Abstract
Introduction and importance
Longitudinal vaginal septum is usually associated with uterine anomalies, such as septate uterus and didelphys uterus. Normal uterus and cervix found in longitudinal vaginal septum is a rare case but can affect sexual activities and reproductive outcomes.
Case presentation
We present a case of a 42-year-old woman with a history of primary infertility for 7 years was referred by the endocrinology division due to the presence of a longitudinal vaginal septum and difficulty in performing intrauterine insemination. Transvaginal ultrasound revealed a normal-shaped and sized uterus. The cervix appeared normal as well and was located 6.27 cm from the vaginal introitus.
Clinical discussion
Incomplete vaginal septum in normal uterus and cervix is very rare, mostly it's associated with partial or complete duplication of the Mullerian ducts. Surgical correction of this condition is necessary for reproductive constraints and patient complaints.
Conclusion
This case is very rare and is associated with the pathophysiology of the vaginal septum It is important to establish a diagnosis for this malformation as surgical intervention generally provide satisfactory outcomes.
Keywords: Case report, Longitudinal vaginal septum, Normal uterus
Highlights
-
•
Longitudinal vaginal septum is mostly found in women with septate uterus during routine examinations or childbirth.
-
•
The vaginal septum can be obstructive, communicative, or non-obstructive.
-
•
Obstructive and communicative can cause symptoms while a non-obstructive septum doesn't.
-
•
Incomplete longitudinal vaginal septum is often associated with duplication of the Mullerian ducts.
1. Introduction
The development of the female genital tract is a complex process that involves various stages of cellular differentiation, migration, fusion, and canalization. If any of these stages fail, it can lead to congenital anomalies. Problems with the hymen and vagina can affect menstruation, sexual activity, fertility, or childbirth. These issues usually arise after puberty, but some infants may have them from birth. Müllerian duct anomalies occur due to the underdevelopment, defects, or failure of resorption of the paramesonephric (Müllerian) ducts. The prevalence of female genital anomalies is around 4–7 % in the general population and as high as 8–10 % in women with recurrent miscarriages. The incidence of Müllerian duct anomalies is approximately 1 % in the general population and around 3 % in patients with infertility [1].
The prevalence of Müllerian duct anomalies is challenging to ascertain as many are unidentified, especially if they do not exhibit symptoms. In a study, it was found that among 5590 women with renal anomalies, 29 % of them had Müllerian anomalies [2]. In a well-designed study involving nearly 700 patients with normal reproductive outcomes, who were evaluated through laparoscopy or laparotomy before tubal ligation and then underwent hysterosalpingography five months after sterilization, the prevalence of congenital uterine anomalies is 3.2 % [3]. In another study, the prevalence of Müllerian duct anomalies was 5 to 10 % among patients with recurrent miscarriages in the first trimester and over 25 % among those experiencing miscarriages in the first to second trimesters/premature birth [4]. The prevalence of Müllerian duct anomalies in patients with primary infertility does not increase and is approximately the same as in fertile patients with normal reproductive outcomes [5].
The female genital tract begins developing in the third week of embryogenesis and continues until the second trimester of pregnancy. Some important steps are: (i) Gonadal development occurs independently of the reproductive tract. Hence, females with uterovaginal anomalies may have normal ovaries and hormone production. (ii) Reproductive tract formation is closely related to the development of the urinary system, and genital tract abnormalities are often associated with kidney, ureter, or bladder abnormalities. (iii) Disruption of normal embryological processes in the Müllerian ducts leads to the development of various congenital anomalies in the female reproductive tract [6].
Vaginal anomalies are rare with vaginal agenesis occurring in approximately 1 in 5000 live-born females. Longitudinal vaginal septum is usually associated with uterine anomalies such as septate uterus and didelphys uterus which was shown in (Fig. 1) [7,8] and can be either partial or complete.
Fig. 1.

Septate uterus and didelphys uterus (Heinonen, 2006) [9].
Patients with vaginal septum may have persistent bleeding, septum tear during tampon placement or sex, and/or dyspareunia. The vaginal septum can be seen as a fibrous structure dividing the vagina into two, and a one-finger internal examination is helpful in diagnosis. A narrow speculum may be used.
