Abstract
Acid inhibitors have been considered in treating gastroesophageal reflux-related cough (GERC). Compared to proton pump inhibitors (PPIs), potassium-competitive acid blockers (P-CABs) have more potent and durable effects on anti-acid secretion. However, whether vonoprazan and esomeprazole have different therapeutic effects on GERC remains unknown. Patients diagnosed with GERC were enrolled in our study and randomly treated with vonoprazan (20 mg, once daily, P-CAB) or esomeprazole (20 mg, twice daily, PPI) for two months. A prokinetic agent was also administered. Patients were followed up once a month. Cough severity visual analogue scale (VAS) was measured as the primary outcome, while cough symptom score (CSS) and scores for cough-related quality-of-life or reflux-related symptoms were the secondary endpoints. A total of 50 patients completed the study, with 25 patients in each group. P-CAB and PPI groups showed similar decreases in cough severity VAS and CSS scores after the 2-month treatment (all P < 0.001). For quality-of-life, the Leicester Cough Questionnaire (LCQ) score increased significantly from baseline in both groups, but the P-CAB group had greater improvement and a higher LCQ score in month 2 (all P ≤ 0.05). For reflux-related symptoms, the Hull Airway Reflux Questionnaire (HARQ) score declined substantially over time in the P-CAB group, while the reflux symptom index (RSI) score decreased in both groups. The P-CAB group tended to have a lower HARQ (P = 0.051) and RSI (P = 0.069) scores in month 2. In conclusion, vonoprazan may be comparable to esomeprazole in cough symptom relief in GERC during the 2-month treatment period, but possibly provides better gains on classic reflux symptoms and quality-of-life. The long-term efficacy of P-CABs on GERC may be worth further exploration.
Trial Registration
Chinese Clinical Trial Registry Identifier: ChiCTR2200067089
Keywords: Gastroesophageal reflux, potassium-competitive acid blocker, proton pump inhibitor, chronic cough, symptom, quality of life
INTRODUCTION
Gastroesophageal reflux-related cough (GERC), an extraesophageal syndrome of gastroesophageal reflux disease (GERD), is one of the common etiologies of chronic cough.1 Globally, the prevalence of GERC varies between regions, ranging from 2% to 86% and accounting for around 4.6% in China.1,2 It poses considerable implications on the quality-of-life and labor productivity of patients.
Proton pump inhibitors (PPIs), such as esomeprazole, have been applied as the first-line treatment for GERD worldwide for more than 20 years.3 The efficacy of PPIs on GERC may not be dismissed, especially for patients with peptic symptoms or acid reflux.4,5 However, there are some pharmacological deficiencies, including short half-life, slow onset of action, short duration of anti-secretion, etc.6
Potassium-competitive acid blockers (P-CABs), such as vonoprazan, are a class of novel acid inhibitors. Compared to PPIs, P-CABs are stable in acidic environments and have a faster onset and a longer duration of acid suppression.6 In the clinical efficacy, P-CABs were non-inferior or superior to PPIs on reflux-related symptoms resolution (such as heartburn or regurgitation) and healing esophagitis in the short-term and long-term maintenance therapy.7,8,9,10 Recently, P-CABs have been recommended as an initial or maintenance treatment for GERD.11
Nevertheless, there is still lack of evidence to clarify whether the efficacy of P-CABs and PPIs on GERC is different. This pilot study aimed to compare the effect of vonoprazan and esomeprazole on cough relief, and the improvement of classic reflux symptoms and quality-of-life in patients with GERC during the two-month treatment period.
MATERIALS AND METHODS
Participants
Patients with chronic cough (lasting for more than 8 weeks) referred to the First Affiliated Hospital of Guangzhou Medical University were screened from 2022 to 2023. According to the diagnostic algorithm in the Chinese national guideline,12 patients initially underwent a series of diagnostic work-ups for cough-etiological diagnoses in our or other hospitals, including the pulmonary function test and bronchial provocation test, induced sputum cytology, fractional exhaled nitric oxide, allergen-specific immunoglobulin E, and chest radiograph or computed tomography. The common etiologies of chronic cough (including cough variant asthma, eosinophilic bronchitis, upper airway cough syndrome, etc.) were ruled out in combination with these diagnostic workups.12 The 24-hour esophageal impedance-pH monitoring was performed on those with unclear etiology and suspected of GERC as possible.
Patients with a DeMeester score ≥ 12.7, symptom association probability ≥ 80%, and/or an increased number of reflux episodes (at least 73 reflux events per 24 hours) were enrolled.12,13 If the ambulatory reflux monitoring was not available, patients needed to meet the criteria: 1) presenting cough associated with eating; 2) with typical GERD symptoms (including heartburn, regurgitation, etc.), or at least one questionnaire score exceeding the cutoff values of gastroesophageal reflux disease questionnaire (GerdQ) score of ≥ 8,14 Hull Airway Reflux Questionnaire (HARQ) score of ≥ 24,15 or reflux symptom index (RSI) score of ≥ 13.16 Those with more than 10-pack-year smoking history, respiratory infection in past four weeks, persistent use of angiotensin-converting enzyme inhibitors, chronic cough with abnormal chest imaging, or a history of esophageal or gastrointestinal disorders that may influence the therapeutic response were excluded.
