Abstract
Continuous subcutaneous insulin infusion (CSII, or insulin pump) and continuous glucose monitoring (CGM) sensors have been increasingly used and associated with improved glycemic control by people with type 1 diabetes and insulin-requiring type 2 diabetes. Commonly used infusion sets in most CSII systems are limited to a wear time of 3 days. In contradistinction, CGM sensors are currently approved for seven and more days of wear. With the motivation to provide a 7-day infusion set that matches the CGM wear time and to improve patient experience, the recently CE-marked and FDA 510k–cleared Medtronic extended infusion set (EIS) was designed.s The EIS offers enhanced new features that include use for up to 7 days, improved convenience, comfort, and better quality of life for insulin pump users.
Keywords: CSII, insulin infusion set, extended wear, unexplained hyperglycemia
Since continuous subcutaneous insulin infusion (CSII) with an external pump was introduced in persons with type 1 diabetes (T1D) in the 1970s, there have been progressive increases in the number of pump users. When used properly, the treatment is considered to be safe and effective.1-3 Major challenges of CSII include infusion set (IS) failure 4 which can lead to hyperglycemia and diabetic ketoacidosis5,6 and local tissue reactions including scarring and infection. 4 The recommendation for changing ISs every 2 to 3 days, published in 1983, was based on limited case reports related to infections. 7 Since then, there have been several published trials assessing IS wear duration which support limiting the use of aforementioned ISs currently on the market to 2 to 3 days.8-12
With the advent of real-time CGM (RT-CGM), many groups have worked on using CSII and RT-CGM to achieve partial or full closed-loop (CL) control of insulin delivery. Current systems require that patients wear an IS at one site and a RT-CGM sensor at a second site. Wearing devices at two sites for different durations is seen as a deterrent to wide-scale adoption of the CL system. Finding suitable sites on which to attach the devices can be challenging, particularly for children. Combining the IS with the glucose sensor on a single platform would reduce the number of devices worn and site insertions. As most CGM sensors are approved for 7 to 14 days of wear, extending the IS wear duration was a significant unmet need. This technology report describes the development of the recently CE-marked and FDA 510k–cleared (K210544) 13 Medtronic extended infusion set (EIS), approved for up to 7-day wear (Figure 1).
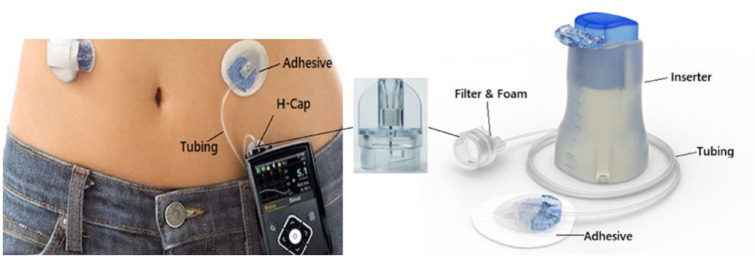
Figure 1.
Illustration of pump-reservoir-extended infusion set (EIS) system (left) and the EIS components (right).
IS Failure Modes During Longer Wear Durations
To develop the EIS, failure modes associated with extending the wear duration of 2/3-day sets in published studies were examined.8-12,14 Data from past studies were somewhat consistent: neither the type of insulin (Novolog vs Humalog) nor the IS type (steel vs Teflon) was a significant factor in determining IS wear time. No IS extended-wear study was performed using Apidra as insulin glulisine is only approved for use in a pump system for 2 days. 15 The study conducted by the Stanford University group 10 had the most detailed analyses of failure modes (Table 1), which was benchmarked for EIS development in 2015. In this study, the most dominant 7-day failure mode was the unexplained hyperglycemia (UH) at 30% failure rate and the strongest predictor of prolonged 7-day IS function was the individual subject. Unexplained hyperglycemia being the dominant failure mode was confirmed by the later studies.16-18 The failure modes associated with the prolonged IS use were summarized by Dr Buckingham in DTM 2021 Symposium (Table 1). 19
Table 1.
