Abstract
Background and Aims
Declines in cardiovascular mortality have stagnated in the USA since 2011. There is growing concern that these patterns reflect worsening cardiovascular health in younger adults. However, little is known about how the burden of acute cardiovascular hospitalizations and mortality has changed in this population. Changes in cardiovascular hospitalizations and mortality among adults aged 25–64 years were evaluated, overall and by community-level income.
Methods
Using the National Inpatient Sample, age-standardized annual hospitalization and in-hospital mortality rates for acute myocardial infarction (AMI), heart failure, and ischaemic stroke were determined among adults aged 25–64 years. Quasi-Poisson and quasi-binominal regression models were fitted to compare outcomes between individuals residing in low- and higher-income communities.
Results
Between 2008 and 2019, age-standardized hospitalization rates for AMI increased among younger adults from 155.0 (95% confidence interval: 154.6, 155.4) per 100 000 to 160.7 (160.3, 161.1) per 100 000 (absolute change +5.7 [5.0, 6.3], P < .001). Heart failure hospitalizations also increased (165.3 [164.8, 165.7] to 225.3 [224.8, 225.8], absolute change +60.0 (59.3, 60.6), P < .001), as ischaemic stroke hospitalizations (76.3 [76.1, 76.7] to 108.1 [107.8, 108.5], absolute change +31.7 (31.2, 32.2), P < .001). Across all conditions, hospitalizations rates were significantly higher among younger adults residing in low-income compared with higher-income communities, and disparities did not narrow between groups. In-hospital mortality decreased for all conditions over the study period.
Conclusions
There was an alarming increase in cardiovascular hospitalizations among younger adults in the USA from 2008 to 2019, and disparities between those residing in low- and higher-income communities did not narrow.
Keywords: Cardiovascular disease, Acute myocardial infarction, Stroke, Heart failure, Mortality, Disparities
Structured Graphical Abstract
Structured Graphical Abstract.
Cardiovascular hospitalizations and mortality among adults aged 25–64 years in the USA. A structured visual abstract that summarizes the main findings of this study is shown.
See the editorial comment for this article ‘Increasing cardiovascular hospitalization rates among young and middle-aged adults in the USA suggest a need for multi-faceted solutions', by S.T. Harris and K.E. Joynt Maddox, https://doi.org/10.1093/eurheartj/ehae027.
Introduction
Although cardiovascular mortality had been declining for decades, this progress has stagnated and even started to reverse since 2011.1–3 There is growing concern that these changes may reflect worsening cardiovascular health in younger working-age adults. Recent evidence suggests a rise in hypertension, diabetes, and obesity among young adults over the past decade, increasing this population’s risk of developing cardiovascular disease and acute cardiovascular events (e.g. myocardial infarction and stroke).4 While cardiovascular disease and outcomes among older adults—especially the Medicare population—have been well studied, less is known about how the burden of acute cardiovascular hospitalizations and deaths has changed among younger adults on a national scale.5–8
Income inequality has risen sharply in the USA, and nearly 38 million Americans are currently living in poverty.9,10 Low-income adults may be at a particularly high risk for worse cardiovascular outcomes compared to their higher-income counterparts. Previous studies have demonstrated that adults living in low-income communities are more likely to be uninsured, experience poor access to care, and often do not receive appropriate management of cardiovascular risk factors.11,12 In addition, this population is more likely to experience food insecurity, housing instability, worse built environment (e.g. lack of green space), and environmental stressors, all of which are strongly linked to cardiovascular health.13–16 As a result, low-income communities have a higher burden of cardiovascular disease.17,18 Despite the known association between income and cardiovascular health, hospitalization rates for acute myocardial infarction (AMI), heart failure, and stroke have not been well characterized on a national scale in younger adults residing in low- and higher-income communities, and little is known about how disparities between these groups have changed in the face of rising income inequality. Understanding these patterns is critically important, and could inform targeted public health and policy strategies to reduce inequities in cardiovascular health nationwide.
Therefore, in this study, we aimed to answer three questions. First, how did hospitalization rates for AMI, heart failure, and ischaemic stroke change among younger adults (aged 25–64 years) between 2008 and 2019, both overall and by community-level income? Second, how did in-hospital mortality rates for these cardiovascular conditions change? Third, did disparities in hospitalizations and in-hospital mortality between younger adults residing in low- vs. higher-income communities narrow or widen over this time period?
Methods
Data sources
We used the Healthcare Cost Utilization Project (HCUP) National Inpatient Sample (NIS) to examine acute cardiovascular hospitalizations and associated in-hospital mortality from 2008 to 2019.19 The HCUP NIS is an all-payer database that includes a 20% sample of discharges from US hospitals, and can be used to generate nationally representative estimates. This dataset captures information on demographics, including age, sex, race/ethnicity [non-Hispanic (NH) White, NH Black, Hispanic, NH Asian, NH Other], primary payer (Medicare, Medicaid, private, self-pay, other), as well as clinical comorbidities (based on the Elixhauser comorbidity index), and hospital geographic region (Northeast, Midwest, South, West). We intentionally elected to exclude 2020 HCUP data because of the onset of the COVID-19 pandemic, which led to major disruptions in access to care and substantial changes in overall hospitalization rates.