Study design and treatment
This was an open-label pilot study to compare the efficacy of P-CABs and PPIs on GERC. Patients recruited into the study were divided by simple randomization and orally treated with vonoprazan (20mg, once daily) or esomeprazole (20 mg, twice daily) for 2 months. These dosages were in common use to treat GERD and GERC in accordance with guidelines or expert consensus.11,12,17 Vonoprazan was taken either before or after a meal, while esomeprazole was administered about 30 minutes before breakfast (or the first substantial meal of the day) and dinner. Randomization numbers were computer generated and allocated in order of enrollment. A prokinetic agent (Itopride, 50 mg, 3 times daily) was also added to provide more potential therapeutic gains, due to the possible combination of esophageal dysmotility18,19 and limited routine use of esophageal manometry in the respiratory clinic. Approximately 30% of patients in each group received dextromethorphan for around 7 days because they suffered from unbearable cough in the initial phrase of treatment.
Patients were followed up once a month. Questionnaires for evaluating cough symptoms (cough severity visual analogue scale [VAS], cough symptom score [CSS]), cough-related quality-of-life (Leicester Cough Questionnaire [LCQ]), and reflux-related symptoms (GerdQ, HARQ, and RSI) were employed at baseline and each follow-up. The reflux-related symptoms addressed in these questionnaires included classic reflux symptoms (such as heartburn, regurgitation, and belching) and extraesophageal manifestations (including cough and pharyngeal symptoms).
Both vonoprazan and esomeprazole used in the study are common medications for GERD or GERC recommended by guidelines or specialist consensus.1,3,4,11,12 The study was approved by the Ethic Committee of the First Affiliated Hospital of Guangzhou Medical University with registration number ChiCTR2200067089. Informed consent was obtained from all patients included in the study.
Statistical analysis
The primary end point was cough severity VAS score after 2 months of treatment along with the change from baseline to post-treatment, while others were defined as the secondary end points including the CSS, LCQ, GerdQ, HARQ, and RSI scores at each visit. The Shapiro-Wilk test was performed on each variable to identify normal distribution. Continuous variables with normal distribution are presented as mean ± standard deviation (SD); otherwise, they are expressed as median and interquartile range. Categorical variables are described as numbers (percentages).
For baseline variables, significant differences between the two groups were analyzed by the independent-samples t test, Mann-Whitney U test, Pearson χ2 test or Fisher’s Exact test as appropriate. Additionally, the change value of each questionnaire score from baseline to posttreatment was also calculated, and the independent-samples t test was performed to identify the differences. For the primary and secondary efficacy outcomes, statistical differences between 2 groups were analyzed by using Generalized Estimation Equations. The Bonferroni test was chosen for multiple comparisons on the differences in efficacy at different time points between the P-CAB group and PPI groups. Statistical analysis was conducted using SPSS (version 25.0; IBM Corp., Armonk, NY, USA). A P value of less than 0.05 was considered statistically significant.
This study was a pilot study for comparing the efficacy of vonoprazan and esomeprazole on GERC. The sample size was set by reference to the published studies on GERD.20,21 Also, according to the previous study on GERC,22 we assumed that the mean VAS score was 38 after 2-month treatment of esomeprazole, and the SD was 19. A difference of 15 in the VAS score has been considered clinically significant.23 Hence, the VAS score in the vonoprazan group was assumed to be 15 points lower than that in the esomeprazole group. The Alpha and Beta risks were set at 5% and 20%. Considering a dropout rate of 20%, 32 patients were planned to be recruited in each group.
RESULTS
Demographic and clinical characteristics
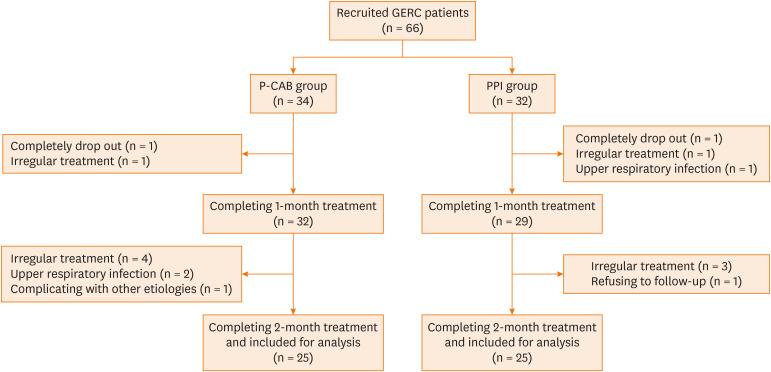
A total of 66 patients with GERC meeting the criteria were recruited in the study; 34 and 32 patients randomly received vonoprazan and esomeprazole, respectively. Finally, there were 25 patients in each group completing 2 phases of treatment (Fig. 1). No significant difference was found in the dropout rate between the P-CAB and PPI groups (26.5% vs. 21.9%, P = 0.663).
