Abstract
This study reports the successful management of a recurrent, refractory skin disease diagnosed clinically as Cutaneous Lichen Planus (CLP) in a female patient with Ayurvedic treatment. A 42-year-old home maker from Coimbatore presented with blackish-red pigmented skin rashes and white streaks. Though mucous membranes were not affected, she did not respond to homoeopathic and biomedical treatment. The lesions were spread all over the body except for the face, scalp, axillary and genital region. In addition, she complained of dry skin, pain, and itching.
The condition was treated as Kapha-Pitta dominant Tridoshaja Kushta based on Ayurvedic clinical assessment. The patient recovered after one year of conservative Ayurvedic intervention. After six years, there was a relapse, and the patient was admitted for a full course of Ayurvedic treatment and recovered within six months. Ayurvedic interventions should be considered an option in refractory skin diseases like Cutaneous Lichen Planus.
Keywords: Case report, Ayurveda, Kushta, Lichen planus, and bio-cleansing
1. Introduction
Skin diseases are among the most common health problems worldwide and contribute considerably to the global disease burden[1]. Lichen Planus (LP) is an autoimmune disease presenting as rashes on the skin.
LP may present as Cutaneous (CLP) or Mucosal (MLP) types. CLP affects the skin in the lower extremities but may also affect the upper extremities and trunk, whereas MLP can affect the oral mucosa and genitals [2]. The biomedical treatment includes systemic corticosteroids, retinoids, cyclosporine, photochemotherapy, hydroxychloroquine, azathioprine, or other immunosuppressants [3] but a tendency to flare up after stopping steroid treatment is very common [4]. The Ayurvedic approach to clinical diagnosis and management of skin diseases is based on the assessment of factors like Dosha (regulatory functional factors of the body), Ama (metabolic by-product generated due to improper or incomplete digestion and metabolism), and Sthana (site of manifestation) [5].
We are reporting the outcomes of Ayurvedic intervention in a patient diagnosed clinically by a dermatologist to be suffering from LP for more than a year. Her clinical presentation was suggestive of CLP. She responded well to conservative Ayurvedic intervention when biomedical and homeopathic interventions failed and her condition had worsened. The Ayurvedic assessment was Kapha-Pitta dominant Tridoshaja Kushta (skin disease with derangement of all three Doshas with dominance of Kapha and Pitta). Six years later, a relapse was also successfully managed with Ayurvedic treatment, which included bio-cleansing therapies. The outcomes suggest that Ayurvedic medicine can facilitate faster recovery in CLP.
2. Patient information
2.1. De-identified patient data
A 42-year-old female homemaker, native and living in Coimbatore, India, presented for clinical consultation during two episodes of her illness.
2.2. Patient concerns & symptoms
The patient complained of blackish-red pigmented skin lesions with white streaks associated with dryness of skin, pain, and itching sensation of two months duration. The lesions were spread all over the body except for the face, scalp, axillary and genital region in the first episode. Six years later, she presented again with a less severe relapse of the same symptoms.
2.3. Medical, family, psychosocial history
The patient did not have any significant medical history. However, her mother’s sister suffered from a similar skin ailment. The patient was stressed due to the discolouration of the skin and persistent itching, which caused sleep disturbance. Genetic predisposition was not assessed.
She was a homemaker and did not suffer from any other health issues before getting afflicted with this condition. She is known to have had some adverse reactions to biomedicines, which she noticed at the time of her child’s delivery (the skin lesions started four months after childbirth).
2.4. Past interventions & outcomes
The patient was healthy before 2010 until she noticed small non-oozing blackish-red eruptions with white shades in the flexor surface of the legs with pain and an itchy sensation. In two months, it eventually became big and spread to the whole body except on the face, axillary, scalp, and genital region. These lesions mainly erupted at night. For this, she first consulted a dermatologist. She was prescribed oral corticosteroid medications and topical ointment for external applications, details of which are unknown. The skin lesions aggravated, so she consulted a homoeopathic practitioner after one month. She was prescribed oral and topical medications by the homoeopath (the patient does not recall the names of the medicines). In the first week, the patient noticed improvements, but then the symptoms aggravated and did not subside even after continuing homoeopathic medicines for one month. The patient was mentally stressed as her body became discoloured throughout, with a persistent itchy sensation, which aggravated at night. As a result, her sleep was disturbed. She tried biomedical interventions, which further worsened her condition. She was constipated and experienced profuse hair loss. At this juncture, she sought Ayurveda treatment for the first time. She was advised to use oral medications and oil application externally and completely recovered in a year.
The patient discontinued all the medicines after recovering. She was asymptomatic for six years after that and led a normal life. In 2018, there was a relapse of skin lesions throughout her body, for which she sought Ayurvedic treatment within one month of its appearance. Initially, she consulted the Outpatient facility twice between November 2018 to March 2019. She was given oral medications for Agni Deepana (enhancing metabolic fire), Ama Pachana (digesting), and Sroto Shodhana (cleansing the body channels). After administering the necessary preparatory procedures, sodhana treatment was implemented. The treatments for the two episodes were administered in two different hospitals, though the chief treating doctor was the same on both occasions.
