Abstract
Stroke may affect physical functioning, cognition, and mental and social aspects of one’s life. Health literacy and self-efficacy are associated with positive health outcomes and are important factors for managing the diverse consequences of a stroke. However, there is very little literature on the association between health literacy and self-efficacy. This study aimed to investigate the association between health literacy and self-efficacy among stroke survivors 1 year after discharge from hospital. Participants in this cross-sectional study were patients diagnosed with a stroke, mainly a mild stroke, who were referred to rehabilitation in primary care after discharge from hospital in Sweden. Data was collected using questionnaires, performance-based tests, and medical records. Ordinal logistic regression was used to analyze the association between general self-efficacy and health literacy in adjusted models. The analysis revealed that higher levels of general self-efficacy and higher levels of performing activities of daily living were associated with higher levels of health literacy. Stroke survivors with higher general self-efficacy also report higher health literacy 1-year post-discharge from hospital. Future studies should focus on the pathways by which health literacy and general self-efficacy work among stroke survivors and in populations with low health literacy, severe stroke or significant cognitive impairments.
Subject terms: Health care, Neurology
Introduction
Stroke is the second leading cause of death worldwide and the third leading cause of death and disability combined1. In Europe, an incidence of 1.12 million cases of stroke was estimated in 2017, and a 30-years projection has predicted an increase in the numbers of stroke events and stroke survivors2. Stroke survivors may experience a range of impairments related to motor or cognitive functions, or a combination of both. It has been observed that physical impairments can be linked to a decline in overall cognition, executive function, and memory3.
There is a cumulative risk of stroke recurrence of 26% during the 5 years following an initial stroke4. Therefore, secondary stroke prevention is necessary for stroke survivors to reduce the risk of recurrence. Secondary stroke prevention comprises surgical and pharmacological interventions, but behavioral changes may also be required, such as smoking cessation, reduction in alcohol consumption, participation in exercise, and dietary changes to reduce lifestyle-related risk5,6. These behavioral changes require substantial knowledge, motivation, and competencies7.
Health literacy is the knowledge, motivation, and competencies that determine a person’s ability to access, understand, appraise, and apply health information in order to promote and maintain good health and make appropriate health decisions8. Health literacy is associated with improved health behavior and health status among patients with cardiovascular disease9. Among stroke survivors, greater health literacy is associated with better function10, and better overall health11. In a previous study, higher levels of health literacy were associated with positive outcomes related to symptoms of depression, walking ability, perceived stroke recovery, and perceived participation12. Furthermore, stroke survivors with inadequate health literacy had poorer retention of health education and recalled only half of the stroke educational material they had received13. This may complicate the undertaking of measures for secondary stroke prevention. Despite the importance of health literacy, there are few studies that specifically target health literacy in stroke survivors.
In addition to health literacy, self-efficacy, i.e., the belief that one can successfully perform a behavior required to produce certain outcomes14, is important for stroke survivors. General self-efficacy can be conceptualized as a global and broad belief in one’s ability to deal effectively with new and stressful situations and can be assessed as a unidimensional and universal construct15, which may be necessary to manage the diverse consequences of a stroke. For example, it has been reported that higher levels of general self-efficacy are associated with lower levels of depression among stroke survivors16, whereas depression and older age are associated with low levels of self-care self-efficacy17. Improved self-efficacy can also have a positive impact on health decisions and contribute to promoting changes in health behavior18. For example, high levels of self-care self-efficacy are associated with increased quality of life and lower levels of depression19, whereas high levels of fall-related self-efficacy are associated with better physical functioning and improved performance of activities of daily living among stroke survivors19.
Hence, both health literacy and self-efficacy are independently associated with health outcomes for stroke survivors. The association between self-efficacy and health literacy has previously been investigated in other populations, but mainly focusing on how health literacy affects self-efficacy20,21. Only one study has investigated this association in stroke survivors, and showed that using a 5-min multidisciplinary intervention to increase health literacy among stroke survivors after discharge from hospital improved patients’ self-efficacy in stroke symptom recognition and knowledge about stroke20. Despite the importance of health literacy and self-efficacy for managing the diverse consequences of a stroke, there is little literature on the association between health literacy and self-efficacy among stroke survivors. Stroke may affect physical functioning, cognition, and the mental and social aspects of one’s life3,22–24, which can affect the management of stroke consequences. As health literacy can be promoted through interventions delivered by health professionals25, and as high self-efficacy is a factor that positively influences stroke recovery, it is relevant to the field to further study the relationship between general self-efficacy and health literacy among stroke survivors26.
