Abstract
Introduction
Carotid body tumor (CBT), a neuroendocrine neoplasm, and benign multinodular goiter (BMNG) are distinct pathologies affecting the neck region. Although rare, they can occur concurrently. This case contributes to the limited evidence regarding the association between these distinct pathologies and their operative management.
Case presentation
The patient was a 45-year-old female with a palpable mass on the right side of her neck. She was diagnosed with Shamblin type III non-secretory CBT alongside BMNG. The surgical intervention included resection of the CBT, carotid artery bypass, and Dunhill thyroidectomy.
Discussion
This case is the third reported instance of coexisting CBT and BMNG. Their causative relationship is evident in the literature without a clear explanation of the underlying mechanism. Both conditions are treated surgically. Dunhill thyroidectomy for BMNG is a safer option, offering more flexibility and advantages over other thyroidectomies.
Conclusion
This case highlights the complexity of managing such dual pathologies and may provide further evidence of their association.
Keywords: Case report, Carotid body tumor, Benign multinodular goiter, Carotid artery bypass, Dunhill thyroidectomy
Highlights
-
•
Concomitant presence of carotid body tumor with multinodular goiter is rare with only two cases reported before.
-
•
This case report represents a Shamblin type III non-secretory carotid body tumor with benign multinodular goiter.
-
•
The therapeutic intervention involved cartotid body tumor resection, carotid artery bypass, and Dunhill thyroidectomy.
-
•
This case highlights the complexity of managing dual pathologies and may provide further evidence of their association.
1. Introduction
Paragangliomas are neuroendocrine tumors originating from embryonic nervous tissue. In the head and neck region, CBTs are the most commonly occurring paragangliomas [1]. These tumors are more common in females and typically present in the fourth to fifth decade of life [2]. The estimated incidence of these tumors in the general population ranges from 1 in 30,000 to 100,000 [3].
While most carotid body tumors are benign, there is a potential for malignancy, accounting for approximately 2 %–12.5 % of cases [4]. The clinical manifestations of both benign and malignant CBTs often share similarities, producing local compressive symptoms such as hearing loss, ear pain, tinnitus, neck mass, or cranial neuropathy leading to swallowing difficulty, facial weakness, and hoarseness [6].
Due to the highly vascular nature of CBTs, biopsies are impractical, emphasizing the crucial role of radiological imaging in preoperative diagnosis and planning [2]. The preferred treatment for CBT is surgical resection, which may be performed with or without adjuvant radiotherapy [4].
Multinodular goiter is characterized by the presence of multiple functional or non-functional nodules in the thyroid gland. It occurs in 5 % of the population in endemic regions and sporadically in less than 5 % [3]. Nodular goiter results from follicular cell hyperplasia or enlargement of newly formed follicles. Etiological factors include iodine levels, genetics, environmental pollutants [8], and conditions like infiltrative disorders, lymphoma, metastatic tumors, lipoma, or paraganglioma [14]. Surgical treatment is recognized as an effective method for managing benign nontoxic multinodular goiter [7].
We presents a rare case report involving a Shamblin type III CBT in conjunction with a BMNG, managed through surgical resection with carotid artery bypass for CBT and Dunhill thyroidectomy for BMNG. The coexistence of CBTs and multinodular goiter is rare, with only two reported cases to date [3,9]. This case study is reported in concordance with the SCARE criteria [10].
2. Case presentation
A 45-year-old woman from a high-altitude region in Afghanistan presented to our hospital with a sizable mass on the right side of her neck that had progressively grown over the past 7 years. At the time of presentation, she reported no symptoms, and her medical and family history revealed no relevant issues. During the physical examination, the patient exhibited normal vital signs. A lobulated, non-tender, pulsating, firm mass measuring 5 × 10 cm extending from the right submandibular region to the right side of the suprasternal notch was identified (Fig. 4-A).
Fig. 4.
A) Preoperative image shows the massive tumor protruding in the right side of the neck. B) 6-Month post-op image. Improvement is evident.