3. Clinical findings
The skin texture was slightly rough, dry, and thick, with slight elevation and scaling. The lesions were maculopapular, diffuse with blackish-red colour, and polygonal in shape with irregular borders. The lesions were distributed all over the body except the face, scalp, head, oral mucosa, nails, and genitals. Flakes with white streaks (Wickham Striae) [6] were also associated with pruritus.
4. Timeline
In the first episode, the patient underwent biomedical and homoeopathic treatments without positive responses. Subsequently, she opted for Ayurvedic treatment, involving Out-Patient treatments focusing on Mrdu Shodhana, Pachana Shodhana, Lekhana, and Shamana. In the second episode, she exclusively pursued Ayurvedic care, encompassing Out-Patient oral medications for Pachana, Shodhana, and Lekhana, along with In-Patient interventions such as Deepana, Pachana, Shodhananga Snehapana (internal oleation for the purpose of Shodhana), and Virechana. Post this, she took oral Rasayana (rejuvenation) as an Out-Patient treatment.
The two episodes of the manifestation of symptoms, the respective interventions, their outcomes and follow-up have been detailed in the timeline. Please refer to Table 1.
Table: 1.
| Date | Patient complaints | Interventions |
|---|---|---|
|
1st Episode: Non- Ayurvedic Interventions | ||
| October 12, 2010 | Patient noticed small non-oozing eruptions in the legs with pain and an itchy sensation. It eventually became big and spread to the whole body except the face, axillary, scalp and genital region within two months and mostly erupted at night. | Took biomedical interventions – Corticosteroids for one month. No Ayurveda interventions were done. |
| November 20, 2010 | Lesions aggravated, and the patient started to feel stressed about the condition as her whole body became blackish-discoloured with profuse, itchy sensations and pain. She experienced a lack of sleep because the lesions aggravated at night and also due to stress. There was excessive hair loss during this time. | Homoeopathic medications for one month. No Ayurveda interventions were done. |
| OP-based Ayurvedic Interventions | ||
| April 03, 2011 | At the time of Ayurveda consultation, she presented with lesions that were maculopapular, diffuse with blackish-red colour, and polygonal in shape with irregular borders. The lesions were distributed all over the body except the face, scalp, head, oral mucosa, nails, and genitals. Flakes with white streaks (Wickham Striae) were seen associated with itching. | Ayurvedic internal medications for Mrdu Shodhana, Pachana Shodhana and Lekhana were prescribed along with external applications for 30 days. |
| May 04, 2011 to July 23, 2011 | After one month of medications, the patches became light. The dryness and pain reduced. Occasional itching was present. | Continued Mrdu Shodhana, Pachana and Shamana medicines as internal medications. Medicated oils to moisten the skin and to normalise the skin colour were advised for three months. |
| July 23, 2011 to April 19, 2012 | Only light marks of the early lesions were visible on the skin, and there was no pain, itching or dryness. | Continued Ayurvedic internal medications and external applications for 9 months. |
| 2nd Episode: OP-based Ayurvedic Interventions | ||
| November 14, 2018 | Recurrence of hard, dry, raised and blackish discolouration of the skin, mainly in hands and legs, with itching and burning sensation. | Started with out-patient-based Pachana, Shodhana and Lekhana treatment for 33 days. |
| IP-based Ayurvedic Interventions | ||
| April 18, 2019 to April 30, 2019 | The blackish-red lesions on the skin reduced in intensity, and there was relief from pain, itching and dryness with oral medications. The lesions still persisted in the hands and legs with mild itching and burning sensation. | Deepana and Pachana medications were given for 2 days. |
| There were no changes in the skin lesions, but the itching and burning sensation had reduced. |
Shodhananga. Snehapana was administered for 7 days, Sarvanga Abhyanga and Bashpa Sweda for 3 days, Virechana 1 day and Samsarjana Krama for 1 day. |
|
| May 01, 2019 | The lesions and itching sensation had resolved. | Discharged and advised to take Madhusnuhi Rasayana for 30 days. |
| Follow-up | ||
| October 20, 2020 | On telephonic conversation, the patient reported no fresh lesions and is symptom-free | No medications from the last six months |
| May 11, 2021 | On telephonic conversation, patient reported to be symptom-free | Stopped taking all the Ayurvedic medications |
| July 30, 2022 | On telephonic conversation, patient reported to be symptom-free | No medications |
5. Diagnostic assessment
5.1. Diagnostic methods
The biomedical diagnosis was based on clinical observations. A confirmatory test, which is a skin biopsy, was not done. Ayurvedic diagnostic methods employed included Dasha Vidha Pariksha (tenfold examination of the patient), providing a comprehensive assessment of the patient. Nidana Panchaka (five diagnostic principles) helped in identifying aggravating and relieving factors, which aided in planning the treatment. These assessments helped us in estimating Ama, Dosha and Sthana and accordingly decide specific medications for Deepana, Pachana, Shodhana, Shamana and Rasayana.
