Abstract
OBJECTIVE.
Evaluate the efficacy of Mindfulness-Oriented Recovery Enhancement (MORE) for past and current military personnel prescribed long-term opioid therapy (LTOT) for chronic pain.
METHODS.
In a clinical trial, 230 past and current U.S. military personnel prescribed LTOT were randomized (1:1) to MORE or supportive psychotherapy (in-person and then online via Zoom after onset of COVID-19). Primary outcomes were 1) chronic pain measured by the Brief Pain Inventory (BPI) and 2) aberrant drug-related behaviors measured by the Current Opioid Misuse Measure (COMM) through 8-month follow-up. Opioid dose was a key secondary outcome. Other outcomes included psychiatric symptoms, catastrophizing, positive affect, ecological momentary assessments of opioid craving, and opioid attentional bias.
RESULTS.
MORE was superior to supportive psychotherapy through 8-month follow-up in reducing pain-related functional interference (p=0.01), pain severity (p=0.048), and opioid dose (p=0.029). MORE reduced opioid dose by 20.7%, compared to 3.9% in supportive psychotherapy. Although there was no overall between-groups difference in opioid misuse (p=0.43), the in-person MORE cohorts outperformed supportive psychotherapy for reducing opioid misuse (p=0.047). MORE reduced anhedonia, pain catastrophizing, craving, and opioid attentional bias, while increasing positive affect to a greater extent than supportive psychotherapy. MORE also modulated therapeutic processes including mindful reinterpretation of pain sensations, nonreactivity, savoring, positive attention, and reappraisal.
CONCLUSIONS.
For past and current U.S. military personnel, MORE led to sustained decreases in chronic pain, opioid use, craving, and opioid cue-reactivity. MORE facilitates opioid dose reduction while preserving adequate pain control and preventing mood decrements, suggesting MORE’s utility for safe opioid tapering.
Keywords: mindfulness, opioid misuse, opioid tapering, savoring, reward
Chronic pain and opioid misuse are threats to U.S. military personnel and Veterans, who may develop problematic opioid use coincident with long-term opioid therapy (LTOT) for painful conditions incurred during military service. Many military personnel and Veterans who suffer from persistent pain conditions are treated with LTOT, which increases risk for escalating to opioid misuse (1). Chronic pain is prevalent among military personnel, with 30% evidencing a chronic pain diagnosis (2) and 44% reporting chronic pain following deployment (3). Among active duty Soldiers returning from deployment, 35% received an opioid prescription (4). Among Veterans, 33% were prescribed an opioid in 2012 (5). While subsequent Veterans Health Administration (VHA) initiatives decreased LTOT rates (6), 25–29% of Veterans receiving LTOT for pain exhibit aberrant drug-related behaviors that mark the transition from medically-appropriate opioid use to misuse (7), such as unauthorized dose escalation and opioid self-medication of negative affective states. Opioid misuse among patients receiving LTOT for chronic pain may arise from the neuroplastic effects of prolonged opioid use on brain reward circuits (8)—increasing opioid cue-reactivity and craving while reducing sensitivity to pleasure derived from natural rewards (8). In turn, such reward dysregulation is thought to result in higher levels of anhedonia and dysphoria that compel opioid dose escalation as a means of maintaining hedonic equilibrium (9). Due in part to the complexities presented by these intersecting, pathogenic mechanisms, there is a dearth of efficacious interventions for Veterans and military personnel with chronic pain treated with LTOT.
To meet this need, we conducted a randomized clinical trial (RCT) of Mindfulness-Oriented Recovery Enhancement (MORE) in a sample of Veterans and military personnel receiving LTOT for chronic pain. MORE unites complementary aspects of mindfulness training, cognitive-behavioral therapy, and principles from positive psychology to restructure dysregulated reward processes underpinning the cycle of behavioral escalation linking chronic pain to opioid misuse. In a recent meta-analysis, MORE was shown to produce statistically significant effects on addictive behavior, chronic pain, and psychiatric symptoms in civilians (10). Yet, MORE’s efficacy in Veterans and military personnel remains unknown. Here we compared MORE’s effects to that of supportive psychotherapy on reducing chronic pain, aberrant drug-related behaviors, and opioid dose, as well as psychiatric symptoms, pain catastrophizing, reward-related processes, opioid craving, and cue-reactivity.
METHODS
Study Design, Setting, Participants
This was a single-blind, parallel randomized controlled superiority trial. The University of Utah institutional review board approved the protocol. From April 1, 2017 to October 1, 2021, participants were recruited from the Salt Lake City VA Medical Center (VAMC), the Utah Army National Guard, and the surrounding Salt Lake valley, Utah. Participants were recruited from electronic medical record (EMR) data pull, physician referral, and advertisements. Following onset of COVID-19, the trial shifted from in-person to a remote format. Eligible participants were U.S. military personnel or Veterans age ≥18 with a physician-confirmed, chronic pain-related diagnosis and daily prescription opioid use for ≥3 months, and average pain ≥3 on a 0–10 numeric rating scale. We excluded participants receiving cancer treatment (due to potential confounding by iatrogenic treatment effects or disease progression), and those experiencing elevated suicide risk, psychosis, and severe non-opioid substance use disorder (as assessed by the Mini-International Neuropsychiatric Interview-MINI) (11), or who had prior exposure to mindfulness interventions (e.g., Mindfulness-Based Stress Reduction). After obtaining informed consent (which covered EMR data extraction), study staff collected demographics and outcomes, and the in-person cohorts completed a dot probe task to measure opioid cue-reactivity. Participants were compensated for completing all study activities.
Masking and Randomization
A researcher uninvolved in assessments or analysis used a computerized random number generator to produce treatment allocations to MORE or supportive psychotherapy with blocked random assignment (1:1 ratio, block sizes 4–8). Participants were not allocated until the day of the first treatment session by the coordinator to maintain allocation concealment and prevent bias. Staff blinded to allocation (which remained concealed throughout the study) conducted assessments. The allocation list was not accessible to staff involved in study treatments or assessments, and participants were prompted to keep their treatment assignment undisclosed before each assessment.
Interventions
The study interventions were delivered in eight, two-hour weekly group therapy sessions comprising 6–12 participants. Sessions were delivered in-person until the onset of COVID-19, at which point sessions were implemented through a HIPAA-complaint Zoom platform. To control for therapist effects, the same two licensed psychologists delivered an equal number of MORE and supportive psychotherapy groups.
