed no cardiac defects.
Primary repair of the abdominal walls can be done in small defects as done in our case; however, large defects require prosthetic mesh repair. In few cases, laparoscopic repair with free fascia late graft reinforcement is reported as well. 4 There is no consensus regarding treatment of these defects due to their rarity; however, treatment of defect before the age of 1 year is recommended. 3
Teaching point: Understanding the pathophysiology, clinical, and imaging findings of congenital LAWH and their management. Change in size of swelling is a major cause of concern for parents, and proper diagnosis and surgical management is advised. Workup for other congenital anomalies including VACTERL syndrome and cardiac anomalies are advised in all patients.
Funding Statement
Funding None.
Conflict of Interest None declared.
Ethical Approval
Written informed consent for participation and publication was obtained from the patient's guardian (parent).
Availability of Data and Material
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
References
- 1.Wakhlu A, Wakhlu A K.Congenital lumbar hernia Pediatr Surg Int 200016(1-2):146–148. [DOI] [PubMed] [Google Scholar]
- 2.Muysoms F E, Miserez M, Berrevoet F et al. Classification of primary and incisional abdominal wall hernias. Hernia. 2009;13(04):407–414. doi: 10.1007/s10029-009-0518-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Montes-Tapia F, Cura-Esquivel I, Gutiérrez S, Rodríguez-Balderrama I, de la O-Cavazos M. Congenital lateral abdominal wall hernia. Pediatr Int. 2016;58(08):788–790. doi: 10.1111/ped.12976. [DOI] [PubMed] [Google Scholar]
- 4.Mansy M, Kotb M, Abouheba M. Congenital lumbar hernia in an 8-month-old boy. Case Rep Gastroenterol. 2021;15(01):431–435. doi: 10.1159/000511006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Harris K, Dorn C, Bloom B. Lumbocostovertebral syndrome with associated VACTERL anomalad: a neonatal case report. J Perinatol. 2009;29(12):826–827. doi: 10.1038/jp.2009.82. [DOI] [PubMed] [Google Scholar]
- 6.Fakhry S M, Azizkhan R G. Observations and current operative management of congenital lumbar hernias during infancy. Surg Gynecol Obstet. 1991;172(06):475–479. [PubMed] [Google Scholar]


