Key Points
Question
What is the year-over-year hernia recurrence rate in patients with prior ventral hernia repair?
Findings
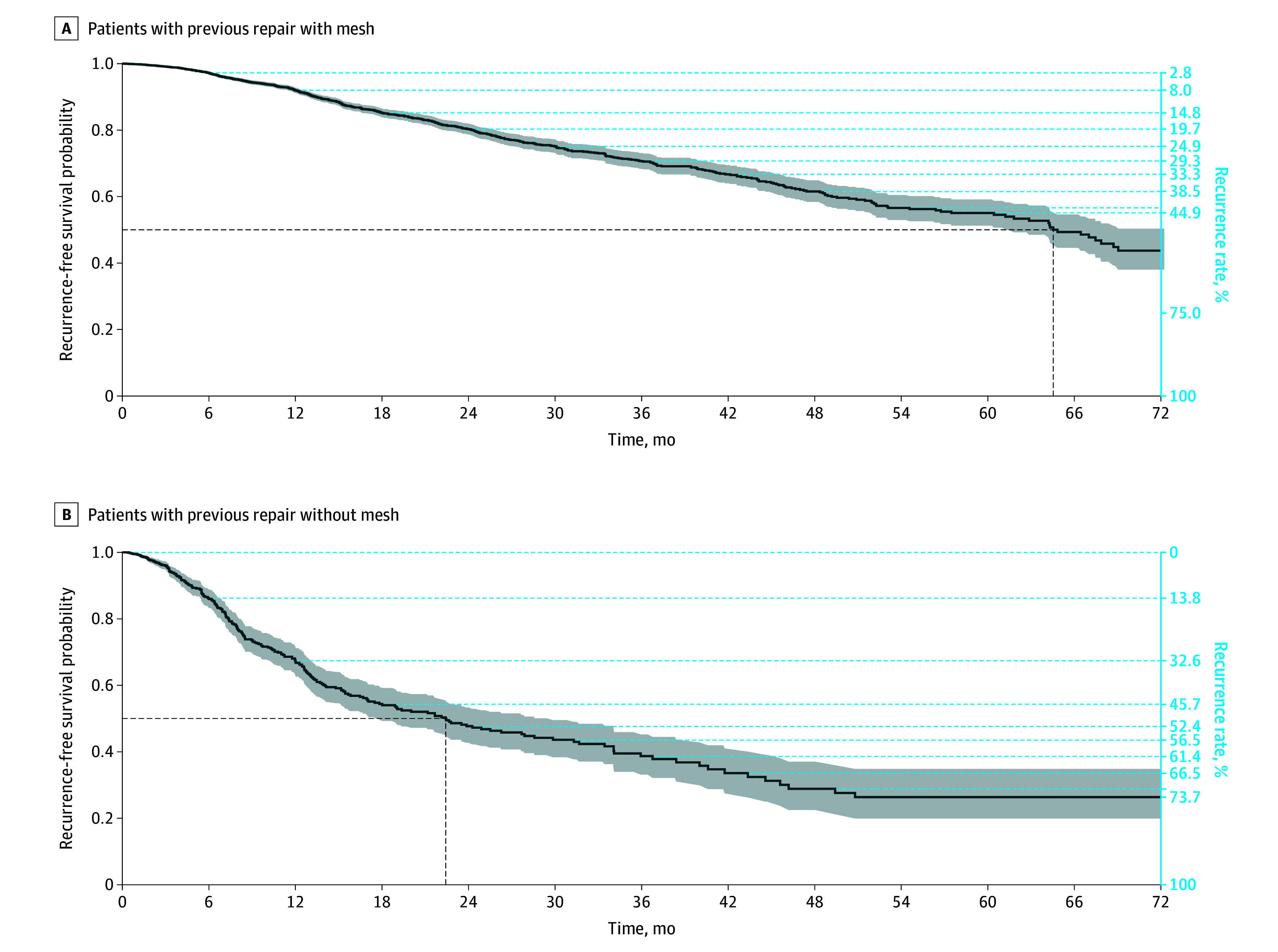
In this US database study of 35 433 patients, year-over year recurrence rates were higher among patients with previous mesh repair than those without and increased in both groups over time.
Meaning
The findings indicate that risk of hernia recurrence increased over time and may be higher than previously reported, reflecting the complex and chronic nature of ventral hernia disease requiring long-term follow-up.
This cohort study evaluates ventral hernia recurrence rates and associated risk factors over 5 years in patients with previous hernia repair.
Abstract
Importance
Recurrence is one of the most challenging adverse events after ventral hernia repair as it impacts quality of life, utilization of resources, and subsequent need for re-repair. Rates of recurrence range from 30% to 80% after ventral hernia repair.
Objective
To determine the contemporary ventral hernia recurrence rate over time in patients with previous hernia repair and to determine risk factors associated with recurrence.
Design, Setting, and Participants
This retrospective, population-based study used the Abdominal Core Health Quality Collaborative registry to evaluate year-over-year recurrence rates in patients with prior ventral hernia repair between January 2012 and August 2022. Patients who underwent at least 1 prior ventral hernia repair were included and categorized into 2 groups based on mesh or no-mesh use. There were 43 960 eligible patients; after exclusion criteria (patients with concurrent inguinal hernias as the primary diagnosis, nonstandard hernia procedure categories, American Society of Anesthesiologists class unassigned, or no follow-up), 29 834 patients were analyzed in the mesh group and 5599 in the no-mesh group.
Main Outcomes and Measures
Ventral hernia recurrence rates. Risk factors analyzed include age, body mass index, sex, race, insurance type, medical comorbidities, American Society of Anesthesiologists class, smoking, indication for surgery, concomitant procedure, hernia procedure type, myofascial release, fascial closure, fixation type, number of prior repairs, hernia width, hernia length, mesh width, mesh length, operative approach, prior mesh placement, prior mesh infection, mesh location, mesh type, postoperative surgical site occurrence, postoperative surgical site infection, postoperative seroma, use of drains, and reoperation.
Results
Among 29 834 patients with mesh, the mean (SD) age was 57.17 (13.36) years, and 14 331 participants (48.0%) were female. Among 5599 patients without mesh, the mean (SD) age was 51.9 (15.31) years, and 2458 participants (43.9%) were female. When comparing year-over-year hernia recurrence rates in patients with and without prior mesh repair, respectively, the Kaplan Meier analysis showed a recurrence rate of 201 cumulative events with 13 872 at risk (2.8%) vs 104 cumulative events with 1707 at risk (4.0%) at 6 months; 411 cumulative events with 4732 at risk (8.0%) vs 184 cumulative events with 427 at risk (32.6%) at 1 year; 640 cumulative events with 1518 at risk (19.7%) vs 243 cumulative events with 146 at risk (52.4%) at 2 years; 731 cumulative events with 670 at risk (29.3%) vs 258 cumulative events with 73 at risk (61.4%) at 3 years; 777 cumulative events with 337 at risk (38.5%) vs 267 cumulative events with 29 at risk (71.2%) at 4 years; and 798 cumulative events with 171 at risk (44.9%) vs 269 cumulative events with 19 at risk (73.7%) at 5 years. Higher body mass index; immunosuppressants; incisional and parastomal hernias; a robotic approach; greater hernia width; use of a biologic or resorbable synthetic mesh; and complications, such as surgical site infections and reoperation, were associated with higher odds of hernia recurrence. Conversely, greater mesh width, myofascial release, and fascial closure had lower odds of recurrence. Hernia type was the most important variable associated with recurrence.