Study population
We identified all hospitalizations for adults aged 25 to 64 years with a primary diagnosis of AMI, heart failure, or ischaemic stroke based on ICD-9 and ICD-10 codes used in national quality and reporting programmes (seeSupplementary data online, Table S1).20,21 The population denominator of adults aged 25 to 64 years was obtained from the US Census Bureau American Community Survey for each respective year.22 We then stratified hospitalizations based on community-level income using ZIP codes. Hospitalizations among those residing in ZIP codes in the bottom quartile of median household income nationally were classified as ‘low-income’, and all others were classified as ‘higher-income.’
Study outcomes
Our primary outcomes were as follows: (i) hospitalization rates for each cardiovascular condition (AMI, heart failure, ischaemic stroke) per 100 000 among adults aged 25–64 years and (ii) in-hospital mortality for each condition.
Statistical analysis
Baseline characteristics of hospitalizations for adults aged 25–64 years, both overall and by community-level income status, were compared at the beginning (2008–09) and end (2018–19) of the study period using t-tests and χ2 tests as appropriate. We then calculated the age-standardized annual hospitalization rate per 100 000 adults (aged 25–64 years) for each condition (e.g. AMI, heart failure, and ischaemic stroke). The direct standardization method was performed using the 2010 US adult population as a reference.4 A delta change analysis was performed to assess the absolute change in age-standardized hospitalization rates from 2008–09 to 2018–19. We then fit quasi-Poisson regression models to determine the age-adjusted relative risk of hospitalization [and 95% confidence interval (CI)] for adults residing in low- vs. higher-income communities, and included an interaction term for income level (low vs. higher) and calendar years (2008–09 vs. 2018–19) to assess whether gaps in hospitalization rates between income groups changed over the study period. To assess risk-adjusted in-hospital mortality among hospitalized adults living in low-income vs. higher-income communities for each condition, a quasi-binomial regression model was fit after adjustment for age, sex, and clinical comorbidities using the Elixhauser comorbidity index. An interaction term between income and calendar years was included to assess for differential changes between low- and higher-income community groups. Nationally representative estimates of hospitalizations were calculated by applying weights provided by HCUP/Agency for Healthcare Research and Quality.23 Because the survey design of NIS changed in 2012, we applied ‘trend weights’ created specifically to assess longitudinal trends before and after 2012, as established by HCUP and consistent with prior studies.24–27 We adhered to the methodological standards and best practices for working with NIS data developed by the Agency for Healthcare Research and Quality’s (AHRQ) (see Supplementary data).28,29
A P-value threshold of <.05 was used to determine statistical significance. All statistical analyses were two-sided and were conducted using SAS Enterprise Guide version 7.1 (SAS Institute, Cary, NC, USA), and R version 4.2.1. Institutional review board approval was not required from Beth Israel Deaconess Medical Center because the study used publicly available de-identified data, as per institutional policy.
Results
Baseline characteristics
The weighted number of cardiovascular hospitalizations for adults 25–64 years over the entire study period was 8 476 762, with 1 291 151 occurring in 2008–09 and 1 628 810 in 2018–19. The sociodemographics (age, sex, race/ethnicity), geographic region, primary payer, and clinical comorbidities of hospitalizations for younger adults are shown both overall, and by community-level income, in Table 1. Over the study period, hospitalized adults from low-income communities were more likely to be female, insured by Medicaid, reside in the Midwest, or Southern United States compared with their counter parts residing in higher-income communities. In addition, hospitalized adults from low-income communities were significantly more likely to be Black compared to those in higher-income communities. Clinical comorbidities are shown in Table 1 and Supplementary data online, Table S2.
Table 1.