The manualized MORE intervention (12) provided training in mindfulness, reappraisal, and savoring techniques (n=69 in person and n=47 via Zoom). Mindfulness training entailed mindful breathing and body scan meditations to attenuate pain and opioid craving by reinterpreting these aversive sensations as innocuous sensory signals, and to self-regulate reactivity to opioid cues. Reappraisal training entailed reframing stress appraisals to reduce catastrophizing and negative emotional reactivity while promoting meaning-making in the face of adversity. Savoring training entailed mindfully focusing attention on pleasant events and pleasurable sensations to boost positive emotions and reduce anhedonia. Psychoeducation addressed opioid misuse and chronic pain. Participants were instructed to complete 15-minute, audio-guided mindfulness, reappraisal, and savoring practices each day. Also, before taking each daily opioid dose, participants were instructed to practice a 3-minute mindfulness technique designed to promote opioid sparing, helping patients to delay PRN opioid doses by using mindful breathing to reduce pain and increase self-control over opioid craving and cue-reactivity. We defined the minimum intervention dose of MORE (and supportive psychotherapy) as ≥4 treatment sessions, in accordance with treatment completion thresholds established in prior mindfulness trials (13, 14).
The active control condition in this trial consisted of supportive psychotherapy, in which therapist-led discussions elicited participants’ thoughts and emotions about coping with chronic pain, opioid misuse, and emotional distress (n=75 in person and n=39 via Zoom). Clinicians encouraged expression of emotions via empathic responding and fostered social support between group members. No skill training or education on mindfulness was provided. To match MORE homework requirements, for 15-minutes each day, participants were instructed to journal about themes discussed at weekly therapy sessions. We selected this control condition, which was designed emulate a widely-available form of process-oriented, client-centered therapy (15), to control for non-specific therapeutic factors (e.g., therapeutic relationship, social support). Prior trials of MORE and other mindfulness interventions have validated this control condition and found no significant difference in treatment credibility ratings between mindfulness interventions and supportive psychotherapy (16, 17).
Sessions were audio-recorded, and treatment fidelity was scored with validated measures (18). Adherence and competence scores were excellent, indicating that both manualized protocols were implemented as intended with no treatment diffusion.
Outcomes
Primary and secondary outcomes were collected over an eight-month period: baseline, post-treatment, and then every two months for the next six months. Our pre-specified primary chronic pain outcome was measured with Brief Pain Inventory (BPI) pain interference and pain severity subscales (19). Our co-primary opioid misuse outcome consisted of the Current Opioid Misuse Measure (COMM), a self-reported measure of aberrant drug-related behaviors including use of opioids for reasons other than pain, taking more opioids than prescribed, obtaining opioids from sources other than a prescribing physician, signs of intoxication and emotional votaility, etc. (20). We chose this continuous measure as our primary measure of opioid misuse severity, unlike the measurement approach used in our prior trial of MORE (14), where all participants entered the trial with a positive score on a binary measure of opioid misuse and opioid misuse outcomes were assessed with this binary measure. We reasoned that for the present study of patients on LTOT where opioid misuse was not an inclusion criterion, changes in a continuous measure of aberrant drug-related behaviors were clinically meaningful. To triangulate self-reports of aberrant drug-related behaviors, we also performed clinical assessment of opioid misuse with the Addiction Behaviors Checklist (ABC) (21), a semi-structured interview performed by clinical staff (i.e., psychologists, social workers, and nurses) blinded to treatment assignment. In addition, at each assessment point for the in-person cohort, we performed urine screens, and as an exploratory outcome, we extracted available random urine screen data from the electronic medical record (EMR) at 12-month follow-up. Urine screens were classified as positive when participants screened positive for illicit drugs (e.g., heroin, cocaine, methamphetamine) or non-prescribed opioid medications.
Changes in morphine equivalent daily opioid dose (MEDD) were computed according to best practice guidelines (22) as assessed by the Timeline Followback (23) and triangulated with the EMR, which was used to obtain opioid dose when participants missed follow-up assessments.
Other secondary outcome measures included the Depression Anxiety Stress Scale-21 (24), the Post-Traumatic Stress Symptom Checklist-Military Version (25), the Pain Catastrophizing subscale of the Coping Strategies Questionnaire (26), the Snaith Hamilton Anhedonia and Pleasure Scale (27), the Positive Affect subscale of the Positive and Negative Affect Schedule (28). Process measures included the Attention to Positive Information Scale (29), the Cognitive Reappraisal subscale of the Emotion Regulation Questionnaire (30), the Momentary Savoring Scale (31), the Mindful Reappraisal of Pain Scale (32), and the Nonreactivity subscale of the Five Facet Mindfulness Questionnaire (33)—selected due to its previously demonstrated association with MORE’s pain-relieving effects (16). Opioid craving in daily life was assessed on a 0–10 scale by ecological momentary assessments (EMA) delivered by smartphone three random times a day during the 8-week study interventions.
Before the trial switched to a remote format at the onset of COVID, opioid cue-reactivity was assessed in the laboratory with an opioid dot-probe task designed to measure attentional bias towards opioid cues (34). Each trial began with a fixation cross (500 ms) followed by a pair of opioid and neutral images which appeared side-by-side for either 200 or 2000ms. Opioid cues included images of opioid pills and pill bottles validated in prior studies (34). Neutral images were matched to opioid images by visual features including color, figure-ground relationships, and presence of human faces. Presentation duration and left/right position of the images were randomized and counterbalanced within each block of 58 trials. After a 50 ms inter-stimulus interval, a target probe replaced one of the images. Participants indicated the location of the target by responding with a left/right button press, and reaction times were recorded.
Statistical Analysis
Based on our pilot data, N=200 (after 30% attrition) would provide power >0.90 at alpha=.05 to estimate small clinical effects (Cohen’s d = .20) for baseline-adjusted treatment effects averaged over four post-randomization timepoints on the BPI, COMM, and other continuous outcomes (Cohen’s d in pilot trials of MORE was 0.50–0.84) (16). We planned to enroll 260 patients to account for loss to follow-up; our actual enrolled N was 230 due to COVID-19.
To control for baseline randomization imbalance, we employed constrained longitudinal data analysis (cLDA) via SAS 9.4 and MPlus. cLDA provides results similar to classic analysis of covariance (ANCOVA) when there is minimal missing data (35, 36). Yet unlike ANCOVA, cLDA is a full information maximum-likelihood procedure that retains every observation and is hence more efficient and less prone to missing data biases. Baseline (time 1) and four post-baseline assessments (2-, 4-, 6-, and 8-month follow-ups) are as described above. Baseline measurements were taken prior to randomization to supportive psychotherapy or MORE conditions, so treatment group means are assumed equal at baseline in cLDA but allowed to differ at follow-up assessments. As detailed above, COVID-19 restrictions, which were instituted mid-study, necessitated a change in format. Therapy sessions were initially conducted in-person but were subsequently implemented remotely via Zoom to comply with requirements. Since this format change could not be randomized, we treat online status as an observational stratification variable. Therefore, treatment group population means were randomized and necessarily equal within in-person and online conditions, but online and in-person effects were uncontrolled and their baseline means were unconstrained. Effects were averaged across in-person and online conditions to compute the principal estimate of overall treatment impact. Serial dependence is modeled by normally distributed random intercepts, along with normally distributed random error. To control for multiple comparisons, we first conducted three independent structural equation models to perform a multivariate omnibus test of no treatment impact on primary, secondary, and process variables. These omnibus tests, which control for multiple comparisons, are likelihood ratio tests with four degrees of freedom between the unrestricted model and the constrained model of H0. Examination of individual outcomes is then pursued if and only if the omnibus test is rejected at alpha=0.05. Opioid dose was square root transformed to reduce skew prior to cLDA.
