Abstract
Purpose
To test cefiderocol, a siderophore-cephalosporin antibiotic for topical monotherapy treatment of experimental extensively drug-resistant (XDR) Pseudomonas aeruginosa keratitis.
Design
Preclinical study.
Subjects and Controls
Deidentified P. aeruginosa keratitis isolates, XDR P. aeruginosa from eye drop outbreak, rabbits, saline, cefiderocol 50 mg/ml, ciprofloxacin 0.3%, and tobramycin 14 mg/ml.
Methods, Intervention, or Testing
Cefiderocol antibacterial activity against P. aeruginosa keratitis isolates (n = 135) was evaluated by minimum inhibitory concentration (MIC) testing. Ocular toxicity/tolerability and antibacterial efficacy were tested in vivo with experimental rabbit models. Corneal concentrations and stability were assessed using a bioassay.
Main Outcome Measures
Minimum inhibitory concentration analysis for susceptibility, graded tests for ocular toxicity/tolerability, colony-forming unit (CFU) analysis for bacterial burden, corneal cefiderocol concentrations.
Results
One hundred percent of P. aeruginosa keratitis isolates were susceptible to cefiderocol (n = 135), the MIC90 was 0.125 μg/ml including the XDR isolate (MIC = 0.125 μg/ml). Topical cefiderocol 50 mg/ml was minimally toxic to the ocular surface and was well tolerated. For the XDR P. aeruginosa isolate, topical cefiderocol 50 mg/ml, significantly decreased corneal CFU compared with ciprofloxacin 0.3%, tobramycin 14 mg/ml, and saline. In addition, tobramycin 14 mg/ml was more effective than the saline control. Mean cefiderocol corneal concentrations were 191× greater than the MIC90 of the P. aeruginosa keratitis isolates. Refrigerated cefiderocol maintained antimicrobial activity over a 1-month period.
Conclusions
These results demonstrate that cefiderocol is well tolerated on rabbit corneas and is effective against P. aeruginosa keratitis isolates in vitro and was effective in vivo against an XDR isolate in a rabbit keratitis model. Given the recent outbreak of keratitis caused by this XDR P. aeruginosa, cefiderocol is a promising additional antibiotic that should be further evaluated for topical treatment of keratitis caused by antibiotic resistant P. aeruginosa.
Financial Disclosure(s)
Proprietary or commercial disclosure may be found in the Footnotes and Disclosures at the end of this article.
Keywords: Antibiotic resistance, Cefiderocol, Keratitis, Ocular infection, Pseudomonas aeruginosa
The Centers for Disease Control and Prevention (CDC) and numerous news organizations recently reported a dangerous outbreak of eye infections linked to the use of artificial tears purchased online.1, 2, 3, 4 Patients identified in this outbreak have experienced serious corneal infections which have led to blindness, loss of eyes, and even death in several patients. Notably, the Pseudomonas aeruginosa bacteria causing the infections was extensively drug resistant (XDR), including to all antibiotics currently used to topically treat eye infections.2,3 Extensive drug resistance has been defined as “non-susceptibility to at least one agent in 3 or more antimicrobial categories.”5 This strain has the Verona integron-mediated metallo-β-lactamase and Guiana extended-spectrum β-lactamase genes.1,4,6
The World Health Organization and CDC consider antibiotic-resistant bacteria to be a global threat.7 Keratitis patients infected with multidrug resistant bacteria have worse clinical outcomes and longer and more costly treatment.8, 9, 10 Although XDR keratitis isolates are unusual, the Antibiotic Resistance in Ophthalmology Monitoring (ARMOR) study has documented a concerning frequency of antibiotic resistant keratitis isolates.11,12 With respect to P. aeruginosa ocular infections, antibiotic resistance to aminoglycosides and fluoroquinolones is generally low in the United States,13,14 Europe,15 and Australia16 whereas a concerning increase in fluoroquinolone resistance has been recently reported for India, with up to 50% of P. aeruginosa keratitis isolates demonstrating ciprofloxacin resistance.17
Because of the existing threat of XDR pathogens, there is a need to identify new antimicrobials for the topical treatment of keratitis. Keratitis caused by XDR pathogens is difficult to treat and has a high rate of failure.18 The latest antibiotic US Food and Drug Administration approved for treatment of eye infections, besifloxacin, was approved in 2009. The major antibiotics (aminoglycosides and fluoroquinolones) used for treatment of bacterial keratitis were approved in the 1970s through the early 2000s. Though generally well tolerated, topical fluoroquinolone use can have side effects.19 As such, there is a clear need for newer approaches to treat keratitis caused by P. aeruginosa.
Cefiderocol is a rationally designed antibiotic that combines a cephalosporin antibiotic and siderophore-like iron binding moiety into one molecule (Fig 1, chemical structure).20,21 It effectively tricks bacteria into taking up the antibiotic because of the siderophore component, so it has been called a Trojan horse strategy antibiotic.22 The commercial formulation of cefiderocol, FETROJA, was US Food and Drug Administration approved in 2019 for the treatment of complicated urinary tract infections caused by gram-negative bacteria.23 Specifically, urinary tract infections caused Enterobacter cloacae complex, Escherichia coli, Klebsiella pneumoniae, Proteus mirabilis, and P. aeruginosa, and nosocomial pneumonia caused by Acinetobacter baumannii, E. cloacae complex, E. coli, K. pneumoniae, P. aeruginosa, and Serratia marcescens. Cefiderocol was the only antibiotic to which artificial tear–associated outbreak XDR P. aeruginosa bacteria was susceptible in vitro1; however, it has not been tested for topical use in the eye.
Figure 1.
Structure of cefiderocol.
The goal of this study is to determine the suitability of cefiderocol as a topical antibiotic for the treatment of experimental P. aeruginosa keratitis. Toward this objective, the susceptibility of a panel of keratitis isolates to cefiderocol was evaluated in vitro. The tolerability of several concentrations of cefiderocol was determined after topical application to New Zealand White (NZW) rabbit eyes. Finally, the ability of highest tolerable concentration of topical cefiderocol to treat P. aeruginosa keratitis caused by an antibiotic-susceptible keratitis isolate and the XDR strain from the artificial tear outbreak (obtained from the CDC) were evaluated in an experimental NZW rabbit keratitis model. The efficacy of cefiderocol was compared with standard-of-care antibiotics ciprofloxacin 0.3% and fortified tobramycin 14 mg/ml. The stability of the topical cefiderocol solutions was evaluated over the course of a month. Last, the cefiderocol concentrations in rabbit corneas were evaluated using a bioassay. Together, the data from this study support the idea that cefiderocol should be further evaluated for use in human patients for P. aeruginosa keratitis caused by an XDR strain.