Conclusions and Relevance
In this study, the 5-year recurrence rate after ventral hernia repair was greater than 40% and 70% in patients with and without mesh, respectively. Rates of ventral hernia recurrence increased over time, underscoring the importance of close, long-term follow up in this population.
Introduction
In the US, more than 350 000 ventral hernia repairs are performed annually, making it one of the most common abdominal surgical procedures.1,2 Hernia recurrence, an important metric of surgical efficacy, has been associated with chronic pain, poor quality of life, and increased costs.1,3 Rates of recurrence vary widely in the literature, from 30% to 80%.4,5,6 However, these rates may underestimate the true clinical recurrence rate, as many of these studies are limited by small sample sizes, short follow-up, and large variability in their characterization of recurrence—with definitions ranging from clinical recurrence, patient-reported recurrence, or reoperation rates as proxies for recurrence.7,8 Moreover, none of these studies report recurrence rate by year postrepair.
Understanding population-based hernia recurrence rates with subsequent emphasis on reduction of recurrence remains a priority to improve patient care and reduce health care costs. The purpose of this study was to determine the clinical recurrence rate over time with more granularity and identify factors associated with recurrence after ventral hernia repair.
Methods
A retrospective cohort study was performed by querying the Abdominal Core Health Quality Collaborative (ACHQC), a national database focused on hernia repairs and abdominal wall diseases, with data from more than 400 surgeons.9 It includes deidentified surgeon-entered patient and operative characteristics, as well as patient-reported outcome measures of more than 90 000 inguinal and ventral hernia repairs in the US.9 The institutional review board at Ohio State University determined exemption of review was applicable to this study. A waiver of informed consent was also granted since only deidentified data were collected in the ACHQC database.
The ACHQC registry was interrogated to generate a subset of patients who underwent at least 1 prior ventral hernia repair between January 2012 and August 2022. Patients with concurrent inguinal hernias as the primary diagnosis; repairs involving more than 1 hernia type, except for incisional and parastomal (eg, lumbar and epigastric or Spigelian and parastomal and umbilical); American Society of Anesthesiologists (ASA) class unassigned; or no follow-up were excluded. Patients were categorized into 2 subgroups based on mesh use. The primary outcome, hernia recurrence, was determined based on clinical evaluation, defined by physical examination or imaging.
Hernia, intraoperative, and postoperative characteristics were compared between patients who did and did not experience recurrence. Patient characteristics; operative and hernia details; intraoperative complications; and 30-day outcomes, such as length of stay, surgical site infection (SSI), and reoperation rates, were also reported.
Statistical Analyses
For each subgroup, bivariate tests for categorical and continuous variables were assessed using Pearson χ2 and Wilcoxon rank sum tests, respectively. Time to recurrence was estimated using the Kaplan-Meier method. To identify factors associated with recurrence, an extended Cox proportional hazards model was used. Time-dependent covariates and coefficients were included based on model evaluation when the proportional hazards assumption was violated and remedied using a step-function approach.10 Age, body mass index, hernia width and length, and mesh width and length were modeled with restricted cubic splines with 3 knots to allow for nonlinearity. Partial effect plots show hazard ratios of recurrence for these continuous variables. Overall covariate significance was evaluated using the likelihood ratio χ2 test and a composite hypothesis test, and variable importance was evaluated by χ2 statistic minus degrees of freedom. R software version 4.0.3 (R Foundation) was used for all statistical analyses. Two-sided P < .05 was considered statistically significant.
Results
Among 29 834 patients with mesh, the mean (SD) age was 57.17 (13.36) years, and 14 331 participants (48.0%) were female. Among 5599 patients without mesh, the mean (SD) age was 51.9 (15.31) years, and 2458 participants (43.9%) were female. A total of 29 834 patients underwent ventral hernia repair with mesh and 5599 patients underwent ventral hernia repair without mesh (eFigure 1 in Supplement 1). The mean (SD) time from index ventral hernia repair to latest follow-up was 127.94 (274.11) days (median [IQR], 29 [16-75]) for patients with mesh and 78.11 (211.40) days (median [IQR], 20 [14-36]) for those without. Among patients who experienced recurrence, the mean (SD) time to recurrence was 495.05 (454.64) days (median [IQR], 363 [184-666]) for patients with mesh and 329.68 (329.89) days (median [IQR], 226 [115-402]) for those without (eTable 1 in Supplement 1). Differences in demographic and surgical characteristics between patients with and without mesh who did and did not experience hernia recurrence are shown in eTable 1 in Supplement 1.
Year-Over-Year Rates of Recurrence
Rates of recurrence increased over time. Patients with ventral hernia repair with mesh experienced lower recurrence rates than those with ventral hernia repair without mesh at 1, 2, 3, 4, and 5 years (Figure). The Kaplan-Meier analysis for mesh and no-mesh groups, respectively, showed a recurrence rate of 201 cumulative events with 13872 at risk (2.8%) vs 104 cumulative events with 1707 at risk (4.0%) at 6 months; 411 cumulative events with 4732 at risk (8.0%) vs 184 cumulative events with 427 at risk (32.6%) at 1 year; 640 cumulative events with 1518 at risk (19.7%) vs 243 cumulative events with 146 at risk (52.4%) at 2 years; 731 cumulative events with 670 at risk (29.3%) vs 258 cumulative events with 73 at risk (61.4%) at 3 years; 777 cumulative events with 337 at risk (38.5%) vs 267 cumulative events with 29 at risk (71.2%) at 4 years; and 798 cumulative events with 171 at risk (44.9%) vs 269 cumulative events with 19 at risk (73.7%) at 5 years.
Figure. Recurrence Rates Over Time Following Ventral Hernia Repair in Patients With and Without Mesh.
