INTRODUCTION
Hip fracture risk increases with age, varies by sex, race and ethnicity,1 and is associated with substantial morbidity and mortality among older adults. Persons living with dementia have two- to three-fold greater risk of hip fracture compared to persons without dementia,2 a relationship partially mediated by falls, polypharmacy, and other geriatric syndromes.3 Though racial and ethnic disparities in dementia and hip fracture are established, few studies have examined racial and ethnic variation in dementia prevalence among adults experiencing hip fracture, a highly vulnerable population who may benefit from socially and culturally appropriate patient and caregiver interventions.
METHODS
This cross-sectional study used data from Kaiser Permanente Northern California (KPNC) members aged ≥ 50 years followed until hip fracture hospitalization (2000–2021) identified by International Classification of Diseases (ICD-9/10) diagnosis codes.1 The study was approved by the KPNC Institutional Review Board with waiver of informed consent.
Prevalent dementia, based on ICD-9 (290.0–290.4, 294.1–294.2, 331.0, 331.1x, 331.82) and ICD-10 (F01-F03.xx, G30.0x) diagnosis codes from ambulatory (or virtual care) visits, hospitalization, and institutional care encounters up to five years before and ≤ 90 days after hip fracture hospitalization, was examined by race and ethnicity. Sex-specific age-adjusted modified log-Poisson regression models with dementia diagnosed (a) before hip fracture, (b) before or during hip fracture hospitalization, and (c) before or ≤ 90 days after hip fracture were examined.
RESULTS
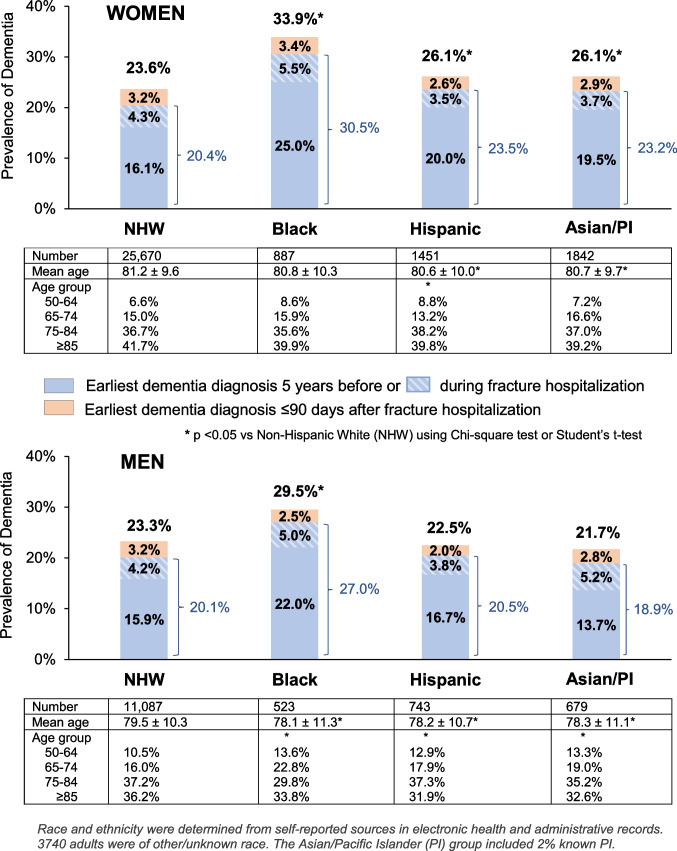
Among 46,622 adults with hip fracture, 69.7% were female and 78.8% were non-Hispanic White (NHW), 3.0% Black, 4.7% Hispanic, 5.4% Asian/Pacific Islander (PI), and 8.0% other/unknown race. Men were slightly younger than women (age 79.4 ± 10.4 vs 81.1 ± 9.7 years, p < 0.001). Hispanic and Asian/PI women and Black, Hispanic, and Asian/PI men were slightly younger than NHW counterparts (Fig. 1).
Figure 1.
Prevalence of dementia among adults with hip fracture by sex, race and ethnicity.
Dementia prevalence was 24.2% overall; 16.8% were diagnosed before hip fracture, 4.2% during hip fracture hospitalization, and 3.2% within ≤ 90-days post-hip fracture hospitalization. Dementia prevalence varied by race and ethnicity (Fig. 1), highest for Black women (33.9%) and men (29.5%) compared to NHW women (23.6%) and men (23.3%). Hispanic and Asian/PI women (26.1%) had higher prevalence than NHW counterparts, but men did not. Similar patterns were seen when excluding dementia diagnoses after hip fracture.
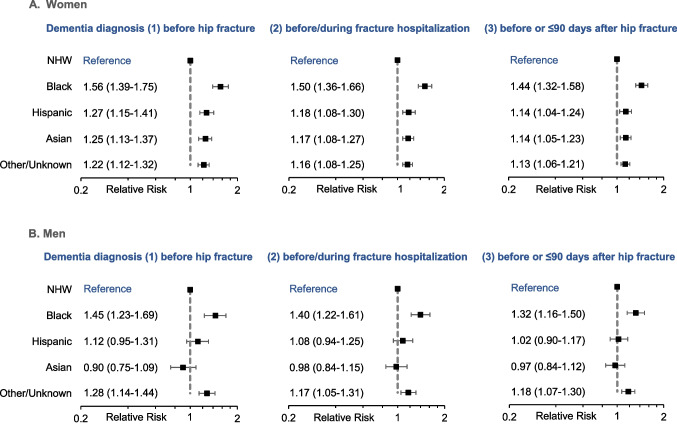
Adjusting for age, prevalence of dementia diagnosed before or ≤ 90-days post-hip fracture was 44% and 32% higher for Black women and men, respectively, compared to NHW counterparts (Fig. 2). Asian/PI and Hispanic women had 14% higher prevalent dementia risk compared to NHW women, whereas risk among men did not differ. These differences were slightly greater when excluding dementia diagnoses occurring after hip fracture.