Methods
Bacterial Strains
For in vitro minimum inhibitory concentration (MIC) determinations, deidentified P. aeruginosa strains were isolated from patients with keratitis presenting to the Charles T. Campbell Ophthalmic Microbiology Laboratory at the Department of Ophthalmology at the University of Pittsburgh School of Medicine. For the in vivo studies, 2 strains of P. aeruginosa were used. Strain K900 is a keratitis isolate previously used in experimental keratitis studies24, 25, 26 and is a cytotoxic ExoU+/ExoS– strain based on its genome sequence (Genbank NZ_JAODAA000000000). Strain CDC1270 (also called AR-1270) is an XDR isolate that was obtained from the CDC. Strain CDC1270 was isolated from the cornea of a patient from the recent artificial tears eye infection outbreak.1,4,6 Isolates of the outbreak strain have been sequenced revealing multiple resistance determinants.2,6
Antibiotic Susceptibility Testing
Minimum inhibitory concentration testing of the deidentified P. aeruginosa keratitis isolates for cefiderocol and other standard of care antibiotics used to treat P. aeruginosa keratitis (tobramycin, ciprofloxacin, and ceftazidime) was performed using MIC strips (LIOFILCHEM) as previously described.27 Resistance was determined using Clinical and Laboratory Standards Institute systemic breakpoints.28 The MIC values for the strains used in the in vivo studies, K900 and CDC1270, are presented in Table 1.
Table 1.
Susceptibility of Pseudomonas aeruginosa Strains Used in This Study
| Antibiotic | K900 (MIC μg/ml) | CDC1270 (MIC μg/ml) |
|---|---|---|
| Cefiderocol | 0.023 (S) | 0.125 (S) |
| Ceftazidime | ND | > 256 (R) |
| Ciprofloxacin | 0.19 (S) | > 32 (R) |
| Tobramycin | 0.5 (S) | > 256 (R) |
MIC = minimum inhibitory concentration; ND = not determined; S = susceptible; R = resistant.
Experimental Drugs
All drugs were purchased from the UPMC Presbyterian inpatient pharmacy. The saline used in this study was 0.9% Sodium Chloride Injection USP (saline) (Baxter Healthcare Corp). To prepare cefiderocol, 1-g vials of the parenteral version of cefiderocol, FETROJA (Cefiderocol for Injection, Shionogi Inc) were used. The vials were stored at 4°C as directed until reconstituted. A fresh preparation of cefiderocol was made for each in vivo experiment. On the morning of each experiment, a 1-g vial of FETROJA was reconstituted with 10 ml of saline, and the vial was gently shaken to dissolve as per the manufacturer’s instructions. The vial was allowed to stand until the foaming generated on the surface had disappeared (typically within 2 minutes). The reconstituted solution had a final volume of approximately 11.2 ml and a concentration of 89 mg/ml. Notably, 8.43 ml of the 89 mg/ml cefiderocol stock was added to 6.57 ml of sterile saline to yield 15 ml of 50 mg/ml cefiderocol. The pH of this concentration was measured at 5.48 (Corning pH/ion analyzer 350, Corning). For the tolerability study, subsequent dilutions of the 50 mg/ml cefiderocol formulation were made in 0.9% sodium chloride injection, USP to produce concentrations of 25, 10, and 5 mg/ml. Dilutions ranged from pH 5.53 to 5.57. For all in vivo experiments, the cefiderocol solutions were kept on ice and out of light in a foil-covered tube at all times. After the experiments, the remaining cefiderocol solutions and any aliquots were refrigerated and were used in subsequent stability testing experiments.
For each keratitis trial, tobramycin 14 mg/ml was prepared from a 40 mg/ml stock of Tobramycin Injection USP (Fresenius Kabi USA, LLC). Notably, 3.5 ml of 40 mg/ml tobramycin was added to 6.5 ml of saline to yield 10 ml of 14 mg/ml of tobramycin. The solution was kept on ice during the experiment. Five ml bottles of Ciprofloxacin Hydrochloride Ophthalmic Solution, 0.3% (Sandoz Inc.) were used. The ciprofloxacin solution contains 0.006% benzalkonium chloride as a preservative. The ciprofloxacin bottles were kept at room temperature as directed. Saline served as the negative control and was kept on ice during dosing.
The cefiderocol, tobramycin, and saline solutions were instilled using a Rainin E4 XLS electronic pipet set in the multi-dispense mode. Thirty-seven μl drops were instilled. Ciprofloxacin 0.3% was instilled using its commercial dropper bottle.
Animals
New Zealand White female SPF rabbits weighing 1.1 to 1.4 kg were obtained from Charles River Laboratories Canadian rabbitry. These studies conformed to the ARVO Statement on the Use of Animals in Ophthalmic and Vision Research and were approved by the University of Pittsburgh’s Institutional Animal Care and Use Committee (IACUC Protocol 23053154).
Ocular Toxicity/Tolerability Study
An ocular toxicity/tolerability study was performed to determine whether several concentrations of topical cefiderocol were toxic to the ocular surface and whether the topical drops were tolerable. Fifteen NZW rabbits underwent a slit-lamp examination on the day before the ocular toxicity/tolerability study to determine whether there were any preexisting abnormalities. On the day of the study, the 15 rabbits were divided into 5 groups of 3 rabbits each: (1) cefiderocol 50 mg/ml; (2) cefiderocol 25 mg/ml; (3) cefiderocol 10 mg/ml; (4) cefiderocol 5 mg/ml; and (5) saline. Topical 37-μl drops were instilled into both eyes every 30 minutes for 6 hours (13 total doses). During each instillation, the behavior of the rabbits was documented and given a numerical score based on their behavior. The scoring system used was the following: no reaction after instillation (0), closed eyes after instillation (1); demonstrated delayed eye wiping (10–30 seconds) after instillation (2); demonstrated immediate eye wiping after instillation (3); flinching after instillation (4); and vocalizing after instillation (5). After the final dose, the eyes were examined using the slit-lamp and graded using the modified MacDonald Shaddock scoring system.29 The eyes were again examined and graded 3 days later to determine whether any delayed toxicity was produced.
P. aeruginosa NZW Rabbit Keratitis Model
A bacterial keratitis model optimized for evaluation of antimicrobials was used as previously described.30,31 A total of 30 NZW rabbits were used in duplicate trials of 15 rabbits for experiments involving each of the 2 P. aeruginosa strains, K900 and the CDC1270. The 30 total rabbits for each P. aeruginosa strain were divided into 5 groups of 6 rabbits.
The rabbits were anesthetized with 40 mg/kg of ketamine and 4 mg/kg of xylazine administered intramuscularly. The corneas of the left eyes were anesthetized with topical 0.5% proparacaine. The eyes were proptosed, and 6-mm areas of the central corneal epithelium of the left eyes were removed using an Amoils epithelial scrubber (Innovative Excimer Solutions). The creation of the epithelial defect was to mimic the large epithelial defects demonstrated in patients with XDR P. aeruginosa keratitis.2 Immediately afterward, the corneas were injected intrastromally with the 25 μl of phosphate buffered saline containing P. aeruginosa (∼2000 colony-forming units [CFUs]) below the area from which the epithelium was removed. Rabbits were treated with intramuscular doses of 1.5 mg/kg of ketoprofen for analgesia.
Actual inocula for each trial was determined using the EddyJet 2 spiral plating system (Neutec Group Inc.) on 5% trypticase soy agar with 5% sheep’s blood plates. Plates were incubated for ∼18 to 20 hours at 37 °C and the colonies were enumerated using the Flash and Grow colony counting system (Neutec Group, Inc.).