Seven-Day Failure Modes for 2- to 3-Day Infusion Sets in the Benchmark Study 10 and for EIS in the Pivotal Design Validation Study.
| 2/3-Day IS
10
(Benchmark) |
% in literature
19
(Mean, range) |
7-Day EIS 13 | ||
|---|---|---|---|---|
| 7-Day failure rate a | 64% | 52% (34%-67%) | 25% | |
| Infusion set failure modes b | Observed | Likely or Identified Causes | Observed | |
| Unexplained hyperglycemia | 30% | 22% (6%-30%) | Site occlusion resulted from biological responses to insertion injury, cannula, insulin, or other foreign materials Gel/aggregates inside the cannula, mechanical cannula kinking |
0.7% |
| Discomfort (pain, erythema, edema) at infusion site | 23% | 10% (3%-14%) | Biological responses to insertion injury, cannula, adhesive, insulin, or other foreign materials | 1.6% |
| Accidental pull-outs | 10% | 7% (1%-13%) | Accidents | 7.3% |
| Adhesive failure | 5% | 8.5% (5%-14%) | Adhesion loss due to wear and tear | 6.2% |
| Infection | 4% | 2.5% (0%-5%) | Biological response to microbial ingression, loss of preservative | 0.5% |
| Others | Not reported | 6.5% (5%-8%) | Miscalculating the time, subject personal decision of removal, and reasons unrelated to the IS | 11.8% |
Abbreviations: EIS, extended infusion set; IS, infusion set.
The rate of IS failure is defined as the number of IS removals associated with the failure mode divided by total number of sets inserted.
Failure modes might be overlapped, as subjects could indicate multiple reasons for one removal.
Although UH has been reported in many CSII clinical studies,8-12,16 the underlying causes of UH remain poorly understood. Early studies disclosed by Novo Nordisk 20 hinted that insulin stability might be an important contributor to the UH. Later, the in vitro chemical testing results by DeFelippis et al 21 and Sharrow et al 22 demonstrated 7- to 14-day insulin stability in a pump system under aggressive conditions of temperature and agitation, which presumed that UH was not due to insulin instability during pumping. Some hypotheses have theorized that preservatives might be the root cause for loss of infusion site viability over time.23-26 However, other studies27-29 have supported the initial finding by Novo Nordisk that the main contributor to UH is not the preservatives but insulin stability in the pump/reservoir/IS system. Other chemicals (eg, silicone oil) have also been shown to aggravate insulin aggregation in the fluid path. 30
In recent years, in vitro/in vivo studies conducted by us confirmed that, although temperature and agitation during pumping had no significant impact on insulin chemical stability, they caused formation of insulin aggregates/fibrils, which were highly inflammatory as tested by macrophage cell culture. 31 Preservative is also very important for insulin formulation stability. Preclinical study using insulin formulated with lower preservative content (≤50% Label Claim) induced more insulin aggregates in pumped infusates, significantly reduced IS wear duration and resulted in more infusion site/cannula occlusion in the T1D porcine model. 31 These findings permitted us to focus on maintaining the insulin stability in the fluid path to extend IS wear duration. 32
EIS Design and Mechanism of Action
Figure 1 illustrates the principal EIS components and its use in a Medtronic insulin pump system. As presented in Table 2, the main EIS design focus was to maintain insulin stability in the fluid path. Other failure modes listed in Table 1 were also addressed. The key EIS features include a proprietary polyvinyl alcohol (PVA) foam and filter with proper pore size in the fluid path. Polyvinyl alcohol is known to stabilize insulin conformationally and thermodynamically.33,34 Our internal study data confirmed the literature findings that the released insulin, after interacting with PVA foam, were more stable in the fluid path. In addition, the foam/filter combination effectively removes particulates/aggregates (≥5 µm) and hydrophobic molecules (eg, lubricant from the reservoir) and reduces site inflammation caused by these foreign molecules. 32 Furthermore, the EIS tubing is optimized for preventing preservative loss, therefore better maintaining insulin formulation stability. 31 Engineering and clinical user studies were conducted to select an adhesive patch for improving skin adhesion and wear comfort as well as well as keeping dermal layer injury to minimum, especially during an accidental pull. 35 Finally, a predicate state-of-art insertion device with soft Teflon cannula at 90° insertion angle was incorporated to ensure insertion reliability, reduce injury/inflammation, and increase comfort. 36
Table 2.
