Highlights
-
•
Cardiac dose constraints dramatically decreased thanks to the new breast RT techniques.
-
•
In ›10% of cases these may only be achieved by using either the DIBH or prone technique.
-
•
The preferable method may be chosen based on the lung volumes and anatomical features.
-
•
The predictors for the optimal heart sparing method may be checked before RT planning.
Keywords: Breast radiotherapy, DIBH, Radiation heart damage, Predictors, Spirometry
Abstract
Introduction
Deep-inspirational breath hold (DIBH) is an option for heart protection in breast radiotherapy; we intended to study its individual benefit.
Materials and Methods
3DCRT treatment planning was performed in a cohort of 103 patients receiving radiotherapy of the whole breast (WBI)/chest wall (CWI) ± nodal regions (NI) both under DIBH and free breathing (FB) in the supine position, and in the WBI only cases prone (n = 45) position, too. A series of patient-related and heart dosimetry parameters were analyzed.
Results
The DIBH technique provided dramatic reduction of all heart dosimetry parameters the individual benefit, however, varied. In the whole population the best predictor of benefit was the ratio of ipsilateral lung volume (ILV)FB and ILVDIBH. In the WBI cohort 9–11 patients and 5–8 patients received less dose to selected heart structures with the DIBH and prone positioning, respectively; based on meeting various dose constraints DIBH was the only solution in 6–13 cases, and prone positioning in 5–6 cases. In addition to other excellent predictors, a small ILVFB or ILVDIBH with outstanding predicting performance (AUC ≥ 0.90) suggested prone positioning. Detailed analysis consistently indicated the outstanding performance of ILVFB and ILVDIBH in predicting the benefit of one over the other technique in lowering the mean heart dose (MHD), left anterior descending coronary artery (LAD) mean dose and left ventricle(LV)-V5Gy. The preference of prone positioning was further confirmed by anatomical parameters measured on a single CT scan at the middle of the heart. Performing spirometry in a cohort of 12 patients, vital capacity showed the strongest correlation with ILVFB and ILVDIBH hence this test could be evaluated as a clinical tool for patient selection.
Discussion
Individual lung volume measures estimated by spirometry and anatomical data examined prior to acquiring planning CT may support the preference of DIBH or prone radiotherapy for optimal heart protection.
Introduction
Postoperative radiotherapy is essential in breast cancer (BC) care, even if its risks are widely known [1], [2], [3], [4]. The most significant concern is radiation-induced heart disease (RIHD) due to the damage of the coronary arteries and microvessels that causes clinical symptoms many years after the irradiation in the form of ischemic heart disease leading to the deterioration of QOL or even a fatal event [1], [2], [3], [4], [5]. RIHD is considered more significant in left-sided cases, clearly radiation dose-dependent and its manifestation depends on individual features including basic cardiovascular risk status, systemic therapies and radiosensitivity [1], [2], [3], [4], [5], [6], [7]. First, the EBCTCG metaanalysis pointed to the increase of the incidence of cardiac death after radiotherapy in left-sided cases [4], [5], [6], [7]. The first evidence on the role of the radiation heart dose was provided by the iconic study of Darby et al. [1]. In that population-based case-control study of 2168 patients irradiated between 1953 and 2001, a retrospective reconstruction of doses from 2D radiotherapy plans demonstrated a significant association of the mean heart dose (MHD) and the increase of risk of major coronary events with a HR of 7.4 % for every one Gy increase of the MHD. Another analysis of randomized clinical studies confirming that, found a strong correlation between the MHD and the LAD dose [2]. Taylor et al. found a direct relationship between laterality and injury to different segments of the left ventricle (LV) and coronary arteries; the highest radiation doses were detected in the distal segments of the LAD [6]. Similar dose–response results were found in a nested case–control study in a more contemporary cohort of young patients: every 1 Gy increase in MHD was associated with a 6.4 % increase in the risk of myocardial infarction; in MHD > 20 Gy cases, the risk was 3.4 times higher [8]. The association between dose and risk was linear in all studies, and no upper or lower threshold of effect was demonstrated [1], [8]. Based on 3DCRT dose-volume data of almost 1000 patients and a median follow-up time of 7.6 years, van Bogaard et al. using the same risk factors and end-points as Darby et al., found an increase of 16.5 % in the cumulative incidence of acute coronary events per one Gy of MHD [9]. In addition, they identified the LV-V5 parameter as the most powerful prognostic indicator with a HR of 1.016 (95 % CI 1.002–1.030); the LV-V5 prognostic dose-volume parameter was implemented in an NTCP model for acute coronary events together with age, and weighed basic risk score. Based on these findings the DEGRO recommendation prioritized the use of LV-V5 among the dose constraints [10].
Many volumes of interest and dose constraints have been used in practice for the study of heart dose, such as the MHD, heart V25Gy, LAD mean dose and LAD maximum dose [2], [3], [8], [10], [11], [12], [13], [14], [15], [16], [17]. The recently introduced LV dosimetry is more and more used [9], [10], [14]. With the aim of optimizing dose reporting a new organ at risk (OAR) volume the LAD region (LADR) has been described; that approach intended to improve delineation consistency if performed without contrast-enhanced CT by including the LAD and its branches in a more generous subvolume than just the LAD [17].
There are many approaches to protect the heart from radiation exposure. While prone positioning modifies the geography of the breast, the DIBH technique alters the position of the heart relative to the chest wall. The advanced IMRT and proton irradiation techniques maximize the conformity of the irradiated volume. While prone radiotherapy dramatically reduces lung doses, heart doses individually differ [2], [11], [12], [13]. The breath-holding technique’s greatest impact is reduced dose to the heart and LAD, and to a lesser extent to the lung [18], [19], [20]. The magnitude of benefit of each technique depends on the patients’ anatomical features and lung capacity. While prone positioning was originally found favorable in patients with large breasts, later on variability in that and other anatomical parameters such as the BMI and position of the heart in the supine position as the most significant predictors were demonstrated [12], [13], [21], [22]. While the DIBH technique was found advantageous in most, in a minority of cases it was neutral or even detrimental [21], [22], [23], [24], [25], [26], [27], [28], [29]. Furthermore, there are completely new approaches by integrating heart protection into multi-OAR composite plan quality scores weighed on the basis of individual risk statuses [30].
The consideration of various cardiac doses and the use of heart protecting techniques (preferably DIBH) is stressed in a recent guideline [10]. We add that the individual features of the patients should be carefully considered for selecting the appropriate method serving optimum heart protection.
We intended to study the individual benefit of DIBH on cardiac sparing based on a set of dosimetry data of various heart structures in a cohort of BC patients needing either WBI or postmastectomy irradiation (PMI) with or without NI. In cases receiving WBI only anatomical and functional predictors for a greater benefit of prone positioning were also analyzed.
Materials and methods
This prospective cohort study had been approved by the Institutional Ethics Review Board of the University of Szeged (#272/2017) and, all the enrolled patients gave their written informed consent to participation. Inclusion criteria were left-sided BC needing postoperative WBI/CWI ± NI, exclusion criteria were the presence of COPD, bronchial asthma or other severe comorbidity (extreme obesity, mental disorder, hypacusis). The patients participating in the dosimetry analysis were enrolled in 2018–2019.
The procedures of training for DIBH-supported radiotherapy have been described earlier in detail [25]. Non-contrast planning CT series were acquired in the supine position with the arms elevated under both normal breathing and DIBH; in the WBI cases CT was performed also in the prone position. Patient-related anatomical data including body weight, height and BMI were prospectively collected.
The aim of our analysis was two-fold. In the entire patient population, the reductions of the various cardiac dosimetry parameters during DIBH vs. FB while in the WBI only cohort the superiority of the DIBH vs. prone technique were analyzed depending on patient-related factors.