Sixteen hours after inoculation, the rabbits were divided into 5 groups (n = 6): (1) cefiderocol 50 mg/ml; (2) ciprofloxacin 0.3% (Standard of Care Control); (3) tobramycin 14 mg/ml (Standard of Care Control); (4) saline (Negative Control); and (5) no treatment (Onset of Therapy Control). Topical therapy for all groups was initiated at this time. The treatment regimen consisted of 1 drop every 15 minutes for 1 hour, then every 30 minutes for 7 hours (19 total doses over 8 hours).
The final group (Group 5) was euthanized at 16 hours postinoculation, and the corneas were harvested before drug treatment to establish baseline colony count determinations at the onset of therapy. The rabbits were systemically anesthetized with ketamine and xylazine as described here and euthanized with an intravenous overdose of Euthasol solution (390 mg/ml pentobarbital sodium, 50 mg/ml phenytoin sodium) following the 2020 AVMA Euthanasia Guidelines. Corneal buttons were harvested from the area encompassing visible corneal opacities using a 10-mm trephine and placed into Lysing Matrix A tubes (MP Biomedicals) containing 1 ml of phosphate buffered saline. The corneas were then homogenized with an MP Fast Prep-24 homogenizer (MP Biomedicals), and the numbers of corneal bacteria were enumerated as described here.
Before the final topical treatments, the rabbits’ eyes were examined using a slit-lamp and photographed using the camera on the slit-lamp. The Onset of Therapy groups were also similarly examined and photographed before euthanasia. After the final topical treatment, the rabbits were euthanized, the corneas harvested and homogenized, and colony count determinations performed as described here. The areas of the corneal infiltrates produced for each treatment group and P. aeruginosa strain were determined using ImageJ software (National Institutes of Health) from photographs taken of the eyes at a consistent distance and magnification.
Semiquantitative Bioassay for Cefiderocol Stability and Corneal Concentrations
The stability of the topical 50 mg/ml concentrations of cefiderocol was determined using a bioassay. After each rabbit experiment (ocular toxicity/tolerability and 4 bacterial keratitis treatment trials), aliquots of the 50 mg/ml cefiderocol solutions were refrigerated. On the day of the final bacterial keratitis study, a bioassay was performed in duplicate comparing the sizes of zones of inhibition produced from previously prepared solutions to the freshly prepared solution.
On the day of the assay, 50 mg/ml cefiderocol solutions prepared 33, 27, 21, and 7 days earlier and a freshly prepared 50 mg/ml solution were serially diluted in sterile saline to produce cefiderocol concentrations of 5, 0.5, 0.05, and 0.005 mg/ml. P. aeruginosa strain K900 was grown overnight at 37 °C on 5% trypticase soy agar with 5% sheep’s blood plates. Several colonies of P. aeruginosa strain were picked up with a sterile Dacron swab, and 10 ml of sterile saline was inoculated with the bacteria until it was turbid. A new sterile Dacron swab was used to inoculate Mueller–Hinton II agar plates to create lawns of bacteria over the entire surface of the plates. Four blank 6-mm filter paper discs were placed onto the surface of each plate. The 4 discs per plate were then inoculated with 20 μl of each of the test cefiderocol concentrations of 5, 0.5, 0.05, and 0.005 mg/ml, and the discs were allowed to dry. The plates were incubated overnight at 37 °C. The following day, the zones of inhibition for each concentration and preparation were measured in millimeters and compared. The assay was performed in duplicate for each preparation.
To determine approximate cefiderocol corneal concentrations, corneas from both the K900 and CDC1270 keratitis studies (n = 12) were used in this analysis as they were all treated with the same regimen of 50 mg/ml cefiderocol. After homogenizing and processing of the corneal buttons for colony count determinations, the supernatants of the homogenates of the cefiderocol treated corneas were processed to determine approximate cefiderocol concentrations in the homogenates. The homogenates were centrifuged and filtered through Costar Sin-X, 0.22 μm cellulose acetate filters to remove the live bacteria. Samples were either assayed at that time or were refrigerated at 4°C before testing for antibiotic activity. For this assay, a 50 mg/ml (50 000 μg/ml) cefiderocol solution was diluted in sterile saline to final concentrations of 50, 25, 12.5, 6.25, 3.125, and 1.56 μg/ml. These concentrations served as the standard concentrations for the assay. Mueller–Hinton II agar plates were prepared as in the Cefiderocol Stability Bioassay. Blank discs were inoculated with 20 μl of each of the standard cefiderocol concentrations and the undiluted corneal homogenate filtrates. The plates were incubated, and the zones of inhibition measured as described here. The zone sizes were modified to subtract the 6-mm disc size. The modified zone sizes of the corneal homogenate solutions were inserted into concentration equations produced using a Linear Fitted Line Plot Regression Analysis of cefiderocol concentration versus zone size for the cefiderocol standards (Minitab Version 19) to determine the approximate active cefiderocol concentrations contained in the corneal homogenates.
Statistical Analysis
The MIC data were placed into a GraphPad Prism worksheet, and the median, mode, range, MIC50 and MIC90 determinations were calculated. The modified MacDonald Shaddock scores and the behavioral scores from the Ocular Toxicity/Tolerability study were analyzed nonparametrically using Kruskal–Wallis analysis of variance with Dunn’s multiple comparisons test (GraphPad Prism). The corneal colony counts + 1 were log10 transformed and analyzed using analysis of variance with Tukey’s multiple comparisons test (GraphPad Prism) for test agent analysis.
Results
Antibiotic Susceptibility Analysis of P. aeruginosa Keratitis Isolates to Cefiderocol and Standard of Care Antibiotics
The MIC values of keratitis isolates to cefiderocol were evaluated, and all were found to be susceptible (Table 2 and Fig 2).28 There was a significantly higher frequency of isolates susceptible to cefiderocol than the other tested antibiotics including P. aeruginosa keratitis standard of care antibiotics ciprofloxacin (93.3% susceptible) and tobramycin (28%). The cephalosporin ceftazidime that has been suggested as an alternative to ciprofloxacin and tobramycin for treating keratitis caused by resistant isolates also had a significantly lower frequency of susceptibility compared with cefiderocol (94.9%).
Table 2.
Susceptibility of Pseudomonas aeruginosa Keratitis Isolates
| Antibiotic | n | Median | Mode | MIC50 | MIC90 | Range | Susceptible, % |
|---|---|---|---|---|---|---|---|
| Cefiderocol | 135 | 0.094 | 0.064 | 0.094 | 0.125 | <0.016–0.94 | 100 |
| Ceftazidime | 137 | 2.0 | 1.5 | 2.0 | 8.0 | 0.75–>256 | 94.9 |
| Ciprofloxacin | 164 | 0.19 | 0.19 | 0.19 | 0.5 | 0.047–1.5 | 93.3 |
| Tobramycin | 164 | 1.5 | 1.5 | 1.5 | 3.0 | 0.047–8 | 28 |
MIC values are expressed in μg/ml. Susceptibility was determined using Clinical and Laboratory Standards Institute breakpoints.28
MIC = minimum inhibitory concentration.