Imaging of the upper reproductive tract is important to determine if there is one or two uterine structures and cervices which can be achieved using ultrasound or MRI for this. Surgery is not needed for asymptomatic patients with a longitudinal vaginal septum, but can help with vaginal delivery.
Longitudinal vaginal septum is commonly found in women with a septate uterus [8]. It is often asymptomatic and detected during routine examinations or childbirth. It can cause dystocia, dyspareunia, or vaginal hygiene issues. Some patients may also experience unilateral vaginal obstruction and ipsilateral renal agenesis, and endometriosis (38 %) is more common in these patients [10].
2. Methods
Method of this study is observational study by observing one patient since the beginning until the end of the surgical therapy. This study has been reported in line with the SCARE criteria [11].
3. Case presentation
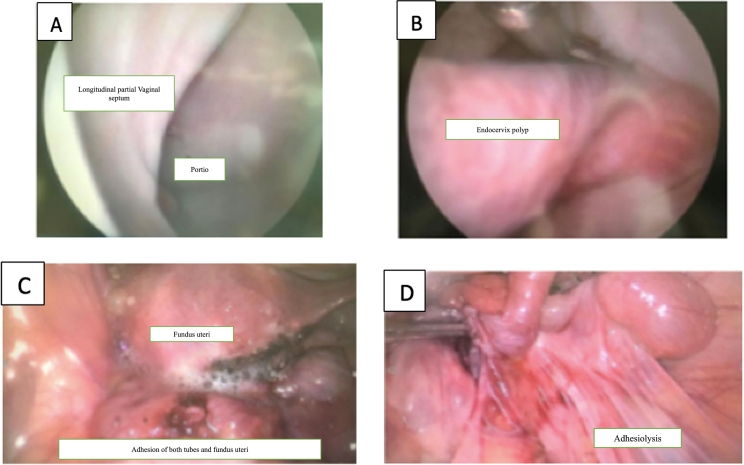
A 42-year-old woman with a history of primary infertility for 7 years was referred by the endocrinology division due to the presence of a longitudinal vaginal septum and difficulty in performing intrauterine insemination. There was no family history of genitourinary malformations. The patient had menarche at the age of 11 and had no complaints of menstruation or menstrual pain. The patient had been married for 7 years but had not conceived and her husband reported a sensation of resistance during sexual intercourse. The patient underwent Laparoscopic for adhesiolysis, and polypectomy 7 months ago, revealing a partial longitudinal vaginal septum, endocervical polyp, and internal genitalia adhesions with both patent fallopian tubes during Laparoscopic (Fig. 2). After the adhesiolysis and polypectomy were done, patient then referred to Dr. Cipto Mangunkusumo hospital for septum resection.
Fig. 2.
Patient's findings through Laparoscopic while undergoing adhesiolysis, and polypectomy.
On physical examination at Dr. Cipto Mangunkusumo Hospital, a septum could be palpated in the 12 o'clock to 6 o'clock position on the right side, shaped like a crescent measuring 2 × 2 cm, covering a portion of the right side of the cervix (Fig. 3).
Fig. 3.

Vaginal septum of the patient found in physical examination.
Transvaginal ultrasound revealed a normal-shaped and sized uterus, with no abnormalities observed in both ovaries. Transperineal ultrasound showed a hematocolpos image in the right vagina with a volume of 4.37 cm3, located 2.99 cm from the vaginal introitus. The cervix appeared normal and was located 6.27 cm from the vaginal introitus as seen on transvaginal (Fig. 4A) and transperineal ultrasound (Fig. 4B). There's no abnormality found in kidney ultrasound. Both kidneys are within normal limits (Fig. 5).
Fig. 4.
Transvaginal and transperineal ultrasound evaluation.
Fig. 5.
Kidney ultrasound.
