Abstract
Ureteral avulsion can be secondary to blunt or penetrating trauma, or can emerge as a surgical complication. Popularization of minimally invasive interventions has significantly decreased ureteral injuries, ranging from 0% to 28% and varying from minor mucosal injury to perforation, and most catastrophically, avulsion. We present a case of complete ureteral avulsion that was not initially appreciated after undergoing ureteroscopy for stone extraction. Eventual recognition of this injury was managed successfully with a subsequent laparoscopically nephrectomy and renal auto-transplantation preserving renal function.
1. Introduction
Ureteral avulsion can occur as a result of blunt force trauma, penetrating injuries, or surgical complications, presenting a considerable medical challenge. Fortunately, the incidence of these injuries has remarkably decrease given the growing adoption of advanced minimally invasive interventions. Nevertheless, when those injuries actually take place, improvements in preservation and transplantation techniques have revolutionized treatment options. Renal auto-transplantation has come to be the gold standard for treating difficult ureteral injuries without compromising renal function. This method accentuates the unparalleled development in surgical procedures, giving a new ray of hope and better results for patients with challenging ureteral injuries such as avulsion.
2. Case presentation
A 29-year-old male, who has a history of recurring urolithiasis, arrived at our clinic with a right nephrostomy tube. This followed an "uncomplicated" right ureteroscopy undertaken due to acute renal colic during his visit to family in Pakistan. Unfortunately, there were no medical records available from his surgery, but the patient reported that a stent was not placed after the procedure, and he was discharged home. Patient then developed fevers, chills, abdominal pain, and distention. At another hospital in Pakistan he was diagnosed with ascites, additionally it was noted that the end of the right ureter was protruding out through the urethral meatus. Patient underwent an emergent right nephrostomy tube placement and a cystoscopy revealed a large ureteral segment attached to the ureteral orifice and moving freely inside the bladder (Fig. 1). Patient presented to our institution in the United States, where cystoscopy found no intra-vesical ureteral segment and the ureteral orifice could not be cannulated as it was severely stenotic. Antegrade nephrostogram revealed no contrast opacification beyond the proximal ureter (Fig. 2). Surgical options were presented, which included an ileal ureter, simple nephrectomy, and renal auto-transplantation. Patient decided to undergo renal auto-transplantation. An uncomplicated right laparoscopic nephrectomy was performed with a small proximal ureteral stump identified. Significant amount of fibrosis was encountered. Ex-vivo kidney examination found viable length of renal vessels and a healthy proximal ureter (Fig. 3). Routine auto-transplantation was performed with an extravesicular bladder anastomosis at the bladder dome. Follow-up at three months with renal ultrasonography revealed no hydronephrosis, normal renal echogenicity, and blood creatinine at 0.8 mg/dL.
Fig. 1.
Right avulsed ureter in bladder.
Fig. 2.
Right retrograde pyelogram.
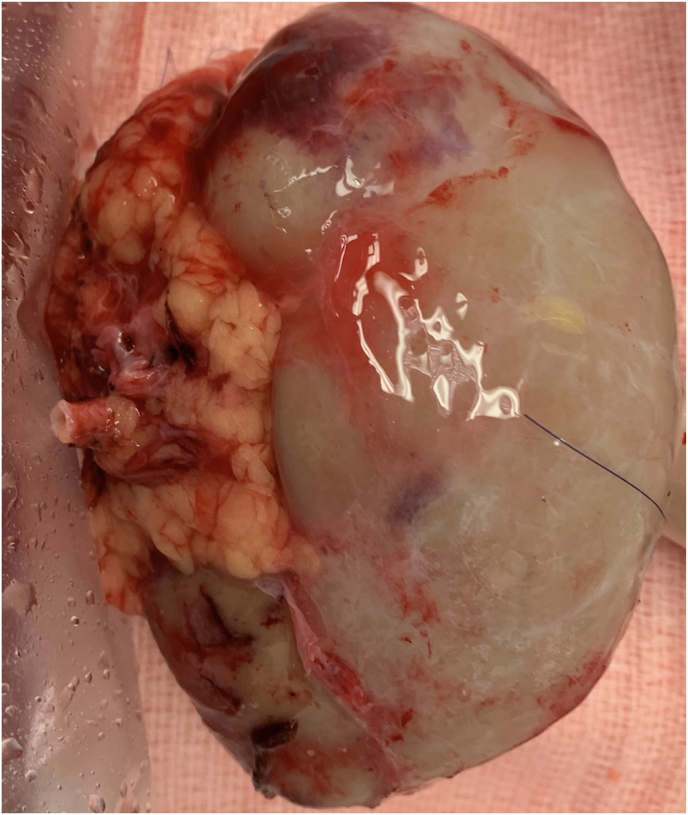
Fig. 3.
Ex vivo right kidney examination.
