Abstract
Background
The purpose of this study was to evaluate the clinical and radiological outcomes of high-flexion total knee arthroplasty (TKA) using Vega Knee System (B. Braun, Aesculap) at a long-term follow-up and to analyze the implant survivorship.
Methods
We enrolled 165 patients (232 knees) with a minimum 7-year follow-up after TKA (VEGA Knee System). For clinical assessment, range of motion (ROM), Knee Injury and Osteoarthritis Outcome Score (KOOS), and Western Ontario and McMaster University Osteoarthritis Index (WOMAC) were used. For radiologic assessment, hip-knee-ankle angle, component position, and the existence of radiolucent lines and loosening were used. Survival analysis was conducted using the Kaplan-Meier method.
Results
The mean follow-up period was 9.8 years. The mean ROM increased from 124.4° to 131.4° at the final follow-up. The WOMAC score decreased from 38.5 to 17.4 at the final follow-up (p < 0.001). All 5 subscales of the KOOS improved at the final follow-up (all subscales, p < 0.001). Revision TKA was performed in 10 cases (4.3%), which included 9 cases of aseptic loosing and 1 case of periprostatic joint infection. Of the 9 aseptic loosening cases (3.9%), 8 cases (3.4%) were loosening of the femoral component and 1 case (0.4%) was loosening of the tibial component. When revision for any reason was considered an endpoint, the 10-year survivorship was 96.2% (95% confidence interval [CI], 93.9%–98.5%). On the other hand, when revision for aseptic loosening was considered the endpoint, the 10-year survivorship was 96.6% (95% CI, 94.4%–98.8%).
Conclusions
The Vega Knee System provided good clinical results in the long-term follow-up period. Although the VEGA Knee System showed acceptable implant survivorship, loosening of the femoral component occurred in about 3.4% of the patients. For more accurate evaluation of the survivorship of high-flexion design TKA with a short posterior flange, it is necessary to conduct more long-term follow-up studies targeting diverse races, especially Asians who frequently perform high-flexion activities.
Keywords: Total knee arthroplasty, High-flexion, Treatment outcome, Survivorship, Prosthesis failure
Factors affecting patient satisfaction after total knee arthroplasty (TKA) are diverse. The most reported predictors of satisfaction were higher overall postoperative function including increased range of motion (ROM).1,2) In particular, high flexion of the knee joint is required in the Asian population due to cultural and religious reasons.1) Several types of high-flexion designs of TKA have been introduced to increase ROM. Such design modifications include changes in the thickness of the femoral component’s posterior condyles, changes in the shape of the posterior lip of the polyethylene insert, and/or the post-cam mechanism in TKAs.3,4) Though there are controversies, these high-flexion prostheses compared with conventional TKA designs showed better ROM and more functional improvement.5,6) However, certain kinds of high-flexion prostheses showed higher rates of early aseptic loosening of the femoral component.7,8) A biomechanical study showed that high-flexion designs have an increased risk for loosening of the femoral component than conventional TKA designs because of the absence of femoral load sharing between the prosthesis component and the condylar bone during high flexion.3)
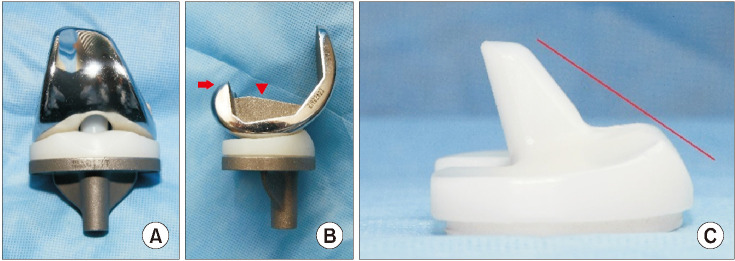
VEGA Knee System (B. Braun, Aesculap) has been developed to meet the needs of high-flexion TKA and the prosthesis has shorter posterior condyles with a small radius for high flexion (Fig. 1). Despite concerns about the risk of early aseptic loosening of the femoral component in high-flexion TKAs, studies using VEGA Knee System have reported good clinical outcomes and no evidence of aseptic loosening of the femoral component.9,10) However, these results might be because of the short-term follow-up after TKAs. Therefore, a long-term follow-up after TKA using VEGA Knee System will make it clearer whether the clinical outcomes of this design continue to be maintained and whether early aseptic loosening of femoral components does not occur.