Baseline characteristics of hospitalizations for adults age 25–64 years, 2008–09 vs. 2018–19a
| 2008–09 | 2018–19 | |||||||
|---|---|---|---|---|---|---|---|---|
| Overall | Low incomeb | Higher income | P-value | Overall | Low income | Higher income | P-value | |
| n of hospitalization (weighted) | 1 291 251 | 452 491 | 838 760 | 1 628 810 | 625 500 | 1 003 310 | ||
| Mean age, years (SD) | 53.6 (0.04) | 53.3 (0.05) | 53.8 (0.04) | <.001 | 54.2 (0.02) | 53.9 (0.03) | 54.4 (0.02) | <.001 |
| Sex (%) | <.0001 | <.001 | ||||||
| Male | 63.8 | 60.6 | 65.5 | 63.8 | 61.1 | 65.5 | ||
| Female | 36.2 | 39.4 | 34.5 | 36.2 | 38.9 | 34.5 | ||
| Race/ethnicity (%) | <.001 | <.001 | ||||||
| NH White | 59.6 | 46.4 | 66.7 | 55.2 | 43.7 | 62.3 | ||
| NH Black | 25.2 | 38.5 | 18.1 | 27.6 | 40.3 | 19.7 | ||
| Hispanic | 8.8 | 10.5 | 8.0 | 11.0 | 11.6 | 10.6 | ||
| NH Asian or Pacific Islander | 2.2 | 0.9 | 2.8 | 2.6 | 1.0 | 3.6 | ||
| NH Other | 4.1 | 3.7 | 4.3 | 3.7 | 3.4 | 3.8 | ||
| Region (%) | <.001 | <.001 | ||||||
| Northeast | 16.2 | 13.0 | 17.8 | 15.3 | 10.6 | 18.2 | ||
| Midwest | 11.3 | 15.1 | 9.2 | 31.6 | 39.6 | 26.7 | ||
| South | 56.6 | 61.9 | 53.8 | 35.2 | 38.1 | 33.3 | ||
| West | 16.0 | 10.0 | 19.2 | 17.9 | 11.7 | 21.8 | ||
| Primary payer (%) | <.001 | <.001 | ||||||
| Medicare | 22.2 | 27.0 | 19.6 | 24.6 | 28.9 | 21.9 | ||
| Medicaid | 17.6 | 24.2 | 14.0 | 26.2 | 31.4 | 23.0 | ||
| Private | 42.7 | 29.6 | 49.7 | 35.6 | 24.9 | 42.3 | ||
| Self-pay | 11.9 | 13.7 | 10.9 | 9.6 | 11.0 | 8.7 | ||
| Other | 5.7 | 5.4 | 5.8 | 4.0 | 3.7 | 4.2 | ||
| Clinical comorbiditiesc (%) | ||||||||
| Congestive heart failure | 2.1 | 2.5 | 1.9 | <.001 | 3.7 | 4.0 | 3.5 | <.001 |
| Chronic pulmonary disease | 23.0 | 26.9 | 20.9 | <.001 | 26.8 | 30.9 | 24.2 | <.001 |
| Chronic kidney disease/renal failure | 19.7 | 22.7 | 18.1 | <.001 | 27.8 | 31.6 | 25.4 | <.001 |
| Diabetes mellitus | 39.6 | 42.3 | 38.1 | <.001 | 45.7 | 48.5 | 43.9 | <.001 |
| Metastatic cancer | 0.7 | 0.6 | 0.8 | <.001 | 0.8 | 0.7 | 0.9 | <.001 |
| Obesity | 19.4 | 19.9 | 19.2 | .05 | 32.0 | 32.4 | 31.7 | .003 |
| Peripheral vascular disease | 7.5 | 7.3 | 7.6 | .13 | 6.2 | 6.0 | 6.3 | .002 |
| Pulmonary circulation disease | 0.5 | 0.5 | 0.5 | .68 | 0.2 | 0.2 | 0.2 | .01 |
| Solid tumour w/out metastasis | 0.8 | 0.8 | 0.8 | .99 | 0.9 | 0.9 | 1.0 | .03 |
| Valvular disease | 1.4 | 1.2 | 1.4 | .004 | 1.4 | 1.3 | 1.5 | <.001 |
| Weight loss | 1.8 | 2.1 | 1.7 | <.001 | 3.2 | 3.4 | 3.0 | <.001 |
aWeighted percentages are shown unless otherwise specified.
b‘Low-income’ represents hospitalizations among individuals residing in ZIP codes in the bottom quartile of median household income nationally. ‘Higher-income’ represents all other hospitalizations.
cSelect comorbidities are shown. A complete list is provided in Supplementary data online, Table S2.
Hospitalization rates for acute cardiovascular conditions
Overall age-standardized hospitalization rates for AMI increased modestly among younger adults from 155.0 (95% CI: 154.6, 155.4) per 100 000 in 2008–09 to 160.7 (95% CI: 160.3, 161.1) per 100 000 in 2018–19 (absolute change from 2008–09 to 2018–19 of +5.7 (95% CI: 5.0, 6.3) hospitalizations per 100 000, P-value of <.001) (Figure 1 and Table 2). While AMI hospitalization rates were consistently higher among adults residing in low-income communities (compared to those in higher-income communities), this population experienced a decline in AMI hospitalizations from 270.5 (95% CI: 269.2, 271.9) to 245.4 (95% CI: 244.2, 246.6) per 100 000 over the study period (absolute change −25.1 (95% CI: −26.9, −23.3) per 100 000, P < .001), while adults in higher-income communities experienced a significant rise 131.5 [95% CI: 131.1, 132.0] to 137.5 [95% CI: 137.1, 138.0] per 100 000, (absolute change +6.0 (95% CI: 5.4, 6.6) per 100 000, P < .001) (Figure 2A and Table 2). The gap in age-standardized AMI hospitalization rates was markedly higher among younger adults in low-income communities than those in higher-income communities, and this gap persisted from 2008–09 (relative risk [RR] 2.01 [95% CI: 1.45, 2.79]) to 2018–19 (RR 1.77 [95% CI: 1.30, 2.39]) (P-value for interaction between income group and year = .63) (see Supplementary data online, Table S3).
Figure 1.
Age-standardized cardiovascular hospitalization rates among adults aged 25–64 years, 2008–19. The figure shows age-standardized hospitalization rates for acute myocardial infarction, heart failure, and ischaemic stroke among young adults aged 25–64 years in the USA. Age-standardized hospitalizations increased significantly for all three conditions from 2008 to 2019
Table 2.