Fig. 1. The flow chart of the study.
GERC, gastroesophageal reflux-related cough; P-CAB, potassium-competitive acid blocker; PPI, proton pump inhibitor.
The mean age of subjects was 42.08 ± 13.36 in the P-CAB group and 37.36 ± 11.54 in the PPI group. Females accounted for 56.0% in the P-CAB group and 60.0% in the PPI group. Chest tightness, sour regurgitation, and belching were common accompanying refluxed-related symptoms in the two groups. Patients with positive DeMeester score, AET, SAP or reflux episodes accounted for 32.5%, 22.5%, 82.5%, and 80%, respectively. The demographic and baseline clinical characteristics were comparable between the two groups (all P > 0.05; Table).
Table. Demographic and clinical characteristics of enrolled patients with gastroesophageal reflux-related cough.
| Characteristics | P-CAB group (n = 25) | PPI group (n = 25) | P value | |
|---|---|---|---|---|
| Age (year) | 42.08 ± 13.36 | 37.36 ± 11.54 | 0.188 | |
| Sex | ||||
| Male | 11 (44.0) | 10 (40.0) | 0.774 | |
| BMI (kg/m2) | 22.07 ± 2.90 | 22.29 ± 3.42 | 0.822 | |
| Clinical features | ||||
| Chest tightness | 15 (60.0) | 15 (60.0) | 1.000 | |
| Chest pain | 2 (8.0) | 5 (20.0) | 0.417 | |
| Sour regurgitation | 15 (60.0) | 14 (56.0) | 0.774 | |
| Belching | 10 (40.0) | 14 (56.0) | 0.258 | |
| Heartburn | 8 (32.0) | 9 (36.0) | 0.765 | |
| Abdominal distension | 6 (24.0) | 9 (36.0) | 0.355 | |
| Abdominal pain | 5 (20.0) | 4 (16.0) | 1.000 | |
| Comorbidities | ||||
| GERD | 1 (4.0) | 1 (4.0) | 1.000 | |
| Gastritis/duodenitis | 9 (36.0) | 9 (36.0) | 1.000 | |
| OSAS | 1 (4.0) | 3 (12.0) | 0.609 | |
| Cardiovascular diseases | 2 (8.0) | 0 (0.0) | 0.490 | |
| Spirometry parameters | n = 22 | n = 24 | ||
| FEV1 %pred | 103.19 ± 10.64 | 96.82 ± 10.24 | 0.044 | |
| FVC %pred | 103.92 ± 12.45 | 100.15 ± 13.74 | 0.337 | |
| FEV1/FVC | 84.26 ± 6.14 | 82.82 ± 7.46 | 0.481 | |
| Reflux monitoring metrics | n = 23 | n = 17 | ||
| DeMeester score | 4.65 (0.68–13.80) | 6.50 (2.34–16.95) | 0.746 | |
| AET | 1.30 (0.10–4.20) | 1.60 (0.38–3.90) | 1.000 | |
| Reflux episodes per 24 h | 88.00 (73.00–115.00) | 116.00 (86.00–148.00) | 1.000 | |
| Acidic reflux | 29.00 (5.00–40.00) | 36.00 (27.00–52.50) | 0.055 | |
| Weakly acidic reflux | 44.00 (32.00–64.00) | 58.00 (34.50–85.50) | 0.126 | |
| Weakly alkaline reflux | 11.00 (1.00–31.00) | 17.00 (6.00–32.00) | 0.315 | |
| SAP | ||||
| Acid reflux ≥ 80% | 11 (48.0) | 10 (59.0) | 0.491 | |
| Weakly acidic reflux ≥ 80% | 13 (57.0) | 10 (59.0) | 0.884 | |
| Weakly alkaline reflux ≥ 80% | 1 (4.0) | 4 (24.0) | 0.144 | |
Data are presented as mean ± standard deviation, medians (interquartile range), or number (%). N is the total number of patients with available data. Cardiovascular diseases included hypertension, coronary artery disease and arrhythmia. The SAP was recorded to evaluate the association between cough and reflux. The significant differences between the two groups were analyzed by the Independent-samples t test, Mann-Whitney U test, Pearson χ2 test or Fisher’s exact test as appropriate.
P-CAB, potassium-competitive acid blocker; PPI, proton-pump inhibitor; BMI, body mass index; GERD, gastroesophageal reflux disease; OSAS, obstructive sleep apnea syndrome; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; AET, acid exposure time; SAP, symptom association probability.