Fig. 1. VEGA Knee System. (A) Frontal view. The anterior flange of the femoral component has a narrow mediolateral width. It prevents a soft-tissue impingement with an extensor mechanism. (B) Lateral view. The posterior condyle has a short proximal-distal dimension (arrow) for increasing knee flexion. It has a low-profile box and no pegs (arrowhead). (C) Polyethylene insert. The anterior part of the polyethylene insert has a 55° inclination to the base of the tibial baseplate (solid line). It avoids a conflict with the extensor mechanism.
The purpose of this study was to evaluate the clinical and radiological outcomes of high-flexion TKA using Vega Knee System (B. Braun, Aesculap) at a long-term follow-up and to analyze the implant survivorship. We hypothesized that the long-term clinical outcomes would be satisfactory, but the loosening rate would be high.
METHODS
This study was performed retrospectively after obtaining Institutional Review Board approval of Haeundae Bumin Hospital (No. 2017-CTDV-001). The requirement for informed consent was waived because of the retrospective nature of this study.
Patients
In 192 patients, 263 primary TKAs were undertaken using VEGA Knee System between March 2011 and February 2015. Patients who underwent TKA for primary osteoarthritis and were followed up for at least 7 years were included in this study. The exclusion criteria were patients who underwent TKA for inflammatory arthritis, post-traumatic osteoarthritis, or osteonecrosis and patients who were followed up for less than 7 years after TKA. Thirty-one TKAs in 27 patients were lost to follow-up because they refused to visit the clinic with well-functioning TKAs (12 cases), were unable to contact (phone or mail; 10 cases), and had death unrelated to TKAs (5 cases). Finally, 165 patients (232 TKAs) were enrolled in this study. The demographic data are summarized in Table 1.
Table 1. Patient Demographic Characteristics.
| Parameter | Value |
|---|---|
| Sex (male : female) | 22 : 210 |
| Age (yr) | 67 (46–85) |
| Height (cm) | 156 (140–174) |
| Weight (kg) | 62 (32–91) |
| Body mass index (kg/m2) | 25.2 (14.6–34.6) |
| Involved knee (right : left) | 110 : 122 |
Values are presented as number or mean (range).
Surgical Procedures
The surgical procedure was performed under the manufacturer’s instructions. The author’s procedure will be briefly described below. All operations were performed by a single surgeon (SSS) using the same technique. An anterior midline skin incision about 12 cm to 14 cm in length was made and followed by a medial parapatellar arthrotomy. A medial soft-tissue release was performed according to the degree of preoperative varus deformity. Resection of the distal femur was performed using an intramedullary (IM) guide with a predetermined valgus angle (usually 5–7 valgus angle from the femoral IM rod). Using an extramedullary tibial guide, the proximal tibial bone was resected perpendicular to the shaft of the tibia in the coronal plane, with a 0° to 3° posterior slope in the sagittal plane. After resection of the proximal tibia, femoral component size and rotation were determined. Anteroposterior (AP) cutting was performed using an anterior referencing system. The femoral component was placed in 3° to 5° of external rotation to the posterior condyles. All the components were cemented with Simplex P (Stryker) after drying and manual pressurization of the cement. The tibial component was fully cemented using the cement in a doughy state, and it was manually pressurized into the proximal tibia. For femoral fixation, cement was used to cover the entire femoral bone surface and the inner surface of the femoral prosthesis including the posterior condyle before it was impacted onto the prepared femur.
Clinical Assessment
The patients were reviewed at 6 weeks, 3 months, 6 months, and 1 year after surgery and annually thereafter. For clinical assessment, the Knee Injury and Osteoarthritis Outcome Score (KOOS),11) Western Ontario and McMaster University Osteoarthritis Index (WOMAC),12) ROM, and complications were used. All the data at follow-up examinations were recorded by the operating surgeon (SSS) and compiled by an independent observer (CRL), who was not part of the surgical team and had no knowledge of the radiological findings.