Hospitalizations (per 100 000) among adults age 25–64 years in low-income vs. higher-income communities, 2008–19
| 2008–09 | 2018–19 | Absolute change (2008–09 to 2018–19) | P-value for absolute change | |
|---|---|---|---|---|
| Acute myocardial infarction | ||||
| Low income | 270.5 (269.2, 271.9) |
245.4 (244.2, 246.6) |
−25.1 (−26.9, −23.3) |
<.001 |
| Higher income | 131.5 (131.1, 132.0) |
137.5 (137.1, 138.0) |
6.0 (5.4, 6.6) |
<.001 |
| Overall | 155.0 (154.6, 155.4) |
160.7 (160.3, 161.1) |
5.7 (5.0, 6.3) |
<.001 |
| Heart failure | ||||
| Low income | 399.6 (397.9, 401.3) |
455.7 (454.1, 457.3) |
56.1 (53.8, 58.4) |
<.001 |
| Higher income | 117.6 (117.2, 118.0) |
162.1 (161.6, 162.6) |
44.6 (43.9, 45.2) |
<.001 |
| Overall | 165.3 (164.8, 165.7) |
225.3 (224.8, 225.8) |
60.0 (59.3, 60.6) |
<.001 |
| Ischaemic stroke | ||||
| Low income | 151.2 (150.2, 152.3) |
183.1 (182.1, 184.1) |
31.9 (30.4, 33.3) |
<.001 |
| Higher income | 61.2 (60.9, 61.5) |
87.5 (87.2, 87.9) |
26.4 (25.9, 26.8) |
<.001 |
| Overall | 76.3 (76.1, 76.7) |
108.1 (107.8, 108.5) |
31.7 (31.2, 32.2) |
<.001 |
Figure 2.
(A–C) Age-standardized hospitalization rates among adults aged 25–64 years by community-level income, 2008–19. The figure shows age-standardized hospitalization rates for acute myocardial infarction, heart failure, and ischaemic stroke among young adults, aged 25–64 years, residing in low-income and higher-income communities in the USA from 2008 to 2019. Hospitalizations among those residing in ZIP codes in the bottom quartile of median household income nationally were classified as ‘low-income’, and all others were classified as ‘higher-income’
For heart failure, age-standardized hospitalization rates increased markedly among younger adults from 165.3 (95% CI: 164.8, 165.7) per 100 000 in 2008–09 to 225.3 (95% CI: 224.8, 225.8) per 100 000 in 2018–19 (absolute change +60.0 (95% CI: 59.3, 60.6) per 100 000, P < .001) (Figure 1 and Table 2). Heart failure hospitalization rates were significantly higher among adults in low-income vs. higher-income communities throughout the study period. Younger adults in low-income communities experienced a significant increase in heart failure hospitalizations from 399.6 (95% CI: 397.9, 401.3) to 455.7 (95% CI: 454.1, 457.3) per 100 000 (absolute change +56.1 (95% CI: 53.8, 58.4) per 100 000, P < .001), while adults in higher-income communities also experienced an increase 117.6 [95% CI: 117.2, 118.0] to 162.1 [95% CI: 161.6, 162.6] per 100 000 (absolute change +44.6 (95% CI: 43.9, 45.2) per 100 000, P < .001) (Figure 2B and Table 2). Hospitalization rates for heart failure were markedly higher among adults in low-income vs. higher-income communities, and this gap did not narrow over the study period (2008–09: RR 3.32 [95% CI: 2.58, 4.11]; 2018–19: RR 2.78 [95% CI: 2.33, 3.31], P-value for interaction = .23) (see Supplementary data online, Table S3).
Age-standardized ischaemic stroke hospitalization rates increased among younger adults from 76.3 (95% CI: 76.1, 76.7) per 100 000 in 2008–09 to 108.1 (95% CI: 107.8, 108.5) per 100 000 in 2018–19 (absolute change +31.7 (95% CI: 31.2, 32.2) per 100 000, P < .001) (Figure 1, Table 2). Adults residing in low-income communities experienced an increase from 151.2 (95% CI: 150.2, 152.3) to 183.1 (95% CI: 182.1, 184.1) per 100 000, (absolute change +31.9 (95% CI: 30.4, 33.3) per 100 000, P < .001) over this period, while adults in higher-income communities experienced an increase from 61.2 (95% CI: 60.9, 61.5) to 87.5 (95% CI: 87.2, 87.9) per 100 000 (absolute change +26.4 (95% CI: 25.9, 26.8) per 100 000, P < .001) (Figure 2C and Table 2). The gap in ischaemic stroke hospitalizations between younger adults in low- vs. higher-income communities did not narrow over the study period (P-value for interaction = .32) (see Supplementary data online, Table S3).