Figure 2.
Susceptibility of Pseudomonas aeruginosa to selected antibiotics based on minimum inhibitory concentration values compared with Clinical and Laboratory Standards Institute break points. Asterisks indicated significant differences from cefiderocol group by chi-square with Yates correction. ∗P < 0.05; ∗∗P < 0.01; ∗∗∗∗P < 0.0001.
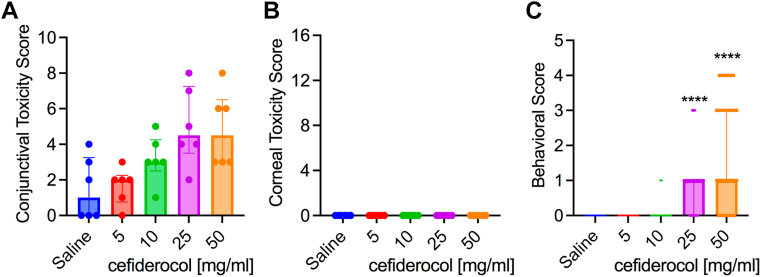
Ocular Toxicity and Tolerability of Topical Cefiderocol
The effect of 4 different concentrations of cefiderocol for ocular toxicity was measured using the modified MacDonald Shadduck scoring system. The results are divided into conjunctival scores with a 10-point total possible score and corneal scores with a 16-point possible score. This was after instillation into both eyes every 30 minutes for 6 hours (13 total doses). There was a dose-dependent increase in scores within the cefiderocol treatment groups for the conjunctival scores (congestion, chemosis, and discharge) but the differences were not significant (Fig 3A). As seen in Figure 3B, there were no clinical signs of corneal pathology seen, and there was no fluorescein staining demonstrated in any of the corneas. Photographs of all eyes on the day of treatment are presented in Figure S4 (available at www.ophthalmologyscience.org).
Figure 3.
Tolerability and behavioral impact of cefiderocol treatment. A, B, Toxicity scores (max 10 for conjunctival, 16 for corneal) of New Zealand White (NZW) rabbits exposed to topical drops of cefiderocol. Medians and interquartile ranges are shown, n = 6. No statistical differences were found between groups. C, Behavioral signs of NZW rabbits exposed to cefiderocol topical drops. Medians and interquartile ranges are shown, n = 39. Asterisks indicate significant differences from saline group by Kruskal–Wallis with Dunn’s post-test, P < 0.001.
Instillation of the 50 and 25 mg/ml cefiderocol solutions produced more behavioral signs from the rabbits than the 10 and 5 mg/ml cefiderocol solutions as well as the saline control over the course of the dosing. Based on the scoring system, both the 50 and 25 mg/ml cefiderocol solutions produced a median score of 1.0, which equates to eye closing after instillation (Fig 3C). This is the minimal score after no reaction. Infrequently, there were other behavioral signs such as eye wiping and flinching demonstrated in the 50 mg/ml group as well as eye wiping in the 25 mg/ml group.
There was resolution of all conjunctival findings from day 0 to day 3, suggesting there was no delayed ocular toxicity associated with topical cefiderocol treatment. Because the maximum tested cefiderocol concentration was well tolerated and was same concentration as other cell-wall-targeting antibiotics (cefazolin, ceftazidime, and vancomycin), the highest concentration tested, 50 mg/ml, was selected for use in the keratitis studies.
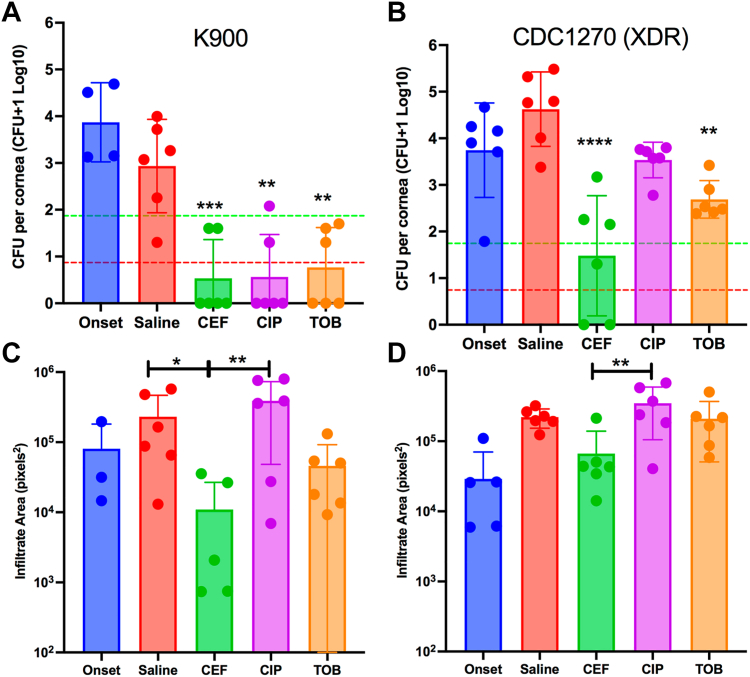
Efficacy of Cefiderocol against an Antibiotic-Susceptible P. aeruginosa Isolate in the NZW Rabbit Keratitis Model
The majority of P. aeruginosa keratitis isolates are not multidrug resistant.11,14 Therefore, we first employed an antibiotic-susceptible strain, K900 (Table 1) in our NZW rabbit keratitis model. These corneas were injected with a mean of 2350 ± 1414 CFU of P. aeruginosa K900 for the 2 trials. At 16 hours postinfection, CFU from one group was measured before treatment (Onset). The Onset group represents the baseline bacterial burden at the start of treatment. All other groups had CFU determined after an additional 8 hours of topical treatment (24 hours postinfection) (Fig 5A). There was no increase in CFU in the saline group compared with the Onset for this strain, suggesting that the maximum bacterial burden had been achieved. All antibiotic treatment groups had significantly reduced CFU compared with the saline control group. These decreases reached the level of bactericidal (99.9%) reductions compared with the Onset control. Furthermore, 67% of the corneas were sterilized with cefiderocol and ciprofloxacin treatments, whereas 50% of the corneas were sterilized with tobramycin treatment. There were no significant differences in CFU or the number of eyes sterilized between the 3 antibiotic treatments.
Figure 5.
Efficacy of antibacterial treatment. A, B, The colony-forming units (CFU) per cornea were determined by dilution plating. The onset group was evaluated at 16 hours postinfection, and before treatment. The other groups had 16 hours of untreated infection, followed by 8 hours of treatment as indicated. Asterisks indicated significant differences from the saline group by analysis of variance (ANOVA) with Tukey’s post-test. The pistachio lines represent a 99% and the red lines a 99.9% reduction in CFU compared with the onset. n = 6 except for onset group n ≥ 3. C, D, Images of eyes were taken before euthanasia from a fixed distance. The onset group was imaged at 16 hours postinfection, and before treatment. The other groups had 16 hours of untreated infection, followed by 8 hours of treatment as indicated. Relative infiltrate area was determined using ImageJ software. Mean and SD are shown and were compared by ANOVA and Tukey’s post-test. ∗P < 0.05; ∗∗P < 0.01; ∗∗∗P < 0.001; ∗∗∗∗P < 0.0001. Panels A, C used strain K900, and panels B, D used strain CDC1270. CEF = cefiderocol; CIP = ciprofloxacin; TOB = tobramycin; XDR = extensively drug-resistant.