Aim
This study aimed to investigate the association between general self-efficacy and health literacy among stroke survivors 1 year after discharge from hospital.
Methods
Study participants
In Stockholm, Sweden, patients who have suffered a stroke are admitted for acute hospital care and rehabilitation at a specialized stroke unit. Participants were patients with a stroke diagnosis who had been referred to neurorehabilitation teams in primary care after discharge from one of two study hospitals and who were included in a longitudinal study with baseline data and follow-ups at 3 and 12 months, carried out between 2016 and 2018. All eligible patients received oral and written information about the study and were included after a signed informed consent form was obtained. Recruitment was carried out by members of the rehabilitation teams working at participating hospitals. Detailed information on selection and recruitment has been described previously27,28. Those eligible to participate in the present study were participants who at 12 months had completed the European Health Literacy Survey Questionnaire and General Self-Efficacy Questionnaire.
The study was approved by the Regional Ethics Committee in Stockholm (registration number 2015/1923-31/2) and is reported according to the STROBE guidelines. All research was performed in accordance with the Declaration of Helsinki.
Data collection
We collected data using questionnaires, performance-based tests, and medical records.
Sociodemographic data was retrieved from medical records and included, age, sex, educational level (elementary, secondary, university/college), working status (yes/no), and cohabiting status (yes/no).
The Modified Rankin Scale (mRS) was used to present the severity of disability 1 year after the stroke. The instrument uses a 6-point scale ranging from 0 to 5, and can be categorized as no symptoms (0), mild disability (1–2), moderate disability (3–4), and severe disability (5)29.
The outcome variable, health literacy, was assessed using the Swedish version of the European Health Literacy Survey Questionnaire (HLS)30.The questionnaire consists of 16 items with five alternatives per item (very easy, easy, difficult, very difficult, and I don’t know), and comprises different dimensions of health literacy: the ability to access, understand, process, and apply health information31. Total scores range from 0 to 16, and are categorized as follows: ≤ 8 = inadequate health literacy, 9–12 = problematic, and ≥ 13 = sufficient31 (Supplementary information).
Independent variables
The General self-efficacy scale (GSES) was used to assess general perceived self-efficacy. This form consists of 10 items and responses are given on a 4-point scale. The total score ranges between 10 and 40, with higher scores indicating greater perceived self-efficacy.
The Barthel Index (BI) was used to assess the need for assistance in performing personal activities of daily living32,33. The questionnaire consists of 10 items about personal care and mobility. The scores range between 0 and 100, with higher scores indicating greater independence33.
The Montreal Cognitive Assessment (MoCA) was used to assess mild cognitive impairment. The MoCA is divided into different domains: attention and concentration, executive function, memory, linguistic ability, visuo-constructive abilities, abstract thinking, numeracy, and orientation. The highest score is 30 and a cutoff of 26 points has been recommended for patients at 1 year after a stroke, where 26 points and above is considered to indicate no cognitive impairment34.
The Fatigue Severity Scale (FSS) was used to assess fatigue after a stroke. This instrument consists of nine statements ranging from 1 to 7 (disagree–agree)35. Higher scores indicate greater fatigue and a mean score of ≥ 4 points is commonly used to classify fatigue after stroke36.
The subscale Depression from the Hospital Anxiety and Depression Scale (HADS-D) was used to assess symptoms of depression. The subscale comprises seven items and the scores range from 0 to 3. The total possible score for this subscale is 21, with higher scores indicating greater levels of depression symptoms. A score of ≥ 4 has been previously suggested as a cutoff for depression symptoms after stroke37.
The Stroke Impact Scale (SIS), domain participation was used to assess the perceived impact of stroke on participation in activities such as work, social activities, recreation, role as a family member or friend, religious or spiritual activities, ability to control one’s own life, and ability to help others38. The score ranges from 0 to 100, with higher scores indicating lower perceived impact.
Statistical analysis
Descriptive statistics were used to describe socio-demographic information, stroke severity, and the variables used in the statistical models.
Ordinal logistic regression was used to identify the association between general self-efficacy and the outcome variable health literacy and carried out according to the following models: Model A (GSES, Age, Sex, BI), Model B (GSES, Age, Sex, BI, Education level), Model C (GSES, Age, Sex, BI, Education level, MoCA), Model D (GSES, Age, Sex, BI, Education level, MoCA, FSS), Model E (GSES, Age, Sex, BI, Education level, MoCA, FSS, HADS-D), and Model F (GSES, Age, Sex, BI, Education level, MoCA, FSS, HADS-D, SIS participation).