Ventral Hernia Repair With Mesh
Patients with ventral hernia repair with mesh who had recurrence had a larger hernia width compared to patients without recurrence (mean [SD], 10.31 [8.08] cm vs 6.85 [5.96] cm; P < .001) (eTable 2 in Supplement 1). Moreover, a greater percentage of ventral hernia repair patients with mesh that had recurrence had prior mesh placed as compared to those without recurrence (289 of 819 [35.29%] vs 5820 of 29 015 [20.06%]; P < .001). Patients with recurrence had a statistically significant greater percentage of 30-day surgical site infections (SSIs), reoperations, and readmissions regardless of whether mesh was previously used. Patients with mesh who experienced recurrence had higher 30-day SSIs (88 of 712 [12.36%] vs 863 of 26 674 [3.24%]; P < .001), 30-day reoperations (69 of 712 [9.69%] vs 394 of 26 674 [1.48%]; P < .001), and 30-day readmissions (72 of 710 [10.14%] vs 1135 of 2663 [42.62%]; P < .001) compared to those with mesh and no recurrence (eTable 2 in Supplement 1).
The 5 most important variables associated with recurrence in the mesh group included hernia type, mesh type, myofascial release, body mass index, and hernia width (eFigure 2 in Supplement 1). Male patients taking immunosuppressants, with a higher body mass index, with an enlarging hernia or a hernia that interfered with activities, incisional hernia only, incisional and parastomal hernia or parastomal hernia only, with a greater hernia width, who had a robotic operative approach, biological tissue–derived mesh, resorbable synthetic mesh, postoperative SSI, or reoperation were more likely to have recurrence after ventral hernia repair with mesh. Patients who had a greater mesh width or who underwent myofascial release or primary fascial closure were less likely to have recurrence (Table 1).
Table 1. Cox Regression Analysis of Patients With Ventral Hernia Repair and Mesh.
| Variable | Hazard ratio (95% CI) | P value |
|---|---|---|
| Agea | NA | .83 |
| BMIa | NA | <.001 |
| Sex (female vs male) | 0.79 (0.68-0.92) | .002 |
| Raceb | .33 | |
| Black vs White | 0.82 (0.60-1.11) | .20 |
| Hispanic vs White | 0.69 (0.39-1.21) | .19 |
| Otherc vs White | 1.04 (0.53-2.03) | .91 |
| Diabetes | 0.95 (0.79-1.15) | .63 |
| Dialysis | 1.33 (0.53-3.34) | .55 |
| COPD | 0.86 (0.64-1.15) | .32 |
| Immunosuppressants | 1.33 (1.02-1.73) | .034 |
| Hypertension | 0.97 (0.83-1.13) | .69 |
| Smoking within 1 y | 1.02 (0.80-1.31) | .85 |
| Indication for surgery: bowel obstruction | 3.44 (1.58-7.51) | .002 |
| Indication for surgery: enlarging/interfering with activities | 1.20 (1.02-1.42) | .03 |
| Indication for surgery: pain | 0.80 (0.66-0.99) | .04 |
| Indication for surgery: fistula | 1.51 (0.93-2.45) | .10 |
| Indication for surgery: infected mesh | 1.02 (0.58-1.78) | .95 |
| ASA class (4 vs 1) | 0.88 (0.43-1.81) | .73 |
| Concomitant procedure | 1.00 (0.83-1.22) | .97 |
| Hernia procedure type | <.001 | |
| Epigastric vs incisional | 0.50 (0.26-0.99) | .047 |
| Incisional and parastomal vs incisional | 2.13 (1.67-2.72) | <.001 |
| Parastomal vs incisional | 3.29 (2.46-4.41) | <.001 |
| Umbilical vs incisional | 0.57 (0.41-0.81) | .002 |
| Insurance: Medicare vs Medicaid | 1.13 (0.81-1.57) | .48 |
| History of open abdominal procedure | 0.85 (0.66-1.10) | .22 |
| Myofascial release | 0.57 (0.45-0.73) | <.001 |
| Fascial closure | 0.67 (0.52-0.86) | .002 |
| Fixation type: adhesives | 2.12 (1.01-4.47) | .24 |
| Fixation type: staples | 1.36 (0.45-4.07) | .72 |
| Fixation type: sutures | 0.84 (0.70-1.03) | .09 |
| Fixation type: tacks | 0.95 (0.69-1.31) | .76 |
| No. of prior repairs: ≥3 vs 0 | 1.31 (0.97-1.76) | .07 |
| Hernia widthd | NA | .002 |
| Hernia lengthd | NA | .66 |
| Mesh widthe | NA | .03 |
| Mesh lengthe | NA | .76 |
| Operative approach | ||
| Robotic vs open | 1.32 (1.03-1.70) | .03 |
| Laparoscopic vs open | 0.83 (0.54-1.26) | .37 |
| MIS converted to open vs open | 1.31 (0.76-2.28) | .33 |
| Prior mesh present | 1.09 (0.88-1.35) | .45 |
| Intraoperative complications | 0.84 (0.58-1.21) | .35 |
| Prior mesh infection | 1.00 (0.73-1.37) | .99 |
| Mesh location | ||
| Inlay vs sublay | 1.33 (0.90-1.96) | .16 |
| Onlay vs sublay | 1.12 (0.80-1.55) | .52 |
| Mesh type | ||
| Biological tissue–derived vs permanent synthetic | 1.94 (1.46-2.57) | <.001 |
| Resorbable synthetic vs permanent synthetic | 2.19 (1.62-2.96) | <.001 |
| Postoperative SSO | 1.21 (0.92-1.59) | .17 |
| Postoperative SSI | 1.78 (1.25-2.52) | .001 |
| Postoperative seroma | 0.38 (0.16-0.89) | .03 |
| Reoperation | 1.77 (1.18-2.66) | .006 |
| Drains used | 1.08 (0.65-1.81) | .77 |
Abbreviations: ASA, American Society of Anesthesiologists; BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); COPD, chronic obstructive pulmonary disease; MIS, minimally invasive surgery; NA, not applicable; SSI, surgical site infection; SSO, surgical site occurrence.
Data were modeled using restricted cubic splines. See eFigure 4 in Supplement 1 for interpretation.
Race and ethnicity were collected via surgeon-entered information based on 6 multiple choice options from the Abdominal Core Health Quality Collaborative database. The 6 categories were Indian or Alaska Native; Asian, Native Hawaiian or Other Pacific Islander; Black or African American; Hispanic; Middle Eastern; and White, not of Hispanic Origin. Race and ethnicity was collected to better understand how hernia recurrence may vary among specific populations.
Other race and ethnicity groups included American Indian or Alaska Native; Asian, Native Hawaiian or Other Pacific Islander; and Middle Eastern. They were consolidated to increase the sample size to draw meaningful statistical comparisons between groups.
Data were modeled using restricted cubic splines. See eFigure 5 in Supplement 1 for interpretation.
Data were modeled using restricted cubic splines. See eFigure 6 in Supplement 1 for interpretation.