Conditional on significance of the omnibus multivariate test, we examined the univariate treatment impact on each outcome using the cLDA approach under a mixed effects model likelihood framework. For each outcome, the null hypothesis posited equal baseline-adjusted mean treatment arm differences over the four post-baseline timepoints, assuming equal treatment arm means at pre-randomization baseline, with compound symmetry covariance structure. The single degree-of-freedom estimates and tests were implemented using SAS “Estimate” coefficients, and evaluated against the null at alpha=.05, two-sided, with conservative Kenward-Roger degrees of freedom. Time was treated as a categorical factor with four post-baseline levels. The overall estimate of between-groups treatment impact is reported in unstandardized response variable metrics. No additional covariates were considered for these primary analyses.
EMA of craving was analyzed with a mixed model including fixed effects of time, treatment, and the treatment X time interaction, as well a random intercept and an AR1 covariance structure. Here the treatment X time interaction (difference in craving trajectory across the possible 180 EMAs per subject) was the primary fixed effect of interest. Similarly specified mixed models were also used to assess treatment effects on opioid atttentional bias scores, with the treatment by time interaction the effect of interest. Attentional bias scores were computed separately for 200 and 2000ms cues using the canonical approach (RTneutral-RTopioid), with higher values indicating a greater attentional bias toward opioids (34).
We followed an intent-to-treat approach and sought to obtain follow-up data on all participants. Study discontinuation rates did not differ significantly by arm, and were similar to rates observed in psychosocial OUD treatment trials (37). No missing data were imputed, because full information maximum likelihood (FIML) methods are theoretically accurate even when dropout rates are substantial, and provided predictors of dropout, such as treatment assignment and prior observations, are modeled as observed variables (38). Sensitivity to missing at random (MAR) was evaluated in FIML multivariate analyses that introduced a larger set of auxiliary demographic and clinical variables expected to correlate with missingness - an alternative to multiple imputation that often produces more accurate and precise parameter estimates (38).
RESULTS
Participant Characteristics
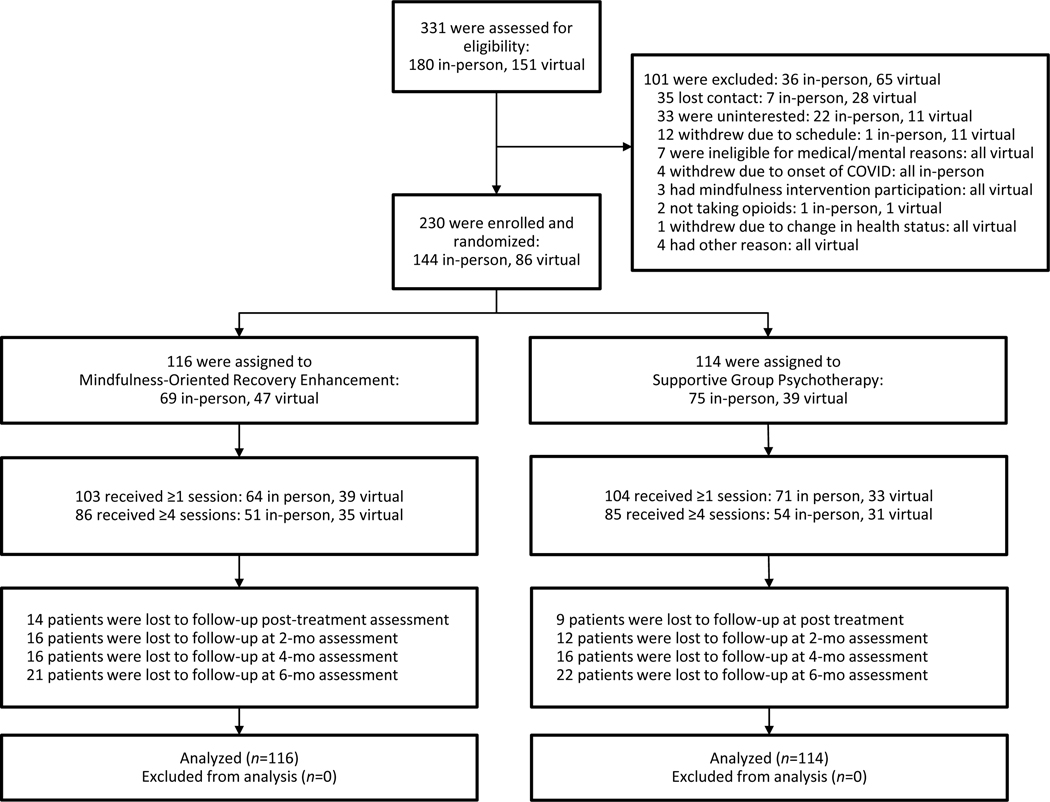
Of the 331 patients assessed for eligibility, we enrolled 230 (Figure 1). Of this sample, 81% were male and 91% were Veterans, with the remainder being current military personnel. Participants had a mean age of 57.5 (SD=11.7) years, mean BPI pain severity score of 5.6 (SD=1.5), mean COMM score of 13.4 (SD=7.8), and a mean MEDD of 105.3 mg (SD=204.6. mg, interquartile range 12.0–90.0 mg). More than half of participants (55%) reported having oxycodone or hydrocodone prescriptions. Participants reported pain for a mean of 19.3 (SD=12.6) years, and most commonly in their low back (81%). Major depressive disorder was prevalent in the sample (60%), but a substantial proportion of participants also met clinical criteria for OUD (34%) or PTSD (19%) on the MINI at baseline (11), with no between-groups differences. Participants in MORE and the SG attended a mean of 5.5 and 5.7 sessions respectively. Eight-month follow-up data for one or more outcome variables were available for 81% of participants. Demographics and baseline clinical characteristics were similar between the two groups (Table 1).
FIGURE 1.
Flow diagram for a randomized clinical trial of Mindfulness-Oriented Recovery Enhancement among veterans and military personnel receiving long-term opioid therapy for chronic pain.