Antibacterial Efficacy of Cefiderocol against an XDR P. aeruginosa Keratitis Isolate in the NZW Rabbit Keratitis Model
By contrast to strain K900, the CDC1270 strain from the artificial tears outbreak was an XDR strain (Table 1). CDC1270 was used in the NZW rabbit keratitis model as was K900 here. A mean of 2325 ± 955 CFU of CDC1270 were injected for the 2 trials. The CFU at the Onset of therapy was nearly identical between strains. Unlike strain K900, the CDC1270 strain continued to proliferate by approximately 10-fold over the 8-hour treatment period in the saline group. Both cefiderocol and tobramycin significantly reduced CFU (Fig 5B) compared with the saline control, whereas ciprofloxacin did not significantly reduce CFU. Cefiderocol was also significantly more effective than both ciprofloxacin and tobramycin in reducing corneal colony counts of XDR P. aeruginosa. Cefiderocol achieved a bactericidal (> 99.9%) reduction compared with the saline treatment group but not the Onset group (> 99%). Tobramycin did not achieve a 99% decrease in CFU compared with the saline control group. Moreover, cefiderocol sterilized 33% of the corneas compared with 0% for tobramycin and ciprofloxacin.
Corneal Infiltrate Size
The areas of corneal infiltrates were measured from photographs taken from each eye before euthanasia (Fig 5C, D). In both K900 and CDC1270, infected eyes treated with ciprofloxacin trended toward being larger than the saline control and smaller than saline when treated with tobramycin and cefiderocol (Fig 5C, D). In all cases, the cefiderocol-treated eyes had significantly smaller infiltrates compared with the ciprofloxacin-treated eyes (P < 0.05).
Approximate Corneal Cefiderocol Concentrations
The mean and standard deviation cefiderocol concentration obtained from the corneal homogenates from eyes infected with K900 and CDC1270 was 23.88 ± 8.69 μg/ml. The concentrations ranged from 12.53 to 38.58 μg/ml per cornea. The mean cefiderocol corneal concentration was 191× greater than the MIC90 (0.125 μg/ml) and 25× greater than the MIC100 (0.94 μg/ml) of the P. aeruginosa keratitis isolates tested. Furthermore, the entire range of cefiderocol corneal concentrations was well above the MIC90 and MIC100 values.
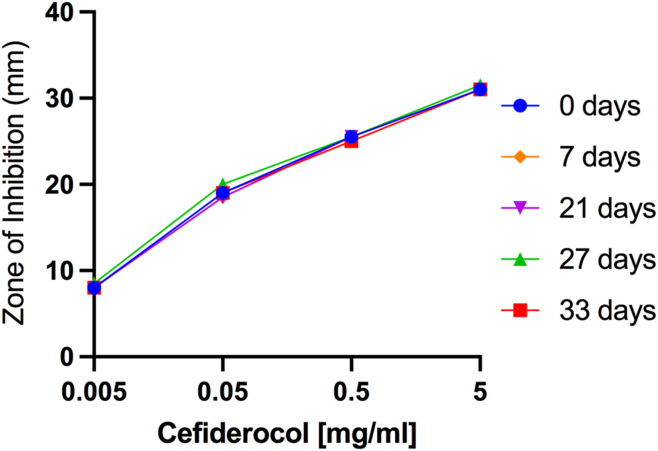
Stability of Refrigerated 50 mg/ml Cefiderocol
The results of stability testing of refrigerated 50 mg/ml cefiderocol solutions are presented in Figure 6. The zone sizes for all cefiderocol concentrations and refrigeration times are essentially the same suggesting that there is no loss in bioactivity of refrigerated 50 mg/ml cefiderocol solutions for up to 33 days.
Figure 6.
The results of stability testing of refrigerated 50 mg/ml cefiderocol solutions. The means of 2 independent assays are shown.
Discussion
The reports of the recent outbreak of XDR P. aeruginosa ocular infections demonstrated a concerning lack of efficacy of conventional topical antibiotics. Several reports describe utilization of off label medications to attempt to control these aggressive infections. In 2 reports, topically applied colistin by itself or in combination with fortified tobramycin-soaked collagen shields was used and resolved the infections after close to 2 months of therapy.32,33 In another paper, a patient was treated topically with polymyxin B/trimethoprim and imipenem-cilastatin, but the infection was not resolved during the 1 month course of the published study.3 In another report, Morelli et al2 used intravenous cefiderocol in combination with topical application of imipenem-cilastatin and polymyxin B/trimethoprim and oral doxycycline. The patient’s infection appeared to resolve, suggesting successful antibiotic treatment. As these reports demonstrate, there is no current consensus as to the most effective antimicrobial strategy to deal with XDR keratitis. Our current study was designed to test cefiderocol as a potential topical therapy for keratitis caused by XDR P. aeruginosa.
We observed that strains from our collection of keratitis isolates were more consistently susceptible to cefiderocol than ceftazidime, ciprofloxacin, or tobramycin. Notably, the Clinical and Laboratory Standards Institute susceptibility breakpoints for tobramycin have recently been changed from 4.0 to 1.0 μg/ml,34 which accounts for the high level of in vitro resistance recorded in this study. The systemic susceptibility breakpoints are not particularly useful for topical application because much higher local concentrations can be achieved in ocular tissue.31,35,36 However, strains such as the artificial tears outbreak XDR isolates have very high MIC values to commonly used antibiotics that may render them unable to reduce corneal bacteria even with topical drops. This study employed Mueller–Hinton II agar, which is commonly used for MIC testing rather than iron-depleted media that can be used for testing susceptibility to cefiderocol.37,38 This means that the measured values reported here may overestimate the MIC values.
A total of 50 and 25 mg/ml cefiderocol were associated with conjunctival congestion, chemosis, and discharge; however, significant changes in the conjunctival signs were not observed. Most importantly, no corneal toxicity or fluorescein staining was produced for any cefiderocol concentration. The most common behavioral sign noted in the 50 and 25 mg/ml concentrations was the closing of eyes after instillation. Occasionally, the rabbits wiped their eyes or even flinched after instillation in those groups. Although these signs were not seen with the lower cefiderocol concentrations or the saline control, they are similar to what has been previously reported with fortified antibiotics such as vancomycin. The pH of 50 mg/ml cefiderocol solution was acidic at 5.36 but is higher than other topical formulations such as ciprofloxacin 0.3% ophthalmic solution (pH 4.5)39 and fortified vancomycin 50 mg/ml (pH ∼3.0).40 There was no ocular toxicity or tolerability issues with the 10 and 5 mg/ml cefiderocol concentrations. The data suggest that the tested formulations were well tolerated, but a specific ocular formulation with a more neutral pH may be advantageous. In this study, however, we followed the manufacturer’s instructions for reconstitution and did not attempt to use a buffered solution for reconstitution to avoid any potential adverse effects on the activity or stability of cefiderocol. Based on the overall data from the ocular toxicity/tolerability study, we chose to use the highest cefiderocol concentration (50 mg/ml) for use in the NZW rabbit bacterial keratitis studies.