Principal Components in the EIS and Their Main Functions.
| Key components in EIS | Design rationale | Benefit provided | Targeted failure mode |
|---|---|---|---|
| In-line PVA foam | PVA is known to stabilize insulin conformationally and thermodynamically.33,34 In addition, the foam can serve as a coarse filter for removing larger particulates and hydrophobic molecules. | Prevents aggregation and thermodynamically stabilizes insulin. | Unexplained hyperglycemia Discomfort Infection |
| In-line filter | Particulates (≥10 µm) and hydrophobic chemicals in insulin infusate can affect insulin stability and induce inflammatory tissue responses. The EIS in-line filter is selected to remove particulates ≥5 µm and hydrophobic molecules. | Removes particulates, aggregates, and hydrophobic substances. | |
| Multilayer tubing | A trilayer medical tubing was thoughtfully designed to reduce gas permeability and mitigate preservative loss. Also, the tubing has a lubricious inner layer for insulin flow. | Mitigates preservative loss in the fluid path and reduces insulin aggregation by reducing gas permeability | |
| New adhesive patch | The adhesive patch was selected based on the material features: nonsensitizing, easy to handle and convert, breathable and conformable, sterilizable, and provides sufficient adhesion over extended wear by engineering and user clinical studies. | Provides breathability and comfortability, whereas maintaining extended wear time | Adhesive failure Discomfort |
| 6-mm or 9-mm soft Teflon cannula at 90° insertion angle | Soft cannula can reduce tissue injury during extended wear. 37 Selection of cannula length and insertion angle was based on the amount of subcutaneous tissue presented in the target users. A 90° angle is chosen to shorten the needle and therefore shorten the injury path in tissue. Both 6- and 9-mm cannula lengths are provided for users with thinner and thicker subcutaneous tissue layers. | Minimizes tissue injury, reduces cannula material in the subcutaneous tissue, reduces the fat lobules impacted, ensures insulin delivery reliability | Unexplained hyperglycemia Discomfort |
| State-of-art insertion device | The preloaded insertion device with automatic needle retraction was leveraged from Mio Advance infusion set (510k K173879). The insertion needle and soft cannula are hidden from the user before, during and after insertion of the soft cannula. | Ensures consistent insertion depth, reduces insertion failure, increases comfort, reduces injury and inflammation |
Abbreviations: EIS, extended infusion set; PVA, polyvinyl alcohol.
Design Validation
The new device was investigated in a pivotal design validation study that enrolled 259 participants (48% men, 45.0 ± 14.1 years), including 132 Humalog users and 127 Novolog users. Detailed data for the EIS pivotal trial have been published in Diabetes Technol Ther. 38 and FDA K210544 summary. 13
This single-arm, multicenter, nonrandomized trial was conducted in individuals with T1D using their own MiniMed 670G systems. Each participant was given 12 EIS devices, with each worn for ≥174 hours or until set failure. The intention-to-treat (ITT) population had a total of 3041 EIS wears. This study demonstrated that the EIS, when worn for up to 7 days, was safe and rated with high satisfaction, without adversely affecting glycemic control in adults with T1D. 38
Including all reasons, EIS 7-day failure rate was 25.2% with the failure modes examined and also presented in Table 1. The top three failure modes were Others, 11.8%; Accidental Pull-outs, 7.3%; and Adhesive Failure, 6.2%. In the previous studies, the “Other” category might have been counted as “Scheduled Removal” or not counted as those were not device-related failures. The EIS failure rates for the other two modes were similar to the corresponding means observed in literature. Improving adhesive longevity and comfortability is needed to further reduce EIS 7-day failure rate.