Table 1.
Demographic and clinical characteristics of the sample of opioid-treated chronic pain patients randomized to Mindfulness-Oriented Recovery Enhancement (MORE) or Supportive Psychotherapy (N = 230).
| Measure | MORE (n=116) | Supportive Psychotherapy (n=114) | ||
|---|---|---|---|---|
|
| ||||
| Mean | SD | Mean | SD | |
| Age | 56.4 | 12.9 | 58.6 | 10.4 |
|
| ||||
| N | % | |||
|
| ||||
| Sex | ||||
| Male, N (%) | 97 | 83.6 | 94 | 82.5 |
| Female, N (%) | 17 | 14.6 | 19 | 16.6 |
| Transgender, N (%) | 2 | 1.7 | 1 | 0.8 |
| Sexual Orientation | ||||
| Heterosexual | 111 | 95.7 | 103 | 90.4 |
| Gay or lesbian | 1 | 0.9 | 3 | 2.6 |
| Bisexual | 3 | 2.6 | 3 | 2.6 |
| Other | 0 | 0.0 | 1 | 0.9 |
| No answer | 1 | 0.9 | 4 | 3.5 |
| Race | ||||
| White | 102 | 87.9 | 95 | 83.3 |
| Black or African American | 6 | 5.2 | 5 | 4.4 |
| Hispanic or Latino | 3 | 2.5 | 4 | 3.5 |
| Native American or Alaskan Native | 2 | 1.7 | 4 | 3.5 |
| Other or No Answer | 2 | 1.7 | 6 | 5.3 |
| Highest Level of Education, N (%) | ||||
| Did not complete high school | 2 | 1.7 | 0 | 0.0 |
| Completed high school | 54 | 46.6 | 38 | 33.3 |
| College degree or greater | 59 | 50.9 | 63 | 55.3 |
| Missing | 1 | 0.8 | 4 | 3.5 |
| Estimated Household Income, N (%) | ||||
| Less than $25,000 | 24 | 20.7 | 28 | 24.6 |
| $25,000–49,999 | 39 | 33.6 | 27 | 23.7 |
| $50,000–99,999 | 32 | 27.6 | 43 | 37.7 |
| $100,000 or Greater | 10 | 8.6 | 12 | 10.5 |
| Missing | 1 | 0.8 | 4 | 3.5 |
| Pain Condition/Location, N (%)* | ||||
| Back Pain | 90 | 77.6 | 96 | 84.2 |
| Osteoarthritis Pain | 63 | 56.9 | 53 | 46.5 |
| Cervical Pain | 17 | 14.7 | 19 | 16.7 |
| Neuropathic Pain | 14 | 12.1 | 8 | 7.0 |
| Fibromyalgia | 11 | 9.5 | 9 | 7.9 |
| Migraine or Tension Headache | 8 | 6.9 | 7 | 6.1 |
| Pain | ||||
| Extremity Pain | 6 | 5.2 | 8 | 7.0 |
| Other | 3 | 2.3 | 7 | 6.1 |
| Opioid Prescription, N (%)* | ||||
| Oxycodone | 37 | 31.9 | 39 | 34.2 |
| Hydrocodone | 20 | 17.2 | 28 | 24.5 |
| Tramadol | 42 | 36.2 | 34 | 29.8 |
| Morphine | 18 | 15.5 | 20 | 17.5 |
| Buprenorphine | 11 | 9.5 | 11 | 9.6 |
| Methadone | 5 | 4.3 | 7 | 6.1 |
| Other | 3 | 2.6 | 4 | 3.5 |
| Mean | SD | Mean | SD | |
|
| ||||
| Pain Severity (0–10), BPI | 5.6 | 1.6 | 5.5 | 1.5 |
| Pain Duration in Years | 17.9 | 12.3 | 20.8 | 12.8 |
| Duration of Opioid Use in Years | 9.8 (7.4) | 7.4 | 11.3 | 8.7 |
| Morphine Equivalent Daily Dose, mg. [IQR] | 104.3 [11.7, 90.0] | 186.9 | 106.3 [13.0, 83.3] | 222.0 |
| Opioid Misuse, COMM Score | 14.2 | 8.4 | 12.7 | 7.2 |
| Opioid Craving (0–10) | 4.5 | 3.1 | 3.6 | 3.2 |
| N | % | N | % | |
|
| ||||
| Opioid Use Disorder | 39 | 33.6 | 40 | 35.1 |
| Alcohol/Non-opioid Substance Use | 12 | 10.3 | 17 | 14.9 |
| Disorder | ||||
| Major Depressive Disorder | 71 | 61.7 | 68 | 59.6 |
| Generalized Anxiety Disorder | 24 | 20.6 | 11 | 9.7 |
| Post-Traumatic Stress Disorder | 24 | 20.6 | 20 | 17.4 |
| Veteran Status | 106 | 91.4 | 103 | 90.4 |
| Current Military Status | 10 | 8.6 | 11 | 9.6 |
Participants self-reported demographic information (e.g., gender). Data are mean (SD) or n (%). IQR = interquartile range [25th %tile, 75th %tile]. BPI = Brief Pain Inventory. COMM = Current Opioid Misuse Measure.
Note - Because patients could report multiple pain conditions/ locations and opioid prescriptions, these percentages could sum to greater than 100%. IQR = interquartile range.
Outcomes
For pain and opioid use outcomes through the 8-month follow-up, the omnibus multivariate likelihood ratio test was significant, X2(4)=13.09, p=0.011, indicating MORE’s superiority to supportive psychotherapy. MORE produced significantly greater reductions in pain interference (0.47, 95% CI=0.10, 0.84, p=0.011) and severity (0.27, 95% CI=0.00, 0.54, p=0.048) than supportive psychotherapy. Although aberrant drug-related behaviors decreased significantly across both groups over time (0.50, 95% CI=0.08, 0.92, p=0.019) with no significant between-groups differences (p=0.43), within the in-person cohorts, MORE reduced aberrant drug-related behaviors to a significantly greater extent than supportive psychotherapy (0.48, 95% CI=0.01, 0.96, p=0.047). No between-groups differences were observed for the clinical interview of opioid misuse or urine drug screen measures, except at an exploratory 12-month follow-up point extracted from the EMR, where among patients administered random urine drug screens (n=38), a smaller percentage of participants in MORE (13.3%, n=2) had a positive urine screen compared to those in supportive psychotherapy (43.5%, n=13, likelihood ratio χ2(1)=4.13, p=0.042). With regard to opioid use, MORE reduced opioid dosing (sqrt) to a significantly greater extent than supportive psychotherapy (0.65, 95% CI= 0.07, 1.23, p=.029), with a 20.7% reduction in the opioid dose sample mean (18.88±8.40 mg) in MORE compared to a 3.9% reduction (3.19±4.38 mg) in supportive psychotherapy. Sensitivity analyses controlling for auxillary variables associated with missingness again found that MORE outperformed supportive psychotherapy in reducing pain interference (p=0.010), pain severity (p=0.025), and opioid dose (p=0.025).