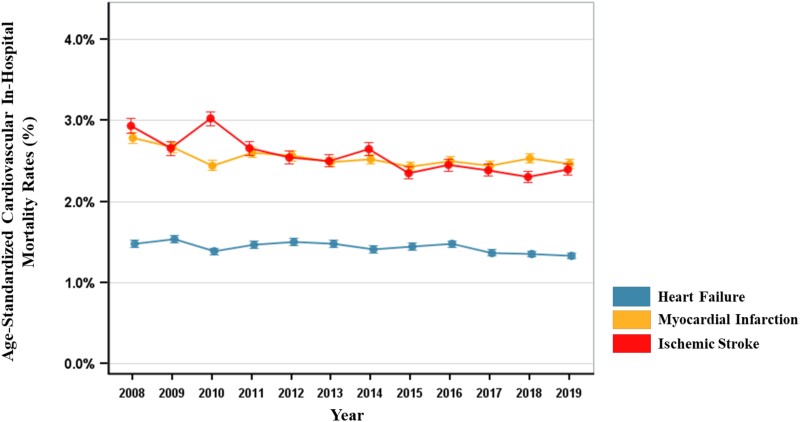
In-hospital mortality for acute cardiovascular conditions
Age-standardized in-hospital mortality rates for all three conditions significantly declined among younger adults. In-hospital mortality for AMI declined from 2.71% (95% CI: 2.67%, 2.75%) in 2008–09 to 2.50% (95% CI: 2.45%, 2.53%) in 2018–19 (P < .001) (Figure 3). For heart failure, in-hospital mortality declined overall (1.52% [95% CI: 1.49%, 1.55%] to 1.35% [95% CI: 1.34%, 1.38%], P < .001), with similar patterns for ischaemic stroke (2.78% [95% CI: 2.72%, 2.85%] to 2.33% [95% CI: 2.28%, 2.38%], P < .001). Changes in mortality for each condition by community-level income are shown in Supplementary data online, Figure S1. After risk-adjustment, there were no significant differences in in-hospital mortality between younger adults living in low- vs. higher-income communities at the end of the study period (see Supplementary data online, Table S4).
Figure 3.
Age-standardized in-hospital mortality for cardiovascular conditions among young adults, 2008–19. The figure shows age-standardized in-hospital mortality rates for young adults aged 25–64 years hospitalized with acute myocardial infarction, heart failure, and ischaemic stroke (red) in the USA
Discussion
In this national analysis, we found that hospitalization rates for AMI, heart failure, and ischaemic stroke all significantly increased among younger adults aged 25–64 years between 2008 and 2019, while associated in-hospital mortality rates for these conditions declined. Concerningly, cardiovascular hospitalizations were two- to three-times higher among younger adults residing in low-income communities compared with those in higher-income communities, and disparities did not narrow between these groups over the study period (Structured Graphical Abstract).
The significant increase in cardiovascular hospitalizations among younger adults in the USA has major public health implications. Our findings correspond with the recent recognition that unhealthy lifestyle habits (e.g. limited physical activity and unhealthy diets) and the prevalence of cardiovascular risk factors—including obesity, hypertension, and diabetes—have increased among younger adults over the same time period.4,30 The rising burden of cardiovascular hospitalizations in this population highlights the urgent need to focus public health and clinical interventions on the primary prevention of cardiovascular risk factors and the management of cardiovascular disease in younger adults. Our results extend upon recent analyses focused on heart failure hospitalizations, by demonstrating similarly concerning trends for both AMI and ischaemic stroke hospitalizations, and evaluating changes in income-based inequities for all three conditions specifically in younger adults.31,32 Notably, the 40% rise in heart failure hospitalizations and 20% rise in stroke hospitalizations observed in our study were particularly prominent, and highlight the critical need for public health campaigns to increase awareness of these conditions (and associated morbidity) in younger individuals.
We also found that cardiovascular hospitalizations were consistently and significantly higher among younger adults living in low-income communities compared to those in higher-income communities. For example, rates of AMI and ischaemic stroke hospitalizations among younger adults residing in low-income communities were ∼2-times higher than those in higher-income communities at the end of the study period, while rates of heart failure hospitalization were nearly three-times higher. Moreover, despite modest improvements in AMI hospitalization rates among younger adults residing in low-income communities from 2008 to 2019, the gap in hospitalization rates between younger adults residing in low- and higher-income communities has not narrowed over the past decade for any of the three conditions. Prior work has demonstrated that compared to wealthier individuals, those with low-incomes have a higher burden of cardiovascular risk factors and disease, as well as higher rates of being uninsured or underinsured, and poor access to reliable, longitudinal outpatient care, all of which likely results in greater acute care utilization and worse outcomes.5,12 While the drivers of these disparities are complex and multifactorial, these findings are particularly concerning given that income inequality continues to grow in the USA.11,12,33
We also found that ∼40% of hospitalized younger adults from low-income communities were NH Black. Black individuals are far more likely to live in low-income areas in the USA due to structurally racist practices, including housing discrimination and residential segregation.34,35 In addition, Black adults disproportionately face economic, social, and environmental barriers, which limit wealth and economic mobility, and ultimately contribute to worse access to health care. As a result, Black Americans are less likely to receive preventive screenings and treatments for cardiovascular risk factors, which along with other important social determinants (e.g. food insecurity, lack of green space, and environmental stressors), contribute to a higher burden of cardiovascular disease in this population.12–15,36
Notably, in-hospital mortality for AMI, heart failure, and ischaemic stroke all declined over the course of our study period. These findings suggest that the acute management of these conditions has been improving, possibly due to advances in technology and/or improvements in hospital quality and systems of care (e.g. quality metrics incentivizing rapid reperfusion for patients with AMI and stroke). Reassuringly, there was no evidence of gaps in in-hospital mortality between hospitalized younger adults from low- vs. higher-income communities.
