Abstract
Introduction and importance
Cystic adventitial disease (CAD) is a rare vascular disorder marked by occlusion stemming from the development of a cystic mass within the outer (subadventitial) layer, with a predominant impact on the popliteal artery. The significance of the case presented herein lies in shedding light on a distinct clinical manifestation involving a 40-year-old man who exhibited sporadic calf claudication during ambulation. This instance contributes to the broader understanding of CAD and its diverse clinical presentations, emphasizing the need for further exploration and awareness within the medical community.
Case presentation
A 40-year-old man, with no significant past medical history, was referred to the cardiovascular department for the evaluation of a new onset of left calf pain persisting over the past three months. An arterial lower limb Doppler ultrasound was performed, revealing a focal hypoechoic image around the popliteal artery with a regular arterial wall, indicative of extrinsic compression. This resulted in significant stenosis of the popliteal artery during plantar flexion of the foot. The diagnosis of CAD of the left popliteal artery was established after limb computed tomography angiography, and a complete resection of the cyst was scheduled. The postoperative course was uneventful, with the patient experiencing relief from left calf claudication.
Clinical discussion
CAD is an uncommon vascular anomaly, representing merely 0.1 % of all vascular conditions. This condition predominantly afflicts men aged between 40 and 50 years old. The etiology of CAD remains a subject of debate, with pathological findings typically involving intramural cysts containing gelatinous material between the media and the adventitia. Surgical intervention becomes necessary when symptoms arise.
Conclusion
CAD of the popliteal artery, though rare, is a significant contributor to peripheral vascular insufficiency in young patients without typical atherosclerotic risk factors.
Keywords: Cystic adventitial disease, Adventitia, Computed tomography angiography, Pathology, Popliteal artery
Highlights
-
•
Cystic adventitial disease in the popliteal artery is very rare and an uncommon occurrence. It is often underdiagnosed due to its low prevalence.
-
•
It poses diagnostic challenges particularly in the popliteal artery. Magnetic resonance imagering is the gold standard for diagnosis and surgical management contributing to improving diagnostic accuracy.
-
•
The management approach for adventitial cystic disease depends on the vascular condition.
1. Introduction
Cystic adventitial disease (CAD) is a rare non-atherosclerotic vascular anomaly, accounting for 0.1 % of all vascular diseases [1]. It is characterized by arterial occlusion resulting from the formation of a cystic mass within the outer (subadventitial) layer, predominantly affecting the popliteal artery in 85 % of cases, leading to symptoms indicative of lower extremity claudication [1]. Although physical examination often yields normal findings, observations may include the presence of a popliteal bruit and/or diminished distal pulses during knee flexion. Diagnosis is substantiated through imaging modalities such as ultrasound examination, computed tomography (CT) scans, magnetic resonance imaging (MRI), and angiography [2]. Treatment options encompass surgical intervention, percutaneous aspiration, and ongoing surveillance [3]. Herein, we describe the case of a 40-year-old man who experienced sporadic calf claudication while walking.
2. Case presentation
A 40-year-old man was referred to the cardiovascular department for evaluation of a new onset of left calf pain persisting over the past three months. The discomfort initiated during walking short distances and alleviated upon rest. Interrogation revealed no significant past medical history or history of trauma. Physical examination indicated the absence of skin discoloration or swelling, and bilateral palpable femoral, popliteal, and posterior tibial pulses were discerned. An arterial lower limb Doppler ultrasound was performed, revealing a focal hypoechoic image around the popliteal artery with a regular arterial wall. This appearance was indicative of extrinsic compression, resulting in significant stenosis of the popliteal artery during plantar flexion of the foot. Velocity measurements indicated accelerated flow (peak systolic velocity = 400 cm/s) with pronounced damping downstream. Additionally, the popliteal vein appeared mildly dilated over a short segment without associated thrombosis (Fig. 1). The diagnosis of CAD has been established. A lower limb computed tomography angiography (CTA) was subsequently performed, revealing an estimated caliber discrepancy of approximately 25 %, with visualization of an intraparietal arterial formation exhibiting liquid density spanning a height of approximately 30 mm. The leg arteries demonstrated patent lumens with homogeneous opacification visualized distally (Fig. 2). The diagnosis of CAD of the left popliteal artery was established, and surgical intervention was scheduled.
Fig. 1.

Doppler ultrasound revealing a focal hypoechoic image around the popliteal artery with a regular arterial wall. Velocity measurements indicated accelerated flow (peak systolic velocity = 400 cm/s) with pronounced damping downstream. Additionally, the popliteal vein appeared mildly dilated over a short segment without associated thrombosis.