For secondary outcomes through the 8-month follow-up, the omnibus multivariate likelihood ratio test was highly significant, χ2(5)=32.51, p<0.00001. No significant between-groups differences were observed for emotional distress (p=0.102) or PTSD symptoms (p=0.175); participants in both treatments improved over time. However, MORE reduced anhedonia (2.27, 95% CI=1.11, 3.42, p<0.001) and pain catastrophizing (2.54, 95% CI=1.19, 3.98, p<.001), and improved positive affect (1.50, 95% CI=0.15, 2.85, p=0.029), to a significantly greater extent than supportive psychotherapy.
For process variables, the omnibus multivariate likelihood ratio test was highly significant X2(5)=32.79, p<0.00001. MORE produced greater increases in all process variables, including mindful reinterpretation of pain sensations (p<0.001), nonreactivity to distressing thoughts and emotions (p=0.030), cognitive reappraisal (p=0.011), savoring (p=0.036), and attention to positive information (p=0.001).
Regarding ecological momentary assessment of opioid craving, EMA craving ratings decreased by 0.67 points more over the course of treatment in the MORE group compared to supportive psychotherapy (95% CI=0.001, 0.007, p=0.019). Finally, participants assigned to MORE exhibited significantly greater decreases in 200 ms opioid attentional bias than those in supportive psychotherapy (29.89 ms; 95% CI=3.77, 56.01; p=0.025). No significant group differences were observed for the 2000 ms attentional bias (p=0.37).
DISCUSSION
In a sample of past and current U.S. miliary personnel on LTOT, treatment with Mindfulness-Oriented Recovery Enhancement (MORE) was associated with significantly greater reductions in chronic pain symptoms and opioid use than supportive group psychotherapy. MORE’s pain relieving effects were coupled with reductions in pain catastrophizing and an increased capacity to mindfully reinterpret pain as an innocuous sensory signal that does not necessarily signify harm. Although on the whole aberrant drug-related behaviors decreased substantially over time for both treatment groups, significatly greater reductions in aberrant drug-related behaviors were observed for the in-person MORE intervention when compared to supportive psychotherapy. Though both MORE and supportive psychotherapy were associated with reduced emotional distress and PTSD symptoms, MORE showed clear superiority for improving reward-related processes including positive affect, anhedonia, savoring, and attention to positive information. Finally, MORE was associated with reduced opioid craving measured in daily life and decreased opioid cue-reactivity measured in the laboratory with a dot-probe task.
These findings converge with our prior reseach in civilians demonstrating the efficacy of MORE for pain and opioid use (14). MORE facilitates opioid dose reduction while preserving adequate pain control and preventing decrements in mood, suggesting MORE’s utility as an adjunctive therapy for safe opioid tapering among Veterans and miltary personnel. MORE produced the largest opioid dose reductions among patients with low back pain or arthritis. The observed dose reductions are especially remarkable given that participants were not given specific tapering instructions as part of the study interventions. Future trials might combine MORE with a patient-centered opioid tapering approach to produce even greater reductions in opioid dosing.
The effects of MORE on opioid misuse in this sample were less robust than those reported in our prior trial, where we found that MORE reduced opioid misuse by 45%, more than doubling the effect of supportive psychotherapy (14). Delivering MORE via teletherapy may have attenuated its effect size. Alternatively, supportive psychotherapy may have been more effective during the COVID-19 pandemic, when social isolation drove despair that fueled opioid misuse and an unprecented number of overdose deaths. Or, military populations may be more difficult to treat than civilians due to chronic exposure to extreme stress. Nonetheless, urine screen data from the EMR suggest that MORE may produce long-term reductions in illict drug use and non-prescribed opioid use; additional studies with distal follow-ups are needed to replicate this effect.
Notably, MORE decreased attentional bias for opioid cues presented for 200ms but not for cues presented for 2000ms, suggesting that MORE’s effects are most evident during initial automatic attentional orienting to the cue and not during the stage of attentional disengagement (39). Thus, instead of an effortful shifting of attention away from drug cues (e.g., avoidance), MORE might decrease drug cue-reactivity in a bottom-up fashion by dampening the incentive salience of the drug. Congruent with this result, prior studies indicated that MORE reduces electrocortical indices of opioid cue-reactivity (40). According to our restructuring reward hypothesis (9), MORE restructures bottom-up reward processing from valuation of drug-related reward back to valuation of natural reward by strengthening cognitive control over reward processing via techniques that devalue the drug (e.g., mindfulness of craving and reappraisal of negative consequences of drug use) and increase the competing value of non-drug natural rewards (e.g., savoring). In that regard, prior studies have shown MORE to increase EEG markers of cognitive control (41) and natural reward responsiveness (9, 40). Concomitantly, in the present study, MORE significantly boosted positive affect, savoring, and attention to positive information while reducing anhedonia, suggesting that MORE improves responsiveness to natural rewards and providing additional support for the restructuring reward hypothesis.
The primary limitation of the trial was the lost-to-follow-up rate, which was exacerbated by COVID-19. Nonetheless, our trial retention rate was superior to that of other psychotherapy trials of opioid users (mean discontinuation 42%) (37) and MOUD trials of shorter (24 week) durations (42). Because dropout did not differ between study arms, missing data were unlikely to bias outcome analyses towards one group. Sensitivity analyses controlling for ancillary covariates associated with missingness showed MORE’s superiority over supportive therapy. The study was also limited because it was not possible to blind participants to treatment assignment; nonetheless, participants were informed that the study compared two active treatments and the experimental condition was not identified. Because the sample was predominately White and male, findings may not generalize to non-White racial groups. Finally, because we had originally intended to test the in-person MORE intervention and only switched to online intervention delivery after onset of COVID-19, we did not have adequate statistical power to test online versus in-person formats as a treatment moderator. Future fully-powered noninferiority trials should assess whether delivering MORE virtually produces comparable results to the in-person format.
In sum, MORE demonstrated efficacy for reducing chronic pain and opioid dose among Veterans and military personnel being treated with LTOT. Implementation and dissemination research should assess how to best deliver MORE across the VHA and the Department of Defense.
Supplementary Material
Table 2.