Radiotherapy and dosimetry data
Radiotherapy techniques and facilities together with radiotherapy planning were described in detail previously [1], [2], [3], [4], [5], [6], [7], [8], [9], [10], [11], [12], [13], [25]. Briefly, all irradiation plans were made in the Eclipse 13.6 (Varian Medical Systems, Palo Alto, CA, USA.) planning system using the AAA dose calculation algorithm for a TrueBeam (Varian) linear accelerator. During the planning, tangential 6 MV high-energy photon beams were used, with the help of 6/10/15 MV energy subfields for better dose homogeneity. Target volumes and OARs were contoured and supervised by two experienced radiation oncologists according to international guidelines. If NI was necessary, all patients received axillary, supraclavicular and IMN radiotherapy. The breast/chest wall IMN and supraclavicular regions were covered using 1 isocenter and asymmetric photon field arrangement. At least 95 % of the target volumes had to receive 95 % of the total dose of 50 Gy (25 x 2 Gy) except the IMN; at least 90 % of the IMN volume had to be covered by the 95 % isodose. The institutional dose constraints are included in Table 1.
Table 1.
Institutional OAR dose constraints.
| Dosimetry parameter | Target goal |
|---|---|
| MHD | 3 Gy |
| Heart V25Gy | 3 % |
| LAD mean dose | 10 Gy |
| LV mean dose | 3 Gy |
| LV-V5Gy | 10 % |
| MLD | 8 Gy |
| Lung V20Gy | 15 % |
| Contralateral breast V10Gy | 1 % |
In the planning CT scans under FB, the following anatomical measurements were performed: the volumes of the ipsilateral breast/chest wall (PTV), heart and ipsilateral lung; the Area (A) and Distance (D) were measured on a single CT scan at the middle of the heart [13] (Fig. 1A); the distances between the heart and breast (DHB), ipsilateral lung and breast (DLB); the in-field heart volume (IFHV) and in-field ipsilateral lung volume (IFILV) were measured in the whole series of CT scans according to Lin et al. [26], as illustrated in Fig. 1B. The laterality of the heart (L) was defined as the distance between the centers of the heart and chest (Fig. 1C). The ratio of the volumes of the heart and ipsilateral lung under FB (HV/ILV) and the difference and ratio of the ipsilateral lung volumes under FB and DIBH (ILVFB and ILVDIBH) were also registered [26].
Fig. 1.
Registered anatomical parameters in CT scans under FB. A: Area (A) and Distance (D) as measured on a single CT scan at the middle of the heart: the shortest distance between the anterior surface of the LAD and the chest wall and the area of the heart included in the radiation fields were measured after placing a straight line between the border of the ipsilateral latissimus dorsi muscle and the lateral edge of the sternum [13]. B: The in-field heart volume (IFHV) and in-field ipsilateral lung volume (IFILV) together with the distances between the heart and breast (DHB), ipsilateral lung and breast (DLB), were measured in the whole series of CT scans according to Lin et al. [26]. C: Laterality of heart (L) is the distance between the centers of the heart and chest [26].
The following OAR structures were considered: heart, LV, LAD, LADR, ipsilateral lung, contralateral breast.
The following dosimetry parameters of the heart OARs were extracted from the plans according to the different techniques: MHD, heart V25 Gy, LV mean dose, LV-V5Gy, LV maximum dose, LAD mean dose, LAD maximum dose, LADR mean dose, LADR maximum dose.
Pilot study on pulmonary functions
To complete the basic analysis, in an additional cohort of 12 left-sided BC patients receiving left breast radiotherapy with the DIBH technique pulmonary function measurements were performed in 2023 May-July. The following parameters were collected using a Spirobank II and MIR Spiro 1.1 Gold Edition software (Medical International Research, Rome, Italy): Vital Capacity (VC), Inspiratory Capacity (IC), Expiratory Reserve Volume (ERV).
Statistical analyses
Continuous data were expressed as mean ± SD and range values if appropriate. Predictive performance of various patient-related anatomical and functional parameters for predicting the advantage of the DIBH technique vs. FB was evaluated with Receiver Operating Characteristics (ROC) curve analysis. Area under ROC curve (AUCROC) and 95 % confidence interval for AUCROC were calculated. AUCROC > 0.8 values were regarded as „excellent” and values > 0.9 were regarded as „outstanding”. Dosimetry parameters were compared in the supine DIBH technique versus prone position with paired t-test. Pearson correlation coefficients were calculated between the patient-related features and the DIBH-related reduction of the various dose parameters. Possible multivariate regression models predicting the reduction of the heart dose parameters due to the DIBH manouvre as compared to that under FB were constructed with the forward likelihood ratio model selection method. Estimated parameters and 95 % confidence intervals for the fitted parameters were calculated. Adjusted multiple R2 values were calculated to describe possible predictive power of the multivariate models. Variance inflation factor VIF values were calculated to avoid multicollinearity in the possible multivariate linear regression models.
Respiratory function and lung volume data were compared applying the Pearson correlation analysis.
Statistical software IBM SPSS statistics version 29.0.0.0 was used for statistical analysis. P-values p < 0.05 were regarded as stitistically significant.
Results
Altogether 103 cases having been irradiated in 2018–2019 were included in the present analysis; the mean age was 57.67 ± 11.93 (31.16 – 78.37) years, the mean BMI was 27.64 ± 5.59 (18.81 – 43.82) kg/m2; chemotherapy and endocrine therapy was given to 42 and 67 of them, respectively; other disease-related data have been reported earlier (30).
The DIBH technique provided dramatic reduction of all heart dosimetry parameters compared to that in the FB plans both in the WBI only and WBI/CWI + NI groups, the individual benefit, however, varied (Table 2A). In general, the relative reduction of heart doses was larger in the WBI cohort, but the importance of dose reduction due to the higher dose values was greater in the WBI/CWI + NI subgroup (Table 2A). Among 62 patients receiving WBI, for technical reasons only 45 went through all the supine DIBH, supine FB and prone planning CT scannings. Almost all dosimetry parameters were similar in the supine position using the DIBH technique and prone position but great individual variability was seen (Table 2B).
Table 2.
A: Doses to various heart structures in the entire study population according to the type of radiotherapy (WBI alone vs. nodal radiotherapy) and the technique applied (DIBH vs. FB). B: Doses to various heart structures in the WBI subgroup applying DIBH in the supine position vs. prone positioning.