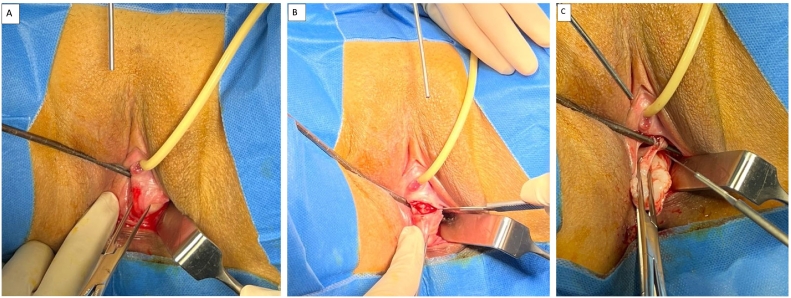
Patient underwent septal resection and purulent secretions were observed at Cipto Mangunkusumo Hospital. The detailed steps about the septum resection are as follows: at first the operator identified the longitudinal septum on the right side of the vagina (Fig. 6A). Then, using a uterus sondage, they measured the width of the septum, which was found to be 2.5 cm (Fig. 6B). After figuring and measured the septum, the next step is to performed Hydro-dissection on the incomplete longitudinal vaginal septum (Fig. 6C).
Fig. 6.
Identifying septum's border and performed hydro-dissection.
The septum's border must be identified on anterior, posterior right and left lateral body (Fig. 7A) and excise the anterior vaginal septum using the sondage as guidance (Fig. 7B, C).
Fig. 7.
Identifying septum's border and excised.
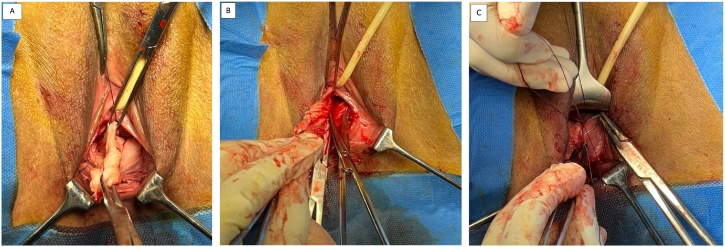
Excision was then continued to the posterior vaginal septum (Fig. 8A, B) and finished with a continuous suture using PGA 2.0 (Fig. 8C).
Fig. 8.
Excised from posterior and finished suturing.
After the resection was done, the final view of patient vagina was observed, the vagina was reconstructed back to its normal shape (Fig. 9) and the septum was released (Fig. 10).
Fig. 9.
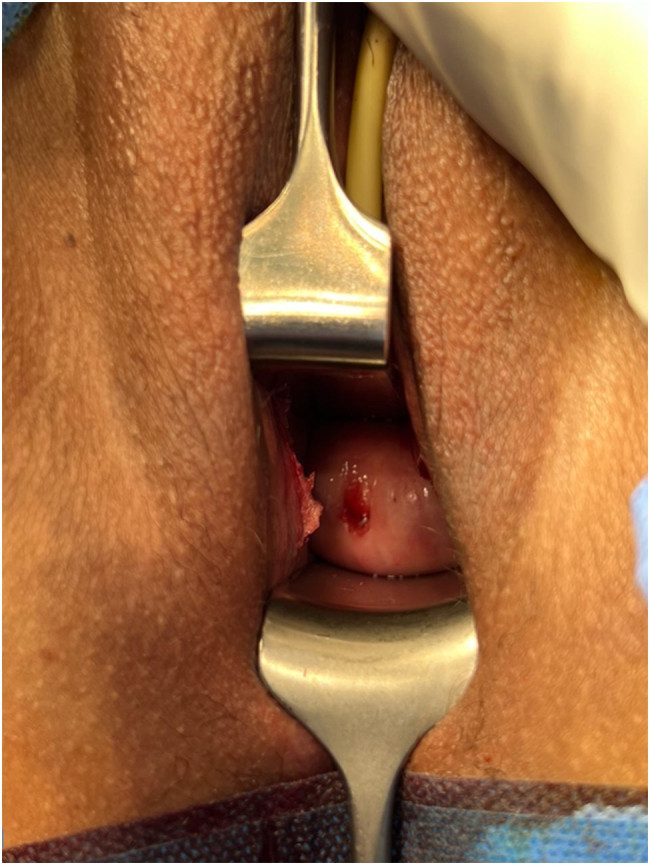
Final view after resection and vaginal reconstruction.