Figure 2.
Age-adjusted prevalent dementia risk comparing racial and ethnic minority groups to non-Hispanic White (NHW) adults.
DISCUSSION
In a diverse cohort of older adults with hip fracture, at least 1 in 5 had diagnosed dementia (1 in 4 when including new dementia diagnoses ≤ 90 days post-hip fracture). Black, Hispanic, and Asian/PI women and Black men had greater prevalent dementia risk compared to NHW counterparts, whereas Hispanic and Asian/PI men had similar risk.
These findings build on prior work identifying racial and ethnic differences in dementia risk4 by focusing on older adults with catastrophic skeletal injury, most commonly fall-related. The higher dementia prevalence among Asian/PI compared to NHW women with hip fracture contrasts with general population findings of lower dementia burden among Asian adults.4 As in the general population, we observed greater dementia burden among Hispanic and, especially, Black adults.5 One-third of recognized dementia cases were not diagnosed until hip fracture hospitalization or shortly thereafter. Others have observed a large subset of new dementia diagnoses from hospital settings,6 highlighting the importance of dementia screening among patients hospitalized with hip fracture.
While our study is limited by cross-sectional design and potential dementia under-ascertainment due to reliance on clinical diagnoses, it is among the first to examine racial and ethnic variation in dementia among adults with hip fracture. Higher dementia burden among non-White women and Black men emphasizes the increased vulnerability of these relatively small hip fracture populations. Future studies should examine what factors might mediate these relationships.
This study underscores the high prevalence of dementia among older adults with hip fracture, a key opportunity for clinicians to identify and address cognitive decline, particularly among at-risk racial and ethnic minority groups. Efforts to understand the drivers of these demographic differences among adults with hip fracture may inform interventions that optimize skeletal and cognitive health in older populations and promote health equity.
Author Contributions
All authors contributed to study conception and development of study methods; Catherine Lee provided biostatistical input; Malini Chandra abstracted the data and conducted the data analyses; all authors provided input on the interpretation of data; David Lee, Joan Lo, and Paola Gilsanz drafted the manuscript and all authors provided input and edits for important intellectual content and approved the final manuscript for publication.
Funding
This study was funded by a grant from the National Institute on Aging, National Institutes of Health (AG069992). The sponsor had no role in the study concept and design, acquisition of data, analyses, and interpretation of data, and writing of the manuscript. This work, submitted by the authors, also does not represent the official viewpoints of the National Institutes of Health or Kaiser Permanente.
Declarations:
Conflict of Interest:
Joan C Lo, Malini Chandra, and Catherine Lee received funding from the National Institute on Aging related to this work but have no other conflicts of interest to report. David Lee and Paola Gilsanz have no conflicts of interest to report.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Lo JC, Chandra M, Lee DR, et al. Sex- and ethnic-specific patterns in the incidence of hip fracture among older US Asian and non-Hispanic White adults. J Am Geriatr Soc. 2023. 10.1111/jgs.18242. [DOI] [PMC free article] [PubMed]
- 2.Melton LJ, Beard CM, Kokmen E, Atkinson EJ, O'Fallon WM. Fracture risk in patients with Alzheimer's Disease. J Am Geriatr Soc. 1994;42(6):614-619. 10.1111/j.1532-5415.1994.tb06859.x. [DOI] [PubMed]
- 3.Friedman SM, Menzies IB, Bukata SV, Mendelson DA, Kates SL. Dementia and hip fractures: development of a pathogenic framework for understanding and studying risk. Geriatr Orthop Surg Rehabil. 2010;1(2):52-62. 10.1177/2151458510389463. [DOI] [PMC free article] [PubMed]
- 4.Mayeda ER, Glymour MM, Quesenberry CP, Whitmer RA. Inequalities in dementia incidence between six racial and ethnic groups over 14 years. Alzheimers Dement. 2016;12(3):216-224. 10.1016/j.jalz.2015.12.007. [DOI] [PMC free article] [PubMed]
- 5.Rajan KB, Weuve J, Barnes LL, McAninch EA, Wilson RS, Evans DA. Population estimate of people with clinical Alzheimer's disease and mild cognitive impairment in the United States (2020-2060). Alzheimers Dement. 2021;17(12):1966-1975. 10.1002/alz.12362. [DOI] [PMC free article] [PubMed]
- 6.Nguyen HQ, Borson S, Khang P, et al. Dementia diagnosis and utilization patterns in a racially diverse population within an integrated health care delivery system. Alzheimers Dement (N Y). 2022;8(1):e12279. 10.1002/trc2.12279. [DOI] [PMC free article] [PubMed]