5.2. Diagnostic challenges
A dermatologist provisionally diagnosed the case as Lichen Planus. There are many variants of LP. A specific diagnosis can be arrived at by clinical assessment and confirmatory biopsy. A biopsy is not routinely performed, and clinicians prefer to rely on the clinical diagnosis. LP may also be associated with Hepatitis C infections, but it is uncommon in South Asia and was not investigated. Being an invasive procedure, the patient was not willing to undergo a punch biopsy.
Arriving at a precise Ayurvedic diagnosis was also a challenge because the clinical presentation of the patient did not correlate with diseases described in Ayurvedic texts.
5.3. Diagnosis
5.3.1. Biomedical diagnosis
The dermatologist diagnosed the condition as LP, but the clinical presentation pointed specifically to Cutaneous Lichen Planus. Our patient presented erythematous, flat-topped, polygonal papules or macules that became umbilicated and took a violaceous colour. Pruritis is also present at the site of the lesions. When the lesions resolve, they leave behind hyperpigmented macules [3].
5.3.2. Ayurvedic diagnosis
We reviewed the clinical presentation of the patient with descriptions of Kushta [7], Kshudra Roga [8] and Visarpa [9] in classical Ayurvedic texts. Yet, we could not correlate it with any known conditions mentioned in Ayurvedic texts.
The probable Ayurvedic diagnoses considered in this case were Udumbara, Pittaja Visarpa, Charmadala, Kaksha, Mandala Kushta, and Charma Kushta, Vicharchika.
Udumbara Kushta: Due to symptoms like reddish nodules, pain, burning, and itchy sensation at the lesions, Udumbara Kushta was included for differential diagnosis, but as excessive brownish hair, the typical appearance of lesions in clusters which are very distinguishing of this Kushta were absent, it was excluded [[7], chapter 5 verse 8].
Charmadala: Due to pustular eruptions associated with an itching sensation seen in the patient, Charmadala was included for differential diagnosis, but as the burning sensation was not that prominent in the patient, it was excluded [[8], chapter 5 verse 10]
Kaksha: Symptoms of reddish-black, round indurated eruptions appearing along with pain predominantly distributed over the arms are seen in Kaksha (Kshudra Kushta). These symptoms were seen in this patient, the absence of fever and lesions in the axillary area, it was excluded [[8], chapter 13 verse 16].
Mandala Kushta: The skin lesions in Mandala Kushta are thick, erupted, with whitish shade, also resembling the symptoms in our patient but as the symptoms such as slimy yellowish copious discharge with maggots were absent this diagnosis was excluded [[7], chapter 5 verse 8].
Charma Kushta: Thick lesions as in Charmadala are seen in this patient and thus it was included for differential diagnosis, but as the lesion was not as thick as the skin of an elephant (lichenification) typical of Charma Kushta, it was excluded [[10], chapter 14 verse 20].
Vicharchika: Due to symptoms of blackish papular lesions and itchy sensation seen in the patient, Vicharchika was included for differential diagnosis, but as there was no discharge from the lesions, it was excluded [[10], chapter 14 verse 18].
Pittaja Visarpa: The lesions in this patient resembled that of Pittaja Visarpa in which there are many eruptions, rapidly spreading and associated with pain, but as it is also known to be suppurative, which was not seen in this case, it was excluded in the differential diagnosis [[8], chapter 5 verse 8]
Based on evaluating the symptoms and comparing them with the above-mentioned differential diagnosis, we could not get a single condition that fitted perfectly into any of them.
Hence, we considered this an Anuktavyadhi (a disease condition with no specific naming mentioned in the Ayurvedic texts) [[11], chapter 18 verses 44–45].
We could identify itching, white shade, and lines on the papules and thickness as the symptoms of aggravated Kapha; burning sensation and tenderness as a prominent symptom indicating the presence of aggravated Pitta; dryness, dark blackish-red discolouration, scaling, pain, and constipation as associated symptoms points to the presence of Vata. Thus, the condition was considered to be a Kapha-Pitta Pradhana Tridoshaja Kushta.
5.4. Prognosis
LP involving the flexor surface of the extremities (Cutaneous LP) is known to be self-limiting (resolves within six months to a year of onset), though the untreated hypertrophic variant can persist for years. In contrast, LP involving mucous membranes is known to have a chronic or progressive nature and does not attain complete remission Our patient presented with features of CLP involving both extremities and trunk, but her condition worsened after biomedical intervention, prompting her to seek Ayurvedic treatment. Kushta is one amongst the eight Mahavyadhis and is generally considered difficult to cure, especially when all three Doshas are involved. In this case, the clinical assessment pointed to a diagnosis of Kapha-Pitta Pradhana Tridoshaja Kushta, a condition difficult to treat.
6. Therapeutic intervention
6.1. Types of therapeutic intervention
Lekhana (scraping), Pachana (digesting), and Shodhana followed by Brmhana (nourishment) was the line of treatments chosen for the management of this condition.