Fig. 10.

Specimen of vaginal septum.
4. Discussion
A patient with an incomplete longitudinal vaginal septum found in a normal uterus and cervix is very rare. An incomplete longitudinal vaginal septum is often associated with partial or complete duplication of the Mullerian ducts resulting from incomplete fusion of the Mullerian ducts. The vaginal septum can be obstructive, communicative, or non-obstructive. Obstruction and communication can cause symptoms such as dysmenorrhea, lower abdominal pain, and intermenstrual bleeding, while a non-obstructive septum generally does not cause complaints [12].
A unique case in this patient is that the vaginal septum was found during physical examination with no evidence of uterus and cervix abnormalities which confirmed by transperineal and transvaginal ultrasound. Patient also undergoes polypectomy and adhesiolysis, during the laparoscopic there is no evidence of uterus and cervix abnormalities. This is a rare case but can be associated with partial or complete duplication of the Mullerian ducts which can cause incomplete fusion of Mullerian ducts while the cervix and uterus growth normally during embryogenesis.
Vaginal septum might cause some symptoms especially in patients with complete vaginal septum. This patient septum was found due to difficulties of insemination device to enter, but no symptoms during her life time such as dysmenorrhea, lower abdominal pain, and the patient still had regular menstruation. The only complaints are infertility and the patient's husband reported resistance sensation during sexual intercourse. Since there are obstructive and non-obstructive vaginal septum, this patient had non-obstructive vaginal septum due to no menstrual complaints. By the physical examination it also palpable and can be seen through inspeculo that the vaginal septum was found and the cervix can be seen. However, the size of the narrowing caused by a non-obstructive septum can lead to pain and difficulty in visualizing the cervix during physical examination. Surgical correction of this condition is necessary for reproductive constraints and patient complaints.
Several surgical techniques have been described for the resection of non-obstructive vaginal septum. The classical approach involves using scissors after clamping the septum with two Kelly or Kocher clamps to prevent blood loss, followed by haemostasis suturing using absorbable 3-0 sutures [13].
It is important for OBGYN to find any anatomy abnormalities or hormonal disorder that causes infertility in patients. The examination through ultrasound is also important to find any abnormalities in uterus or cervix even-though there are no symptoms that led to uterus or cervix abnormalities. This can help OBGYN to decide which sub-department to refer the patient for more advance treatment. Septum resection surgical technique also needs to be studied and understand, any size of septum must be released in order to the help patient to have a better reproductive system and help increase the quality of sexual activity.
To summarize, this particular case is quite uncommon and is linked to the pathophysiology of the vaginal septum, which is caused by partial or complete duplication of the Mullerian ducts. This occurs due to incomplete fusion of the Mullerian ducts. It is crucial to diagnose this malformation, particularly when the patient is under anaesthesia. Follow-up with patients after surgery to monitor reproductive outcomes is important. Post-surgery results often improve menstrual and sexual activities.
Ethical approval
The Ethics Committee of the Faculty of Medicine-University of Indonesia-Cipto Mangunkusumo Hospital with regards of the protection of human rights and welfare in medical research entitled: “Longitudinal Vaginal Septum With Normal Uterus And Cervix: A Case Report”.
Protocol number: 23-09-1393.
Principal investigator: Surahman Hakim, OBGYN(C)-MPH.
Name of the institution: Obstetrics and Gynaecology Department, Faculty of Medicine-Cipto Mangunkusumo Hospital.
Date Approval: 25th September 2023 (valid for 1 year).
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contribution
Surahman Hakim: Operator of the operation, study concept, data collection.
Fernandi Moegni: Data collection, Ultrasonography operator of the patient.
I Gede Manu Mahendra: Operation assistant, data analysis, paper writing.
Gracia Natalia Theresia: paper writing, paper editor, others.
Guarantor
The Guarantor of this case report is Surahman Hakim, OBGYN (C)-MPH as our first author/principal investigator.
Research registration number
None.
Conflicts of interest
The authors declare that they have no conflict of interest.