| A | ||||
|---|---|---|---|---|
| Dosimetry parameter | WBI (mean ± SD, range) (n = 61) |
WBI/CW + Nodal irradiation (mean ± SD, range) (n = 42) |
||
| DIBH | FB | DIBH | FB | |
| MHD (Gy) | 1.79 ± 1.02, 0.69–5.54 | 3.42 ± 1.54, 0.92–8.56 | 3.07 ± 2.11, 1.11–10.51 | 5.09 ± 1.98, 2.17–11.66 |
| Heart V25Gy (%) | 1.28 ± 2.06, 0.00–10.37 | 4.52 ± 3.16, 0.00–14.63 | 3.19 ± 4.33, 0–18.59 | 7.29 ± 4.09, 1.6–21.04 |
| LADmean dose (Gy) | 6.54 ± 5.42, 2.06–24.23 | 14.38 ± 9.04, 2.17–37.43 | 12.26 ± 9.78, 3.37–38.07 | 20.98 ± 8.26, 3.88–40.37 |
| LADmax dose (Gy) | 23.23 ± 15.28, 3.81–50.70 | 40.70 ± 13.43, 5.36–50.76 | 37.06 ± 11.78, 10.43–52.23 | 47.29 ± 5.71, 15.54–51.60 |
| LADRmean dose (Gy) | 7.21 ± 6.03, 2.29–29.12 | 14.77 ± 8.54, 2.41–31.87 | 12.85 ± 10.44, 3.86–39.67 | 22.26 ± 8.32, 4.33–41.40 |
| LADRmax dose (Gy) | 28.98 ± 16.00, 3.78–50.76 | 43.71 ± 10.66, 7.05–51.02 | 39.71 ± 10.04, 11.55–52.37 | 47.88 ± 5.22, 16.42–51.66 |
| LVmean dose (Gy) | 2.39 ± 1.68, 0.88–9.90 | 4.81 ± 2.57, 1.17–13.69 | 3.62 ± 2.75, 1.29–13.78 | 6.57 ± 2.95, 1.62–16.70 |
| LVmax dose (Gy) | 31.75 ± 16.28, 4.97–50.14 | 45.80 ± 8.30, 7.11–51.47 | 37.1 ± 13.64, 6.3–50.84 | 47.27 ± 4.83, 23.24–51.09 |
| LV-V5Gy (%) | 5.47 ± 6.10, 0.00–29.35 | 14.20 ± 8.28, 0.44–39.28 | 9.71 ± 9.41, 0.1–40.29 | 19.68 ± 9.44, 3.14–48.13 |
| B | |||
|---|---|---|---|
| Dosimetry parameter | WBI (mean±SD, range) (n=45) |
p | |
| DIBH | Prone | ||
| MHD (Gy) | 1.71±1.01, 0.69–5.54 | 2.05±1.16, 0.85–6.81 | 0.162 |
| Heart V25Gy (%) | 1.15±2.16, 0–10.37 | 1.38±2.36, 0.00–11.67 | 0.641 |
| LADmean dose (Gy) | 6.58±5.87, 2.06–24.23 | 9.48±7.23, 1.82–25.03 | 0.056 |
| LADmax dose (Gy) | 22.39±15.39, 3.81–50.70 | 30.1±14.87, 3.30–49.69 | 0.017 |
| LADRmean dose (Gy) | 7.58±6.72, 2.29–29.12 | 10.47±8.25, 2.02–32.99 | 0.081 |
| LADRmax dose (Gy) | 28.31±16.17, 3.78–50.76 | 33.48±14.15, 4.11–50.38 | 0.116 |
| LVmean dose (Gy) | 2.37±1.82, 0.95–9.90 | 2.64±1.92, 0–12.21 | 0.529 |
| LVmax dose (Gy) | 29.61±16.43, 4.97–50.17 | 26.91±18.48, 0.00–49.70 | 0.433 |
| LV-V5Gy (%) | 5.05±6.49, 0–29.35 | 5.38±6.71, 0.00–33.45 | 0.827 |
Strong correlations were found between the DIBH-related reductions of the following dosimetry parameters: MHD and V25Gy heart (r = 0.987, p < 0.001), LAD mean dose and LADR mean dose (r = 0.870, p < 0.001), LV-V5Gy and LV mean dose (r = 0.965, p < 0.001), MHD and LV-V5Gy (r = 0.853, p < 0.001), and LV-V5Gy and LADR mean dose (r = 0.801, p < 0.001); no similar strong correlations were found in the case of the MHD and the mean dose of the LAD (r = 0.583, p < 0.001) or LADR (r = 0.726, p < 0.001) and the LV-V5Gy and LAD mean dose (r = 0.666, p < 0.001) (Suppl. Fig. 1A–H).
Prediction of the benefit of DIBH over FB in the whole population
For identifying patients who benefit the most from the DIBH technique first, correlation analysis was performed between the patient-related features and DIBH-related reductions of the various dose parameters; weak correlations were found. The best and consistent predictive parameter was the ratio of ILVFB and ILVDIBH (the following Pearson correlation coefficients were found with that and the MHD r = -0.452, p < 0.001, Heart V25 Gy r = -0.444, p < 0.001, LAD mean dose r = -0.306, p = 0.002, LADR mean dose r = -0.338, p < 0.001, LV mean dose r = -0.451, p < 0.001, and LV-V5Gy r = -0.489, p < 0.001).
Next, we looked for the effect of combining the best predictors into multivariate models. The most promising predictors were selected by the forward likelihood ratio model selection method. Again, the most consistently selected predictor was the ratio of ILVFB and ILVDIBH. Although the coefficient of determination r2 values were improved, the performance of the models still remained inappropriate for routine use (Suppl. Table 1).
DIBH vs. prone positioning in the WBI only subgroup
With the aim of identifying possible predictive parameters for the advantage of one technique over the other, we analyzed the effects of the collected patient-related data on the dosimetry parameters in 2 settings. First we selected those cases which had benefit in heart sparing by one or the other technique using arbitrary classifier thresholds of relevant dose differences. The following values were used: MHD = 1 Gy, heart V25Gy = 1 %, LV mean dose = 1 Gy, LV-V5Gy = 5 %, LAD mean dose = 10 Gy, LADR mean dose = 10 Gy. Second, we identified those cases in which the use of anyone of the two heart-sparing methods did not fulfill the institutional dose limits but the other did. By the clinically relevant arbitrary threshold values approach we identified 9–11 patients according to the selected dosimetry parameter who had advantage of using the DIBH technique instead of prone positioning while another 5–8 patients had advantage of using prone positioning instead of the DIBH technique (Table 3A). When the analysis of the technique preference was based on meeting dose constraints, DIBH was the only solution in 6–13 cases, and prone positioning in 5–6 cases depending on the selected dosimetry parameter (Table 3B). With the two approaches overlapping cases were identified shown later. Note that we ignored maximum doses due to their variable and inconsistent nature.
Table 3.
Comparison of dosimetry parameters in patients for whom prone positioning provided benefit vs. the rest of the subgroup;
| A: case selection was performed by the indicated arbitrary thresholds of dose differences considered relevant for prefering one technique over the other as indicated in parentheses | ||||
|---|---|---|---|---|
| Dosimetry parameter (threshold of dose difference) | DIBH advantageous (mean ± SD, range) |
Prone advantageous (mean ± SD, range) |
||