The outcome variable, health literacy, was analyzed as a categorical variable (inadequate, problematic, sufficient) in the regression models. The variables GSES and age were analyzed as continuous variables. The other variables were analyzed as dichotomous variables: sex (male/female), education level (elementary and secondary/university or college), BI (0–95, dependent/95–100, independent), MoCA (up to 25/26–30), and SIS participation (0–84/85–100), and FSS (fatigue ≥ 4 points/no fatigue 0–3 points).
The accuracy of the statistically significant predictions was analyzed using receiver-operating-characteristic (ROC) curve analysis and reported as sensitivity, specificity, area under the curve (AUC), and 95% confidence interval. Health literacy was analyzed in these models as two dichotomous variables: inadequate and problematic health literacy versus sufficient health literacy, and inadequate health literacy versus problematic and sufficient health literacy.
Results were considered statistically significant if p < 0.05. All analyses were carried out using IBM SPSS Statistics, version 28.0.1.1.
Results
The participants had a mean age of 72 years (SD = 12) and the majority were male (64%). Most of the participants had at least a high-school education (71%) and reported no or mild disability after the stroke (81%) (Table 1).
Table 1.
Participants’ characteristics 1 year after discharge from hospital.
| Participants’ characteristics (n = 108) | |
|---|---|
| Age at inclusion [mean (SD)] | 72 (12) |
| Sex [n (%)] | |
| Male | 69 (64) |
| Female | 39 (36) |
| Education level [n (%)] | |
| Elementary | 31 (29) |
| Secondary | 25 (23) |
| University/College | 52 (48) |
| Working [n (%)] | 30 (28) |
| Cohabitation with partner [n (%)] | 74 (69) |
| MRS [n (%)]* | |
| No symptoms (0) | 26 (24) |
| Mild disability (1–2) | 61 (57) |
| Moderate disability (3–4) | 20 (19) |
| Severe disability (5) | 0 (0) |
*Missing n = 1.
Health literacy was sufficient among almost two thirds of the sample (62%). General self-efficacy was above 30 points on the 0–40-point scale among 66% of the participants. Other characteristics of participants—such as cognitive impairment, fatigue, depression symptoms, and the perceived impact of stroke on participation in activities—are presented in Table 2.
Table 2.
Descriptive information about the variables used in the statistical models.
| Variable | N (%) and median (IQR) |
|---|---|
| Health literacy scale | |
| Sufficient | 67 (62) |
| Problematic | 31 (29) |
| Inadequate | 10 (9) |
| Median (IQR) | 14 (11–16) |
| General self-efficacy (GSES) | |
| Mean (SD) | 30.5 (6.6) |
| Barthel index | |
| Independent = 100 | 83 (77) |
| Dependent = less than 100 | 25 (23) |
| Median (IQR) | 100 (100–100) |
| Montreal cognitive assessment* | |
| More than 26 | 52 (55) |
| 1–25 | 43 (45) |
| Median (IQR) | 26 (23–28) |
| HADS-depression | |
| 0–3 | 77 (71) |
| At least 4 | 31 (29) |
| Median (IQR) | 2(1–4) |
| Fatigue severity scale** | |
| < 3.99 = no fatigue | 59 (55) |
| ≥ 4 = fatigue | 48 (45) |
| Median (IQR) | 3.2 (2–4.4) |
| SIS participation | |
| 85–100 | 59 (55) |
| 0–84 | 49 (45) |
| Median (IQR) | 88.9 (64–100) |
*Missing n = 12, **Missing n = 1.
General self-efficacy was significantly associated with health literacy in all regression models, regardless of adjustments (Table 3). The only additional variable that remained statistically significant in all regression models was the need for assistance in performing personal activities of daily living assessed using the BI. Higher levels of general self-efficacy and higher levels of independence in performing activities of daily living were associated with greater levels of health literacy.
Table 3.
Ordinal logistic regression models of associations between general self-efficacy and health literacy.