References
- 1.Dwivedi D., Jain M., Jain S., Jain S. A rare case report on complete cervical agenesis with vaginal atresia and suspended didelphys uterus with hematometra and left haematosalpinx. Int. J. Reprod. Contracept. Obstet. Gynecol. 2020;9(3):1274–1278. [Google Scholar]
- 2.O’Brien K.L.F., Bhatia V., Homafar M., Gong Y.Y., Winsten M.T., Gerber J., et al. The prevalence of Müllerian anomalies in women with a diagnosed renal anomaly. J. Pediatr. Adolesc. Gynecol. 2021;34(2):154–160. doi: 10.1016/j.jpag.2020.11.015. [DOI] [PubMed] [Google Scholar]
- 3.Simón C., Martinez L., Pardo F., Tortajada M., Pellicer A. Müllerian defects in women with normal reproductive outcome. Int. J. Fertil. Steril. 1991;56(6):1192–1193. doi: 10.1016/s0015-0282(16)54741-4. [DOI] [PubMed] [Google Scholar]
- 4.Acien P. Incidence of Müllerian defects in fertile and infertile women. Hum. Reprod. 1997;12(7):1372–1376. doi: 10.1093/oxfordjournals.humrep.a019588. [DOI] [PubMed] [Google Scholar]
- 5.Grimbizis G.F., Camus M., Tarlatzis B.C., Bontis J.N., Devroey P. Clinical implications of uterine malformations and hysteroscopic treatment results. Hum. Reprod. 2001;7(2):161–174. doi: 10.1093/humupd/7.2.161. [DOI] [PubMed] [Google Scholar]
- 6.Herlin M., Bjørn A.-M.B., Rasmussen M., Trolle B., Petersen M.B. Prevalence and patient characteristics of Mayer–Rokitansky–Küster–Hauser syndrome: a nationwide registry-based study. Hum. Reprod. 2016;31(10):2384–2390. doi: 10.1093/humrep/dew220. [DOI] [PubMed] [Google Scholar]
- 7.Louden E.D., Awonuga A.O., Gago L.A., Singh M. Rare Müllerian anomaly: complete septate uterus with simultaneous longitudinal and transverse vaginal septa. J. Pediatr. Adolesc. Gynecol. 2015;28(6):e189–e191. doi: 10.1016/j.jpag.2015.04.012. [DOI] [PubMed] [Google Scholar]
- 8.Haddad B., Louis-Sylvestre C., Poitout P., Paniel B.-J. Longitudinal vaginal septum: a retrospective study of 202 cases. Eur. J. Obstet. Gynecol. Reprod. Biol. 1997;74(2):197–199. doi: 10.1016/s0301-2115(97)00105-x. [DOI] [PubMed] [Google Scholar]
- 9.Heinonen P.K. Complete septate uterus with longitudinal vaginal septum. Int. J. Fertil. Steril. 2006;85(3):700–705. doi: 10.1016/j.fertnstert.2005.08.039. [DOI] [PubMed] [Google Scholar]
- 10.Candiani G., Fedele L., Candiani M. Double uterus, blind hemivagina, and ipsilateral renal agenesis: 36 cases and long-term follow-up. Obstet. Gynecol. 1997;90(1):26–33. doi: 10.1016/S0029-7844(97)83836-7. [DOI] [PubMed] [Google Scholar]
- 11.Sohrabi C., Mathew G., Maria N., Kerwan A., Franchi T., Agha R.A. The SCARE 2023 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. Lond. Engl. 2023;109(5):1136. doi: 10.1097/JS9.0000000000000373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Miller R.J., Breech L.L. Surgical correction of vaginal anomalies. Clin. Obstet. Gynecol. 2008;51:223. doi: 10.1097/GRF.0b013e31816d2181. [DOI] [PubMed] [Google Scholar]
- 13.Montevecchi L., Valle R.F. Resectoscopic treatment of complete longitudinal vaginal septum. Int. J. Gynaecol. Obstet. 2004;84:65. doi: 10.1016/j.ijgo.2003.08.010. [DOI] [PubMed] [Google Scholar]