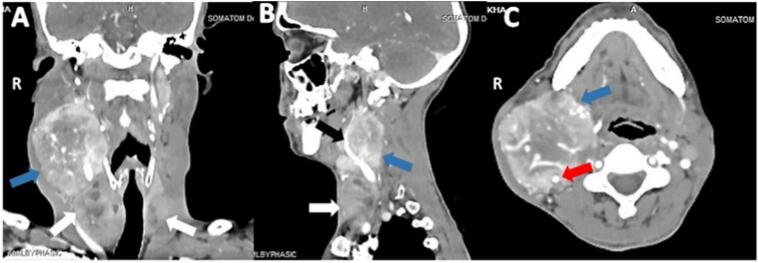
Ultrasonography disclosed an oval-shaped, hypoechoic, highly vascular mass just above the right carotid bifurcation enveloping the external carotid artery, suggestive of a carotid body tumor. Additionally, two complex nodules with smooth margins and spongiform textures were observed in the thyroid gland. The nodules measured 4.7 × 3.2 cm in the right lobe and 2.7 × 2 cm in the left lobe. Normal thyroid function tests and the absence of serum antithyroglobulin antibodies or thyroperoxidase antibodies were noted. Tests for catecholamine and metanephrine levels in serum and urine were within normal ranges. Fine needle aspiration confirmed the presence of nonmalignant cells. Contrast-enhanced CT scan unveiled a highly vascular mass measuring 6 × 6 × 7.6 cm between the external and internal carotid arteries, causing significant displacement. The lesion completely encased the external carotid artery and partially encased the internal carotid artery. Multiple thyroid nodules were also evident (Fig. 1). These findings were conclusive of non-secretory right-sided CBT along with bilateral BMNG.
Fig. 1.
Preoperative images of the tumor. A) Carotid body tumor (blue arrow) and multinodular goiter (white arrows) in a contrast-enhanced CT scan coronal view. B) External carotid artery (black arrow) completely encased with carotid body tumor (blue arrow) and multinodular goiter (white arrow) in sagittal view. C) Partial encasement of the internal carotid artery (red arrow) along with carotid body tumor (blue arrow). (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
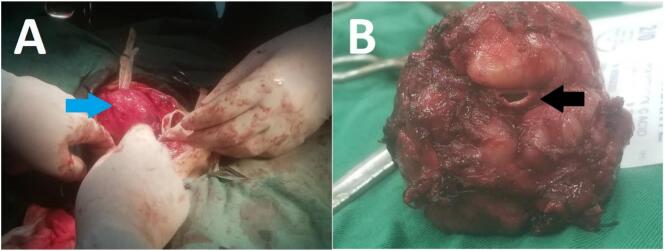
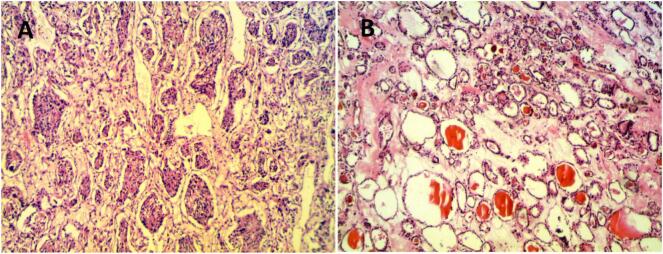
The treatment plan involved a 12 cm incision along the anterior border of the sternocleidomastoid muscle for the resection of the carotid body tumor mass coupled with a collar extension for Dunhill thyroidectomy. Due to the tumor's attachment to the common carotid artery, en-bloc resection was performed, followed by reconstruction using a common carotid artery to internal carotid bypass with a saphenous vein graft. Two lymph node resections were conducted to rule out metastasis (Fig. 2). After Dunhill's procedure, about 3 g of thyroid tissue remained in the left thyroid lobe. The pathology report revealed the Zellballen nests surrounded by a fibrovascular network with no signs of lymph node invasion suggestive of a benign CBT. The thyroid tissue was benign, exhibiting colloid-filled follicles and stroma (Fig. 3). The patient's recovery phase was uneventful, and she was discharged on the fourth day after operation and advised to continue levothyroxine hormone therapy. She experienced some hoarseness, which resolved within 3 weeks. In 6 months of follow-up, the patient was satisfied with the surgery, with no reported operation-related complications (Fig. 4-B).
Fig. 2.
A) Carotid body tumor (blue arrow) at the beginning of the dissection. B) Common carotid artery (black arrow) in the middle of carotid body tumor after tumor resection. (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
Fig. 3.
A) Zellballen nests surrounded by fibrovascular network suggestive of carotid body tumor. B) Thyroid follicles and thyroid stroma suggestive of benign pathology.