The rate of EIS failure due to UH (the main target of EIS design) at the end of day 7 (168 hours) was <1%, as presented in Table 3 for those using Humalog or Novolog in the ITT population. Results from the EIS pivotal study validated the design intents as described in Table 2. There was no predictor of prolonged 7-day IS function and no significant difference was observed between Humalog and Novolog users in any of the clinical outcomes evaluated.
Table 3.
Rate of Infusion Set Failure Due to Unexplained Hyperglycemia at the End of the Day 6 and Day 7.
| Wear time (at the end of) | Insulin used in ITT population | Number of subjects | Number of infusion sets | Number of failed infusion sets due to unexplained hyperglycemia (number of subjects) | Rate of infusion set failure a | Prespecified threshold (upper CL) | Actual result (upper CL) | Success criteria met? |
|---|---|---|---|---|---|---|---|---|
| Day 6 (Primary Endpoint) | Humalog | 132 | 1561 | 1 (1) | 0.06% | 20% | 0.45% | Yes |
| Novolog | 127 | 1480 | 4 (4) | 0.27% | 20% | 0.71% | Yes | |
| Day 7 (Secondary Endpoint) | Humalog | 132 | 1561 | 2 (2) | 0.13% | 20% | 0.51% | Yes |
| Novolog | 127 | 1480 | 6 (5) | 0.41% | 20% | 1.00% | Yes |
Abbreviations: CL, closed loop; EIS, extended infusion set; IS, infusion set; ITT, intention to treat; UH, unexplained hyperglycemia.
The rate of IS failure is defined as the number of EIS removals associated with UH divided by total number of sets inserted.
Excluding “Not for Cause” failures, the overall survival rate of the EIS for 7 days was 77.8%, comparable with the survival rate of 3-day sets used for 3 days in the benchmark study. 10
Conclusion
In conclusion, recent availability of the EIS, which comprises a thoughtfully designed fluid path that allows insulin infusion with less particulates/aggregates and hydrophobic chemicals, may reduce site inflammation and site pain for CSII users. This, in addition to use for up to 7 days, improved convenience and comfort, can help provide better quality of life for insulin pump users.
Acknowledgments
The authors thank Robert A. Vigersky, MD, for his review of the manuscript.
Footnotes
Abbreviations: CE, Conformitè Europëenne; CGM, continuous glucose monitoring; CL, closed loop; CSII, continuous subcutaneous insulin infusion; DKA, diabetic ketoacidosis; EIS, extended infusion set; FDA, Food and Drug Administration; IS, infusion set; ITT, intention-to-treat; PVA, polyvinyl alcohol; RT, real time; T1D, type 1 diabetes; UH, unexplained hyperglycemia.
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: The authors are all Medtronic employees.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was funded by Medtronic.
ORCID iDs: Gina Zhang  https://orcid.org/0000-0001-8310-016X
https://orcid.org/0000-0001-8310-016X
Sarnath Chattaraj  https://orcid.org/0000-0003-0409-0886
https://orcid.org/0000-0003-0409-0886
References
- 1. Pickup J, Mattock M, Kerry S. Glycaemic control with continuous subcutaneous insulin infusion compared with intensive insulin injections in patients with type 1 diabetes: meta-analysis of randomised controlled trials. BMJ. 2002;324:705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hoogma RP, Hammond PJ, Gomis R, et al. Comparison of the effects of continuous subcutaneous insulin infusion (CSII) and NPH-based multiple daily insulin injections (MDI) on glycaemic control and quality of life: results of the 5-nations trial. Diabet Med. 2006;23(2):141-147. [DOI] [PubMed] [Google Scholar]
- 3. Pickup JC, Sutton AJ. Severe hypoglycaemia and glycaemic control in type 1 diabetes: meta-analysis of multiple daily insulin injections compared with continuous subcutaneous insulin infusion. Diabet Med. 2008;25:765-774. [DOI] [PubMed] [Google Scholar]