Changes in cough symptom scores and quality-of-life
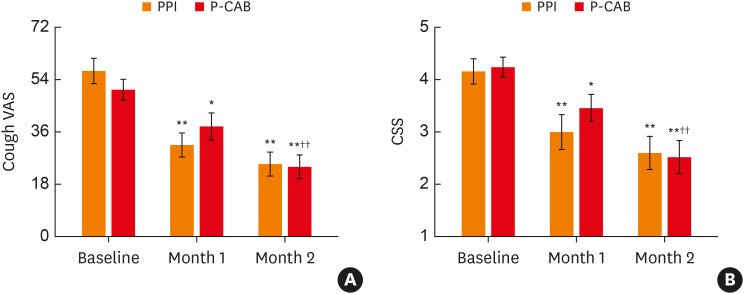
For cough symptom, the cough severity (VAS and CSS) scores showed significant reductions from baseline to month 1 and month 2 in the P-CAB and PPI groups (Fig. 2). However, no significant differences were found in these scores between two groups at any visit (all P > 0.05). The mean changes in VAS and CSS scores after two-month treatment were 26.60 ± 22.95 and 1.72 ± 1.70, respectively, in the P-CAB group; and 32.08 ± 24.80 and 1.56 ± 1.50, respectively, in the PPI group. There were no significant differences in the mean changes between the 2 groups.
Fig. 2. Changes in cough symptom scores over time in the P-CAB and PPI groups.
(A) Changes in cough VAS score. (B) Changes in CSS score.
P-CAB, potassium-competitive acid blocker; PPI, proton pump inhibitor; VAS, visual analogue scale; CSS, cough symptom score. Each score is presented as the mean value and standard error. *P < 0.05 and **P < 0.01 were compared with baseline, while †P < 0.05 and ††P < 0.01 were compared with month 1.
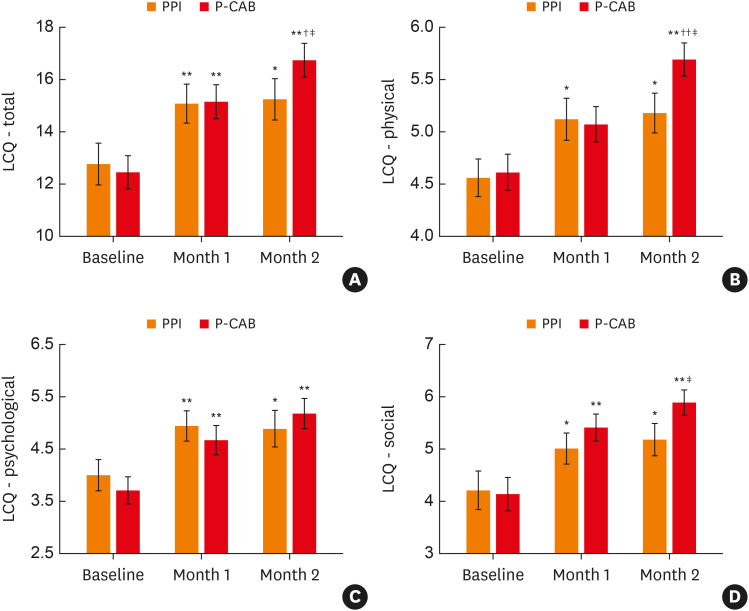
With regard to quality-of-life, the P-CAB and PPI groups showed significant increases in the total LCQ score and three domain scores (Fig. 3). Compared to the PPI group, the P-CAB group had greater improvement and a higher score in total LCQ in month 2 (mean changes: 4.66 ± 3.98 vs. 2.07 ± 4.23; P = 0.05), so did in the physical and social domains (mean changes: 1.16 ± 1.04 vs. 0.49 ± 1.12 for physical domain, P = 0.053; 1.97 ± 1.72 vs. 0.75 ± 1.67 for social domain, P = 0.028).
Fig. 3. Changes in scores for cough-related quality-of-life over time in the P-CAB and PPI groups.
(A) Changes in the total LCQ score. (B) Changes in the physical domain score. (C) Changes in the psychological domain score. (D) Changes in the social domain score.
P-CAB, potassium-competitive acid blocker; PPI, proton pump inhibitor; LCQ, Leicester Cough Questionnaire. Each score is presented as the mean value and standard error. *P < 0.05 and **P < 0.01 were compared with baseline, while †P < 0.05 and ††P < 0.01 were compared with month 1. ‡p < 0.05 was compared with the PPI group.