3. Discussion
CBTs are uncommon chemical receptor tumors, constituting 0.6 % of head and neck tumors, and are typically benign, with a 2 %–12.5 % chance of malignancy [4]. These specialized spherical organs, located in the carotid bifurcation's adventitia, have a reddish-brown color and are mainly supplied by feeding arteries of the external carotid artery. Although residents at higher altitudes often exhibit larger carotid bodies [11], 30 % of paragangliomas stem from genetic mutations, demonstrating autosomal dominant inheritance [2]. Though genetic testing wasn't feasible, no family history indicated hereditary syndromes. Shamblin and colleagues developed a classification for CBT based on tumor size and carotid artery involvement, aiding in assessing the risk of nerve injuries, intraoperative blood loss, and the need for carotid artery reconstruction. Shamblin Type I tumors are small and located at the carotid bifurcation; Type II tumors are larger and split the carotid arteries; and Type III tumors are large, often encasing the carotid arteries. Operating on a Shamblin III CBT is associated with neurovascular complications and may require arterial resection and vascular grafting [12].
CBTs are commonly detected secondarily during physical examination or imaging studies. However, further imaging and histopathological studies are necessary to confirm this diagnosis. Common imaging techniques include Doppler ultrasonography, CT scan, MRI, and conventional angiography. While angiography traditionally served as the mainstay for CBT diagnosis and preoperative planning, CT angiography and MR angiography are now preferred modalities [11]. Surgical resection is the medical treatment of choice for CBT, with a reported local control rate of 94 to 100 % [13].
Among the endocrine disorders, the majority of surgical interventions are performed for BMNG [16], to address compressive symptoms, malignancy suspicion, substernal development of goiter, drug-resistant hyperthyroidism, and cosmetic concerns [18]. Surgical techniques include total thyroidectomy, bilateral subtotal thyroidectomy, Dunhill thyroidectomy, and modification of the methods mentioned above [7]. When evaluating treatment options, it is essential to assess each patient individually, considering factors such as the risk-benefit relationship, patient preference, and the treating physician's experience [8]. Despite the decline in subtotal thyroidectomy for BMNG due to perceived safety in total thyroidectomy, it remains prevalent globally [17]. According to a study by Mauriello C. and colleagues, opting for total thyroidectomy over the Dunhill thyroidectomy would result in only 1.75 % of patients being able to avoid a second surgery. However, this choice carries a higher risk of at least 8.4 % for developing permanent hypoparathyroidism and a 0.9 % increased risk of permanent recurrent nerve palsy [18]. Dunhill thyroidectomy provides more operative flexibility and advantages over bilateral subtotal thyroidectomy. Firstly, only one side needs exploration in case of reoperation, and in papillary microcarcinoma cases, hemithyroidectomy is enough, avoiding completion thyroidectomy [15].
Paraganglioma may exhibit associations with other tumor types, including kidney cancer, parathyroid adenoma, thyroid carcinoma, and others [5]. However, only one article has noted a direct link between thyroid nodules and paraganglioma, but without explaining the underlying mechanism [14]. While two cases have described the concurrent presence of BMNG with Shamblin type II CBT, for none of them arterial reconstruction required, this case report details a Shamblin Type III large carotid body tumor treated with resection and vascular graft alongside asymptomatic BMNG treated with Dunhill thyroidectomy that wasn't used in the previous cases.
4. Conclusion
CBT and multinodular goiter are distinct pathologies; however, they can coexist. Their association is documented in the literature, yet the underlying mechanism remains unexplained. The preferred treatment for CBT is complete surgical resection. Regarding multinodular goiter, among various thyroidectomies, Dunhill thyroidectomy is considered safer than total thyroidectomy and offers more flexibility and advantages compared to bilateral subtotal thyroidectomy.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal upon request.
Ethical approval
Ethical approval was waived by the author's institution.
Funding
The authors received no funding for the writing of this article.
Author contribution
Ahmad Fawad Wardak: Conceptualization, Writing – review & editing, Data curation. Torgot Ghani: Writing – review & editing, Data curation, Supervision. Sayed Ismatullah Ardam: Data curation, Munir Ahmad Musamim: Supervision. Turan Ghani: Data curation. Haroon Alamy: Data curation. All authors have seen and approved the final manuscript.
Guarantor
Dr. Ahmad Fawad Wardak
Dr. Torgot Ghani
Conflict of interest statement
All authors declare no conflict of interest.
Acknowledgment
None.