Public health strategies to address worsening cardiovascular health among younger adults are urgently needed. A combination of community-based and national initiatives that screen for and treat cardiovascular risk factors (e.g. hypertension, hyperlipidaemia, and diabetes) in younger adults could help slow the growing burden of cardiovascular disease in this population. For example, outreach programmes that screen and treat hypertension in barber shops and churches have both been shown to improve blood pressure control in communities that interface with health care inconsistently.37–39 Additionally, improved secondary prevention of individuals with established cardiovascular disease, by ensuring reliable access to specialty providers as well as affordable guideline-directed therapies, could help lower rates of cardiovascular hospitalization and death. Finally, given the concentration of cardiovascular morbidity and mortality among younger adults in low-income communities, these efforts must also address social determinants of health. On a national level, the Centers for Medicare and Medicaid Services has started requiring all hospitals to collect health-related social needs (food insecurity, housing instability, transportation difficulties, utility difficulties, or interpersonal safety) for all hospitalized individuals 18 years and older.40,41 This may be a critical first step to connect patients with important social services that address health-related social needs, and could ultimately lead to targeted interventions that reduce disparities.
This study has limitations. First, both cardiovascular hospitalizations and mortality were identified using ICD codes, which may be subject to misclassification. However, these codes are used in national public reporting and quality programmes,15 and we would not expect the degree of misclassification to change over time or to differ between subgroups. Second, for the analysis focused on cardiovascular hospitalizations, the unit of analysis was hospitalization (rather than unique patient), because NIS does not include unique patient identifiers. However, our primary goal was to understand the epidemiological burden of hospitalizations in the population of younger adults, which does not require patient-level identifiers. Third, there was a change in NIS survey design beginning in 2012, but we used established methods provided by HCUP to account for this change and generate nationally representative estimates.22–25
Conclusion
In the USA, there has been an alarming increase in cardiovascular hospitalization rates among younger adults aged 25–64 years. The burden of cardiovascular hospitalizations was significantly higher among younger adults residing in low-income vs. higher-income communities, and disparities between these groups did not narrow from 2008 to 2019.
Supplementary data
Supplementary data are available at European Heart Journal online.
Declarations
Disclosure of Interest
All authors declare no disclosure of interest for this contribution.
Supplementary Material
Contributor Information
Chantal M Henry, Richard A. and Susan F. Smith Center for Outcomes Research, Beth Israel Deaconess Medical Center and Harvard Medical School, 375 Longwood Ave, 4th Floor, Boston, MA 02215, USA; Meharry Medical College, Nashville, TN, USA.
Andrew S Oseran, Richard A. and Susan F. Smith Center for Outcomes Research, Beth Israel Deaconess Medical Center and Harvard Medical School, 375 Longwood Ave, 4th Floor, Boston, MA 02215, USA; Division of Cardiology, Massachusetts General Hospital, Boston, MA, USA; Division of Cardiology, Beth Israel Deaconess Medical Center and Harvard Medical School, 330 Brookline Avenue, Boston, MA 02215, USA.
ZhaoNian Zheng, Richard A. and Susan F. Smith Center for Outcomes Research, Beth Israel Deaconess Medical Center and Harvard Medical School, 375 Longwood Ave, 4th Floor, Boston, MA 02215, USA.
Huaying Dong, Richard A. and Susan F. Smith Center for Outcomes Research, Beth Israel Deaconess Medical Center and Harvard Medical School, 375 Longwood Ave, 4th Floor, Boston, MA 02215, USA.
Rishi K Wadhera, Richard A. and Susan F. Smith Center for Outcomes Research, Beth Israel Deaconess Medical Center and Harvard Medical School, 375 Longwood Ave, 4th Floor, Boston, MA 02215, USA; Division of Cardiology, Beth Israel Deaconess Medical Center and Harvard Medical School, 330 Brookline Avenue, Boston, MA 02215, USA.
Data Availability
HCUP data are available through a data use agreement with AHRQ. CDC WONDER data are publicly available on the NCHS website.
Funding
This study was funded by the National Heart, Lung and Blood Institute (NHLBI) grants R01HL164561 and K23HL148525 (R.K.W.) from the National Institutes of Health and the Sarnoff Cardiovascular Research Fellowship (C.M.H.).
Ethical Approval
The study was approved by the Beth Israel Deaconess Medical Center Institutional Review Board.
Pre-registered Clinical Trial Number
Not applicable.