We employed a rabbit bacterial keratitis model that has previously been used for preclinical testing of antibiotics such as besifloxacin and gatifloxacin before their ophthalmic adoption. The XDR outbreak strain and a more typical antibiotic-susceptible P. aeruginosa keratitis isolate were used, as were standard-of-care antibiotics ciprofloxacin 0.3% and fortified tobramycin 14 mg/ml. Cefiderocol 50 mg/ml, ciprofloxacin 0.3%, and tobramycin 14 mg/ml showed equivalent efficacy against the antibiotic-susceptible strain K900. This is a similar outcome to a prior report for strain K900 and ciprofloxacin25 and served to demonstrate that the ciprofloxacin and tobramycin antibiotics and treatment protocol used in this study were effective against a susceptible strain.
Although all the antibiotic treatments indicated antibacterial efficacy against the antibiotic-susceptible P. aeruginosa strain K900, that was not the case with the XDR P. aeruginosa strain CDC1270. Cefiderocol produced a significant > 3 log10 decrease in colony counts compared with the saline control, a > 2 log10 decrease compared with ciprofloxacin, and a > 1.4 log10 compared with tobramycin. These differences were all significant. In addition, tobramycin 14 mg/ml also significantly decreased CDC1270 colony counts compared with the saline control.
Using a semiquantitative method for determining cefiderocol concentrations, we determined that with aggressive topical treatment, the corneas achieved mean cefiderocol concentrations 25× higher than the MIC100 of the P. aeruginosa keratitis isolates tested in this study. These results demonstrate that high concentrations of cefiderocol can be achieved in corneas in which the corneal epithelium has been largely removed, which is the usual case with patients presenting with P. aeruginosa corneal ulcers.
We generally find no differences between the clinical signs produced among the various treatments in P. aeruginosa keratitis studies. This is because of clinical signs of infection being already present at the Onset of Therapy and the short treatment duration (8 hours). However, during a review of the photographs of the bacterial keratitis studies, one notable clinical finding was observed. Corneal infiltrate areas were smallest in the cefiderocol treated eyes in all experiments suggesting that it is not proinflammatory or antagonistic to healing.
When designing this study, we had a concern about the stability of the cefiderocol solution. The product insert for FETROJA states that reconstituted solution can be stored at room temperature for up to 1 hour in the vial. Furthermore, it is recommended that FETROJA solution in the vial be immediately diluted. Diluted FETROJA was said to be stable for up to 6 hours at room temperature and up to 24 hours when refrigerated and protected from light (FETROJA Product Insert FET-PI-03). Because of these statements, we immediately diluted the FETROJA from the vial to produce the 50 mg/ml cefiderocol solution. This solution was made on the days of the experiments and kept on ice and in foil-covered tubes during the dosing, and all excess was stored in foil-covered tubes in a refrigerator. We chose to assess the stability of the 50 mg/ml cefiderocol solutions using a bioassay to determine activity. We found that there was no loss in antibiotic activity up to 33 days when stored refrigerated and out of light. This is important because patients will be using the drops for several days. Typically, fortified antibiotics have an expiration of 72 hours after preparation. Additional studies investigating the stability of the cefiderocol solutions at other temperature and storage conditions are indicated to mimic the potential storage conditions in the patient setting.
Limitations of the study include only testing P. aeruginosa, whereas keratitis can be caused by a number of bacterial pathogens, and our data cannot speak to cefiderocol’s activity against them. One clear limitation of cefiderocol is its lack of documented efficacy against gram-positive bacteria such as Staphylococcus aureus, which is a frequent cause of keratitis. A longer-term study showing final outcomes would also be helpful. Cefiderocol was well tolerated during this study’s short treatment experiment. Meta-analysis of clinical trials and case reports found good safety profiles for systemic use of cefiderocol, suggesting that it will be well tolerated with topical use.41,42 However, systematic studies of safety for topical treatment are necessary. Although mutations that diminish cefiderocol efficacy occur, resistance remains rare among systemic isolates of P. aeruginosa.43, 44, 45 Studies to evaluate the frequency of resistance development in ocular models are warranted. Penetration of antibiotics into the cornea can be a barrier for antibiotic efficacy,35,46 and although this study demonstrated reductions of bacteria injected into the cornea, the rabbits were young and work with larger subjects may help to address this issue. Nevertheless, this study demonstrates that topical cefiderocol is effective for treatment of P. aeruginosa in an animal model that is predictive of patient efficacy. This was true for a nonantibiotic resistant strain and for an XDR P. aeruginosa isolate from the recent outbreak. Our results suggest that further development of cefiderocol for use as a topical ophthalmic drop for treatment of XDR P. aeruginosa keratitis is warranted.
Manuscript no. XOPS-D-23-00215R2.
Footnotes
Supplemental material available atwww.ophthalmologyscience.org.
Disclosure(s):
All authors have completed and submitted the ICMJE disclosures form.
The author(s) have made the following disclosures:
E.G.R.: Grant – Microbiotix, Oyster Point Pharma, Okogen, AiCuris Anti-infective Cures, Stowe Pharmaceuticals, Asepticys, Inc., Alcon Laboratories, American Genomics, Department of Defense VR200112, NEI R01 EY032517 (Shanks, PI), TRB Chemedica Internationale SA; Consultant – Invirsa, Inc.
M.E.Z.: Grant – Department of Surgery Faculty research award, 2022-23; Advisory board – DETECT Study – NEI, ZEDS Study- NEI
R.M.Q.S.: Honoraria – Loyola Medical School, Wayne State Medical School; Patent – US8609110 - Citrobacter freundii antibacterial agents and their use, 11529389 - Delivering Biological Drugs to Tissues; Advisory board – University of Pittsburgh IBC Committee; Other – Equity in AnkyrBio, LLC.
The other authors have no proprietary or commercial interest in any materials discussed in this article.
Funded by the Charles T. Campbell Ophthalmic Microbiology Laboratory, The Campbell Family Foundation, National Institutes of Health grants R01EY027331 (to R.M.Q.S.), and CORE Grant P30 EY08098 to the University of Pittsburgh Department of Ophthalmology. The Eye and Ear Foundation of Pittsburgh and from an unrestricted grant from Research to Prevent Blindness, New York, NY provided additional departmental funding.
No human subjects were included in this study.
ANIMAL SUBJECTS: Animal subjects were included in this study. These studies conformed to the ARVO Statement on the Use of Animals in Ophthalmic and Vision Research and were approved by the University of Pittsburgh’s Institutional Animal Care and Use Committee (IACUC Protocol 23053154).