In the first episode, the Lekhana and Pachana, and Mrdu Shodhana (mild bio-cleansing) were done. In the second episode, as the treatment was being done after a gap of six years, Lekhana and Pachana had to be repeated, and a classical method of Shodhana was also administered. As a follow-up, mild bio-cleansing, Prasadana (quality enhancing), and Rasayana medications were also administered.
6.2. Administration of therapeutic intervention
6.2.1. Internal mediations
For first episode: Manibhadra Lehyam [[12], chapter 19 verse 31–32], Aragwadhadi Kashayam [[5], chapter 15 verse 17-18 ], Patolamuladi Kashayam [[12], chapter 19 verse 28–30], Patolakaturohinyadi Kashayam [[5], chapter 15 verse15], Shaddharana Churnam [[12], chapter 21 verse 14], Drakshadi Lehyam [[12], chapter 16 verse 29–31], Trvrt Lehyam [[13] chapter 2 verse 9–10], Mahatiktakam Kashayam [[12], chapter 19 verse 8–11], Tiktaka Ghrtam [[12], chapter 19 verse 2–7], Mulakadi Kashayam, Hriberadi Kashayam [[14], Soothika roga p.107 ]and Drakshadi Kashayam [[12], chapter 1 verses 55–58].
For the second episode: Along with the above-said medicines, the following are the additional medications given in the second episode: Hinguvachadi Churnam [[12], chapter 14 verse 31–33], Nimbamrtasavam [[12], chapter 21 verse 58–61], Vaishvanara Churnam [[14], Choorna yoga p.190], Panchakola Phanta [[5], Chapter 6 verse 166]., Madhusnuhi Rasayana [[14], lehya prakarana. p. 229] and Mahatiktaka Ghrtam [[12], chapter 19 verse 8–11], Refer to Table 2 for a complete list of internal medications.
Table: 2.
Administration of internal Therapeutic intervention.
| Date | Rationale | Interventions | Dosage | Adjuvant | Duration |
|---|---|---|---|---|---|
| 03/04/2011 to 19/04/2012 | Mrdu | Manibhadra Lehyam (Herbal) | 10 gm at bedtime | hot water | 31 |
| Shodhana | |||||
|
Pachana Shodhana |
Aragwadhadi Kashayam (Herbal) | 15 ml before 1 Hr before breakfast and dinner | 45 ml of warm water | 291 | |
| Patolamuladi Kashayam (Herbal) | 15 ml before 1 Hr before breakfast and dinner | 45 ml of warm water | 100* | ||
| Pachana | Shaddharana Churnam (Herbal) | 5 gm before lunch | with buttermilk | 360* | |
| Lekhana | Patolakaturohinyadi Kashayam | 15 ml before 1 Hr before breakfast and dinner | 45 ml of warm water | 291* | |
| Mrdu | Drakshadi Lehyam + Trvrt Lehyam (Herbal) | 15 gm in the morning, empty stomach on weekends | with warm water | 48* | |
| Shodhana | |||||
| Shamana | Mahatiktakam Kashayam (Herbal) | 15 ml before 1 Hr of breakfast and dinner | 45 ml of warm water | 69 | |
| Mulakadi Kashayam (Herbal) | 15 ml before 1 Hr of breakfast and dinner | 45 ml of warm water | 329 | ||
| Tiktaka Ghrtam (Herbal) | 15 ml before 1 Hr of breakfast and dinner | 45 ml of warm water | 260 | ||
| Hriberadi Kashayam (Herbal) | 15 ml before 1 Hr of breakfast and dinner | 45 ml of warm water | 260 | ||
| Drakshadi Kashayam + Tiktakam Kashayam | 15 ml before 1 Hr of breakfast and dinner | 45 ml of warm water | 260* | ||
| 14/11/2018 to 03/06/2019 | Pachana, Shodhana & Lekhana | Patolamuladi Kashayam (Herbal) | 15 ml before 1 Hr of breakfast and dinner - For the first week, only | With 45 ml of warm water | 7* |
| Patolakaturohinyadi Kashayam (Herbal) | 15 ml at 06:00 a.m.m and 03:00 p.m.m | With 45ml warm water | 42* | ||
| Shaddharana Churnam (Herbal) | 5 gm before lunch | With buttermilk | 113* | ||
| Mrdu Shodhana | Drakshadi Lehyam + Trvrt Lehyam (Herbal) | 10 gm in the morning, empty stomach on weekends | with warm water | 4* | |
| Mrdu Shodhana | Trvrt Lehyam (Herbal) | 10 g at bedtime | with warm water | 119 | |
| Shamana | Drakshadi Kashayam + Tiktakam Kashayam (Herbal) | 15 ml before 1 Hr before breakfast and dinner | 45 ml of warm water | 188* | |
| Drakshadi Kashayam (Herbal) | 15 ml before 1 Hr before breakfast and dinner | 45 ml of warm water | 39 | ||
| Pachana | Hinguvachadi Churnam (Herbal) | 2 tsp | With warm water before lunch | 113 | |
| Nimbamrtasavam (Herbal) | 25 ml after lunch and dinner | – | 80 | ||
| Pachana | Vaishvanara Churnam (Herbal) | 5 gm at bedtime | Warm water | 42 | |
| Pachana | Panchakola Phanta (Herbal) | 500 ml to be taken throughout the day | – | 1 | |
| Rasayana | Madhusnuhi Rasayana (Herbal) | 1tsp twice daily | 33 | ||
| Shamana | Tiktakam Kashayam (Herbal) | 15ml before 1 Hr before breakfast and dinner | 45 ml of warm water | 42 | |
| Snehapana |
Mahatiktaka Ghrtam (Herbal) |
30 ml, 80 ml, 60 ml, 90 ml, 120 ml, 150 ml, 200 ml | hot water | 6 | |
*Note: Total duration of intake of Patolamuladi Kashayam is 107 days, Patolakaturohinyadi Kashayam is 333 days, Shaddharana Churnam is 473 days, Drakshadi Lehyam + Trvrt Lehyam is 52 days, Drakshadi Kashayam + Tiktakam Kashayam is 448 days.