3. Discussion
Ureteral avulsion, occurring in only 0–2% of cases during ureteroscopy, is a rare but potentially catastrophic complication.1 Although there is no established standard protocol for its management, several factors must be carefully considered in determining the most suitable surgical intervention. These factors include the extent of avulsion, bladder size and function, history of prior abdominal interventions, and existing medical comorbidities.2 Additionally, certain risk factors predispose individuals to ureteral avulsion, such as the presence of longstanding symptomatic stones (lasting more than 3 months), large stones (greater than 5 mm in size), impacted stones firmly embedded into the ureteral wall, and previous extracorporeal shockwave lithotripsy treatment.3
Traditionally, the treatment of ureteral avulsion has been a surgical approach to restore ureteral continuity. Clear treatment guidelines are unresolved. Treatment is dependent on the length and location of viable remaining ureter and the functional status of the renal unit. If the avulsion involves the distal ureter, ureteroneocystostomy is the most appropriate approach. Avulsion originating from the middle third of the ureter may require a psoas hitch or Boari flap. Proximal ureteral injuries may require a nephrectomy, ileal ureteral interposition, transuretero-ureterostomy, chronic nephrostomy tube drainage or nephrectomy with autotransplantation.3
Renal auto transplantation was initially described in 1963 as an open intervention (midline xiphopubic incision) by Hardy, performed due to a high ureteral injury sustained during aortic surgery.4 Since then and with improved renal preservation techniques, this landmark procedure sparked the development of bench-side surgery that has been more frequently used in cases of complex ureteral injury. Potential benefits of auto-transplantation include a relatively bloodless surgical field and hypothermic protection of the kidney against ischemia.5 Meng and associates reported a case series of 7 patients with severe ureteral injuries not amenable to routine reconstruction with preoperative evaluation demonstrating comparable split renal function. Transperitoneal laparoscopic nephrectomy and auto-transplantation to the ipsilateral pelvis were performed. This study demonstrated acceptable perioperative morbidity and excellent graft function during 17-months follow up.6 Similarly, Novick et al. performed renal auto-transplants in 27 patients requiring replacement for injuries to the ureter. Renal function was preserved successfully in 92% patients.7 Likewise, Zhang and associates treated 2 patients who had severe iatrogenic proximal ureteral injury. Retroperitoneal laparoscopic nephrectomy and auto-transplantation was successfully performed, no perioperative complications occurred. At the end of the follow-up, the transplanted kidneys were functional, and the patients had returned to their normal activity.8 Despite the supporting evidence of renal auto-transplant success in cases of complicated proximal ureteral injuries, there are some limitations that need to be accounted for, such as patients age, comorbidities and surgical team expertise and center facilities.6
Given that our patient was deemed to be an ideal candidate and our team had the experience necessary to perform this surgical procedure, we decided to perform a right laparoscopic nephrectomy followed by renal auto-transplantation, achieving excellent renal function preservation and no intra or post-operative complications, further demonstrating the safety and efficacy of this surgical procedure in experienced hands. Close cooperation with a transplant team is crucial to coordinate graft harvest, ensure appropriate organ preparation and select the optimal urinary anastomosis.
4. Conclusion
To our best knowledge, this case stands as a rare instance where a patient has undergone successful treatment for complete ureteral avulsion through a renal auto-transplant. The significance of this case lies in its rarity, highlighting the scarcity of reported instances. The successful outcome suggests that renal auto-transplantation can be a viable and effective solution for addressing complete ureteral avulsion, thereby encouraging further research and consideration of this approach in similar clinical scenarios.
CRediT authorship contribution statement
Riya Sanampudi: Conceptualization, Methodology, Writing – original draft, Writing – review & editing. Maria C. Velasquez: Escobar, Conceptualization, Writing – original draft, Writing – review & editing. Chris E. Freise: Conceptualization, Supervision, Writing – original draft, Writing – review & editing. Marshall L. Stoller: Conceptualization, Supervision, Writing – original draft, Writing – review & editing.
References
- 1.Gupta P., Prabha V., Vernekar R., Devaraju S., Deole S., Adhikar P. Management of ureteric avulsion during ureteroscopy: our experience in A case series. World Journal of Nephrology and Urology. 2020;9(2):45–51. View at: Publisher Site | Google Scholar. [Google Scholar]
- 2.Shekar P.A., Kochhar G., Reddy D., Dumra A. Management of ureteric avulsion during ureteroscopy: a systematic review and our experience. Afr J Urol. 2020;26(58) View at: Publisher Site | Google Scholar. [Google Scholar]
- 3.Denis D., Moreno S., Velasco A., Salvadó J.A. Ureteral avulsion during retrograde intrarenal surgery: when the unexpected happens. J Endourol. 2020;6(3):177–179. doi: 10.1089/cren.2020.0006. View at: Publisher Site | Google Scholar. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hardy J.D. High ureteral injuries management by autotransplantation of the kidney. JAMA Network. 1963;184(2):97–101. doi: 10.1001/jama.1963.03700150051008. View at: Publisher Site | Google Scholar. [DOI] [PubMed] [Google Scholar]
- 5.Soto J.S., Phillips M., Cernigliaro J., Haley W. Renal autotransplantation for iatrogenic high-grade ureteric stricture. Case Reports in Urology. 2012;2012 doi: 10.1155/2012/259527. View at: Publisher Site | Google Scholar. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Meng M.V., Freise C.E., Stoller M.L. Expanded experience with laparoscopic nephrectomy and autotransplantation for severe ureteral injury. J Urol. 2003 Apr;169(4):1363–1367. doi: 10.1097/01.ju.0000054927.18678.5e. View at: Publisher Site | Google Scholar. [DOI] [PubMed] [Google Scholar]
- 7.Novick A.C., Jackson C.L., Straffon R.A. The role of renal autotransplantation in complex urological reconstruction. J Urol. 1990 Mar;143(3):452–457. doi: 10.1016/s0022-5347(17)39988-3. View at: Publisher Site | Google Scholar. [DOI] [PubMed] [Google Scholar]
- 8.Zhang H.X., Zhao L., Ma L.L., Hou X.F., Liu L., Deng S.H. Retroperitoneal laparoscopic nephrectomy with autotransplantation for severe iatrogenic ureteral injury. Xue Xue Bao Yi Xue Ban. 2016 Aug;48(4):622–626. View at: Publisher Site | Google Scholar. [PubMed] [Google Scholar]