| Independent factors* | Odds ratio | 95% CI | p-value |
|---|---|---|---|
| Model A (n = 108) | |||
| GSES | 1.13 | 1.06–1.20 | < 0.001 |
| Age | 1 | 0.96–1.04 | 0.99 |
| Sex | 0.72 | 0.30–1.75 | 0.47 |
| BI | 6.67 | 2.45–18.19 | < 0.001 |
| Model B (n = 108) | |||
| GSES | 1.14 | 1.06–1.22 | < 0.001 |
| Age | 0.99 | 0.96–1.03 | 0.83 |
| Sex | 0.75 | 0.30–1.83 | 0.52 |
| BI | 6.4 | 2.35–17.39 | < 0.001 |
| Education level | 1.63 | 0.66–4.04 | 0.29 |
| Model C (n = 95) | |||
| GSES | 1.13 | 1.05–1.21 | < 0.001 |
| Age | 1 | 0.96–1.04 | 0.9 |
| Sex | 0.75 | 0.28–2.00 | 0.57 |
| BI | 5.43 | 1.75–16.83 | 0.003 |
| Education level | 1.63 | 0.63–4.24 | 0.31 |
| MoCA | 1.56 | 0.59–4.12 | 0.37 |
| Model D (n = 94) | |||
| Self-efficacy | 1.11 | 1.03–1.19 | 0.01 |
| Age | 1 | 0.97–1.05 | 0.69 |
| Sex | 0.66 | 0.24–1.82 | 0.43 |
| BI | 5.93 | 1.86–18.80 | 0.003 |
| Education level | 1.65 | 0.63–4.32 | 0.3 |
| MoCA | 1.5 | 0.55–4.11 | 0.43 |
| FSS | 0.56 | 0.20–1.63 | 0.29 |
| Model E (n = 94) | |||
| GSES | 1.1 | 1.01–1.19 | 0.02 |
| Age | 1 | 0.97–1.05 | 0.74 |
| Sex | 0.66 | 0.24–1.81 | 0.41 |
| BI | 5.91 | 1.84–18.88 | 0.003 |
| Education level | 1.65 | 0.63–4.32 | 0.31 |
| MoCA | 1.3 | 0.50–3.87 | 0.53 |
| FSS | 0.62 | 0.21–1.85 | 0.39 |
| HADS-D | 0.68 | 0.22–2.07 | 0.5 |
| Model F (n = 94) | |||
| GSES | 1.09 | 1.01–1.19 | 0.03 |
| Age | 1.01 | 0.96–1.05 | 0.77 |
| Sex | 0.61 | 0.21–1.77 | 0.36 |
| BI | 5.14 | 1.45–18.21 | 0.01 |
| Education level | 1.57 | 0.60–4.14 | 0.36 |
| MoCA | 1.34 | 0.48–3.75 | 0.57 |
| FSS | 0.63 | 0.21–1.88 | 0.4 |
| HADS-D | 0.72 | 0.23–2.22 | 0.57 |
| SIS participation | 1.34 | 0.43–4.22 | 0.61 |
*GSES, General Self-Efficacy Scale; BI, Barthel Index; FSS, Fatigue Severity Scale; MoCA, Montreal Cognitive Assessment; HADS-D: Hospital and Anxiety Scale, Depression; SIS participation, Stroke Impact Scale 3.0 (SIS), domain participation.
Significance values are bold.
Accuracy of the predictions
The ROC curve for the predictions based on health literacy (inadequate/problematic vs. sufficient health literacy) is presented in Fig. 1. The area under the curve for general self-efficacy was 0.78 (CI 0.69–0.87), and for the BI it was 0.67 (CI 0.56–0.78). For general self-efficacy, the model had 1.0 sensitivity and 0.95 specificity at a 14.50 cutoff. At an 82.50 cutoff from the BI, the model presented 0.99 sensitivity and 0.88 specificity Fig. 1.
Figure 1.
Specificity and sensitivity based on dichotomous variable health literacy (inadequate/problematic vs. sufficient).
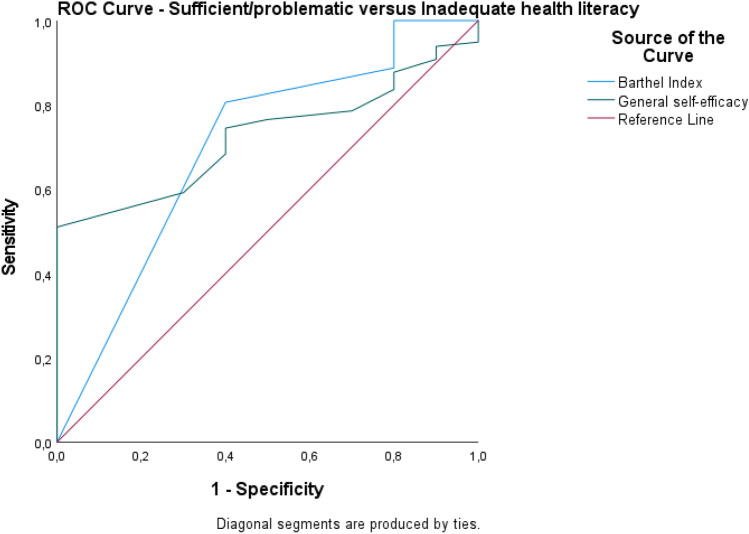
The ROC curve for the predictions based on health literacy (sufficient/problematic vs. inadequate health literacy) is presented in Fig. 2. The area under the curve for general self-efficacy was 0.72 (CI 0.61–0.84), and for the BI it was 0.70 (CI 0.51–0.89). At a cut-off of 14.50 on the General Self-Efficacy Scale, the model presented 0.98 sensitivity and 1.0 specificity. At a cut-off of 70 on the BI, the model presented 1.0 sensitivity and 0.80 specificity.