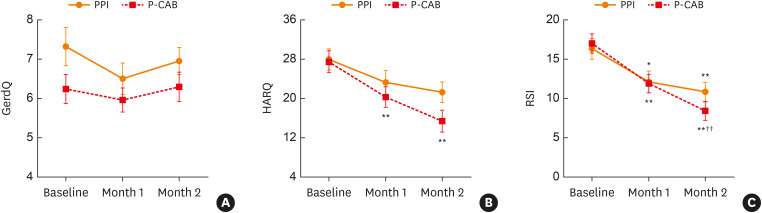
Changes in reflux-related scores
The two groups had no significant changes in the GerdQ score from baseline to months 1 and 2. There were also no statistical differences in the GerdQ score between the two groups either at any time points (Fig. 4A). The mean HARQ score significantly declined in the P-CAB group compared to baseline (all P < 0.01), but no statistical significance was found in the PPI group (Fig. 4B). The RSI score decreased over time in the two groups. In the P-CAB group, unlike in the PPI group, the RSI score was significantly lower in month 2 than in month 1 (Fig. 4C). both HARQ and RSI scores were lower in the P-CAB group than in the PPI group in month 2 (15.39 ± 11.10 vs. 21.26 ± 9.50 for HARQ, P = 0.051; 8.41 ± 5.70 vs. 10.84 ± 5.36 for RSI, P = 0.069 each).
Fig. 4. Changes in scores for reflux-related symptoms over time in the P-CAB and PPI groups.
(A) Changes in GerdQ score. (B) Changes in HARQ score. (C) Changes in RSI score.
P-CAB, potassium-competitive acid blocker; PPI, proton pump inhibitor; GerdQ, gastroesophageal reflux disease questionnaire; HARQ, Hull Airway Reflux Questionnaire; RSI, reflux symptom index.
Each score is presented as the mean value and standard error. *P < 0.05 and **P < 0.01 were compared with baseline, while †P < 0.05 and ††P < 0.01 were compared with month 1.
DISCUSSION
To our knowledge, this is the first study to compare the efficacy of P-CABs and PPIs in patients with GERC. The results suggested that vonoprazan and esomeprazole could have similar efficacy on cough relief, while vonoprazan may improve classic reflux symptoms and quality-of-life more significantly after the two-month treatment. As reported in previous studies on GERD, there were no significant differences in or non-inferiority to P-CABs to PPIs in relieving reflux-related symptoms (such as heartburn and regurgitation) and healing erosive esophagitis at 4 or 8 weeks of treatment.7,8,21,24,25 In the long-term maintenance studies, vonoprazan could provide persistent effects and may be highly efficacious than some PPIs.9,10,25 However, the long-term efficacy of P-CABs on GERC and the differences from PPIs need further exploration.
The cough symptom was alleviated after acid suppressive therapy, which indicated that the efficacy of anti-acid secretion on GERC may not be dismissed. Previous studies reported that both proximal acidic reflux and distal reflux reflexes correlated to reflux-related cough in patients with GERD, with distal reflux predominant.26 In guinea pig models, repeated acid perfusion into the lower esophagus could potentiate cough hypersensitivity, airway/esophageal inflammation (especially neurogenic inflammation), and tracheal microvascular leakage.27,28 Therefore, the esophageal-bronchial cough reflex has been increasingly considered the primary mechanism of GERC, rather than aspiration that directly irritates trachea.29,30 It is indicated that inhibiting acid secretion may help prevent the persistent occurrence of neurogenic inflammation in esophagus and trachea, thereby decreasing cough hypersensitivity and improving cough symptom.
The clinical efficacy of P-CABs and PPIs may be associated with their distinct pharmacodynamic and pharmacokinetic activities. In contrast to PPIs, P-CABs reversibly inhibit the activity of gastric hydrogen potassium adenosine triphosphatase (H+, K+-ATPase) by competing with luminal K+ ions.6 The metabolism of P-CABs is mainly via CYP 3A4/5 rather than CYP 2C19, and is not susceptible to genetic polymorphisms of CYP 2C19.6 Therefore, P-CABs present higher bioavailability, prolonged half-life, and more potent and durable acid inhibition than PPIs.6 These may explain that patients with vonoprazan possibly showed greater improvement in classic reflux symptoms than those with esomeprazole in month 2.
Moreover, as PPIs are acid-labile,6,31 formulation type and timing of dosing can affect the efficacy of PPIs. To achieve maximum therapeutic efficiency, dosing should be given 30–60 minutes before breakfast or the first substantial meal of the day. For twice-daily dosing, the others should be received 30–60 minutes before dinner.3,31 Conversely, as P-CABs are independent on acid-catalyzed activation and stable in acidic environments, the efficacy of gastric acid inhibition is irrespective of meal time.6 The recommended dosage of vonoprazan for GERD is 20 mg once daily,7,11 while the suggested dosage of PPIs was twice daily for GERD-suspected chronic cough.12,17 Overall, P-CABs may provide simpler usages and enhance patients’ compliance, and thus improve the effectiveness and quality-of-life.