Fig. 2.

A lower limb computed tomography angiography showing an estimated caliber discrepancy of approximately 25 % (arrow), with visualization of an intraparietal cyst formation exhibiting liquid density spanning a height of approximately 30 mm. The leg arteries demonstrated patent lumens with homogeneous opacification visualized distally.
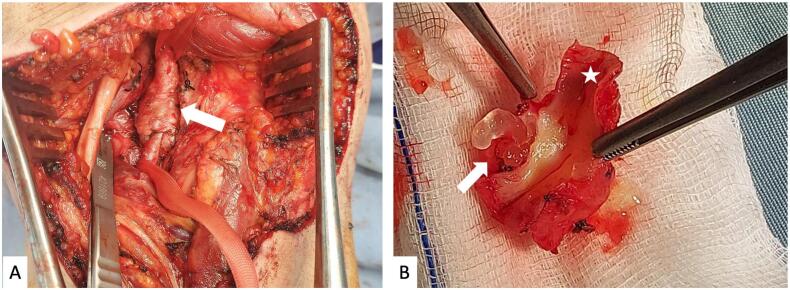
Following dissection, we identified a concentric, circular, and loculated cystic lesion encompassing the popliteal artery (Fig. 3). The cyst exhibited a soft, elastic texture and contained a transparent, gelatinous substance. A complete resection of the cyst was performed as well as the affected segment of the popliteal artery, followed by arterial reconstruction using a great saphenous vein graft. Histopathological examination confirmed the diagnosis of advential cyst revealing a cyst with a relatively clear margin involving vascular adventitia. The cyst with arterial elements in the wall contained mucinous content (Fig. 4). The postoperative course was uneventful, with the patient experiencing relief from left calf claudication. There was no recurrence of the disease, and a follow-up ultrasound examination six months later demonstrated satisfactory patency of the vein graft. The work has been reported in line with the SCARE 2020 criteria [4].
Fig. 3.
A: Per-operatively, a concentric, circular and loculated cystic lesion (arrow) encompassing the popliteal artery was identified. B: After incision of the resected popliteal artery (asterix), a mucoid material between adventitia and intact media (arrow) was identified.
Fig. 4.
HE magnification ×40: Histopathological examination confirmed the diagnosis of advential cyst revealing a cyst with a relatively clear margin involving vascular adventitia. The cyst with arterial elements in the wall, contained mucinous content, without a lining epithelium.
3. Discussion
CAD is an uncommon vascular anomaly, representing merely 0.1 % of all vascular conditions, with its initial documentation by Atkins and Key et al. in 1947 involving the right external iliac artery [5,6]. Since then, over 300 cases have been reported, primarily affecting the popliteal artery unilaterally (85 %), typically manifesting as intermittent claudication [2]. However, bilateral involvement has been documented in five cases, and other arteries, including the external iliac, common femoral, radial, and ulnar arteries, and veins have also been affected [[6], [7], [8]].
This condition predominantly afflicts men aged between 40 and 50 years old [9,10]. Given the relatively young age and low vascular disease risk of the affected population, clinical diagnosis proves challenging. Patients present with intermittent vascular claudication in 81 % of the cases, with a history of trauma reported in only 4 % of those [11]. Some complications reported include intimal tear and arterial thrombosis [12,13]. In our case, the patient had vascular claudication.
The etiology of CAD remains largely elusive. The formation of cysts involves the accumulation of gelatinous mucoid substance situated between the adventitial and medial layers of the artery, resulting in luminal stenosis or occlusion upon enlargement [13]. Typically unilocular, these cysts lack a cellular lining but consist of hyaluronic acid, protein, and proteoglycans, exhibiting biochemical and histological similarities to ganglia [14]. Due to the uncommon occurrence of CAD, the pathogenesis remains incompletely understood and subject to ongoing debate. Four primary hypotheses have been proposed to elucidate the origin:
Cyst development is triggered by the infiltration of synovial fluid from the joint space into the adjacent arterial or venous adventitia [15]. While joint capsule damage may result from trauma, it is postulated that the exudation of synovial fluid contributes to the pathology. Various imaging techniques, such as CT, MRI, and arthrogram of affected joints, have purportedly identified a connection in CAD patients [16]. However, the presence of hyaluronic acid, protein, and proteoglycans in CAD cysts, lacking lubricating properties, suggests a ganglionic origin rather than a synovial one [14].