Figure 2.
Specificity and sensitivity based on dichotomous variable health literacy (sufficient/problematic vs. inadequate).
Discussion
This study investigated the association between general self-efficacy and health literacy among stroke survivors 1 year after discharge from hospital. General self-efficacy was positively associated with health literacy and with performing personal activities.
In this study, higher levels of general self-efficacy were associated with higher levels of health literacy in all statistical models. In other populations, an association between self-efficacy and health literacy has been identified for patients with diabetes39,40, patients with coronary disease41, patients in cardiac rehabilitation42, and older adults with hypertension43. In stroke survivors, a previous study found a positive association between health literacy and self-efficacy in the use and understanding of medication44. Therefore, it can be suggested that there is an interplay between general self-efficacy and health literacy, in which health literacy enables patients to understand and apply health information, whilst self-efficacy facilitates acting in the ways that are necessary to change health behaviors.
In addition, independence in performing personal activities of daily living was associated with higher levels of health literacy. This association has been less thoroughly studied12. It can be suggested that patients with greater health literacy are more liable to engage in behaviors that can enhance the performance of personal activities such as physical exercise45, but this association, as well as the impact of such proactive behaviors on stroke outcomes, needs further exploration.
In this study, the variables sex, age, education level, cognitive impairment, post-stroke fatigue, depression symptoms, and perceived impact on participation did not appear to be associated with health literacy in the adjusted statistical models. In contrast, one previous study found that lower levels of health literacy were associated with lower educational levels, lower income, multimorbidity, and/or moderate to severe functional limitations among patients with chronic diseases46. It is worth noting that social determinants and contextual factors such as healthcare organizations may play a role in health literacy, which may explain differences between the results of the different studies47.
The results of this study are relevant for understanding the interplay between general self-efficacy and health literacy. Previous programs for stroke self-management have found positive results regarding self-efficacy, indicating that our results could be used in future studies to tailor interventions that support both health literacy and general self-efficacy and could have the potential to improve the performance of personal activities48.
The literature addressing factors associated with health literacy among stroke survivors, especially regarding general self-efficacy, is limited. This study provides knowledge that could be used in the future for exploring pathways leading to improved health literacy among stroke survivors. Despite being a cross-sectional study with a small sample, the statistical models were built and analyzed with careful consideration of the relevant factors impacting upon recovery after stroke, based on the previous literature and clinical experience.
One limitation of this study concerns the population making up the sample. Most of the participants had experienced a mild stroke, which makes it difficult to generalize the results to survivors of a severe stroke or those with significant cognitive impairments. Furthermore, most of the sample presented a high level of health literacy and general self-efficacy. Therefore, the results may vary in a population with lower levels of health literacy and/or general self-efficacy 1 year post-discharge after a stroke.
Conclusion
There is an association between health literacy and general self-efficacy, whereby stroke survivors with greater general self-efficacy also report higher levels of health literacy 1 year post-discharge from hospital. These results must be interpreted with caution due to the small sample size. Future studies should focus on the pathways by which health literacy and general self-efficacy work among stroke survivors and in populations with low levels of health literacy.
Supplementary Information
Author contributions
A.H.E.: Conceptualization (supporting), data curation, methodology (supporting), formal analysis, visualization, writing original draft, writing – review and editing; M.F.: Conceptualization (supporting), methodology (supporting), writing – review and editing; S.L.: Data curation, investigation, writing – review and editing; L.V.K.: Methodology (supporting), writing – review and editing; C.Y.: Conceptualization (lead), methodology (lead), project administration, funding acquisition, supervision.
Funding
Open access funding provided by Karolinska Institute. This study was funded by the Doctoral School in Healthcare Sciences, Karolinska Institute [2–134/2016], Neuro Sweden, and the Swedish Stroke Association.
Data availability
The dataset generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-024-57738-z.