| DIBH | Prone | DIBH | Prone | |
| MHD (>1 Gy) n | 11 | 5 | ||
| MHD (>1 Gy) | 1.51 ± 0.55, 0.69–2.75 | 3.77 ± 1.12, 2.74–6.81 | 4.12 ± 1.22, 2.96–5.54 | 1.34 ± 0.23, 1.06–1.66 |
| Heart V25Gy (>1 %) n | 11 | 7 | ||
| Heart V25Gy (>1 %) | 0.82 ± 0.88, 0.00–2.94 | 4.80 ± 2.65, 1.72–11.67 | 5.11 ± 3.22, 1.91–10.37 | 0.12 ± 0.15, 0.00–0.37 |
| LADmean dose (>10 Gy) n | 10 | 5 | ||
| LADmean dose (>10 Gy) | 5.14 ± 2.59, 2.06–9.75 | 20.95 ± 3.71, 14.63–25.03 | 21.55 ± 1.99, 18.84–24.23 | 4.00 ± 1.03, 3.45–5.83 |
| LADRmean dose (>10 Gy) n | 9 | 5 | ||
| LADRmean dose (>10 Gy) | 4.45 ± 1.83, 2.29–8.13 | 21.72 ± 5.96, 15.56–32.99 | 23.53 ± 4.39, 19.38–29.12 | 4.36 ± 1.34, 2.94–6.01 |
| LVmean dose (>1 Gy) n | 11 | 6 | ||
| LVmean dose (>1 Gy) | 1.64 ± 0.51, 0.95–2.60 | 4.74 ± 2.80, 2.33–12.21 | 5.89 ± 3.13, 2.35–9.90 | 1.41 ± 0.74, 0.00–2.02 |
| LV-V5Gy (>5 %) n | 10 | 8 | ||
| LV-V5Gy (>5 %) | 2.63 ± 2.54, 0.00–7.07 | 14.42 ± 8.31, 5.44–33.45 | 15.07 ± 9.55, 5.61–29.35 | 0.90 ± 0.91, 0.00–2.49 |
| B: case selection was based on fulfilment or not of the respective institutional dose constraint | ||||
|---|---|---|---|---|
| Dosimetry parameter (institutional OAR limits) | DIBH advantageous (mean±SD, range) |
Prone advantageous (mean±SD, range) |
||
| DIBH | Prone | DIBH | Prone | |
| MHD (3 Gy) n | 10 | 5 | ||
| MHD (3 Gy) | 1.39±0.38, 0.69–1.83 | 3.76±1.18, 2.74–6.81 | 4.12±1.22, 2.96–5.54 | 1.34±0.23, 1.06–1.66 |
| Heart V25Gy (3 %) n | 9 | 5 | ||
| Heart V25Gy (3 %) | 0.98±0.90, 0.00–2.94 | 5.47±2.46, 3.04–11.67 | 6.32±3.02, 2.63–10.37 | 0.07±0.12, 0.00–0.28 |
| LADmean dose (10 Gy) n | 13 | 5 | ||
| LADmean dose (10 Gy) | 5.27±2.42, 2.06–9.75 | 19.03±4.89, 11.38–25.03 | 21.55±1.99, 18.84–24.23 | 4.00±1.03, 3.45–5.83 |
| LADRmean dose (10 Gy) n | 13 | 6 | ||
| LADRmean dose (10 Gy) | 5.05±2.22, 2.29–9.87 | 19.10±6.47, 10.83–32.99 | 21.42±6.48, 10.91–29.12 | 3.97±1.53, 2.02–6.01 |
| LVmean dose (3 Gy) n | 9 | 6 | ||
| LVmean dose (3 Gy) | 1.73±0.50, 0.95–2.60 | 5.24±2.88, 3.31–12.21 | 6.60±2.92, 3.15–9.90 | 1.69±0.28, 1.35–2.02 |
| LV-V5Gy (10 %) n | 6 | 5 | ||
| LV-V5Gy (10 %) | 3.23±2.96, 0.00–7.07 | 18.73±8.17, 12.44–33.45 | 20.43±7.99, 10.38–29.35 | 0.96±0.95, 0.00–2.49 |
Next, ROC analysis was performed for finding out the role of the various patient-related features in the prediction of the benefit of prone positioning over the DIBH technique in decreasing the various heart dose parameters. The outcome is shown in Table 4A. A, D, LBD, HV/ILV, IFILV showed excellent predictive potential on the reduction of the doses of all heart subvolumes or at least one of them due to prone positioning; reduced lung volumes both at FB or DIBH (ILVFB and ILVDIBH) showed outstanding performance (AUC ≥ 0.90) in predicting the advantage of prone positioning (Table 4A). Among the various patient-related parameters a large A and small D, a large LBD favored prone positioning over the use of DIBH (Table 4B). Accordingly a larger HV/LV and IFHV or smaller IFILV favored prone positioning (Table 4B). Notably, the measurement of A and D (considered on a single CT scan) and the estimation of lung capacity are possible prior to the planning CT.
Table 4A.
ROC analyses of various patient-related anatomical and functional parameters for predicting the advantage of prone positioning over the DIBH technique; those potential predictors which resulted in good predictive performance AUC ≥ 0.8 are highlighted in bold while those which among them may be considered without performing a full CT series are highlighted in grey (note that lung volumes during DIBH may be estimated performing spirometry); the predictors with AUC ≥ 0.90 are considered as showing outstanding performance.
| Dosimetry/Predictor | MHD |
Heart V25Gy |
LADmean |
LADmax |
LADRmean |
LADRmax |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| AUC | 95 %CI | p | AUC | 95 %CI | p | AUC | 95 %CI | p | AUC | 95 %CI | p | AUC | 95 %CI | p | AUC | 95 %CI | p | |
| BMI | 0.682 | 0.485–0.879 | 0.189 | 0.625 | 0.445–0.806 | 0.297 | 0.786 | 0.602–0.935 | 0.026 | 0.802 | 0.652–0.953 | 0.008 | 0.715 | 0.536–0.895 | 0.059 | 0.744 | 0.591–0.897 | 0.017 |
| Area | 0.826 | 0.659–0.992 | 0.019 | 0.745 | 0.574–0.917 | 0.042 | 0.896 | 0.772–1.000 | 0.001 | 0.868 | 0.740–0.996 | 0.001 | 0.896 | 0.787–1.000 | 0.001 | 0.886 | 0.758–0.987 | <0.001 |
| Median Distance# | 0.836 | 0.625–1.000 | 0.015 | 0.768 | 0.586–0.950 | 0.026 | 0.890 | 0.734–1.000 | 0.001 | 0.807 | 0.602–1.000 | 0.007 | 0.832 | 0.654–1.000 | 0.004 | 0.763 | 0.589–0.937 | 0.010 |
| PTV | 0.713 | 0.520–0.906 | 0.15 | 0.672 | 0.485–0.859 | 0.153 | 0.799 | 0.640–0.959 | 0.013 | 0.799 | 0.652- 0.945 |
0.009 | 0.701 | 0.497–0.924 | 0.078 | 0.727 | 0.548–0.906 | 0.026 |
| Lung volume FB# | 0.923 | 0.842–1.000 | 0.002 | 0.903 | 0.803–1.000 | 0.0001 | 0.834 | 0.699–0.969 | 0.006 | 0.771 | 0.603–0.939 | 0.018 | 0.750 | 0.557–0.943 | 0.028 | 0.716 | 0.545–0.886 | 0.034 |
| Lung volume DIBH# | 0.974 | 0.930–1.000 | 0.001 | 0.857 | 0.698–1.000 | 0.003 | 0.880 | 0.705–1.000 | 0.002 | 0.819 | 0.626–1.00 | 0.005 | 0.889 | 0.734–1.000 | 0.001 | 0.813 | 0.637–0.988 | 0.002 |
| Lung volumeDIBH-FB# | 0.867 | 0.745–0.988 | 0.008 | 0.691 | 0.465–0.917 | 0.112 | 0.780 | 0.582–0.978 | 0.020 | 0.753 | 0.569–0.938 | 0.026 | 0.823 | 0.643–1.00 | 0.005 | 0.753 | 0.558–0.947 | 0.013 |
| Lung volume DIBH/FB# |
0.477–0.887 | 0.189 | 0.514 | 0.269–0.758 | 0.911 | 0.618 | 0.409–0.827 | 0.328 | 0.628 | 0.437–0.820 | 0.260 | 0.681 | 0.477–0.884 | 0.681 | 0.651 | 0.455–0.847 | 0.140 | |
| Heart volume | 0.636 | 0.455–0.817 | 0.327 | 0.51 | 0.310–0.709 | 0.936 | 0.707 | 0.537–0.876 | 0.086 | 0.726 | 0.570–0.882 | 0.048 | 0.698 | 0.535–0.861 | 0.083 | 0.710 | 0.550–0.871 | 0.039 |