Maximum flexion was measured before surgery and at follow-up using a manual goniometer with the arms aligned along the long axes of the femur and tibia on the lateral side of the knee joint. Patients were told to bend until they felt the slightest pain. Flexion contracture was measured and reported similarly. ROM was calculated by subtracting the flexion contracture from the maximum flexion.
Radiological Assessment
Pre- and postoperative radiographs included standing knee AP, lateral, patellar axial, and standing full-length AP films. These were assessed for the alignment of the lower extremity, component positioning, and the presence and location of radiolucent lines (RLLs) at the bone-cement interface. The alignment of the lower extremity was evaluated by the hip-knee-ankle angle. The varus alignment was expressed as a negative number and the valgus alignment as a positive number.
The evaluation of the component position and RLLs was based on the Knee Society roentgenographic evaluation system.13) The component position was evaluated by measuring the valgus angle of the femoral component (α), varus angle of the tibial component (β), flexion angle of the femoral component (γ), and posterior slope of the tibial component (δ). The width of the RLLs was measured on the basis of 7 zones on the lateral radiograph of the femur, 7 on an AP radiograph of the tibia, and 3 on a lateral radiograph of the tibia. Loosening was defined as a condition with a progressive RLL of more than 2 mm in width or a change in the component position.8) All the radiographs were analyzed by 1 author (KJS) with no knowledge of the patient’s name, and the findings were recorded by a research assistant who again did not know the identity of the patient. Intra- or inter-observer analysis of the radiological findings was not performed.
Statistical Analysis
For statistical analysis, SPSS ver. 12 (SPSS Inc.) and R software version 4.1.2 (R Foundation for Statistical Computing) were used. The paired t-test was used to compare the preoperative ROM and patient-reported outcomes with the final values. For survival analysis, the Kaplan-Meier survivorship analysis curve was used. The endpoints were defined as revision for any reason and revision for prosthesis-related reasons only. The level of statistically significant difference was set at p < 0.05.
RESULTS
The mean follow-up period was 9.8 years (range, 7–11 years). Table 2 shows ROM and patient-reported outcomes. The mean ROM increased from 124.4° to 131.4° at the final follow-up (p < 0.001). Flexion contracture also improved from 7.4° to 0° at the final follow-up. The WOMAC score decreased from 38.5 to 17.4 at the final follow-up (p < 0.001). All 5 subscales of the KOOS score (pain, symptoms, activities of daily living, sport and recreation function, and quality of life) improved at the final follow-up (all subscales, p < 0.001). There was no statistically significant change in the alignment of the implant measured as the coronal and sagittal alignments of femoral and tibial components at the last follow-up compared to the immediate postoperative values (all parameters, p > 0.05) (Table 3).
Table 2. Changes in Clinical Results between the Preoperative and Last Follow-up Assessments.
| Parameter | Preoperative | Postoperative | Difference | p-value |
|---|---|---|---|---|
| Range of motion (°) | 124.4 ± 10.6 | 131.4 ± 10.1 | 7.0 | < 0.001 |
| KOOS pain | 58.4 ± 19.4 | 86.1 ± 11.5 | 27.6 | < 0.001 |
| KOOS symptom | 62.5 ± 20.7 | 83.3 ± 14.3 | 20.7 | < 0.001 |
| KOOS ADL | 59.3 ± 19.7 | 79.9 ± 15.2 | 20.6 | < 0.001 |
| KOOS sports/rec | 23.9 ± 18.4 | 39.8 ± 22.9 | 15.9 | < 0.001 |
| KOOS QOL | 29.6 ± 15.8 | 60.6 ± 22.7 | 31.0 | < 0.001 |
| WOMAC score | 38.5 ± 17.9 | 17.4 ± 13.1 | –21.1 | < 0.001 |
Values are presented as mean ± standard deviation.
KOOS: Knee Injury and Osteoarthritis Outcome Score, ADL: activities of daily living, Sports/rec: sport and recreation function, QOL: quality of life, WOMAC: Western Ontario and McMaster University Osteoarthritis Index.