Author Contributions:
Conception and design: Romanowski, Zegans, R.M.Q. Shanks
Analysis and interpretation: Romanowski, Mumper, H.Q. Shanks, Zegans, R.M.Q. Shanks
Data collection: Romanowski, Mumper, H.Q. Shanks, Yates, Mandell, R.M.Q. Shanks
Obtained funding: R.M.Q. Shanks, Romanowski
Overall responsibility: Romanowski, Mumper, H.Q. Shanks, Yates, Mandell, Zegans, R.M.Q. Shanks
Supplementary Data
References
- 1.Centers for Disease Control and Prevention Outbreak of Extensively Drug-resistant Pseudomonas aeruginosa Associated with Artificial Tears. 2023. https://www.cdc.gov/hai/outbreaks/crpa-artificial-tears.html
- 2.Morelli M.K., Kloosterboer A., Fulton S.A., et al. Investigating and treating a corneal ulcer due to extensively drug-resistant Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2023;67 doi: 10.1128/aac.00277-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shoji M.K., Gutkind N.E., Meyer B.I., et al. Multidrug-resistant Pseudomonas aeruginosa keratitis associated with artificial tear use. JAMA Ophthalmol. 2023;141:499–500. doi: 10.1001/jamaophthalmol.2023.1109. [DOI] [PubMed] [Google Scholar]
- 4.Velcani F., Kuo I.C., Shanks R.M.Q., et al. Association of artificial tears with ocular and systemic infection: carbapenem-resistant Pseudomonas aeruginosa (VIM-GES-CRPA) outbreak. Ophthalmology. 2023;130:1118–1120. doi: 10.1016/j.ophtha.2023.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Magiorakos A.P., Srinivasan A., Carey R.B., et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012;18:268–281. doi: 10.1111/j.1469-0691.2011.03570.x. [DOI] [PubMed] [Google Scholar]
- 6.Sundermann A.J., Srinivasa V.R., Mills E.G., et al. Two artificial tears outbreak-associated cases of extensively drug-resistant pseudomonas aeruginosa detected through whole genome sequencing-based surveillance. J Infect Dis. 2023 doi: 10.1093/infdis/jiad318. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Salam M.A., Al-Amin M.Y., Salam M.T., et al. Antimicrobial resistance: a growing serious threat for global public health. Healthcare (Basel) 2023;11:1946. doi: 10.3390/healthcare11131946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hilliam Y., Kaye S., Winstanley C. Pseudomonas aeruginosa and microbial keratitis. J Med Microbiol. 2020;69:3–13. doi: 10.1099/jmm.0.001110. [DOI] [PubMed] [Google Scholar]
- 9.Pachigolla G., Blomquist P., Cavanagh H.D. Microbial keratitis pathogens and antibiotic susceptibilities: a 5-year review of cases at an urban county hospital in north Texas. Eye Contact Lens. 2007;33:45–49. doi: 10.1097/01.icl.0000234002.88643.d0. [DOI] [PubMed] [Google Scholar]
- 10.Vazirani J., Wurity S., Ali M.H. Multidrug-resistant Pseudomonas aeruginosa keratitis: risk factors, clinical characteristics, and outcomes. Ophthalmology. 2015;122:2110–2114. doi: 10.1016/j.ophtha.2015.06.007. [DOI] [PubMed] [Google Scholar]
- 11.Bispo P.J.M., Sahm D.F., Asbell P.A. A systematic review of multi-decade antibiotic resistance data for ocular bacterial pathogens in the United States. Ophthalmol Ther. 2022;11:503–520. doi: 10.1007/s40123-021-00449-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thomas R.K., Melton R., Vollmer P.M., Asbell P.A. In vitro antibiotic resistance among bacteria from the cornea in the antibiotic resistance monitoring in ocular microorganisms surveillance study. Optom Vis Sci. 2021;98:1113–1121. doi: 10.1097/OPX.0000000000001768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shah S., Wozniak R.A.F. Staphylococcus aureus and Pseudomonas aeruginosa infectious keratitis: key bacterial mechanisms that mediate pathogenesis and emerging therapeutics. Front Cell Infect Microbiol. 2023;13 doi: 10.3389/fcimb.2023.1250257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shekhawat N.S., Hall L.N., Sulewski M.E., Jr., et al. Corneal culture and antibiotic susceptibility results for microbial keratitis in the mid-Atlantic region of the United States, 2016 to 2020. Eye Contact Lens. 2023;49:267–274. doi: 10.1097/ICL.0000000000000993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mediero S., Boto de Los Bueis A., Spiess K., et al. Clinical and microbiological profile of infectious keratitis in an area of Madrid, Spain. Enferm Infecc Microbiol Clin (Engl Ed) 2018;36:409–416. doi: 10.1016/j.eimc.2017.08.002. [DOI] [PubMed] [Google Scholar]
- 16.Daley J.R., Lee M.K., Wang X., et al. Epidemiology and economic cost analysis of microbial keratitis from a Tertiary Referral Hospital in Australia. Pathogens. 2023;12:413. doi: 10.3390/pathogens12030413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Joseph J., Karoliya R., Sheba E., et al. Trends in the microbiological spectrum of nonviral keratitis at a Single Tertiary Care Ophthalmic Hospital in India: a review of 30 years. Cornea. 2023;42:837–846. doi: 10.1097/ICO.0000000000003105. [DOI] [PubMed] [Google Scholar]
- 18.Fernandes M., Vira D., Medikonda R., Kumar N. Extensively and pan-drug resistant Pseudomonas aeruginosa keratitis: clinical features, risk factors, and outcome. Graefes Arch Clin Exp Ophthalmol. 2016;254:315–322. doi: 10.1007/s00417-015-3208-7. [DOI] [PubMed] [Google Scholar]
- 19.Kim S.J., Toma H.S. Antimicrobial resistance and ophthalmic antibiotics: 1-year results of a longitudinal controlled study of patients undergoing intravitreal injections. Arch Ophthalmol. 2011;129:1180–1188. doi: 10.1001/archophthalmol.2011.213. [DOI] [PubMed] [Google Scholar]
- 20.Choi J.J., McCarthy M.W. Cefiderocol: a novel siderophore cephalosporin. Expert Opin Investig Drugs. 2018;27:193–197. doi: 10.1080/13543784.2018.1426745. [DOI] [PubMed] [Google Scholar]
- 21.Domingues S., Lima T., Saavedra M.J., Da Silva G.J. An overview of cefiderocol’s therapeutic potential and underlying resistance mechanisms. Life (Basel) 2023;13:1427. doi: 10.3390/life13071427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tonziello G., Caraffa E., Pinchera B., et al. Present and future of siderophore-based therapeutic and diagnostic approaches in infectious diseases. Infect Dis Rep. 2019;11:8208. doi: 10.4081/idr.2019.8208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Naseer S., Weinstein E.A., Rubin D.B., et al. US Food and Drug Administration (FDA): benefit-risk considerations for cefiderocol (Fetroja®) Clin Infect Dis. 2021;72:e1103–e1111. doi: 10.1093/cid/ciaa1799. [DOI] [PubMed] [Google Scholar]