References
- 1. Dani SS, Lone AN, Javed Z, Khan MS, Khan MZ, Kaluski E, et al. Trends in premature mortality from acute myocardial infarction in the United States, 1999 to 2019. J Am Heart Assoc 2022;11:e021682. 10.1161/JAHA.121.021682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ma J, Ward EM, Siegel RL, Jemal A. Temporal trends in mortality in the United States, 1969–2013. JAMA 2015;314:1731–9. 10.1001/jama.2015.12319 [DOI] [PubMed] [Google Scholar]
- 3. Khatana SAM, Venkataramani AS, Nathan AS, Dayoub EJ, Eberly LA, Kazi DS, et al. Association between county-level change in economic prosperity and change in cardiovascular mortality among middle-aged US adults. JAMA 2021;325:445–53. 10.1001/jama.2020.26141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Aggarwal R, Yeh RW, Joynt Maddox KE, Wadhera RK. Cardiovascular risk factor prevalence, treatment, and control in US adults aged 20 to 44 years, 2009 to March 2020. JAMA 2023;329:899–909. 10.1001/jama.2023.2307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Gupta A, Fonarow GC. The hospital readmissions reduction program: evidence for harm. JACC Heart Fail 2018;6:607–9. 10.1016/j.jchf.2018.02.012 [DOI] [PubMed] [Google Scholar]
- 6. Khera R, Dharmarajan K, Krumholz HM. Rising mortality in patients with heart failure in the United States: facts versus fiction. JACC Heart Fail 2018;6:610–2. 10.1016/j.jchf.2018.02.011 [DOI] [PubMed] [Google Scholar]
- 7. Wadhera RK, Wang Y, Figueroa JF, Dominici F, Yeh RW, Maddox J. Mortality and hospitalizations for dually enrolled and nondually enrolled medicare beneficiaries aged 65 years and older, 2004 to 2017. JAMA 2020;323:961–9. 10.1001/jama.2020.1021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Loccoh E, Joynt Maddox KE, Xu J, Shen C, Figueroa JF, Kazi DS, et al. Rural-urban disparities in all-cause mortality among low-income medicare beneficiaries, 2004–17. Health Aff 2021;40:289–96. 10.1377/hlthaff.2020.00420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bivens J, Banerjee A. Inequality’s drag on aggregate demand: The macroeconomic and fiscal effects of rising income shares of the rich. The Economic Policy Institute, May 2022.https://www.epi.org/publication/inequalitys-drag-on-aggregatedemand/#:∼:text=The%20way%20that%20income%20inequality,which%20save%20a%2higher%20share(accessed 27 October 2023).
- 10. Creamer J, Shrider EA, Burns K, Chen F. Poverty in the United States 2021. U.S. Census Bureau Current Population Reports, 2022, 60–277.
- 11. Oseran AS, Sun T, Wadhera RK. Health care access and management of cardiovascular risk factors among working-age adults with low income by state medicaid expansion status. JAMA Cardiol 2022;7:708–14. 10.1001/jamacardio.2022.1282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hermes Z, Joynt Maddox KE, Yeh RW, Zhao Y, Shen C, Wadhera RK. Neighborhood socioeconomic disadvantage and mortality among medicare beneficiaries hospitalized for acute myocardial infarction, heart failure, and pneumonia. J Gen Intern Med 2021;37:1894–901. 10.1007/s11606-021-07090-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Havranek EP, Mujahid MS, Barr DA, Blair IV, Cohen MS, Cruz-Flores S, et al. Social determinants of risk and outcomes for cardiovascular disease. Circulation 2015;132:873–98. 10.1161/CIR.0000000000000228 [DOI] [PubMed] [Google Scholar]
- 14. Josey KP, Delaney SW, Wu X, Nethery R, DeSouza P, Braun D, et al. Air pollution and mortality at the intersection of race and social class. N Engl J Med 2023;388:1396–404. 10.1056/NEJMsa2300523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Jbaily A, Zhou X, Liu J, Lee TH, Kamareddine L, Verguet S, et al. Air pollution exposure disparities across US population and income groups. Nature 2022;601:228–33. 10.1038/s41586-021-04190-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Sallis JF, Floyd MF, Rodriguez DA, Saelens BE. Role of built environments in physical activity, obesity, and cardiovascular disease. Circulation 2012;125:729–37. 10.1161/CIRCULATIONAHA.110.969022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Wang SY, Tan ASL, Claggett B, Chandra A, Khatana SAM, Lutsey PL, et al. Longitudinal associations between income changes and incident cardiovascular disease: the atherosclerosis risk in communities study. JAMA Cardiol 2019;4:1203–12. 10.1001/jamacardio.2019.3788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Abdalla SM, Yu S, Galea S. Trends in cardiovascular disease prevalence by income level in the United States. JAMA Netw Open 2020;3:e2018150. 10.1001/jamanetworkopen.2020.18150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Overview of the National (Nationwide) Inpatient Sample (NIS) . Agency for Healthcare Research and Quality.https://hcup-us.ahrq.gov/nisoverview.jsp(accessed 1 March 2023).
- 20. Yale New Haven Services Corporation-Center for Outcomes Research and Evaluation . Mortality Measures Methodology. Center for Medicare & Medicaid Services.https://qualitynet.cms.gov/inpatient/measures/mortality/methodology(accessed 1 March 2023).
- 21. Wadhera RK, Joynt Maddox KE, Wasfy JH, Haneuse S, Shen C, Yeh RW. Association of the hospital readmissions reduction program with mortality among medicare beneficiaries hospitalized for heart failure, acute myocardial infarction, and pneumonia. JAMA 2018;320:2542–52. 10.1001/jama.2018.19232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. US Census Bureau . American Community Survey Data.https://www.census.gov/programs-surveys/acs/data.html(accessed 3 March 2023).