6.2.2. External therapies
First episode: External therapies included Tiktaka ghrtam[[12], chapter 19 verse 2–7], to be applied on the lesions, Nimbadi Churnam [[15], Bh.Ra.vatarakta adhikara.31–38] to be applied as a Lepa (herbal paste). Oils Eladi Keram [15], Durvadi Tailam [9] [S.Y. taila prakarana. p. 149], Ksheerabala Tailam [[14], Taila prakarana p.315] and Vitpala Tailam for oil massage before bath.
Second episode: External application of Eladi Tailam [[5], chapter 15 verse 43–44], Nalpamaradi Tailam [[14], taila prakarana. p.289] for oil massage before bath.
Refer to Table 3 for a complete list of medications for external therapies.
Table: 3.
Administration of external Therapeutic intervention.
| Date | Changes in therapeutic interventions | Interventions | Duration |
|---|---|---|---|
| April 03, 2011 to April 19, 2012 | For moisturising the skin and normalise the skin colour | External application of Eladi Churnam, Vitpala Tailam, Eladi Keram (Herbal) | 31 |
| For moisturising the skin and normalise the skin colour | External application of Tiktaka Ghrtam, Eladi Keram, Durvadi Tailam, Nimbadi Churnam, Ksheerabala Tailam (Herbal) | 260 | |
| For moisturising the skin and normalise the skin colour | External application of Tiktaka Ghrtam (Herbal) | 69 | |
| For moisturising the skin and scraping off the thickened skin | External application of Eladi Keram, Durvadi Tailam, Nimbadi Churnam, Ksheerabala Tailam (Herbal) | 260 | |
| April 26, 2019 to April 28, 2019 | Used for Sarvanga Abhyanga before Virechana | External application of Eladi Tailam, Nalpamaradi Tailam (Herbal) | 2 |
6.2.3. Pathya (diet and lifestyle modifications advised)
The patient was put on a strict vegetarian diet and was advised to avoid green chillies, green peas, chickpeas, brinjal, spicy foods, curds, Upma, Puttu, Idli, Sambar. Excessive use of salt, pungent and sour foods was also restricted. She was advised to incorporate easily digestible, non-allergy-causing and natural foods into her diet. The lifestyle modifications suggested were avoiding day sleep, snacking/taking meals frequently, being awake late at night, and using irritant cosmetics. This diet was advised for both episodes. However, patient compliance was better in the second episode. This was advised based on the principles of diet and lifestyle recommended in Ayurveda classical texts on Kushta.
6.3. Changes in the therapeutic intervention
During the first episode, after the removal of Dosha through Lekhana and Pachana medications, signs of body heat and burning sensation started to show up, indicating aggravation of Pitta even though the itching had subsided to some extent. In this stage, Shamana was attempted by Mahatiktakam Kashayam and then by Mulakadi Kashayam because of its indication in Visarpa. However, this did not give much relief, and the medication was changed to Drakshadi and Hriberadi Kashayam, which provided good relief from body heat and burning sensation. The other Kashayams were also continued at this time. During this phase, Shaddharana Churnam was also introduced for Pachana and to balance Pitta.
Even as these treatments continued, the patient began to complain of constipation. To prevent further accumulation of Dosha and to maintain the movement of Dosha from Sakha to Koshta (from the peripheries of the body to the GIT), Manibhadra Lehyam was prescribed. However, the patient could not tolerate the medicine for longer due to its palatability. Hence, the medications were changed to Trvrt Lehyam and Drakshadi Lehyam, which were mixed and given at bedtime. It helped keep the bowel movements stable.
In the second episode, the treatment started with oral medications for Deepana and Pachana and upon achieving Niramavastha, In-Patient based Snehapana and Shodhana treatments followed. This time, the medicines were not changed during the treatment as there was better compliance.