| Heart-Breast distance | 0.280–0.725 | 0.985 | 0.517 | 0.331–0.704 | 0.885 | 0.587 | 0.388–0.786 | 0.470 | 0.615 | 0.427–0.803 | 0.315 | 0.535 | 0.336–0.733 | 0.761 | 0.554 | 0.361–0.747 | 0.597 | |
| Lung-Breast distance | 0.800 | 0.613–0.987 | 0.031 | 0.792 | 0.642–0.941 | 0.015 | 0.849 | 0.703–0.996 | 0.004 | 0.806 | 0.648–0.963 | 0.007 | 0.760 | 0.0554–0.966 | 0.022 | 0.716 | 0.532–0.900 | 0.034 |
| Heart volume /Ipsilateral Lungvolume | 0.877 | 0.769–0.985 | 0.007 | 0.795 | 0.647–0.944 | 0.014 | 0.876 | 0.773–0.980 | 0.002 | 0.847 | 0.732–0.963 | 0.002 | 0.813 | 0.662–0.963 | 0.006 | 0.801 | 0.663–0.939 | 0.003 |
| Laterality of Heart | 0.818 | 0.673–0.963 | 0.022 | 0.743 | 0.565–0.922 | 0.043 | 0.747 | 0.534–0.960 | 0.040 | 0.703 | 0.497–0.909 | 0.075 | 0.714 | 0.513–0.914 | 0.061 | 0.692 | 0.522–0.861 | 0.060 |
| In-field Ipsilateral Lung Volume# | 0.821 | 0.671–0.971 | 0.021 | 0.826 | 0.702–0.951 | 0.007 | 0.792 | 0.639–0.944 | 0.015 | 0.743 | 0.577–0.909 | 0.033 | 0.747 | 0.583–0.910 | 0.031 | 0.713 | 0.547–0.879 | 0.037 |
| In-field Heart Volume | 0.836 | 0.643–1.000 | 0.015 | 0.724 | 0.521–0.926 | 0.063 | 0.826 | 0.663–0.989 | 0.007 | 0.790 | 0.626–0.954 | 0.011 | 0.809 | 0.657–0.961 | 0.007 | 0.766 | 0.616–0.915 | 0.009 |
| Dose/ Predictor | LVmean |
LVmax |
LV-V5Gy |
||||||
|---|---|---|---|---|---|---|---|---|---|
| AUC | 95%CI | p | AUC | 95%CI | p | AUC | 95%CI | p | |
| BMI | 0.731 | 0.508–0.954 | 0.132 | 0.641 | 0.497–0.802 | 0.124 | 0.682 | 0.515–0.850 | 0.083 |
| Area | 0.872 | 0.697–1.000 | 0.015 | 0.781 | 0.624–0.938 | 0.002 | 0.856 | 0.739–0.973 | 0.001 |
| Median Distance# | 0.795 | 0.547–1.000 | 0.054 | 0.710 | 0.554–0.866 | 0.022 | 0.818 | 0.669–0.967 | 0.002 |
| PTV | 0737 | 0.512–0.962 | 0.122 | 0.781 | 0.633–0.930 | 0.002 | 0.659 | 0.459–0.859 | 0.130 |
| Lung volume FB# | 0.885 | 0.785–0.985 | 0.012 | 0.596 | 0.417–0.775 | 0.294 | 0.735 | 0.567–0.904 | 0.025 |
| Lung volume DIBH# | 0.949 | 0.882–1.000 | 0.003 | 0.647 | 0.451–0.844 | 0.107 | 0.779 | 0.589–0.969 | 0.008 |
| Lung volume DIBH-FB# | 0.827 | 0.699–0.955 | 0.033 | 0.594 | 0.397–0.790 | 0.306 | 0.685 | 0.461–0.910 | 0.078 |
| Lung volume DIBH/FB# | 0.603 | 0.412–0.793 | 0.503 | 0.563 | 0.385–0.740 | 0.495 | 0.438 | 0.220–0.656 | 0.556 |
| Heart volume | 0.673 | 0.485–0.861 | 0.477 | 0.618 | 0.448–0.789 | 0.196 | 0.600 | 0.419–0.781 | 0.341 |
| Heart-Breast distance | 0.609 | 0.436–0782 | 0.477 | 0.596 | 0.426–0.765 | 0.294 | 0.532 | 0.347–0.718 | 0.758 |
| Lung-Breast distance | 0.795 | 0.572–1.000 | 0.054 | 0.688 | 0.528–0.847 | 0.040 | 0.732 | 0.545–0.919 | 0.027 |
| Heart volume /Ipsilateral Lung volume | 0.865 | 0.740–0.990 | 0.017 | 0.643 | 0474–0.812 | 0.118 | 0.750 | 0.595–0.905 | 0.017 |
| Laterality of Heart | 0.779 | 0.607–0.950 | 0.069 | 0.661 | 0.491–0.831 | 0.079 | 0.737 | 0.566–0.908 | 0.024 |
| In-field Ipsilateral Lung volume# | 0.769 | 0.913–0.925 | 0.079 | 0.540 | 0.354–0.726 | 0.661 | 0.712 | 0.549–0.875 | 0.044 |
| In-field Heart volume | 0.936 | 0.859–1.000 | 0.004 | 0.700 | 0.539–0.861 | 0.029 | 0.782 | 0.630–0.935 | 0.007 |
Table 4B.
ROC analyses of various patient-related anatomical and functional parameters for predicting the benefit of prone positioning over the DIBH technique by means of reduced MHD, LAD mean dose and LV-V5Gy; the analyses were performed based on both arbitrary classifier thresholds for dose reductions (Table 4A) and meeting dose constraints (Table 1) if prone positioning were used and the DIBH technique would have failed to meet that; the predictors with excellent performance (AUC ≥ 0.80) are indicated in bold; those predictors with AUC ≥ 0.90 are considered as outstanding.
| Predictor | Prone selected by dose reduction based on arbitrary thresholds of MHD, LAD mean dose and LV-V5Gy |
Prone selected by dose reduction based on dose constraints (MHD, LAD mean dose and LV-V5Gy) |
||||
|---|---|---|---|---|---|---|
| AUC | 95 %CI | p | AUC | 95 %CI | p | |
| BMI | 0.690 | 0.497–0.883 | 0.053 | 0.740 | 0.575–0.904 | 0.004 |
| Area | 0.820 | 0.648–0.992 | <0.001 | 0.851 | 0.710–0.993 | <0.001 |
| Heart-Breast distance | 0.535 | 0.317–0,753 | 0.753 | 0.591 | 0.406–0.777 | 0.335 |
| Lung-Breast distance | 0.830 | 0.652–1.008 | <0.001 | 0.882 | 0.759–1.004 | <0.001 |
| Median Distance# | 0.835 | 0.621–1.049 | 0.002 | 0.835 | 0.621–1.049 | 0.002 |
| Lung volume FB# | 0.900 | 0.809–0.991 | <0.001 | 0.900 | 0.809–0.991 | 0.0001 |
| Lung volume DIBH# | 0.965 | 0.910–1.020 | <0.001 | 0.965 | 0.910–1.020 | <0.001 |
| Lung volume DIBH-FB# | 0.870 | 0.751–0.989 | <0.001 | 0.870 | 0.751–0.989 | <0.001 |
| Lung volume DIBH/FB# | 0.690 | 0.489–0.891 | 0.063 | 0.690 | 0.489–0.891 | 0.063 |
| PTV | 0.720 | 0.531–0.909 | 0.022 | 0.747 | 0.570–0.923 | 0.006 |
| Ratio of heart and lung | 0.875 | 0.765–0.985 | <0.001 | 0.821 | 0.684–0.958 | <0.001 |
| Laterality of Heart | 0.798 | 0.651–0.944 | <0.001 | 0.738 | 0.547–0.929 | 0.014 |
| In-field Lung Volume# | 0.815 | 0.660–0.970 | <0.001 | 0.815 | 0.660–0.970 | <0.001 |
| In-field Heart Volume | 0.815 | 0.623–1.007 | 0.001 | 0.750 | 0.570–0.930 | 0.006 |
The predictors which support the preference of prone positioning if their value is smaller are distincted with the # symbol; in other cases a larger value indicates the benefit of prone positioning.
Since we found strong correlations between the changes of the MHD and heart V25Gy, the LAD mean dose and LADR mean dose, and the LV mean dose and LV-V5Gy (Suppl. Fig. 1A–H) for the sake of simplicity, in further analyses we selected one out of each doublet: on the basis of wide acceptance the MHD, LAD mean dose and LV-V5Gy were selected to be evaluated in common.