Treatment effects of Mindfulness-Oriented Recovery Enhancement (MORE) versus Supportive Psychotherapy (Support) on primary/secondary outcomes and process variables.
| Pre-Treatment | 2 months | 4 months | 6 months | 8 months | Between-groups treatment effect (SE) [95% CI], p-value | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||||||
| Mean | SE | N | Mean | SE | N | Mean | SE | N | Mean | SE | N | Mean | SE | N | ||
| Pain Interference-BPI | ||||||||||||||||
| MORE | 6.04 | 0.30 | 116 | 5.10 | 0.21 | 92 | 5.37 | 0.22 | 84 | 5.44 | 0.22 | 81 | 5.33 | 0.22 | 79 | −0.47 (0.19) [−0.84, −0.10] |
| SG | 5.93 | 0.32 | 114 | 5.71 | 0.22 | 87 | 5.76 | 0.22 | 80 | 5.71 | 0.23 | 80 | 5.93 | 0.23 | 73 | p=.011 |
| Pain Severity-BPI | ||||||||||||||||
| MORE | 5.58 | 0.20 | 116 | 5.14 | 0.16 | 92 | 5.37 | 0.16 | 84 | 5.43 | 0.16 | 81 | 5.31 | 0.16 | 79 | −0.27 (0.14) [−0.54, 0.00] |
| SG | 5.59 | 0.22 | 114 | 5.48 | 0.16 | 87 | 5.58 | 0.16 | 80 | 5.53 | 0.16 | 80 | 5.76 | 0.17 | 73 | p=.048 |
| Aberrant Drug-Related Behaviors-COMM | ||||||||||||||||
| MORE | 10.46 | 1.04 | 116 | 10.84 | 0.63 | 92 | 9.61 | 0.65 | 84 | 9.48 | 0.65 | 81 | 8.89 | 0.66 | 79 | −0.46 (0.59) [−1.62, 0.69] |
| SG | 12.23 | 0.97 | 114 | 10.42 | 0.66 | 87 | 10.52 | 0.66 | 80 | 9.84 | 0.67 | 80 | 9.87 | 0.69 | 73 | p=.430 |
| Opioid Dose (sqrt) a | ||||||||||||||||
| MORE | 7.74 | 0.90 | 116 | 7.25 | 0.49 | 102 | 6.93 | 0.50 | 100 | 6.91 | 0.50 | 84 | 6.84 | 0.50 | 95 | −0.65 (0.30) [−1.23, −0.07] |
| SG | 8.00 | 0.94 | 114 | 7.75 | 0.50 | 105 | 7.85 | 0.50 | 93 | 7.64 | 0.50 | 98 | 7.29 | 0.51 | 92 | p=.029 |
| Emotional Distress-DASS | ||||||||||||||||
| MORE | 20.60 | 1.88 | 115 | 17.81 | 1.13 | 85 | 17.38 | 1.15 | 81 | 15.79 | 1.15 | 78 | 16.77 | 1.16 | 76 | −1.56 (0.95) [−3.42, 0.31) |
| SG | 17.52 | 1.93 | 108 | 18.89 | 1.18 | 80 | 19.13 | 1.17 | 80 | 17.41 | 1.21 | 72 | 17.88 | 1.46 | 70 | p.102 |
| Post-Traumatic Stress Symptoms-PCL | ||||||||||||||||
| MORE | 45.51 | 2.23 | 114 | 42.52 | 1.31 | 85 | 40.87 | 1.65 | 81 | 40.70 | 1.69 | 78 | 40.81 | 1.69 | 76 | −1.43 (1.06) [−3.51, 0.64] |
| SG | 41.80 | 2.22 | 108 | 42.52 | 1.35 | 80 | 43.38 | 1.36 | 79 | 41.54 | 1.38 | 72 | 41.57 | 1.38 | 70 | p.175 |
| Positive Affect-PANAS | ||||||||||||||||
| MORE | 28.54 | 1.07 | 115 | 33.15 | 0.74 | 85 | 32.11 | 0.75 | 81 | 31.95 | 0.76 | 77 | 32.11 | 0.76 | 76 | 1.50 (0.69) [0.15, 2.85] |
| SG | 34.22 | 1.22 | 108 | 36.81 | 0.78 | 79 | 36.37 | 0.77 | 80 | 34.47 | 0.80 | 71 | 36.19 | 0.80 | 69 | p=029 |
| Anhedonia-SHAPS | ||||||||||||||||
| MORE | 25.78 | 0.96 | 115 | 23.19 | 0.65 | 85 | 23.63 | 0.66 | 81 | 25.53 | 0.66 | 78 | 23.81 | 0.67 | 76 | −2.27 (0.59) [−3.42, −1.11] |
| SG | 26.87 | 0.95 | 108 | 24.85 | 0.68 | 79 | 25.30 | 0.68 | 80 | 26.57 | 0.71 | 72 | 26.51 | 0.70 | 71 | p<.001 |
| Attention to Positive Information-APNIS | ||||||||||||||||
| MORE | 40.53 | 0.91 | 115 | 43.26 | 0.59 | 85 | 43.06 | 0.60 | 80 | 43.28 | 0.60 | 78 | 43.49 | 0.60 | 76 | 1.72 (0.53) [−0.69, 2.76] |
| SG | 41.97 | 0.95 | 108 | 41.41 | 0.62 | 80 | 41.99 | 0.61 | 80 | 41.31 | 0.63 | 72 | 41.48 | 0.63 | 70 | p=.001 |
| Mindful Reappraisal of Pain Sensations-MRPS | ||||||||||||||||
| MORE | 13.87 | 1.44 | 115 | 22.36 | 1.04 | 85 | 21.58 | 1.06 | 81 | 20.57 | 1.06 | 78 | 19.84 | 1.12 | 76 | 6.38 (0.98) [4.46, 8.31] |
| SG | 12.43 | 1.38 | 108 | 15.02 | 1.09 | 80 | 14.82 | 1.08 | 80 | 16.00 | 1.12 | 73 | 15.70 | 1.12 | 71 | p<.001 |
| Nonreactivity to Distressing Thoughts and Emotions-FFMQ | ||||||||||||||||
| MORE | 22.31 | 0.63 | 115 | 22.79 | 0.48 | 85 | 23.45 | 0.49 | 81 | 23.18 | 0.49 | 79 | 23.81 | 0.49 | 76 | 0.95 (0.44) [0.09, 1.81] |
| SG | 23.41 | 0.78 | 109 | 22.72 | 0.48 | 81 | 22.47 | 0.50 | 79 | 22.55 | 0.52 | 73 | 21.98 | 0.51 | 71 | p=.030 |
| Pain Catastrophizing-CSQ | ||||||||||||||||
| MORE | 13.75 | 1.18 | 115 | 10.32 | 0.75 | 85 | 9.16 | 0.76 | 81 | 9.40 | 0.76 | 78 | 8.91 | 0.77 | 76 | −2.54 (0.69) [−3.98, −1.19] |
| SG | 12.43 | 1.22 | 108 | 11.98 | 0.78 | 79 | 11.96 | 0.78 | 80 | 11.70 | 0.80 | 73 | 12.31 | 0.80 | 71 | p<.001 |
MORE = Mindfulness-Oriented Recovery Enhancement. SG = Supportive Group Psychotherapy. Post-treatment data are maximum likelihood estimates at each time point based on the longitudinal statistical model. Pre-treatment data are descriptive sample means. The between-groups treatment effect represents the main treatment effect (MORE - SG) estimated from the constrained longitudinal data analytic (cLDA) model in the original, unstandardized response variable metric.