7. Follow-up and outcomes
In the first episode, the Shodhana treatment was not done, and with this treatment, she got relief after one year. The second time, she came for a follow-up treatment after six years due to recurrence.
After completion of treatment during the second episode, the follow-up medications were prescribed after a course of Virechana (purgative therapy) focusing on Rasayana Chikitsa specific to the skin so that the relapsing episodes could be restricted. She was prescribed Madhusnuhi Rasayana to end the treatment in the final stage. The patient observed complete remission in symptoms and was advised to stop all the oral medications after 30 days upon getting discharged from the hospital. The patient also had been in touch with us telephonically thrice till the date after medications were stopped. The first time at an interval of 18 months, the second time after seven months of the previous contact and the third time after 14 months of the second follow-up. There has been no recurrence, and she is symptom-free.
7.1. Clinician and patient-assessed outcomes
7.1.1. Clinician assessed outcomes
In the first episode of Out-Patient based treatment:
When the patient last reported for consultation after the first Out-Patient based treatment, only light marks of the early lesions were visible on the skin, and the other symptoms had subsided. The skin had also got a normal texture.
See Fig. 1:Episode 1 of Out-Patient based treatment.
Fig: 1.
1st Episode of OP treatment.
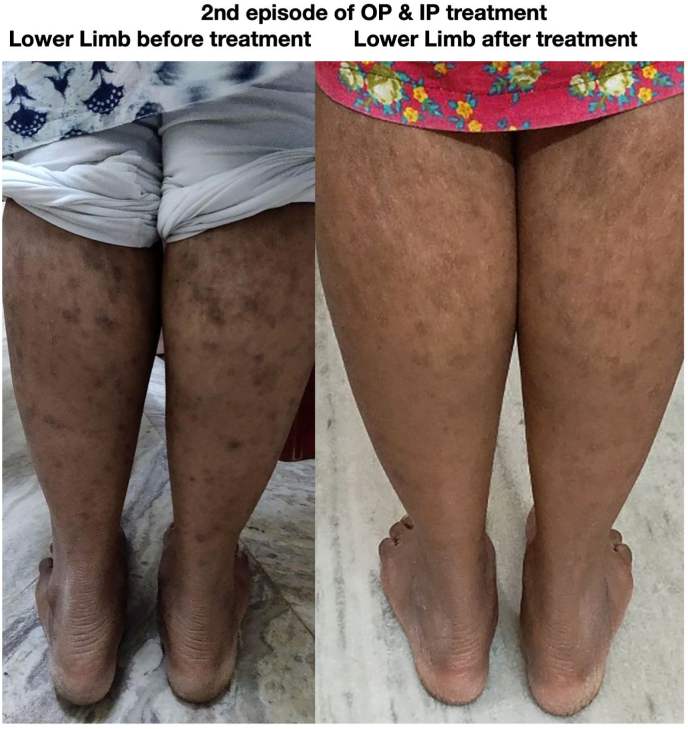
In the second episode of Out-Patient & In-Patient-based treatment:
After six years, all previous symptoms reappeared with less intensity. After one month of Outpatient-based treatment, the lesions reduced considerably throughout the body, with no itching, burning sensation, or body heat but did not resolve completely. Hence, Shodhana (bio-cleansing) treatment was done.
See Fig. 2 & Fig. 3: Episode 2 of Out-Patient & In-Patient based treatment.
Fig. 2.
2nd episode of OP & IP treatment.
Fig. 3.
2nd episode of OP & IP treatment.
7.1.2. Patient-assessed outcomes
An immediate outcome the patient could appreciate was pain reduction of the lesions in the first episode. The intensity of pain started to reduce within a day of the application of Maha Tiktaka Ghrtam externally. Another significant outcome that the patient reported is that no new lesions appeared after the start of Ayurveda treatment orally. The patient also noted that the skin recovered to normal appearance and texture, which reduced stress.
Similarly, even in the second episode, the patient started to respond immediately after the start of oral medications intended to prepare her body for an In-Patient-based classical bio-cleansing treatment. Soon after completing the in-patient treatment, new lesions stopped occurring. The follow-up medicines helped bring back the normal texture and colour of the skin.
7.2. Important follow-up diagnostic and other test results
The patient was not advised to undergo any investigatory tests during the follow-up as it was not necessary.
7.3. Intervention adherence and tolerability
The patient could not tolerate taking Manibhadra Lehyam for a more extended period due to palatability. During the second episode, she complied well and tolerated both the Out and Inpatient based treatments. She also adhered to the diet, which she felt was very restrictive.
7.4. Adverse and unanticipated events
No serious adverse events were noticed throughout the complete course of treatment for both episodes.
There was a notable unanticipated event during the second episode of treatment. During the In-Patient treatment, the patient was given medicine to purge. It was expected that she would get bowel movements a minimum of ten times, but she had it only five times. It probably could be because of the low dosage of the purgative administered. It was later compensated with administering a mild purgative daily in the follow-up medications, and the patient responded positively to it.