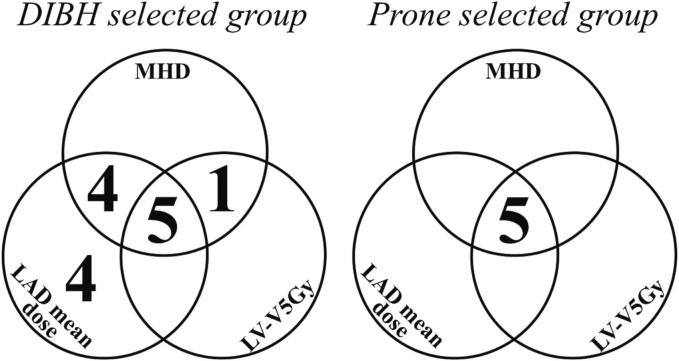
When considering the MHD, LAD mean dose and LV-V5Gy altogether 8 patients had better heart sparing in the prone position than during DIBH by means of at least 1 of the 3 dosimetry parameters based on the arbitrary thresholds of differences (’Prone selected group’). All 3 parameters were reduced in 5 cases while another 3 had a reduced LV-V5Gy difference larger than the arbitrary threshold of 17 % (Fig. 2A). With the DIBH technique 6 patients showed likewise improved dosimetry compared to that in the prone position in all 3 parameters; in another 4 cases 2 dosimetry parameters, while in 4 cases a single parameter was reduced in a similar way (’DIBH selected group’)(Fig. 2A). Next we used the other approach: applying the institutional dose constraints as limits, those cases were selected in which any of the 3 heart dose constraints was not met with one technique but was fulfilled with the other technique, and similar’Prone selected’ and’DIBH selected’ groups were created (Fig. 2B). This selection approach resulted in very consistent results with the former one by identifying similar numbers of patients: in the same 5 cases only prone positioning provided acceptable heart doses as with the first approach, and in the same 14 cases was the DIBH technique the only one that ensured the fulfilment of dose constraints of all dosimetry parameters (n = 5), two or at least one of them (n = 5, and n = 4, respectively) (Fig. 2B).
Fig. 2.
Advantage in heart sparing due to the DIBH technique vs. prone positioning as indicated by one or more of the MHD, LAD mean dose and LV-V5Gy dosimetry parameters; cases belonged to the’Prone selected group’ or’DIBH selected group’ if one or more dose parameters favored the use of the respective technique as described below. A: Improved dosimetry parameters with one or the other technique according to various arbitrary thresholds as described. B: Improved dosimetry parameters with one or the other technique if any of the heart dose constraints with one technique was not met but the other method provided solution.
Then ROC analyses of the various patient-related anatomical and functional parameters for predicting the benefit of prone positioning over the DIBH technique by means of reduced MHD, LAD mean dose and LV-V5Gy were performed based on both arbitrary classifier thresholds for dose reductions and meeting dose constraints if prone positioning were used to replace the DIBH technique that would have failed to meet that (Suppl. Table 1). In both settings the A, LBD, D, the difference of ILVDIBH and ILVFB, HV/LV, IFILV and IFHV were predictors with excellent performance (AUC ≥ 0.80), while ILVFB and ILVDIBH showed outstanding predictive potential with AUC ≥ 0.90.
Pilot study on pulmonary functions
Among the various lung function parameters recorded in a cohort of 12 patients (Table 5A) the strongest correlations were found between VC and ILVDIBH (r = 0.796, p = 0.002), total lung volume during DIBH (r = 0.793, p = 0.002) and the differences between ILVDIBH and ILVFB (r = 0.677, p = 0.022) and total lung volumes during DIBH and FB (r = 0.696, p = 0,012) (Table 5B).
Table 5A.
Patient-related and lung function test parameters in a cohort of 12 breast cancer patients receiving left-sided breast radiotherapy; 3 consecutive vital capacity (VC) measurements and their mean and the lung volumes measured on the planning CTs (supine position, DIBH or FB) are indicated.
| Patient # | BMI (kg/m2) | Smoking status | VC1 (l) | VC2 (l) | VC3 (l) | VCmean (l) | ILVDIBH (cm3) | ILVFB (cm3) | total lung volume DIBH (cm3) | total lung volume FB (cm3) |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 31.20 | Non-smoker | 2.98 | 2.92 | 3.01 | 2.97 | 2692.4 | 1460.3 | 2692.4 | 1460.3 |
| 2 | 22.04 | Non-smoker | 2.70 | 2.52 | 2.54 | 2.59 | 2210.1 | 1270.9 | 2210.1 | 1270.9 |
| 3 | 28.04 | Non-smoker | 2.66 | 2.66 | 2.69 | 2.67 | 2665.5 | 1177.6 | 2665.5 | 1177.6 |
| 4 | 35.56 | Non-smoker | 2.09 | 2.15 | 2.15 | 2.13 | 2202.5 | 1360.9 | 2202.5 | 1360.9 |
| 5 | 21.79 | Non-smoker | 2.56 | 2.74 | 2.68 | 2.66 | 2141.5 | 1327.8 | 2141.5 | 1327.8 |
| 6 | 26.30 | Non-smoker | 1.94 | 1.87 | 1.77 | 1.86 | 1501.8 | 1202.1 | 1501.8 | 1202.1 |
| 7 | 26.73 | Non-smoker | 3.58 | 3.87 | 3.93 | 3.79 | 2787.8 | 1524.9 | 2787.8 | 1524.9 |
| 8 | 33.66 | Non-smoker | 2.54 | 2.52 | 2.39 | 2.48 | 2533.4 | 1561.1 | 2533.4 | 1561.1 |
| 9 | 29.07 | Non-smoker | 3.42 | 3.25 | 3.26 | 3.31 | 2443.2 | 1262.6 | 2443.2 | 1262.6 |
| 10 | 25.78 | Smoker | 2.41 | 2.93 | 2.49 | 2.61 | 2182.1 | 1579.8 | 2182.1 | 1579.8 |
| 11 | 26.56 | Non-smoker | 2.15 | 2.27 | 2.23 | 2.22 | 1992.7 | 1022.0 | 1992.7 | 1022.0 |
| 12 | 28.23 | Non-smoker | 1.63 | 1.75 | 1.72 | 1.70 | 1896.1 | 1210.8 | 1896.1 | 1210.8 |
Table 5B.
Pearson correlation analysis of vital capacity (VC, mean) data and predictors of DIBH benefit such as the lung volumes measured on CT under DIBH or FB and derived indicators in a cohort of 12 breast cancer patients receiving left-sided breast radiotherapy.
| ILVDIBH | total lung volume DIBH | ILVFB | total lung volume FB | ILVDIBH minus FB | ILVDIBH per FB | total lung volume DIBH minus FB | total lung volume DIBH per FB | ||
|---|---|---|---|---|---|---|---|---|---|
| VC | r | 0.796** | 0.793** | 0.451 | 0.560 | 0.677 | 0.462 0.462 |
0.696 | 0.524 |
| 95 % CI | 0.561–0.932 | 0.539–0.918 | −0.005–0.772 | 0.041–0.861 | 0.377–0.888 | 0.068–0.829 | 0.386–0.880 | 0.183–0.830 | |
| p | 0.002 | 0.002 | 0.142 | 0.058 | 0.022 | 0.152 | 0.012 | 0.081 | |
| IC | r | 0.576 | 0.643 | 0.451 | 0.560 | 0.677 | 0.462 0.462 |
0.696 | 0.524 |
| 95 % CI | 0.122–0.882 | 0.223–0.891 | −0.005–0.772 | 0.041–0.861 | 0.377–0.888 | 0.068–0.829 | 0.386–0.880 | 0.183–0.830 | |
| p | 0.064 | 0.033 | 0.142 | 0.058 | 0.022 | 0.152 | 0.012 | 0.081 | |
| ERV | r | 0.796** | 0.793** | 0.451 | 0.560 | 0.677 | 0.462 0.462 |
0.696 | 0.524 |
| 95 % CI | 0.561–0.932 | 0.539–0.918 | −0.005–0.772 | 0.041–0.861 | 0.377–0.888 | 0.068–0.829 | 0.386–0.880 | 0.183–0.830 | |
| p | 0.002 | 0.002 | 0.142 | 0.058 | 0.022 | 0.152 | 0.012 | 0.081 |
Discussion
Our study demonstrated variable utility of the DIBH technique in the reduction of heart doses in left-sided breast radiotherapy. The main outcome of our study is the systematic evaluation of a series of potential predictors and OAR volumes related to heart sparing. Lung volume proved the most important factor in predicting the benefit of the DIBH technique: while a high value of ILVDIBH/ILVFB was the best predictor of heart dose reduction due to DIBH overall, in the WBI subgroup the limited value of the DIBH technique could be detected by a low ILVDIBH or ILVFB and the preference of prone positioning could be further confirmed with a large A and/or small D. Of note all these parameters could be estimated without completing a planning CT; spirometry-testing of VC could assist patient selection.