Ventral Hernia Repair Without Mesh
Patients with ventral hernia repair without mesh who had recurrence had a larger hernia width compared to patients without recurrence (mean [SD], 6.00 [5.99] cm vs 2.08 [2.75] cm; P < .001) (eTable 2 in Supplement 1). Moreover, a greater percentage of patients with ventral hernia repair without mesh who had recurrence had prior mesh placed compared to those without recurrence (110 of 269 [40.89%] vs 393 of 5330 [7.37%]; P < .001). Patients without mesh who experienced recurrence had higher 30-day SSIs (30 of 225 [13.33%] vs 98 of 5010 [1.96%]; P < .001), 30-day reoperations (26 of 225 [11.56%] vs 35 of 5010 [0.70%]; P < .001), and 30-day readmissions (22 of 225 [9.78%] vs 82 of 4998 [1.64%]; P < .001) compared to those without mesh and no recurrence (eTable 2 in Supplement 1).
The 5 most important variables associated with recurrence in the no-mesh group included hernia type, ASA class, operative approach, myofascial release, and number of prior repairs (eFigure 3 in Supplement 1). Patients who had ventral hernia repair without mesh were more likely to have recurrence with a greater ASA class, greater hernia width, an umbilical hernia, had 3 or more prior repairs, or had a robotic, laparoscopic, or minimally invasive surgery converted to open surgery operative approach. Patients who underwent myofascial release or fascial closure were less likely to have recurrence (Table 2).
Table 2. Cox Regression Analysis of Patients With Ventral Hernia Repair and No Mesh.
| Variable | Hazard ratio (95% CI) | P value |
|---|---|---|
| BMIa | NA | .86 |
| Diabetes | 0.77 (0.55-1.08) | .13 |
| COPD | 0.82 (0.50-1.34) | .43 |
| Immunosuppressants | 1.10 (0.64-1.89) | .73 |
| Smoking within 1 y | 1.14 (0.80-1.64) | .47 |
| Indication for surgery: fistula | 0.81 (0.52-1.27) | .36 |
| Indication for surgery: infected mesh | 0.95 (0.64-1.42) | .82 |
| ASA class (4 vs 1) | 3.02 (1.26-7.26) | .01 |
| Hernia procedure type | ||
| Epigastric vs incisional | 0.87 (0.44-1.74) | .69 |
| Incisional and parastomal vs incisional | 1.37 (0.76-2.48) | .29 |
| Parastomal vs incisional | 1.51 (0.86-2.64) | .15 |
| Umbilical vs incisional | 0.46 (0.31-0.69) | <.001 |
| Myofascial release | 0.16 (0.04-0.68) | .01 |
| Fascial closure | 0.50 (0.28-0.89) | .02 |
| Hernia widtha | NA | .04 |
| Operative approach | ||
| Laparoscopic vs open | 2.23 (1.39-3.59) | .001 |
| Robotic vs open | 2.11 (1.11-4.02) | .02 |
| MIS converted to open vs open | 2.32 (1.07-5.04) | .03 |
| Intraoperative complications | 0.66 (0.39-1.11) | .12 |
| No. of prior repairs: ≥3 vs 0 | 1.97 (1.20-3.25) | .008 |
| Postoperative SSO | 1.59 (0.97-2.58) | .06 |
| Postoperative SSI | 1.50 (0.83-2.71) | .18 |
| Reoperation | 0.97 (0.39-2.42) | .94 |
Abbreviations: ASA, American Society of Anesthesiologists; BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); COPD, chronic obstructive pulmonary disease; MIS, minimally invasive surgery; NA, not applicable; SSI, surgical site infection; SSO, surgical site occurrence.
Data were modeled using restricted cubic splines. See eFigure 7 in Supplement 1 for interpretation.
Discussion
In this large, national database retrospective cohort study, we demonstrated that after ventral hernia repair, the 5-year clinical recurrence rate was 44.9% in patients with prior mesh repair and 73.7% in patients without prior mesh repair. Patients without mesh had a recurrence rate greater than 50% at 2-year follow-up, whereas those with mesh experienced a similar rate of recurrence after 6 years. While previous literature has suggested that most ventral hernia recurrences occur within 2 years of index operation, our study found increasing recurrence rates up to 5 years from initial repair.11
Previous literature has attempted to quantify recurrence rates following ventral hernia repair; however, most studies fail to stratify recurrence rates at defined time points4,12 or underestimate the true clinical recurrence rate, as patients with recurrence may choose to forgo reoperation.8 Flum et al5 reported a 5-year reoperation rate of approximately 12% after primary incisional hernia repair in the early 2000s, while more recent studies have described reoperation rates between 14% to 16% after index operation.7,13 Helgstrand and colleagues8 analyzed the Danish Ventral Hernia Database and reported a 4-year clinical recurrence risk of 15% after umbilical or epigastric repair and 37% after incisional hernia repair. However, this study was limited by a small sample size, exclusion of patients with mesh, and patient-reported occurrences of recurrence. We report a 5-year clinical recurrence rate of approximately 45%, which is higher than that cited in the literature, demonstrating that recurrence remains a serious complication following hernia repair.
Our study found that incisional and parastomal hernias were independently and concomitantly associated with increased risk of recurrence, while epigastric and umbilical hernias were associated with lower risk of recurrence. Similar studies corroborate these findings.4,5,7,14,15,16,17,18 This may be explained by the increased complexity of incisional and parastomal hernias compared to other hernia types. Hernia type was found to be the most important factor associated with recurrence for patients with and without mesh, underscoring its importance when selecting appropriate surgical candidates.
Conflicting evidence exists regarding the impact of surgical approach on hernia recurrence. While some studies indicate that laparoscopic and robotic repairs are associated with lower odds of reoperation for recurrence,13 others show no difference.19,20,21,22 Conversely, a study by Howard et al7 found that minimally invasive hernia repair was associated with a higher incidence of reoperation for recurrence compared to open hernia repair. However, it is unclear how the results differ between laparoscopic and robotic techniques, as no distinction was made between the two. The present study showed that any minimally invasive approach (robotic, laparoscopic, or minimally invasive surgery converted to open surgery) was associated with clinical recurrence in patients without mesh repair. In patients with mesh repair, robotic surgery was associated with increased recurrence, while laparoscopic surgery had no significant association. These findings may be explained by the fact that minimally invasive techniques described in this database may have used bridged repairs instead of mesh-reinforced primary musculofascial reapproximation, thereby resulting in higher recurrence over time. Further research is needed to fully elucidate the role of robotic surgery in ventral hernia repair and its impact on recurrence.