8. Discussion
8.1. Strengths and limitations
One of the strengths of this case report is the long follow-up of twelve years that helped to document the long-term outcomes of remission and recurrence. This case report also demonstrates how a disease could be looked at from the perspective of Ama, Dosha and Sthana and the changing patterns of predominant Dosha from time to time. Positive outcomes could be achieved when the treatment was tailored, focusing on these patterns.
In this case, the specific biomedical diagnosis was not confirmed using a biopsy by the dermatologist who treated the patient before the initiation of Ayurveda treatment.
8.2. Discussion of relevant medical literature
This case was tentatively diagnosed as a case of LP without specifying the variant by the treating dermatologist. However, the clinical presentation points to the diagnosis of a sub-type of Cutaneous Lichen Planus [2].
In Ayurveda, we could not find a single disease in the context of Kushta, Visarpa or Kshudra Roga, which matches the patient’s presentation of CLP. Hence, this condition was considered an Anuktavyadhi (not listed or described in the classical texts) and assessment was made considering the Nidana (aetiology), Dosha and Dushya (that which gets vitiated) following the guideline laid in the Charakasamhita.
Ama plays an important role, especially in the manifestation of skin conditions, and the success of treatment depends on how the Ama is managed.
In the first episode, the case was treated based on the assessment of Ama, Dosha and Sthana.
The Sthana being Tvak (skin) and the disease being Amashayodbhava (originating from the alimentary tract), Pachana and Shodhana Chikitsa were administered considering the Bahudoshavastha (copious quantity of vitiated Dosha) and Chala Ama (mobile Ama). As the patient was not willing to undergo a bio-cleansing therapy, Mrdushodhana (mild repeated bio-cleansing) and Shamana (pacifying) treatment were administered. She responded well to this treatment and was disease-free for six years, after which there was a relapse.
We assumed that the relapse was likely because of not administering Shodhana treatment during the first episode due to the patient's non-compliance. In the second episode, we planned for a Shodhana Chikitsa, followed by Rasayana treatment after bio-cleansing to prevent further relapse. The treatment during the second episode was also aimed at removing the Leena (deep-seated) Ama by Lekhana and Pachana treatments. It was observed that the recovery was faster this time, with no relapse of symptoms over the last two years despite stopping all medications and diet restrictions.
8.3. Conclusions
A literature search for Ayurveda case reports on LP retrieved three case reports on hypertrophic LP [16], Lichen Simplex Chronicus [17] and LP Pigmentosus [18]. These three cases showed effective outcomes from Ayurveda treatment, but the presentations of all three are different from ours. Hence, our case report is not a repetition of previously published case reports on LP.
From the point of view of bio-medicine, LP is self-limiting if the mucous membrane is not involved. However, on the contrary, our case had not responded to biomedical and homoeopathy treatments and had also aggravated after the interventions.
This case report also highlights the importance of Shodhana therapy in Kushta, which gave faster results than the Shamana treatment. Nevertheless, the effect of Shodhana (therapy cannot be fully confirmed until the patient’s condition is followed up for a much longer time until we conclude that the disease did not recur after Shodhana therapy is pursued.
8.4. The primary takeaway lessons of this case report
This case report suggests that Ayurvedic treatment has the potential to hasten recovery in CLP that is not responding to the standard of care. It also points to the need for long-term follow-up of the patients to gain a better understanding of the remission and relapse patterns of the disease. This case report also demonstrates how Ayurvedic principles of diagnosis and treatment can be applied to successfully manage diseases that are Anuktavyadhi.
9. Patient’s perspective
“Allopathic medications do not suit me at all. Ayurveda treatment was very effective and comfortable for me. I do not have words to describe how good I feel about the treatment. I should say that the Ayurveda treatment worked best for me.
The pain in the lesions subsided first after the start of Ayurveda treatment. My skin was very sensitive to touch back then. After that, the new lesions ceased to appear. Following this, the dark blackish-red discolouration of the skin started to become normal. The discolouration was very dark previously but has now become normal.
The results that I got were very quick with regard to pain. After applying Maha Tiktaka Ghrtam externally, the pain subsided within a day. I got 100% relief after taking this treatment and did not experience any discomfort after starting the Ayurveda treatment. While I was on allopathic medicine, the skin condition had aggravated very much, but after Ayurveda treatment, there wasn’t even a single aggravation of symptoms. Whatever symptoms I had started to reduce day by day. I am very much satisfied with the treatment.”
10. Informed consent
Informed consent was obtained from the patient to publish de-identified medical information.
Author contributions
SN: Writing, Visualization, Validation, Formal Analysis – Original Draft.
SK: Visualization, Validation, Formal Analysis.
AAR: Compilation of data.
RP: Writing – Review and Editing.
Funding sources, if any
We have not received any funding for this reporting.
Declaration of competing interest
The authors declare that the research was conducted without any commercial or financial relationships that could be construed as a potential conflict of interest. All the physicians who treated the case in both episodes are included as authors; hence, there is no conflict of interest. Moreover, the chief physician who treated the patient was the same in both episodes.