References
- 1.Feigin VL, et al. World Stroke Organization (WSO): Global stroke fact sheet 2022. Int. J. Stroke. 2022;17:18–29. doi: 10.1177/17474930211065917. [DOI] [PubMed] [Google Scholar]
- 2.Wafa HA, Wolfe CDA, Emmett E, Roth GA, Johnson CO, Wang Y. Burden of stroke in Europe. Stroke. 2000;51:2418–2427. doi: 10.1161/STROKEAHA.120.029606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Einstad MS, et al. Associations between post-stroke motor and cognitive function: A cross-sectional study. BMC Geriatr. 2021;21:103. doi: 10.1186/s12877-021-02055-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mohan KM, Wolfe CDA, Rudd AG, Heuschmann PU, Kolominsky-Rabas PL, Grieve AP. Risk and cumulative risk of stroke recurrence: A systematic review and meta-analysis. Stroke. 2011;42:1489–1494. doi: 10.1161/STROKEAHA.110.602615. [DOI] [PubMed] [Google Scholar]
- 5.Lawrence M, et al. Stroke secondary prevention, a non-surgical and non-pharmacological consensus definition: Results of a Delphi study. BMC Res. Notes. 2019;12:823. doi: 10.1186/s13104-019-4857-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hall P, von Koch L, Wang X, Lennon O. A scoping review of non-pharmacological, non-surgical secondary prevention strategies in Ischaemic stroke and TIA in national stroke guidelines and clinical audit documents. Healthc Basel Switz. 2022;10:481. doi: 10.3390/healthcare10030481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gladstone DJ, et al. Canadian stroke best practice recommendations: Secondary prevention of stroke update 2020. Can. J. Neurol. Sci. J. Can. Sci. Neurol. 2022;49:315–337. doi: 10.1017/cjn.2021.127. [DOI] [PubMed] [Google Scholar]
- 8.Sørensen K, et al. Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health. 2012;12:80. doi: 10.1186/1471-2458-12-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aaby A, Friis K, Christensen B, Rowlands G, Maindal HT. Health literacy is associated with health behaviour and self-reported health: A large population-based study in individuals with cardiovascular disease. Eur. J. Prev. Cardiol. 2017;24:1880–1888. doi: 10.1177/2047487317729538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Feldman PH, McDonald MV, Eimicke J, Teresi J. Black/Hispanic disparities in a vulnerable post-stroke home care population. J. Racial Ethn. Health Disparities. 2019;6:525–535. doi: 10.1007/s40615-018-00551-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hahn EA, et al. Health and functional literacy in physical rehabilitation patients. Health Lit. Res. Pract. 2017;1:e71–e85. doi: 10.3928/24748307-20170427-02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Flink M, Lindblom S, von Koch L, Carlsson AC, Ytterberg C. Health literacy is associated with less depression symptoms, higher perceived recovery, higher perceived participation, and walking ability one year after stroke: A cross-sectional study. Top Stroke Rehabil. 2023;30:865–871. doi: 10.1080/10749357.2023.2178133. [DOI] [PubMed] [Google Scholar]
- 13.Sanders K, et al. Assessing the impact of health literacy on education retention of stroke patients. Prev. Chron. Dis. 2014;11:E55. doi: 10.5888/pcd11.130259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bandura A. Self-efficacy: Toward a unifying theory of behavioral change. Psychol. Rev. 1977;84:191–215. doi: 10.1037/0033-295X.84.2.191. [DOI] [PubMed] [Google Scholar]
- 15.Scholz U, Doña BG, Sud S, Schwarzer R. Is general self-efficacy a universal construct? Psychometric findings from 25 countries. Eur. J. Psychol. Assess. 2002;18:242–251. doi: 10.1027//1015-5759.18.3.242. [DOI] [Google Scholar]
- 16.Volz M, Voelkle MC, Werheid K. General self-efficacy as a driving factor of post-stroke depression: A longitudinal study. Neuropsychol. Rehabil. 2019;29:1426–1438. doi: 10.1080/09602011.2017.1418392. [DOI] [PubMed] [Google Scholar]
- 17.Brouwer-Goossensen D, van Genugten L, Lingsma HF, Dippel DWJ, Koudstaal PJ, den Hertog HM. Self-efficacy for health-related behaviour change in patients with TIA or minor ischemic stroke. Psychol. Health. 2018;33:1490–1501. doi: 10.1080/08870446.2018.1508686. [DOI] [PubMed] [Google Scholar]