Table 3. Radiologic Outcomes.
| Angle measurement | Immediate postoperative | Last follow-up | Mean angle difference | p-value |
|---|---|---|---|---|
| HKA angle (°) | –0.9 ± 2.7 | –1.1 ± 2.8 | –0.14 | 0.24 |
| α Angle (°) | 95.5 ± 2.3 | 95.4 ± 2.6 | –0.12 | 0.92 |
| β Angle (°) | 90.0 ± 1.8 | 89.8 ± 1.6 | –0.12 | 0.35 |
| γ Angle (°) | 25.2 ± 3.3 | 25.4 ± 3.5 | –0.11 | 0.37 |
| δ Angle (°) | 88.8 ± 2.2 | 88.7 ± 2.1 | –0.10 | 0.48 |
Values are presented as mean ± standard deviation.
HKA: hip-knee-ankle.
In 33 cases (14.2%), non-progressive RLLs around the femoral component with a width of less than 2 mm were observed. An RLL was identified in zone 1 in 9 cases, zone 4 in 15 cases, and zones 1 and 4 in 10 cases. There were no cases with non-progressive RLLs around the tibial component. Aseptic loosening occurred in 9 cases (3.8%), of which 8 cases (3.4%) occurred in the femoral component and 1 case (0.4%) occurred in the tibial component (Table 4, Fig. 2). In 1 case, 2-stage revision TKA was performed for periprosthetic joint infection. There were no other complications. When revision for any reason was considered as the endpoint, the 10-year survivorship was 96.2% (95% confidence interval, 93.9%–98.5%). On the other hand, when revision for aseptic loosening was considered as the endpoint, the 10-year survivorship was 96.6% (95% confidence interval, 94.4%–98.8%) (Fig. 3).
Table 4. Details of Patients Who Underwent Revision Total Knee Arthroplasty.
| Case No. | Sex | Age at index surgery | Side | BMI (kg/m2) | BMD (femur neck) | Cause of revision surgery | Time to revision (yr) |
|---|---|---|---|---|---|---|---|
| 1 | Female | 74 | Left | 21.0 | –1.8 | Periprosthetic joint infection | 1.9 |
| 2 | Female | 60 | Left | 25.2 | 0.4 | Femoral component loosening | 5.9 |
| 3 | Female | 65 | Right | 23.0 | –2.3 | Femoral component loosening | 6.1 |
| 4 | Female | 65 | Left | 23.0 | –2.3 | Tibial component loosening | 6.1 |
| 5 | Male | 61 | Right | 23.5 | –0.5 | Femoral component loosening | 6.8 |
| 6 | Female | 68 | Left | 25.4 | 0.6 | Femoral component loosening | 7.4 |
| 7 | Female | 64 | Left | 27.5 | –2.0 | Femoral component loosening | 7.8 |
| 8 | Female | 69 | Left | 24.8 | –1.8 | Femoral component loosening | 8.9 |
| 9 | Female | 56 | Right | 25.2 | NA | Femoral component loosening | 9.7 |
| 10 | Female | 54 | Right | 27.9 | 0.3 | Femoral component loosening | 9.8 |
BMI: body mass index, BMD: bone mineral density, NA: not available.
Fig. 2. Sequential lateral radiographs of the left knee after total knee arthroplasty and intraoperative findings in revision surgery. Progressive radiolucent lines and positional changes of the femoral component were observed in the lateral knee radiographs, which were obtained at 1 year (A), 8 years (B), and 9 years (C) after surgery. Intraoperative photo (D) taken at the time of revision surgery showing debonding of the cement.
Fig. 3. Kaplan-Meier survivorship curves for VEGA Knee System.

DISCUSSION
In this study, the VEGA Knee System showed excellent results in ROM and patient-reported outcomes. Although satisfactory implant survivorship of more than 95% was observed at an average follow-up of 9.8 years, 3.4% of the patients experienced loosening of the femoral component.