There were nonparallel changes between the improvements in cough and classic reflux symptoms after the treatment with vonoprazan when compared to esomeprazole. It might be associated with the heterogeneity on clinical features between GERD and GERC. Additionally, 43%–75% of GERC patients without classic reflux symptoms presented with cough as the main or sole symptom.17 When reflux causes cough, there may be no gastrointestinal symptoms up to 75% of time.32 The guideline on GERC suggested that gastrointestinal symptoms will respond within 4–8 weeks, while the improvement in cough may take up to 3 months.33 Another potential contributor might be the mechanistic heterogeneity on cough and reflux symptoms. The esophageal-bronchial cough reflex possibly contributes to GERC.29,30 Reflux and neurogenic inflammation often initiate a vicious cycle, causing consistent cough hypersensitivity.30 However, the classic reflux symptoms are directly triggered by noxious refluxates (especially acidic refluxate) activating nociceptive receptors in the esophagus.34,35 Suppressing gastric acid secretion can reduce the noxious stimulation or injury of esophageal mucosa rather than directly inhibiting neurogenic inflammation, which may be related to the faster resolution of reflux symptoms.
Additionally, the cough relief was also not parallel to the improvement of quality-of-life, which may correlate to different measurement dimensions and time frames of the questionnaires. The cough symptom scores used in the study assess one dimension on the impact of cough, and mainly focus on the current conditions.36 The LCQ comprises of three domains (physical, psychological, and social) for evaluating quality-of-life within 2 weeks.36 There was only moderate correlation between cough severity VAS score and LCQ score.37 What is more, the perception of the impact on quality-of-life has individual variances due to age, education, social background, and so on.
There are some limitations in the study. First, this is an open-label pilot study aiming to preliminarily describe the different efficacy between P-CAB and PPI on GERC. Due to lack of a control group or crossover design, the potential occurrence of natural improvement and the placebo effect of medications cannot be ruled out. Randomized, double-blind, and placebo-controlled clinical trials with larger sample sizes and greater statistical powers should be planned and performed in subsequent research. Secondly, the objective cough frequency monitoring was not performed to assess the efficacy of treatment due to the unavailable use of cough monitor devices in China.
In conclusion, vonoprazan and esomeprazole possibly achieved comparable efficacy on cough symptom relief in patients with GERC during the two-month treatment period. In terms of classic reflux symptoms and quality-of-life, P-CABs may provide better therapeutic gains. The long-term efficacy of P-CABs on GERC may be worth further exploration.
ACKNOWLEDGMENTS
The authors are grateful to all patients who participated in the study. We also acknowledge the clinicians and paramedical staff from the First Affiliated Hospital of Guangzhou Medical University for their technical, organizational and managerial support to this work.
The work was supported by Incubation Program of National Science Foundation for Distinguished Young Scholars from Guangzhou Medical University (GMU2020-207).
Footnotes
Disclosure: Ruchong Chen has received research fundings from AstraZeneca, GlaxoSmithKline, and honoraria for lectures, presentations or speaker bureaus from AstraZeneca, GlaxoSmithKline, Novartis and Sanofi, outside the submitted work. The other authors have no relevant financial or non-financial interests to disclose.
References
- 1.Irwin RS, French CL, Chang AB, Altman KW CHEST Expert Cough Panel*. Classification of cough as a symptom in adults and management algorithms: CHEST Guideline and Expert Panel Report. Chest. 2018;153:196–209. doi: 10.1016/j.chest.2017.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lai K, Chen R, Lin J, Huang K, Shen H, Kong L, et al. A prospective, multicenter survey on causes of chronic cough in China. Chest. 2013;143:613–620. doi: 10.1378/chest.12-0441. [DOI] [PubMed] [Google Scholar]