Large randomized clinical trials and database studies have led to general acceptance that mesh reinforcement decreases recurrence rates; however, debate still exists around the optimal mesh location and type.18,23,24,25,26 We found that, compared to ventral hernia repair without mesh, use of mesh was associated with lower 5-year recurrence rates (73.7% vs 44.9% respectively) and delayed time to 50% recurrence (2 vs 6 years). Although the use of mesh is increasing,13 conflicting evidence regarding the ideal mesh placement exists. Some argue that the retromuscular position is optimal for open ventral hernia repair, while intraperitoneal underlay may be useful in laparoscopic repair.14,21,23,25,27 We found no difference in recurrence rates based on mesh location, which is consistent with recent studies.18,28 Furthermore, high-quality data are scarce regarding the superiority of any specific mesh type.29,30,31,32,33,34 In our study, we found that biologic mesh and resorbable synthetic mesh were associated with an increase in risk of recurrence compared to permanent synthetic mesh. This finding may be explained by differences in mesh degradation and properties over time, as well as variability in immune responses, and warrants further investigation. In addition, biologic and resorbable meshes have often been used in contaminated conditions, which can lead to both mesh-related complications as well as reoperation and recurrence.34 Furthermore, we demonstrated that greater mesh width was associated with lower recurrence rates. This may be attributed to increased coverage and support of the hernia defect, enhanced tissue ingrowth and incorporation, and improved tension distribution across the abdominal wall.35,36 Limited studies have analyzed effects of mesh overlap37 as well as mesh area-to-defect ratio on recurrence38,39; however, few if any have specifically examined the impact of exact mesh size on recurrence rates. The paucity of literature analyzing mesh size or comparing mesh types necessitates additional high-caliber evidence to elucidate these outcomes.
Our study found that obesity and immunosuppressants were associated with increased odds of recurrence, while smoking, greater ASA class, and prior mesh infection were not. Obesity, smoking,12,40,41 mesh infection,42 and greater ASA class12 have been described as independent risk factors for postoperative complications43,44 and hernia recurrence following ventral hernia repair.44,45,46 Increased intra-abdominal pressure in patients with obesity may affect fascial integrity and impair wound healing, while smoking decreases tissue oxygenation and reduces the inflammatory cell response, leading to decreased wound healing potential and increased infection risk.44,47 Our study strengthens the existing literature indicating that obesity is associated with increased recurrence, particularly at a body mass index greater than 35 (calculated as weight in kilograms divided by height in meters squared). Interestingly, this association was demonstrated in our mesh population only. It is possible that in patients with higher body mass index, increased tension and strain on the repair may lead to increased stress on the mesh, potentially resulting in mesh disruption, thus predisposing to recurrence. Absence of this association in the no-mesh group may be due to a smaller sample size.
Meta-analyses and prospective studies12,40,48,49,50 have found increased ventral hernia recurrence rates in smokers following open and laparoscopic ventral hernia repair; however, our study found no such association. Kudsi et al51 found no difference in recurrence between individuals who smoke and those who do not following robotic ventral hernia repair.
With regard to immunosuppression, literature analyzing its effect on hernia recurrence is sparse and mixed. Retrospective studies42,52 have described immunosuppressants as associated with hernia recurrence, whereas a recent meta-analysis12 found no association. We found that immunosuppressants were associated with increased hernia recurrence in patients with mesh. Immunosuppressive agents reduce the body’s immune response, which may facilitate biofilm formation in patients with mesh, thus potentially weakening the mesh and predisposing to recurrence.52 We hypothesize that smoking may act as an indirect risk factor of hernia recurrence by predisposing patients to SSI, while immunosuppression may act as a direct risk factor. Further studies should analyze the impact of immunosuppression and smoking among robotic, laparoscopic, and open approaches.
Studies have analyzed the association between various hernia size thresholds and recurrence with conflicting results28; however, a recent meta-analysis12 found that as defect size increased, the likelihood of recurrence increased as well. Our results support the idea that larger hernias are more likely to recur, thus highlighting the importance of hernia width, as well as mesh width, mesh type, and surgical technique in evaluating the risk for hernia recurrence.
Occasionally, component separation or myofascial release is needed to accommodate larger mesh or assist with primary fascial closure as it allows for release and medialization of the rectus complex. Studies have demonstrated that use of this technique has increased in the US over the past decade and is associated with lower recurrence rates, particularly in elective hernia repairs.13,53,54 By reapproximating the fascia primarily, with or without additional myofascial release, the abdominal wall is returned to its normal anatomy, thereby restoring its function and reducing the likelihood of recurrence. Our study found that fascial closure and myofascial release were associated with decreased recurrence rates. Other studies have shown that mesh-reinforced primary musculofascial repair, with or without component separation, is associated with lower recurrence rates compared to bridged repair.55,56,57,58
Postoperative SSIs and reoperations have been associated with increased rates of hernia recurrence.4,28,48 In a recent study, surgical site occurrences were found to be the most significant independent factor associated with hernia recurrence, with patients who experienced any surgical site occurrence having more than twice the 5-year cumulative incidence of recurrence of those without.28 Most surgical site occurrences in that study were explained by superficial SSIs. In our study, postoperative SSIs were associated with increased recurrence. We infer that SSIs may be a large driver of recurrence and suggest that even relatively minor complications may affect long-term morbidity. Holihan et al4 found that 30.2% patients who had a hernia recurrence and 34.2% of patients who had reoperation had a preceding SSI, which was associated with twice the chance of hernia recurrence, leading to a vicious cycle. Furthermore, recurrent repairs have been reported to be associated with hernia recurrence.28 Our study suggests that postoperative SSI and reoperation are factors associated with hernia recurrence, thereby contributing to the vicious cycle that subsequent repairs are likely to increase the risk of recurrence.4
Limitations
This study has limitations. Due to the inherent nature of a retrospective study, data accuracy was contingent on user entry, leading to potentially incomplete data and selection bias. Similarly, attrition biases may have also influenced our study. To overcome this, we established strict inclusion and exclusion criteria and maintained an adequate sample size to draw meaningful associations between variables. We used clinical recurrence as our metric rather than image-proven recurrence, thereby excluding asymptomatic or clinically silent hernia recurrences. However, obtaining routine imaging in patients with recurrent hernias is not commonly performed unless required for oncologic surveillance. Further, the ACQHC recognizes composite recurrence as a valid recurrence metric, which is often obtained by patient-reported outcomes.59 Because this article focuses on clinical recurrence, our follow-up period may appear short; however, we accounted for this by performing time-to-event analyses. Also, due to lack of granularity in the ACHQC database, we were unable to include only primary ventral hernia repairs, nor analyze the percentage of patients undergoing minimally invasive surgery who achieved primary musculofascial reapproximation vs those undergoing mesh repair. In addition, the inclusion of parastomal hernias in our study, which are known to have high recurrence rates, may have influenced the high year-to-year rates of recurrence found. Additionally, we could not compare the mesh and no-mesh repairs, as these were 2 different populations which precluded comparison.