Based on the dose difference values implied in the study as relevant, 50–90 % of the patients had improved heart sparing during DIBH depending on the dosimetry data. In 9 of the NI cases the IMRT technique had to be used. In the WBI only group the DIBH technique and prone positioning provided similar heart sparing but, in a few cases one over the other provided superior results. Eber et al., in a similar analysis found that although 3DCRT with DIBH benefited most patients, in 2/10 cases alternative solution was needed in order to meet the dose constraints [31].
The heart sparing effect of DIBH in breast radiotherapy is well established, nevertheless, its individual variation is less clearly studied. A closer situation of the heart to the chest wall reflected by the maximum heart distance has been found as associated with larger heart and LAD doses [32], [33]. Cao et al. found a strong relationship between both the heart’s contact with the chest wall and its distance laterally from it and the reduction of the MHD during DIBH [28]. Dell Oro et al. besides maximum heart distance found although weak but significant associations between the total lung volume during FB and dose reductions to the heart and LAD by DIBH [24]. In a large study, among other parameters the lung volume changes related to DIBH were associated with greater MHD improvements [23].
Many authors urge the identification of appropriate predictors for a certain heart sparing technique [20], [21], [22], [23], [24]. Lin et al. introduced 10 anatomical features and developed nine models with different outcomes. Their complex approach distincted heart toxicity-based and OAR-overall toxicity-based classifications [26]. The conclusions were made that the studied models are able to assist selection between the DIBH and prone positioning techniques, and that based on clinical features the individual strategy should be modified. Our ambition was to identify such patient-specific parameters that could be easily implemented in clinical practice for optimizing breast radiotherapy. Hence in a pilot series we correlated spirometry data with lung volumes and found strong correlations. Spirometry as yet was suggested for predicting increased heart and lung doses during breast radiotherapy to select those who need DIBH [34], [35]. Based on the good correlations between the VC and both ILVDIBH and total lung volume during DIBH we rather recommend to evaluate spirometry as a screening method for selecting the efficient heart sparing method.
Thanks to the utilization of the heart-sparing techniques, recommended cardiac dose constraints and dosimetry data are more and more limited [11], [12], [13], [20]. A consensus paper with dose limits to the heart, LAD and LV represents strict conditions for safety [10]. In our study, in most cases these dose constraint were met only if special techniques (DIBH or prone) were applied. We conclude that since heart doses should be minimized, individual consideration of anatomical and functional features is essential for the decision on the radiotherapy technique applied.
Disclosure statement: The authors report there are no competing interests to declare.
CRediT authorship contribution statement
Szilvia Gaál: Methodology, Project administration. Zsuzsanna Kahán: Conceptualization, Methodology, Project administration, Supervision, Writing, review & editing. Ferenc Rárosi: Conceptualization, Data curation, Formal analysis, Validation, Writing, review & editing. Gergely H.Fodor: Methodology. József Tolnai: Methodology. Bence Deák: Data curation. Katalin Hideghéty: Methodology, Supervision. Zoltán Varga: Conceptualization, Data curation, Formal analysis, Methodology, Project administration, Supervision, Validation, Writing, review & editing.
Acknowledgement
The excellent work of the radiographers related to this study at the Department of Oncotherapy is highly appreciated.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ctro.2024.100746.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Darby S.C., Ewertz M., McGale P., Bennet A.M., Blom-Goldman U., Brønnum D., et al. Risk of ischemic heart disease in women after radiotherapy for breast cancer. N Engl J Med. 2013;368:987–998. doi: 10.1056/NEJMoa1209825. [DOI] [PubMed] [Google Scholar]
- 2.Taylor C., Kirby A. Cardiac side-effects from breast cancer radiotherapy. Clin Oncol (r Coll Radiol) 2015;27:621–629. doi: 10.1016/j.clon.2015.06.007. [DOI] [PubMed] [Google Scholar]
- 3.Taylor C., Correa C., Duane F.K., Aznar M.C., Anderson S.J., Bergh J., et al. Early Breast Cancer Trialists’ Collaborative Group. Estimating the Risks of Breast Cancer Radiotherapy: Evidence From Modern Radiation Doses to the Lungs and Heart and From Previous Randomized Trials. J Clin Oncol. 2017;35:1641–1649. doi: 10.1200/JCO.2016.72.0722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Early Breast Cancer Trialists’ Collaborative Group. Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: an overview of the randomised trials. Lancet 2005;366:2087e2106. [DOI] [PubMed]
- 5.Sárközy M., Varga Z., Gáspár R., Szűcs G., Kovács M.G., Kovács Z.Z.A., et al. Pathomechanisms and therapeutic opportunities in radiation-induced heart disease: from bench to bedside. Clin Res Cardiol. 2021;110:507–531. doi: 10.1007/s00392-021-01809-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Taylor C., McGale P., Brønnum D., Correa C., Cutter D., Duane F.K., et al. Cardiac structure injury after radiotherapy for breast cancer: cross-sectional study with individual patient data. J Clin Oncol. 2018;36:2288–2296. doi: 10.1200/JCO.2017.77.6351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Darby S.C., McGale P., Taylor C.W., Peto R. Long-term mortality from heart disease and lung cancer after radiotherapy for early breast cancer: prospective cohort study of about 300,000 women in US SEER cancer registries. Lancet Oncol. 2005;6:557–565. doi: 10.1016/S1470-2045(05)70251-5. [DOI] [PubMed] [Google Scholar]
- 8.Jacobse J.N., Duane F.K., Boekel N.B., Schaapveld M., Hauptmann M., Hooning M.J., et al. Radiation dose-response for risk of myocardial infarction in breast cancer survivors. Int J Radiat Oncol Biol Phys. 2019;103:595–604. doi: 10.1016/j.ijrobp.2018.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.van den Bogaard V.A., Ta B.D., van der Schaaf A., Bouma A.B., Middag A.M., Bantema-Joppe E.J., et al. Validation and modification of prediction model for acute cardiac events in patients wiith breast cancer treated with radiotherapy based on three-dimensional dose distributions to cardiac substructures. J Clin Oncol. 2017;35:1171–1178. doi: 10.1200/JCO.2016.69.8480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Duma M.N., Baumann R., Budach W., Dunst J., Feyer P., Fietkau R., et al. Heart-sparing radiotherapy techniques in breast cancer patients: a recommendation of the breast cancer expert panel of the german society of radiation oncology (DEGRO) Strahlenther Onkol. 2019;195:861–871. doi: 10.1007/s00066-019-01495-w. [DOI] [PubMed] [Google Scholar]
- 11.Varga Z., Hideghéty K., Mező T., Nikolényi A., Thurzó L., Kahán Z. Individual positioning: a comparative study of adjuvant breast radiotherapy in the prone versus supine position. Int J Radiat Oncol Biol Phys. 2009;75:94–100. doi: 10.1016/j.ijrobp.2008.10.045. [DOI] [PubMed] [Google Scholar]