- 3.Katz PO, Dunbar KB, Schnoll-Sussman FH, Greer KB, Yadlapati R, Spechler SJ. ACG clinical guideline for the diagnosis and management of gastroesophageal reflux disease. Am J Gastroenterol. 2022;117:27–56. doi: 10.14309/ajg.0000000000001538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Morice AH, Millqvist E, Bieksiene K, Birring SS, Dicpinigaitis P, Domingo Ribas C, et al. ERS guidelines on the diagnosis and treatment of chronic cough in adults and children. Eur Respir J. 2020;55:1901136. doi: 10.1183/13993003.01136-2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kahrilas PJ, Howden CW, Hughes N, Molloy-Bland M. Response of chronic cough to acid-suppressive therapy in patients with gastroesophageal reflux disease. Chest. 2013;143:605–612. doi: 10.1378/chest.12-1788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Abdel-Aziz Y, Metz DC, Howden CW. Review article: potassium-competitive acid blockers for the treatment of acid-related disorders. Aliment Pharmacol Ther. 2021;53:794–809. doi: 10.1111/apt.16295. [DOI] [PubMed] [Google Scholar]
- 7.Ashida K, Sakurai Y, Nishimura A, Kudou K, Hiramatsu N, Umegaki E, et al. Randomised clinical trial: a dose-ranging study of vonoprazan, a novel potassium-competitive acid blocker, vs. lansoprazole for the treatment of erosive oesophagitis. Aliment Pharmacol Ther. 2015;42:685–695. doi: 10.1111/apt.13331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Xiao Y, Zhang S, Dai N, Fei G, Goh KL, Chun HJ, et al. Phase III, randomised, double-blind, multicentre study to evaluate the efficacy and safety of vonoprazan compared with lansoprazole in Asian patients with erosive oesophagitis. Gut. 2020;69:224–230. doi: 10.1136/gutjnl-2019-318365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mizuno H, Nishino M, Yamada K, Kamiyamamoto S, Hinoue Y. Efficacy of vonoprazan for 48-week maintenance therapy of patients with healed reflux esophagitis. Digestion. 2020;101:411–421. doi: 10.1159/000500399. [DOI] [PubMed] [Google Scholar]
- 10.Miwa H, Igarashi A, Teng L, Uda A, Deguchi H, Tango T. Systematic review with network meta-analysis: indirect comparison of the efficacy of vonoprazan and proton-pump inhibitors for maintenance treatment of gastroesophageal reflux disease. J Gastroenterol. 2019;54:718–729. doi: 10.1007/s00535-019-01572-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Iwakiri K, Fujiwara Y, Manabe N, Ihara E, Kuribayashi S, Akiyama J, et al. Evidence-based clinical practice guidelines for gastroesophageal reflux disease 2021. J Gastroenterol. 2022;57:267–285. doi: 10.1007/s00535-022-01861-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lai K, Shen H, Zhou X, Qiu Z, Cai S, Huang K, et al. Clinical practice guidelines for diagnosis and management of Cough-Chinese Thoracic Society (CTS) Asthma Consortium. J Thorac Dis. 2018;10:6314–6351. doi: 10.21037/jtd.2018.09.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shay S, Tutuian R, Sifrim D, Vela M, Wise J, Balaji N, et al. Twenty-four hour ambulatory simultaneous impedance and pH monitoring: a multicenter report of normal values from 60 healthy volunteers. Am J Gastroenterol. 2004;99:1037–1043. doi: 10.1111/j.1572-0241.2004.04172.x. [DOI] [PubMed] [Google Scholar]
- 14.Xu X, Chen Q, Liang S, Lv H, Qiu Z. Comparison of gastroesophageal reflux disease questionnaire and multichannel intraluminal impedance pH monitoring in identifying patients with chronic cough responsive to antireflux therapy. Chest. 2014;145:1264–1270. doi: 10.1378/chest.13-1634. [DOI] [PubMed] [Google Scholar]
- 15.Wen S, Wang S, Niu S, Zhang M, Shi C, Qiu Z, et al. Sensitivity and specificity of combination of Hull Airway Reflux Questionnaire and gastroesophageal reflux disease questionnaire in identifying patients with gastroesophageal reflux-induced chronic cough. Ann Transl Med. 2020;8:1564. doi: 10.21037/atm-20-3236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Belafsky PC, Postma GN, Koufman JA. Validity and reliability of the reflux symptom index (RSI) J Voice. 2002;16:274–277. doi: 10.1016/s0892-1997(02)00097-8. [DOI] [PubMed] [Google Scholar]
- 17.Hom C, Vaezi MF. Extra-esophageal manifestations of gastroesophageal reflux disease: diagnosis and treatment. Drugs. 2013;73:1281–1295. doi: 10.1007/s40265-013-0101-8. [DOI] [PubMed] [Google Scholar]
- 18.Burke JM, Jackson W, Morice AH. The role of high resolution oesophageal manometry in occult respiratory symptoms. Respir Med. 2018;138:47–49. doi: 10.1016/j.rmed.2018.03.027. [DOI] [PubMed] [Google Scholar]
- 19.Sykes DL, Crooks MG, Hart SP, Jackson W, Gallagher J, Morice AH. Investigating the diagnostic utility of high-resolution oesophageal manometry in patients with refractory respiratory symptoms. Respir Med. 2022;202:106985. doi: 10.1016/j.rmed.2022.106985. [DOI] [PubMed] [Google Scholar]