VEGA Knee system was designed to allow high flexion after TKA by shortening the proximal-distal length of the posterior condylar flange of the femoral component. In addition to the design change of the femoral prosthesis, the cam and post mechanism was thickened and elongated to provide greater jump distance in deep degrees of flexion while providing proper rollback and to prevent posterior subluxation of the tibia.10) Jain et al.9) reported the clinical outcomes of short-term follow-up for 2 years using the VEGA Knee System. Compared to 2 established prosthesis, VEGA-PS prosthesis showed comparable or superior clinical performance. In a follow-up study of TKA using the VEGA Knee System, of which the mean follow-up period was 47.3 months, Lee10) reported improvements in the maximum flexion of the knee and patient-reported outcomes without a report of loosening, though 3 cases of periprosthetic osteolysis occurred. In this study, the mean maximal flexion angle after TKA using VEGA Knee System was more than 130° and ranged from 115° to 140°. In this study, ROM was not compared with other types of high-flexion design TKAs. However, compared with the results obtained from previous studies on other high-flexion design TKAs reporting the mean maximal flexion of 131°–138°, ROM obtained in this study is thought to be comparable to ROMs reported in other studies.5,6,7,14)
When evaluating the outcomes of high-flexion TKA, the survivorship of the implant should be also paid attention to in addition to ROM. Some studies, mainly published in Asian countries, reported a high incidence of loosening after high-flexion TKAs. Cho et al.7) reported that 30 cases (13.8%) had a progressive RLL around the femoral component at an average follow-up of 51 months in 218 cases of high-flexion TKA. In a follow-up study of 72 cases of TKA using high-flexion prostheses, of which the mean follow-up period was 34 months, Han et al.8) reported that aseptic loosening occurred in 38% of the patients. Another study evaluated the revision rate related to aseptic loosening among 851 cases of high-flexion TKA and 1,512 cases of conventional TKA.15) In their study, aseptic loosening was found in 4.9% of the patients after high-flexion TKA and 0.6% of the patients after conventional TKA during the follow-up period of about 70 months, and there was a significant difference in the revision rate related to loosening between the 2 types of TKA. In contrast, other studies published in Asia reported good survivorship without early aseptic loosening among the patients who received high-flexion TKA.5,16,17) Kim et al.16) reported that the average 10-year survivorship was 100% for conventional TKA and 99% for high-flexion TKA without a report of aseptic loosening. In the present study, aseptic loosening occurred in 9 cases (3.9%), of which 8 cases (3.4%) were loosening of the femoral component. Compared with the previous literature that has reported a high incidence of aseptic loosening after high-flexion TKA, in this study, a relatively low rate of loosening of the femoral component was observed at about 3.4%. However, the present study showed that a relatively higher rate of loosening was observed for the VEGA Knee System compared to conventional TKA, of which the rate of loosening was reported to be less than 1%.18)
There is still debate as to whether high-flexion TKA actually has a high risk of aseptic loosening. Some studies reported that larger net quadriceps moments and net posterior forces are generated during high flexion than during routine ambulatory activities and that this increase in load can lead to pathological changes in the knee joint.19) High contact stress applied to the post-cam mechanism during high flexion has also been suggested as a possible cause.20) A finite element study reported that tensile and shear stress increased at the implant-cement interface beneath the proximal part of the anterior flange during high flexion greater than 120°, which could increase the risk of loosening of the femoral component.21) Considering the study results of Cho et al.7) reporting that patients were able to squat in 23 out of 30 cases (76.7%) with a progressive RLL around the femoral component, the elevated mechanical load applied to the knee joint during high flexion may cause the occurrence of loosening in patients after high-flexion TKA. However, it is still difficult to conclude that the increased mechanical load due to high flexion is the main cause of loosening. This is because although Asians are generally thought to perform high-flexion activities more frequently than Westerners, there is no objective data showing that loosening occurs more often in Asians after conventional TKA than in Westerners.