Opioid dose was skewed and square-root transformed (sqrt) prior to analysis.
Note - means of nonlinearly transformed variables do not yield raw means under inverse transformation.
BPI = Brief Pain Inventory, range 0–10, score >4 indicates moderate pain; COMM = Current Opioid Misuse Measure, range 0–68, score >8 indicates misuse; DASS = Depression Anxiety Stress Scale, range 0–63, score >20 indicates at least moderate levels of distress; PCL = Posttraumatic Symptom Checklist-Military Version, range 18–90, score >44 indicates a likely PTSD diagnosis; PANAS = Positive and Negative Affect Schedule-Short Form, positive affect subscale range 10–50, score >31.3 exceeds the mean in healthy samples; SHAPS = Snaith Hamilton Anhedonia and Pleasure Scale, range 14–56, score >23 indicates anhedonia in people with chronic pain; APNIS = Attention to Positive and Negative Information Scale, attention to positive information subscale range 11–55; MRPS = Mindful Reappraisal of Pain Sensations Scale, range 0–54; FFMQ = Five Facet Mindfulness Questionnaire, nonreactivity subscale range 7–35; CSQ = Coping Strategies Questionnaire, pain catastrophizing subscale range 0–36, score >10.3 exceeds the mean in chronic pain samples.
Acknowledgements
This work was supported by the Office of the Assistant Secretary of Defense for Health Affairs, through the Peer Reviewed Medical Research Program under Award No. W81XWH-16-1-0522 (PI: Garland). Dr. Garland was also supported by R01AT011772 (PI: Garland), R01DA056537 (PI: Garland), and R01DA057631 (PI: Garland) from the National Institutes of Health during the preparation of this manuscript. Opinions, interpretations, conclusions and recommendations are those of the author and are not necessarily endorsed by the Department of Defense or the National Institutes of Health.
We would like to acknowledge Jennifer Markelz, Katie Wilson, Kammy Jacobsen, Brandon Yabko, and the staff at the Center on Mindfulness and Integrative Intervention Development (paid by the DOD grant) for their assistance with study coordination, recruitment, and data collection.
PRIMARY FUNDING SOURCE.
Department of Defense (W81XWH-16-0522, PI: Garland).
Declaration of interests
Eric Garland, PhD, LCSW is the Director of the Center on Mindfulness and Integrative Health Intervention Development. The Center provides Mindfulness-Oriented Recovery Enhancement (MORE), mindfulness-based therapy, and cognitive behavioral therapy in the context of research trials for no cost to research participants; however, Dr. Garland has received honoraria and payment for delivering seminars, lectures, and teaching engagements (related to training clinicians in mindfulness) sponsored by institutions of higher education, government agencies, academic teaching hospitals, and medical centers. Dr. Garland also receives royalties from the sale of books related to MORE. Dr. Garland is a licensor to BehaVR, LLC.
Footnotes
No other authors have any related conflicts of interest to disclose.
Data sharing
De-identified patient data will be shared upon reasonable request with an approved data sharing agreement. Data will be made available upon publication of this manuscript.
TRIAL REGISTRATION NUMBER. NCT02935621
References
- 1.Chou R, Turner JA, Devine EB, et al. : The Effectiveness and Risks of Long-Term Opioid Therapy for Chronic Pain: A Systematic Review for a National Institutes of Health Pathways to Prevention Workshop. Ann Intern Med 2015; 162:276. [DOI] [PubMed] [Google Scholar]
- 2.Smith HJ, Taubman SB, Clark LL: A burden and prevalence analysis of chronic pain by distinct case definitions among active Duty US military service members, 2018. Pain Physician 2020; 23:E429. [PubMed] [Google Scholar]
- 3.Toblin RL, Quartana PJ, Riviere LA, et al. : CHronic pain and opioid use in us soldiers after combat deployment. JAMA Intern Med 2014; 174:1400–1401 [DOI] [PubMed] [Google Scholar]
- 4.Adams RS, Thomas CP, Ritter GA, et al. : Predictors of Postdeployment Prescription Opioid Receipt and Long-term Prescription Opioid Utilization Among Army Active Duty Soldiers. Mil Med 2019; 184:e101–e109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mosher HJ, Krebs EE, Carrel M, et al. : Trends in prevalent and incident opioid receipt: an observational study in Veterans Health Administration 2004–2012. J Gen Intern Med 2015; 30:597–604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Minegishi T, Garrido MM, Stein M, et al. : Opioid Discontinuation Among Patients Receiving High-Dose Long-Term Opioid Therapy in the Veterans Health Administration. J Gen Intern Med 2020; 35:903–909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tam CC, Zeng C, Li X: Prescription opioid misuse and its correlates among veterans and military in the United States: A systematic literature review. Drug Alcohol Depend 2020; 216:108311 [DOI] [PubMed] [Google Scholar]
- 8.Koob GF: Neurobiology of opioid addiction: opponent process, hyperkatifeia, and negative reinforcement. Biol Psychiatry 2020; 87:44–53 [DOI] [PubMed] [Google Scholar]
- 9.Garland EL: Mindful positive emotion regulation as a treatment for addiction: from hedonic pleasure to self-transcendent meaning. Curr Opin Behav Sci 2021; 39:168–177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Parisi A, Roberts RL, Hanley AW, et al. : Mindfulness-Oriented Recovery Enhancement for Addictive Behavior, Psychiatric Distress, and Chronic Pain: A Multilevel Meta-Analysis of Randomized Controlled Trials. Mindfulness 2022; 13:2396–2412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sheehan D, Janavs J, Baker R, et al. : Mini international neuropsychiatric interview–version 7.0. 0 DSM-5. 2014. Harm Research Press, Tampa, FL, 2015 [Google Scholar]
- 12.Garland EL: Mindfulness-oriented recovery enhancement for addiction, stress, and pain. NASW Press, National Association of Social Workers, 2013 [Google Scholar]
- 13.Kuyken W, Hayes R, Barrett B, et al. : Effectiveness and cost-effectiveness of mindfulness-based cognitive therapy compared with maintenance antidepressant treatment in the prevention of depressive relapse or recurrence (PREVENT): a randomised controlled trial. The Lancet 2015; 386:63–73 [DOI] [PubMed] [Google Scholar]