References
- 1.Xing J., Cheng Y., Ying H., Guan M., Jia N., Bai C. Systemic treatment of a metastatic carotid body tumor: a case report and literature review. Medicine (Baltimore) 2020;99(47) doi: 10.1097/MD.0000000000022811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Berger G., Łukasiewicz A., Grinevych V., Tarasów E. Carotid body tumor - radiological imaging and genetic assessment. Pol. Przegl. Chir. 2020;92(6):39–44. doi: 10.5604/01.3001.0014.4872. [DOI] [PubMed] [Google Scholar]
- 3.Garcia-Alva R., Bobadilla-Rosado L.O., Arzola L.H., Escobar-Preciado M., Anaya-Ayala J.E., Hinojosa C.A. A case report of a concomitant total thyroidectomy and carotid body tumor resection in a 43 year old female. Int. J. Surg. Case Rep. 2018;53:17–20. doi: 10.1016/j.ijscr.2018.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Archang M.M., Lee S., Ziu I., et al. Malignant carotid paraganglioma: a case report. Cureus. 2023;15(7) doi: 10.7759/cureus.41765. (Published 2023 Jul 12) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lin B., Yang H.Y., Yang H.J., Shen S.Y. Concomitant paraganglioma and thyroid carcinoma: a case report. World J. Clin. Cases. 2019;7(5):656–662. doi: 10.12998/wjcc.v7.i5.656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.López-Arcas J.M., Colmenero C.M., Martínez R., Martín-Hernán F., Ruiz-Sánchez B., Aragoneses J.M. Giant carotid chemodectoma treated with a combination of surgery and CyberKnife radiotherapy: a case report and review of the literature. J. Med. Case Rep. 2022;16(1):92. doi: 10.1186/s13256-021-03237-y. (Published 2022 Feb 25) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kaliszewski K., Wojtczak B., Grzegrzółka J., et al. Nontoxic multinodular goitre and incidental thyroid cancer: what is the best surgical strategy?-A retrospective study of 2032 patients. Int. J. Endocrinol. 2018;2018 doi: 10.1155/2018/4735436. (Published 2018 May 14) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Unlu M.T., Kostek M., Aygun N., Isgor A., Uludag M. Non-toxic multinodular goiter: from etiopathogenesis to treatment. Sisli Etfal Hastan Tip Bul. 2022;56(1):21–40. doi: 10.14744/SEMB.2022.56514. 10.14744/SEMB.2022.56514 Published 2022 Mar 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Corbett A.J., McClintock J.C. Tumor of the carotid body associated with nodular goiter; report of a case. Arch. Surg. (1920) 1950;60(1) doi: 10.1001/archsurg.1950.01250010097008. [DOI] [PubMed] [Google Scholar]
- 10.Sohrabi C., Mathew G., Maria N., Kerwan A., Franchi T., Agha R.A. The SCARE 2023 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. Lond. Engl. 2023;109(5):1136. doi: 10.1097/JS9.0000000000000373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hoang V.T., Trinh C.T., Lai T.A.K., Doan D.T., Tran T.T.T. Carotid body tumor: a case report and literature review. J. Radiol. Case Rep. 2019;13(8):19–30. doi: 10.3941/jrcr.v13i8.3681. Published 2019 Aug 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alfawaz A.A., Albloushi D., Quttaineh D., Alsafran S., AlQabandi O., Albader M. Malignant carotid body tumor: a report of two cases. Ann. Med. Surg. (Lond). 2023;85(5):1857–1862. doi: 10.1097/MS9.0000000000000402. Published 2023 Apr 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Huang P., Bao H., Zhang L., Liu R. Surgical treatments and diagnosis of the carotid-body tumor. Asian J. Surg. 2023;46(2):941–942. doi: 10.1016/j.asjsur.2022.07.068. [DOI] [PubMed] [Google Scholar]
- 14.Wong R., Farrell S.G., Grossmann M. Thyroid nodules: diagnosis and management. Med. J. Aust. 2018;209(2):92–98. doi: 10.5694/mja17.01204. [DOI] [PubMed] [Google Scholar]
- 15.Rayes N., Steinmüller T., Schröder S., et al. Bilateral subtotal thyroidectomy versus hemithyroidectomy plus subtotal resection (Dunhill procedure) for benign goiter: long-term results of a prospective, randomized study. World J. Surg. 2013;37(1):84–90. doi: 10.1007/s00268-012-1793-8. [DOI] [PubMed] [Google Scholar]
- 16.Agarwal G., Aggarwal V. Is total thyroidectomy the surgical procedure of choice for benign multinodular goiter? An evidence-based review. World J. Surg. 2008;32(7):1313–1324. doi: 10.1007/s00268-008-9579-8. [DOI] [PubMed] [Google Scholar]
- 17.Makay Ö. Less than total thyroidectomy for goiter: when and how? Gland Surg. 2017;6(Suppl. 1):S49–S58. doi: 10.21037/gs.2017.10.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mauriello C., Marte G., Canfora A., et al. Bilateral benign multinodular goiter: what is the adequate surgical therapy? A review of literature. Int. J. Surg. 2016;28(Suppl. 1):S7–S12. doi: 10.1016/j.ijsu.2015.12.041. [DOI] [PubMed] [Google Scholar]