- 4. Heinemann L, Krinelke L. Insulin infusion set: the Achilles heel of continuous subcutaneous insulin infusion. J Diabetes Sci Technol. 2012;6:954-964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Brown SA, Kovatchev BP, Raghinaru D, et al. Six-month randomized, multicenter trial of closed-loop control in type 1 diabetes. N Engl J Med. 2019;381:1707-1717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Breton MD, Kanapka LG, Beck RW, et al. A randomized trial of closed-loop control in children with type 1 diabetes. N Engl J Med. 2020;383:836-845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Centers for Disease Control. Toxic-shock syndrome in a patient using a continuous subcutaneous insulin infusion pump—Idaho. MMWR Morb Mortal Wkly Rep. 1983;32:404-406. [PubMed] [Google Scholar]
- 8. Thethi TK, Rao A, Kawji H, et al. Consequences of delayed pump infusion line change in patients with type 1 diabetes mellitus treated with continuous subcutaneous insulin infusion. J Diabetes Complications. 2010;24(2):73-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Schmid V, Hohberg C, Borchert M, Forst T, Pfützner A. Pilot study for assessment of optimal frequency for changing catheters in insulin pump therapy-trouble starts on day 3. J Diabetes Sci Technol. 2010;4:976-982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Patel PJ, Benasi K, Ferrari G, et al. Randomized trial of infusion set function: steel versus Teflon. Diabetes Technol Ther. 2014;16:15-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Pfützner A, Sachsenheimer D, Grenningloh M, et al. Using insulin infusion sets in CSII for longer than the recommended usage time leads to a high risk for adverse events: results from a prospective randomized crossover study. J Diabetes Sci Technol. 2015;9:1292-1298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. van Bon AC, Bode BW, Sert-Langeron C, DeVries JH, Charpentier G. Insulin glulisine compared to insulin aspart and to insulin lispro administered by continuous subcutaneous insulin infusion in patients with type 1 diabetes: a randomized controlled trial. Diabetes Technol Ther. 2011;13:607-614. [DOI] [PubMed] [Google Scholar]
- 13. Food and Drug Administration. K210544, Medtronic Extended Infusion Set. https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfpmn/pmn.cfm?ID=K210544. Accessed July 2, 2022.
- 14. Kerr D, Morton J, Whately-Smith C, Everett J, Begley JP. Laboratory-based non-clinical comparison of occlusion rates using three rapid-acting insulin analogs in continuous subcutaneous insulin infusion catheters using low flow rates. J Diabetes Sci Technol. 2008;2(3):450-455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Food and Drug Administration. Apidra Label. https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/021629s039s040lbl.pdf. Accessed July 2, 2022.
- 16. Waldenmaier D, Zschornack E, Buhr A, Pleus S, Haug C, Freckmann G. A prospective study of insulin infusion set use for up to 7 days: early replacement reasons and impact on glycemic control. Diabetes Technol Ther. 2020;22(10):734-741. [DOI] [PubMed] [Google Scholar]
- 17. Karlin AW, Ly TT, Pyle L, et al. Duration of infusion set survival in lipohypertrophy versus nonlipohypertrophied tissue in patients with type 1 diabetes. Diabetes Technol Ther. 2016;18(7):429-435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Lal RA, Hsu L, Zhang J, Schøndorff PK, Heschel M, Buckingham B. Longevity of the novel ConvaTec infusion set with lantern technology. Diabetes Obes Metab. 2021;23(8):1973-1977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Nguyen KT, Xu NY, Buckingham BA, et al. Improving the patient experience with longer wear infusion sets symposium report. J Diabetes Sci Technol. 2022;16(3):775-782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Food and Drug Administration. Center for Drug Evaluation and Research Medical Review of Novolog Application 20-986/SE3-003. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2001/20-986SE3003_NovoLog_medr.pdf. Accessed July 2, 2022.