- 20.Oshima T, Arai E, Taki M, Kondo T, Tomita T, Fukui H, et al. Randomised clinical trial: vonoprazan versus lansoprazole for the initial relief of heartburn in patients with erosive oesophagitis. Aliment Pharmacol Ther. 2019;49:140–146. doi: 10.1111/apt.15062. [DOI] [PubMed] [Google Scholar]
- 21.Sakurai K, Suda H, Fujie S, Takeichi T, Okuda A, Murao T, et al. Short-term symptomatic relief in gastroesophageal reflux disease: a comparative study of esomeprazole and vonoprazan. Dig Dis Sci. 2019;64:815–822. doi: 10.1007/s10620-018-5365-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Faruqi S, Molyneux ID, Fathi H, Wright C, Thompson R, Morice AH. Chronic cough and esomeprazole: a double-blind placebo-controlled parallel study. Respirology. 2011;16:1150–1156. doi: 10.1111/j.1440-1843.2011.02014.x. [DOI] [PubMed] [Google Scholar]
- 23.Fukumitsu K, Kanemitsu Y, Asano T, Takeda N, Ichikawa H, Yap JM, et al. Tiotropium attenuates refractory cough and capsaicin cough reflex sensitivity in patients with asthma. J Allergy Clin Immunol Pract. 2018;6:1613–1620.e2. doi: 10.1016/j.jaip.2018.01.016. [DOI] [PubMed] [Google Scholar]
- 24.Cheng Y, Liu J, Tan X, Dai Y, Xie C, Li X, et al. Direct comparison of the efficacy and safety of vonoprazan versus proton-pump inhibitors for gastroesophageal reflux disease: a systematic review and meta-analysis. Dig Dis Sci. 2021;66:19–28. doi: 10.1007/s10620-020-06141-5. [DOI] [PubMed] [Google Scholar]
- 25.Ashida K, Sakurai Y, Hori T, Kudou K, Nishimura A, Hiramatsu N, et al. Randomised clinical trial: vonoprazan, a novel potassium-competitive acid blocker, vs. lansoprazole for the healing of erosive oesophagitis. Aliment Pharmacol Ther. 2016;43:240–251. doi: 10.1111/apt.13461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Li X, Lin S, Wang Z, Zhang H, Sun X, Li J, et al. Gastroesophageal reflux disease and chronic cough: a possible mechanism elucidated by ambulatory pH-impedance-pressure monitoring. Neurogastroenterol Motil. 2019;31:e13707. doi: 10.1111/nmo.13707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chen Z, Sun L, Chen H, Gu D, Zhang W, Yang Z, et al. Dorsal vagal complex modulates neurogenic airway inflammation in a guinea pig model with esophageal perfusion of HCl. Front Physiol. 2018;9:536. doi: 10.3389/fphys.2018.00536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhi H, Zhong M, Huang J, Zheng Z, Ji X, Xu Y, et al. Gabapentin alleviated the cough hypersensitivity and neurogenic inflammation in a guinea pig model with repeated intra-esophageal acid perfusion. Eur J Pharmacol. 2023;959:176078. doi: 10.1016/j.ejphar.2023.176078. [DOI] [PubMed] [Google Scholar]
- 29.Houghton LA, Lee AS, Badri H, DeVault KR, Smith JA. Respiratory disease and the oesophagus: reflux, reflexes and microaspiration. Nat Rev Gastroenterol Hepatol. 2016;13:445–460. doi: 10.1038/nrgastro.2016.91. [DOI] [PubMed] [Google Scholar]
- 30.Irwin RS, Madison JM, Fraire AE. The cough reflex and its relation to gastroesophageal reflux. Am J Med. 2000;108(Suppl 4a):73S–78S. doi: 10.1016/s0002-9343(99)00341-1. [DOI] [PubMed] [Google Scholar]
- 31.Welage LS. Pharmacologic properties of proton pump inhibitors. Pharmacotherapy. 2003;23:74S–80S. doi: 10.1592/phco.23.13.74s.31929. [DOI] [PubMed] [Google Scholar]
- 32.Irwin RS, Madison JM. Diagnosis and treatment of chronic cough due to gastro-esophageal reflux disease and postnasal drip syndrome. Pulm Pharmacol Ther. 2002;15:261–266. doi: 10.1006/pupt.2002.0348. [DOI] [PubMed] [Google Scholar]
- 33.Kahrilas PJ, Altman KW, Chang AB, Field SK, Harding SM, Lane AP, et al. Chronic cough due to gastroesophageal reflux in adults: CHEST Guideline and Expert Panel Report. Chest. 2016;150:1341–1360. doi: 10.1016/j.chest.2016.08.1458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ustaoglu A, Woodland P. Sensory phenotype of the oesophageal mucosa in gastro-oesophageal reflux disease. Int J Mol Sci. 2023;24:2502. doi: 10.3390/ijms24032502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yu M, Chang C, Undem BJ, Yu S. Capsaicin-sensitive vagal afferent nerve-mediated interoceptive signals in the esophagus. Molecules. 2021;26:3929. doi: 10.3390/molecules26133929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cho PS, Birring SS, Fletcher HV, Turner RD. Methods of cough assessment. J Allergy Clin Immunol Pract. 2019;7:1715–1723. doi: 10.1016/j.jaip.2019.01.049. [DOI] [PubMed] [Google Scholar]
- 37.Turner RD, Birring SS. Measuring cough: what really matters? J Thorac Dis. 2023;15:2288–2299. doi: 10.21037/jtd-23-230. [DOI] [PMC free article] [PubMed] [Google Scholar]