- 12.Varga Z., Cserháti A., Rárosi F., Boda K., Gulyás G., Együd Z., et al. Individualized positioning for maximum heart protection during breast irradiation. Acta Oncol. 2014;53:58–64. doi: 10.3109/0284186X.2013.781674. [DOI] [PubMed] [Google Scholar]
- 13.Kahán Z., Rárosi F., Gaál S., Cserháti A., Boda K., Darázs B., et al. A simple clinical method for predicting the benefit of prone vs. supine positioning in reducing heart exposure during left breast radiotherapy. Radiother Oncol. 2018;126:487–492. doi: 10.1016/j.radonc.2017.12.021. [DOI] [PubMed] [Google Scholar]
- 14.Chen F., Jen Y.M., He K., Yin Z., Shi J. Heart-sparing effect of postmastectomy radiotherapy for breast cancer patients: a dosimetric study of cardiac substructures. Med Dosim. 2020;45:246–251. doi: 10.1016/j.meddos.2020.01.004. [DOI] [PubMed] [Google Scholar]
- 15.Jacob S., Camilleri J., Derreumaux S., Walker V., Lairez O., Lapeyre M., et al. Is mean heart dose a relevant surrogate parameter of left ventricle and coronary arteries exposure during breast cancer radiotherapy: a dosimetric evaluation based on individually-determined radiation dose (BACCARAT study) Radiat Oncol. 2019;14:29. doi: 10.1186/s13014-019-1234-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Naimi Z., Moujahed R., Neji H., Yahyaoui J., Hamdoun A., Bohli M., et al. Cardiac substructures exposure in left-sided breast cancer radiotherapy: is the mean heart dose a reliable predictor of cardiac toxicity? Cancer Radiother. 2021;25:229–236. doi: 10.1016/j.canrad.2020.09.003. [DOI] [PubMed] [Google Scholar]
- 17.Lee J., Hua K.L., Hsu S.M., Lin J.B., Lee C.H., Lu K.W., et al. Development of delineation for the left anterior descending coronary artery region in left breast cancer radiotherapy: an optimized organ at risk. Radiother Oncol. 2017;122:423–430. doi: 10.1016/j.radonc.2016.12.029. [DOI] [PubMed] [Google Scholar]
- 18.Lai J., Hu S., Luo Y., Zheng R., Zhu Q., Chen P., et al. Meta-analysis of deep inspiration breath hold (DIBH) versus free breathing (FB) in postoperative radiotherapy for left-side breast cancer. Breast Cancer. 2020;27:299–307. doi: 10.1007/s12282-019-01023-9. [DOI] [PubMed] [Google Scholar]
- 19.Latty D., Stuart K., Wang W., Ahern V. Review of deep inspiration breath-hold techniques for the treatment of breast cancer. J Med Radiat Sci. 2015;62:74–81. doi: 10.1002/jmrs.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Salvestrini V., Iorio G.C., Borghetti P., De Felice F., Greco C., Nardone V., et al. The impact of modern radiotherapy on long-term cardiac sequelae in breast cancer survivor: a focus on deep inspiration breath-hold (DIBH) technique. J Cancer Res Clin Oncol. 2022;148:409–417. doi: 10.1007/s00432-021-03875-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kirby A.M., Evans P.M., Donovan E.M., Convery H.M., Haviland J.S., Yarnold J.R. Prone versus supine positioning for whole and partial-breast radiotherapy: a comparison of non-target tissue dosimetry. Radiother Oncol. 2010;96:178–184. doi: 10.1016/j.radonc.2010.05.014. [DOI] [PubMed] [Google Scholar]
- 22.Formenti S.C., DeWyngaert J.K., Jozsef G., Goldberg J.D. Prone vs supine positioning for breast cancer radiotherapy. JAMA. 2012;308:861–863. doi: 10.1001/2012.jama.10759. [DOI] [PubMed] [Google Scholar]
- 23.Tanguturi S., Lyatskaya Y., Chen Y., Catalano P., Chen M., Yeo W., et al. Prospective assessment of deep inspiration breath hold using 3-dimensional surface tracking for irradiation of left-sided breast cancer. Int J Radiat Oncol Biol Phys. 2015;5:358–365. doi: 10.1016/j.prro.2015.06.002. [DOI] [PubMed] [Google Scholar]
- 24.Dell’Oro M., Giles E., Sharkey A. A retrospective dosimetric study of radiotherapy patients with left-sided breast cancer; patient selection criteria for deep inspiration breath hold technique. Cancers (basel) 2019;11:259. doi: 10.3390/cancers11020259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gaál S., Kahán Z., Paczona V., Kószó R., Drencsényi R., Szabó J., et al. Deep-inspirational breath-hold (DIBH) technique in left-sided breast cancer: various aspects of clinical utility. Radiat Oncol. 2021;16:89. doi: 10.1186/s13014-021-01816-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lin H., Liu T., Shi C., Petillion S., Kindts I., Weltens C., et al. Feasibility study of individualized optimal positioning selection for left-sided whole breast radiotherapy: DIBH or prone. J Appl Clin Med Phys. 2018;19:218–229. doi: 10.1002/acm2.12283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yamauchi R., Mizuno N., Itazawa T., Saitoh H., Kawamori J. Dosimetric evaluation of deep inspiration breath hold for left-sided breast cancer: analysis of patient-specific parameters related to heart dose reduction. J Radiat Res. 2020;61:447–456. doi: 10.1093/jrr/rraa006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cao N., Kalet A.M., Young L.A., Fang L.C., Kim J.N., Mayr N.A., et al. Predictors of cardiac and lung dose sparing in DIBH for left breast treatment. Phys Med. 2019;67:27–33. doi: 10.1016/j.ejmp.2019.09.240. [DOI] [PubMed] [Google Scholar]
- 29.Wang X., Fargier-Bochaton O., Dipasquale G., Laouiti M., Kountouri M., Gorobets O., et al. Is prone free breathing better than supine deep inspiration breath-hold for left whole-breast radiotherapy? A Dosimetric Analysis Strahlenther Onkol. 2021;197:317–331. doi: 10.1007/s00066-020-01731-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gaasch A., Schönecker S., Simonetto C., Eidemüller M., Pazos M., Reitz D., et al. Heart sparing radiotherapy in breast cancer: the importance of baseline cardiac risks. Radiat Oncol. 2020;15:117. doi: 10.1186/s13014-020-01520-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Eber J., Schmitt M., Dehaynin N., Le Fèvre C., Antoni D., Noël G. Evaluation of cardiac substructures exposure of DIBH-3DCRT, FB-HT, and FB-3DCRT in hypofractionated radiotherapy for left-sided breast cancer after breast-conserving surgery: an in silico planning study. Cancers (basel) 2023;15:3406. doi: 10.3390/cancers15133406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rochet N., Drake J.I., Harrington K., Wolfgang J.A., Napolitano B., Sadek B.T., et al. Deep inspiration breath-hold technique in leftsided breast cancer radiation therapy: evaluating cardiac contact distance as a predictor of cardiac exposure for patient selection. Pract Radiat Oncol. 2015;5:e127–e134. doi: 10.1016/j.prro.2014.08.003. [DOI] [PubMed] [Google Scholar]
- 33.Ferdinand S., Mondal M., Mallik S., Goswami J., Das S., Manir K.S., et al. Dosimetric analysis of deep inspiratory breath-hold technique (DIBH) in left-sided breast cancer radiotherapy and evaluation of pre-treatment predictors of cardiac doses for guiding patient selection for DIBH. Tech Innov Patient Support Radiat Oncol. 2021;17:25–31. doi: 10.1016/j.tipsro.2021.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hjelstuen M.H., Mjaaland I., Vikström J., Madebo T., Dybvik K.I. Pulmonary function tests - an easy selection method for respiratory-gated radiotherapy in patients with left-sided breast cancer. Acta Oncol. 2015;54:1025–1031. doi: 10.3109/0284186X.2014.990107. [DOI] [PubMed] [Google Scholar]
- 35.Koide Y., Shimizu H., Aoyama T., Kitagawa T., Miyauchi R., Watanabe Y., et al. Preoperative spirometry and BMI in deep inspiration breath-hold radiotherapy: the early detection of cardiac and lung dose predictors without radiation exposure. Radiat Oncol. 2022;17:35. doi: 10.1186/s13014-022-02002-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.