- 14.Garland EL, Hanley AW, Nakamura Y, et al. : Mindfulness-Oriented Recovery Enhancement vs supportive group therapy for co-occurring opioid misuse and chronic pain in primary care: A randomized clinical trial. JAMA Intern Med 2022; 182:407–417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rogers C: Client-centered therapy: Its current practice, implications, and theory. New York, Constable, 2003 [Google Scholar]
- 16.Garland EL, Manusov EG, Froeliger B, et al. : Mindfulness-oriented recovery enhancement for chronic pain and prescription opioid misuse: results from an early-stage randomized controlled trial. J Consult Clin Psychol 2014; 82:448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gaylord SA, Palsson OS, Garland EL, et al. : Mindfulness training reduces the severity of irritable bowel syndrome in women: Results of a randomized controlled trial. Am J Gastroenterol 2011; 106:1678–1688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hanley AW, Garland EL: The Mindfulness-Oriented Recovery Enhancement Fidelity Measure (MORE-FM): Development and validation of a new tool to assess therapist adherence and competence. J Evid-Based Soc Work 2020; manuscript accepted for publication [DOI] [PubMed] [Google Scholar]
- 19.Cleeland CS, Ryan KM: Pain assessment: Global use of the Brief Pain Inventory. Ann Acad Med Singap 1994; 23:129–138 [PubMed] [Google Scholar]
- 20.Butler SF, Budman SH, Fernandez KC, et al. : Development and validation of the Current Opioid Misuse Measure. Pain 2007; 130:144–56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wu SM, Compton P, Bolus R, et al. : The addiction behaviors checklist: validation of a new clinician-based measure of inappropriate opioid use in chronic pain. J Pain Symptom Manage 2006; 32:342–351 [DOI] [PubMed] [Google Scholar]
- 22.Dowell D, Haegerich TM, Chou R: CDC guideline for prescribing opioids for chronic pain—United States, 2016. Jama 2016; 315:1624–1645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fals-Stewart W, O’Farrell TJ, Freitas TT, et al. : The Timeline Followback reports of psychoactive substance use by drug-abusing patients: Psychometric properties. J Consult Clin Psychol J Consult Clin Psychol 2000; 68:134. [DOI] [PubMed] [Google Scholar]
- 24.Beaufort IN, De Weert-Van Oene GH, Buwalda VAJ, et al. : The Depression, Anxiety and Stress Scale (DASS-21) as a screener for depression in substance use disorder inpatients: a pilot study. Eur Addict Res 2017; 23:260–268 [DOI] [PubMed] [Google Scholar]
- 25.Blanchard EB, Jones-Alexander J, Buckley TC, et al. : Psychometric properties of the PTSD checklist (PCL). Behav Res Ther 1996; 34:669–673 [DOI] [PubMed] [Google Scholar]
- 26.Rosenstiel AK, Keefe FJ: The use of coping strategies in chronic low back pain patients: Relationship to patient characteristics and current adjustment. Pain 1983; 17:33–44 [DOI] [PubMed] [Google Scholar]
- 27.Snaith RP, Hamilton M, Morley S, et al. : A scale for the assessment of hedonic tone the Snaith–Hamilton Pleasure Scale. Br J Psychiatry 1995; 167:99–103 [DOI] [PubMed] [Google Scholar]
- 28.Watson D, Clark LA, Tellegen A: Development and validation of brief measures of positive and negative affect: The PANAS scales. J Pers Soc Psychol 1988; 54:1063. [DOI] [PubMed] [Google Scholar]
- 29.Noguchi K, Gohm CL, Dalsky DJ: Cognitive tendencies of focusing on positive and negative information. J Res Personal 2006; 40:891–910 [Google Scholar]
- 30.Gross JJ, John OP: Individual differences in two emotion regulation processes: implications for affect, relationships, and well-being. J Pers Soc Psychol 2003; 85:348. [DOI] [PubMed] [Google Scholar]
- 31.Jose PE, Lim BT, Bryant FB: Does savoring increase happiness? A daily diary study. J Posit Psychol 2012; 7:176–187 [Google Scholar]
- 32.Garland EL, Roberts RL, Hanley AW, et al. : The Mindful Reappraisal of Pain Scale (MRPS): Validation of a New Measure of Psychological Mechanisms of Mindfulness-Based Analgesia. Mindfulness 2022; 1–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Baer RA, Smith GT, Hopkins J, et al. : Using self-report assessment methods to explore facets of mindfulness. Assessment 2006; 13:27–45 [DOI] [PubMed] [Google Scholar]
- 34.MacLean RR, Sofuoglu M, Brede E, et al. : Attentional bias in opioid users: A systematic review and meta-analysis. Drug Alcohol Depend 2018; 191:270–278 [DOI] [PubMed] [Google Scholar]
- 35.Liu GF, Lu K, Mogg R, et al. : Should baseline be a covariate or dependent variable in analyses of change from baseline in clinical trials? Stat Med 2009; 28:2509–2530 [DOI] [PubMed] [Google Scholar]
- 36.Coffman CJ, Edelman D, Woolson RF: To condition or not condition? Analysing ‘change’in longitudinal randomised controlled trials. BMJ Open 2016; 6:e013096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lappan SN, Brown AW, Hendricks PS: Dropout rates of in-person psychosocial substance use disorder treatments: a systematic review and meta-analysis. Addiction 2020; 115:201–217 [DOI] [PubMed] [Google Scholar]
- 38.Graham JW: Missing data analysis: Making it work in the real world. Annu Rev Psychol 2009; 60:549–576 [DOI] [PubMed] [Google Scholar]
- 39.Field M, Cox W: Attentional bias in addictive behaviors: A review of its development, causes, and consequences. Drug Alcohol Depend 2008; 97:1–20 [DOI] [PubMed] [Google Scholar]
- 40.Garland EL, Atchley RM, Hanley AW, et al. : Mindfulness-Oriented Recovery Enhancement remediates hedonic dysregulation in opioid users: Neural and affective evidence of target engagement. Sci Adv 2019; 5:eaax1569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Garland EL, Hanley AW, Hudak J, et al. : Mindfulness-induced endogenous theta stimulation occasions self-transcendence and inhibits addictive behavior. Sci Adv 2022; 8:eabo4455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Haight BR, Learned SM, Laffont CM, et al. : Efficacy and safety of a monthly buprenorphine depot injection for opioid use disorder: a multicentre, randomised, double-blind, placebo-controlled, phase 3 trial. The Lancet 2019; 393:778–790 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.