- 23. Introduction to the Healthcare Cost and Utilization Project (HCUP) National Inpatient Sample. Agency for Healthcare Research and Quality. https://hcup-us.ahrq.gov/db/nation/nis/NIS_Introduction_2018.jsp (accessed 1 March 2023). [PubMed]
- 24. Houchens R, Ross D, Elixhauser A, Jiang J. National Inpatient Sample (NIS) Redesign Final Report 2014; HCUP Methods Series Report # 2014-04. Agency for Healthcare Research and Quality.http://www.hcup-us.ahrq.gov/reports/methods/methods.jsp(accessed 5 March 2023).
- 25. Houchens R, Ross D, Elixhauser A. Using the HCUP National Inpatient Sample to Estimate Trends 2015. HCUP Methods Series Report # 2006-05. US Agency for Healthcare Research and Quality.http://www.hcup-us.ahrq.gov/reports/methods/methods.jsp(accessed 5 March 2023).
- 26. HCUP NIS Trend Weights . Healthcare Cost and Utilization Project (HCUP) October 2021. Agency for Healthcare and Research Quality.www.hcup-us.ahrq.gov/db/nation/nis/trendwghts.jsp(accessed 5 March 2023). [PubMed]
- 27. Khera R, Cram P, Lu X, Vyas A, Gerke A, Rosenthal GE, et al. Trends in the use of percutaneous ventricular assist devices. JAMA Intern Med 2015;175:941. 10.1001/jamainternmed.2014.7856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Khera R, Angraal S, Couch T, Welsh JW, Nallamothu B, Girotra S, et al. Adherence to methodological standards in research using the national inpatient sample. JAMA 2017;318:2011–8. 10.1001/jama.2017.17653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Khera R, Krumholz HM. With great power comes great responsibility big data research from the National Inpatient Sample. Circ Cardiovasc Qual Outcomes 2017;10:e003846. 10.1161/CIRCOUTCOMES.117.003846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. George MG, Tong X, Bowman BA. Prevalence of cardiovascular risk factors and strokes in younger adults. JAMA Neurol 2017;74:695–703. 10.1001/jamaneurol.2017.0020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Jain V, Minhas AMK, Khan SU, Greene SJ, Pandy A, Van Spall HGC, et al. Trends in HF hospitalizations among young adults in the United States from 2004 to 2018. JACC Heart Fail 2022;10:350–62. 10.1016/j.jchf.2022.01.021 [DOI] [PubMed] [Google Scholar]
- 32. Jain V, Minhas AMK, Morris AA, Greene SJ, Pandey A, Khan SS, et al. Demographic and regional trends of heart failure–related mortality in young adults in the US, 1999–2019. JAMA Cardiol 2022;7:900–4. 10.1001/jamacardio.2022.2213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Pabayo R, Kawachi I, Gilman SE. US state-level income inequality and risks of heart attack and coronary risk behaviors: longitudinal findings. Int J Public Health 2015;60:573–88. 10.1007/s00038-015-0678-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Bailey ZD, Feldman JM, Bassett MT. How structural racism works: racist policies as a root cause of US racial health inequities. N Engl J Med 2021;384:768–73. 10.1056/NEJMms2025396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. South E, Venkataramani A, Dalembert G. Building black wealth: the role of health systems in closing the gap. N Engl J Med 2022;387:844–9. 10.1056/NEJMms2209521 [DOI] [PubMed] [Google Scholar]
- 36. Wadhera RK, Dahabreh IJ. The US health equity crisis—an economic case for a moral imperative? JAMA 2023;329:1647–9. 10.1001/jama.2023.4018 [DOI] [PubMed] [Google Scholar]
- 37. Victor RG, Ravenell JE, Freeman A, Leonard D, Bhat DG, Shafiq M, et al. Effectiveness of a barber-based intervention for improving hypertension control in black men: the BARBER-1 study: a cluster randomized trial. Arch Intern Med 2011;171:342–50. 10.1001/archinternmed.2010.390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Schoenthaler AM, Lancaster KJ, Chaplin W, Butler M, Forsyth J, Ogedegbe G. Cluster randomized clinical trial of FAITH (Faith-Based Approaches in the Treatment of Hypertension) in blacks. Circ Cardiovasc Qual Outcomes 2018;11:e004691. 10.1161/CIRCOUTCOMES.118.004691 [DOI] [PubMed] [Google Scholar]
- 39. Brook RD, Dawood K, Foster B, Foust RM, Gaughan C, Kurian P, et al. Utilizing mobile health units for mass hypertension screening in socially vulnerable communities across Detroit. Hypertension 2022;79:e106–8. 10.1161/HYPERTENSIONAHA.122.19088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Sandhu S, Liu M, Wadhera RK. Hospitals and health equity—translating measurement into action. N Engl J Med 2022;387:2395–7. 10.1056/NEJMp2211648 [DOI] [PubMed] [Google Scholar]
- 41. Gondi S, Joynt Maddox K, Wadhera RK. “REACHing” for equity-moving from regressive toward progressive value-based payment. N Engl J Med 2022;387:97–9. 10.1056/NEJMp2204749 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
HCUP data are available through a data use agreement with AHRQ. CDC WONDER data are publicly available on the NCHS website.