Footnotes
Peer review under responsibility of Transdisciplinary University, Bangalore.
References
- 1.Basra M.K., Shahrukh M. Burden of skin diseases. Expert Rev Pharmacoecon Outcomes Res. 2009 Jun;9(3):271–283. doi: 10.1586/erp.09.23. PMID: 19527100. [DOI] [PubMed] [Google Scholar]
- 2.Gorouhi F., Davari P., Fazel N. Cutaneous and mucosal lichen planus: a comprehensive review of clinical subtypes, risk factors, diagnosis, and prognosis. Sci World J. 2014 Jan 30;2014 doi: 10.1155/2014/742826. PMID: 24672362; PMCID: PMC3929580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boch K., Langan E.A., Zillikens D., Ludwig R.J., Kridin K. Retrospective analysis of the clinical characteristics and patient-reported outcomes in vulval lichen planus: results from a single-centre study. J Dermatol. 2021 Dec;48(12):1913–1917. doi: 10.1111/1346-8138.16191. Epub 2021 Oct 19. PMID: 34668211. [DOI] [PubMed] [Google Scholar]
- 4.Arnold D.L., Krishnamurthy K. StatPearls [internet]. Treasure island (FL) StatPearls Publishing; 2022 Jan. Lichen planus. 2022 Aug 21. PMID: 30252382. [PubMed] [Google Scholar]
- 5.Srikantha Murthy K.R. vol. 1. 2003. (Ashtanga hridayam of vagbhata. Sutra sthana). Doshabhediya Adyaya 12/65; Varanasi Chaukamba. [Google Scholar]
- 6.Ioannides D., Vakirlis E., Kemeny L., Marinovic B., Massone C., Murphy R., Nast A., Ronnevig J., Ruzicka T., Cooper S.M., Trüeb R.M., Pujol Vallverdú R.M., Wolf R., Neumann M. European S1 guidelines on the management of lichen planus: a cooperation of the European Dermatology Forum with the European Academy of Dermatology and Venereology. J Eur Acad Dermatol Venereol. 2020 Jul;34(7):1403–1414. doi: 10.1111/jdv.16464. PMID: 32678513. [DOI] [PubMed] [Google Scholar]
- 7.Sharma Priyavrat., editor. vol. 3. Chaukamba Orientalia; Varanasi: 2010. (Charaka Samhita of Charaka. Nidana sthana). [Google Scholar]
- 8.Sharma Priya Vrat., editor. vol. 2. Chaukamba Vishvabharathi; Varanasi: 2000. (Susruta Samhita of Dalhana. Nidana sthana). [Google Scholar]
- 9.Sharma Priyavrat., editor. vol. 5. Chaukamba Orientalia; Varanasi: 2010. (Charaka Samhita of Charaka. Chikitsa sthana). [Google Scholar]
- 10.Srikantha Murthy K.R. vol. 2. Varanasi Chaukamba; 2003. (Ashtanga Hridayam of Vagbhata. Nidana sthana). [Google Scholar]
- 11.Sharma Priyavrat., editor. vol. 1. Chaukamba Orientalia; Varanasi: 2010. p. 130. (Charaka Samhita of Charaka. Sutra sthana). [Google Scholar]
- 12.Srikantha Murthy K.R. vol. 2. Varanasi Chaukamba; 2003. (Ashtanga Hridayam of Vagbhata. Chikitsa sthana). [Google Scholar]
- 13.Srikantha Murthy K.R. vol. 2. 2003. p. 208. (Ashtanga Hridayam of Vagbhata. Kalpa sthana). Varanasi Chaukamba. [Google Scholar]
- 14.Vagbhatan Abhinava, KrishnanVydhar Aravattazhikathu K.V. 2010. Aanekkalleelil S Gopalapilla(Prasadakar)-Sahasrayogam-Vidyarambham Publikeshan. [Google Scholar]
- 15.Bhisagratna Shri Brahma Shankar Mishra (editor) Bhaishajyaratnavali of Shri Govinda Dasji -1st Volume, vatarakta chikitsa 28-35, Varanasi Chaukamba Sanskrit sthana vol. 200, p.591. .
- 16.Ratha K.K., Barik L., Panda A.K., Hazra J. A single case study of treating hypertrophic lichen planus with Ayurvedic medicine. Ayu. 2016 Jan-Mar;37(1):56–61. doi: 10.4103/ayu.AYU_1_16. PMID: 28827956; PMCID: PMC5541468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pandey O., Makwana S., Bedarkar P. Ayurvedic management of Lichen simplex chronicus-A case report. Annals of Ayurved. Med. 2020 Oct 23;9(3):220. [Google Scholar]
- 18.Makwana S.M., Kapadiya M.M., Bedarakar P., Patgiri B.J. A case report of chronic lichen planus Pigmentosus treating with Ayurveda management. Annals of Ayurved. Med. 2020 Sep 7;9(1):44. [Google Scholar]