- 18.Sheeran P, et al. The impact of changing attitudes, norms, and self-efficacy on health-related intentions and behavior: A meta-analysis. Health Psychol. Off. J. Div. Health Psychol. Am. Psychol. Assoc. 2016;35:1178–1188. doi: 10.1037/hea0000387. [DOI] [PubMed] [Google Scholar]
- 19.Jones F, Riazi A. Self-efficacy and self-management after stroke: A systematic review. Disabil. Rehabil. 2011;33:797–810. doi: 10.3109/09638288.2010.511415. [DOI] [PubMed] [Google Scholar]
- 20.Denny MC, Vahidy F, Vu KYT, Sharrief AZ, Savitz SI. Video-based educational intervention associated with improved stroke literacy, self-efficacy, and patient satisfaction. PLoS ONE. 2017;12:e0171952. doi: 10.1371/journal.pone.0171952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Espernberger KR, Fini NA, Peiris CL. Personal and social factors that influence physical activity levels in community-dwelling stroke survivors: A systematic review of qualitative literature. Clin. Rehabil. 2021;35:1044–1055. doi: 10.1177/0269215521993690. [DOI] [PubMed] [Google Scholar]
- 22.Acciarresi M, Bogousslavsky J, Paciaroni M. Post-stroke fatigue: Epidemiology, clinical characteristics and treatment. Eur. Neurol. 2014;72:255–261. doi: 10.1159/000363763. [DOI] [PubMed] [Google Scholar]
- 23.Kalaria RN, Akinyemi R, Ihara M. Stroke injury, cognitive impairment and vascular dementia. Biochim. Biophys. Acta. 2016;1862:915–925. doi: 10.1016/j.bbadis.2016.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Medeiros GC, Roy D, Kontos N, Beach SR. Post-stroke depression: A 2020 updated review. Gen. Hosp. Psychiatry. 2020;66:70–80. doi: 10.1016/j.genhosppsych.2020.06.011. [DOI] [PubMed] [Google Scholar]
- 25.Farley H. Promoting self-efficacy in patients with chronic disease beyond traditional education: A literature review. Nurs. Open. 2020;7:30–41. doi: 10.1002/nop2.382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nott M, Wiseman L, Seymour T, Pike S, Cuming T, Wall G. Stroke self-management and the role of self-efficacy. Disabil. Rehabil. 2021;43:1410–1419. doi: 10.1080/09638288.2019.1666431. [DOI] [PubMed] [Google Scholar]
- 27.Lindblom S, Tistad M, Flink M, Laska AC, von Koch L, Ytterberg C. Referral-based transition to subsequent rehabilitation at home after stroke: One-year outcomes and use of healthcare services. BMC Health Serv. Res. 2022;22:594. doi: 10.1186/s12913-022-08000-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lindblom S, Flink M, Sjöstrand C, Laska AC, von Koch L, Ytterberg C. Perceived quality of care transitions between hospital and the home in people with stroke. J. Am. Med. Dir. Assoc. 2020;21:1885–1892. doi: 10.1016/j.jamda.2020.06.042. [DOI] [PubMed] [Google Scholar]
- 29.van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJ, van Gijn J. Interobserver agreement for the assessment of handicap in stroke patients. Stroke. 1988;19:604–607. doi: 10.1161/01.STR.19.5.604. [DOI] [PubMed] [Google Scholar]
- 30.Bergman L, Nilsson U, Dahlberg K, Jaensson M, Wångdahl J. Validity and reliability of the Swedish versions of the HLS-EU-Q16 and HLS-EU-Q6 questionnaires. BMC Public Health. 2023;23:724. doi: 10.1186/s12889-023-15519-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wångdahl J, Lytsy P, Mårtensson L, Westerling R. Health literacy among refugees in Sweden: A cross-sectional study. BMC Public Health. 2014;14:1030. doi: 10.1186/1471-2458-14-1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Duffy L, Gajree S, Langhorne P, Stott DJ, Quinn TJ. Reliability (inter-rater agreement) of the Barthel Index for assessment of stroke survivors: Systematic review and meta-analysis. Stroke. 2013;44:462–468. doi: 10.1161/STROKEAHA.112.678615. [DOI] [PubMed] [Google Scholar]
- 33.Mahoney FI, Barthel DW. Functional evaluation: the Barthel Index. Md. State Med. J. 1965;14:61–65. [PubMed] [Google Scholar]
- 34.Shi D, Chen X, Li Z. Diagnostic test accuracy of the Montreal Cognitive Assessment in the detection of post-stroke cognitive impairment under different stages and cutoffs: A systematic review and meta-analysis. Neurol. Sci. Off. J. Ital. Neurol. Soc. Ital. Soc. Clin. Neurophysiol. 2018;39:705–716. doi: 10.1007/s10072-018-3254-0. [DOI] [PubMed] [Google Scholar]