- 21. DeFelippis MR, Bell MA, Heyob JA, Storms SM. In vitro stability of insulin lispro in continuous subcutaneous insulin infusion. Diabetes Technol Ther. 2006;8(3):358-368. [DOI] [PubMed] [Google Scholar]
- 22. Sharrow SD, Glass LC, Dobbins MA. 14-Day in vitro chemical stability of insulin lispro in the MiniMed paradigm pump. Diabetes Technol Ther. 2012;14(3):264-270. [DOI] [PubMed] [Google Scholar]
- 23. Singh SM, Hutchings RL, Mallela KM. Mechanisms of m-cresol-induced protein aggregation studied using a model protein cytochrome c. J Pharm Sci. 2011;100(5):1679-1689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hutchings RL, Singh SM, Cabello-Villegas J, Mallela KM. Effect of antimicrobial preservatives on partial protein unfolding and aggregation. J Pharm Sci. 2013;102(2):365-376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Weber C, Kammerer D, Streit B, Licht AH. Phenolic excipients of insulin formulations induce cell death, pro-inflammatory signaling and MCP-1 release. Toxicol Rep. 2015;2:194-202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. van Faassen I, Verweij-van Vught AM, Lomecky-Janousek MZ, Razenberg PP, van der Veen EA. Preservatives in insulin preparations impair leukocyte function. Diabetes Care. 1990;13(1):71-74. [DOI] [PubMed] [Google Scholar]
- 27. Teska BM, Alarcón J, Pettis RJ, Randolph TW, Carpenter JF. Effects of phenol and meta-cresol depletion on insulin analog stability at physiological temperature. J Pharm Sci. 2014;103(8):2255-2267. [DOI] [PubMed] [Google Scholar]
- 28. Swinney MR, Cox AL, Hawkins ED, et al. Insulin, not the preservative m-cresol, instigates loss of infusion site patency over extended durations of CSII in diabetic swine. J Pharm Sci. 2021;110(3):1418-1426. [DOI] [PubMed] [Google Scholar]
- 29. Zhang JY, Shang T, Chattaraj S, et al. Advances in insulin pump infusion sets symposium report. J Diabetes Sci Technol. 2021;15(3):705-709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Nayef L, Khan MF, Brook MA. The stability of insulin solutions in syringes is improved by ensuring lower molecular weight silicone lubricants are absent. Heliyon. 2017;3(3):e00264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Chattaraj S, Zhang G, Anselmo E, Fusselman J. 1012-P: study of insulin stability impact on pump therapy: test model development. Diabetes. 2020;69(suppl 1):1012-P. [Google Scholar]
- 32. Chattaraj S, Zhang G, Anselmo E, Cordero T, Cohen O. P192: the Medtronic extended wear infusion set: determining mechanisms of action. Diabetes Technol Ther. 2021;23(S2):P192. [Google Scholar]
- 33. Kimura T, Sato K, Sugimoto K, et al. Oral administration of insulin as poly(vinyl alcohol)-gel spheres in diabetic rats. Biol Pharm Bull. 1996;19(6):897-900. [DOI] [PubMed] [Google Scholar]
- 34. Rawat S, Gupta P, Kumar A, et al. Molecular mechanism of poly(vinyl alcohol) mediated prevention of aggregation and stabilization of insulin in nanoparticles. Mol Pharm. 2015;12(4):1018-1030. [DOI] [PubMed] [Google Scholar]
- 35. Zhang G, Chattaraj S, Anselmo E, Hoffman LP, Tran M, Bondy S. 986-P: assessment of adhesive patches for an extended wear infusion set. Diabetes. 2020;69(suppl 1):986-P. [Google Scholar]
- 36. Food and Drug Administration. K173879, MiniMed Mio Advance Infusion Set. https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfpmn/pmn.cfm?ID=K173879. Accessed July 2, 2022.
- 37. Hauzenberger J, Münzker J, Kotzbeck P, et al. Systematic in vivo evaluation of the time-dependent inflammatory response to steel and Teflon insulin infusion catheters. Sci Rep. 2018;8:1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Brazg R, Garg SK, Bhargava A, et al. Evaluation of extended infusion set performance in adults with type 1 diabetes: infusion set survival rate and glycemic outcomes from a pivotal trial [published online ahead of print March 24, 2022]. Diabetes Technol Ther. doi: 10.1089/dia.2021.0540. [DOI] [PMC free article] [PubMed] [Google Scholar]