Conclusions
In this study, the risk of ventral hernia recurrence increased over time, with more than 40% and 70% recurrence in patients with and without prior mesh repair, respectively, at 5 years. Higher body mass index, immunosuppressants, hernia type (incisional or parastomal), surgical technique (robotic approach), greater hernia width, mesh type (biologic or resorbable synthetic mesh), SSI, and reoperation were associated with increased recurrence. Greater mesh width, myofascial release, and fascial closure were associated with lower recurrence rates. Hernia type was the most important variable associated with recurrence. Collectively, these findings suggest that ventral hernias should be viewed as a complex and chronic disease requiring close, long-term follow-up. Further research should focus on determining factors associated with recurrence at specific time points following ventral hernia repair.
eFigure 1. Inclusion and exclusion criteria
eTable 1. Demographic data, time to follow up, and time to recurrence in patients with ventral hernia repair
eTable 2. Surgical characteristics of patients with ventral hernia repair
eFigure 2. Dot chart illustrating rank order of importance of each variable on hernia recurrence in patients with mesh (as measured by χ2-degrees of freedom)
eFigure 3. Dot chart illustrating rank order of importance of each variable on hernia recurrence in patients without mesh (as measured by χ2-degrees of freedom)
eFigure 4. Plot depicting the relationship between hazard ratio and age (above) and BMI (below) in patients with mesh.
eFigure 5. Plot depicting the relationship between hazard ratio and hernia width (above) and hernia length (below) in patients with mesh.
eFigure 6. Plot depicting the relationship between hazard ratio and mesh width (above) and mesh length (below) in patients with mesh.
eFigure 7. Plot depicting the relationship between hazard ratio and BMI (above) and hernia width (below) in patients without mesh.
Data sharing statement
References
- 1.Poulose BK, Shelton J, Phillips S, et al. Epidemiology and cost of ventral hernia repair: making the case for hernia research. Hernia. 2012;16(2):179-183. doi: 10.1007/s10029-011-0879-9 [DOI] [PubMed] [Google Scholar]
- 2.Holihan JL, Alawadi ZM, Harris JW, et al. Ventral hernia: patient selection, treatment, and management. Curr Probl Surg. 2016;53(7):307-354. doi: 10.1067/j.cpsurg.2016.06.003 [DOI] [PubMed] [Google Scholar]
- 3.Ciomperlik H, Dhanani NH, Cassata N, et al. Patient quality of life before and after ventral hernia repair. Surgery. 2021;169(5):1158-1163. doi: 10.1016/j.surg.2020.11.003 [DOI] [PubMed] [Google Scholar]
- 4.Holihan JL, Alawadi Z, Martindale RG, et al. Adverse events after ventral hernia repair: the vicious cycle of complications. J Am Coll Surg. 2015;221(2):478-485. doi: 10.1016/j.jamcollsurg.2015.04.026 [DOI] [PubMed] [Google Scholar]
- 5.Flum DR, Horvath K, Koepsell T. Have outcomes of incisional hernia repair improved with time? a population-based analysis. Ann Surg. 2003;237(1):129-135. doi: 10.1097/00000658-200301000-00018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Huerta S, Varshney A, Patel PM, Mayo HG, Livingston EH. Biological mesh implants for abdominal hernia repair: US food and drug administration approval process and systematic review of its efficacy. JAMA Surg. 2016;151(4):374-381. doi: 10.1001/jamasurg.2015.5234 [DOI] [PubMed] [Google Scholar]
- 7.Howard R, Thumma J, Ehlers A, Englesbe M, Dimick J, Telem D. Reoperation for recurrence up to 10 years after hernia repair. JAMA. 2022;327(9):872-874. doi: 10.1001/jama.2022.0744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Helgstrand F, Rosenberg J, Kehlet H, Strandfelt P, Bisgaard T. Reoperation versus clinical recurrence rate after ventral hernia repair. Ann Surg. 2012;256(6):955-958. doi: 10.1097/SLA.0b013e318254f5b9 [DOI] [PubMed] [Google Scholar]
- 9.Poulose BK, Roll S, Murphy JW, et al. Design and implementation of the Americas Hernia Society Quality Collaborative (AHSQC): improving value in hernia care. Hernia. 2016;20(2):177-189. doi: 10.1007/s10029-016-1477-7 [DOI] [PubMed] [Google Scholar]
- 10.Therneau TM, Grambsch PM. Modeling Survival Data: Extending the Cox Model. Springer; 2000. doi: 10.1007/978-1-4757-3294-8 [DOI] [Google Scholar]
- 11.Singhal V, Szeto P, VanderMeer TJ, Cagir B. Ventral hernia repair: outcomes change with long-term follow-up. JSLS. 2012;16(3):373-379. doi: 10.4293/108680812X13427982377067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Parker SG, Mallett S, Quinn L, et al. Identifying predictors of ventral hernia recurrence: systematic review and meta-analysis. BJS Open. 2021;5(2):zraa071. doi: 10.1093/bjsopen/zraa071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Howard R, Thumma J, Ehlers A, Englesbe M, Dimick J, Telem D. Trends in surgical technique and outcomes of ventral hernia repair in the United States. Ann Surg. 2023;278(2):274-279. doi: 10.1097/SLA.0000000000005654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hawn MT, Snyder CW, Graham LA, Gray SH, Finan KR, Vick CC. Long-term follow-up of technical outcomes for incisional hernia repair. J Am Coll Surg. 2010;210(5):648-655, 655-657. doi: 10.1016/j.jamcollsurg.2009.12.038 [DOI] [PubMed] [Google Scholar]
- 15.Carne PWG, Robertson GM, Frizelle FA. Parastomal hernia. Br J Surg. 2003;90(7):784-793. doi: 10.1002/bjs.4220 [DOI] [PubMed] [Google Scholar]
- 16.Helgstrand F, Rosenberg J, Kehlet H, Jorgensen LN, Wara P, Bisgaard T. Risk of morbidity, mortality, and recurrence after parastomal hernia repair: a nationwide study. Dis Colon Rectum. 2013;56(11):1265-1272. doi: 10.1097/DCR.0b013e3182a0e6e2 [DOI] [PubMed] [Google Scholar]
- 17.Rubin MS, Schoetz DJ Jr, Matthews JB. Parastomal hernia. is stoma relocation superior to fascial repair? Arch Surg. 1994;129(4):413-418. doi: 10.1001/archsurg.1994.01420280091011 [DOI] [PubMed] [Google Scholar]
- 18.Kokotovic D, Bisgaard T, Helgstrand F. Long-term recurrence and complications associated with elective incisional hernia repair. JAMA. 2016;316(15):1575-1582. doi: 10.1001/jama.2016.15217 [DOI] [PubMed] [Google Scholar]