- 35.Krupp LB, LaRocca NG, Muir-Nash J, Steinberg AD. The fatigue severity scale: application to patients with multiple sclerosis and systemic lupus erythematosus. Arch. Neurol. 1989;46:1121–1123. doi: 10.1001/archneur.1989.00520460115022. [DOI] [PubMed] [Google Scholar]
- 36.Cumming TB, Packer M, Kramer SF, English C. The prevalence of fatigue after stroke: A systematic review and meta-analysis. Int. J. Stroke Off. J. Int. Stroke Soc. 2016;11:968–977. doi: 10.1177/1747493016669861. [DOI] [PubMed] [Google Scholar]
- 37.Sagen U, Vik TG, Moum T, Mørland T, Finset A, Dammen T. Screening for anxiety and depression after stroke: Comparison of the hospital anxiety and depression scale and the Montgomery and Asberg depression rating scale. J. Psychosom. Res. 2009;67:325–332. doi: 10.1016/j.jpsychores.2009.03.007. [DOI] [PubMed] [Google Scholar]
- 38.Duncan PW, Wallace D, Lai SM, Johnson D, Embretson S, Laster LJ. The stroke impact scale version 2.0.: Evaluation of reliability, validity, and sensitivity to change. Stroke. 1999;30:2131–2140. doi: 10.1161/01.STR.30.10.2131. [DOI] [PubMed] [Google Scholar]
- 39.Bohanny W, Wu SFV, Liu CY, Yeh SH, Tsay SL, Wang TJ. Health literacy, self-efficacy, and self-care behaviors in patients with type 2 diabetes mellitus. J. Am. Assoc. Nurse Pract. 2013;25:495–502. doi: 10.1111/1745-7599.12017. [DOI] [PubMed] [Google Scholar]
- 40.Lee YJ, Shin SJ, Wang RH, Lin KD, Lee YL, Wang YH. Pathways of empowerment perceptions, health literacy, self-efficacy, and self-care behaviors to glycemic control in patients with type 2 diabetes mellitus. Patient Educ. Couns. 2016;99:287–294. doi: 10.1016/j.pec.2015.08.021. [DOI] [PubMed] [Google Scholar]
- 41.Du S, Feng Z, Wang W, Tian L, Wang Y. A structural equation model linking health literacy, self efficacy and quality of life in adults with coronary heart disease. BMC Cardiovasc. Disord. 2022;22:285. doi: 10.1186/s12872-022-02720-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Walters R, Leslie SJ, Sixsmith J, Gorely T. Health literacy for cardiac rehabilitation: An examination of associated illness perceptions, self-efficacy, motivation and physical activity. Int. J. Environ. Res. Public Health. 2020;17:8641. doi: 10.3390/ijerph17228641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Darvishpour A, Mansour-Ghanaei R, Mansouri F. The relationship between health literacy, self-efficacy, and self-care behaviors in older adults with hypertension in the north of Iran. Health Lit. Res. Pract. 2022;6:e262–e269. doi: 10.3928/24748307-20221013-01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Appalasamy JR, Joseph JP, Ramaiah SS, Quek KF, Anuar Zaini M, Zain K. Exploring stroke survivors’ self-efficacy in understanding and taking medication and determining associated factors: A cross-sectional study in a neurology clinic in Malaysia. Patient Prefer Adher. 2019;13:1463–1475. doi: 10.2147/PPA.S215271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Saunders DH, et al. Physical fitness training for stroke patients. Cochrane Database Syst. Rev. 2020;3:CD003316. doi: 10.1002/14651858.CD003316.pub7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Heijmans M, Waverijn G, Rademakers J, van der Vaart R, Rijken M. Functional, communicative and critical health literacy of chronic disease patients and their importance for self-management. Patient Educ. Couns. 2015;98:41–48. doi: 10.1016/j.pec.2014.10.006. [DOI] [PubMed] [Google Scholar]
- 47.Nutbeam D, Lloyd JE. Understanding and responding to health literacy as a social determinant of health. Annu. Rev. Public Health. 2021;42:159–173. doi: 10.1146/annurev-publhealth-090419-102529. [DOI] [PubMed] [Google Scholar]
- 48.Lo SHS, Chang AM, Chau JPC. Stroke self-management support improves survivors’ self-efficacy and outcome expectation of self-management behaviors. Stroke. 2018;49:758–760. doi: 10.1161/STROKEAHA.117.019437. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The dataset generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.