Adventitial cysts induce arterial lumen compression, appearing as scimitar or “hourglass signs” on angiograms, and may exhibit symptoms even if the affected popliteal artery appears angiographically normal, indicating functional flow obstruction during dynamic exercise. The manifestation of Ishikawa's sign, characterized by the absence of foot pulses upon knee flexion, is indicative of CAD. This serves as a distinguishing feature from popliteal entrapment syndrome, where the pulse diminishes with the contraction of the gastrocnemius during active plantar flexion or passive dorsiflexion of the foot [17].
Pathological findings typically involve intramural cysts containing gelatinous material between the media and the adventitia. The most differential diagnosis of CAS is a ganglion cyst, which is likely attributable to a defect in the joint capsule or tendon sheath, leading to the exudation of joint fluid, protrusion, and encapsulation by fibrous connective tissues resembling other pseudocysts or pseudoaneurysms [18]. In our case, the cyst, in contact with the popliteal artery, exhibited mucinous content with vascular elements in the wall findings.
Various diagnostic modalities are employed, with gray scale Doppler ultrasonography serving as a less invasive routine diagnostic tool, while CT and MRI offer a more detailed assessment of cyst morphology and potential communication with adjacent joints. CT reconstructions and magnetic resonance angiography aid in preoperative planning, while digital subtraction angiography is infrequently used due to its invasive nature. Actually, MRI is the gold standard for diagnosis and surgical management of CAD [19]. Differential diagnosis considerations include popliteal artery entrapment syndrome (PAES) [2,6,20].
The occurrence of spontaneous regression of cysts is infrequent, as evidenced by a mere nine documented instances [8,21]. This atypical outcome implies that, particularly in meticulously monitored cases exhibiting minimal or no pronounced symptoms, the initial course of action should involve conservative medical intervention and ambulatory rehabilitation [22]. The management approach for adventitial cystic disease depends on the vascular condition. Cyst aspiration, while less invasive, carries a high recurrence rate. Evacuation of cyst content while preserving the involved artery proves effective, and resection of the affected vessel segment with vein graft or prosthesis interposition shows promise. Long-term follow-up is essential due to the potential for recurrence or graft occlusion. Endovascular interventional therapy has demonstrated unsatisfactory outcomes [2].
4. Conclusion
In conclusion, CAD of the popliteal artery, though rare and underdiagnosed due to its low prevalence, is a significant contributor to peripheral vascular insufficiency in young patients without typical atherosclerotic risk factors. Therefore, it warrants consideration when assessing cases of intermittent claudication in relatively young individuals.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Ethical approval
The study is exempt from ethical approval in Rabta hospital's institution as all the patient's data were anonymised.
Funding
No.
Author contribution
All the authors read and approved the final version of the manuscript.
Farah Sassi (MD): conception, acquisition of clinical data, literature research, and preparing the manuscript.
Heifa Azouz (MD): revising the manuscript.
Sahbi Hermes (MD): acquisition of clinical data.
Alia Zehani (MD): revising the manuscript.
Haouet Slim (MD): Supervision, editing and approving the final version of the manuscript.
Guarantor
Sassi Farah.
Research registration number
-
1.
Name of the registry: No.
-
2.
Unique identifying number or registration ID: No.
-
3.
Hyperlink to your specific registration (must be publicly accessible and will be checked): No.
Declaration of competing interest
The authors report no declarations of interest.