In addition to the increased mechanical load applied to the knee joint during high flexion, the design of the high-flexion TKA prosthesis itself can increase the risk of loosening of the femoral component. In general, modern high-flexion design TKA prostheses have increased posterior condylar metal thickness and/or posteriorly beveled tibial inserts.3) The NexGen Legacy-Flex total knee system (Zimmer), classified as high flexion TKA, extends the posterior condyle of the femoral component to increase the articular contact area in high flexion, which requires an additional 2-mm bone resection from the posterior femoral condyles.16) In conventional TKA, the load is shared between the femoral component and the posterior condylar bone during high flexion. However, it has been reported that in high-flexion TKA, the extent of load sharing in high flexion is reduced, which can cause greater shear forces in the femoral component.3) The VEGA Knee System is different from the existing high-flexion TKA in that the proximal-distal length of the posterior condylar flange of the femoral component is shortened to obtain a high-flexion angle. However, it is thought that these design characteristics can cause loosening due to the increase in mechanical load or shear stress applied to the femoral component during high flexion.
In addition to the implant design, surgical techniques including the cementing technique may also be possible causes of loosening of the femoral component.22) However, since pressurizing and bi-surface cementing techniques were used in all surgeries performed in this study, it is thought that the influence of surgical technique-related factors on femoral component loosening can be excluded.
This study has a few limitations. First, this study is a retrospective study with a small number of cases. Second, this study is a case series without comparisons with other types of high-flexion design TKA or conventional TKA. Therefore, it was difficult to evaluate whether the loosening rate of the high-flexion design prosthesis (VEGA) was lower than that of other high-flexion design prosthesis. Third, in the VEGA Knee System, the shortened proximaldistal length of a posterior condylar flange of the femoral component may affect stability in mid-flexion, but this study did not evaluate mid-flexion instability. Lastly, the association between postoperative lifestyle and loosening in patients who underwent TKA was not evaluated. To evaluate the factors associated with loosening of the femoral component in high-flexion TKA, of which incidence is relatively high, it is necessary to evaluate whether the patient continues the activities requiring high flexion even after TKA. However, because the number of cases in which loosening occurred was very small in this study, it was not possible to analyze the association between the lifestyle of the patients and loosening.
The VEGA Knee System provided good clinical results in the long-term follow-up period. Although the VEGA Knee System showed acceptable implant survivorship, loosening of the femoral component occurred in about 3.4% of the patients. For more accurate evaluation of the survivorship of high-flexion design TKA with a short posterior flange, it is necessary to conduct more long-term follow-up studies targeting diverse races, especially Asians who frequently perform high-flexion activities.
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KD. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res. 2010;468(1):57–63. doi: 10.1007/s11999-009-1119-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Devers BN, Conditt MA, Jamieson ML, Driscoll MD, Noble PC, Parsley BS. Does greater knee flexion increase patient function and satisfaction after total knee arthroplasty? J Arthroplasty. 2011;26(2):178–186. doi: 10.1016/j.arth.2010.02.008. [DOI] [PubMed] [Google Scholar]
- 3.Bollars P, Luyckx JP, Innocenti B, Labey L, Victor J, Bellemans J. Femoral component loosening in high-flexion total knee replacement: an in vitro comparison of high-flexion versus conventional designs. J Bone Joint Surg Br. 2011;93(10):1355–1361. doi: 10.1302/0301-620X.93B10.25436. [DOI] [PubMed] [Google Scholar]