- 24.Brothers K.M., Kowalski R.P., Tian S., et al. Bacteria induce autophagy in a human ocular surface cell line. Exp Eye Res. 2018;168:12–18. doi: 10.1016/j.exer.2017.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kowalski R.P., Romanowski E.G., Mah F.S., et al. Topical levofloxacin 1.5% overcomes in vitro resistance in rabbit keratitis models. Acta Ophthalmol. 2010;88:e120–e125. doi: 10.1111/j.1755-3768.2010.01897.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Brothers K.M., Callaghan J.D., Stella N.A., et al. Blowing epithelial cell bubbles with GumB: ShlA-family pore-forming toxins induce blebbing and rapid cellular death in corneal epithelial cells. PLOS Pathog. 2019;15 doi: 10.1371/journal.ppat.1007825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Harshaw N.S., Stella N.A., Lehner K.M., et al. Antibiotics used in empiric treatment of ocular infections trigger the bacterial Rcs stress response system independent of antibiotic susceptibility. Antibiotics (Basel) 2021;10:1033. doi: 10.3390/antibiotics10091033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Simner P.J., Patel R. Cefiderocol antimicrobial susceptibility testing considerations: the Achilles’ heel of the Trojan horse? J Clin Microbiol. 2020;59 doi: 10.1128/JCM.00951-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Altmann S., Emanuel A., Toomey M., et al. A quantitative rabbit model of vaccinia keratitis. Invest Ophthalmol Vis Sci. 2010;51:4531–4540. doi: 10.1167/iovs.09-5106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kowalski R.P., Romanowski E.G., Yates K.A., Gordon Y.J. Lomefloxacin is an effective treatment of experimental bacterial keratitis. Cornea. 2001;20:306–308. doi: 10.1097/00003226-200104000-00013. [DOI] [PubMed] [Google Scholar]
- 31.Mah F.S., Romanowski E.G., Kowalski R.P., et al. Zymar (gatifloxacin 0.3%) shows excellent Gram-negative activity against Serratia marcescens and Pseudomonas aeruginosa in a New Zealand White rabbit keratitis model. Cornea. 2007;26:585–588. doi: 10.1097/ICO.0b013e318033a6f2. [DOI] [PubMed] [Google Scholar]
- 32.Rezaei S., Steen D., Amin S. Successful treatment of an extensively drug-resistant pseudomonal ulcer associated with contaminated artificial tears. Am J Ophthalmol Case Rep. 2023;32 doi: 10.1016/j.ajoc.2023.101909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Maticorena-Quevedo J., Patiño-Valderrama L., Arellano-Caro K. Use of topical colistin in bacterial keratitis caused by extensively drug-resistant Pseudomonas aeruginosa: a case report. Arq Bras Oftalmol. 2023;86:384–387. doi: 10.5935/0004-2749.20230039. [DOI] [PubMed] [Google Scholar]
- 34.Humphries R.M. Updated Aminoglycoside Breakpoints for Enterobacterales and Pseudomonas aeruginosa. Clinical and Laboratory Standards Institute; Wayne, PA: 2023. AST News Update June 2023: New! CLSI M100-Ed33. v. 2023. [Google Scholar]
- 35.Kowalski R.P., Romanowski E.G., Yates K.A., et al. Is there a role for topical penicillin treatment of Staphylococcus aureus keratitis based on elevated corneal concentrations? J Clin Ophthal Optom. 2018;2:103. [Google Scholar]
- 36.Romanowski E.G., Mah F.S., Yates K.A., et al. The successful treatment of gatifloxacin-resistant Staphylococcus aureus keratitis with Zymar (gatifloxacin 0.3%) in a NZW rabbit model. Am J Ophthalmol. 2005;139:867–877. doi: 10.1016/j.ajo.2005.01.021. [DOI] [PubMed] [Google Scholar]
- 37.Ito A., Kohira N., Bouchillon S.K., et al. In vitro antimicrobial activity of S-649266, a catechol-substituted siderophore cephalosporin, when tested against non-fermenting Gram-negative bacteria. J Antimicrob Chemother. 2016;71:670–677. doi: 10.1093/jac/dkv402. [DOI] [PubMed] [Google Scholar]
- 38.Ito A., Sato T., Ota M., et al. In vitro antibacterial properties of cefiderocol, a novel siderophore cephalosporin, against Gram-negative bacteria. Antimicrob Agents Chemother. 2018;62 doi: 10.1128/AAC.01454-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wilhelmus K.R., Abshire R.L. Corneal ciprofloxacin precipitation during bacterial keratitis. Am J Ophthalmol. 2003;136:1032–1037. doi: 10.1016/s0002-9394(03)00636-6. [DOI] [PubMed] [Google Scholar]
- 40.Lin J.M., Tsai Y.Y., Fu Y.L. The fixed combination of fortified vancomycin and amikacin ophthalmic solution—VA solution: in vitro study of the potency and stability. Cornea. 2005;24:717–721. doi: 10.1097/01.ico.0000154231.10994.6d. [DOI] [PubMed] [Google Scholar]
- 41.Lin M.H., Shen Y.C., Cheng H.Y., et al. Comparative efficacy and safety of non-polymyxin antibiotics against nosocomial pneumonia, complicated intra-abdominal infection, or complicated urinary tract infection: a network meta-analysis of randomised clinical trials. J Glob Antimicrob Resist. 2023;34:46–58. doi: 10.1016/j.jgar.2023.05.011. [DOI] [PubMed] [Google Scholar]
- 42.Sansone P., Giaccari L.G., Coppolino F., et al. Cefiderocol for carbapenem-resistant bacteria: handle with care! A review of the real-world evidence. Antibiotics (Basel) 2022;11:904. doi: 10.3390/antibiotics11070904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Malisova L., Vrbova I., Pomorska K., et al. In vitro activity of cefiderocol against carbapenem-resistant Enterobacterales and Pseudomonas aeruginosa. Microb Drug Resist. 2023;29:485–491. doi: 10.1089/mdr.2023.0090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Shields R.K., Kline E.G., Squires K.M., et al. In vitro activity of cefiderocol against Pseudomonas aeruginosa demonstrating evolved resistance to novel beta-lactam/beta-lactamase inhibitors. JAC Antimicrob Resist. 2023;5:dlad107. doi: 10.1093/jacamr/dlad107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Karakonstantis S., Rousaki M., Vassilopoulou L., Kritsotakis E.I. Global prevalence of cefiderocol non-susceptibility in Enterobacterales, Pseudomonas aeruginosa, Acinetobacter baumannii, and Stenotrophomonas maltophilia: a systematic review and meta-analysis. Clin Microbiol Infect. 2024;30:178–188. doi: 10.1016/j.cmi.2023.08.029. [DOI] [PubMed] [Google Scholar]
- 46.Diamond J.P., White L., Leeming J.P., et al. Topical 0.3% ciprofloxacin, norfloxacin, and ofloxacin in treatment of bacterial keratitis: a new method for comparative evaluation of ocular drug penetration. Br J Ophthalmol. 1995;79:606–609. doi: 10.1136/bjo.79.6.606. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.