References
- 1.Paravastu S.C.V., Regi J.M., Turner D.R., Gaines P.A. A contemporary review of cystic adventitial disease. Vasc. Endovasc. Surg. 2012;46:5–14. doi: 10.1177/1538574411419377. [DOI] [PubMed] [Google Scholar]
- 2.Kawarai S., Fukasawa M., Kawahara Y. Adventitial cystic disease of the popliteal artery. Ann. Vasc. Dis. 2012;5:190–193. doi: 10.3400/avd.cr.11.00069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nieto L.A., Cabrera Vargas L.F., Lozada-Martínez I.D., Guardo-Carmona D., Contreras M., Pedraza M., et al. Cystic adventitial disease of popliteal artery, the both sides of the coin: arterial resection vs cyst excision. Clin. Case Reports. 2022;10 doi: 10.1002/ccr3.5754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sohrabi C., Mathew G., Maria N., Kerwan A., Franchi T., Agha R.A., et al. The SCARE 2023 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2023;109:1136–1140. doi: 10.1097/JS9.0000000000000373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Atkins H.J.B., Key J.A. A case of myxomatous tumour arising in the adventitia of the left external iliac artery; case report. Br. J. Surg. 1947;34:426. doi: 10.1002/bjs.18003413618. [DOI] [PubMed] [Google Scholar]
- 6.Li S., King B.N., Velasco N., Kumar Y., Gupta N. Cystic adventitial disease—case series and review of literature. Ann Transl Med. 2017;5(327) doi: 10.21037/atm.2017.05.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.França M., Pinto J., Machado R., Fernandez G.C. Case 157: bilateral adventitial cystic disease of the popliteal artery. Radiology. 2010;255:655–660. doi: 10.1148/radiol.10082211. [DOI] [PubMed] [Google Scholar]
- 8.Affes M., Chaabouni M., Attia M., Jaber C., Baccouche I., Kchaou S., et al. Cystic adventitial disease of the popliteal artery with unusual spontaneous regression: a case report with literature review. Clin. Case Reports. 2022;10 doi: 10.1002/ccr3.5757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ksepka M., Li A., Norman S. Cystic adventitial disease. Ultrasound Quarterly. 2015;31:224. doi: 10.1097/RUQ.0000000000000160. [DOI] [PubMed] [Google Scholar]
- 10.Reik L.J.U., Lottspeich C., Jobst B., Czihal M. Cystic adventitial disease. Eur. Heart J. Cardiovasc. Imaging. 2023:jead298. doi: 10.1093/ehjci/jead298. [DOI] [PubMed] [Google Scholar]
- 11.Desy N.M., Spinner R.J. The etiology and management of cystic adventitial disease. J. Vasc. Surg. 2014;60(235–45):245. doi: 10.1016/j.jvs.2014.04.014. e1-11. [DOI] [PubMed] [Google Scholar]
- 12.Yada M., Sekine Y., Sato S., Nishina T. Adventitial cystic disease of the popliteal artery with intimal tear. J. Cardiol. Cases. 2019;19:197. doi: 10.1016/j.jccase.2019.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lezotte J., Le Q.P., Shanley C., Hans S. Adventitial cystic disease: complicated and uncomplicated. Ann. Vasc. Surg. 2018;46:370.e13–370.e15. doi: 10.1016/j.avsg.2017.08.037. [DOI] [PubMed] [Google Scholar]
- 14.Jay G.D., Ross F.L., Mason R.A., Giron F. Clinical and chemical characterization of an adventitial popliteal cyst. J. Vasc. Surg. 1989;9:448–451. doi: 10.1067/mva.1989.vs0090448. [DOI] [PubMed] [Google Scholar]
- 15.Spinner R.J., Desy N.M., Agarwal G., Pawlina W., Kalra M., Amrami K.K. Evidence to support that adventitial cysts, analogous to intraneural ganglion cysts, are also joint-connected. Clin. Anat. 2013;26:267–281. doi: 10.1002/ca.22152. [DOI] [PubMed] [Google Scholar]
- 16.Frenken M.R.M., Arnoldussen C.W.K.P., Janssen R.J.L. Cystic adventitial disease of the (Ilio) femoral artery with a connection to the hip joint: case report and a review of the literature. 2022;55:9–14. doi: 10.1016/j.ejvsvf.2022.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rich N.M. Popliteal entrapment and adventitial cystic disease. Surg. Clin. N. Am. 1982;62:449–465. doi: 10.1016/S0039-6109(16)42737-4. [DOI] [PubMed] [Google Scholar]
- 18.Yukata K., Nakai S., Goto T., Ikeda Y., Shimaoka Y., Yamanaka I., et al. Cystic lesion around the hip joint. World J. Orthop. 2015;6:688–704. doi: 10.5312/wjo.v6.i9.688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jheun A., Cutmore C., Lee K., Rajendran S. Cystic adventitial disease of the popliteal artery. ANZ J. Surg. 2023;93:2535–2536. doi: 10.1111/ans.18519. [DOI] [PubMed] [Google Scholar]
- 20.Smith J.L., Hariri N., Oriowo B., Lurie F. Cystic adventitial disease of the popliteal artery presenting with features of entrapment syndrome. J. Vasc. Surg. Cases Innov. Tech. 2020;6:75–79. doi: 10.1016/j.jvscit.2019.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nemoto M., Hosaka A. Spontaneous regression of cystic adventitial disease of the popliteal artery: a case report. Ann. Vasc. Surg. 2020;62:498.e11–498.e13. doi: 10.1016/j.avsg.2019.06.023. [DOI] [PubMed] [Google Scholar]
- 22.Zhang L., Guzman R., Kirkpatrick I., Klein J. Spontaneous resolution of cystic adventitial disease: a word of caution. Ann. Vasc. Surg. 2012;26(422):e1–e4. doi: 10.1016/j.avsg.2011.05.044. [DOI] [PubMed] [Google Scholar]