- 4.Sumino T, Tomita T, Sugamoto K, Yamazaki T, Okazaki K. Semi-constrained posterior stabilized total knee arthroplasty reproduces natural deep knee bending kinematics. BMC Musculoskelet Disord. 2020;21(1):107. doi: 10.1186/s12891-020-3059-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Huang HT, Su JY, Wang GJ. The early results of high-flex total knee arthroplasty: a minimum of 2 years of follow-up. J Arthroplasty. 2005;20(5):674–679. doi: 10.1016/j.arth.2004.09.053. [DOI] [PubMed] [Google Scholar]
- 6.Kim TH, Lee DH, Bin SI. The NexGen LPS-flex to the knee prosthesis at a minimum of three years. J Bone Joint Surg Br. 2008;90(10):1304–1310. doi: 10.1302/0301-620X.90B10.21050. [DOI] [PubMed] [Google Scholar]
- 7.Cho SD, Youm YS, Park KB. Three- to six-year follow-up results after high-flexion total knee arthroplasty: can we allow passive deep knee bending? Knee Surg Sports Traumatol Arthrosc. 2011;19(6):899–903. doi: 10.1007/s00167-010-1218-x. [DOI] [PubMed] [Google Scholar]
- 8.Han HS, Kang SB, Yoon KS. High incidence of loosening of the femoral component in legacy posterior stabilised-flex total knee replacement. J Bone Joint Surg Br. 2007;89(11):1457–1461. doi: 10.1302/0301-620X.89B11.19840. [DOI] [PubMed] [Google Scholar]
- 9.Jain NP, Lee SY, Morey VM, Chong S, Kang YG, Kim TK. Early clinical outcomes of a new posteriorly stabilized total knee arthroplasty prosthesis: comparisons with two established prostheses. Knee Surg Relat Res. 2017;29(3):180–188. doi: 10.5792/ksrr.16.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee SJ. High flexion total knee arthroplasty using short posterior flange of femoral component mid-term results. Australas Med J (Online) 2019;12(1):27–33. [Google Scholar]
- 11.Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee Injury and Osteoarthritis Outcome Score (KOOS): development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28(2):88–96. doi: 10.2519/jospt.1998.28.2.88. [DOI] [PubMed] [Google Scholar]
- 12.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15(12):1833–1840. [PubMed] [Google Scholar]
- 13.Ewald FC. The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res. 1989;(248):9–12. [PubMed] [Google Scholar]
- 14.Weeden SH, Schmidt R. A randomized, prospective study of primary total knee components designed for increased flexion. J Arthroplasty. 2007;22(3):349–352. doi: 10.1016/j.arth.2006.04.007. [DOI] [PubMed] [Google Scholar]
- 15.Choi YJ, Lee KW, Ha JK, et al. Comparison of revision rates due to aseptic loosening between high-flex and conventional knee prostheses. Knee Surg Relat Res. 2018;30(2):161–166. doi: 10.5792/ksrr.17.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim YH, Park JW, Kim JS. High-flexion total knee arthroplasty: survivorship and prevalence of osteolysis: results after a minimum of ten years of follow-up. J Bone Joint Surg Am. 2012;94(15):1378–1384. doi: 10.2106/JBJS.K.01229. [DOI] [PubMed] [Google Scholar]
- 17.Rhee SJ, Hong SM, Suh JT. High-flexion total knee arthroplasty using NexGen LPS-Flex System: minimum 5-year follow-up results. Knee Surg Relat Res. 2015;27(3):156–162. doi: 10.5792/ksrr.2015.27.3.156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rhee SJ, Kim HJ, Lee CR, Kim CW, Gwak HC, Kim JH. A comparison of long-term outcomes of computer-navigated and conventional total knee arthroplasty: a meta-analysis of randomized controlled trials. J Bone Joint Surg Am. 2019;101(20):1875–1885. doi: 10.2106/JBJS.19.00257. [DOI] [PubMed] [Google Scholar]
- 19.D’Lima DD, Steklov N, Fregly BJ, Banks SA, Colwell CW., Jr In vivo contact stresses during activities of daily living after knee arthroplasty. J Orthop Res. 2008;26(12):1549–1555. doi: 10.1002/jor.20670. [DOI] [PubMed] [Google Scholar]
- 20.Nakayama K, Matsuda S, Miura H, Iwamoto Y, Higaki H, Otsuka K. Contact stress at the post-cam mechanism in posterior-stabilised total knee arthroplasty. J Bone Joint Surg Br. 2005;87(4):483–488. doi: 10.1302/0301-620X.87B4.15684. [DOI] [PubMed] [Google Scholar]
- 21.Zelle J, Janssen D, Van Eijden J, De Waal Malefijt M, Verdonschot N. Does high-flexion total knee arthroplasty promote early loosening of the femoral component? J Orthop Res. 2011;29(7):976–983. doi: 10.1002/jor.21363. [DOI] [PubMed] [Google Scholar]
- 22.Han HS, Lee MC. Cementing technique affects the rate of femoral component loosening after high flexion total knee arthroplasty. Knee. 2017;24(6):1435–1441. doi: 10.1016/j.knee.2017.08.002. [DOI] [PubMed] [Google Scholar]