- 19.Asencio F, Aguiló J, Peiró S, et al. Open randomized clinical trial of laparoscopic versus open incisional hernia repair. Surg Endosc. 2009;23(7):1441-1448. doi: 10.1007/s00464-008-0230-4 [DOI] [PubMed] [Google Scholar]
- 20.Sauerland S, Walgenbach M, Habermalz B, Seiler CM, Miserez M. Laparoscopic versus open surgical techniques for ventral or incisional hernia repair. Cochrane Database Syst Rev. 2011;16(3):CD007781. doi: 10.1002/14651858.CD007781.pub2 [DOI] [PubMed] [Google Scholar]
- 21.Liang MK, Holihan JL, Itani K, et al. Ventral hernia management: Expert consensus guided by systematic review. Ann Surg. 2017;265(1):80-89. doi: 10.1097/SLA.0000000000001701 [DOI] [PubMed] [Google Scholar]
- 22.Eker HH, Hansson BME, Buunen M, et al. Laparoscopic vs. open incisional hernia repair: a randomized clinical trial. JAMA Surg. 2013;148(3):259-263. doi: 10.1001/jamasurg.2013.1466 [DOI] [PubMed] [Google Scholar]
- 23.Wéber G, Baracs J, Horváth OP. “Onlay mesh provides significantly better results than “sublay” reconstruction. prospective randomized multicenter study of abdominal wall reconstruction with sutures only, or with surgical mesh–results of a five-years follow-up. Magy Seb. 2010;63(5):302-311. [DOI] [PubMed] [Google Scholar]
- 24.Venclauskas L, Maleckas A, Kiudelis M. One-year follow-up after incisional hernia treatment: results of a prospective randomized study. Hernia. 2010;14(6):575-582. doi: 10.1007/s10029-010-0686-8 [DOI] [PubMed] [Google Scholar]
- 25.Holihan JL, Nguyen DH, Nguyen MT, Mo J, Kao LS, Liang MK. Mesh location in open ventral hernia repair: a systematic review and network meta-analysis. World J Surg. 2016;40(1):89-99. doi: 10.1007/s00268-015-3252-9 [DOI] [PubMed] [Google Scholar]
- 26.Hartog FPJD, Sneiders D, Darwish EF, et al. Favorable outcomes after retro-rectus (rives-stoppa) mesh repair as treatment for noncomplex ventral abdominal wall hernia, a systematic review and meta-analysis. Ann Surg. 2022;276(1):55-65. doi: 10.1097/SLA.0000000000005422 [DOI] [PubMed] [Google Scholar]
- 27.Albino FP, Patel KM, Nahabedian MY, Sosin M, Attinger CE, Bhanot P. Does mesh location matter in abdominal wall reconstruction? a systematic review of the literature and a summary of recommendations. Plast Reconstr Surg. 2013;132(5):1295-1304. doi: 10.1097/PRS.0b013e3182a4c393 [DOI] [PubMed] [Google Scholar]
- 28.Jolissaint JS, Dieffenbach BV, Tsai TC, et al. Surgical site occurrences, not body mass index, increase the long-term risk of ventral hernia recurrence. Surgery. 2020;167(4):765-771. doi: 10.1016/j.surg.2020.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Miserez M, Lefering R, Famiglietti F, et al. Synthetic versus biological mesh in laparoscopic and open ventral hernia repair (LAPSIS): results of a multinational, randomized, controlled, and double-blind trial. Ann Surg. 2021;273(1):57-65. doi: 10.1097/SLA.0000000000004062 [DOI] [PubMed] [Google Scholar]
- 30.Bondre IL, Holihan JL, Askenasy EP, et al. ; Ventral Hernia Outcomes Collaborative . Suture, synthetic, or biologic in contaminated ventral hernia repair. J Surg Res. 2016;200(2):488-494. doi: 10.1016/j.jss.2015.09.007 [DOI] [PubMed] [Google Scholar]
- 31.Rosen MJ, Bauer JJ, Harmaty M, et al. Multicenter, prospective, longitudinal study of the recurrence, surgical site infection, and quality of life after contaminated ventral hernia repair using biosynthetic absorbable mesh: the COBRA study. Ann Surg. 2017;265(1):205-211. doi: 10.1097/SLA.0000000000001601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sivaraj D, Henn D, Fischer KS, et al. Reinforced biologic mesh reduces postoperative complications compared to biologic mesh after ventral hernia repair. Plast Reconstr Surg Glob Open. 2022;10(2):e4083. doi: 10.1097/GOX.0000000000004083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Harris HW, Primus F, Young C, et al. Preventing recurrence in clean and contaminated hernias using biologic versus synthetic mesh in ventral hernia repair: the PRICE randomized clinical trial. Ann Surg. 2021;273(4):648-655. doi: 10.1097/SLA.0000000000004336 [DOI] [PubMed] [Google Scholar]
- 34.Rosen MJ, Krpata DM, Petro CC, et al. Biologic vs synthetic mesh for single-stage repair of contaminated ventral hernias: a randomized clinical trial. JAMA Surg. 2022;157(4):293-301. doi: 10.1001/jamasurg.2021.6902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rastegarpour A, Cheung M, Vardhan M, Ibrahim MM, Butler CE, Levinson H. Surgical mesh for ventral incisional hernia repairs: understanding mesh design. Plast Surg (Oakv). 2016;24(1):41-50. doi: 10.1177/229255031602400110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kroese LF, Mommers EH, Robbens C, Bouvy ND, Lange JF, Berrevoet F. Complications and recurrence rates of patients with Ehlers-Danlos syndrome undergoing ventral hernioplasty: a case series. Hernia. 2018;22(4):611-616. doi: 10.1007/s10029-018-1739-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.LeBlanc K. Proper mesh overlap is a key determinant in hernia recurrence following laparoscopic ventral and incisional hernia repair. Hernia. 2016;20(1):85-99. doi: 10.1007/s10029-015-1399-9 [DOI] [PubMed] [Google Scholar]
- 38.Hauters P, Desmet J, Gherardi D, Dewaele S, Poilvache H, Malvaux P. Assessment of predictive factors for recurrence in laparoscopic ventral hernia repair using a bridging technique. Surg Endosc. 2017;31(9):3656-3663. doi: 10.1007/s00464-016-5401-0 [DOI] [PubMed] [Google Scholar]
- 39.Kozan R, Anadol AZ, Sare M. A new criterion to predict recurrence after laparoscopic ventral hernia repair: mesh/defect area ratio. Pol Przegl Chir. 2021;93(6):40-46. doi: 10.5604/01.3001.0015.0237 [DOI] [PubMed] [Google Scholar]
- 40.Soppe S, Slieker S, Keerl A, Muller MK, Wirsching A, Nocito A. Emergency repair and smoking predict recurrence in a large cohort of ventral hernia patients. Hernia. 2022;26(5):1337-1345. doi: 10.1007/s10029-022-02672-0 [DOI] [PubMed] [Google Scholar]
- 41.Langbach O, Bukholm I, Benth JŠ, Røkke O. Long term recurrence, pain and patient satisfaction after ventral hernia mesh repair. World J Gastrointest Surg. 2015;7(12):384-393. doi: 10.4240/wjgs.v7.i12.384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lee LD, Stroux A, Nickisch D, et al. Operative outcome of hernia repair with synthetic mesh in immunocompromised patients. ANZ J Surg. 2020;90(11):2248-2253. doi: 10.1111/ans.16212 [DOI] [PubMed] [Google Scholar]
- 43.Rosen MJ, Aydogdu K, Grafmiller K, Petro CC, Faiman GH, Prabhu A. A multidisciplinary approach to medical weight loss prior to complex abdominal wall reconstruction: is it feasible? J Gastrointest Surg. 2015;19(8):1399-1406. doi: 10.1007/s11605-015-2856-6 [DOI] [PubMed] [Google Scholar]
- 44.Menzo EL, Hinojosa M, Carbonell A, Krpata D, Carter J, Rogers AM. American Society for Metabolic and Bariatric Surgery and American Hernia Society consensus guideline on bariatric surgery and hernia surgery. Surg Obes Relat Dis. 2018;14(9):1221-1232. doi: 10.1016/j.soard.2018.07.005 [DOI] [PubMed] [Google Scholar]
- 45.Ko JH, Wang EC, Salvay DM, Paul BC, Dumanian GA. Abdominal wall reconstruction: lessons learned from 200 “components separation” procedures. Arch Surg. 2009;144(11):1047-1055. doi: 10.1001/archsurg.2009.192 [DOI] [PubMed] [Google Scholar]
- 46.Sauerland S, Korenkov M, Kleinen T, Arndt M, Paul A. Obesity is a risk factor for recurrence after incisional hernia repair. Hernia. 2004;8(1):42-46. doi: 10.1007/s10029-003-0161-x [DOI] [PubMed] [Google Scholar]
- 47.Sørensen LT. Wound healing and infection in surgery: the pathophysiological impact of smoking, smoking cessation, and nicotine replacement therapy: a systematic review. Ann Surg. 2012;255(6):1069-1079. doi: 10.1097/SLA.0b013e31824f632d [DOI] [PubMed] [Google Scholar]
- 48.Stey AM, Russell MM, Sugar CA, et al. Extending the value of the National Surgical Quality Improvement Program claims dataset to study long-term outcomes: rate of repeat ventral hernia repair. Surgery. 2015;157(6):1157-1165. doi: 10.1016/j.surg.2014.12.027 [DOI] [PubMed] [Google Scholar]
- 49.Bencini L, Sanchez LJ, Bernini M, et al. Predictors of recurrence after laparoscopic ventral hernia repair. Surg Laparosc Endosc Percutan Tech. 2009;19(2):128-132. doi: 10.1097/SLE.0b013e31819cb04b [DOI] [PubMed] [Google Scholar]
- 50.Sørensen LT, Hemmingsen UB, Kirkeby LT, Kallehave F, Jørgensen LN. Smoking is a risk factor for incisional hernia. Arch Surg. 2005;140(2):119-123. doi: 10.1001/archsurg.140.2.119 [DOI] [PubMed] [Google Scholar]
- 51.Kudsi OY, Kaoukabani G, Bou-Ayash N, Gokcal F. Does smoking influence the clinical outcomes of robotic ventral hernia repair? a propensity score matching analysis study. J Robot Surg. 2023;17(5):2229-2236. doi: 10.1007/s11701-023-01645-4 [DOI] [PubMed] [Google Scholar]
- 52.Bueno-Lledó J, Bonafe-Diana S, Carbonell-Tatay F, Torregrosa-Gallud A, Pous-Serrano S. Component separation and large incisional hernia: predictive factors of recurrence. Hernia. 2021;25(6):1593-1600. doi: 10.1007/s10029-021-02489-3 [DOI] [PubMed] [Google Scholar]
- 53.Maloney SR, Schlosser KA, Prasad T, et al. Twelve years of component separation technique in abdominal wall reconstruction. Surgery. 2019;166(4):435-444. doi: 10.1016/j.surg.2019.05.043 [DOI] [PubMed] [Google Scholar]
- 54.Novitsky YW, Elliott HL, Orenstein SB, Rosen MJ. Transversus abdominis muscle release: a novel approach to posterior component separation during complex abdominal wall reconstruction. Am J Surg. 2012;204(5):709-716. doi: 10.1016/j.amjsurg.2012.02.008 [DOI] [PubMed] [Google Scholar]
- 55.Itani KMF, Rosen M, Vargo D, Awad SS, Denoto G III, Butler CE; RICH Study Group . Prospective study of single-stage repair of contaminated hernias using a biologic porcine tissue matrix: the RICH study. Surgery. 2012;152(3):498-505. doi: 10.1016/j.surg.2012.04.008 [DOI] [PubMed] [Google Scholar]
- 56.Booth JH, Garvey PB, Baumann DP, et al. Primary fascial closure with mesh reinforcement is superior to bridged mesh repair for abdominal wall reconstruction. J Am Coll Surg. 2013;217(6):999-1009. doi: 10.1016/j.jamcollsurg.2013.08.015 [DOI] [PubMed] [Google Scholar]
- 57.Holihan JL, Askenasy EP, Greenberg JA, et al. ; Ventral Hernia Outcome Collaboration Writing Group . Component separation vs. bridged repair for large ventral hernias: a multi-institutional risk-adjusted comparison, systematic review, and meta-analysis. Surg Infect (Larchmt). 2016;17(1):17-26. doi: 10.1089/sur.2015.124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Nguyen DH, Nguyen MT, Askenasy EP, Kao LS, Liang MK. Primary fascial closure with laparoscopic ventral hernia repair: systematic review. World J Surg. 2014;38(12):3097-3104. doi: 10.1007/s00268-014-2722-9 [DOI] [PubMed] [Google Scholar]
- 59.Poulose BK, Schwartzman H, Huang LC, et al. ; Multistakeholder Collaborative Effort to Enhance Long-Term Follow-Up in the Abdominal Core Health Quality Collaborative . Multistakeholder collaborative effort to enhance long-term follow-up in the Abdominal Core Health Quality collaborative. Ann Surg Open. 2021;2(1):e052. doi: 10.1097/AS9.0000000000000052 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure 1. Inclusion and exclusion criteria
eTable 1. Demographic data, time to follow up, and time to recurrence in patients with ventral hernia repair
eTable 2. Surgical characteristics of patients with ventral hernia repair
eFigure 2. Dot chart illustrating rank order of importance of each variable on hernia recurrence in patients with mesh (as measured by χ2-degrees of freedom)
eFigure 3. Dot chart illustrating rank order of importance of each variable on hernia recurrence in patients without mesh (as measured by χ2-degrees of freedom)
eFigure 4. Plot depicting the relationship between hazard ratio and age (above) and BMI (below) in patients with mesh.
eFigure 5. Plot depicting the relationship between hazard ratio and hernia width (above) and hernia length (below) in patients with mesh.
eFigure 6. Plot depicting the relationship between hazard ratio and mesh width (above) and mesh length (below) in patients with mesh.
eFigure 7. Plot depicting the relationship between hazard ratio and BMI (above) and hernia width (below) in patients without mesh.
Data sharing statement


